Applying Structural Equation Modelling to Understand the Implementation of Social Distancing in the Professional Lives of Healthcare Workers
Abstract
1. Introduction
1.1. Need for and Objectives of the Study
- To explore the contemporary dilemma of how to satisfy the calls of policy implementation researchers with sound theoretical support and quantitative research design.
- To develop guidance for other low and middle-income countries by identifying the weak areas in order to normalize and ultimately implement healthcare intervention as a novel and complex intervention and address translational gaps.
2. Previous Research on Healthcare Intervention and SD
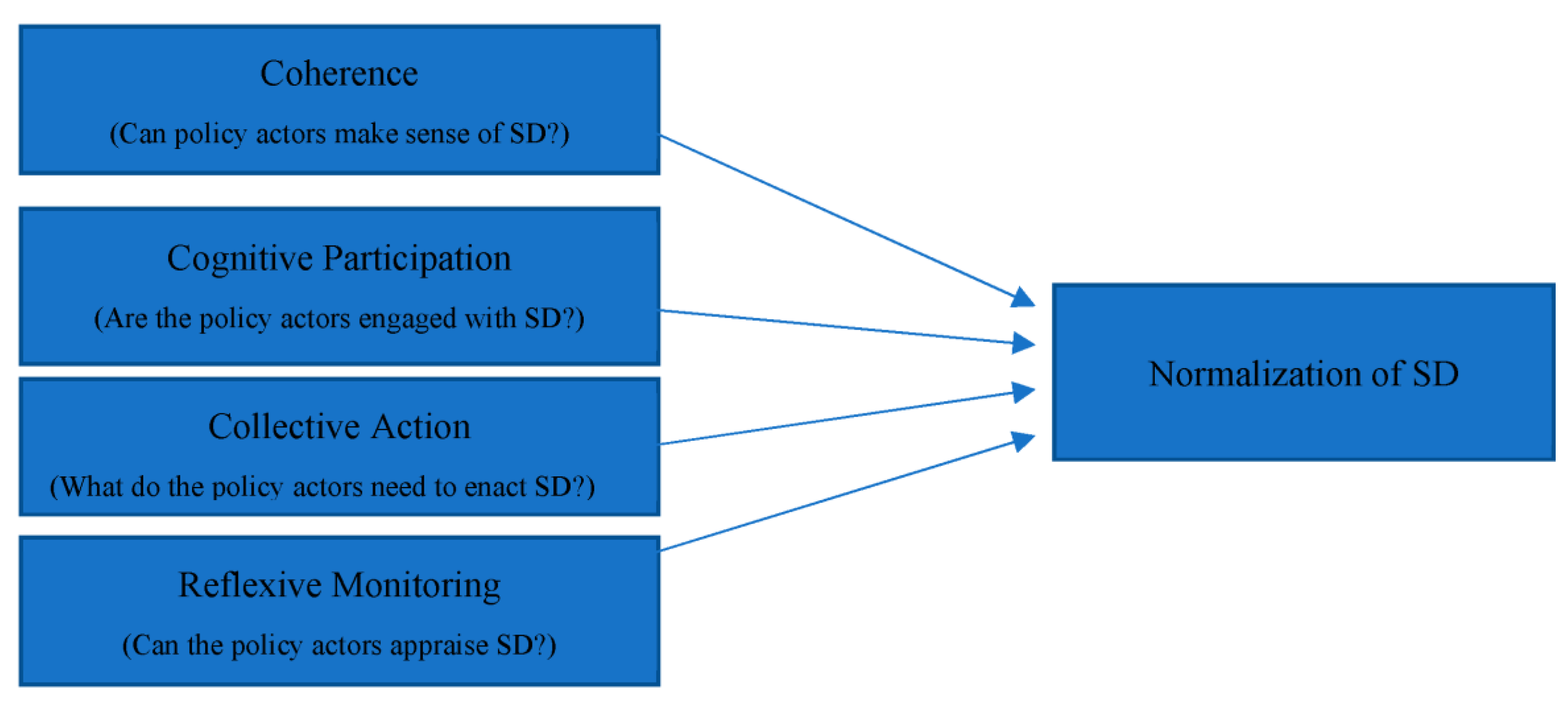
3. Theoretical Model
4. Hypothesis Development
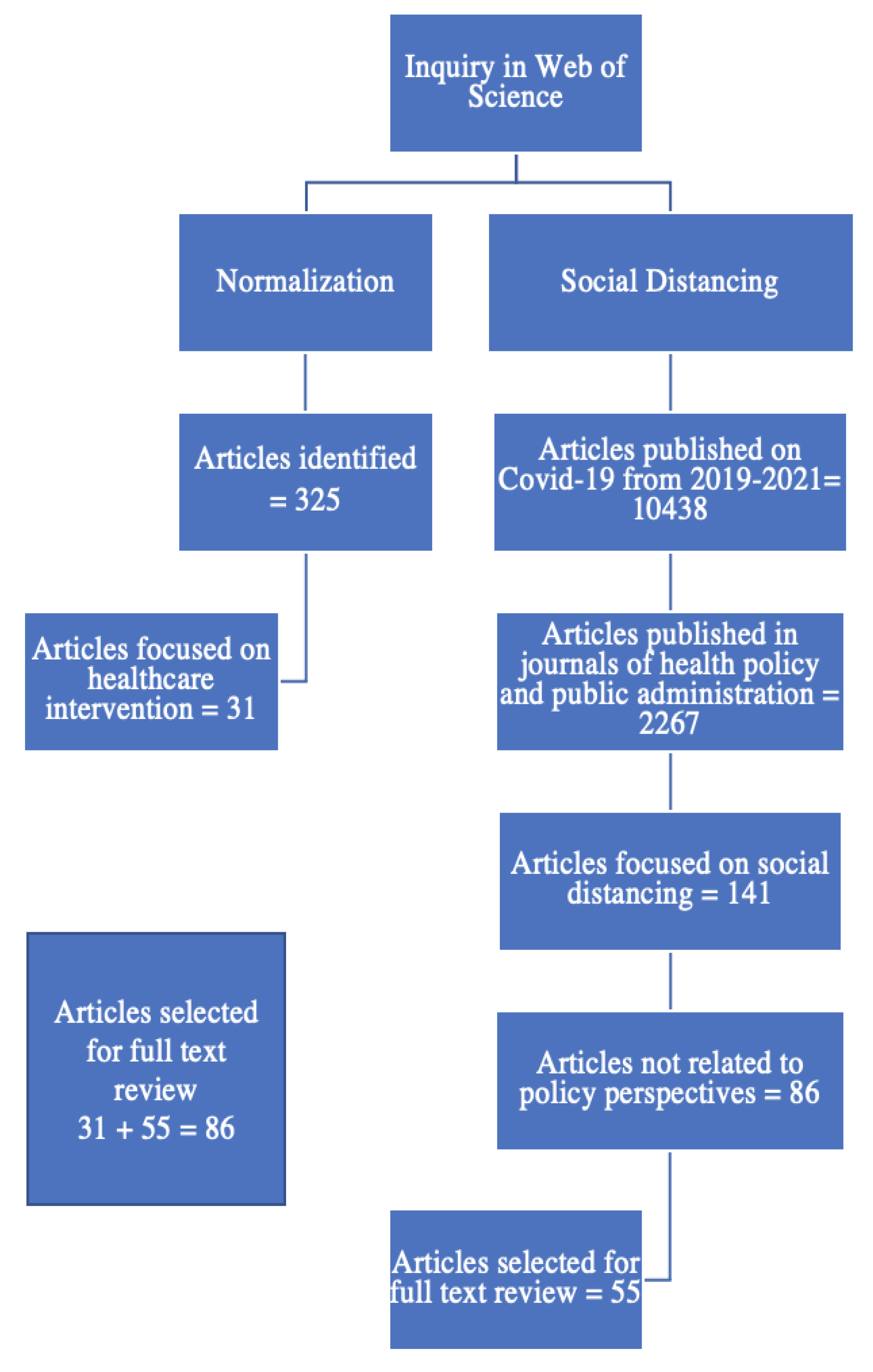
5. Methods and Data
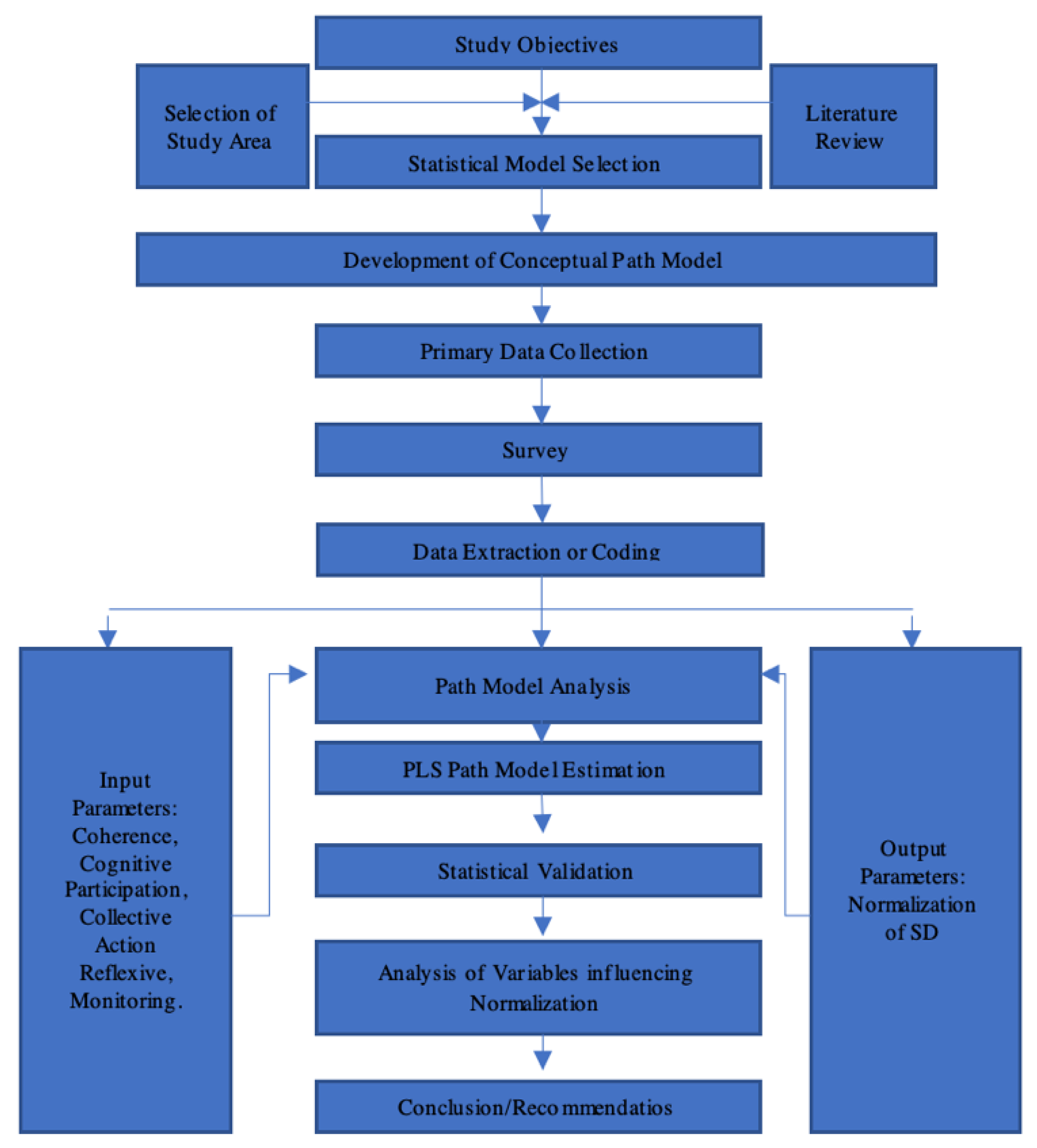
5.1. Research Design
5.2. Ethical Procedures Statement
5.3. Research Instrument
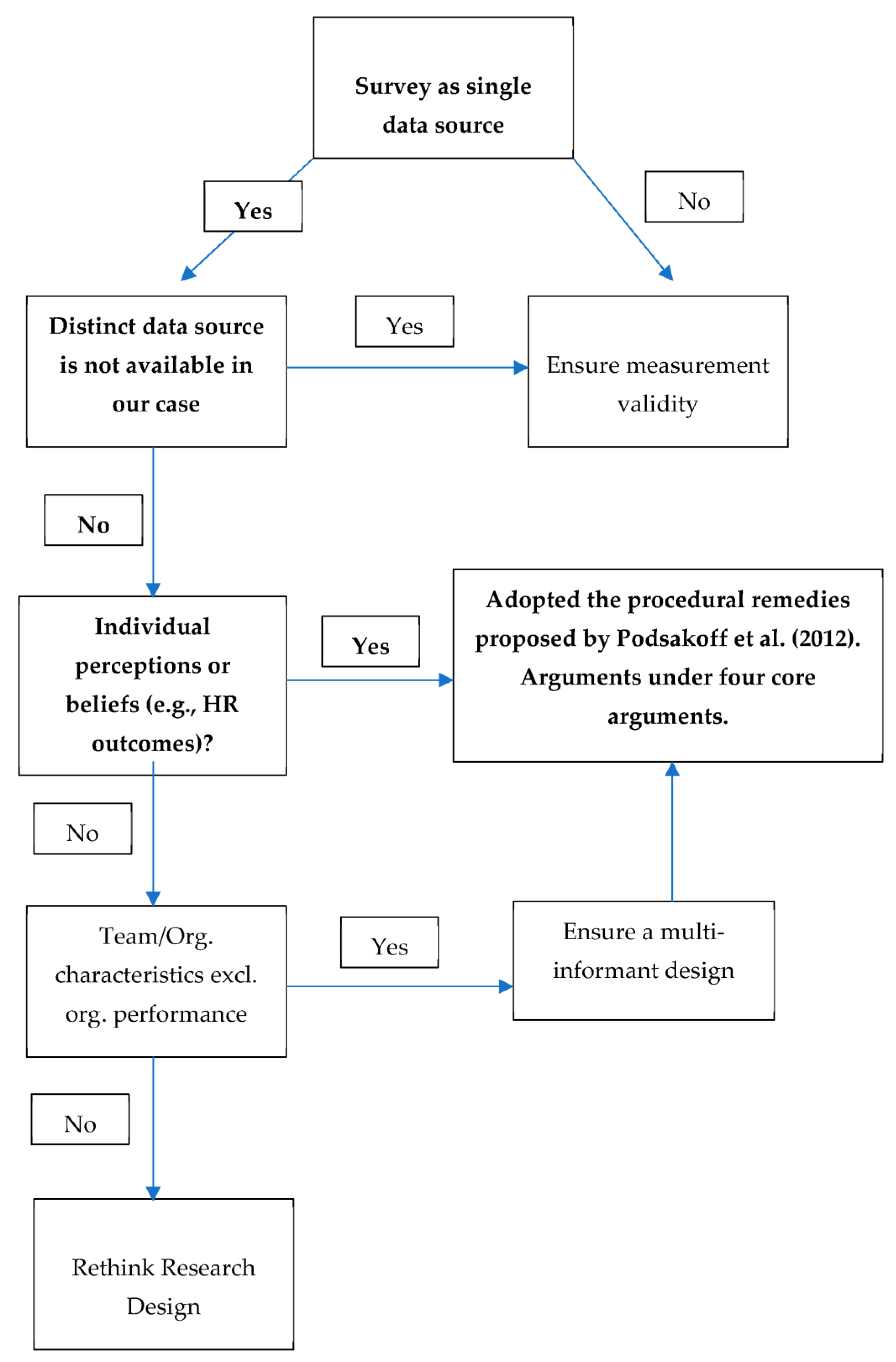
5.4. Common Source Bias
5.5. Justification of Research Instrument
5.6. Sampling
5.7. Data Coding and Collection
5.8. Testing Common Source Bias
5.9. Descriptive Statistics and ANOVA-Based Tests
5.10. Assumptions of Normality
5.11. Non-Parametric Analysis
5.12. Application of SEM
6. Results
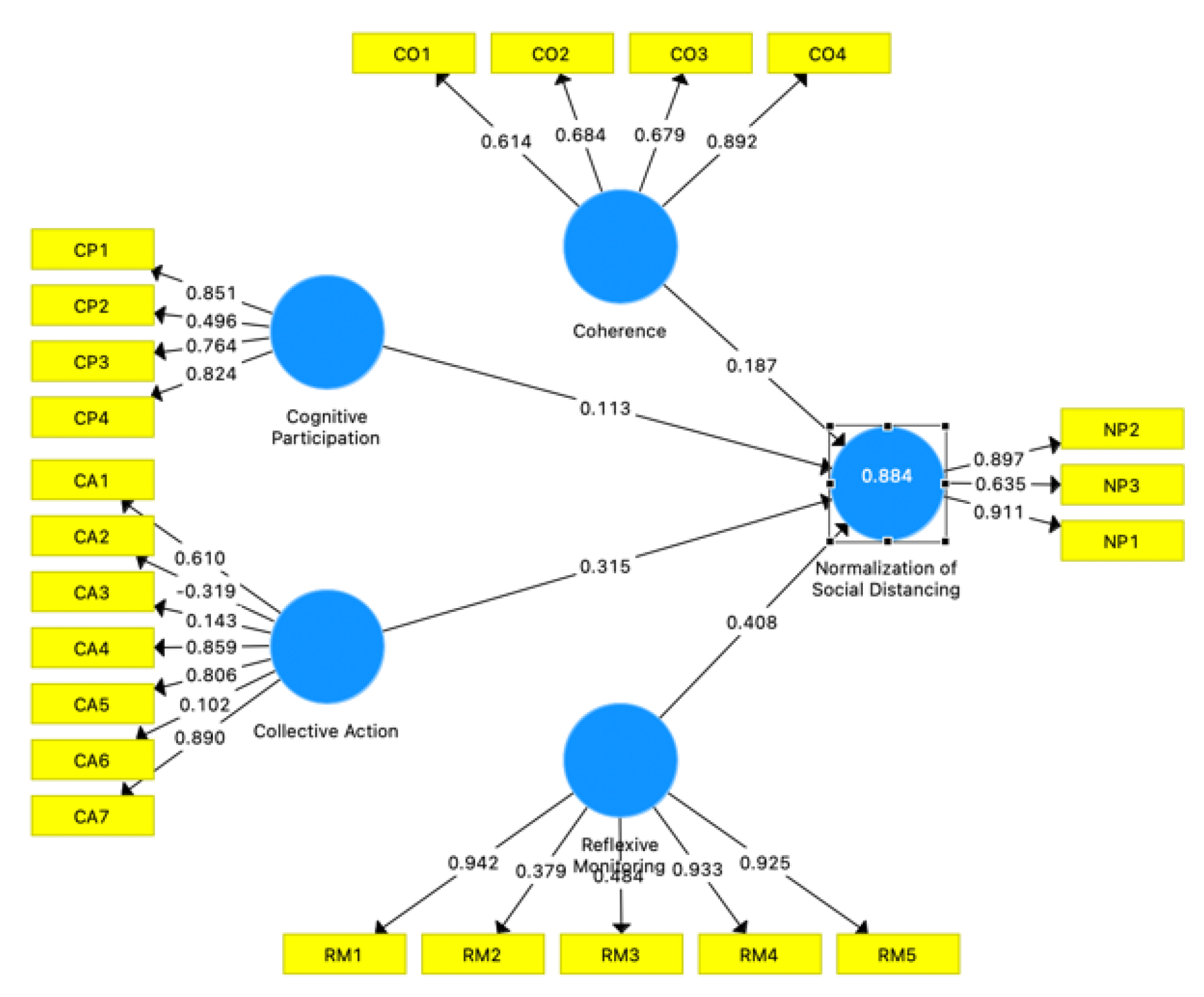
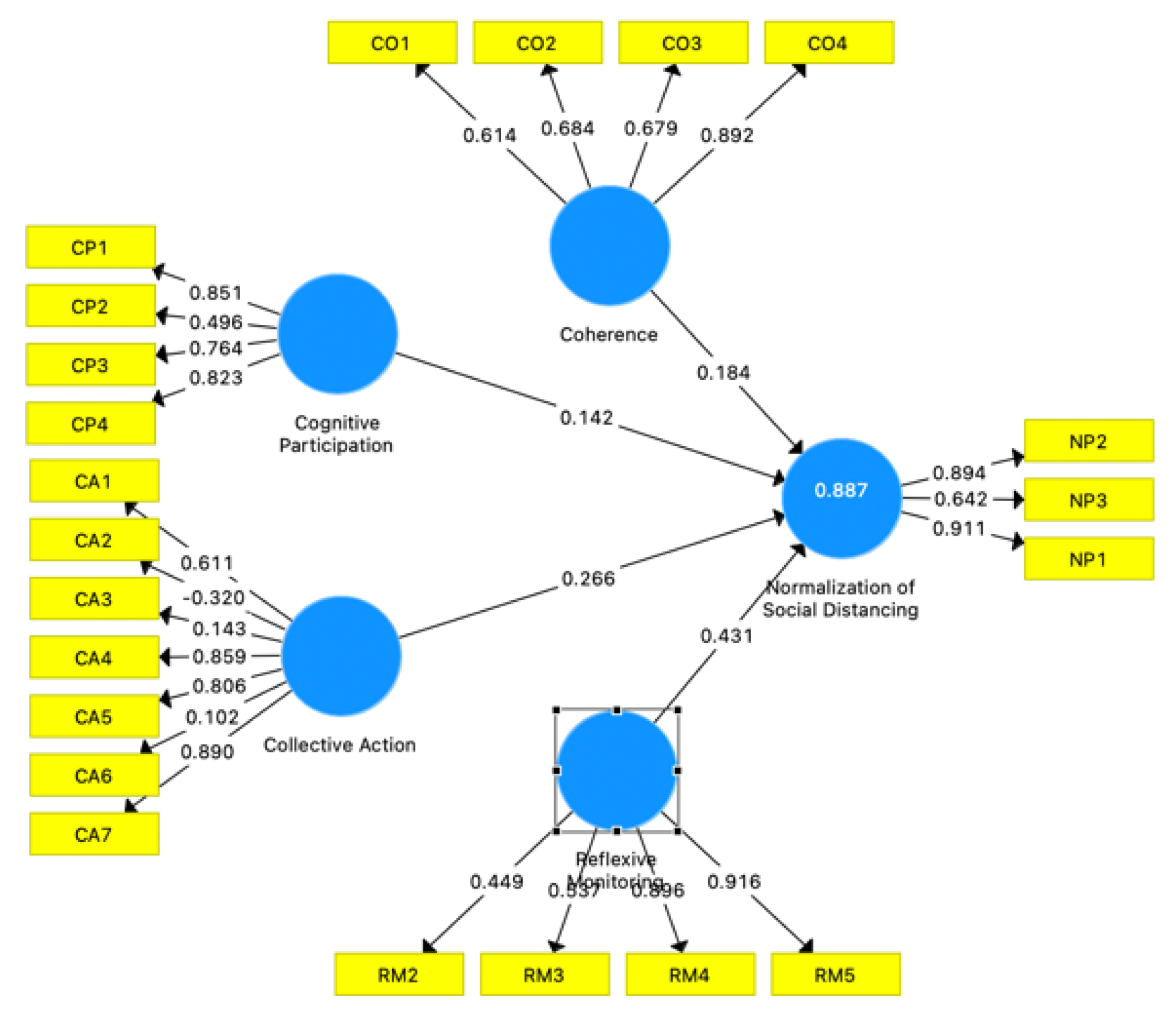
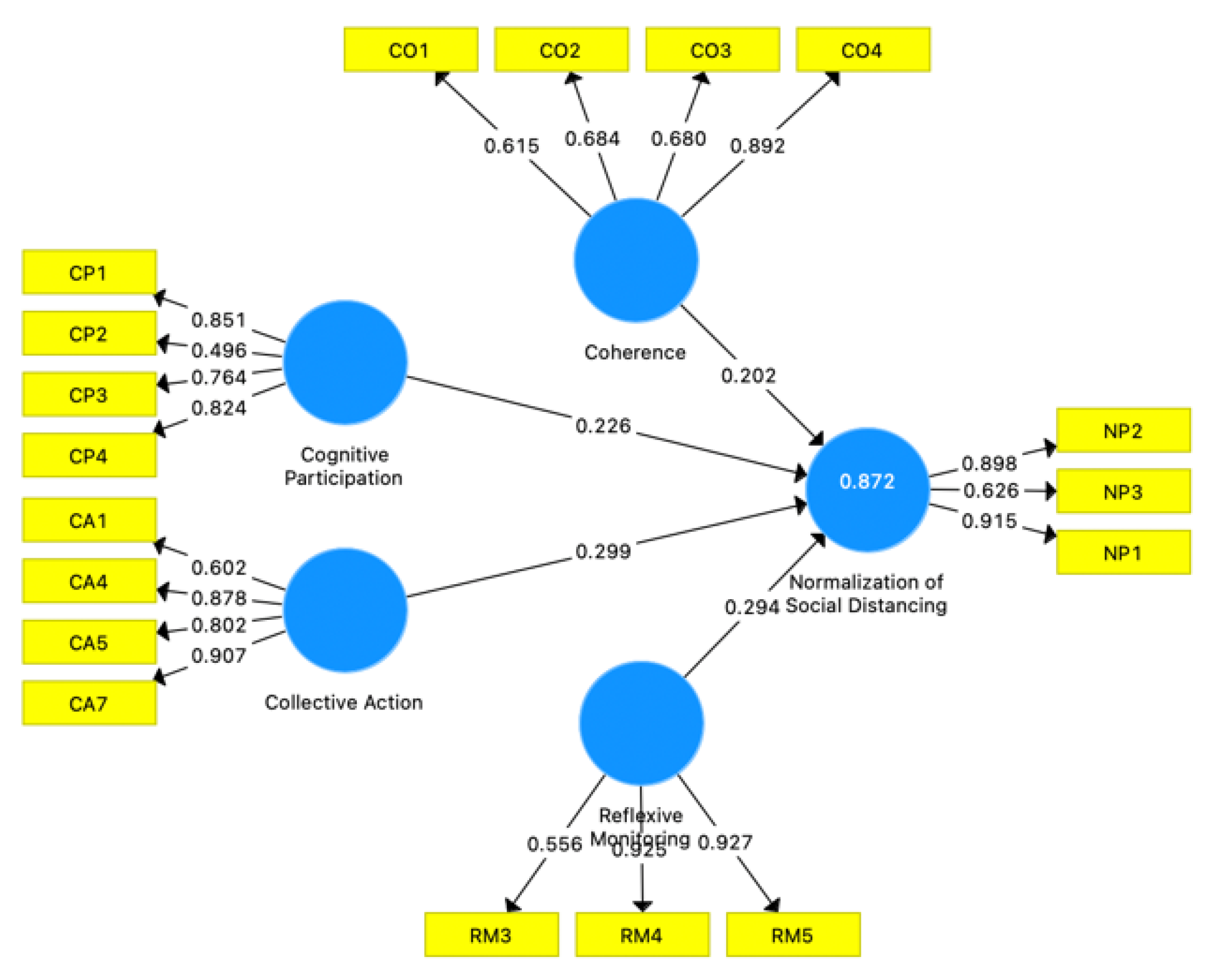
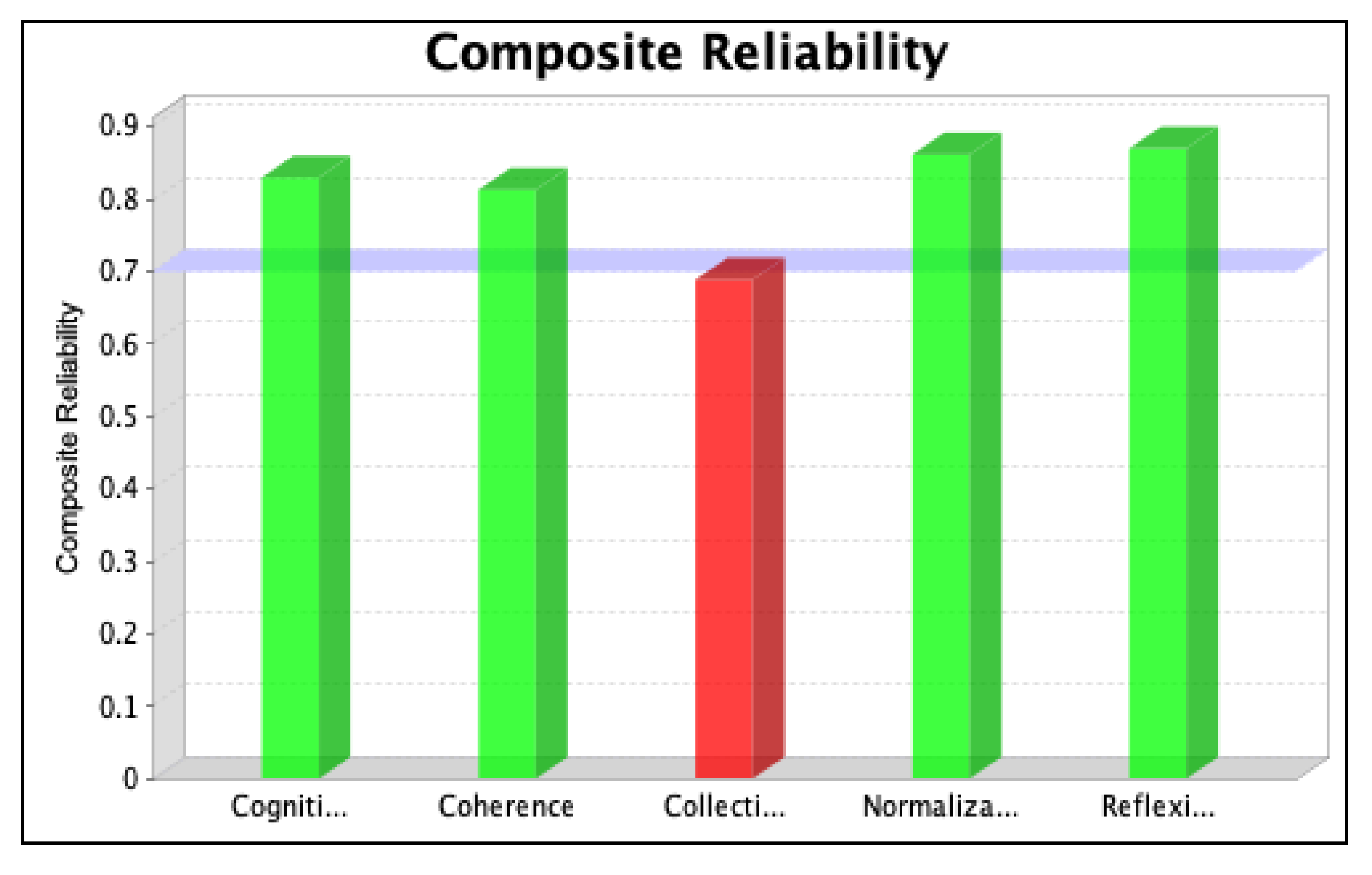
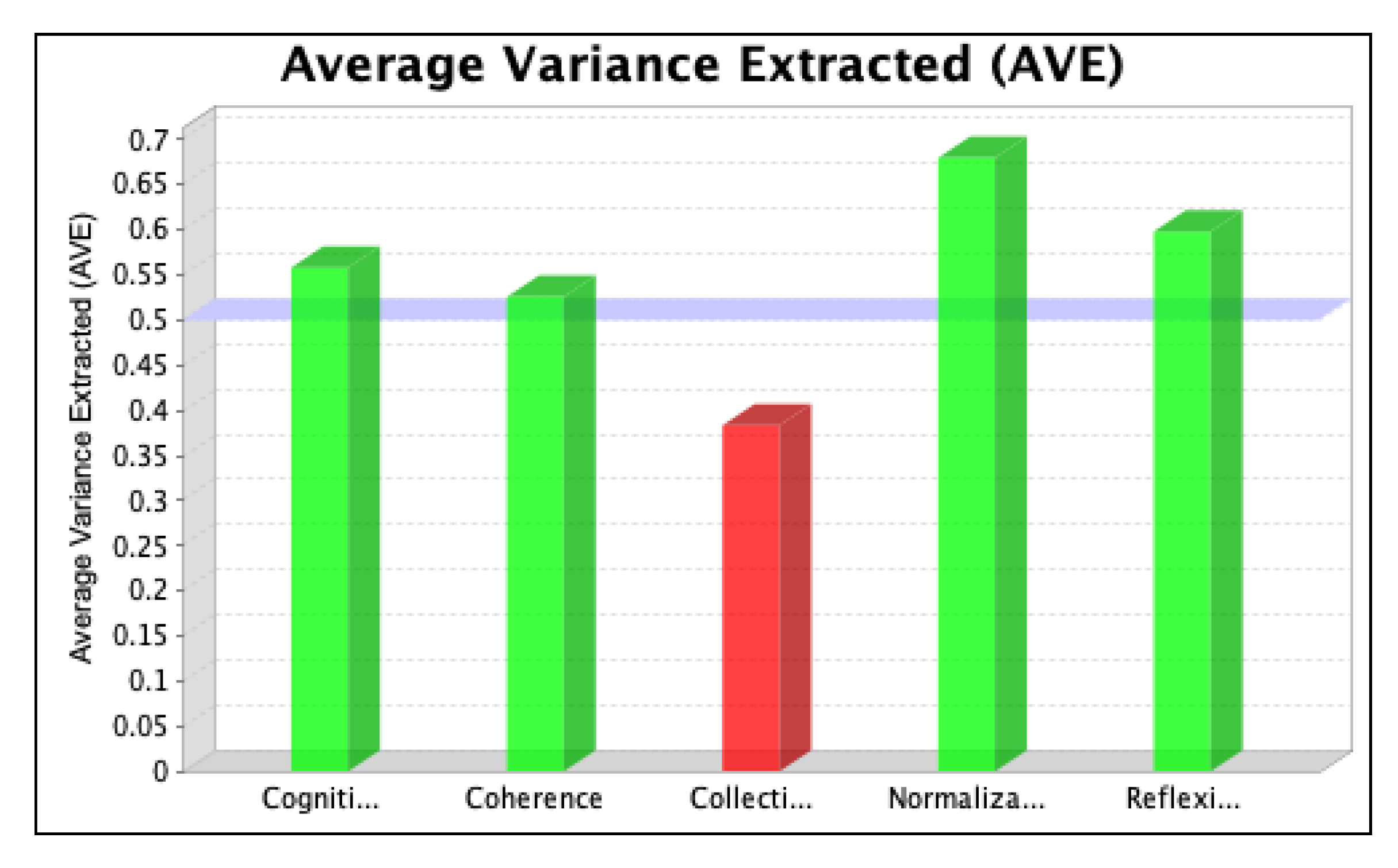
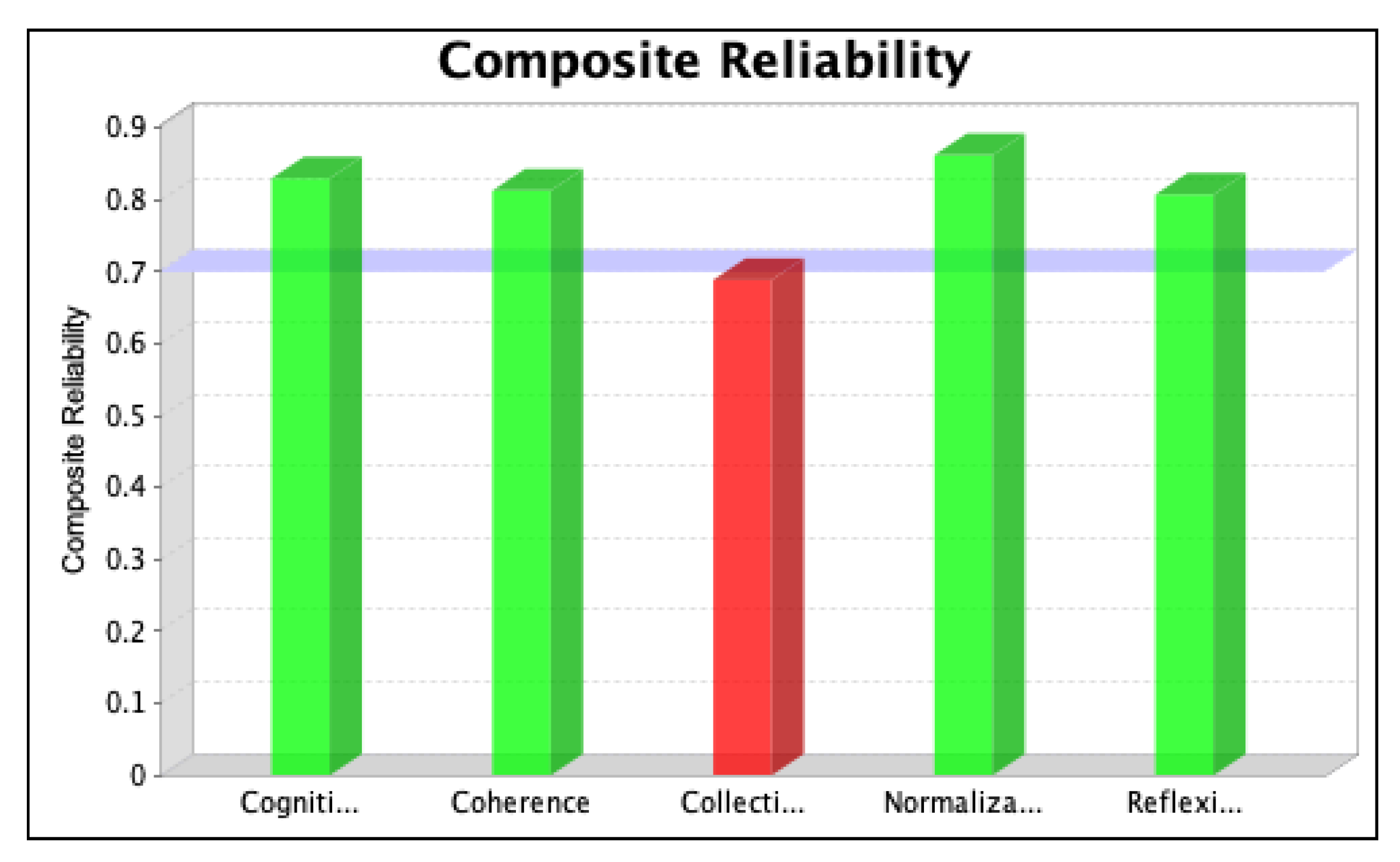
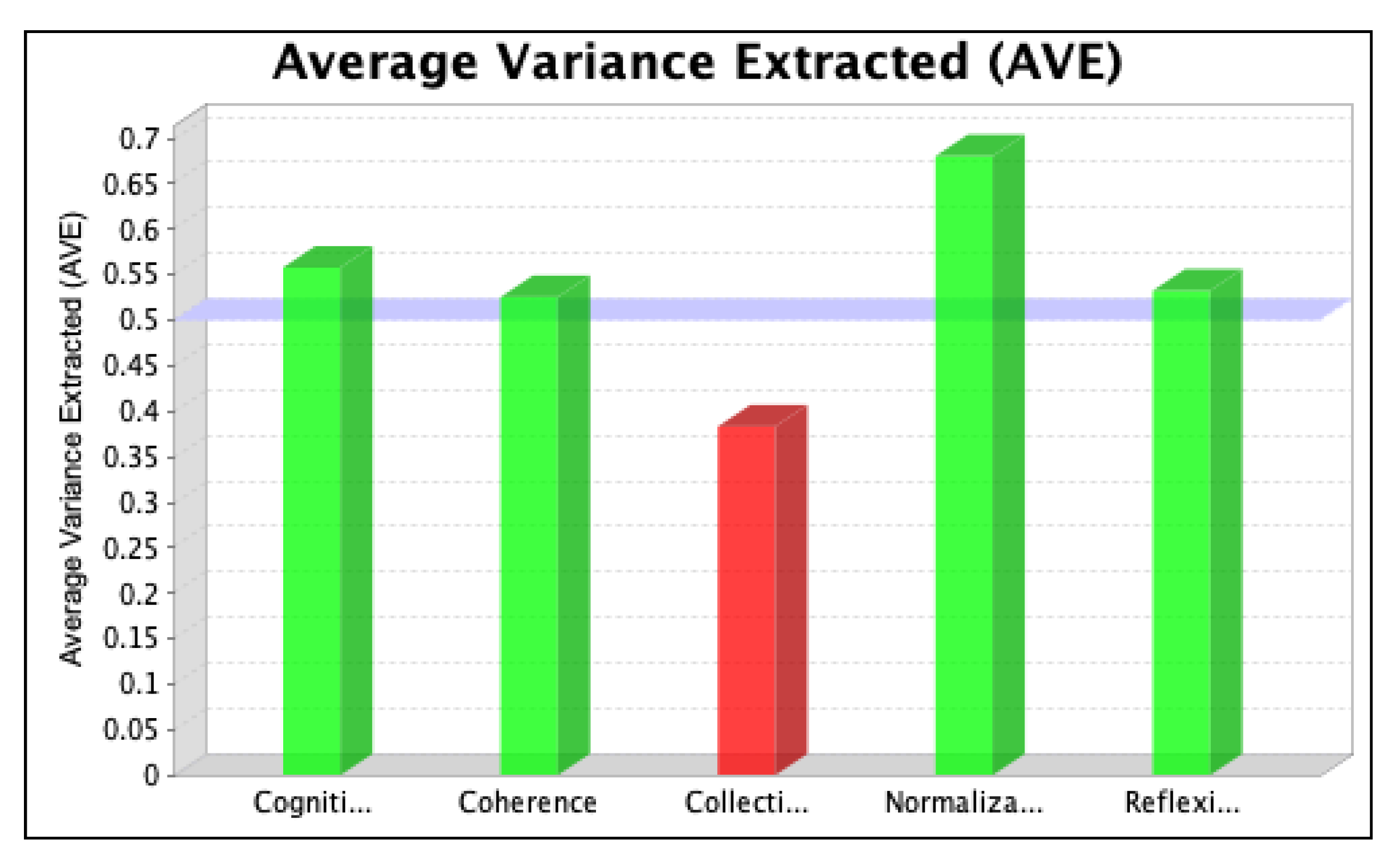
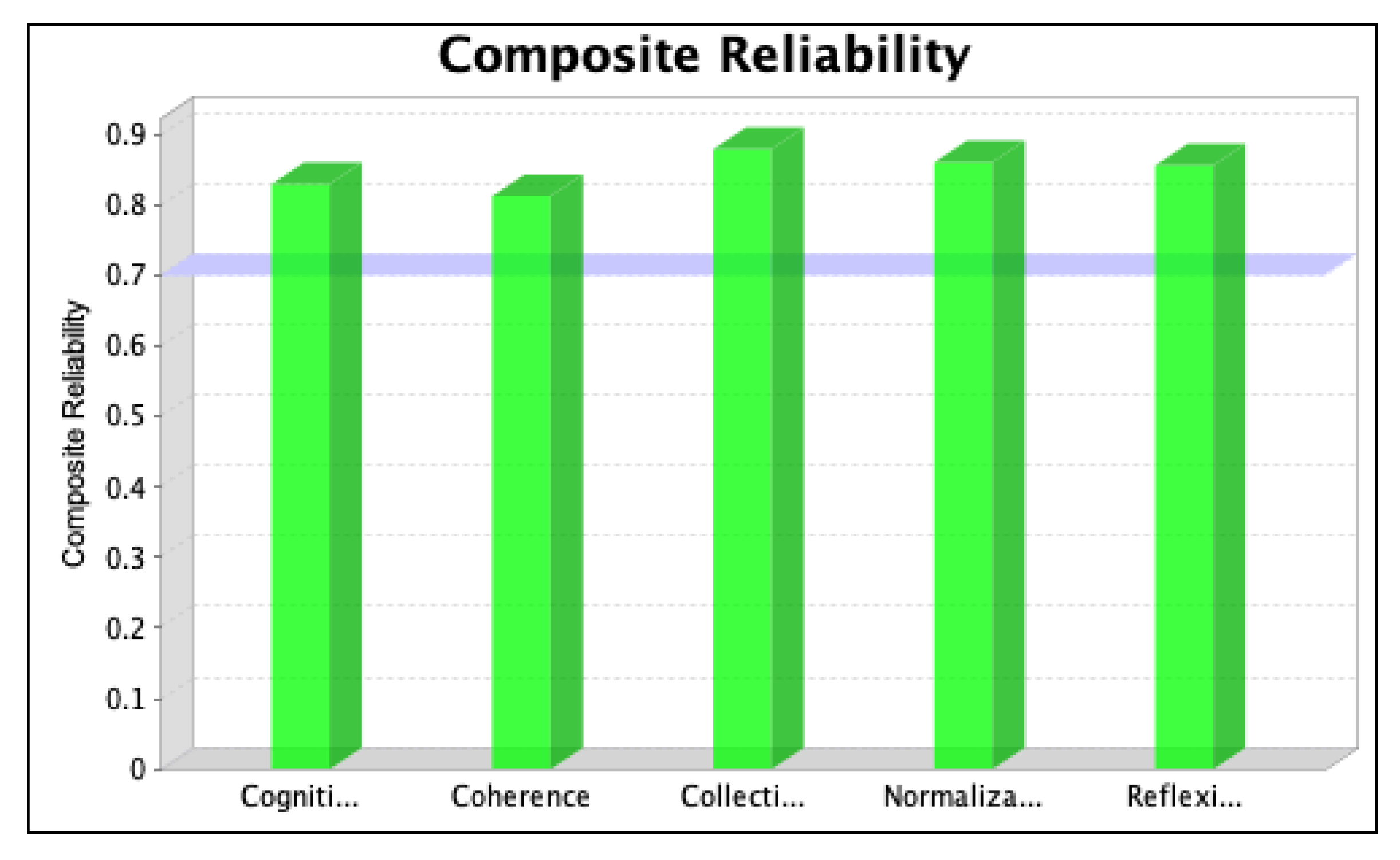
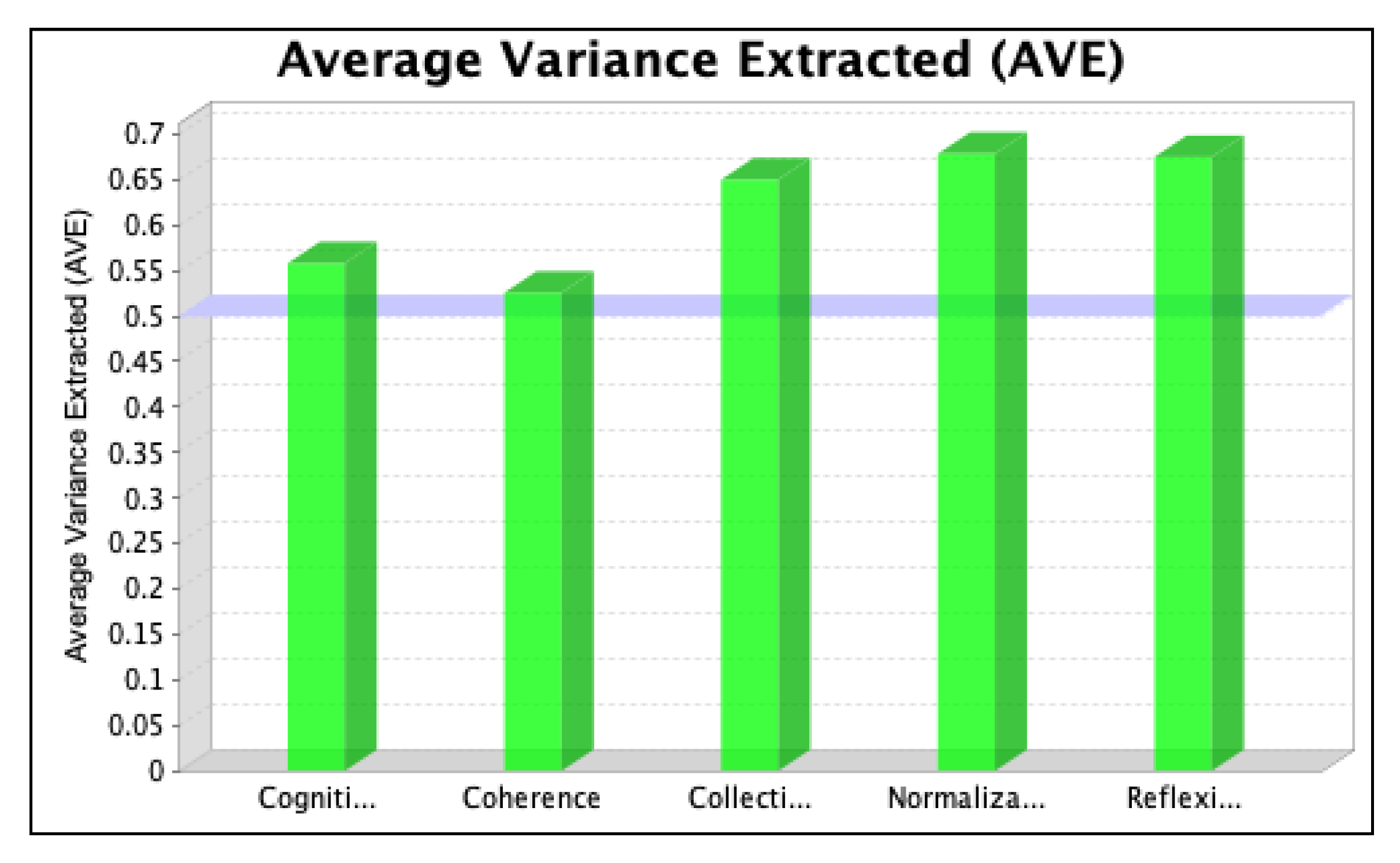
6.1. Individual Item Validity and Convergent Validity
6.2. Discriminant Validity
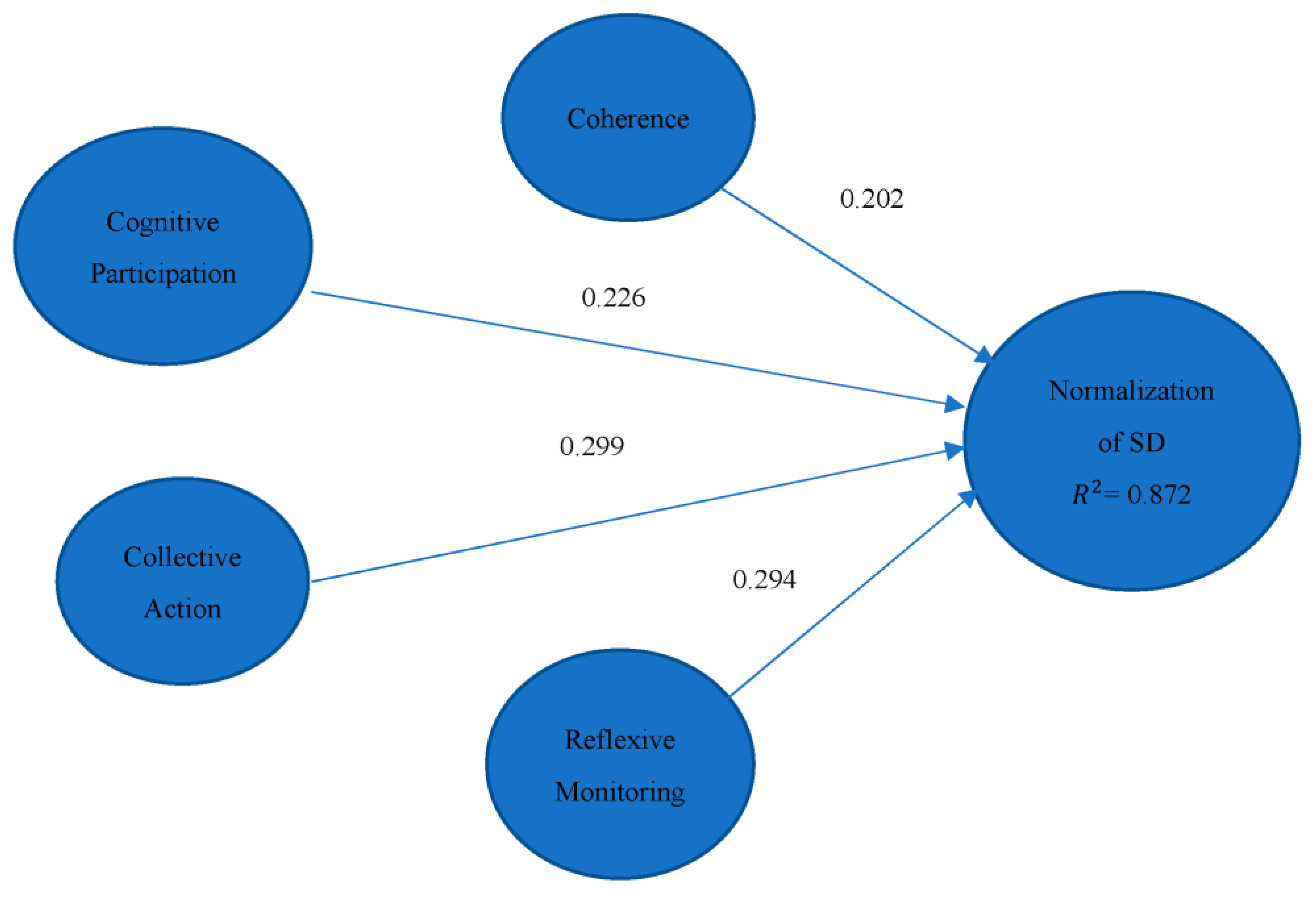
6.3. Structural Model Relationship
6.4. Overall Fitness of the Model
7. Discussion
7.1. Summary of Results
7.2. Discussion
7.3. Limitations of the Study
- NPT is a widely discussed theory in the policy implementation of the literature. The theory originated in a developed country, and limited evidence of its applicability in an LMIC is a limitation of this study.
- The application of NPT in a novel and complex situation such as COVID-19 is another limitation of the study.
- The study was conducted at the peak of COVID-19 infections, which greatly impacted the data collection activity regarding the number of responses.
7.4. Contribution of the Study
- The study explores a healthcare intervention’s implementation, contributing to the implementation literature.
- The study explores how SD is normalized in healthcare workers’ professional lives, ultimately contributing to the normalization literature.
- The study applies NPT in the unique and complex situation of a healthcare crisis, and the results confirm the applicability of NPT. The study thereby validates the utility of the NPT in situations of a novel and complex nature.
- The study is the first attempt to understand the implementation–normalization of a healthcare intervention (SD) in a healthcare crisis according to a sound theory and multivariate statistical modelling to develop a basis for the policy learning of LMICs. The study results have policy implications which are detailed in the next section.
7.5. Implications of the Study
- Well-known and subtle gaps exist when translating research results into policy and practice [91], such as the know–do gap: the development and implementation of innovative healthcare interventions in practice with the intended users [92], such as, in our case, healthcare workers. Our study identifies loopholes in the implementation process by examining the normalization of an innovative healthcare intervention, addressing the know–do gap.
- Another well-known gap relates to the use of health research results to inform health policy [93]. The results of our study illustrate the weak coherence (sense-making) and cognitive participation (engagement) on the part of healthcare workers that should inform policy institutions to put more effort into the sense-making and engagement of healthcare workers in Pakistan. This can lead to stronger relationships among the latent variables and the implementation–normalization of a healthcare intervention.
- However, the think–do gap shows that the groups or individuals involved in the implementation should consider the nature and complexity of the implementation work to better inform their actions. Our study explores the implementation of a complex healthcare intervention through the resources they need to enact it and whether they can appraise it. The resources required and the outcome of the appraisal depend upon the nature and complexity of the intervention. Our study also provides an insight into the think–do gap while understanding the normalization of a complex healthcare intervention in the healthcare workers’ professional roles.
7.6. Future Research
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AVE | Average Variance Extracted |
| CA | Collective Action |
| Co | Coherence |
| CP | Cognitive Participation |
| CR | Composite Reliability |
| CSB | Common Source Bias |
| DHQ | District Headquarters Hospital |
| FJWH | Fatima Jinnah Women’s Hospital |
| GOF | Goodness of Fit |
| NMU | Nishtar Medical University |
| NoMAD | Normalization Measure Assessment |
| NPI | Nonpharmaceutical Intervention |
| NPT | Normalization Process Theory |
| RM | Reflexive Monitoring |
| SD | Social Distancing |
| SEM | Structural Equation Modelling |
| SPLS | Smart Partial Least Squares |
| WHO | World Health Organization |
Appendix A. Conceptualization
| Constructs | Previous Research | Operationalization |
|---|---|---|
| Coherence | Given in the literature review | Can policy actors make sense of SD? For strong coherence, there should be a shared understanding across the policy actors of what this work will entail for individuals. There should be a mutual understanding of the value and purpose of SD. |
| Cognitive Participation | Given in the literature review | Are the policy actors engaged with SD? There should be legitimate reasons and strong motivation for policy actors to engage with SD for strong cognitive participation. |
| Collective Action | Given in the literature review | What do the policy actors need to enact SD? For decisive collective action, there should be a shared understanding of the roles and responsibilities of policy actors, and required resources should be available. |
| Reflexive Monitoring | Given in the literature review | Can policy actors formally or informally appraise the impact of SD? There should be precise evaluation mechanisms for strong reflexive monitoring, and policy actors should be aware of the changes required to adopt SD. |
Appendix B. Data Collection
Survey Form
- Permission to use the survey instrument from the original authors was received and could be presented on demand.
- The updated survey instrument is available at the link: https://drive.google.com/drive/folders/1mbK8y_RZX3WvMxfJL6-xZ6tJKbhzpBBa?usp=sharing.
| NoMAD Quantitative Data Coding Framework | ||||
|---|---|---|---|---|
| Groups | Theme | Description | Code | |
| Respondents General Information | Organization | RI-1 | Nishter Medical University Hospital | 1 |
| Civil Hospital/DHQ | 2 | |||
| FJ Women Hospital, | 3 | |||
| Gender | RI-2 | Male | 1 | |
| Female | 2 | |||
| Age Groups | RI-3 | 21 years to 30 years | 1 | |
| 31 years to 40 years | 2 | |||
| Above 40 years | 3 | |||
| Education | RI-4 | Graduate | 1 | |
| Postgraduate | 2 | |||
| Designation | RI-5 | Charge Nurses, | 1 | |
| Consultant Medicine, | 2 | |||
| Dy Medical Superintendents, | 3 | |||
| Doctor-Medical Officer, | 4 | |||
| Doctor-Pathology, | 5 | |||
| Doctor-Post Graduate Registrar, | 6 | |||
| Doctor-Pulmonology, | 7 | |||
| Head Nurse, | 8 | |||
| Lab Technologist, | 9 | |||
| Male Nurse, | 10 | |||
| Member NCOC | 11 | |||
| Member PTC | 12 | |||
| Principal Medical Officer | 13 | |||
| Psychologist, | 14 | |||
| Respiratory Therapist/Technologist | 15 | |||
| Senior Respiratory Therapist | 16 | |||
| Senior Lab Technologist, | 17 | |||
| Senior Medical Officer, | 18 | |||
| Senior Registrar Pulmonology | 19 | |||
| Ward Registrar | 20 | |||
| Women Medical Officer | 21 | |||
| Theoretical Constructs | General Questions | GQ | First general question from the survey | GQ-1 |
| Second general question from the survey | GQ-2 | |||
| Third general question from the survey | GQ-3 | |||
| Normalization | N | The first question on normalization | NP-1 | |
| The second question on normalization | NP-2 | |||
| The third question on normalization | NP-3 | |||
| Coherence | CO | The first question on Coherence | CO-1 | |
| The second question on Coherence | CO-2 | |||
| The third question on Coherence | CO-3 | |||
| Fourth question on Coherence | CO-4 | |||
| Cognitive Participation | CP | The first question on Cognitive Participation | CP-1 | |
| The second question on Cognitive participation | CP-2 | |||
| The third question on Cognitive participation | CP-3 | |||
| Fourth question on Cognitive Participation | CP-4 | |||
| Collective Action | CA | The first question on Collective Action | CA-1 | |
| The second question on Collective Action | CA-2 | |||
| The third question on Collective Action | CA-3 | |||
| The fourth question on Collective Action | CA-3 | |||
| The fifth question on Collective Action | CA-5 | |||
| The sixth question on Collective Action | CA-6 | |||
| The seventh question on Collective Action | CA-7 | |||
| Reflexive Monitoring | RM | The first question of Reflexive Monitoring | RM-1 | |
| The second question of Reflexive monitoring | RM-2 | |||
| The third question of Reflexive monitoring | RM-3 | |||
| The fourth question of Reflexive monitoring | RM-4 | |||
| The fifth question of Reflexive Monitoring | RM-5 | |||
| Level of Response | Strongly agree | 1 | ||
| Agree | 2 | |||
| Neither Agree nor Disagree | 3 | |||
| Disagree | 4 | |||
| Strongly Disagree | 5 | |||
| Not relevant to my role | 6 | |||
| Not relevant at this stage | 7 | |||
| Not relevant to the intervention | 8 | |||
| Groups | Theme | Description | Code | |
| Respondents General Information | Designation | RI-5 | Nurses (Charge Nurse, Head Nurse, Male Nurse) | 1 |
| Doctors (Consultant Medicine, Dy. Medical Superintendent, Medical Officer, Pathology, PGR, Pulmonology, Member NCOC, Member PTC, PMO, Senior Medical Officer, SR Pulmonology, Ward Registrar, WMO) | 2 | |||
| Allied Health Professional (Lab Technologist, Psychologist, Respiratory Therapist/Technologist, Senior Respiratory Therapist, Senior Lab Technologist) | 3 | |||
| Characteristics | NMU Hospital | DHQ Hospital | FJW Hospital | Total | % of Total Responses |
|---|---|---|---|---|---|
| Age Group: | |||||
| 21 years to 30 years | 100/132 | 66/85 | 53/71 | 219/288 | 76.04% |
| 31 years to 40 years | 30/132 | 17/85 | 17/71 | 64/288 | 22.22% |
| Above 40 years | 02/132 | 02/85 | 01/71 | 05/288 | 1.74% |
| Gender: | |||||
| Male | 68/132 | 40/85 | 4/71 | 112/288 | 38.89% |
| Female | 64/132 | 45/85 | 67/71 | 176/288 | 61.11% |
| Designations: | |||||
| Charge Nurses, | 30 | 15 | 15 | 60 | 20.833 |
| Consultant Medicine, | 2 | - | 1 | 3 | 1.041 |
| Dy Medical Superintendents, | 4 | 2 | 2 | 8 | 2.777 |
| Doctor-Medical Officer, | 28 | 28 | 1 | 57 | 19.791 |
| Doctor-Pathology, | 2 | 1 | 1 | 4 | 1.388 |
| Doctor-Post Graduate Registrar, | 12 | - | 9 | 21 | 7.291 |
| Doctor-Pulmonology, | 4 | 2 | 2 | 8 | 2.777 |
| Head Nurse, | 5 | 3 | 4 | 12 | 4.166 |
| Lab Technologist, | 2 | 1 | 1 | 4 | 1.388 |
| Male Nurse, | 8 | 4 | - | 12 | 4.166 |
| Member NCOC | - | - | - | 1 | 0.347 |
| Member PTC | - | - | - | - | 0% |
| Principal Medical Officer | - | 1 | - | - | 0% |
| Psychologist, | 3 | 3 | 2 | 8 | 2.777 |
| Respiratory Therapist/Technologist | 7 | 4 | - | 11 | 3.819 |
| Senior Respiratory Therapist | 1 | - | - | 1 | 0.347 |
| Senior Lab Technologist, | 3 | 1 | - | 4 | 1.388 |
| Senior Medical Officer, | 4 | 2 | 2 | 8 | 2.777 |
| Senior Registrar Pulmonology | 2 | 1 | 1 | 4 | 1.388 |
| Women Medical Officer | 15 | 17 | 30 | 62 | 21.527 |
| Total | 132 | 85 | 71 | 288 |
Appendix C. Tests
| Total Variance Explained | ||||||
|---|---|---|---|---|---|---|
| Factor | Initial Eigenvalues | Extraction Sums of Squared Loadings | ||||
| Total | % of Variance | Cumulative % | Total | % of Variance | Cumulative % | |
| 1 | 10.052 | 43.706 | 43.706 | 9.679 | 42.084 | 42.084 |
| 2 | 1.857 | 8.076 | 51.782 | |||
| 3 | 1.825 | 7.937 | 59.718 | |||
| 4 | 1.464 | 6.364 | 66.082 | |||
| 5 | 1.100 | 4.783 | 70.865 | |||
| 6 | 0.988 | 4.297 | 75.162 | |||
| 7 | 0.890 | 3.869 | 79.031 | |||
| 8 | 0.769 | 3.344 | 82.375 | |||
| 9 | 0.684 | 2.974 | 85.349 | |||
| 10 | 0.563 | 2.448 | 87.797 | |||
| 11 | 0.536 | 2.330 | 90.127 | |||
| 12 | 0.471 | 2.049 | 92.175 | |||
| 13 | 0.425 | 1.849 | 94.024 | |||
| 14 | 0.343 | 1.491 | 95.515 | |||
| 15 | 0.304 | 1.323 | 96.837 | |||
| 16 | 0.238 | 1.033 | 97.870 | |||
| 17 | 0.179 | 0.779 | 98.650 | |||
| 18 | 0.097 | 0.423 | 99.073 | |||
| 19 | 0.073 | 0.319 | 99.392 | |||
| 20 | 0.056 | 0.241 | 99.633 | |||
| 21 | 0.049 | 0.214 | 99.847 | |||
| 22 | 0.025 | 0.110 | 99.958 | |||
| 23 | 0.010 | 0.042 | 100.000 | |||
| Case Processing Summary | |||||||
| Gender | Cases | ||||||
| Valid | Missing | Total | |||||
| N | Percent | N | Percent | N | Percent | ||
| Normality | Male | 112 | 100.0% | 0 | 0.0% | 112 | 100% |
| Female | 176 | 100.0% | 0 | 0.0% | 176 | 100% | |
| Tests of Normality | |||||||
| Gender | Kolmogorov–Smirnov a | Shapiro–Wilk b | |||||
| Statistic | df | Sig. | Statistic | df | Sig | ||
| Male | 0.194 | 112 | 0.000 | 0.877 | 112 | 0.000 | |
| Female | 0.229 | 176 | 0.000 | 0.848 | 176 | 0.000 | |
| Case Processing Summary | |||||||
| Education | Cases | ||||||
| Valid | Missing | Total | |||||
| N | Percent | N | Percent | N | Percent | ||
| Normality | Graduate | 220 | 100.0% | 0 | 0.0% | 220 | 100% |
| Post-Graduate | 68 | 100.0% | 0 | 0.0% | 68 | 100% | |
| Tests of Normality | |||||||
| Education | Kolmogorov–Smirnov a | Shapiro–Wilk b | |||||
| Statistic | df | Sig. | Statistic | df | Sig | ||
| Male | 0.236 | 220 | 0.000 | 0.829 | 220 | 0.000 | |
| Female | 0.170 | 68 | 0.000 | 0.889 | 68 | 0.000 | |
| Case Processing Summary | |||||||
| Age | Cases | ||||||
| Valid | Missing | Total | |||||
| N | Percent | N | Percent | N | Percent | ||
| Normality | 21–30 | 220 | 100.0% | 0 | 0.0% | 220 | 100% |
| 31–40 | 64 | 100.0% | 0 | 0.0% | 64 | 100% | |
| 40 and above | 4 | 100.0% | 0 | 0.0% | 4 | 100% | |
| Tests of Normality | |||||||
| Age | Kolmogorov–Smirnov a | Shapiro–Wilk b | |||||
| Statistic | df | Sig. | Statistic | df | Sig | ||
| Male | 0.213 | 220 | 0.000 | 0.860 | 220 | 0.000 | |
| Female | 0.241 | 64 | 0.000 | 0.845 | 64 | 0.000 | |
| 0.283 | 4 | 0.000 | 0.863 | 4 | 0.272 | ||
| Case Processing Summary | |||||||
| Organization | Cases | ||||||
| Valid | Missing | Total | |||||
| N | Percent | N | Percent | N | Percent | ||
| Normality | NMU | 131 | 100.0% | 0 | 0.0% | 131 | 100% |
| DHQ | 85 | 100.0% | 0 | 0.0% | 85 | 100% | |
| FJWH | 72 | 100.0% | 0 | 0.0% | 72 | 100% | |
| Tests of Normality | |||||||
| Organization | Kolmogorov–Smirnov a | Shapiro–Wilk b | |||||
| Statistic | df | Sig. | Statistic | Df | Sig | ||
| NMU | 0.245 | 131 | 0.000 | 0.846 | 131 | 0.000 | |
| DHQ | 0.242 | 85 | 0.000 | 0.827 | 85 | 0.000 | |
| FJWH | 0.156 | 72 | 0.000 | 0.901 | 72 | 0.000 | |
| Case Processing Summary | |||||||
| Designation | Cases | ||||||
| Valid | Missing | Total | |||||
| N | Percent | N | Percent | N | Percent | ||
| Normality | Nurses | 85 | 100.0% | 0 | 0.0% | 85 | 100% |
| Doctors | 176 | 100.0% | 0 | 0.0% | 176 | 100% | |
| AHP | 27 | 100.0% | 0 | 0.0% | 27 | 100% | |
| Tests of Normality | |||||||
| Designation | Kolmogorov–Smirnov a | Shapiro–Wilk b | |||||
| Statistic | df | Sig. | Statistic | Df | Sig | ||
| Nurses | 0.308 | 85 | 0.000 | 0.693 | 85 | 0.000 | |
| Doctors | 0.163 | 176 | 0.000 | 0.891 | 176 | 0.000 | |
| AHP | 0.301 | 27 | 0.000 | 0.784 | 27 | 0.000 | |
| Hypothesis Test Summary | ||||
|---|---|---|---|---|
| Null Hypothesis | Test | Significance | Decision | |
| 1 | The distribution of the normalization of SD is the same across the categories of the gender | Independent-Samples Mann–Whitney U Test | 0.038 | Reject the null hypothesis |
| Asymptotic significances are displayed. The significance level is 0.05. | ||||
| Hypothesis Test Summary | ||||
| Null Hypothesis | Test | Significance | Decision | |
| 1 | The distribution of the normalization of SD is the same across the categories of education | Independent-Samples Mann–Whitney U Test | 0.034 | Reject the null hypothesis |
| Asymptotic significances are displayed. The significance level is 0.05. | ||||
| Hypothesis Test Summary | ||||
| Null Hypothesis | Test | Significance | Decision | |
| 1 | The distribution of the normalization of SD is the same across the categories of age | Independent-Samples Kruskal–Wallis Test | 0.672 | Retain the null hypothesis |
| Asymptotic significances are displayed. The significance level is 0.05. | ||||
| Hypothesis Test Summary | ||||
| Null Hypothesis | Test | Significance | Decision | |
| 1 | The distribution of the normalization of SD is the same across the categories of the organization | Independent-Samples Kruskal–Wallis Test | 0.030 | Reject the null hypothesis |
| Asymptotic significances are displayed. The significance level is 0.05. | ||||
| Hypothesis Test Summary | ||||
| Null Hypothesis | Test | Significance | Decision | |
| 1 | The distribution of the normalization of SD is the same across the categories of designation | Independent-Samples Kruskal–Wallis Test | 0.001 | Reject the null hypothesis |
| Collinearity Statistics | |||
|---|---|---|---|
| Outer VIF Values | |||
| Items | 1st Iteration | 2nd Iteration | 3rd Iteration |
| Value | Value | Value | |
| NP1 | 2214 | 2.214 | 2.214 |
| NP2 | 2.048 | 2.048 | 2.048 |
| NP3 | 1.280 | 1.280 | 1.280 |
| CO1 | 1.233 | 1.233 | 1.233 |
| CO2 | 1.392 | 1.392 | 1.392 |
| CO3 | 1.361 | 1.361 | 1.361 |
| CO4 | 1.474 | 1.474 | 1.474 |
| CP1 | 1.726 | 1.726 | 1.726 |
| CP2 | 1.148 | 1.148 | 1.148 |
| CP3 | 1.438 | 1.438 | 1.438 |
| CP4 | 1.636 | 1.636 | 1.636 |
| CA1 | 1.453 | 1.453 | 1.254 |
| CA2 | 1.160 | 1.160 | Deleted |
| CA3 | 1.054 | 1.054 | Deleted |
| CA4 | 4.404 | 4.404 | 4.372 |
| CA5 | 1.604 | 1.604 | 1.522 |
| CA6 | 1.196 | 1.196 | Deleted |
| CA7 | 4.789 | 4.789 | 4.774 |
| RM1 | 10.874 | Deleted | - |
| RM2 | 1.095 | 1.089 | Deleted |
| RM3 | 1.119 | 1.114 | 1.112 |
| RM4 | 9.190 | 3.546 | 3.523 |
| RM5 | 4.402 | 3.660 | 3.501 |
Appendix D. Results/Models
References
- Sarwar, S.; Waheed, R.; Sarwar, S.; Khan, A. COVID-19 challenges to Pakistan: Is GIS analysis useful to draw solutions? Sci. Total Environ. 2020, 730, 139089. [Google Scholar] [CrossRef]
- Guimarães, R.M.; Monteiro da Silva, J.H.; Brusse, G.P.; Martins, T.C. Effect of physical distancing on COVID-19 incidence in Brazil: Does the strictness of mandatory rules matter? Health Policy Plan. 2021, 36, 1605–1612. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. World Health Organization’s Global Health Workforce Statistics, OECD, Supplemented by Country Data. In Physicians (per 1000 People)—Pakistan. Data; 2019. Available online: https://data.worldbank.org/indicator/SH.MED.PHYS.ZS?locations=PK (accessed on 15 October 2022).
- Khan, S.A. Situation analysis of health care system of Pakistan: Post 18 amendments. Health Care Curr. Rev. 2019, 7, 244. [Google Scholar] [CrossRef]
- Razaq, A.; Harrison, D.; Barr, B.; Asaria, M.; Routen, A.; Khunti, K. BAME COVID-19 Deaths-What Do We Know? Rapid Data & Evidence Review. 2020. Available online: https://www.cebm.net/covid-19/bame-covid-19-deaths-what-do-we-know-rapid-data-evidence-review/ (accessed on 20 October 2021).
- Rostami, P.; Ashcroft, D.M.; Tully, M.P. A formative evaluation of the implementation of a medication safety data collection tool in English healthcare settings: A qualitative interview study using normalization process theory. PLoS ONE 2018, 13, e0192224. [Google Scholar] [CrossRef] [PubMed]
- Lotta, G.; Coelho, V.S.; Brage, E. How COVID-19 Has Affected Frontline Workers in Brazil: A Comparative Analysis of Nurses and Community Health Workers. J. Comp. Policy Anal. Res. Pract. 2020, 23, 63–73. [Google Scholar] [CrossRef]
- Anthony Jnr, B. Integrating telemedicine to support digital health care for the management of COVID-19 pandemic. Int. J. Healthc. Manag. 2021, 14, 280–289. [Google Scholar] [CrossRef]
- Damschroder, L.; Aron, D.; Keith, R.; Kirsh, S.; Alexander, J.; Lowery, J. Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implement. Sci. 2009, 4, 50. [Google Scholar] [CrossRef]
- Greenhalgh, T.; Wherton, J.; Papoutsi, C.; Lynch, J.; Hughes, G.; A’Court, C.; Hinder, S.; Fahy, N.; Proctor, R.; Shaw, S. Beyond adoption: A new framework for theorizing and evaluating nonadoption, abandonment, and challenges to the scale-up, spread and sustainability of health and care technologies. J. Med. Internet Res. 2017, 19, e367. [Google Scholar] [CrossRef]
- Morrison, D.; Mair, F.S. Telehealth in practice: Using normalisation process theory to bridge the Translational Gap. Prim. Care Respir. J. 2011, 20, 351–352. [Google Scholar] [CrossRef]
- Sen-Crowe, B.; McKenney, M.; Elkbuli, A. Social distancing during the COVID-19 pandemic: Staying home save lives. Am. J. Emerg. Med. 2020, 38, 1519–1520. [Google Scholar] [CrossRef]
- Prem, K.; Liu, Y.; Russell, T.W.; Adam, J.K.; Rosalind, M.E.; Nicholas, D.; Centre for the Mathematical Modelling of Infectious Diseases COVID-19 Working Group. The effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: A modeling study. Lancet Public Health 2020, 5, e261–e270. [Google Scholar] [CrossRef] [PubMed]
- Barberia, L.G.; Cantarelli, L.G.; Oliveira, M.L.C.D.F.; Moreira, N.D.P.; Rosa, I.S.C. The effect of state-level social distancing policy stringency on mobility in the states of Brazil. Rev. De Adm. Pública 2021, 55, 27–49. [Google Scholar] [CrossRef]
- Iwaya, G.H.; Cardoso, J.G.; Sousa JH, D.; Steil, A.V. Predictors of the intention to maintain social distancing. Rev. De Adm. Pública 2020, 54, 714–734. [Google Scholar] [CrossRef]
- Mishra, M.; Majumdar, P. Social distancing during COVID-19: Will it change the Indian society? J. Health Manag. 2020, 22, 224–235. [Google Scholar] [CrossRef]
- Ramos, G.; Vieites, Y.; Jacob, J.; Andrade, E.B. Political orientation and support for social distancing during the COVID-19 pandemic: Evidence from Brazil. Rev. De Adm. Pública 2020, 54, 697–713. [Google Scholar] [CrossRef]
- Alimohamadi, Y.; Holakouie-Naieni, K.; Sepandi, M.; Taghdir, M. Effect of social distancing on COVID-19 incidence and mortality in Iran since February 20 to May 13, 2020: An interrupted time series analysis. Risk Manag. Healthc. Policy 2020, 13, 1695–1700. [Google Scholar] [CrossRef]
- Jadidzadeh, A.; Kneebone, R. Homeless Shelter Flows in Calgary and the Potential Impact of COVID-19. Can. Public Policy 2020, 46, S160–S165. [Google Scholar] [CrossRef]
- Asiamah, N.; Opuni, F.F.; Mends-Brew, E.; Mensah, S.W.; Mensah, H.K.; Quansah, F. Short-Term changes in behaviors resulting from COVID-19-Related social isolation and their influences on mental health in Ghana. Community Ment. Health J. 2021, 57, 79–92. [Google Scholar] [CrossRef]
- Iwuoha, V.C.; Aniche, E.T.; Obiora, C.A.; Umeifekwem, U.T. Citizens lack access to healthcare facilities: How COVID-19 lockdown and social distancing policies boost roadside chemist businesses in South-Eastern Nigeria. Int. J. Health Plan. Manag. 2021, 36, 2411–2423. [Google Scholar] [CrossRef]
- George, B.; Pandey, S.K. We know the Yin—But where is the Yang? Toward a balanced approach on common source bias in public administration scholarship. Rev. Public Pers. Adm. 2017, 37, 245–270. [Google Scholar] [CrossRef]
- Pereira, A.K.; Oliveira, M.S.; Sampaio, T.D.S. Asymmetries of state government social distancing policies in the face of COVID-19: Political and technical-administrative aspects. Rev. De Adm. Pública 2020, 54, 678–696. [Google Scholar] [CrossRef]
- Rahman, S.Y. “Social distancing’during COVID-19: The metaphors and politics of pandemic response in India. Health Sociol. Rev. 2020, 29, 131–139. [Google Scholar] [CrossRef] [PubMed]
- Hornik, R.; Kikut, A.; Jesch, E.; Woko, C.; Siegel, L.; Kim, K. Association of COVID-19 misinformation with face mask wearing and social distancing in a nationally representative US sample. Health Commun. 2021, 36, 6–14. [Google Scholar] [CrossRef] [PubMed]
- Schaefer, B.M.; Resende, R.C.; Epitácio, S.D.S.F.; Aleixo, M.T. Government actions against the new coronavirus: Evidence from the Brazilian states. Rev. De Adm. Pública 2020, 54, 1429–1445. [Google Scholar] [CrossRef]
- Jiang, X.; Hwang, J.; Shah, D.V.; Ghosh, S.; Brauer, M. News attention and social-distancing behavior amid COVID-19: How media trust and social norms moderate a mediated relationship. Health Commun. 2021, 37, 768–777. [Google Scholar] [CrossRef]
- Alotaibi, N.; Almutairi, S.; Alotaibi, M.; Alotaibi, M.M.; Alsufian, T. The Extent of Commitment of Saudis During Holy Ramadan to Social Distancing Measures Required for the Prevention of Transmission of COVID-19. J. Community Health 2021, 46, 693–702. [Google Scholar] [CrossRef] [PubMed]
- Cronin, C.J.; Evans, W.N. Total shutdowns, targeted restrictions, or individual responsibility: How to promote social distancing in the COVID-19 Era? J. Health Econ. 2021, 79, 102497. [Google Scholar] [CrossRef]
- Jehn, A.; Stackhouse, M.; Zajacova, A. COVID-19 Health Precautions: Identifying Demographic and Socioeconomic Disparities and Changes over Time. Can. Public Policy 2021, 47, 252–264. [Google Scholar] [CrossRef]
- Roy, S.; Ghosh, P. A Comparative Study on Distancing, Mask and Vaccine Adoption Rates from Global Twitter Trends. In Healthcare; Multidisciplinary Digital Publishing Institute: Basel, Switzerland, 2021; Volume 9, p. 488. [Google Scholar]
- Yeom, M.; Stewart, F.; Stewart, A. The impact of social distancing on community case count in the United States: Testing the efficacy of protection motivation theory during early stages of the COVID-19 pandemic. Risk Hazards Crisis Public Policy 2021, 12, 303–327. [Google Scholar] [CrossRef]
- Cunha, M.; Domingos, A.; Rocha, V.; Torres, M. How many could have been saved? Effects of social distancing on COVID-19. Rev. De Adm. Pública 2021, 55, 12–26. [Google Scholar] [CrossRef]
- Yu, D.; Anser, M.K.; Peng, M.Y.P.; Nassani, A.A.; Askar, S.E.; Zaman, K.; Jabor, M.K. Nationwide Lockdown, Population Density, and Financial Distress Brings Inadequacy to Manage COVID-19: Leading the Services Sector into the Trajectory of Global Depression. In Healthcare; Multidisciplinary Digital Publishing Institute: Basel, Switzerland, 2021; Volume 9, p. 220. [Google Scholar]
- Buckingham, S.; Kendall, M.; Ferguson, S.; MacNee, W.; Sheikh, A.; White, P.; Worth, A.; Boyd, K.; Murray, S.A.; Pinnock, H. HELPing older people with very severe chronic obstructive pulmonary disease (HELP-COPD): Mixed-method feasibility pilot randomized controlled trial of a novel intervention. NPJ Prim. Care Respir. Med. 2015, 25, 15020. [Google Scholar] [CrossRef]
- Stevenson, F. The use of electronic patient records for medical research: Conflicts and contradictions. BMC Health Serv. Res. 2015, 15, 124. [Google Scholar] [CrossRef]
- Carter, M.; Davey, A.; Wright, C.; Elmore, N.; Newbould, J.; Roland, M.; Campbell, J.; Burt, J. Capturing patient experience: A qualitative study of implementing real-time feedback in primary care. Br. J. Gen. Pract. 2016, 66, e786–e793. [Google Scholar] [CrossRef]
- Porter, A.; Kingston, M.R.; Evans, B.A.; Hutchings, H.; Whitman, S.; Snooks, H. It could be a “Golden goose”: A qualitative study of views in primary care on an emergency admission risk prediction tool prior to implementation. BMC Fam. Pract. 2016, 17, 1. [Google Scholar]
- Bayliss, K.; Riste, L.; Band, R.; Peters, S.; Wearden, A.; Lovell, K.; Fisher, L.; Chew-Graham, C.A. Implementing resources to support the diagnosis and management of chronic fatigue syndrome/Myalgic encephalomyelitis (CFS/ME) in primary care: A qualitative study. BMC Fam. Pract. 2016, 17, 66. [Google Scholar] [CrossRef] [PubMed]
- Ricketts, E.J.; Francischetto, E.O.C.; Wallace, L.M.; Hogan, A.; McNulty, C.A. Tools to overcome potential barriers to chlamydia screening in general practice: Qualitative evaluation of the implementation of a complex intervention. BMC Fam. Pract. 2016, 17, 33. [Google Scholar] [CrossRef]
- Blickem, C.; Kennedy, A.; Jariwala, P.; Morris, R.; Bowen, R.; Vassilev, I.; Brooks, H.; Blakeman, T.; Rogers, A. Aligning everyday life priorities with people’s self-management support networks: An exploration of the work and implementation of a needs-led telephone support system. BMC Health Serv. Res. 2014, 14, 262. [Google Scholar] [CrossRef] [PubMed]
- Bouamrane, M.-M.; Mair, F.S. A qualitative evaluation of general practitioners’ views on protocol-driven eReferral in Scotland. BMC Med. Inf. Decis. Mak. 2014, 14, 30. [Google Scholar] [CrossRef]
- Reeve, J.; Britten, N.; Byng, R.; Fleming, J.; Heaton, J.; Krska, J. Identifying enablers and barriers to individually tailored prescribing: A survey of healthcare professionals in the UK. BMC Fam. Pract. 2018, 19, 17. [Google Scholar] [CrossRef]
- Teunissen, E.; Gravenhorst, K.; Dowrick, C.; van Weel-Baumgarten, E.; Van den Driessen, M.F.; de Brún, T.; Burns, N.; Lionis, C.; Mair, F.S.; O’Donnell, C.; et al. Implementing guidelines and training initiatives to improve cross-cultural communication in primary care consultations: A qualitative participatory European study. Int. J. Equity Health 2017, 16, 32. [Google Scholar] [CrossRef]
- Browne, S.; Macdonald, S.; May, C.R.; Macleod, U.; Mair, F.S. Patient, carer and professional perspectives on barriers and facilitators to quality care in advanced heart failure. PLoS ONE 2014, 9, e93288. [Google Scholar] [CrossRef]
- Coupe, N.; Anderson, E.; Gask, L.; Sykes, P.; Richards, D.A.; Chew-Graham, C. Facilitating professional liaison in collaborative care for depression in UK primary care; a qualitative study utilizing normalization process theory. BMC Fam. Pract. 2014, 15, 78. [Google Scholar] [CrossRef]
- Nutley, S.; Walter, I.; Davies, H. Using Evidence: How Research can Inform Public Services; Policy Press: Bristol, UK, 2007. [Google Scholar]
- Greenhalgh, T.; Robert, G.; MacFarlane, F. Diffusion of innovations in service organizations: Systematic review and recommendations. Milbank Q. 2004, 82, 581–629. [Google Scholar] [CrossRef] [PubMed]
- Henseler, J.; Schuberth, F. Using confirmatory composite analysis to assess emergent variables in business research. J. Bus. Res. 2020, 120, 147–156. [Google Scholar] [CrossRef]
- Hair, J.F., Jr.; Sarstedt, M.; Hopkins, L.; Kuppelwieser, V.G. Partial least squares structural equation modeling (PLS-SEM). Eur. Bus. Rev. 2014, 26, 106–121. [Google Scholar] [CrossRef]
- Finch, T.L.; Girling, M.; May, C.R.; Mair, F.S.; Murray, E.; Treweek, S.; Rapley, T. Improving the normalization of complex interventions: Part 2-validation of the NoMAD instrument for assessing implementation work based on normalization process theory (NPT). BMC Med. Res. Methodol. 2018, 18, 135. [Google Scholar] [CrossRef]
- Meier, K.J.; O’Toole, L.J., Jr. I think (I am doing well), therefore I am: Assessing the validity of administrators’ self-assessments of performance. Int. Public Manag. J. 2013, 16, 1–27. [Google Scholar] [CrossRef]
- Garson, D. Partial Least Squares: Regression & Structural Equation Modeling; Statistical Associates Publishing: Asheboro, NC, USA, 2016. [Google Scholar]
- Podsakoff, P.M.; MacKenzie, S.B.; Podsakoff, N.P. Sources of method bias in social science research and recommendations on how to control it. Annu. Rev. Psychol. 2012, 63, 539–569. [Google Scholar] [CrossRef] [PubMed]
- Kock, N. Harman’s single factor test in PLS-SEM: Checking for common method bias. Data Anal. Perspect. J. 2021, 2, 1–6. [Google Scholar]
- Razali, N.M.; Wah, Y.B. Power comparisons of shapiro-wilk, kolmogorov-smirnov, lilliefors and anderson-darling tests. J. Stat. Model. Anal. 2011, 2, 21–33. [Google Scholar]
- Harwell, M.R. Choosing between parametric and nonparametric tests. J. Couns. Dev. 1988, 67, 35–38. [Google Scholar] [CrossRef]
- Fagerland, M.W.; Sandvik, L. The ilcoxon–mann–whitney test under scrutiny. Stat. Med. 2009, 28, 1487–1497. [Google Scholar] [CrossRef] [PubMed]
- Hecke, T.V. Power study of anova versus Kruskal-Wallis test. J. Stat. Manag. Syst. 2012, 15, 241–247. [Google Scholar] [CrossRef]
- Graf, A.S.; Knepple Carney, A. Ageism as a Modifying Influence on COVID-19 Health Beliefs and Intention to Social Distance. J. Aging Health 2021, 33, 518–530. [Google Scholar] [CrossRef] [PubMed]
- Henseler, J.; Chin, W.W. A Comparison of Approaches for the Analysis of Interaction Effects Between Latent Variables Using Partial Least Squares Path Modeling. Struct. Equ. Model. A Multidiscip. J. 2010, 17, 82–109. [Google Scholar] [CrossRef]
- Hair, J.F.; Ringle, C.M.; Sarstedt, M. PLS-SEM: Indeed a Silver Bullet. J. Mark. Theory Pract. 2011, 19, 139–152. [Google Scholar] [CrossRef]
- Ali, F.; Kim, W.G.; Ryu, K. The effect of physical environment on passenger delight and satisfaction: Moderating effect of national identity. Tour. Manag. 2016, 57, 213–224. [Google Scholar] [CrossRef]
- Esposito Vinzi, V.; Chin, W.W.; Henseler, J.; Wang, H. Handbook of Partial Least Squares: Concepts, Methods and Applications; Springer: Berlin/Heidelberg, Germany, 2010. [Google Scholar]
- Siqueira, G.D.; Adeel, A.; Pasha, P.; Balushi, A.A.; Shah, S.A.R. Sustainable transportation and policy development: A study for impact analysis of mobility patterns and neighborhood assessment of walking behavior. Sustainability 2021, 13, 1871. [Google Scholar] [CrossRef]
- Fornell, C.; Larcker, D.F. Evaluating structural equation models with unobservable variables and measurement error. J. Mark. Res. 1981, 18, 39–50. [Google Scholar] [CrossRef]
- Barclay, C.; Thompson, D.; dan Higgins, R. The Partial Least Squares (PLS) Approach to Causal Modeling: Personal Computer Adoption and Use an Illustration. Technol. Stud. 1995, 2, 285–309. [Google Scholar]
- Liu, Y. A new antihypertensive drug ameliorate insulin resistance. Acta Pharmacol. Sin. 2012, 33, 429–430. [Google Scholar] [CrossRef]
- Chin, W.W. The partial least squares approach to structural equation modeling. Mod. Methods Bus. Res. 1998, 295, 295–336. [Google Scholar]
- Hair, J.F.; Risher, J.J.; Sarstedt, M.; Ringle, C.M. When to use and how to report the results of PLS-SEM. Eur. Bus. Rev. 2019, 31, 2–24. [Google Scholar] [CrossRef]
- Kushary, D. Bootstrap Methods and their Application. Technometrics 2000, 42, 216–217. [Google Scholar] [CrossRef]
- Hair, J.F.; Sarstedt, M.; Ringle, C.M.; Mena, J.A. An assessment of the use of partial least squares structural equation modeling in marketing research. J. Acad. Mark. Sci. 2012, 40, 414–433. [Google Scholar] [CrossRef]
- Aibinu, A.A.A.A.; Al-Lawati, A.M. Using PLS-SEM technique to model construction organizations’ willingness to participate in e-bidding. Autom. Constr. 2010, 19, 714–724. [Google Scholar] [CrossRef]
- Akter, S.; D’Ambra, J.; Ray, P. An Evaluation of PLS-based Complex Models: The Roles of Power Analysis, Predictive Relevance and GoF Index. In Proceedings of the Renaissance of Information Technology for Sustainability and Global Competitiveness, 17th Americas Conference on Information Systems (AMCIS 2011), Detroit, MI, USA, 4–8 August 2011. [Google Scholar]
- Cohen, J.; Cohen, P.; West, S.G.; Aiken, L.S. Applied Multiple Regression/Correlation Analysis for the Behavioral Sciences; Routledge: London, UK, 2013. [Google Scholar]
- Athab, N.A. An analytical study of cervical spine pain according to the mechanical indicators of the administrative work staff. Indian J. Public Health 2019, 10, 1348–1353. [Google Scholar] [CrossRef]
- Askariazad, M.H.; Babakhani, N. An application of European Customer Satisfaction Index (ECSI) in business to business (B2B) context. J. Bus. Ind. Mark. 2015, 30, 17–31. [Google Scholar] [CrossRef]
- Henseler, J.; Sarstedt, M. Goodness-of-fit indices for partial least squares path modeling. Comput. Stat. 2013, 28, 565–580. [Google Scholar] [CrossRef]
- Davies, P.; Walker, A.E.; Grimshaw, J.M. A systematic review of the use of theory in the design of guideline dissemination and implementation strategies and interpretation of the results of rigorous evaluations. Implement. Sci. 2010, 5, 14. [Google Scholar] [CrossRef]
- Wetzels, M.; Odekerken-Schröder, G.; Van Oppen, C. Using PLS path modeling for assessing hierarchical construct models: Guidelines and empirical illustration. MIS Q. 2009, 33, 177–195. [Google Scholar] [CrossRef]
- Finch, T.L.; Girling, M.; May, C.R.; Mair, F.S.; Murray, E.; Treweek, S.; Rapley, T. NoMAD: Implementation Measure Based on Normalization Process Theory. [Measurement Instrument]. 2015. Available online: http://www.normalizationprocess.org (accessed on 11 November 2021).
- May, C. Implementing, embedding and integrating practices: An outline of normalization process theory. Sociology 2009, 43, 535–554. [Google Scholar] [CrossRef]
- Hair, J.F.; Hult, G.T.M.; Ringle, C.; Sarstedt, M. A Primer on Partial Least Squares Structural Equation Modelling (PLS-SEM); Sage Publications: Los Angeles, CA, USA, 2013. [Google Scholar]
- Chin, W.W.; Peterson, R.A.; Brown, P.S. Structural equation modelling in marketing: Some practical reminders. J. Mark. Theory Pract. 2008, 16, 287–298. [Google Scholar] [CrossRef]
- Huddlestone, L.; Turner, J.; Eborall, H.; Hudson, N.; Davies, M.; Martin, G. Application of normalisation process theory in understanding implementation processes in primary care settings in the UK: A systematic review. BMC Fam. Pract. 2020, 21, 52. [Google Scholar] [CrossRef] [PubMed]
- Streiner, D.L.; Norman, G.R. Health Measurement Scales. A Practical Guide to Their Development and Use; Oxford University Press: Oxford, UK, 2004. [Google Scholar]
- Moraes, R.F.D. Determinants of physical distancing during the COVID-19 epidemic in Brazil: Effects from mandatory rules, numbers of cases and duration of rules. Ciência Saúde Coletiva 2020, 25, 3393–3400. [Google Scholar] [CrossRef] [PubMed]
- Battiston, P.; Gamba, S. COVID-19: R0 is lower where outbreak is larger. Health Policy 2021, 125, 141–147. [Google Scholar] [CrossRef]
- Elf, M.; Nordmark, S.; Lyhagen, J.; Lindberg, I.; Finch, T.; Åberg, A.C. The Swedish version of the Normalization Process Theory Measure S-NoMAD: Translation, adaptation, and pilot testing. Implement. Sci. 2018, 13, 146. [Google Scholar] [CrossRef] [PubMed]
- May, C.R.; Cummings, A.; Girling, M.; Bracher, M.; Mair, F.S.; May, C.M.; Finch, T. Using Normalization Process Theory in feasibility studies and process evaluations of complex healthcare interventions: A systematic review. Implement. Sci. 2018, 13, 80. [Google Scholar] [CrossRef] [PubMed]
- Eccles, M.P.; Armstrong, D.; Baker, R.; Cleary, K.; Davies, H.; Davies, S.; Sibbald, B. An implementation research agenda. Implement. Sci. 2009, 4, 18. [Google Scholar] [CrossRef]
- Woolf, S.H. The meaning of translational research and why it matters. JAMA 2008, 299, 211–213. [Google Scholar] [CrossRef] [PubMed]
- Mackenzie, M.; O’Donnell, C.; Halliday, E.; Sridharan, S.; Platt, S. Do health improvement programmes fit with MRC guidance on evaluating complex interventions? BMJ 2010, 340, c185. [Google Scholar] [CrossRef] [PubMed]
- Eccles, M.P.; Weijer, C.; Mittman, B. Requirements for ethics committee review for studies submitted to Implementation Science. Implement. Sci. 2011, 6, 32. [Google Scholar] [CrossRef] [PubMed]
- de Brún, T.; O’Reilly-de Brún, M.; O’Donnell, C.A.; MacFarlane, A. Learning from doing: The case for combining normalisation process theory and participatory learning and action research methodology for primary healthcare implementation research. BMC Health Serv. Res. 2016, 16, 346. [Google Scholar] [CrossRef] [PubMed]
- Eckhard, S.; Parizek, M. Policy implementation by international organizations: A comparative analysis of strengths and weaknesses of national and international staff. J. Comp. Policy Anal. Res. Pract. 2020, 24, 254–270. [Google Scholar] [CrossRef]
| Constructs | Items | First Iteration | Second Iteration | Third Iteration | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Loading | CR | AVE | Loading | CR | AVE | Loading | CR | AVE | ||
| SD Normalization | NP1 NP2 NP3 | 0.911 0.897 0.635 | 0.861 | 0.680 | 0.911 0.894 0.642 | 0.862 | 0.680 | 0.915 0.898 0.626 | 0.860 | 0.678 |
| Coherence | CO1 CO2 CO3 CO4 | 0.614 0.684 0.679 0.892 | 0.813 | 0.526 | 0.614 0.684 0.679 0.892 | 0.813 | 0526 | 0.615 0.684 0.680 0.892 | 0.813 | 0.526 |
| Cognitive Participation | CP1 CP2 CP3 CP4 | 0.851 0.496 0.764 0.824 | 0.830 | 0.558 | 0.851 0.496 0.794 0.823 | 0.830 | 0.558 | 0.851 0.496 0.764 0.824 | 0.830 | 0558 |
| Collective Action | CA1 CA2 CA3 CA4 CA5 CA6 CA7 | 0.610 -0.319 0.143 0.859 0.806 0.102 0.890 | 0.689 | 0.383 | 0.611 −0.320 0.143 0.859 0.806 0.102 0.890 | 0.689 | 0.383 | 0.602 Omitted Omitted 0.878 0.802 Omitted 0.907 | 0.879 | 0.650 |
| Reflexive Monitoring | RM1 RM2 RM3 RM4 RM5 | 0.942 0.379 0.484 0.933 0.925 | 0.870 | 0.598 | Omitted 0.449 0.537 0.896 0.916 | 0.807 | 0.533 | - Omitted 0.556 0.925 0.927 | 0.856 | 0.675 |
| Analysis of Discriminant Validity through Cross-Loadings | |||||
|---|---|---|---|---|---|
| Constructs | Normalization of Social Distancing | Coherence | Cognitive Participation | Collective Action | Reflexive Monitoring |
| NP1 | 0.915 | 0.835 | 0.813 | 0.837 | 0.759 |
| NP2 | 0.898 | 0.598 | 0.842 | 0.813 | 0.830 |
| NP3 | 0.626 | 0.316 | 0.409 | 0.429 | 0.367 |
| CO1 | 0.349 | 0.615 | 0.267 | 0.263 | 0.283 |
| CO2 | 0.347 | 0.684 | 0.296 | 0.250 | 0.347 |
| CO3 | 0.367 | 0.680 | 0.326 | 0.338 | 0.348 |
| CO4 | 0.846 | 0.892 | 0.809 | 0.775 | 0.738 |
| CP1 | 0.790 | 0.634 | 0.851 | 0.808 | 0.717 |
| CP2 | 0.318 | 0.212 | 0.496 | 0.360 | 0.345 |
| CP3 | 0.659 | 0.491 | 0.764 | 0.601 | 0.558 |
| CP4 | 0.734 | 0.600 | 0.824 | 0.691 | 0.814 |
| CA1 | 0.464 | 0.401 | 0.440 | 0.602 | 0.419 |
| CA4 | 0.679 | 0.524 | 0.701 | 0.878 | 0.670 |
| CA5 | 0.738 | 0.527 | 0.784 | 0.802 | 0.790 |
| CA7 | 0.771 | 0.642 | 0.756 | 0.907 | 0.698 |
| RM3 | 0.496 | 0.508 | 0.393 | 0.475 | 0.556 |
| RM4 | 0.790 | 0.590 | 0.828 | 0.730 | 0.925 |
| RM5 | 0.841 | 0.511 | 0.837 | 0.862 | 0.927 |
| Constructs | Path Coefficients | Sample Mean | Standard Deviation | t-Value | p-Values | Result |
|---|---|---|---|---|---|---|
| CO | 0.202 | 0.201 | 0.060 | 3.359 | 0.000 | Significant |
| CP | 0.226 | 0.233 | 0.060 | 3.772 | 0.001 | Significant |
| CA | 0.299 | 0.297 | 0.091 | 3.289 | 0.001 | Significant |
| RM | 0.294 | 0.290 | 0.068 | 4.346 | 0.000 | Significant |
| Original Sample (O) | Sample Mean (M) | Standard Deviation | T Statistics | p Values | Hypothesis Testing | |
|---|---|---|---|---|---|---|
| NP1—Normalization of SD | 0.915 | 0.915 | 0.009 | 105.203 | 0.000 | |
| NP2—Normalization of SD | 0.898 | 0.898 | 0.012 | 77.241 | 0.000 | |
| NP3—Normalization of SD | 0.626 | 0.622 | 0.045 | 14.021 | 0.000 | |
| CO1—Coherence | 0.615 | 0.616 | 0.053 | 11.657 | 0.000 | |
| CO2—Coherence | 0.684 | 0.687 | 0.047 | 14.509 | 0.000 | |
| CO3—Coherence | 0.680 | 0.678 | 0.053 | 12.932 | 0.000 | |
| CO4—Coherence | 0.892 | 0.893 | 0.008 | 116.133 | 0.000 | |
| Coherence to Normalization of SD | Supported | |||||
| CP1—Cognitive Participation | 0.851 | 0.851 | 0.017 | 50.169 | 0.000 | |
| CP2—Cognitive Participation | 0.496 | 0.498 | 0.097 | 5.094 | 0.000 | |
| CP3—Cognitive Participation | 0.764 | 0.762 | 0.035 | 22.094 | 0.000 | |
| CP4—Cognitive Participation | 0.824 | 0.823 | 0.031 | 26.958 | 0.000 | |
| Cognitive Participation to Normalization of SD | Supported | |||||
| CA1—Collective Action | 0.602 | 0.604 | 0.060 | 10.097 | 0.000 | |
| CA4—Collective Action | 0.878 | 0.878 | 0.026 | 33.466 | 0.000 | |
| CA5—Collective Action | 0.802 | 0.803 | 0.024 | 33.711 | 0.000 | |
| CA7—Collective Action | 0.907 | 0.904 | 0.021 | 42.345 | 0.000 | |
| Collective Action to Normalization of SD | Supported | |||||
| RM3—Reflexive Monitoring | 0.556 | 0.556 | 0.064 | 8.636 | 0.000 | |
| RM4—Reflexive Monitoring | 0.925 | 0.925 | 0.019 | 49.739 | 0.000 | |
| RM5—Reflexive Monitoring | 0.927 | 0.928 | 0.010 | 92.582 | 0.000 | |
| Reflexive Monitoring to Normalization of SD | Supported | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nazir, M.F.; Qureshi, S.F. Applying Structural Equation Modelling to Understand the Implementation of Social Distancing in the Professional Lives of Healthcare Workers. Int. J. Environ. Res. Public Health 2023, 20, 4630. https://doi.org/10.3390/ijerph20054630
Nazir MF, Qureshi SF. Applying Structural Equation Modelling to Understand the Implementation of Social Distancing in the Professional Lives of Healthcare Workers. International Journal of Environmental Research and Public Health. 2023; 20(5):4630. https://doi.org/10.3390/ijerph20054630
Chicago/Turabian StyleNazir, Muhammad Fayyaz, and Shahzadah Fahed Qureshi. 2023. "Applying Structural Equation Modelling to Understand the Implementation of Social Distancing in the Professional Lives of Healthcare Workers" International Journal of Environmental Research and Public Health 20, no. 5: 4630. https://doi.org/10.3390/ijerph20054630
APA StyleNazir, M. F., & Qureshi, S. F. (2023). Applying Structural Equation Modelling to Understand the Implementation of Social Distancing in the Professional Lives of Healthcare Workers. International Journal of Environmental Research and Public Health, 20(5), 4630. https://doi.org/10.3390/ijerph20054630





