Physician’s Burnout during the COVID-19 Pandemic: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
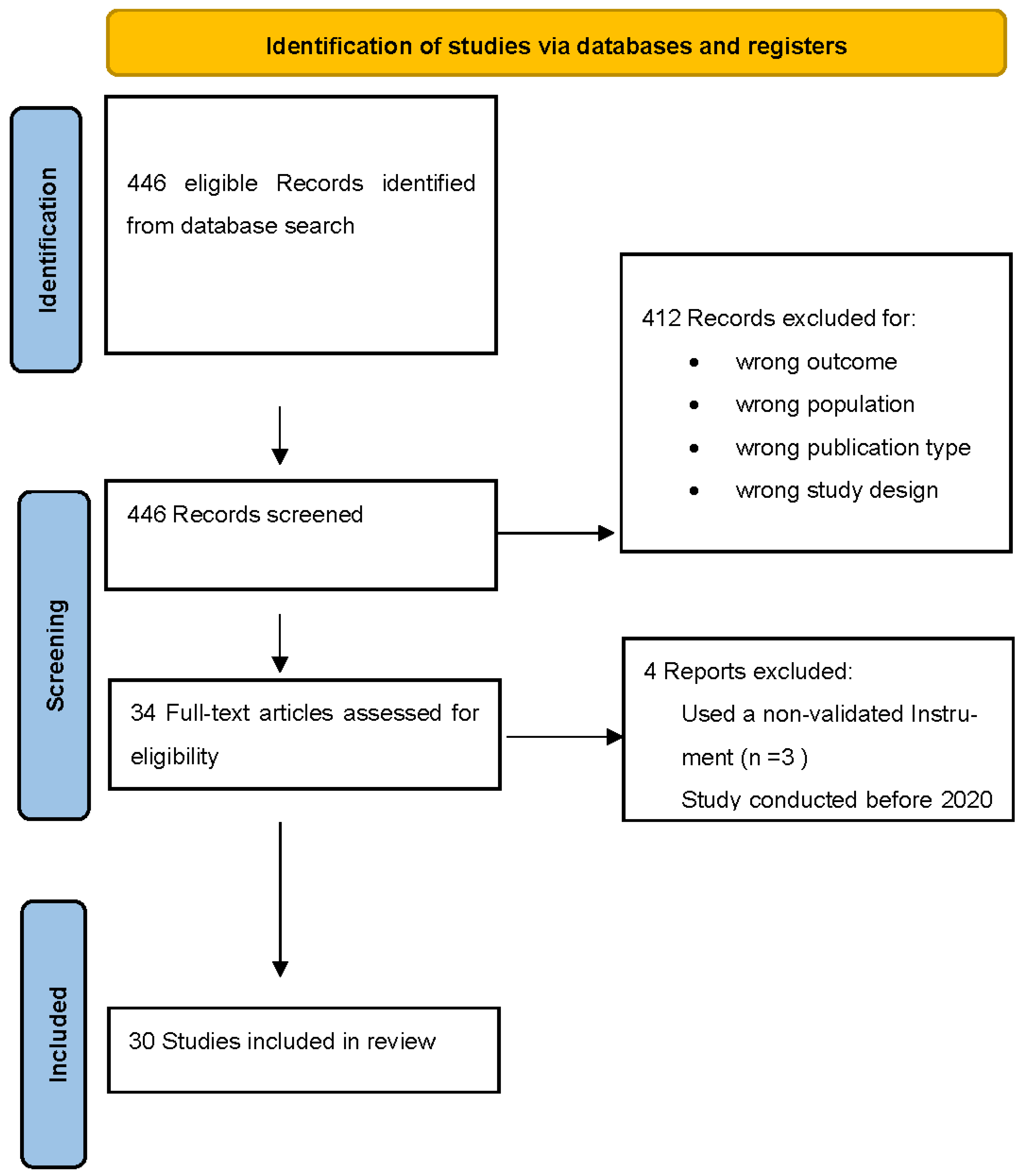
2. Methods
2.1. Inclusion and Exclusion Criteria
2.2. Search Strategy and Selection Criteria
2.3. Data Extraction and Quality Assessment
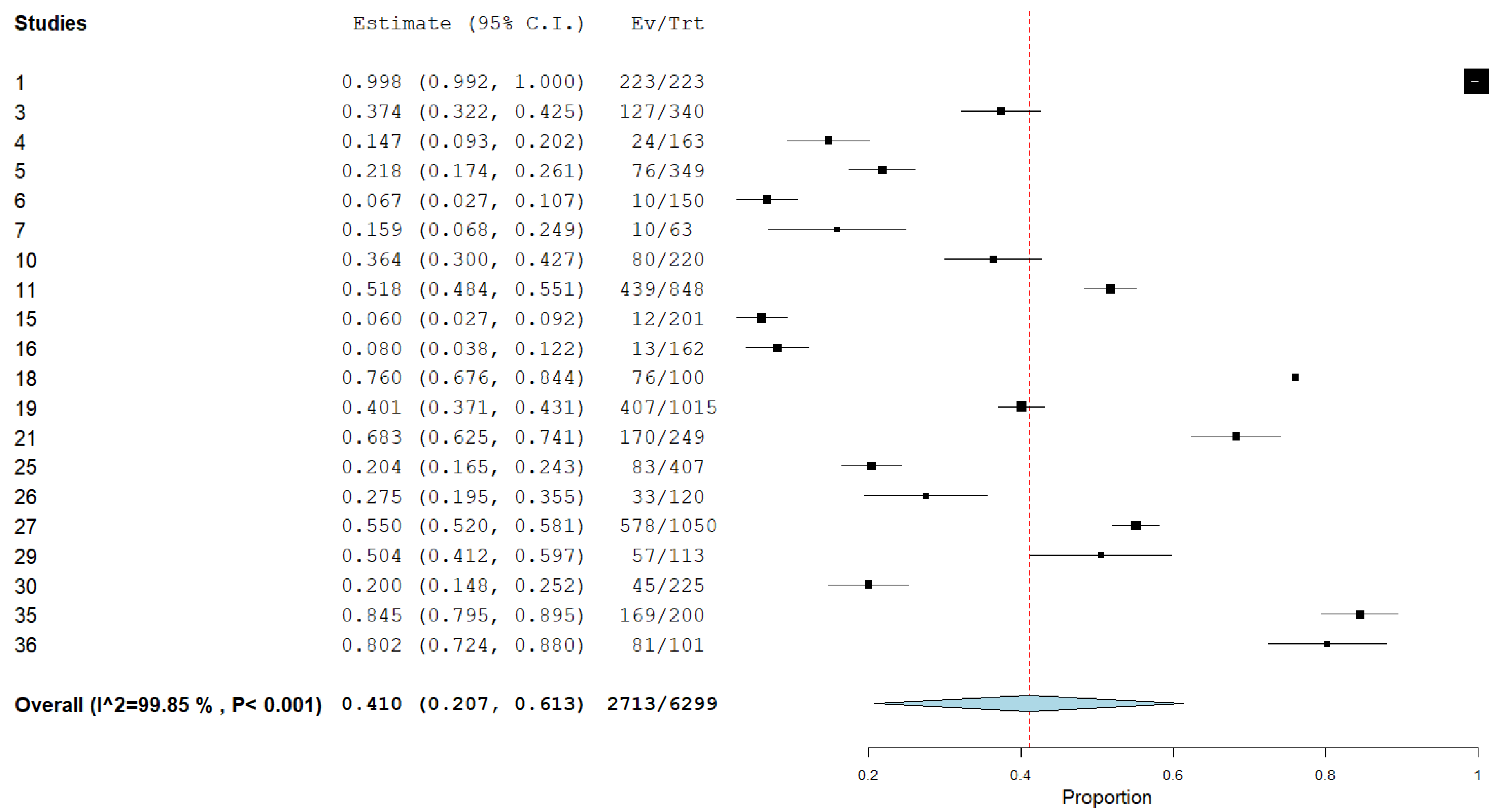
2.4. Statistical Analyses
3. Results
3.1. Characteristics of Studies
3.2. Measurement Tools for Burnout
3.3. Aggregate Prevalence of Burnout
4. Discussion
Limitations
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kincaid, E. One Year into the Pandemic, More Than 3000 Healthcare Workers Have Died of COVID-19. Available online: https://www.medscape.com/viewarticle/947304 (accessed on 11 March 2022).
- Mhango, M.; Dzobo, M.; Chitungo, I.; Dzinamarira, T. COVID-19 Risk Factors Among Health Workers: A Rapid Review. Saf. Health Work 2020, 11, 262–265. [Google Scholar] [CrossRef] [PubMed]
- Sasangohar, F.; Jones, S.L.; Masud, F.N.; Vahidy, F.S.; Kash, B.A. Provider Burnout and Fatigue During the COVID-19 Pandemic: Lessons Learned from a High-Volume Intensive Care Unit. Anesth. Analg. 2020, 131, 106–111. [Google Scholar] [CrossRef] [PubMed]
- Shanafelt, T.; Ripp, J.; Trockel, M. Understanding and Addressing Sources of Anxiety among Health Care Professionals During the COVID-19 Pandemic. JAMA 2020, 323, 2133–2134. [Google Scholar] [CrossRef] [PubMed]
- Magnavita, N.; Soave, P.M.; Ricciardi, W.; Antonelli, M. Occupational Stress and Mental Health among Anesthetists during the COVID-19 Pandemic. IJERPH 2020, 17, 8245. [Google Scholar] [CrossRef] [PubMed]
- Elbay, R.Y.; Kurtulmuş, A.; Arpacıoğlu, S.; Karadere, E. Depression, anxiety, stress levels of physicians and associated factors in Covid-19 pandemics. Psychiatry Res. 2020, 290, 113130. [Google Scholar] [CrossRef] [PubMed]
- Patel, R.S.; Bachu, R.; Adikey, A.; Malik, M.; Shah, M. Factors Related to Physician Burnout and Its Consequences: A Review. Behav. Sci. 2018, 8, 98. [Google Scholar] [CrossRef]
- Freudenberger, H.J. The staff burn-out syndrome in alternative institutions. Psychol. Psychother. 1975, 12, 73–82. [Google Scholar] [CrossRef]
- Maslach, C. The Cost of Caring; Ishk: Los Altos, CA, USA, 2003. [Google Scholar]
- Panagioti, M.; Geraghty, K.; Johnson, J.; Zhou, A.; Panagopoulou, E.; Chew-Graham, C.; Peters, D.; Hodkinson, A.; Riley, R.; Esmail, A. Association Between Physician Burnout and Patient Safety, Professionalism, and Patient Satisfaction: A Systematic Review and Meta-analysis. JAMA Intern. Med. 2018, 178, 1317–1331. [Google Scholar] [CrossRef]
- Peckham, C. Medscape Physician Lifestyle Report. 2015. Available online: https://www.medscape.com/slideshow/lifestyle-2015-overview-6006535 (accessed on 11 March 2022).
- Kane, L. Medscape National Physician Burnout & Suicide Report 2020: The Generational Divide. Available online: https://www.medscape.com/slideshow/2020-lifestyle-burnout-6012460 (accessed on 11 March 2022).
- Kane, L. Death by 1000 Cuts”: Medscape National Physician Burnout & Suicide Report. 2021. Available online: https://www.medscape.com/slideshow/2021-lifestyle-burnout-6013456 (accessed on 11 March 2022).
- Rotenstein, L.S.; Torre, M.; Ramos, M.A.; Rosales, R.C.; Guille, C.; Sen, S.; Mata, D.A. Prevalence of Burnout Among Physicians: A Systematic Review. JAMA 2018, 320, 1131–1150. [Google Scholar] [CrossRef]
- Hiver, C.; Villa, A.; Bellagamba, G.; Lehucher-Michel, M.-P. Burnout prevalence among European physicians: A systematic review and meta-analysis. Int. Arch. Occup. Environ. Health 2022, 95, 259–273. [Google Scholar] [CrossRef]
- Menon, N.K.; Shanafelt, T.D.; Sinsky, C.A.; Linzer, M.; Carlasare, L.; Brady, K.J.S.; Stillman, M.J.; Trockel, M.T. Association of Physician Burnout with Suicidal Ideation and Medical Errors. JAMA Netw. Open 2020, 3, e2028780. [Google Scholar] [CrossRef] [PubMed]
- West, C.P.; Tan, A.D.; Habermann, T.M.; Sloan, J.A.; Shanafelt, T.D. Association of Resident Fatigue and Distress With Perceived Medical Errors. JAMA 2009, 302, 1294–1300. [Google Scholar] [CrossRef] [PubMed]
- Dewa, C.S.; Loong, D.; Bonato, S.; Trojanowski, L. The relationship between physician burnout and quality of healthcare in terms of safety and acceptability: A systematic review. BMJ Open 2017, 7, e015141. [Google Scholar] [CrossRef]
- Hyman, S.A.; Shotwell, M.S.; Michaels, D.R.; Han, X.; Card, E.B.; Morse, J.L.; Weinger, M.B. A Survey Evaluating Burnout, Health Status, Depression, Reported Alcohol and Substance Use, and Social Support of Anesthesiologists. Anesth. Analg. 2017, 125, 2009–2018. [Google Scholar] [CrossRef] [PubMed]
- Stehman, C.R.; Testo, Z.; Gershaw, R.S.; Kellogg, A.R. Burnout, Drop Out, Suicide: Physician Loss in Emergency Medicine, Part I. West. J. Emerg. Med. 2019, 20, 485–494. [Google Scholar] [CrossRef] [PubMed]
- Kruse, C.S.; Mileski, M.; Dray, G.; Johnson, Z.; Shaw, C.; Shirodkar, H. Physician Burnout and the Electronic Health Record Leading Up to and during the First Year of COVID-19: Systematic Review. J. Med. Internet. Res. 2022, 24, e36200. [Google Scholar] [CrossRef] [PubMed]
- Shaikh, C.F.; Palmer Kelly, E.; Paro, A.; Cloyd, J.; Ejaz, A.; Beal, E.W.; Pawlik, T.M. Burnout Assessment Among Surgeons and Surgical Trainees During the COVID-19 Pandemic: A Systematic Review. J. Surg. Educ. 2022, 79, 1206–1220. [Google Scholar] [CrossRef]
- Claponea, R.M.; Pop, L.M.; Iorga, M.; Iurcov, R. Symptoms of Burnout Syndrome among Physicians during the Outbreak of COVID-19 Pandemic & mdash; A Systematic Literature Review. Healthcare 2022, 10, 979. [Google Scholar]
- Amanullah, S.; Ramesh Shankar, R. The Impact of COVID-19 on Physician Burnout Globally: A Review. Healthcare 2020, 8, 421. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 2010, 25, 603–605. [Google Scholar] [CrossRef] [PubMed]
- Wallace, B.C.; Schmid, C.H.; Lau, J.; Trikalinos, T.A. Meta-Analyst: Software for meta-analysis of binary, continuous and diagnostic data. BMC Med. Res. Methodol. 2009, 9, 80. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savović, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.C. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [PubMed]
- Civantos, A.M.; Byrnes, Y.; Chang, C.; Prasad, A.; Chorath, K.; Poonia, S.K.; Jenks, C.M.; Bur, A.M.; Thakkar, P.; Graboyes, E.M.; et al. Mental health among otolaryngology resident and attending physicians during the COVID-19 pandemic: National study. Head Neck 2020, 42, 1597–1609. [Google Scholar] [CrossRef] [PubMed]
- Lazarides, A.L.; Belay, E.S.; Anastasio, A.T.; Cook, C.E.; Anakwenze, O.A. Physician burnout and professional satisfaction in orthopedic surgeons during the COVID-19 Pandemic. Work 2021, 69, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Khalafallah, A.M.; Lam, S.; Gami, A.; Dornbos, D.L.; Sivakumar, W.; Johnson, J.N.; Mukherjee, D. Burnout and career satisfaction among attending neurosurgeons during the COVID-19 pandemic. Clin. Neurol. Neurosurg. 2020, 198, 106193. [Google Scholar] [CrossRef]
- Coleman, J.R.; Abdelsattar, J.M.; Glocker, R.J.; Carmichael, H.; Vigneshwar, N.G.; Ryan, R.; Qiu, Q.; Nayyar, A.; Visenio, M.R.; Sonntag, C.C.; et al. COVID-19 Pandemic and the Lived Experience of Surgical Residents, Fellows, and Early-Career Surgeons in the American College of Surgeons. J. Am. Coll. Surg. 2021, 232, 119–135.e120. [Google Scholar] [CrossRef]
- Kannampallil, T.G.; Goss, C.W.; Evanoff, B.A.; Strickland, J.R.; McAlister, R.P.; Duncan, J. Exposure to COVID-19 patients increases physician trainee stress and burnout. PLoS ONE 2020, 15, e0237301. [Google Scholar] [CrossRef]
- Ofei-Dodoo, S.; Mullen, R.; Pasternak, A.; Hester, C.M.; Callen, E.; Bujold, E.J.; Carroll, J.K.; Kimminau, K.S. Loneliness, Burnout, and Other Types of Emotional Distress Among Family Medicine Physicians: Results from a National Survey. JABFM 2021, 34, 531–541. [Google Scholar] [CrossRef]
- Al-Humadi, S.M.; Cáceda, R.; Bronson, B.; Paulus, M.; Hong, H.; Muhlrad, S. Orthopaedic Surgeon Mental Health during the COVID-19 Pandemic. Geriatr. Orthop. Surg. Rehabil 2021, 12, 21514593211035230. [Google Scholar] [CrossRef]
- Chalhub, R.; Menezes, M.S.; Aguiar, C.V.N.; Santos-Lins, L.S.; Netto, E.M.; Brites, C.; Lins-Kusterer, L. Anxiety, health-related quality of life, and symptoms of burnout in frontline physicians during the COVID-19 pandemic. Braz. J. Infect. Dis. 2021, 25, 101618. [Google Scholar] [CrossRef] [PubMed]
- Civantos, A.M.; Bertelli, A.; Gonçalves, A.; Getzen, E.; Chang, C.; Long, Q.; Rajasekaran, K. Mental health among head and neck surgeons in Brazil during the COVID-19 pandemic: A national study. Am. J. Otolaryngol. 2020, 41, 102694. [Google Scholar] [CrossRef] [PubMed]
- Khan, N.; Palepu, A.; Dodek, P.; Salmon, A.; Leitch, H.; Ruzycki, S.; Townson, A.; Lacaille, D. Cross-sectional survey on physician burnout during the COVID-19 pandemic in Vancouver, Canada: The role of gender, ethnicity and sexual orientation. BMJ Open 2021, 11, e050380. [Google Scholar] [CrossRef] [PubMed]
- Ovalle Diaz, J.; Gorgen, A.R.H.; Teixeira da Silva, A.G.; de Oliveira Paludo, A.; Timóteo de Oliveira, R.; Rosito, N.; Barroso, U.; Corbetta, J.P.; López Egaña, P.-J.; Tavares, P.M.; et al. Burnout syndrome in pediatric urology: A perspective during the COVID-19 pandemic—Ibero-American survey. J. Pediatr. Urol. 2021, 17, 402.e401–402.e407. [Google Scholar] [CrossRef] [PubMed]
- Mong, M.; Noguchi, K. Emergency Room Physicians’ Levels of Anxiety, Depression, Burnout, and Coping Methods During the COVID-19 Pandemic. J. Loss Trauma 2022, 27, 212–228. [Google Scholar] [CrossRef]
- Alkhamees, A.A.; Assiri, H.; Alharbi, H.Y.; Nasser, A.; Alkhamees, M.A. Burnout and depression among psychiatry residents during COVID-19 pandemic. Hum. Resour. Health 2021, 19, 46. [Google Scholar] [CrossRef]
- Alwashmi, A.H.; Alkhamees, A.A. Burnout and the Psychological Impact among Physiatrists in Saudi Arabia during COVID-19. IJERPH 2021, 18, 9621. [Google Scholar] [CrossRef]
- Hussain, M.; Amjad, M.B.; Ahsan, J.; Minhas, S.O. Implementation of National Institute of Health Guidelines and Other Factors Contributing to Work-Related Burnout in Covid Isolation Ward and ICU Physicians. J. Ayub Med. Coll. Abbottabad 2021, 33, 283–288. [Google Scholar]
- Asghar, M.S.; Yasmin, F.; Alvi, H.; Shah, S.M.I.; Malhotra, K.; Farhan, S.A.; Ali Naqvi, S.A.; Yaseen, R.; Anwar, S.; Rasheed, U. Assessing the Mental Impact and Burnout among Physicians during the COVID-19 Pandemic: A Developing Country Single-Center Experience. Am. J. Trop. Med. Hyg. 2021, 104, 2185–2189. [Google Scholar] [CrossRef]
- Dinibutun, S.R. Factors Associated with Burnout Among Physicians: An Evaluation During a Period of COVID-19 Pandemic. J. Healthc. Leadersh. 2020, 12, 85–94. [Google Scholar] [CrossRef]
- Tuna, T.; Özdin, S. Levels and Predictors of Anxiety, Depression, and Burnout Syndrome in Physicians during the COVID-19 Pandemic. Int. J. Ment. Health Addict. 2021, 19, 2470–2483. [Google Scholar] [CrossRef] [PubMed]
- Buran, F.; Altın, Z. Burnout among physicians working in a pandemic hospital during the COVID-19 pandemic. Leg. Med. 2021, 51, 101881. [Google Scholar] [CrossRef] [PubMed]
- Treluyer, L.; Tourneux, P. Burnout among paediatric residents during the COVID-19 outbreak in France. Eur. J. Pediatr. 2021, 180, 627–633. [Google Scholar] [CrossRef] [PubMed]
- Baptista, S.; Teixeira, A.; Castro, L.; Cunha, M.; Serrão, C.; Rodrigues, A.; Duarte, I. Physician Burnout in Primary Care during the COVID-19 Pandemic: A Cross-Sectional Study in Portugal. J. Prim. Care Community Health 2021, 12, 21501327211008437. [Google Scholar] [CrossRef]
- Azoulay, E.; De Waele, J.; Ferrer, R.; Staudinger, T.; Borkowska, M.; Povoa, P.; Iliopoulou, K.; Artigas, A.; Schaller, S.J.; Hari, M.S.; et al. Symptoms of burnout in intensive care unit specialists facing the COVID-19 outbreak. Ann. Intensiv. Care 2020, 10, 110. [Google Scholar] [CrossRef] [PubMed]
- Meynaar, I.A.; Ottens, T.; Zegers, M.; van Mol, M.M.C.; van der Horst, I.C.C. Burnout, resilience and work engagement among Dutch intensivists in the aftermath of the COVID-19 crisis: A nationwide survey. J. Crit. Care 2021, 62, 1–5. [Google Scholar] [CrossRef]
- Dimitriu, M.C.T.; Pantea-Stoian, A.; Smaranda, A.C.; Nica, A.A.; Carap, A.C.; Constantin, V.D.; Davitoiu, A.M.; Cirstoveanu, C.; Bacalbasa, N.; Bratu, O.G.; et al. Burnout syndrome in Romanian medical residents in time of the COVID-19 pandemic. Med. Hypotheses 2020, 144, 109972. [Google Scholar] [CrossRef]
- Macía-Rodríguez, C.; Alejandre de Oña, Á.; Martín-Iglesias, D.; Barrera-López, L.; Pérez-Sanz, M.T.; Moreno-Diaz, J.; González-Munera, A. Burn-out syndrome in Spanish internists during the COVID-19 outbreak and associated factors: A cross-sectional survey. BMJ Open 2021, 11, e042966. [Google Scholar] [CrossRef]
- Mion, G.; Hamann, P.; Saleten, M.; Plaud, B.; Baillard, C. Psychological impact of the COVID-19 pandemic and burnout severity in French residents: A national study. Eur. J. Psychiatry 2021, 35, 173–180. [Google Scholar] [CrossRef]
- Ismail, T.I.; Shehata, S.F.; Mahrous, R.S.S. Occupational stress and burnout among frontline Egyptian anesthesiologists during COVID-19 outbreak in Egypt. Egypt. J. Anaesth. 2021, 37, 91–99. [Google Scholar] [CrossRef]
- Abdelhafiz, A.S.; Ali, A.; Ziady, H.H.; Maaly, A.M.; Alorabi, M.; Sultan, E.A. Prevalence, Associated Factors, and Consequences of Burnout Among Egyptian Physicians during COVID-19 Pandemic. Front. Public Health 2020, 8, 590190. [Google Scholar] [CrossRef] [PubMed]
- Elhadi, M.; Msherghi, A.; Elgzairi, M.; Alhashimi, A.; Bouhuwaish, A.; Biala, M.; Abuelmeda, S.; Khel, S.; Khaled, A.; Alsoufi, A.; et al. Burnout Syndrome among Hospital Healthcare Workers during the COVID-19 Pandemic and Civil War: A Cross-Sectional Study. Front. Psychiatry 2020, 11, 579563. [Google Scholar] [CrossRef] [PubMed]
- Elghazally, S.A.; Alkarn, A.F.; Elkhayat, H.; Ibrahim, A.K.; Elkhayat, M.R. Burnout Impact of COVID-19 Pandemic on Health-Care Professionals at Assiut University Hospitals, 2020. IJERPH 2021, 18, 5368. [Google Scholar] [CrossRef] [PubMed]
- Barello, S.; Palamenghi, L.; Graffigna, G. Stressors and Resources for Healthcare Professionals During the Covid-19 Pandemic: Lesson Learned From Italy. Front. Psychol. 2020, 11, 2179. [Google Scholar] [CrossRef] [PubMed]
- Barker, G.G.; Volk, F.; Peters, C. Cultural influences on burnout: A Swedish and American comparison. Int. J. Workplace Health Manag. 2020, 14, 181–200. [Google Scholar] [CrossRef]
- Dyrbye, L.N.; West, C.P.; Satele, D.; Boone, S.; Tan, L.; Sloan, J.; Shanafelt, T.D. Burnout Among U.S. Medical Students, Residents, and Early Career Physicians Relative to the General U.S. Population. Acad. Med. 2014, 89, 443–451. [Google Scholar] [CrossRef]
- Bretland, R.J.; Thorsteinsson, E.B. Reducing workplace burnout: The relative benefits of cardiovascular and resistance exercise. PeerJ 2015, 3, e891. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alkhamees, A.A.; Aljohani, M.S.; Kalani, S.; Ali, A.M.; Almatham, F.; Alwabili, A.; Alsughier, N.A.; Rutledge, T. Physician’s Burnout during the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2023, 20, 4598. https://doi.org/10.3390/ijerph20054598
Alkhamees AA, Aljohani MS, Kalani S, Ali AM, Almatham F, Alwabili A, Alsughier NA, Rutledge T. Physician’s Burnout during the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2023; 20(5):4598. https://doi.org/10.3390/ijerph20054598
Chicago/Turabian StyleAlkhamees, Abdulmajeed A., Moath S. Aljohani, Simindokht Kalani, Amira Mohammed Ali, Fahad Almatham, Afnan Alwabili, Naif Abdullah Alsughier, and Thomas Rutledge. 2023. "Physician’s Burnout during the COVID-19 Pandemic: A Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 20, no. 5: 4598. https://doi.org/10.3390/ijerph20054598
APA StyleAlkhamees, A. A., Aljohani, M. S., Kalani, S., Ali, A. M., Almatham, F., Alwabili, A., Alsughier, N. A., & Rutledge, T. (2023). Physician’s Burnout during the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 20(5), 4598. https://doi.org/10.3390/ijerph20054598








