Abstract
Objective: Chronic Ankle Instability (CAI) or Functional Ankle Instability (FAI) is a condition characterized by laxity and mechanical instability in the ankle joint. This instability interferes with the activities and physical-functional parameters of athletes, which leads to repetitive ankle sprains. The current systematic review was carried out to identify the effects of whole-body vibration exercise (WBVE) in athletes with CAI. Methods: We conducted electronic searches in Pubmed, the Cochrane Library, Embase, Web of Science, Scopus, Science Direct, Allied Health Literature (CINAHL) and Academic Search Premier (ASP) (EBSCO) databases on 26 February 2022. Registers were identified, and studies were selected for inclusion according to the eligibility criteria. The methodological quality was assessed by the Physiotherapy Evidence Database (PEDro) scale. Results: Seven studies were included with a mean methodological quality score of 5.85, considered ‘regular’ quality on the PEDro scale. WBVE interventions in athletes with CAI showed that this exercise contributes to a better response on parameters of neuromuscular performance, muscle strength and consequently in balance and postural control, variables that are for the management of CAI. Conclusion: WBVE interventions in sports modalities promote physiological responses that may lead to positive effects in several parameters. The protocols proposed in each modality can be carried out in practice and are considered effective additional exercise and training methods beyond traditional types of training for athletes. However, more studies are needed on athletes with this condition, with specific protocols, to highlight the possible physiological and physical-functional responses. Protocol study registration: PROSPERO (CRD42020204434).
1. Introduction
Ankle injuries are common, especially in physically active individuals, and the second most injured part of the body during sports practice is the complex of the ankle joint. Indeed, ankle sprains are one of the most common musculoskeletal injuries among athletes, representing approximately 25–30% of all sport-related injuries [1,2]. The high incidence of acute ankle sprains varies quote by sport, with the highest rates usually reported in sports that involve running, cutting, and jumping, such as football, soccer, basketball, and volleyball [3,4]. This is mainly related to the biomechanics of sports movements, which involve jumping, running, and changing direction [5]. Additionally, Pietro et al. have shown that it is possible that the surface of artificial grass soccer fields contributes to causing more injuries than the natural grass surface in amateur footballers [6].
The ankle functions as a joint complex with cooperation from the talocrural, subtalar, and inferior tibiofibular joints. Typically, lateral ankle sprains occur when the rearfoot undergoes excessive supination with an externally rotated lower leg [7]. Studies suggest that about 73% of individuals affected by ankle sprains may develop residual physical disabilities characterized by persistent symptoms and features, including acute pain, swelling, muscle weakness, loss of range of motion (ROM), deficits in postural control, and joint-sagging sensations. Consequently, there is an increase in recurrent injury with the development of chronic ankle instability (CAI), which denotes the occurrence of repetitive bouts of lateral ankle instability, promoting various ankle sprains [7,8,9,10].
CAI may be due to mechanical instability, functional instability, or, most likely, a combination of these two phenomena. Mechanical instability may be due to specific insufficiencies such as laxity, arthrokinematic changes, synovial inflammation, or degenerative changes. Functional instability would be caused by insufficiencies in neuromuscular control and proprioception. [2,11].
CAI results from a combination of deficits in strength, proprioception [12,13], and neuromuscular control [14], including increased peroneal reaction time [15], reduced activity of the tibialis anterior and peroneus longus [16], an impaired sense of joint position and range of motion [9,10], and decreased balance, and postural stability [13,17,18].
In this context, different exercises that can yield benefits in terms of disabilities due to CAI in athletes have been investigated in this clinical condition, including rehabilitation programs with balance training [19,20,21], strength [20,22], stimuli mechanical vibration, as systemic vibratory therapy (SVT), [10,23,24] and combined training [25,26,27]. However, the evidence is conflicting, and there remains a gap in the literature regarding which type of intervention is most effective and which intervention should be performed after an ankle injury, specifically in athletes, to enable a safe return to sports activity.
SVT promotes the whole-body vibration exercise (WBVE) whereby the individual is in contact with the base of a vibrating platform (VP), which generates mechanical vibrations that are transmitted to the body of the individual. Several parameters must be clearly defined, such as the frequency, amplitude, peak-to-peak displacement, work time, rest time, periodicity of the sessions, and positioning on the VP, amongst others [28,29,30,31].
During WBVE, the mechanical vibrations transmitted by the VP are thought to interact with skin receptors, muscle spindles and joint mechanoreceptors, activating alpha motoneurons that lead to muscle contractions [32,33]. These contractions promoted by WBVE can influence joint stability. Consequently, improvements can be observed in sensorimotor deficits involving balance, joint position sense, and dynamic postural control, with greater brain activity, strength, power, flexibility, and adaptations in motor control, even in populations with joint instability [34,35,36,37,38,39,40,41,42]. Furthermore, in studies with SVT, as a strategy of intervention for athletes, different postures of the individuals and exercises in the base of VP were considered, ranging from one-legged and two-legged exercises, with and without heel lift, involving balance and stability [34,35,36,37,38,39,40,41,42].
In this context, WBVE is a biophysical modality that provides systemic mechanical vibration signals through mechanical stimulation and is an exercise strategy that is gaining popularity and is being increasingly used as a preventive and rehabilitation tool. Currently, there is only one systematic review about WBVE and sensorimotor effects that supports the use of WBVE to improve sensorimotor deficits involving strength, balance, muscle activity, and joint position sense, but it was in individuals with CAI, not athletes [43]. Considering this rationale, the idea is to present the possibility of using an efficient exercise program to assist in the dysfunctions promoted by CAI, which is useful to stimulate the physical-functional performance of the athlete, as well as the return to sports practice. So, the aim of this study was to present a systematic review to identify the effects of WBVE in athletes with CAI.
2. Materials and Methods
The review was realized according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA, Supplementary Materials) guidelines [44] and the Synthesis without meta-analysis (SWiM) in systematic reviews [45]. The protocol for the review was registered with the International Prospective Register of Systematic Reviews (PROSPERO—CRD42020204434).
2.1. Search Strategy
An electronic search in databases was realized in Pubmed, Cochrane Library, Embase, Scopus, Science Direct, Web of Science, Allied Health Literature (CINAHL) and Academic Search Premier (ASP) (EBSCO) on 3 September 2021 and updated on 26 February 2023, using the following search strings: (“whole body vibration” OR “vibration therapy” OR “vibration training”) AND (“chronic ankle instability” OR “ankle instability” OR “functional ankle instability” OR “mechanical ankle instability” OR “recurrent ankle instability”). Using the PICOS strategy, the keywords used in the search were defined, such as athletes with CAI (Participants) receiving WBVE intervention (Intervention), allowing comparison to control/no intervention, placebo or usual care (Comparison). All reported outcomes related to balance, muscle strength, muscle activity and body composition (Outcomes) were allowed if they were considered relevant to the population studied and were “randomized clinical trials” (RCT) (Study design) [46]. Additionally, a hand search was performed in gray literature and in studies references.
2.2. Eligibility Criteria
Inclusion criterion: RCT, studies with the use of WBVE in athletes with ankle instability, independently of the year of the publication, and with no restrictions on language.
Exclusion criteria: Congress abstracts, incomplete articles, abstracts, pilot studies, protocols, postintervention results not reported, and findings not related to CAI and athletes and WBVE.
2.3. Level of Evidence of the Selected Articles
The level of evidence of the included studies was evaluated using the National Health and Medical Research Council hierarchy of evidence [47] and defined according to below Table 1.

Table 1.
Level Classification.
2.4. Methodological Quality and Risk of Bias
The Physiotherapy Evidence Database (PEDro)scale (http://www.pedro.org.au/english/downloads/pedro-scale/ (accessed on 5 April 2022)), with eleven items, was used to the methodological quality of the randomized controlled trials included. The first item of the PEDro scale is related to external validity and is not used to calculate the scale score. Therefore, the scores range from 0 to 10. Articles with a score greater than or equal to 7 were of ‘high’ methodological quality, those with a score of 5 to 6 were of ‘regular’ quality, and those with a score of 4 or less were of ‘poor’ quality [48,49].
The Cochrane Collaboration tool, with 7 domains, was used to assess the risk of bias in the articles included. The domains encompass selection, performance, detection, attrition, reporting, and other sources of bias. The domains are classified into 1 of 3 categories: low, high or uncertain risk of bias [50].
2.5. Selections and Data Extraction
All references found by the database searches were exported to a data management software (EndNote X9 (Clarivate Analytics, London, UK)), and duplicates were removed. Studies were independently reviewed by 2 authors (A.C.C.-O. and J.P.-F.) according to the eligibility criteria at all stages of the review. If disagreements could not be resolved through discussion, a third reviewer (DC) was consulted. For data extraction, both reviewers extracted the following information: study information (author and year), study design, subjects (sample size), demographics characteristics (age, sex, body mass index), modality of athletes, instruments, tests/measured variables, WBVE intervention, WBVE protocols, and outcomes.
3. Results
A total of 135 records were identified through database searches (Pubmed = 14, Cochrane Library = 22, Embase = 16, Scopus = 18, Science Direct = 22, Web of Science = 24, CINAHL = 8 and ASP (EBSCO) = 11) and, after the removal of 76 duplicates, 59 studies were identified. During the screening process, the titles and abstracts of 59 publications were read, and 47 were excluded because they were abstracts, reviews (systematic, scoping or narrative), and meta-analyses, they did not meet the topic criteria, were with individuals or patients with CAI and did not use vibratory therapy. The complete text of 12 publications was reviewed in detail. After careful analysis, five studies were excluded because they were not athletes with CAI and because they did not contain available results. Finally, seven articles were included in the current systematic review. The selection process is shown in Figure 1.
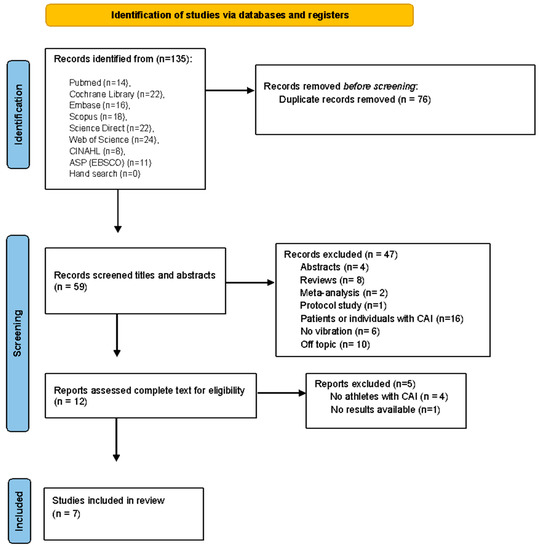
Figure 1.
PRISMA flow diagram of the study selection process.
The publications included had a mean methodological quality score of 5.85 as assessed, with the PEDro scale (Figure 2), with a minimum of 3 points and a maximum of 7, reflecting ‘regular’ methodological quality. Only in one study [51] was the allocation of groups performed blindly, and no included study was able to blind all subjects or therapists who administered the therapy; two studies [40,51] applied the blinding of all assessors who measured at least one key outcome, three studies [10,23,36] did not provide at least one key result; only one study [23] failed to provide measurements of all outcomes.
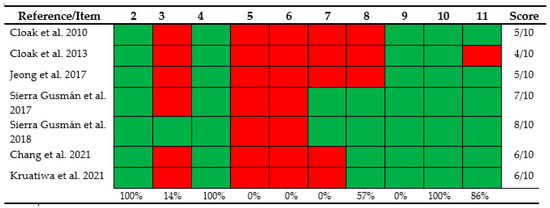
Figure 2.
Assessment of the methodological quality of the included studies using the PEDro scale. (2) Subjects were randomly allocated to groups; (3) allocation concealed; (4) the groups were similar at baseline regarding the prognostic indicators; (5) was blinding of all subjects; (6) was blinding of all therapists who administered the intervention; (7) was blinding of all assessors who measured at minimal one key outcome; (8) measures of at least one key outcome were obtained from more than 85%; of the subjects firstly allocated to groups; (9) all subjects for whom outcome measures were disposable received the treatment or control condition as allocated or, where this was not possible, data for at least one key outcome was analyzed by “intention to treat”; (10) the results of between-group statistical comparisons are reported for at minimal one key outcome; (11) the study give both point measures and measures of variability for at minimal one key outcome [10,23,24,26,36,40,51].
For the risk of bias (Figure 3), among the studies included in this review, only one study [51] guaranteed that it performed allocation concealment, five studies [10,23,26,40,51] did not involve blinding of participants and personnel, two studies [24,36] presented insufficient information to judge this domain. Two studies [40,51] blinded the evaluation of the results, all studies included had no missing data, and all reported the results of the variables analyzed. However, according to the Cochrane classification tool, all the studies included had the potential for other biases due to methodological flaws. The articles included in this review were finally classified as high-risk (two studies [10,23]), low-risk (two studies [40,51]), and uncertain risk (three studies [24,26,36]).
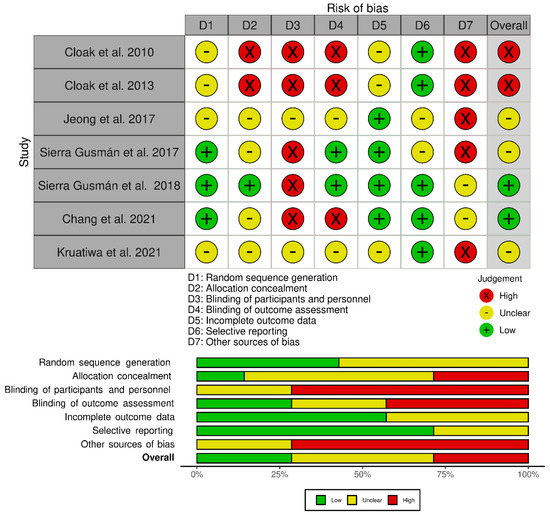
Figure 3.
Assessment for risk of bias for the included studies [10,23,24,26,36,40,51].
Table 2 displays the characteristics of the articles included, including the author and year of the study, the participants involved, the objectives, the variables evaluated, the results found and the level of evidence. The level of evidence (NHMRC, 2003–2007) [47] of all selected studies was Level of Evidence II.

Table 2.
Table of the characteristics of selected studies.
Regarding the main findings (Table 2), WBVE: improves single-leg balance and SEBT performance in dancers with unilateral functional ankle instability (FAI) [10]; Combined vibration and wobble board training improves COM distribution, modified SEBT scores, and SLTHD among footballers suffering from FAI [23] and may have a beneficial effect on the improvement of lower extremity muscle activity and balance ability in CAI football players [36]. WBVE improved the RT of the PB, PL and TA muscles in CAI recreational athletes [40]; resulted in different enhancements in balance ability on the BBS and SEBT [51]; exhibited very small or small effect sizes for CAI in the SEBT, the joint position sense test, and the isokinetic strength test [26]; and, it appears that the WBT is superior to the conventional PPT program for improving dynamic balance in athletes with FAI while COM and ECC were enhanced at an ankle inversion of 30°/s [24].
The sample sizes ranged from 30 to 63 athletes (totaling 300 athletes, 155 female, 95 male, and 50 unspecified), the average age was 21.5 years and included dancers [10], football [23] or soccer players [36], women’s basketball and volleyball teams [26], physically active recreational athletes [40,51], and collegiate athletes (basketball, football, netball, and handball players) [24], and the conditions varied between unilateral [10,23,40] and bilateral [24,51] ankle instability, and two studies [26,36] did not report specific instability.
The protocols and biomechanical parameters of the WBVE (frequency, peak-to-peak displacement, positioning of the individual at the base of the VP, the VP model and the type of stimulus) are reported in Table 3.

Table 3.
Protocol for WBVE interventions with selected studies.
Considering the biomechanical parameters, the vibration frequencies used ranged from 5 to 50 Hz; only one publication defined only the frequency of 5 Hz [26], one study used a progressive frequency from 5 to 25 Hz [33], four studies used frequencies of 30, 35 and 40 Hz [10,23,40,51], and only one article reported frequencies of 30, 40, and 50 Hz [24], on the other hand, the amplitude varied between 2 mm and 8 mm [24,26,36,40,51], and two studies did not report which amplitude was used during vibration [10,23].
Considering the WBVE intervention protocols, in general, the included studies used the VP or other vibration devices with synchronous and alternating vertical stimuli. Four studies used another tool on top of the VP [26,36,40,51], one study performed the exercise directly on the VP [24], and two studies used another vibrating device [10,23]. In five studies, the participants were barefoot [10,23,26,40,51], and in two studies [24,36], they were wearing sneakers. Participants performed different positions and exercises on the platform, ranging from two-legged and one-legged exercises, with and without heel lift, involving balance and stability; the working time involved training lasting from 10 to 30 min, including protocols with progressive training as the exercise weeks progressed.
All studies included were homogeneous with regard to the time of application of the WBVE protocol lasting 6 weeks; however, five studies [24,26,36,40,51] used a frequency of three times a week, totaling 18 sessions, and two [10,23] twice a week, totaling 12 sessions.
4. Discussion
The main goal of this systematic review was to identify the effects of WBVE in athletes with ankle instability. After analyzing the studies included and considering their limitations, the results suggest that WBVE may be a feasible and valid intervention for athletes with CAI. The methodological quality of the included studies was regular. However, according to the risk of bias, the included clinical trials have methodological errors and still lack detailed information on the methods used and which may compromise their internal validity.
As observed, among the consequences of CAI, there is a deficit in balance and stability. Five included studies [10,23,24,36,51] suggest that vibration provided additional benefits regarding improvements in unipedal balance, dynamic balance, center of mass distribution (COM), and SEBT, MSEBT, SLTHD, and BBS test performance and scores, even with the authors using different VP devices, different WBVE protocols and parameters, as well as different athlete modalities. Corroborating with these findings, Sofla et al. [52] and Tohidast et al. [53] also suggest that WBVE may induce some improvement in postural control in individuals with CAI using protocols of 4 and 6 weeks of vibration, respectively. On the other hand, Chang et al., 2021 [26] observed very small or small effect sizes for the vibration results in the balance and stability test in athletes. Moreover, Adelman et al., 2016 [54] and Rendos et al. [39] did not observe significant changes with WBVE in terms of balance/stability; however, these studies used an acute effect WBVE protocol (a single session), and the participants were not athletes, which suggests that one session would not be enough to promote changes and adaptations in these parameters regardless of physical activity level. The tests performed in the pre- and post-intervention studies with WBVE are considered indicative of postural control, and balance training improves the individual’s ability to maintain the center of gravity and posture, stimulating the musculoskeletal and vestibular systems. Therefore, stability is the result of the activation of the proprioceptive system and is of fundamental importance for the performance of motor tasks, mainly in the ca of athletes with CAI [24,55].
Regarding muscle strength, Sierra-Guzman et al. [40] and Chang et al. [26] did not find significant results regarding muscle strength of the ankle muscles or found very small or small effects after the intervention, suggesting that the WBVE protocols and parameters applied in the studies (frequency of 30, 35 and 40 Hz and amplitude varying from 2 to 4 mm, and 5 Hz and 3 mm, respectively), may not have promoted sufficient stimuli to provide an increase in the isokinetic strength of the ankle invertor and evertor muscles, even with 6 weeks of training. Similarly, Sofla et al. [52] did not observe significant changes regarding ankle muscle strength in individuals with CAI with a 4-week protocol (frequency 30–40 Hz and 3 mm amplitude) of vibration exercises. In the studies by Sierra-Guzman et al. [40], Chang et al. [26] and Sofla et al. [52], although they used different protocols, exercises and populations, strength was assessed with an isokinetic dynamometer, considered the “gold standard” instrument to measure muscle strength and performance [56]. On the other hand, Cloak et al. [23] observed significant effects on strength with the combined vibration and oscillating board training; however, they used the triple jump test for distance (SLTHD) to assess muscle strength, which is a valid clinical tool to assess strength and power characteristics. The reported differences in ankle, knee, and hip kinematics, kinetics, and muscle activation patterns in individuals with CAI, could be due to those lower limb muscle strength deficits and imbalances, and the proposed WBVE protocols, although progressive and associated with exercises, were not sufficient to balance the musculatures involved to support the sports demand of athletes.
Considering that CAI is one of the commonly observed sports conditions, and given that it causes decreased neuromuscular control and loss of proprioception, with respect to the results for muscle activation, Jeong et al., 2017 [36] suggest that WBVE may have a beneficial effect in improving muscle activity of the lower limbs in soccer players, as well as Cloak et al., 2010 [10] found that WBVE can lead to long term effects in the recruitment of motor units of the peroneus longus in dancers. These findings suggest that effective exercise protocols, independent of the type of vibrating platform, stimulus intensity and exposure time, can be used to increase α motor neuron excitability and motor unit synchronization to increase ankle motor control. In contrast, Sierra-Guzman et al., 2017 [40] found no significant changes in EMG activity after a 6-week WBVE training program on a soft surface, although it could improve ankle muscle RT of the PB, PL and TA muscles in recreational athletes with CAI. Similarly, Otzel et al., 2019 [57] observed changes in motoneuron function with a single session of WBVE, suggesting that both acute and cumulative protocols did not represent a sufficient stimulus to the ankle muscles. Neuromuscular control is therefore important for athletes as it helps maintain functional ankle stability, while proprioception influences the sensation of movement and the ankle joint position.
The strength of the current systematic review lies in offering a possibility for an efficient exercise program to counter the dysfunctions promoted by CAI and useful to stimulate the physical-functional performance of the athlete, as well as the return to sports practice with greater safety and, consequently, less chance of recurrence of the lesion that promoted instability. However, this systematic review has some limitations, and the results should be interpreted with caution. Despite the positive results of interventions with WBVE, the diversity of WBVE training protocols makes it difficult to interpret the findings. On the other hand, there is also a lack of objective evidence to support the use of WBVE in athletes with CAI. In addition, different sports modalities were studied, each with different characteristics which may influence the athlete’s performance. Therefore, it is not possible to draw convincing conclusions based on a small number of relevant studies (only seven publications) evaluating WBVE intervention in the athletic population. In addition, some studies used multiple instruments or tools together with the vibration stimulus, and it was not possible to evaluate the vibration stimulus alone.
In this context, as facts and perspectives, the WBVE is a systemic mechanical vibration intervention capable of stimulating the physical-functional performance of the athletes through efficient exercise to promote benefits in the dysfunctions promoted by CAI. Regarding its prospects, and in view of the limitations of the association of WBVE with other “interventions,” it would be interesting that more studies on systemic vibration, applying WBVE alone, focusing on protocol parameters that would help determine the most efficient and effective protocol to promote beneficial effects in athletes with CAI.
5. Conclusions
WBVE interventions in athletes with CAI show that this exercise method improves the response in parameters of neuromuscular performance, muscle strength and, consequently, balance and postural control, which are all indispensable variables for the management of this clinical condition. However, more studies are needed on athletes with this condition, with specific protocols, to highlight the possible physiological and physical-functional responses. The implementation of WBVE interventions in this population, regardless of the sport modality, promotes positive effects in several parameters and is a viable intervention to be carried out in practice. However, more studies are indeed needed to investigate the effects of WBVE in athletes with CAI, as there is evidence that WBVE can be an additional exercise, promising and effective, as a training method beyond traditional types of training for athletes.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph20054522/s1, PRISMA 2020 Checklist.
Author Contributions
Conceived and designed the review: A.C.C.-O., J.P.-F., A.R.-S., L.T.J.-A. and M.B.-F. Performed the review steps: A.C.C.-O., J.P.-F., L.F.F.-S., A.R.-S., L.T.J.-A., A.L. and M.C.M.-F. Analyzed the data (interpreted results of experiments, prepared figures, drafted manuscript, edited and revised manuscript): A.C.C.-O., A.R.-S., L.T.J.-A., A.L., L.F.F.-S., V.A.M., A.C.R.L., B.S., R.T., F.C.B., A.S., M.B.-F. and D.S.-C. Contributed materials/analysis tools: A.C.C.-O., V.A.M., A.C.R.L., B.S., R.T., A.S., F.C.B., M.B.-F., A.R. and D.S.-C. All authors have read and agreed to the published version of the manuscript.
Funding
The authors would like to thank the national public agencies for academic support, Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), Fundação Carlos Chagas Filho de Amparo à Pesquisa do Estado do Rio de Janeiro (FAPERJ), and Coordenação de Aperfeiçoamento de Pessoal de Nível Superior—Brazil (CAPES)—Finance Code 001.
Institutional Review Board Statement
The study is a systematic review and was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and MetaAnalysis (PRISMA) Guidelines, and the methods were prespecified in a protocol with the PROSPERO International Prospective Register of Systematic Reviews (CRD42020204434).
Informed Consent Statement
Not applicable.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Acknowledgments
The authors are thankful to Conselho Nacional de Pesquisa e Desenvolvimento (CNPq), Fundação de Amparo à Pesquisa do Estado do Rio de Janeiro (FAPERJ), Coordenação de Aperfeiçoamento de Pessoal de Nível Superior—Brazil (CAPES)—Finance Code 001 and Universidade do Estado do Rio de Janeiro (UERJ) for the financial support.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Fong, D.T.; Hong, Y.; Chan, L.K.; Yung, P.S.; Chan, K.M. A systematic review on ankle injury and ankle sprain in sports. Sport. Med. 2007, 37, 73–94. [Google Scholar] [CrossRef] [PubMed]
- Jaber, H.; Lohman, E.; Daher, N.; Bains, G.; Nagaraj, A.; Mayekar, P.; Shanbhag, M.; Alameri, M. Neuromuscular control of ankle and hip during performance of the star excursion balance test in subjects with and without chronic ankle instability. PLoS ONE 2018, 13, e0201479. [Google Scholar] [CrossRef] [PubMed]
- Gribble, P.A.; Bleakley, C.M.; Caulfield, B.M.; Docherty, C.L.; Fourchet, F.; Fong, D.T.; Hertel, J.; Hiller, C.E.; Kaminski, T.W.; McKeon, P.O.; et al. Evidence review for the 2016 International Ankle Consortium consensus statement on the prevalence, impact and long-term consequences of lateral ankle sprains. Br. J. Sport. Med. 2016, 50, 1496–1505. [Google Scholar] [CrossRef] [PubMed]
- Doherty, C.; Delahunt, E.; Caulfield, B.; Hertel, J.; Ryan, J.; Bleakley, C. The incidence and prevalence of ankle sprain injury: A systematic review and meta-analysis of prospective epidemiological studies. Sport. Med. 2014, 44, 123–140. [Google Scholar] [CrossRef] [PubMed]
- Silva, D.C.F.; Santos, R.; Vilas-Boas, J.P.; Macedo, R.; Montes, A.M.; Sousa, A.S.P. Different Cleat Models do Not Influence Side Hop Test Performance of Soccer Players with and without Chronic Ankle Instability. J. Hum. Kinet. 2019, 70, 156–164. [Google Scholar] [CrossRef]
- Pietro, M.; Rocco, S.; Felice, S.; Madonna, G.; Filomena, M. Soccer fields in synthetic and natural grass: A comparative study on muscular injuries of the lower limb. Sport Sci. 2020, 14, 7–12. [Google Scholar]
- Hertel, J. Functional Anatomy, Pathomechanics, and Pathophysiology of Lateral Ankle Instability. J. Athl. Train. 2002, 37, 364–375. [Google Scholar]
- Tropp, H. Commentary: Functional Ankle Instability Revisited. J. Athl. Train. 2002, 37, 512–515. [Google Scholar]
- Wenning, M.; Schmal, H. Chronic Ankle Instability—Mechanical vs. Functional. Z. Fur Orthop. Und Unf. 2022, Epub ahead of print. [CrossRef]
- Cloak, R.; Nevill, A.M.; Clarke, F.; Day, S.; Wyon, M.A. Vibration training improves balance in unstable ankles. Int. J. Sport. Med. 2010, 31, 894–900. [Google Scholar] [CrossRef]
- Safran, M.R.; Benedetti, R.S.; Bartolozzi, A.R., 3rd; Mandelbaum, B.R. Lateral ankle sprains: A comprehensive review: Part 1: Etiology, pathoanatomy, histopathogenesis, and diagnosis. Med. Sci. Sport. Exerc. 1999, 31, S429–S437. [Google Scholar] [CrossRef] [PubMed]
- Xue, X.; Ma, T.; Li, Q.; Song, Y.; Hua, Y. Chronic ankle instability is associated with proprioception deficits: A systematic review and meta-analysis. J. Sport Health Sci. 2021, 10, 182–191. [Google Scholar] [CrossRef]
- Alghadir, A.H.; Iqbal, Z.A.; Iqbal, A.; Ahmed, H.; Ramteke, S.U. Effect of Chronic Ankle Sprain on Pain, Range of Motion, Proprioception, and Balance among Athletes. Int. J. Environ. Res. Public Health 2020, 17, 5318. [Google Scholar] [CrossRef]
- Gribble, P.A.; Delahunt, E.; Bleakley, C.; Caulfield, B.; Docherty, C.L.; Fourchet, F.; Fong, D.; Hertel, J.; Hiller, C.; Kaminski, T.W.; et al. Selection criteria for patients with chronic ankle instability in controlled research: A position statement of the International Ankle Consortium. J. Orthop. Sport. Phys. Ther. 2013, 43, 585–591. [Google Scholar] [CrossRef] [PubMed]
- Kavanagh, J.J.; Bisset, L.M.; Tsao, H. Deficits in reaction time due to increased motor time of peroneus longus in people with chronic ankle instability. J. Biomech. 2012, 45, 605–608. [Google Scholar] [CrossRef] [PubMed]
- Feger, M.A.; Donovan, L.; Hart, J.M.; Hertel, J. Lower extremity muscle activation during functional exercises in patients with and without chronic ankle instability. PM&R J. Inj. Funct. Rehabil. 2014, 6, 602–611. [Google Scholar] [CrossRef]
- Hertel, J. Sensorimotor deficits with ankle sprains and chronic ankle instability. Clin. Sports Med. 2008, 27, 353–370. [Google Scholar] [CrossRef]
- Ahern, L.; Nicholson, O.; O’Sullivan, D.; McVeigh, J.G. Effect of Functional Rehabilitation on Performance of the Star Excursion Balance Test Among Recreational Athletes With Chronic Ankle Instability: A Systematic Review. Arch. Rehabil. Res. Clin. Transl. 2021, 3, 100133. [Google Scholar] [CrossRef]
- Cain, M.S.; Ban, R.J.; Chen, Y.P.; Geil, M.D.; Goerger, B.M.; Linens, S.W. Four-Week Ankle-Rehabilitation Programs in Adolescent Athletes with Chronic Ankle Instability. J. Athl. Train. 2020, 55, 801–810. [Google Scholar] [CrossRef]
- Hall, E.A.; Chomistek, A.K.; Kingma, J.J.; Docherty, C.L. Balance- and Strength-Training Protocols to Improve Chronic Ankle Instability Deficits, Part I: Assessing Clinical Outcome Measures. J. Athl. Train. 2018, 53, 568–577. [Google Scholar] [CrossRef]
- Burcal, C.J.; Trier, A.Y.; Wikstrom, E.A. Balance Training Versus Balance Training with STARS in Patients with Chronic Ankle Instability: A Randomized Controlled Trial. J. Sport Rehabil. 2017, 26, 347–357. [Google Scholar] [CrossRef] [PubMed]
- Hall, E.A.; Chomistek, A.K.; Kingma, J.J.; Docherty, C.L. Balance-and strength-training protocols to improve chronic ankle instability deficits, part II: Assessing patient-reported outcome measures. J. Athl. Train. 2018, 53, 578–583. [Google Scholar] [CrossRef]
- Cloak, R.; Nevill, A.; Day, S.; Wyon, M. Six-Week Combined Vibration and Wobble Board Training on Balance and Stability in Footballers with Functional Ankle Instability. Clin. J. Sport Med. 2013, 23, 384–391. [Google Scholar] [CrossRef] [PubMed]
- Kruatiwa, N.; Yimlamai, T. Effects of Two Rehabilitation Programs on Dynamic Balance in Athletes with Functional Ankle Instability. J. Exerc. Physiol. Online 2021, 24, 109–119. [Google Scholar]
- Alahmari, K.A.; Kakaraparthi, V.N.; Reddy, R.S.; Silvian, P.; Tedla, J.S.; Rengaramanujam, K.; Ahmad, I. Combined Effects of Strengthening and Proprioceptive Training on Stability, Balance, and Proprioception Among Subjects with Chronic Ankle Instability in Different Age Groups: Evaluation of Clinical Outcome Measures. Indian J. Orthop. 2021, 55, 199–208. [Google Scholar] [CrossRef] [PubMed]
- Chang, W.D.; Chen, S.; Tsou, Y.A. Effects of whole-body vibration and balance training on female athletes with chronic ankle instability. J. Clin. Med. 2021, 10, 2380. [Google Scholar] [CrossRef]
- Melam, G.; Alhusaini, A.; Perumal, V.; Buragadda, S.; Albarrati, A.; Lochab, R.J.S. Effect of weight-bearing overload using elastic tubing on balance and functional performance in athletes with chronic ankle instability. Sci. Sport. 2018, 33, e229–e236. [Google Scholar] [CrossRef]
- Rittweger, J. Vibration as an exercise modality: How it may work, and what its potential might be. Eur. J. Appl. Physiol. 2010, 108, 877–904. [Google Scholar] [CrossRef]
- Rauch, F.; Sievanen, H.; Boonen, S.; Cardinale, M.; Degens, H.; Felsenberg, D.; Roth, J.; Schoenau, E.; Verschueren, S.; Rittweger, J.; et al. Reporting whole-body vibration intervention studies: Recommendations of the International Society of Musculoskeletal and Neuronal Interactions. J. Musculoskelet. Neuronal Interact. 2010, 10, 193–198. [Google Scholar]
- van Heuvelen, M.J.G.; Rittweger, J.; Judex, S.; Sañudo, B.; Seixas, A.; Fuermaier, A.B.M.; Tucha, O.; Nyakas, C.; Marín, P.J.; Taiar, R.; et al. Reporting Guidelines for Whole-Body Vibration Studies in Humans, Animals and Cell Cultures: A Consensus Statement from an International Group of Experts. Biology 2021, 10, 965. [Google Scholar] [CrossRef]
- de Sá-Caputo, D.D.C.; Seixas, A.; Taiar, R.; Bernardo-Filho, M. Vibration Therapy for Health Promotion. In Complementary Therapies; Mario, B.-F., Redha, T., Danúbia da Cunha de, S.-C., Adérito, S., Eds.; IntechOpen: Rijeka, Croatia, 2022; Chapter 12. [Google Scholar] [CrossRef]
- Musumeci, G. The Use of Vibration as Physical Exercise and Therapy. J. Funct. Morphol. Kinesiol. 2017, 2, 17. [Google Scholar] [CrossRef]
- Cardinale, M.; Bosco, C.J.E. The use of vibration as an exercise intervention. Exerc. Sport Sci. Rev. 2003, 31, 3–7. [Google Scholar] [CrossRef]
- Far, A.A.; Hedayati, R.; Bagheri, P.; Yaghubi, Z. Effects of whole body vibration on concentric torque of ankle invertor and evertor muscles in people with functional ankle instability. Koomesh 2016, 18, 286–294. [Google Scholar]
- Feland, J.B.; Thalman, L.; Hunter, I.; Hopkins, J.T. Improving Dorsiflexion ROM In Subjects with Chronic Ankle Instability with Whole Body Vibration. Med. Sci. Sport. Exerc. 2014, 46, 200. [Google Scholar] [CrossRef]
- Jeong, Y.-S.; Kim, J.-H. Effects of Whole Body Vibration Exercise on Lower Extremity Muscle Activity and Balance Ability in Football Player with Chronic Ankle Instability. J. Korean Phys. Ther. 2017, 29, 293–298. [Google Scholar] [CrossRef]
- Jun, H.P.; Harriell, K.; Kuenze, C.; Signorile, J.F. Whole Body Vibration Effect on Time-to-Boundary Measures in Persons with Chronic Ankle Instability. Med. Sci. Sport. Exerc. 2014, 46, 415–416. [Google Scholar] [CrossRef]
- Otzel, D.M.; Hass, C.J.; Wikstrom, E.A.; Bishop, M.D.; Borsa, P.A.; Tillman, M.D. Neuromotor and Functional Measures Following Whole-body Vibration in Individuals with Chronic Ankle Instability. Med. Sci. Sport. Exerc. 2013, 45, 707. [Google Scholar]
- Rendos, N.K.; Jun, H.P.; Pickett, N.M.; Lew Feirman, K.; Harriell, K.; Lee, S.Y.; Signorile, J.F. Acute effects of whole body vibration on balance in persons with and without chronic ankle instability. Res. Sport. Med. 2017, 25, 391–407. [Google Scholar] [CrossRef]
- Sierra-Guzmán, R.; Jiménez, J.F.; Ramírez, C.; Esteban, P.; Abián-Vicén, J. Effects of Synchronous Whole Body Vibration Training on a Soft, Unstable Surface in Athletes with Chronic Ankle Instability. Int. J. Sport. Med. 2017, 38, 447–455. [Google Scholar] [CrossRef] [PubMed]
- Gao, X.J.; Chu, Z.W.; Li, W.Y.; Hou, Y.; Ma, R.; Li, J. Effects of vibration training with adjusted frequency on functional ankle instability. J. Med. Biomech. 2020, 35, 685–691. [Google Scholar]
- Abstracts of the Eighth Meeting of the European Society of Biomechanics Rome, Italy, 21–24 June 1992. J. Biomech. 1993, 26, 765–908. [CrossRef]
- Tan, J.; Wu, X.; Clark, C.C.T.; Barton, V.; Chen, S.; Liu, S.; Zhou, X.; Xu, C.; Ma, T.; Qi, B.; et al. The effect of whole body vibration on sensorimotor deficits in people with chronic ankle instability: A systematic review and meta-analysis. Clin. Rehabil. 2022, 36, 1016–1031. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Int. J. Surg. 2021, 372, n71. [Google Scholar] [CrossRef]
- Campbell, M.; McKenzie, J.E.; Sowden, A.; Katikireddi, S.V.; Brennan, S.E.; Ellis, S.; Hartmann-Boyce, J.; Ryan, R.; Shepperd, S.; Thomas, J.; et al. Synthesis without meta-analysis (SWiM) in systematic reviews: Reporting guideline. BMJ 2020, 368, l6890. [Google Scholar] [CrossRef] [PubMed]
- Costantino, G.; Montano, N.; Casazza, G. When should we change our clinical practice based on the results of a clinical study? Searching for evidence: PICOS and PubMed. Intern. Emerg. Med. 2015, 10, 525–527. [Google Scholar] [CrossRef] [PubMed]
- Merlin, T.; Weston, A.; Tooher, R. Extending an evidence hierarchy to include topics other than treatment: Revising the Australian ‘levels of evidence’. BMC Med. Res. Methodol. 2009, 9, 34. [Google Scholar] [CrossRef]
- de Morton, N.A. The PEDro scale is a valid measure of the methodological quality of clinical trials: A demographic study. Aust. J. Physiother. 2009, 55, 129–133. [Google Scholar] [CrossRef]
- Maher, C.G.; Sherrington, C.; Herbert, R.D.; Moseley, A.M.; Elkins, M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys. Ther. 2003, 83, 713–721. [Google Scholar] [CrossRef]
- De Carvalho, A.; Silva, V.; Grande, A.J.D.T. Avaliação do risco de viés de ensaios clínicos randomizados pela ferramenta da colaboração Cochrane. Diagn Trat. 2013, 18, 38–44. [Google Scholar]
- Sierra-Guzmán, R.; Jiménez-Diaz, F.; Ramírez, C.; Esteban, P.; Abián-Vicén, J. Whole-Body—Vibration Training and Balance in Recreational Athletes with Chronic Ankle Instability. J. Athl. Train. 2018, 53, 355–363. [Google Scholar] [CrossRef]
- Shamseddini Sofla, F.; Hadadi, M.; Rezaei, I.; Azhdari, N.; Sobhani, S. The effect of the combination of whole body vibration and shoe with an unstable surface in chronic ankle instability treatment: A randomized clinical trial. BMC Sport. Sci. Med. Rehabil. 2021, 13, 28. [Google Scholar] [CrossRef] [PubMed]
- Tohidast, S.A.; Bagheri, R.; Safavi-Farokhi, Z.; Khaleghi Hashemian, M.; Delkhosh, C.T. The Effects of Acute and Long-Term Whole-Body Vibration Training on the Postural Control During Cognitive Task in Patients with Chronic Ankle Instability. J. Sport Rehabil. 2021, 30, 1121–1128. [Google Scholar] [CrossRef] [PubMed]
- Adelman, D.; Pamukoff, D.; Goto, S.; Guskiewicz, K.; Ross, S.; Blackburn, T. Acute Effects of Whole Body Vibration on Dynamic Postural Control and Muscle Activity in Individuals with Chronic Ankle Instability. Athl. Train. Sport. Health Care 2016, 8, 63–69. [Google Scholar] [CrossRef]
- Ergen, E.; Ulkar, B. Proprioception and ankle injuries in soccer. Clin. Sport. Med. 2008, 27, 195–217. [Google Scholar] [CrossRef] [PubMed]
- Hartsell, H.D.; Spaulding, S.J. Eccentric/concentric ratios at selected velocities for the invertor and evertor muscles of the chronically unstable ankle. Br. J. Sport. Med. 1999, 33, 255–258. [Google Scholar] [CrossRef] [PubMed]
- Otzel, D.M.; Hass, C.J.; Wikstrom, E.A.; Bishop, M.D.; Borsa, P.A.; Tillman, M.D. Motoneuron Function Does not Change Following Whole-Body Vibration in Individuals with Chronic Ankle Instability. J. Sport Rehabil. 2019, 28, 614–622. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).