Abstract
The purpose of this study was to investigate the relationship between cognitive function and depressive symptoms among Chinese adults aged 40 years and above, as well as the series of multiple mediating effects of Instrument Activities of Daily Living disability and life satisfaction on this relationship. The data was obtained from the China Health and Retirement Longitudinal Study (CHARLS, 2013–2018), including 6466 adults aged 40 years and above. The mean age of the adults was 57.7 ± 8.5. The SPSS PROCESS macro program was conducted to examine the mediating effects. The results indicated that there was a significant association between cognitive function and depressive symptoms five years later (B = −0.1500, 95%CI: −0.1839, −0.1161), which could also be demonstrated through three mediation pathways: (1) the mediating pathway through IADL disability (B = −0.0247, 95%CI: −0.0332, −0.0171); (2) the mediating pathway through life satisfaction (B = 0.0046, 95%CI: 0.0000, 0.0094); and (3) the chain mediation pathway through IADL disability and life satisfaction (B = −0.0012, 95%CI: −0.0020, −0.0003). Both IADL disability and life satisfaction have been proven to be crucial mediators for the relationship between cognitive function and depressive symptoms five years later. It is necessary to improve individuals’ cognitive function and reduce the negative impact of disability on them, which is important to enhance their life satisfaction and prevent depressive symptoms.
1. Introduction
Depression is a common clinical mental disorder and is characterized by a persistent depressive mood [1,2], and it has become one of the most common medical illnesses [3,4]. It not only places a heavy burden on society because of long-term medicines and health services but also severely affects the health and quality of life of individuals [5,6]. A study reported that direct and indirect spending on treating major depression has been steadily increasing each year in the United States [7]. The prevalence of depressive symptoms was also quite common in China [8]. There were 2.2% of males and 3.3% of females in China suffering from major depressive disorders [9]. Wen et al. found that the incidence of depressive symptoms was as high as 22.3% through a 4-year follow-up among Chinese adults [10]. As such, it is essential to identify the factors related to depressive symptoms and probe into the mechanism among these factors.
As part of the aging process, increasing age is often accompanied by a decline in cognitive function [11], which is characterized by decreased memory, attention, and reasoning ability [12]. The link between cognitive function and depression has attracted a lot of attention, and there are many studies that have proven the relationship between them. The relationship between cognitive function and depression is bidirectional. That is, depression affects cognitive function, and, conversely, cognitive decline can also lead to depression. For example, depression can accelerate brain aging and increase the risk of cognitive impairment [13] through peripheral and cerebral microvascular dysfunction [14]. At the same time, studies have demonstrated that cognitive decline reduces people’s learning and thinking ability and then affects all aspects of life, work, and social interaction, which could increase their psychological stress and even lead to depression or other mental illnesses [15]. Tatiana et al. found that cognitive decline might predict depressive symptoms among older Hispanic adults living in the community [16]. Archana et al. used dynamic change models and potential difference scores to find that memory performance related to cognitive function predicted the changes in depression two years later [17]. By establishing the relationship between cognitive impairment and mood, Jennifer et al. found that participants with mild cognitive impairment had increased odds of depressive symptoms, but participants without cognitive impairment had no change in the rates of depressive symptoms [18]. In China, Yang et al. found that people with cognitive decline have a higher incidence of depression [19]. A cohort study has shown that participants with cognitive impairment had poorer mental status and an increased risk of depression one year later [20]. Clinical studies involving younger and elderly individuals have also established the inverse relationship between cognitive function and depression [21,22,23]. Moreover, in terms of gender differences, females in their mid-to-late 40s will go through menopause, which is the time of life when women in their mid-to-late 40s experience 12 consecutive months of amenorrhea because of a loss of follicular activity [24]. Due to the relative deficiency of androgens, estrogen, and progestin, postmenopausal women may experience depression and cognitive decline, which severely impairs postmenopausal females’ quality of life [25,26]. In consequence, it is also worth considering that the effect of cognitive function on depressive symptoms seems to differ by gender.
Although previous studies have explored the relationship between cognitive decline and depression, the impact of individual physical and psychological changes following cognitive decline on depression is also worthy of attention. As one of the adverse physical consequences of cognitive decline [27,28], disability can be considered as a series of physical limitations that influences individuals’ daily social, recreational, and work activities, which is generally measured by the activities of daily living (ADL) scale or the instrumental activities of daily living (IADL) scale. A cross-sectional study of elderly people in China indicated that nearly one in five individuals had difficulties with ADL disability but two in five had difficulties with IADL disability. Most elderly people need help with IADL, such as bathing and shopping [29]. IADL generally involve the more complex and varied activities of daily living compared with ADL, which require multiple cognitive domains and cognitive flexibility to complete together [30]. A study suggests that the association between cognitive function and ADL depends substantially on IADL [31]. Moreover, hippocampal and cortical gray matter volumes are correlated with IADL [32], suggesting that cognitive decline contributes to the incidence of IADL disability. According to a study involving 10,898 Chinese people, one of the most common risk factors for males regarding IADL disability was cognitive impairment [33]. Therefore, we chose IADL disability, which was more closely associated with cognitive function, as one of the indicators in this study. Regarding whether disability affects depressive symptoms in adults, prior studies have shown that compared with individuals without disabilities, individuals with disabilities were at increased risk of onset depression [34,35]. By constructing a Back Propagation neural network model, Chinese scholars found that disability ranked fourth among the risk factors of depression among Chinese individuals aged 45 or older [36]. These findings strongly suggest that disability is not just a consequence of cognitive decline but is also a key predictive factor for depression. In terms of IADL disability, previous research has confirmed that people with worse IADL performance were more likely to develop depressive symptoms over time [37]. A nationally representative study has shown that depressive symptoms were associated with an increase in IADL disability among Latinos [38]. In China, Li et al. found that IADL disability was significantly associated with an increased incidence of depression among older adults in both males and females [39]. Decreased ability of IADL may be a precursor of depression [40]. Therefore, it is of interest to explore the effect of IADL disability on the relationship between cognitive function and depressive symptoms.
Life satisfaction is a subjective judgment process, which is often considered a fundamental dimension for measuring individuals’ quality of life [41]. Among the studies on the relationship between cognitive function and life satisfaction, previous research has shown that elderly people with cognitive decline had lower life satisfaction [42]. A national study on 10,081 elderly South Koreans showed that cognitive function was an important factor in life satisfaction [43]. In a longitudinal study, life dissatisfaction was found to be related to the development of mild cognitive impairment among older adults [44]. However, there are few reports about the association between cognitive function and life satisfaction among Chinese people, which is worth exploring. In terms of the relationship between disability and life satisfaction, research has demonstrated that people with ADL and IADL disabilities were negatively associated with life satisfaction. The loss of independence for daily living abilities, especially for IADL ability, would trigger a significant decline in perceptions of quality of life and a lower level of life satisfaction [45]. In addition, life satisfaction has been proven to be linked to mental disorders, such as depression [42,46]. Zhang et al. studied nationally representative data in China and found that compared with those who were satisfied with their lives, the elderly with lower life satisfaction were more than twice as likely to be depressed [47]. Scholars have also found that cognitive decline was related to disability incidence, which was more common among elderly people who were dissatisfied with their lives [48]. It is concluded that cognitive function, IADL disability, and life satisfaction are related to each other. Given the relationship between cognitive function, life satisfaction, and depressive symptoms, life satisfaction may mediate the relationship between cognitive function and depressive symptoms.
Exploring the effect of IADL disability and life satisfaction on the relationship between cognitive function and depressive symptoms is conducive to a better understanding of the relationship between cognitive function and depressive symptoms and its internal mechanism, which also provides a reference for prevention and intervention for depression after cognitive decline. This study aimed to assess the relationships between cognitive function, IADL disability, life satisfaction, and depressive symptoms five years later among Chinese adults aged 40 years and above. We proposed three hypotheses for this study: H1, Cognitive function can have an impact on depressive symptoms five years later; H2, IADL disability and life satisfaction may have an independent mediating effect on the association between cognitive function and depressive symptoms five years later; and H3, IADL disability and life satisfaction would have a serial mediation effect between cognitive function and depressive symptoms five years later. We used data from three waves of the China Health and Retirement Longitudinal Study (CHARLS) that was conducted in 2013, 2015, and 2018, respectively, to empirically test the serial multiple mediating effects of IADL disability and life satisfaction between cognitive function and depressive symptoms five years later. At the same time, the influence of gender differences on this study was also considered.
2. Materials and Methods
2.1. Data and Study Design
The data were freely obtained from three waves of the China Health and Longitudinal Retirement Survey (CHARLS) conducted in 2013, 2015, and 2018. The CHARLS is a national longitudinal survey implemented by the National School for Development (China Center for Economic Research), which was first performed in 2011, and the participants have been followed up every two years [49]. The survey covers 28 provinces, 150 county-level units, and 450 communities in China, including information about Chinese adults, such as demographic background, family structure, socioeconomic status, and health behaviors [50].
We ascertained each participant’s cognitive function at baseline in 2013, his/her condition of IADL disability and life satisfaction in 2015, and his/her depressive symptoms in 2018. For the time frame, we excluded the participants who had already developed IADL disability, dissatisfaction with life, and depressive symptoms at baseline, as well as the participants with memory-related disorders, such as Alzheimer’s disease, brain atrophy, and Parkinson’s disease. Using data from each time frame, we evaluated the associations among cognitive function, IADL disability, life satisfaction, and depressive symptoms.
At baseline in 2013, the total sample consisted of 18,612 participants. We excluded 4349 individuals who were lost to follow-up from 2013 to 2018. Meanwhile, 28 participants were excluded due to memory-related disorders, such as Alzheimer’s disease, brain atrophy, and Parkinson’s disease, while 36 participants under 40 years old were also excluded. We further excluded those who had already developed IADL disability (n = 3758), life dissatisfaction (n = 507), or depressive symptoms (n = 2046) at baseline in 2013. Then, 1422 participants without complete information on the core variables, such as IADL disability and life satisfaction or other covariates, were also excluded. The final number of participants aged 40 years and above who were available for the follow-up survey was 6466. The details are shown in Figure 1.
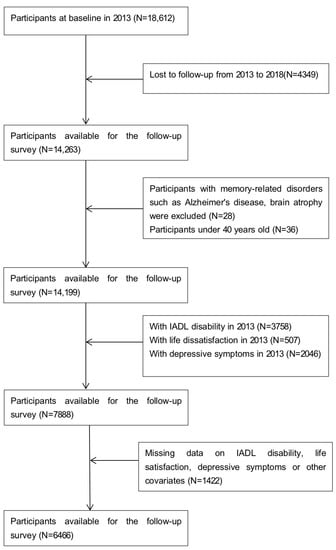
Figure 1.
Flowchart of the inclusion of participants.
2.2. Measurements
2.2.1. Cognitive Function
The cognitive function in the CHARLS (2013) was assessed by the TICS-10 (orientation and attention), word recall (episodic memory), and figure drawing (visual-spatial abilities) [51]. The TICS (Telephone Interview of Cognitive Status) included the serial subtraction of 7 from 100 (up to five times), date (day, month, and year), day of the week, and season of the year. The scores of the TICS-10 ranged from 0 to 10. Word recall was used to assess episodic memory. After being shown 10 Chinese nouns, the participants were asked to recall as many words as they could immediately (immediate memory), in any order, and to recall them again four to ten minutes later (delayed recall). The episodic memory score includes the average number of immediate and delayed word recalls and ranged from 0 to 10. In terms of visuospatial ability, the respondents were shown a picture of two overlapped pentagons and asked to draw a similar figure. The participants received a score of 1 if they drew it correctly and no score otherwise [52,53]. The overall score ranged from 0 to 21, with higher scores indicating better cognitive function.
2.2.2. IADL Disability
Disability in the instrumental activities of daily living (IADL) was described as dependence on at least one IADL task: doing housework, preparing meals, shopping, taking medication, managing money, and making a phone call [54]. The answers included 0 (no, I do not have any difficulty), 1 (I have difficulty but still can do it), 2 (yes, I have difficulty and need help), or 3 (I cannot do it). Those respondents were seen as dependent when they could not carry out the IADL scale activities independently (last three options) [55]. The total score ranged from 0 to 18, with higher scores indicating the more severe the dependence on the IADL item.
2.2.3. Life Satisfaction
Life satisfaction was assessed by one broad question: “How satisfied were you about your life?” The respondents rated based on a 5-point Likert scale in which the higher scores indicated lower levels of life satisfaction. Assessing life satisfaction with an intuitive single question is easier to understand and accept, especially for older adults, which has been used in previous research [56,57].
2.2.4. Depressive Symptoms
Depressive symptoms in the CHARLS were assessed by the 10-item short form of the Center for Epidemiologic Studies Depression Scale (CESD-10) [58]. Compared with the original CESD, the Chinese version of the CESD-10 also showed considerable accuracy in classifying the participants’ depressive symptoms (kappa = 0.84, p < 0.01) [58]. The CESD-10 comprised 10 questions about depression, and the answers included four options: 0 (rarely), 1 (some days; 1–2 days per week), 2 (occasionally; 3–4 days per week) and 3 (most of the time; 5–7 days per week) [59]. The total score ranged from 0 to 30, with a higher value indicating more depressive symptoms [60]. Individuals who scored more than 10 were identified as having depressive symptoms [61].
2.2.5. Demographic Characteristics
We also considered the demographic characteristics of the individuals from the baseline in 2013, including age (years), gender (male, female), marital status (not married, married), smoking (yes, no), drinking (yes, no), social activities (yes, no), physical activities (yes, no), chronic disease (inapplicable, no, one, two and above), and self-rated health (very healthy, healthy, general, unhealthy, very unhealthy).
2.3. Data Analysis
In this study, IBM SPSS Statistics version 24 was employed for analysis and processing. We used descriptive analysis to describe the general characteristics of the study population. t-tests or chi-squared tests were applied to compare the group differences in gender. The PROCESS macro (Model 6) designed by Hayes [62] was used to examine whether IADL disability and life satisfaction mediated the association between cognitive function and depressive symptoms five years later. We also stratified the entire sample by sex to explore whether this relationship still existed. Based on bias-corrected bootstrapping with 5000 samples, we set the bootstrap confidence interval (CI) at 95%. Bootstrap intervals are considered to be significant when the 95%CI does not contain zero [63].
3. Results
3.1. Characteristics of Participants
As shown in Table 1, a total of 6466 participants aged 40 years or above were included in our study, and their mean age was 57.7 ± 8.5. The majority of the participants were married (92.8%), didn’t smoke (84.0%), and performed some physical activities (89.4%) or social activities (64.5%). A total of 7.6% of the participants clearly knew they had more than one chronic disease, and 40.4% of the participants drank. Among all the participants, only 6.9% and 15.9% had rated themselves as “very healthy” or “healthy”, respectively. In terms of gender, there were 3506 males and 2960 females, accounting for 54.2% and 45.8%, respectively. The mean age for the males was 58.8 ± 8.4 and for the females was 56.4 ± 8.3. The results of the t-tests or chi-squared tests showed that compared with the males, the females were more likely to be married, smoke, have lower than moderate self-rated health status, and were less likely to drink. More detailed demographic characteristics are shown in Table 1.

Table 1.
Demographic characteristics of the participants (n = 6466).
3.2. Correlation between the Core Variables
Correlation analysis revealed that cognitive function was negatively correlated with IADL disability (r = −0.214, p < 0.01) and depressive symptoms five years later (r = −0.152, p < 0.01). Cognitive function was positively correlated with life satisfaction (r = 0.026, p < 0.05). IADL disability (r = 0.152, p < 0.01) and life satisfaction (r = 0.147, p < 0.01) were positively correlated with depressive symptoms five years later. IADL disability (r = 0.039, p < 0.01) was positively correlated with life satisfaction (Table 2).

Table 2.
Correlations among cognitive function, IADL disability, life satisfaction, and depressive symptoms.
3.3. Mediating Effect Analyses
To further elucidate the underlying mechanisms by which cognitive function is associated with depressive symptoms five years later, we explored the mediating roles of IADL disability and life satisfaction in this relationship. All the analyses in this study were conducted on the basis of adjusting for all the demographic characteristics. The analysis results are shown in Table 3 and Figure 2. Cognitive function had a significant and negative association with depressive symptoms five years later (B = −0.1712, 95%CI: −0.2050, −0.1374). Cognitive function had a significant and negative association with IADL disability (B = −0.0655, 95%CI: −0.0747, −0.0564). IADL disability had a significant and positive association with depressive symptoms five years later (B = 0.3765, 95%CI: 0.2874, 0.4655). Cognitive function had a significant and positive association with life satisfaction (B = 0.0048, 95%CI: 0.0003, 0.0094). Life satisfaction had a significant and positive association with depressive symptoms five years later (B = 0.9587, 95%CI: 0.7771, 1.1402). When controlling for IADL disability and life satisfaction, cognitive function was still negatively correlated with depressive symptoms five years later, although the coefficient decreased (B = −0.1500, 95%CI: −0.1839, −0.1161).

Table 3.
Hypothesized serial mediation model of cognitive function, IADL disability, life satisfaction, and depressive symptoms.
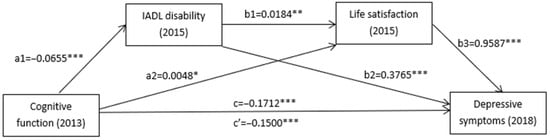
Figure 2.
Serial mediation models for cognitive function, IADL disability, life satisfaction, and depressive symptoms. Note: Path coefficients were shown in the standardized regression coefficient. * p < 0.05, ** p < 0.01, *** p < 0.001.
In addition, Table 3 presents the total and direct effects of cognitive function on depressive symptoms five years later and the mediating effect of IADL disability and life satisfaction. The results demonstrated that the total and direct effects of cognitive function on depressive symptoms five years later were −0.1712 and −0.1500, respectively. When IADL disability and life satisfaction were modelled as mediators, respectively, the path coefficients of cognitive function on depressive symptoms five years later indicated that IADL disability and life satisfaction had a significant mediating effect (Indirect effect1 = −0.0247, 95%CI: −0.0332, −0.0171; Indirect effect2 = 0.0046, 95%CI: 0.0000, 0.0094). In addition, IADL disability and life satisfaction played a serial mediating role in the association between cognitive function and depressive symptoms five years later (Indirect effect 3 = −0.0012, 95%CI: −0.0020, −0.0003). Therefore, three types of mediating effects were found in the relationship between cognitive function and depressive symptoms five years later: first, the mediating effect of IADL disability (effect = −0.0247); second, the mediating effect of life satisfaction (effect = 0.0046); and third, the serial mediating effect of IADL disability and life satisfaction (effect = −0.0012). All the results confirmed the hypothesis we made at the beginning of the study.
3.4. Gender Differences
With respect to gender differences, the full sample was divided into male (n = 3506) and female (n = 2960) groups for the mediating effect analyses. As shown in Table 3, IADL disability and life satisfaction partially mediated the relationship between cognitive function and depressive symptoms five years later for females. Additionally, the indirect roles of IADL disability and life satisfaction were also significant, respectively. However, for males, there is only one significant mediation path: cognitive function→ IADL disability→ depressive symptoms, which means that IADL disability was a mediator in the relationship between cognitive function and depressive symptoms five years later.
4. Discussion
Based on the national longitudinal dataset from CHARLS (2013, 2015, and 2018), we explored the relationship between cognitive function and depressive symptoms five years later among Chinese individuals aged 40 years and older and formulated a mediation model to examine the underlying mechanisms behind this specific association. The results showed that cognitive function is significantly associated with depressive symptoms five years later. In other words, cognitive decline is a risk factor for future depressive symptoms. Disability and life satisfaction play partial mediating roles and a serial mediation role in the relationship between cognitive function and depressive symptoms five years later.
The results suggested that cognitive function is significantly associated with subsequent depressive symptoms five years later, which is in accordance with previous studies [64,65]. This means that the worse the cognitive function, the higher the risk of depressive symptoms in the future. Several longitudinal studies have provided evidence that cognitive decline precedes the onset of depressive symptoms [66]. Clinically speaking, cognitive impairment has several pathophysiological mechanisms, such as disturbances in the hypothalamic–pituitary–adrenal axis and abnormalities in brain-derived neurotrophic signaling [67], which as risk factors might lead to increased chances of future depressive symptoms. In general, the risk of depression is most commonly diagnosed in relation to cognitive decline, such as memory lapses, slower thoughts, and confusion [68]. At the same time, people with cognitive decline experience depressive symptoms, which can be interpreted as a psychological response. In other words, depression can be conceptualized as a kind of psychological reaction to the perception of cognitive decline [69]. In addition, cognitive impairment may also make individuals more susceptible to cognitive distortions (e.g., unrealistic expectations, hyper-responsive to external stimulation), which can impair peoples’ regulatory emotions and further lead to depression [70,71].
After exploring the internal mechanism of the relationship between cognitive function and depressive symptoms five years later, we demonstrated that the indirect effect of this association can be mediated by IADL disability and life satisfaction, respectively. On the one hand, the results revealed that better baseline cognitive performance reduced the incidence of future IADL disability, which is consistent with previous findings that participants with impaired cognition were less likely to be independent [72,73]. A systematic review and meta-analysis established that IADL disability existed over a continuous course of cognitive decline [74]. Cognitive decline can affect people’s operational skills and fine control ability through neuropathological damage, resulting in IADL disability [75] and leading to losses of independence and productivity. When people become aware of the various adverse effects of cognitive decline on their daily life, such as the inconvenience of life and behaviors, it will break the psychological balance to cause many individuals obvious psychological burdens and will bring a series of depressive symptoms in the future [76]. On the other hand, life satisfaction played a mediating role between cognitive function and depressive symptoms. Interestingly, contrary to previous studies [77,78], we found that cognitive decline actually increased people’s life satisfaction, which in turn reduced the risk of developing depressive symptoms. With aging, there is a gradual decline in cognitive function among some people. Correspondingly, they may receive more material and emotional help from friends and relatives, which may prevent them from experiencing more negative emotions, improve their life satisfaction, and, thus, reduce the development of depressive symptoms [79]. Furthermore, the relevant policy guarantees and medical services for people with cognitive disorders provided by the government and departments also make them feel the care and support from society to a large extent [80,81], which will also improve their quality of life and life satisfaction to effectively prevent the occurrence of depression.
We also found that IADL disability and life satisfaction played partial mediating roles in the relationship between cognitive function and depressive symptoms five years later. In detail, baseline cognitive decline was significantly associated with future IADL disability and then reduced life satisfaction, which was in turn related to depressive symptoms in the future. Poor baseline cognitive ability increases the incidence of future IADL disability [27,82]. Adverse outcomes of IADL disability, such as social withdrawal, lack of energy/interest, and decreased self-efficacy, have been identified as strong predictors of reduced life satisfaction. Meanwhile, a large number of studies have shown that lower life satisfaction is an effective indicator of an individual’s exposure to significant depressive symptoms [83]. Compared with the general population, individuals with life dissatisfaction are more likely to have depressive symptoms and other mental health problems [84]. Therefore, IADL impairment caused by cognitive decline renders most adults unable to perform their social roles and daily life normally, thus affecting their life satisfaction [85]. To a certain extent, this will cause personal psychological distress that is difficult to adjust to and may even develop into depression in severe cases [86].
From the perspective of gender difference, our findings showed that IADL disability and life satisfaction played a chain mediating role between cognitive function and depressive symptoms five years later in females, while for males, only IADL disability had a significant mediating effect, which may be due to personality and biological differences between males and females. Moreover, menopause seems to expose women to the odds of cognitive impairment due to changes in sex hormone levels. The decline in cognitive function may interfere with an individual’s activities of daily living [87]. Increased sensitivity to hormonal changes in some menopausal women makes them more susceptible to the negative emotions associated with cognitive decline and IADL disability, leading to lower life satisfaction and an increased risk of depressive symptoms.
Finally, there are some limitations in this study. Firstly, the assessments of variables through self-report questions or a single item may have led to results bias and a lack of sensitivity [88], which made it difficult to detect subtle changes between the samples and also resulted in significant but very small correlations between some variables. In order to make the research results more convincing, future studies should try to introduce more objective and rich measurement methods to provide multidimensional information about the participants’ related indicators. Secondly, the dependent variable of depressive symptoms in this study was continuous. In order to explore the association between cognitive function and future depressive symptoms and its internal mechanism more clearly, clinical diagnosis results and more complex psychological tests should be combined, with the incidence of major depression as the endpoint for in-depth analysis. Thirdly, all the variables were collected through three waves of data from different years. This was neither a cross-sectional nor longitudinal study in nature, so in order to make the findings more convincing, longitudinal research should be conducted to analyze the changes regarding the relationship between cognitive function and future depressive symptoms over time and their causality.
5. Conclusions
This study provides evidence of the association between cognitive function and depressive symptoms five years later among Chinese individuals aged 40 years and older, and the support for the sequential mediating effects of IADL disability and life satisfaction between this relationship was confirmed. Future studies on this topic should reconsider and scrutinize in more depth the relationship between cognitive function and depressive symptoms while considering the differences in other factors. It is necessary to improve cognitive function and reduce the negative impact of disability on individuals, especially females, which is very important to enhance their life satisfaction and prevent depressive symptoms.
Author Contributions
Conceptualization, S.Y. and Y.L.; Methodology, Y.L.; Software, Y.L. and X.Y.; Formal analysis, Y.X.; Data curation, Y.W. and Y.Z.; Writing—original draft preparation, Y.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The raw data used in this study are freely available from the China Health and Retirement Longitudinal Study (CHARLS; http://charls.pku.edu.cn/, accessed on 3 May 2022). Researchers are required to apply for permission to use the data.
Acknowledgments
We would like to thank the China Health and Retirement Longitudinal Study (CHARLS) team for providing the data.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Casey, D.A. Depression in Older Adults: A Treatable Medical Condition. Prim. Care 2017, 44, 499–510. [Google Scholar] [CrossRef] [PubMed]
- Perera, S.; Eisen, R.; Bhatt, M.; Bhatnagar, N.; de Souza, R.; Thabane, L.; Samaan, Z. Light therapy for non-seasonal depression: Systematic review and meta-analysis. BJPsych Open 2016, 2, 116–126. [Google Scholar] [CrossRef] [PubMed]
- Whiteford, H.A.; Degenhardt, L.; Rehm, J.; Baxter, A.J.; Ferrari, A.J.; Erskine, H.E.; Charlson, F.J.; Norman, R.E.; Flaxman, A.D.; Johns, N.; et al. Global burden of disease attributable to mental and substance use disorders: Findings from the Global Burden of Disease Study 2010. Lancet 2013, 382, 1575–1586. [Google Scholar] [CrossRef] [PubMed]
- Nayak, S.; Mohapatra, M.K.; Panda, B. Prevalence of and factors contributing to anxiety, depression and cognitive disorders among urban elderly in Odisha—A study through the health systems’ Lens. Arch. Gerontol. Geriatr. 2019, 80, 38–45. [Google Scholar] [CrossRef]
- Yang, G.; Wang, Y.; Zeng, Y.; Gao, G.F.; Liang, X.; Zhou, M.; Wan, X.; Yu, S.; Jiang, Y.; Naghavi, M.; et al. Rapid health transition in China, 1990–2010: Findings from the Global Burden of Disease Study 2010. Lancet 2013, 381, 1987–2015. [Google Scholar] [CrossRef]
- Charlson, F.J.; Baxter, A.J.; Cheng, H.G.; Shidhaye, R.; Whiteford, H.A. The burden of mental, neurological, and substance use disorders in China and India: A systematic analysis of community representative epidemiological studies. Lancet 2016, 388, 376–389. [Google Scholar] [CrossRef]
- Greenberg, P.E.; Fournier, A.-A.; Sisitsky, T.; Pike, C.T.; Kessler, R.C. The Economic Burden of Adults With Major Depressive Disorder in the United States (2005 and 2010). J. Clin. Psychiatry 2015, 76, 155–162. [Google Scholar] [CrossRef]
- Xu, Y.; Yang, J.; Gao, J.; Zhou, Z.; Zhang, T.; Ren, J.; Li, Y.; Qian, Y.; Lai, S.; Chen, G. Decomposing socioeconomic inequalities in depressive symptoms among the elderly in China. BMC Public Health 2016, 16, 1214. [Google Scholar] [CrossRef]
- Baxter, A.J.; Charlson, F.J.; Cheng, H.G.; Shidhaye, R.; Ferrari, A.J.; Whiteford, H.A. Prevalence of mental, neurological, and substance use disorders in China and India: A systematic analysis. Lancet Psychiatry 2016, 3, 832–841. [Google Scholar] [CrossRef]
- Wen, Y.; Liu, C.; Liao, J.; Yin, Y.; Wu, D. Incidence and risk factors of depressive symptoms in 4 years of follow-up among mid-aged and elderly community-dwelling Chinese adults: Findings from the China Health and Retirement Longitudinal Study. BMJ Open 2019, 9, e029529. [Google Scholar] [CrossRef]
- Clouston, S.A.; Brewster, P.; Kuh, D.; Richards, M.; Cooper, R.; Hardy, R.; Rubin, M.S.; Hofer, S.M. The Dynamic Relationship Between Physical Function and Cognition in Longitudinal Aging Cohorts. Epidemiol. Rev. 2013, 35, 33–50. [Google Scholar] [CrossRef] [PubMed]
- Gao, M.; Kuang, W.; Qiu, P.; Wang, H.; Lv, X.; Yang, M. The time trends of cognitive impairment incidence among older Chinese people in the community: Based on the CLHLS cohorts from 1998 to 2014. Age Ageing 2017, 46, 787–793. [Google Scholar] [CrossRef] [PubMed]
- Alexopoulos, G.S. Mechanisms and treatment of late-life depression. Transl. Psychiatry 2019, 9, 188. [Google Scholar] [CrossRef]
- van Agtmaal, M.J.M.; Houben, A.; Pouwer, F.; Stehouwer, C.D.A.; Schram, M.T. Association of Microvascular Dysfunction with Late-Life Depression: A Systematic Review and Meta-analysis. JAMA Psychiatry 2017, 74, 729–739. [Google Scholar] [CrossRef] [PubMed]
- Diaz-Galvan, P.; Cedres, N.; Figueroa, N.; Barroso, J.; Westman, E.; Ferreira, D. Cerebrovascular Disease and Depressive Symptomatology in Individuals With Subjective Cognitive Decline: A Community-Based Study. Front. Aging Neurosci. 2021, 13, 656990. [Google Scholar] [CrossRef]
- Perrino, T.; Mason, C.A.; Brown, S.C.; Spokane, A.; Szapocznik, J. Longitudinal Relationships Between Cognitive Functioning and Depressive Symptoms Among Hispanic Older Adults. J. Gerontol. Ser. B 2008, 63, P309–P317. [Google Scholar] [CrossRef] [PubMed]
- Jajodia, A.; Borders, A. Memory Predicts Changes in Depressive Symptoms in Older Adults: A Bidirectional Longitudinal Analysis. J. Gerontol. Ser. B 2011, 66B, 571–581. [Google Scholar] [CrossRef]
- Yates, J.A.; Clare, L.; Woods, R.T.; Matthews, F.E. Subjective Memory Complaints are Involved in the Relationship between Mood and Mild Cognitive Impairment. J. Alzheimer’s Dis. 2015, 48, S115–S123. [Google Scholar] [CrossRef]
- Yang, C.; Hu, Y.; Ma, H.; Li, J.; Zhou, Y.; Wang, Y. Study on the relationship between subjective cognitive decline and anxiety and depression in elderly patients. Chin. Evid.-Based Nurs. 2022, 8, 2233–2237. [Google Scholar]
- Wang, W.; Si, H.; Yu, R.; Qiao, X.; Jin, Y.; Ji, L.; Liu, Q.; Bian, Y.; Yu, J.; Wang, C. Effects of reversible cognitive frailty on disability, quality of life, depression, and hospitalization: A prospective cohort study. Aging Ment. Health 2021, 26, 2031–2038. [Google Scholar] [CrossRef]
- Lyness, S.A.; Eaton, E.M.; Schneider, L.S. Cognitive Performance in Older and Middle-Aged Depressed Outpatients and Controls. J. Gerontol. 1994, 49, P129–P136. [Google Scholar] [CrossRef] [PubMed]
- Tarbuck, A.F.; Paykel, E.S. Effects of major depression on the cognitive function of younger and older subjects. Psychol. Med. 1995, 25, 285–295. [Google Scholar] [CrossRef] [PubMed]
- Stordal, K.I.; Lundervold, A.J.; Egeland, J.; Mykletun, A.; Asbjørnsen, A.; Landrø, N.I.; Roness, A.; Rund, B.R.; Sundet, K.; Oedegaard, K.J.; et al. Impairment across executive functions in recurrent major depression. Nord. J. Psychiatry 2004, 58, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, T.A.; Johnson, K.M. Menopause. Med. Clin. N. Am. 2015, 99, 521–534. [Google Scholar] [CrossRef] [PubMed]
- Avis, N.E.; Colvin, A.; Bromberger, J.T.; Hess, R.; Matthews, K.A.; Ory, M.; Schocken, M. Change in health-related quality of life over the menopausal transition in a multiethnic cohort of middle-aged women: Study of Women’s Health Across the Nation. Menopause 2009, 16, 860–869. [Google Scholar] [CrossRef]
- Brown, L.; Bryant, C.; Brown, V.M.; Bei, B.; Judd, F.K. Self-compassion weakens the association between hot flushes and night sweats and daily life functioning and depression. Maturitas 2014, 78, 298–303. [Google Scholar] [CrossRef]
- Gong, B.; Shang, S.; Wu, C. Association between cognitive declines and disability in activities of daily living in older adults with COPD: Evidence from the China health and retirement longitudinal study. BMJ Open 2020, 10, e040098. [Google Scholar] [CrossRef]
- Lau, K.M.; Parikh, M.; Harvey, D.J.; Huang, C.-J.; Farias, S.T. Early Cognitively Based Functional Limitations Predict Loss of Independence in Instrumental Activities of Daily Living in Older Adults. J. Int. Neuropsychol. Soc. 2015, 21, 688–698. [Google Scholar] [CrossRef]
- Zhao, L.; Wang, J.; Deng, H.; Chen, J.; Ding, D. Depressive Symptoms and ADL/IADL Disabilities Among Older Adults from Low-Income Families in Dalian, Liaoning. Clin. Interv. Aging 2022, 17, 733–743. [Google Scholar] [CrossRef]
- Mitchell, M.; Miller, L.S. Executive Functioning and Observed Versus Self-Reported Measures of Functional Ability. Clin. Neuropsychol. 2008, 22, 471–479. [Google Scholar] [CrossRef]
- Rosenthal, E.; Brennan, L.; Xie, S.; Hurtig, H.; Milber, J.; Weintraub, D.; Karlawish, J.; Siderowf, A. Association between cognition and function in patients with Parkinson disease with and without dementia. Mov. Disord. 2010, 25, 1170–1176. [Google Scholar] [CrossRef] [PubMed]
- Cahn-Weiner, D.A.; Farias, S.T.; Julian, L.; Harvey, D.J.; Kramer, J.H.; Reed, B.R.; Mungas, D.; Wetzel, M.; Chui, H. Cognitive and neuroimaging predictors of instrumental activities of daily living. J. Int. Neuropsychol. Soc. 2007, 13, 747–757. [Google Scholar] [CrossRef] [PubMed]
- Chiu, C.-J.; Li, M.-L.; Chou, C.-Y. Trends and biopsychosocial correlates of physical disabilities among older men and women in Taiwan: Examination based on ADL, IADL, mobility, and frailty. BMC Geriatr. 2022, 22, 148. [Google Scholar] [CrossRef]
- Jiang, J.; Tang, Z.; Futatsuka, M. The impact of ADL disability on depression symptoms in a community of Beijing elderly, China. Environ. Health Prev. Med. 2002, 7, 199–204. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.-M.; Mullan, J.; Su, Y.-Y.; Griffiths, D.; Kreis, I.A.; Chiu, H.-C. The Longitudinal Relationship Between Depressive Symptoms and Disability for Older Adults: A Population-Based Study. J. Gerontol. Ser. A 2012, 67, 1059–1067. [Google Scholar] [CrossRef]
- Fan, X.; Guo, X.; Ren, Z.; Li, X.; He, M.; Shi, H.; Zha, S.; Qiao, S.; Zhao, H.; Li, Y.; et al. The prevalence of depressive symptoms and associated factors in middle-aged and elderly Chinese people. J. Affect. Disord. 2021, 293, 222–228. [Google Scholar] [CrossRef]
- Li, X.; Wang, W.; Gao, Q.; Wu, L.; Luo, Y.; Tang, Z.; Guo, X. The Trajectories and Correlation between Physical Limitation and Depression in Elderly Residents of Beijing, 1992–2009. PLoS ONE 2012, 7, e42999. [Google Scholar] [CrossRef]
- Bowen, M.E.; Ruch, A. Depressive Symptoms and Disability Risk Among Older White and Latino Adults by Nativity Status. J. Aging Health 2015, 27, 1286–1305. [Google Scholar] [CrossRef]
- Li, M.; Yang, Y.; Pang, L.; Wu, M.; Wang, Z.; Fu, Y.; Li, K. Gender-specific associations between activities of daily living disability and depressive symptoms among older adults in China: Evidence from the China Health and Retirement Longitudinal Study. Arch. Psychiatr. Nurs. 2019, 33, 160–166. [Google Scholar] [CrossRef]
- Schillerstrom, J.E.; Royall, D.R.; Palmer, R.F. Depression, Disability and Intermediate Pathways: A Review of Longitudinal Studies in Elders. J. Geriatr. Psychiatry Neurol. 2008, 21, 183–197. [Google Scholar] [CrossRef]
- Fastame, M.C. Life satisfaction in late adult span: The contribution of family relationships, health self-perception and physical activity. Aging Clin. Exp. Res. 2020, 33, 1693–1698. [Google Scholar] [CrossRef]
- St John, P.D.; Mackenzie, C.; Menec, V. Does life satisfaction predict five-year mortality in community-living older adults? Aging Ment. Health 2015, 19, 363–370. [Google Scholar] [CrossRef]
- Ko, H.; Jung, S. Association of Social Frailty with Physical Health, Cognitive Function, Psychological Health, and Life Satisfaction in Community-Dwelling Older Koreans. Int. J. Environ. Res. Public Health 2021, 18, 818. [Google Scholar] [CrossRef]
- Rawtaer, I.; Gao, Q.; Nyunt, M.S.Z.; Feng, L.; Chong, M.S.; Lim, W.S.; Lee, T.-S.; Yap, P.; Yap, K.B.; Ng, T.P. Psychosocial Risk and Protective Factors and Incident Mild Cognitive Impairment and Dementia in Community Dwelling Elderly: Findings from the Singapore Longitudinal Ageing Study. J. Alzheimer’s Dis. 2017, 57, 603–611. [Google Scholar] [CrossRef]
- Meltzer, H.; Bebbington, P.; Brugha, T.; McManus, S.; Rai, D.; Dennis, M.S.; Jenkins, R. Physical ill health, disability, dependence and depression: Results from the 2007 national survey of psychiatric morbidity among adults in England. Disabil. Health J. 2012, 5, 102–110. [Google Scholar] [CrossRef]
- Van Damme-Ostapowicz, K.; Cybulski, M.; Galczyk, M.; Krajewska-Kulak, E.; Sobolewski, M.; Zalewska, A. Life satisfaction and depressive symptoms of mentally active older adults in Poland: A cross-sectional study. BMC Geriatr. 2021, 21, 466. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhang, X.; Cao, B.; Wang, H.; Liu, Y.; Guo, Q.; Liu, S.; Zhang, W. Study on the status quo and in fluencing factors of subthreshold depression in the elderly living alone in China based on CLHLS. Chin. Evid. -Based Nurs. 2022, 8, 1068–1071. [Google Scholar]
- Katayama, O.; Lee, S.; Bae, S.; Makino, K.; Chiba, I.; Harada, K.; Shinkai, Y.; Shimada, H. Life Satisfaction and the Relationship between Mild Cognitive Impairment and Disability Incidence: An Observational Prospective Cohort Study. Int. J. Environ. Res. Public Health 2021, 18, 6595. [Google Scholar] [CrossRef]
- Li, J.; Chang, Y.-P.; Riegel, B.; Keenan, B.T.; Varrasse, M.; Pack, A.I.; Gooneratne, N.S. Intermediate, But Not Extended, Afternoon Naps May Preserve Cognition in Chinese Older Adults. J. Gerontol. Ser. A 2017, 73, 360–366. [Google Scholar] [CrossRef]
- Zhao, Y.; Hu, Y.; Smith, J.P.; Strauss, J.; Yang, G. Cohort Profile: The China Health and Retirement Longitudinal Study (CHARLS). Int. J. Epidemiol. 2014, 43, 61–68. [Google Scholar] [CrossRef]
- Lei, X.; Smith, J.P.; Sun, X.; Zhao, Y. Gender differences in cognition in China and reasons for change over time: Evidence from CHARLS. J. Econ. Ageing 2014, 4, 46–55. [Google Scholar] [CrossRef]
- Li, M.; Wang, N.; Dupre, M.E. Association between the self-reported duration and quality of sleep and cognitive function among middle-aged and older adults in China. J. Affect. Disord. 2022, 304, 20–27. [Google Scholar] [CrossRef]
- Li, J.; Cacchione, P.; Hodgson, N.; Riegel, B.; Ms, B.T.K.; Scharf, M.T.; Richards, K.; Gooneratne, N.S. Afternoon Napping and Cognition in Chinese Older Adults: Findings from the China Health and Retirement Longitudinal Study Baseline Assessment. J. Am. Geriatr. Soc. 2016, 65, 373–380. [Google Scholar] [CrossRef]
- Lawton, M.P.; Brody, E.M. Assessment of Older People: Self-Maintaining and Instrumental Activities of Daily Living. Gerontologist 1969, 9, 179–186. [Google Scholar] [CrossRef]
- Chen, L.; Hao, Z.; Wei, X.; Wang, F.; Jing, L.; Xing, F. Comparison of three ADL scales in sidability assessment of middle-aged and elderly people in China-based on the analysis of CHARLS 2018. Mod. Prev. Med. 2021, 48, 2401–2404, 2413. [Google Scholar]
- Pan, L.; Li, L.; Peng, H.; Fan, L.; Liao, J.; Wang, M.; Tan, A.; Zhang, Y. Association of depressive symptoms with marital status among the middle-aged and elderly in Rural China-Serial mediating effects of sleep time, pain and life satisfaction. J. Affect Disord. 2022, 303, 52–57. [Google Scholar] [CrossRef]
- Li, A.; Wang, D.; Lin, S.; Chu, M.; Huang, S.; Lee, C.-Y.; Chiang, Y.-C. Depression and Life Satisfaction Among Middle-Aged and Older Adults: Mediation Effect of Functional Disability. Front. Psychol. 2021, 12, 755220. [Google Scholar] [CrossRef]
- Boey, K.W. Cross-validation of a short form of the CES-D in Chinese elderly. Int. J. Geriatr. Psychiatry 1999, 14, 608–617. [Google Scholar] [CrossRef]
- Wu, C. The mediating and moderating effects of depressive symptoms on the prospective association between cognitive function and activities of daily living disability in older adults. Arch. Gerontol. Geriatr. 2021, 96, 104480. [Google Scholar] [CrossRef]
- Su, D.; Chen, Z.; Chang, J.; Gong, G.; Guo, D.; Tan, M.; Zhang, Y.; Liu, Y.; Chen, X.; Chen, X.; et al. Effect of Social Participation on the Physical Functioning and Depression of Empty-Nest Elderly in China: Evidence from the China Health and Retirement Longitudinal Survey (CHARLS). Int. J. Environ. Res. Public Health 2020, 17, 9438. [Google Scholar] [CrossRef]
- Luo, H.; Li, J.; Zhang, Q.; Cao, P.; Ren, X.; Fang, A.; Liao, H.; Liu, L. Obesity and the onset of depressive symptoms among middle-aged and older adults in China: Evidence from the CHARLS. BMC Public Health 2018, 18, 909. [Google Scholar] [CrossRef]
- Preacher, K.J.; Hayes, A.F. Asymptotic and Resampling Strategies for Assessing and Comparing Indirect Effects in Multiple Mediator Models. Behav. Res. Methods 2008, 40, 879–891. [Google Scholar] [CrossRef]
- Zhang, H.; Han, T.; Ma, S.; Qu, G.; Zhao, T.; Ding, X.; Sun, L.; Qin, Q.; Chen, M.; Sun, Y. Association of child maltreatment and bullying victimization among Chinese adolescents: The mediating role of family function, resilience, and anxiety. J. Affect. Disord. 2021, 299, 12–21. [Google Scholar] [CrossRef]
- Lyketsos, C.G.; Lopez, O.; Jones, B.; Fitzpatrick, A.L.; Breitner, J.; DeKosky, S. Prevalence of neuropsychiatric symptoms in dementia and mild cognitive impairment: Results from the cardiovascular health study. JAMA 2002, 288, 1475–1483. [Google Scholar] [CrossRef]
- Ravaglia, G.; Forti, P.; Lucicesare, A.; Rietti, E.; Pisacane, N.; Mariani, E.; Dalmonte, E. Prevalent Depressive Symptoms as a Risk Factor for Conversion to Mild Cognitive Impairment in an Elderly Italian Cohort. Am. J. Geriatr. Psychiatry 2008, 16, 834–843. [Google Scholar] [CrossRef]
- Vink, D.; Aartsen, M.J.; Schoevers, R.A. Risk factors for anxiety and depression in the elderly: A review. J. Affect. Disord. 2008, 106, 29–44. [Google Scholar] [CrossRef]
- Liu, C.S.; Carvalho, A.F.; McIntyre, R.S. Towards a “metabolic” subtype of major depressive disorder: Shared pathophysiological mechanisms may contribute to cognitive dysfunction. CNS Neurol. Disord.-Drug Targets 2014, 13, 1693–1707. [Google Scholar] [CrossRef]
- Aichele, S.; Ghisletta, P.; Corley, J.; Pattie, A.; Taylor, A.M.; Starr, J.M.; Deary, I.J. Fluid Intelligence Predicts Change in Depressive Symptoms in Later Life: The Lothian Birth Cohort 1936. Psychol. Sci. 2018, 29, 1984–1995. [Google Scholar] [CrossRef]
- Lee, C.H.; Kim, D.H.; Moon, Y.S. Differential associations between depression and cognitive function in MCI and AD: A cross-sectional study. Int. Psychogeriatr. 2019, 31, 1151–1158. [Google Scholar] [CrossRef]
- Rabin, L.; Borgos, M.; Saykin, A.; Wishart, H.; Crane, P.; Nutter-Upham, K.; Flashman, L. Judgment in older adults: Development and psychometric evaluation of the Test of Practical Judgment (TOP-J). J. Clin. Exp. Neuropsychol. 2007, 29, 752–767. [Google Scholar] [CrossRef]
- Shifren, K.; Park, D.C.; Bennett, J.M.; Morrell, R.W. Do cognitive processes predict mental health in individuals with rheumatoid arthritis? J. Behav. Med. 1999, 22, 529–547. [Google Scholar] [CrossRef] [PubMed]
- Han, L.; Gill, T.; Jones, B.L.; Allore, H. Cognitive Aging Trajectories and Burdens of Disability, Hospitalization and Nursing Home Admission Among Community-living Older Persons. J. Gerontol. Ser. A 2015, 71, 766–771. [Google Scholar] [CrossRef] [PubMed]
- Njegovan, V.; Man-Son-Hing, M.; Mitchell, S.L.; Molnar, F.J. The Hierarchy of Functional Loss Associated With Cognitive Decline in Older Persons. J. Gerontol. Ser. A 2001, 56, M638–M643. [Google Scholar] [CrossRef] [PubMed]
- Lindbergh, C.A.; Dishman, R.K.; Miller, L.S. Functional Disability in Mild Cognitive Impairment: A Systematic Review and Meta-Analysis. Neuropsychol. Rev. 2016, 26, 129–159. [Google Scholar] [CrossRef] [PubMed]
- Livingston, G.; Huntley, J.; Sommerlad, A.; Ames, D.; Ballard, C.; Banerjee, S.; Brayne, C.; Burns, A.; Cohen-Mansfield, J.; Cooper, C.; et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet 2020, 396, 413–446. [Google Scholar] [CrossRef] [PubMed]
- Carpenter, B.D.; Xiong, C.; Ma, E.K.P.; Lee, M.M.; Ma, P.J.B.; Coats, M.; Johnson, D.; Morris, J.C. Reaction to a Dementia Diagnosis in Individuals with Alzheimer’s Disease and Mild Cognitive Impairment. J. Am. Geriatr. Soc. 2008, 56, 405–412. [Google Scholar] [CrossRef]
- Runowicz, C.D.; Leach, C.R.; Henry, N.L.; Henry, K.S.; Mackey, H.T.; Cowens-Alvarado, R.L.; Cannady, R.S.; Pratt-Chapman, M.; Edge, S.B.; Jacobs, L.A.; et al. American Cancer Society/American Society of Clinical Oncology Breast Cancer Survivorship Care Guideline. CA A Cancer J. Clin. 2015, 66, 43–73. [Google Scholar] [CrossRef]
- Janelsins, M.C.; Heckler, C.E.; Peppone, L.J.; Kamen, C.; Mustian, K.M.; Mohile, S.G.; Magnuson, A.; Kleckner, I.R.; Guido, J.J.; Young, K.L.; et al. Cognitive Complaints in Survivors of Breast Cancer After Chemotherapy Compared With Age-Matched Controls: An Analysis From a Nationwide, Multicenter, Prospective Longitudinal Study. J. Clin. Oncol. 2017, 35, 506–514. [Google Scholar] [CrossRef]
- Fu, L.; Wang, Y.; He, L. Factors Associated with the Psychological Health of Caregiving Older Parents and Support from Their Grown Children: Results from the China Health and Retirement Longitudinal Study. Int. J. Environ. Res. Public Health 2020, 17, 556. [Google Scholar] [CrossRef]
- Mingyan, L. Comparison of the Mainland and Taiwan Dementia Patient Care Model and Resources. Chinese Primary Health Care. Chin. Prim. Health Care 2016, 30, 7–9. [Google Scholar]
- Yadan, X. Thoughts on Establishing Long-term Nursing Insurance for the Elderly with Dementia in Qingdao. China Soc. Welf. 2018, 7, 25–28. [Google Scholar]
- Raji, M.A.; Al Snih, S.; Ray, L.A.; Patel, K.V.; Markides, K.S. Cognitive status and incident disability in older Mexican Americans: Findings from the Hispanic established population for the epidemiological study of the elderly. Ethn. Dis. 2004, 14, 26–31. [Google Scholar] [PubMed]
- Ghimire, S.; Baral, B.K.; Karmacharya, I.; Callahan, K.; Mishra, S.R. Life satisfaction among elderly patients in Nepal: Associations with nutritional and mental well-being. Health Qual. Life Outcomes 2018, 16, 118. [Google Scholar] [CrossRef] [PubMed]
- Strine, T.W.; Chapman, D.P.; Balluz, L.S.; Moriarty, D.G.; Mokdad, A.H. The Associations Between Life Satisfaction and Health-related Quality of Life, Chronic Illness, and Health Behaviors among U.S. Community-dwelling Adults. J. Community Health 2007, 33, 40–50. [Google Scholar] [CrossRef] [PubMed]
- Lin, I.F.; Wu, H.S. Does informal care attenuate the cycle of ADL/IADL disability and depressive symptoms in late life? J. Gerontol. B Psychol. Sci. Soc. Sci. 2011, 66, 585–594. [Google Scholar] [CrossRef]
- Banjare, P.; Dwivedi, R.; Pradhan, J. Factors associated with the life satisfaction amongst the rural elderly in Odisha, India. Health Qual. Life Outcomes 2015, 13, 201. [Google Scholar] [CrossRef]
- Park, J.; Lee, Y.J. Patterns of instrumental activities of daily living and association with predictors among community-dwelling older women: A latent class analysis. BMC Geriatr. 2017, 17, 158. [Google Scholar] [CrossRef]
- Albert, M.S.; DeKosky, S.T.; Dickson, D.; Dubois, B.; Feldman, H.H.; Fox, N.C.; Gamst, A.; Holtzman, D.M.; Jagust, W.J.; Petersen, R.C.; et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimer’s Dement. 2011, 7, 270–279. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).