Test–Retest Reliability and Internal Consistency of a Newly Developed Questionnaire to Assess Explanatory Variables of 24-h Movement Behaviors in Adults
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
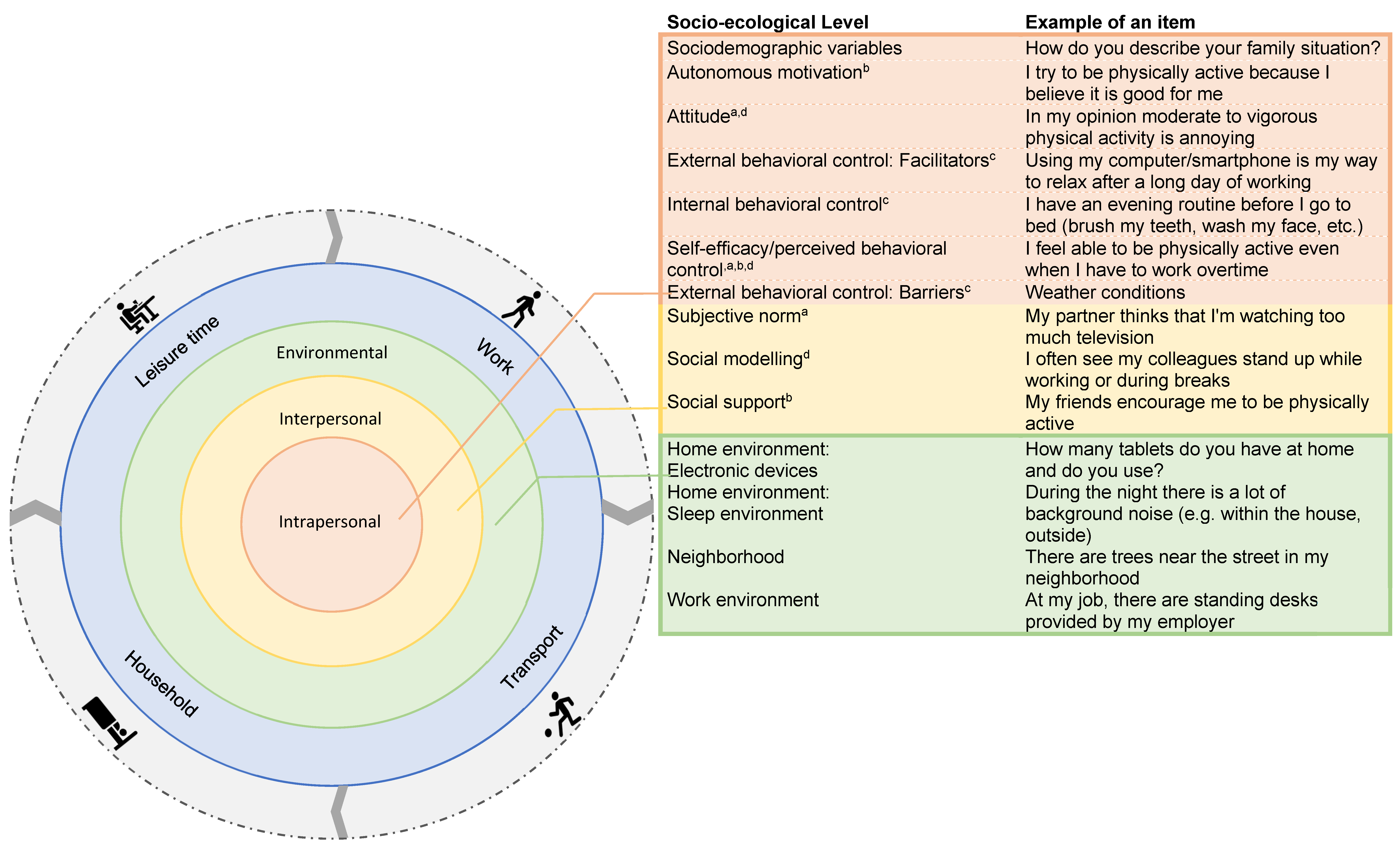
2.2. Questionnaire Development
2.3. Intrapersonal Level
2.3.1. Interpersonal Level
2.3.2. Physical Environmental Level
2.4. Procedure
2.5. Statistical Analyses
3. Results
3.1. Sample Characteristics
3.2. Test–Retest Reliability
3.3. Internal Consistency
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Itani, O.; Jike, M.; Watanabe, N.; Kaneita, Y. Short sleep duration and health outcomes: A systematic review, meta-analysis, and meta-regression. Sleep Med. 2017, 32, 246–256. [Google Scholar] [CrossRef] [PubMed]
- Jike, M.; Itani, O.; Watanabe, N.; Buysse, D.J.; Kaneita, Y. Long sleep duration and health outcomes: A systematic review, meta-analysis and meta-regression. Sleep Med. Rev. 2018, 39, 25–36. [Google Scholar] [CrossRef] [PubMed]
- Ekelund, U.; Brown, W.J.; Steene-Johannessen, J.; Fagerland, M.W.; Owen, N.; Powell, K.E.; Bauman, A.E.; Lee, I.M. Do the associations of sedentary behaviour with cardiovascular disease mortality and cancer mortality differ by physical activity level? A systematic review and harmonised meta-analysis of data from 850,060 participants. Br. J. Sport. Med. 2019, 53, 886–894. [Google Scholar] [CrossRef] [PubMed]
- Kraus, W.E.; Powell, K.E.; Haskell, W.L.; Janz, K.F.; Campbell, W.W.; Jakicic, J.M.; Troiano, R.P.; Sprow, K.; Torres, A.; Piercy, K.L. Physical Activity, All-Cause and Cardiovascular Mortality, and Cardiovascular Disease. Med. Sci. Sport. Exerc. 2019, 51, 1270–1281. [Google Scholar] [CrossRef]
- Battista, F.; Ermolao, A.; van Baak, M.A.; Beaulieu, K.; Blundell, J.E.; Busetto, L.; Carraça, E.V.; Encantado, J.; Dicker, D.; Farpour-Lambert, N.; et al. Effect of exercise on cardiometabolic health of adults with overweight or obesity: Focus on blood pressure, insulin resistance, and intrahepatic fat—A systematic review and meta-analysis. Obes. Rev. 2021, 22 (Suppl. 4), e13269. [Google Scholar] [CrossRef]
- Dumuid, D.; Pedišić, Ž.; Palarea-Albaladejo, J.; Martín-Fernández, J.A.; Hron, K.; Olds, T. Compositional data analysis in time-use epidemiology. In Advances in Compositional Data Analysis: Festschrift in Honour of Vera Pawlowsky-Glahn; Filzmoser, P., Hron, K., Martín-Fernández, J.A., Palarea-Albaladejo, J., Eds.; Springer International Publishing: Cham, Switzerland, 2021; pp. 383–404. [Google Scholar] [CrossRef]
- Ross, R.; Chaput, J.P.; Giangregorio, L.M.; Janssen, I.; Saunders, T.J.; Kho, M.E.; Poitras, V.J.; Tomasone, J.R.; El-Kotob, R.; McLaughlin, E.C.; et al. Canadian 24-Hour Movement Guidelines for Adults aged 18–64 years and Adults aged 65 years or older: An integration of physical activity, sedentary behaviour, and sleep. Appl. Physiol. Nutr. Metab. 2020, 45, S57–S102. [Google Scholar] [CrossRef]
- Janssen, I.; Clarke, A.E.; Carson, V.; Chaput, J.P.; Giangregorio, L.M.; Kho, M.E.; Poitras, V.J.; Ross, R.; Saunders, T.J.; Ross-White, A.; et al. A systematic review of compositional data analysis studies examining associations between sleep, sedentary behaviour, and physical activity with health outcomes in adults. Appl. Physiol. Nutr. Metab. 2020, 45, S248–S257. [Google Scholar] [CrossRef]
- Chaput, J.P.; Dutil, C.; Featherstone, R.; Ross, R.; Giangregorio, L.; Saunders, T.J.; Janssen, I.; Poitras, V.J.; Kho, M.E.; Ross-White, A.; et al. Sleep timing, sleep consistency, and health in adults: A systematic review. Appl. Physiol. Nutr. Metab. 2020, 45, S232–S247. [Google Scholar] [CrossRef]
- Rossen, J.; Von Rosen, P.; Johansson, U.B.; Brismar, K.; Hagströmer, M. Associations of physical activity and sedentary behavior with cardiometabolic biomarkers in prediabetes and type 2 diabetes: A compositional data analysis. Phys. Sportsmed. 2020, 48, 222–228. [Google Scholar] [CrossRef]
- Swindell, N.; Rees, P.; Fogelholm, M.; Drummen, M.; MacDonald, I.; Martinez, J.A.; Navas-Carretero, S.; Handjieva-Darlenska, T.; Boyadjieva, N.; Bogdanov, G.; et al. Compositional analysis of the associations between 24-h movement behaviours and cardio-metabolic risk factors in overweight and obese adults with pre-diabetes from the PREVIEW study: Cross-sectional baseline analysis. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 29. [Google Scholar] [CrossRef]
- Taylor, N.; Lawton, R.; Conner, M. Development and initial validation of the determinants of physical activity questionnaire. Int. J. Behav. Nutr. Phys. Act. 2013, 10, 74. [Google Scholar] [CrossRef]
- Eldredge, L.K.B.; Markham, C.M.; Ruiter, R.A.; Fernández, M.E.; Kok, G.; Parcel, G.S. Planning Health Promotion Programs: An Intervention Mapping Approach; John Wiley & Sons: Hoboken, NJ, USA, 2016. [Google Scholar]
- Oluka, O.C.; Nie, S.; Sun, Y. Quality assessment of TPB-based questionnaires: A systematic review. PLoS ONE 2014, 9, e94419. [Google Scholar] [CrossRef]
- Motl, R.W.; Sasaki, J.E.; Cederberg, K.L.; Jeng, B. Social-cognitive theory variables as correlates of sedentary behavior in multiple sclerosis: Preliminary evidence. Disabil. Health J. 2019, 12, 622–627. [Google Scholar] [CrossRef]
- Duan, Y.; Shang, B.; Liang, W.; Du, G.; Yang, M.; Rhodes, R.E. Effects of eHealth-Based Multiple Health Behavior Change Interventions on Physical Activity, Healthy Diet, and Weight in People with Noncommunicable Diseases: Systematic Review and Meta-analysis. J. Med. Internet Res. 2021, 23, e23786. [Google Scholar] [CrossRef]
- Gardner, B.; Smith, L.; Lorencatto, F.; Hamer, M.; Biddle, S.J. How to reduce sitting time? A review of behaviour change strategies used in sedentary behaviour reduction interventions among adults. Health Psychol. Rev. 2016, 10, 89–112. [Google Scholar] [CrossRef]
- Connell, L.E.; Carey, R.N.; de Bruin, M.; Rothman, A.J.; Johnston, M.; Kelly, M.P.; Michie, S. Links Between Behavior Change Techniques and Mechanisms of Action: An Expert Consensus Study. Ann. Behav. Med. 2019, 53, 708–720. [Google Scholar] [CrossRef]
- Curran, F.; Blake, C.; Cunningham, C.; Perrotta, C.; van der Ploeg, H.; Matthews, J.; O’Donoghue, G. Efficacy, characteristics, behavioural models and behaviour change strategies, of non-workplace interventions specifically targeting sedentary behaviour; a systematic review and meta-analysis of randomised control trials in healthy ambulatory adults. PLoS ONE 2021, 16, e0256828. [Google Scholar] [CrossRef]
- Galli, F.; Chirico, A.; Mallia, L.; Girelli, L.; De Laurentiis, M.; Lucidi, F.; Giordano, A.; Botti, G. Active lifestyles in older adults: An integrated predictive model of physical activity and exercise. Oncotarget 2018, 9, 25402–25413. [Google Scholar] [CrossRef]
- Hagger, M.S.; Chatzisarantis, N.L. Integrating the theory of planned behaviour and self-determination theory in health behaviour: A meta-analysis. Br. J. Health Psychol. 2009, 14, 275–302. [Google Scholar] [CrossRef]
- Young, M.D.; Plotnikoff, R.C.; Collins, C.E.; Callister, R.; Morgan, P.J. Social cognitive theory and physical activity: A systematic review and meta-analysis. Obes. Rev. 2014, 15, 983–995. [Google Scholar] [CrossRef]
- Gillison, F.B.; Rouse, P.; Standage, M.; Sebire, S.J.; Ryan, R.M. A meta-analysis of techniques to promote motivation for health behaviour change from a self-determination theory perspective. Health Psychol. Rev. 2019, 13, 110–130. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, F.; Bento, T.; Cid, L.; Pereira Neiva, H.; Teixeira, D.; Moutão, J.; Almeida Marinho, D.; Monteiro, D. Can Interpersonal Behavior Influence the Persistence and Adherence to Physical Exercise Practice in Adults? A Systematic Review. Front. Psychol. 2018, 9, 2141. [Google Scholar] [CrossRef] [PubMed]
- Sallis, J.; Cervero, R.; Ascher, W.; Henderson, K.; Kraft, M.; Kerr, J. An Ecological Approach to Creating More Physically Active Communities. Annu. Rev. Public Health 2006, 27, 297–322. [Google Scholar] [CrossRef] [PubMed]
- Bronfenbrenner, U. Toward an experimental ecology of human development. Am. Psychol. 1977, 32, 513–531. [Google Scholar] [CrossRef]
- Lee, Y.; Park, S. Understanding of Physical Activity in Social Ecological Perspective: Application of Multilevel Model. Front. Psychol. 2021, 12, 622929. [Google Scholar] [CrossRef]
- Mullane, S.L.; Toledo, M.J.L.; Rydell, S.A.; Feltes, L.H.; Vuong, B.; Crespo, N.C.; Pereira, M.A.; Buman, M.P. Social ecological correlates of workplace sedentary behavior. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 117. [Google Scholar] [CrossRef]
- Grandner, M.A. (Ed.) Chapter 5—Social-ecological model of sleep health. In Sleep and Health; Academic Press: Cambridge, MA, USA, 2019; pp. 45–53. [Google Scholar] [CrossRef]
- Bujang, M.A.; Baharum, N. A simplified guide to determination of sample size requirements for estimating the value of intraclass correlation coefficient: A review. Arch. Orofac. Sci. 2017, 12, 1–11. [Google Scholar]
- Yurdugül, H. Minimum Sample Size for Cronbach’s Coefficient Alpha: A Monte-Carlo Study. Acettepe Univ. J. Educ. 2008, 35, 397–405. [Google Scholar]
- Bujang, M.A.; Omar, E.D.; Baharum, N.A. A Review on Sample Size Determination for Cronbach’s Alpha Test: A Simple Guide for Researchers. Malays. J. Med. Sci. 2018, 25, 85–99. [Google Scholar] [CrossRef]
- McLeroy, K.R.; Bibeau, D.; Steckler, A.; Glanz, K. An ecological perspective on health promotion programs. Health Educ. Q. 1988, 15, 351–377. [Google Scholar] [CrossRef]
- Pinchevsky, Y.; Butkow, N.; Raal, F.J.; Chirwa, T.; Rothberg, A. Demographic and Clinical Factors Associated with Development of Type 2 Diabetes: A Review of the Literature. Int. J. Gen. Med. 2020, 13, 121–129. [Google Scholar] [CrossRef]
- Hagger, M.S.; Chatzisarantis, N.L.D. An Integrated Behavior Change Model for Physical Activity. Exerc. Sport Sci. Rev. 2014, 42, 62–69. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef]
- Park, M.S.; Kang, K.J.; Jang, S.J.; Lee, J.Y.; Chang, S.J. Evaluating test-retest reliability in patient-reported outcome measures for older people: A systematic review. Int. J. Nurs. Stud. 2018, 79, 58–69. [Google Scholar] [CrossRef]
- Streiner, D.L.; Norman, G.R.; Cairney, J. Health Measurement Scales: A Practical Guide to Their Development and Use, 5th ed.; Oxford University Press: Oxford, UK, 2014. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef]
- Taber, K.S. The Use of Cronbach’s Alpha When Developing and Reporting Research Instruments in Science Education. Res. Sci. Educ. 2018, 48, 1273–1296. [Google Scholar] [CrossRef]
- IBM Corp. Released 2020. IBM SPSS Statistics for Windows; Version 27.0; IBM Corp: Armonk, NY, USA.
- Wilding, S.; Conner, M.; Sandberg, T.; Prestwich, A.; Lawton, R.; Wood, C.; Miles, E.; Godin, G.; Sheeran, P. The question-behaviour effect: A theoretical and methodological review and meta-analysis. Eur. Rev. Soc. Psychol. 2016, 27, 196–230. [Google Scholar] [CrossRef]
- Wood, C.; Conner, M.; Miles, E.; Sandberg, T.; Taylor, N.; Godin, G.; Sheeran, P. The Impact of Asking Intention or Self-Prediction Questions on Subsequent Behavior: A Meta-Analysis. Pers. Soc. Psychol. Rev. 2016, 20, 245–268. [Google Scholar] [CrossRef]
- Phillips, C.J.; Marshall, A.P.; Chaves, N.J.; Jankelowitz, S.K.; Lin, I.B.; Loy, C.T.; Rees, G.; Sakzewski, L.; Thomas, S.; To, T.P.; et al. Experiences of using the Theoretical Domains Framework across diverse clinical environments: A qualitative study. J. Multidiscip. Healthc. 2015, 8, 139–146. [Google Scholar] [CrossRef]
- Cane, J.; O’Connor, D.; Michie, S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement. Sci. 2012, 7, 37. [Google Scholar] [CrossRef]
- Ajzen, I. The theory of planned behavior. Organ. Behav. Hum. Decis. Process. 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Senkowski, V.; Gannon, C.; Branscum, P. Behavior Change Techniques Used in Theory of Planned Behavior Physical Activity Interventions among Older Adults: A Systematic Review. J. Aging Phys. Act. 2019, 27, 746–754. [Google Scholar] [CrossRef] [PubMed]
- Grandner, M.A.; Jackson, N.; Gooneratne, N.S.; Patel, N.P. The development of a questionnaire to assess sleep-related practices, beliefs, and attitudes. Behav. Sleep Med. 2014, 12, 123–142. [Google Scholar] [CrossRef] [PubMed]
- Edinger, J.D.; Wohlgemuth, W.K. Psychometric comparisons of the standard and abbreviated DBAS-10 versions of the dysfunctional beliefs and attitudes about sleep questionnaire. Sleep Med. 2001, 2, 493–500. [Google Scholar] [CrossRef]
- Adan, A.; Fabbri, M.; Natale, V.; Prat, G. Sleep Beliefs Scale (SBS) and circadian typology. J. Sleep Res. 2006, 15, 125–132. [Google Scholar] [CrossRef]
- Rhodes, R.E.; Boudreau, P.; Josefsson, K.W.; Ivarsson, A. Mediators of physical activity behaviour change interventions among adults: A systematic review and meta-analysis. Health Psychol. Rev. 2021, 15, 272–286. [Google Scholar] [CrossRef]
- Rhodes, R.E.; Cox, A.; Sayar, R. What Predicts the Physical Activity Intention-Behavior Gap? A Systematic Review. Ann. Behav. Med. 2022, 56, 1–20. [Google Scholar] [CrossRef]
- Hardeman, W.; Houghton, J.; Lane, K.; Jones, A.; Naughton, F. A systematic review of just-in-time adaptive interventions (JITAIs) to promote physical activity. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 31. [Google Scholar] [CrossRef]
| Sample Characteristics | Descriptive Numbers |
|---|---|
| Total sample size recruited (#) | 40 |
| Drop out (#) | 5 |
| Total sample size participated (#) | 35 |
| Age in years (mean (SD)) | 42.94 (±16.07) |
| Sex: female (# (%)) | 21 (60.00) |
| Unemployed (# (%)) | 3 (8.57) |
| Early retired/retired (# (%)) | 4 (11.43) |
| High educational level (# (%)) | 23 (65.70) |
| Net family income >2000 euro/month (# (%)) | 28 (80.00) |
| Average time between T1–T2 (mean in days (SD)) | 15.82 (±2.00) |
| Explanatory Variable Constructs | Items | Test–Retest Reliability (ICC) | IC (α) | ||||
|---|---|---|---|---|---|---|---|
| Excellent | Good | Moderate | Poor | ||||
| n | ICC-Range | n (%) | n (%) | n (%) | n (%) | α | |
| General information | |||||||
| Intrapersonal level | |||||||
| Sociodemographic variables | 14 | 0.758–1.000 | 13 (92.86) | 1 (7.14) | 0 | 0 | NA |
| Physical activity | |||||||
| Intrapersonal level | |||||||
| Autonomous motivation | 2 | 0.322–0.577 | 0 | 0 | 1 (50.00) | 1 (50.00) | 0.585 |
| Attitude: Overall | 10 | 0.071–0.616 | 0 | 0 | 3 (30.00) | 7 (70.00) | 0.840 |
| Attitude LPA | 5 | 0.193–0.616 | 0 | 0 | 1 (20.00) | 4 (80.00) | 0.861 |
| Attitude MVPA | 5 | 0.071–0.571 | 0 | 0 | 2 (40.00) | 3 (60.00) | 0.811 |
| Facilitators | 14 | 0.141–0.654 | 0 | 0 | 3 (21.43) | 11 (78.57) | 0.769 |
| Internal behavioral control | 2 | 0.344–0.781 | 0 | 1 (50.00) | 0 | 1 (50.00) | 0.772 |
| Self-efficacy | 10 | 0.443–0.763 | 0 | 1 (10.00) | 7 (70.00) | 2 (20.00) | 0.896 |
| Barriers | 16 | 0.054–0.821 | 0 | 3 (18.75) | 8 (50.00) | 5 (31.25) | 0.942 |
| Interpersonal level | |||||||
| Subjective norm | 5 | 0.416–0.851 | 0 | 1 (20.00) | 3 (60.00) | 1 (20.00) | 0.869 |
| Social modeling | 5 | 0.693–0.849 | 0 | 4 (80.00) | 1 (20.00) | 0 | 0.561 |
| Social support | 6 | 0.071–0.826 | 0 | 2 (33.33) | 2 (33.33) | 2 (33.33) | 0.623 |
| Summary physical activity | 70 | 0.054–0.851 | 0 | 12 (17.14) | 28 (40.00) | 30 (42.86) | |
| Sedentary behavior | |||||||
| Intrapersonal level | |||||||
| Autonomous motivation | 2 | 0.218–0.554 | 0 | 0 | 1 (50.00) | 1 (50.00) | 0.789 |
| Attitude: Long sitting period | 5 | 0.106–0.720 | 0 | 0 | 3 (60.00) | 2 (40.00) | 0.695 |
| Attitude: Interrupting sitting period | 5 | 0.159–0.724 | 0 | 0 | 2 (40.00) | 3 (60.00) | 0.804 |
| Facilitators: Overall | 8 | 0.485–0.846 | 0 | 2 (25.00) | 5 (62.50) | 1 (12.50) | 0.788 |
| Leisure time | 4 | 0.485–0.766 | 0 | 1 (25.00) | 2 (50.00) | 1 (25.00) | 0.722 |
| Work | 2 | 0.561 −0.744 | 0 | 0 | 2 (100.00) | 0 | 0.876 |
| Household | 2 | 0.670–0.846 | 0 | 1(50) | 1 (50.00) | 0 | 0.910 |
| Internal behavioral control | 5 | 0.089–0.782 | 0 | 1 (20.00) | 2 (40.00) | 2 (40.00) | 0.398 |
| Self-efficacy: Overall | 17 | 0.065–0.848 | 0 | 1 (5.88) | 8 (47.06) | 8 (47.06) | 0.855 |
| Leisure time | 7 | 0.222–0.740 | 0 | 0 | 3 (42.86) | 4 (57.14) | 0.744 |
| Transport | 4 | 0.425–0.654 | 0 | 0 | 2 (50.00) | 2 (50.00) | 0.729 |
| Work | 3 | 0.550–0.848 | 0 | 1 (33.33) | 2 (66.67) | 0 | 0.835 |
| Household | 3 | 0.065–0.677 | 0 | 0 | 1 (33.33) | 2 (66.67) | 0.533 |
| Barriers: Overall | 16 | 0.024–0.781 | 0 | 1 (6.25) | 8 (50.00) | 7 (43.75) | 0.874 |
| Leisure time | 4 | 0.227–0.436 | 0 | 0 | 0 | 4 (100.00) | 0.812 |
| Transport | 5 | 0.491–0.781 | 0 | 1 (20.00) | 3 (60.00) | 1 (20.00) | 0.801 |
| Work | 5 | 0.594–0.696 | 0 | 0 | 5 (100.00) | 0 | 0.951 |
| Household | 2 | 0.024–0.239 | 0 | 0 | 0 | 2 (100.00) | 0.809 |
| Interpersonal level | |||||||
| Subjective norm: Overall | 12 | 0.435–0.860 | 0 | 3 (25.00) | 5 (41.67) | 4 (33.33) | 0.887 |
| Leisure time | 6 | 0.470–0.826 | 0 | 2 (33.33) | 3 (50.00) | 1 (16.67) | 0.856 |
| Transport | 3 | 0.435–0.860 | 0 | 1 (33.33) | 0 | 2 (66.67) | 0.638 |
| Work | 1 | 0.635 | 0 | 0 | 1 (100.00) | 0 | NA |
| Household | 2 | 0.498–0.730 | 0 | 0 | 1 (50.00) | 1 (50.00) | 0.732 |
| Social modeling: Overall | 20 | 0.377–0.911 | 3 (15.00) | 7 (35.00) | 8 (40.00) | 2 (10.00) | 0.724 |
| Leisure time | 12 | 0.588–0.911 | 3 (25.00) | 5 (41.57) | 4 (33.33) | 0 | 0.771 |
| Transport | 4 | 0.553–0.853 | 0 | 2 (50.00) | 2 (50.00) | 0 | 0.814 |
| Work | 2 | 0.584–0.655 | 0 | 0 | 2 (100.00) | 0 | 0.874 |
| Household | 2 | 0.377–0.428 | 0 | 0 | 0 | 2 (100.00) | 0.779 |
| Social support: Overall | 12 | 0.498–0.787 | 0 | 3 (25.00) | 8 (66.67) | 1 (8.33) | 0.910 |
| Leisure time | 6 | 0.530–0.779 | 0 | 2 (33.33) | 4 (66.67) | 0 | 0.886 |
| Transport | 3 | 0.502–0.787 | 0 | 1 (33.33) | 2 (66.67) | 0 | 0.789 |
| Work | 1 | 0.612 | 0 | 0 | 1 (100.00) | 0 | NA |
| Household | 2 | 0.498–0.714 | 0 | 0 | 1 (50.00) | 1 (50.00) | 0.645 |
| Summary sedentary behavior | 102 | 0.024–0.911 | 3 (2.94) | 18 (17.65) | 50 (49.02) | 31 (30.39) | |
| Sleep | |||||||
| Intrapersonal level | |||||||
| Autonomous motivation | 2 | 0.260–0.379 | 0 | 0 | 0 | 2 (100.00) | 0.817 |
| Attitude: Overall | 10 | 0.079–0.724 | 0 | 0 | 5 (50.00) | 5 (50.00) | 0.742 |
| Optimal sleep pattern | 5 | 0.079–0.605 | 0 | 0 | 2 (40.00) | 3 (60.00) | 0.734 |
| Electronic devices | 5 | 0.407–0.724 | 0 | 0 | 3 (60.00) | 2 (40.00) | 0.749 |
| Facilitators | 6 | 0.315–0.640 | 0 | 0 | 3 (50.00) | 3 (50.00) | 0.867 |
| Internal behavioral control | 2 | 0.630–0.641 | 0 | 0 | 2 (100.00) | 0 | 0.760 |
| Self-efficacy | 6 | 0.461–0.812 | 0 | 1 (16.67) | 3 (50.00) | 2 (33.33) | 0.804 |
| Barriers: Overall | 12 | 0.156–0.730 | 0 | 1 (8.33) | 9 (75.00) | 2 (16.67) | 0.821 |
| Optimal sleep pattern | 9 | 0.156–0.730 | 0 | 0 | 7 (77.78) | 2 (22.22) | 0.807 |
| Electronic devices | 3 | 0.578–0.848 | 0 | 1 (33.33) | 2 (66.67) | 0 | 0.748 |
| Interpersonal level | |||||||
| Subjective norm | 2 | 0.522–0.656 | 0 | 0 | 2 (100) | 0 | 0.745 |
| Social modeling | 3 | 0.679–0.805 | 0 | 2 (66.67) | 1 (33.33) | 0 | 0.832 |
| Social support | 2 | 0.446–0.526 | 0 | 0 | 1 (50.00) | 1 (50.00) | 0.687 |
| Summary sleep | 45 | 0.079–0.848 | 0 | 4 (8.89) | 26 (57.78) | 15 (33.33) | |
| Environment | |||||||
| Physical environment level | |||||||
| Home environment: Electronic devices | 10 | 0.622–0.896 | 0 | 7 (70.00) | 3 (30.00) | 0 | 0.664 |
| Home environment: Sleep environment | 7 | 0.474–0.850 | 0 | 5 (71.43) | 1 (14.29) | 1 (14.29) | 0.526 |
| Neighborhood | 13 | 0.437–0.934 | 2 (15.38) | 3 (23.08) | 7 (53.85) | 1 (7.69) | 0.797 |
| Work environment | 5 | 0.823–1.000 | 3 (60.00) | 2 (40.00) | 0 | 0 | 0.916 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Willems, I.; Verbestel, V.; Calders, P.; Lapauw, B.; De Craemer, M. Test–Retest Reliability and Internal Consistency of a Newly Developed Questionnaire to Assess Explanatory Variables of 24-h Movement Behaviors in Adults. Int. J. Environ. Res. Public Health 2023, 20, 4407. https://doi.org/10.3390/ijerph20054407
Willems I, Verbestel V, Calders P, Lapauw B, De Craemer M. Test–Retest Reliability and Internal Consistency of a Newly Developed Questionnaire to Assess Explanatory Variables of 24-h Movement Behaviors in Adults. International Journal of Environmental Research and Public Health. 2023; 20(5):4407. https://doi.org/10.3390/ijerph20054407
Chicago/Turabian StyleWillems, Iris, Vera Verbestel, Patrick Calders, Bruno Lapauw, and Marieke De Craemer. 2023. "Test–Retest Reliability and Internal Consistency of a Newly Developed Questionnaire to Assess Explanatory Variables of 24-h Movement Behaviors in Adults" International Journal of Environmental Research and Public Health 20, no. 5: 4407. https://doi.org/10.3390/ijerph20054407
APA StyleWillems, I., Verbestel, V., Calders, P., Lapauw, B., & De Craemer, M. (2023). Test–Retest Reliability and Internal Consistency of a Newly Developed Questionnaire to Assess Explanatory Variables of 24-h Movement Behaviors in Adults. International Journal of Environmental Research and Public Health, 20(5), 4407. https://doi.org/10.3390/ijerph20054407








