Abstract
Poor posture is a well-known problem in all age groups and can lead to back pain, which in turn can result in high socio-economic costs. Regular assessment of posture can therefore help to identify postural deficits at an early stage in order to take preventive measures and can therefore be an important tool for promoting public health. We measured the posture of 1127 symptom-free subjects aged 10 to 69 years using stereophotogrammetry and determined the sagittal posture parameters flèche cervicale (FC), flèche lombaire (FL), and kyphosis index (KI) as well as the values standardized to the trunk height (FC%, FL%, KI%). FC, FC%, KI, and KI% showed an increase with age in men but not in women, and a difference between the sexes. FL remained largely constant with age, although FL% had significantly greater values in women than men. Postural parameters correlated only moderately or weakly with body mass index. Reference values were determined for different age groups and for both sexes. Since the parameters analyzed can also be determined by simple and non-instrumental methods in medical office, they are suitable for performing preventive checks in daily medical or therapeutic practice.
1. Introduction
Postural deficits are known to be common in children and adolescents as well as in adults in industrialized countries. Various studies show a prevalence of occurrence of postural deficits in adolescents ranging from 25% to 60% [1,2,3]. In their study, Maulik et al. found musculoskeletal deficits in 73.3% of adults [4]. The causes include prolonged and unfavorable sitting postures, which, in the long term, can lead to muscular weaknesses and imbalances [5]. Muscular imbalance, in turn, causes various changes in posture that manifest as postural weakness [6,7]. This can include a forward-shifted (protracted) head, which is usually associated with increased lordosis of the cervical spine [8,9] and increased kyphosis of the thoracic spine, which can lead to a hunchback [10] and affect breathing [11,12]. In the lumbar spine, an increased forward-tilted pelvis and a hollow back can develop [13]. Such poor posture places a high load on the facet joints of the spine, which can lead to increased joint degeneration, muscular tightness, and, ultimately, pain [14,15,16]. Back pain, on the other hand, is responsible for a large proportion of work absence days in Germany [17] and other countries [18,19,20], also affects children and adolescents [21,22,23], and is, meanwhile, considered a global health problem [24]. Thus, it is clear that postural imbalance is becoming a significant factor in maintaining public health.
In a comprehensive review, Potthoff and colleagues called for further study of sagittal postural alignment as one of several risk factors for the development of low back pain in adolescence [25]. Sugai and colleagues [26] furthermore demonstrated that measuring thoracic kyphosis in the elderly could predict a future decline in their activities of daily living. This shows that an analysis of sagittal posture is useful in all age groups. In order to detect postural deficiencies at an early stage and to take necessary preventive measures, regular assessment of posture is useful. This makes posture measurement an important tool for promoting public health. However, a major problem is determining when a sagittal spinal curvature can still be described as normal and when it should be considered a postural weakness requiring treatment [27]. In daily medical practice, an initial assessment is made only by visual inspection and is based on the examiner’s experience. Invasive procedures such as X-rays are only performed when pathology is suspected, due to radiation exposure, especially in children and adolescents. However, assessing the back contour by visual inspection is subjective and prone to error. For example, a comparative study in which 28 chiropractors, physical therapists, rheumatologists, and orthopedic surgeons were asked to assess the posture of subjects from lateral photographs reported only mediocre intrarater reliability (kappa = 0.50) and weak interrater reliability (kappa = 0.16) [28].
Therefore, in order to objectify the analysis and quantify the shape of the back and spine in the sagittal plane, various measurements have been defined that can be determined non-invasively, such as the kyphosis angle, according to Debrunner [29]. The depth of cervical and lumbar lordosis can be assessed relatively easily with the parameters flèche cervicale (French for ‘cervical arrow’) and flèche lombaire (‘lumbar arrow’), usually using a plumb bob and a ruler [30,31]. Since these measurements can be collected quickly and inexpensively and are also reliable and reproducible [32], they have high practical suitability [33].
However, the above-mentioned methods have the disadvantage that the person being tested must usually be touched lightly during the measurement, so it cannot be ruled out that he or she will reflexively change posture as a result of the touch. In the case of postural defects due to immobile anatomical changes in the vertebrae, such as in Scheuermann’s disease, it can be assumed that the contour of the back will not change much as a result of touch. However, this cannot be ruled out in the case of postural deficiencies, where the shape of the back is determined primarily by muscular (dys)balance. Therefore, measurement methods that work via mechanical scanning of the back (e.g., Debrunner’s kyphometer [34], SpinalMouse® [35], ultrasound systems [36], manual inclinometers [37], flexicurve [38]) sometimes have limited informative value, especially in people sensitive to touch.
One approach to counter this fundamental methodological problem is to use a stereophotogrammetric system that can scan the back contour without contact and radiation exposure by means of light grids and digital cameras and record its spatial shape with a high degree of accuracy [37,39,40,41]. With this method, conclusions about the deformation of the underlying spine can be made based on the body surface using mathematical models. Fortin et al., in a comprehensive review, concluded that non-contact methods (such as digital photographs or 3D scans) provide an accurate and rapid way to perform clinical postural assessment [42].
Nevertheless, the problem remains of defining reference values on this basis in order to identify the types of deviations in postural weakness that do not yet represent serious pathology and therefore do not require the use of invasive measurement methods such as X-rays. Since postural parameters can develop over a lifetime and can differ between the sexes, it is helpful to have a practical database that provides reference values to support medical diagnoses. The studies of Ohlendorf et al., who defined reference values for individual target groups using stereophotogrammetry [43,44,45,46,47], should be mentioned here in particular. Furthermore, Wolf et al. [48] provided reference values for vertebral position in the thoracic and lumbar regions in women between 20 and 69 years of age using 3D stereophotogrammetry, and Huthwelker and colleagues collected reference data of three-dimensional spinal parameters in symptom-free subjects 18 to 70 years of age [49]. In a review, Ribeiro et al. summarized photogrammetrically determined reference data for posture in young women [50].
These recent works provide a suitable database for assessing posture in healthy individuals. However, stereophotogrammetry, in addition to its many measurement advantages, has the disadvantage of high investment cost and is therefore rarely used in many application areas. In contrast, photogrammetric posture analysis is based on digital photographs. Using this measurement method, Stolinski and colleagues, for example, established reference ranges of posture values for 7- to 10-year-old children [51], and Ludwig et al. provided reference values for a posture index for children and adolescents 6 to 17 years old [52]. Gong et al. used posture photographs to examine changes in various sagittal posture angles across an age range of 20 to 90 years, but with small sample sizes in each subgroup [53].
In summary, it can be stated that to the best of the authors’ knowledge, there is no study to date that covers all of the following criteria and is thus suitable for screening and preventive examinations of posture in everyday medical, physiotherapeutic, or occupational practice (compare also [31]):
(1) The parameters should be reliably and validly measurable with simple methods, without extensive effort and cost-intensive instruments;
(2) The parameters should be able to cover several levels of the trunk in the sagittal plane (cervical, thoracic, lumbar spine);
(3) Reference values should exist that define when postural parameters deviate from the norm depending on age and sex.
The aim of this study was, therefore, to assess the distribution of three sagittal posture parameters (flèche cervicale, flèche lombaire, kyphosis index) based on sex in a symptom-free population including different age groups and thus to provide diagnostically useful reference values. A non-contact and accurate measurement method should be used, from which parameters can be extracted that also can be measured with sufficient accuracy in daily medical or therapeutic practice using simpler methods, for example, based on evaluating posture photos.
2. Materials and Methods
Subjects were recruited from companies and associations. They were informed verbally and in writing about the study procedure and the applicable data protection regulations and provided their written informed consent. In the case of minors, additional consent was obtained from their legal guardians. The study was conducted according to the guidelines of the Declaration of Helsinki and was approved by the institutional ethics committees.
2.1. Subjects
This study included 1150 participants. Exclusion criteria were acute complaints, chronic diseases of the spine or musculoskeletal system, previous spinal surgery, leg length discrepancies greater than 5 mm, and vertigo.
2.2. Measurements
The examinations were carried out on site at the participating companies or associations in a separate room during health days. Participants’ body height was measured with a stadiometer (Seca Stadiometer 213, Seca, Hamburg, Germany), weight was determined with a scale, and body mass index (BMI) was calculated. A mobile scanner (Balance 4D, Paromed bodybalance GmbH & Co KG, Neubeuern, Germany) was used to measure posture. The Paromed scanner uses a Vialux scanning unit (Vialux GmbH, Chemnitz, Germany), whose accuracy and reliability have been demonstrated (coefficients of variations 0.3–2.5% [54]). The system works by projecting a moving light stripe pattern (LED light source, wavelength 460 ± 20 nm) onto the subject’s back and achieves a spatial resolution of <1 mm. The validity of stereophotogrammetric measurement methods for assessing trunk shape has been confirmed in previous studies [55]. The subjects stood without shoes in their habitual posture with free upper body (women in bra) at a distance of about 2.30 m from the device. For our measurements, several anatomical landmarks were marked with white tape dots (diameter 12 mm) by the examiner beforehand: the spinous process of the seventh cervical vertebra (C7); the apices of cervical, thoracic, and lumbar spine curves; the spinous process of the first sacral vertebra (S1); the posterior superior iliac spines (PSIS); and the apices of the scapulae. Each scan was performed 4 times and the values obtained were averaged.
The anatomical landmarks were automatically recognized by the system and manually checked and confirmed by the examiner. The measurement system calculated the horizontal distances of the 3 vertices to the perpendicular through S1 (Figure 1). From this, the analyzed posture parameters were calculated as follows:
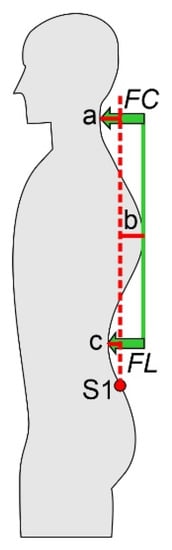
Figure 1.
Red lines: horizontal distances of the 3 vertices to the perpendicular (dotted red line) through the first sacral vertebra (S1). Green arrows: flèche cervicale (FC) and flèche lombaire (FL).
- Flèche cervicale FC = a + b;
- Flèche lombaire FL = b + c;
- Kyphosis index KI = (FC + FL)/2.
where a, b, and c represent the absolute values of the horizontal distances of the vertices from the perpendicular through S1 (Figure 1).
FC, FL, and KI were additionally calculated as percentages of trunk height (perpendicular distance between C7 and S1), denoted as FC%, FL%, and KI%.
2.3. Statistics
Subjects were divided into 10-year age groups. Exceptions were the two younger age groups: boys were grouped into 12–16 and 17–19 years and girls were grouped into 10–15 and 16–19 years. This unequal division was based on the different growth curves between sexes, since the growth spurt in boys normally does not begin until the age of 12, while in girls it begins at the age of 10, but also ends earlier [56]. Since only 3 individuals were older than 70 years, their data were excluded from further analysis; data on boys under 12 years (n = 11) and girls under 10 years (n = 4) were also excluded. Furthermore, separately for each sex-specific age group, extreme outliers exceeding 3 times the interquartile range were excluded (n = 5). Ultimately, data on 1127 subjects were used for final analysis.
Pearson correlation was used to calculate possible correlations between posture parameters. Because it was unclear whether the studied posture parameters depended on age and sex, a multivariate analysis of variance (MANOVA) was performed to test whether it was necessary to distinguish between age groups and sex. To avoid multicollinearity of the dependent variables, the non-normalized and normalized posture parameters were separately analyzed by MANOVA twice. The normal distribution of the data was checked using the Kolmogorov–Smirnov test. Because MANOVA is robust to deviations from the normal distribution [57], no transformation or non-parametric test was applied to data that were not normally distributed. The assumptions for MANOVA were checked and could be confirmed. Wilk’s lambda values are presented for the results of the MANOVA omnibus test. Effect size is reported as Cohen’s f, where f = 0.10 indicates a weak effect, f = 0.25 indicates a moderate effect, and f = 0.40 indicates a strong effect [58]. Bonferroni correction was applied to the post hoc tests. Adjusted p-values were reported and compared with an alpha level of 0.05.
In addition to age and sex, BMI is also reported in the literature as an influencing factor for posture, but the results are inconsistent [43,59]. In the present study, however, BMI was not included as separate factor in the MANOVA model because this would have resulted in very small subgroups and the focus of the paper is on age- and sex-specific differences. However, in order to evaluate sex-specific correlations of posture parameters with BMI, Pearson correlations were calculated.
Due to partly non-normally distributed data, means and medians, as well as corresponding bootstrap confidence intervals (1000 samples), were calculated to present group-specific values [60].
Calculations and visualizations were performed in SPSS (version 28, SPSS Inc., Chicago, IL, USA).
3. Results
3.1. Correlations of Postural Parameters
Table 1 shows the correlations of the posture parameters. KI, FC, and FL correlate very strongly with the corresponding normalized parameters KI%, FC%, and FL%. There are no or weak correlations between FL/FL% and FC/FC%. KI/KI% correlates strongly with the other parameters due to mathematical dependence.

Table 1.
Correlation coefficients between postural parameters.
3.2. Analysis of the Variables KI, FC, and FL
MANOVA showed significant differences for age (F(12, 2224) = 5.73, p < 0.001, np2 = 0.03, f = 0.18, Wilk’s Λ = 0.94) and sex (F(2, 1112) = 80.20, p < 0.001, np2 = 0.13, f = 0.39, Wilk’s Λ = 0.87) for the combined dependent variables KI, FC, and FL, but no interaction for age group and sex (F(12, 2224) = 1.60, p = 0.084, Wilk’s Λ = 0.98).
Post hoc univariate ANOVA showed statistically significant differences for both sex (KI: F(1, 1113) = 74.56, p ≤ 0.001, np2 = 0.06, f = 0.25; FC: F(1, 1113) = 156.02, p < 0.001, np2 = 0.12, f = 0.37) and age (KI: F(6, 1113) = 8.67, p < 0.001, np2 = 0.05, f = 0.23; FC: F(6, 1113) = 9.40, p < 0.001, np2 = 0.05, f = 0.23) for the dependent variables KI and FC. For FL, only differences between age groups were found (F(6, 1113) = 2.76, p = 0.01, np2 = 0.02, f = 0.14) but not for sex.
An interaction effect of age and sex was found for FC (F(6, 1113) = 2.80, p = 0.01, np2 = 0.02, f = 0.14), suggesting an increase in sex differences with increasing age. No further interaction effects were found (p > 0.05). Figure 2a,c,e shows the differences, including the results of the post hoc tests. Respective subgroup characteristics are presented in Table 2.
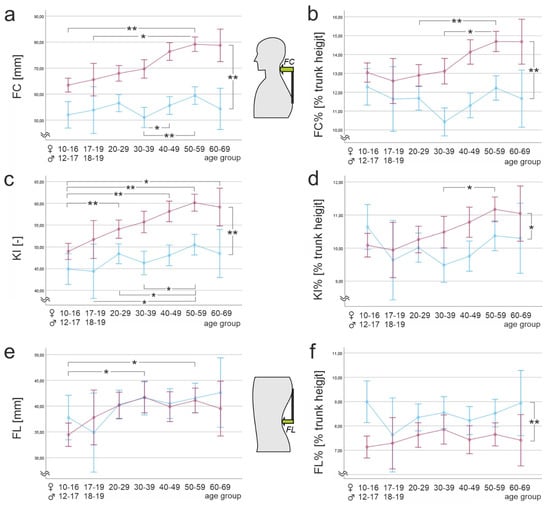
Figure 2.
Posture parameters depending on age and sex. (a) flèche cervicale (FC); (b) flèche cervicale normalized to trunk height (FC%); (c) kyphosis index (KI); (d) kyphosis index normalized to trunk height (KI%); (e) flèche lombaire (FL); (f) flèche lombaire normalized to trunk height (FL%). Blue: women; red: men. Note that Y-scales do not start at 0 for better resolution. * p < 0.05, ** p < 0.001.

Table 2.
Reference data of non-normalized posture parameters. Non-normally distributed data according to the Kolmogorov–Smirnov test are shown in italics. FC, flèche cervicale; FL, flèche lombaire; KI, kyphosis index.
3.3. Analysis of Variables Normalized to Trunk Height: KI%, FC%, and FL%
MANOVA showed significant differences for age (F(12, 2224) = 2.87, p < 0.001, np2 = 0.02, f = 0.14, Wilk’s Λ = 0.97) and sex (F(2, 1112) = 42.49, p < 0.001, np2 = 0.07, f = 0.27, Wilk’s Λ = 0.93) for the combined dependent variables KI%, FC%, and FL%. An interaction effect of age and sex for the combined dependent variables could also be found (F(12, 2224) = 1.76, p = 0.05, np2 = 0.01, f = 0.10, Wilk’s Λ = 0.98).
Post hoc univariate ANOVAs showed statistically significant differences for both sex (KI%: F(1, 1113) = 7.95, p = 0.005, np2 = 0.01, f = 0.10; FC%: F(1, 1113) = 59.57, p < 0.001, np2 = 0.05, f = 0.23) and age (KI%: F(6, 1113) = 2.89, p = 0.008, np2 = 0.02, f = 0.14; FC%: F(6, 1113) = 5.19, p < 0.001, np2 = 0.03, f = 0.18) for the dependent variables KI% and FC%. For FL%, statistically significant differences were found only between the sexes (F(1, 1113) = 18.14, p < 0.001, np2 = 0.02, f = 0.14). We found interaction effects of age and sex for KI% (F(6, 1113) = 2.25, p = 0.036, np2 = 0.01, f = 0.10) and FC% (F(6, 1113) = 2.74, p = 0.012, np2 = 0.02, f = 0.14). Sex differences seem to increase with increasing age for both variables. Figure 2b,d,f illustrates the differences found, including the post hoc tests. The statistical characteristics of subgroups are shown in Table 3.

Table 3.
Reference data of posture parameters normalized to the trunk height. Non-normally distributed data according to the Kolmogorov–Smirnov test are shown in italics.
3.4. Correlations of the Posture Parameters with BMI
When considering sex, BMI is significantly correlated with the posture parameters FC, FC%, KI, and KI%, but following Cohen [58], only a moderately strong positive correlation could be identified for FC in both sexes (male: r = 0.35, p < 0.001 and female: r = 0.31, p < 0.001). Other correlations could be classified as weak (CI: male: r = 0.27, p < 0.001 and female: r = 0.20, p < 0.001; CI%: male: r = 0.15, p < 0.001 and female: r = 0.11, p = 0.02; FC%: male: r = 0.25, p < 0.001 and female: r = 0.24, p < 0.001; FL%: female: r = −0.11, p = 0.02). No correlations were found for FL (female: r = −0.04, p = 0.40 and male: r = 0.3, p = 0.49) and FL% for men (r = −0.05, p = 0.19). The anthropometric data of the subjects are shown in Table 4.

Table 4.
Anthropometric data of subjects. BMI, body mass index.
4. Discussion
The aim of the present study was to find reference values for postural parameters in the sagittal plane and to show possible differences with respect to age and sex.
It is well known that, especially at the transition points between lordosis and kyphosis, a particularly strong structural stress of the vertebrae and their joints, especially the facet joints, occurs [61,62]. Against this background, the postural parameters flèche cervicale and flèche lombaire are particularly interesting because they are calculated from the magnitude of differences in the maximum points of kyphosis and lordosis in the sagittal plane. Thus, according to the biomechanical analysis of vertebral loading, Bruno et al. emphasize that measuring kyphosis depth alone is not sufficient to provide information about the loading of vertebral segments [62]. Both flèche parameters were introduced by Stagnara in 1982 and are part of orthopedic diagnostics [33]. Their advantage is that they can be measured quickly and with sufficient accuracy in medical practice using very simple materials.
4.1. Flèche Cervicale
For flèche cervicale (FC), an increase over the life span in men was observed, with differences becoming statistically significant mainly in relation to the younger age groups (Figure 2). In women, differences were seen only with respect to the 30–39 age group. This trend remained even when normalized to trunk height (FC%). Here, differences between the older age groups (50–59 years) and the middle and younger age groups (<40 years) were particularly evident in men. Here a deterioration of posture was seen, possibly originating from increasing muscular insufficiency, especially of the dorsal cervical and thoracic muscle groups. However, since the studied subjects came from all occupational categories, it is not possible to assign them, for example, to more sedentary or standing activities. The difference between the sexes increased over the life span, as shown by the interaction effects.
Drzał-Grabiec et al. studied two age cohorts of women (20–25 and 60–90 years) and reported a statistically significant increase in thoracic kyphosis with age [63]. They cited osteoporotic changes in the spine, which are more highly prevalent in women and lead to increased thoracic spine kyphotic curvature, as an explanation. In the present study, an increase, although not significant, was found only in men, who had a significantly higher flèche cervicale than women. Gong et al. also examined changes in various sagittal postural angles photogrammetrically over an age range of 20 to 90 years [53]. They found a decrease in the neck angle they measured, corresponding to an increase in cervical lordosis with age. Similar findings have been confirmed in other studies [64,65,66].
Ohlendorf et al. described three-dimensional posture parameters in men and women in four age groups between 21 and 60 years in several publications [43,44,45,46,47]. With increasing age, thoracic kyphosis and lumbar lordosis angles (women > men) increased regardless of sex. Although the kyphosis angle is not directly comparable to flèche cervicale, our data also show an increase, but it is significant only between a few age cohorts. However, an age-related increase in thoracic kyphosis in women, as described by Ohlendorf et al., did not affect flèche values in the parameters we examined [43].
4.2. Flèche Lombaire
The flèche lombaire values, in turn, are stable over the course of adulthood. While the absolute values for flèche lombaire (FL) were found to be the same between men and women and no longer changed significantly with age, when normalized to trunk height (FL%), a significant difference was found between the sexes, with higher values in women. This result is in agreement with Huthwelker et al. [49], who also used stereophotogrammetry to study 201 subjects 18–70 years of age and found a higher lordosis angle in women than in men. In a review, Arshad et al. [67] demonstrated significantly greater lumbar lordosis in women than in men. Ohlendorf et al. also reported greater lordosis depth in women [43]. A greater degree of lumbar lordosis and thoracic kyphosis in women is considered to be, among other factors, a biomechanical adaptation process to breast size [68]. However, it is interesting to note here that for the flèche lombaire parameter we studied, a significant difference between the sexes was found only when normalized to trunk height. Since flèche lombaire is defined as the relative difference between the apices of the lumbar and thoracic spines and structural load on the spine depends more on the degree of curvature, especially in the thoracolumbar junction, than on absolute value [61,62], it could be a more meaningful parameter for preventive assessment than absolute lordosis and kyphosis depth.
4.3. Kyphosis Index
The kyphosis index, which was calculated mathematically from the flèche values, showed a marked increase with age, more pronounced in men than in women. This was mainly due to the increase in FC. The percentage kyphosis index (KI%) allows a distinction between the sexes, but it is largely stable with age. Thus, it allows a summary description of posture and should be investigated in further studies, especially in patients, to determine possible relationships between postural abnormalities and pain.
4.4. Body Mass Index
A comparison of the anthropometric data of the subjects who were examined in the present study with reference values from the German population [69,70] showed that the cohorts were representative of the overall population in terms of height, weight, and BMI. Correlations between individual posture parameters and BMI were only weak to moderate. Other studies also did not show homogeneous results; Ohlendorf et al. found an increase in curvature parameters with BMI, especially in women [43]. Kocur et al. also found only a moderate association between BMI and postural parameters of the head and neck region [59].
4.5. Limitations
The present study has several limitations. First, it must be emphasized that we should speak only of reference data and not normative data. Even though a total of more than 1000 healthy subjects were examined, an age dependency of posture parameters was found in some cases. Therefore, to provide true standard values, a larger sample would have to be collected for each subgroup. The size of the subgroups is also not homogeneous. In the younger age groups, there was significantly fewer female than male participants, so sex differences that are to be statistically validated should be viewed with caution. Furthermore, the studied subjects were symptom-free, so one cannot extrapolate the results to patients. It is known that back pain patients show changes in posture [16,71].
Even if the anthropometric data of the examined subjects in their respective age groups corresponded to the reference values of the German population, it is not possible to speak of a representative sample. For example, neither the level of physical activity nor the occupational activity was examined.
The measurement methodology used has been well studied in terms of its accuracy, and all test quality criteria have been confirmed [72,73]. Nevertheless, it cannot be excluded that errors occurred during the manual positioning of individual marker points. Attempts were made to avoid this by providing extensive training for the researchers involved, who all have many years of experience in the field of posture analysis and work according to a standardized procedure.
4.6. Application in Everyday Medical Routine
For the examination of posture in the sagittal plane, the X-ray method is certainly the most informative and, therefore, the gold standard. In terms of non-invasive measurement methods, 3D stereophotogrammetry has been established as a very accurate non-contact method [72]. Its disadvantage, however, is the associated high cost, which makes it inaccessible in daily medical or therapeutic practice. However, preventive examinations are of great importance in promoting public health [74]. For this reason, we deliberately chose simple postural parameters that also can be determined without elaborate instrumental measurement methods. The advantage of the posture parameters we examined in more detail is that they can be determined with suitable accuracy even with very simple tools (pendulum and ruler) quickly and without computational effort (Figure 3). This makes them useful for screening in different settings (general practice, pediatric or physiotherapy offices, clubs, schools, and companies in the context of occupational health), and they can make an important contribution in terms of preventing postural weaknesses.
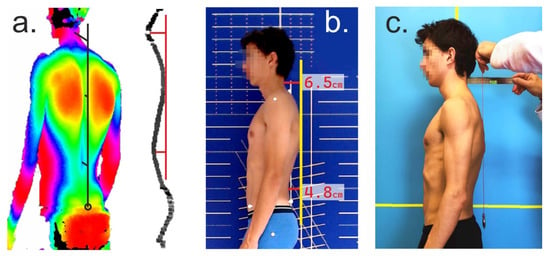
Figure 3.
Different methods to determine the parameters flèche cervicale and lombaire. (a) 3D stereophotogrammetry, dorsal contour, and lateral profile; (b) 2D photogrammetric analysis (analysis of digital photos with graphics software); (c) plumb bob and ruler. Note that the ruler has a spirit level to check the horizontal position.
Further studies should, in particular, delineate the reference values from pathological findings such as postural disorders. Likewise, an analysis of patients with different clinical symptoms would appear to be useful.
5. Conclusions
Flèche cervicale and flèche lombaire, as well as the kyphosis index calculated from it, represent easy-to-measure parameters with which posture can be quickly assessed. FL values appear to remain stable from adulthood onward, whereas FC, FC%, KI, and KI% increase with age in males, and sex differences become more pronounced with age. Taking into account age and sex differences, the posture can thus be assessed using the reference values presented in this study in order to initiate preventive or therapeutic measures if necessary.
Author Contributions
Conceptualization, O.L. and J.K.; methodology, O.L. and C.D.; software, C.D.; investigation, O.L., S.S., and F.N.; resources, M.F.; writing—original draft preparation, O.L., C.D., J.K., and M.F.; visualization, C.D. and O.L.; supervision, O.L., J.K., and M.F. All authors have read and agreed to the published version of the manuscript.
Funding
The study received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Ethics Committees (Saarland University: UdS 15-6-08; RPTU: 23-57).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. The person shown in Figure 3 provided written consent to be reprinted in this journal article as part of this study.
Data Availability Statement
The data will be made available upon justified request.
Acknowledgments
The authors thank P.P. Zender for assistance with measurement techniques and P. Buchberger for help with data acquisition.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Kratenova, J.; Zejglicova, K.; Maly, m.; Filipova, V. Prevalence and risk factors of poor posture in school children in the Czech Republic. J. Sch. Health 2007, 77, 131–137. [Google Scholar] [CrossRef] [PubMed]
- Wirth, B.; Humphreys, B.K. Pain characteristics of adolescent spinal pain. BMC Pediatr. 2015, 15, 42. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.-H. Effects of forward head posture on static and dynamic balance control. J. Phys. Ther. Sci. 2016, 28, 274–277. [Google Scholar] [CrossRef] [PubMed]
- Maulik, S.; Iqbal, R.; De, A.; Chandra, A.M. Evaluation of the working posture and prevalence of musculoskeletal symptoms among medical laboratory technicians. J. Back Musculoskelet. Rehabil. 2014, 27, 453–461. [Google Scholar] [CrossRef]
- Sainz de Baranda, P.; Cejudo, A.; Martínez-Romero, M.T.; Aparicio-Sarmiento, A.; Rodríguez-Ferrán, O.; Collazo-Diéguez, M.; Hurtado-Avilés, J.; Andújar, P.; Santonja-Medina, F. Sitting posture, sagittal spinal curvatures and back pain in 8 to 12-year-old children from the region of murcia (Spain): ISQUIOS programme. Int. J. Environ. Res. Public Health 2020, 17, 2578. [Google Scholar] [CrossRef]
- Czaprowski, D.; Stoliński, Ł.; Tyrakowski, M.; Kozinoga, M.; Kotwicki, T. Non-structural misalignments of body posture in the sagittal plane. Scoliosis Spinal Disord. 2018, 13, 6. [Google Scholar] [CrossRef]
- Frank, C.; Page, P.; Lardner, R. Assessment and Treatment of Muscle Imbalance: The Janda Approach; Human Kinetics: Champaign, IL, USA, 2009. [Google Scholar]
- Janet, A.; Rajalaxmi, V.; Ramachandran, S.; Priya, C.; Yuvarani, G.; Tharani, G.; Kamatchi, K. Prevalence of forward neck posture and influence of smartphones in physiotherapy students. Biomedicine 2021, 41, 660–664. [Google Scholar] [CrossRef]
- Nejati, P.; Lotfian, S.; Moezy, A.; Moezy, A.; Nejati, M. The relationship of forward head posture and rounded shoulders with neck pain in Iranian office workers. Med. J. Islam. Repub. Iran 2014, 28, 26. [Google Scholar]
- Singla, D.; Veqar, Z. Association Between Forward Head, Rounded Shoulders, and Increased Thoracic Kyphosis: A Review of the Literature. J. Chiropr. Med. 2017, 16, 220–229. [Google Scholar] [CrossRef]
- Han, J.; Park, S.; Kim, Y.; Choi, Y.; Lyu, H. Effects of forward head posture on forced vital capacity and respiratory muscles activity. J. Phys. Ther. Sci. 2016, 28, 128–131. [Google Scholar] [CrossRef]
- Kim, M.S.; Cha, Y.J.; Choi, J.D. Correlation between forward head posture, respiratory functions, and respiratory accessory muscles in young adults. J. Back Musculoskelet. Rehabil. 2017, 30, 711–715. [Google Scholar] [CrossRef]
- Jorgensson, A. The iliopsoas muscle and the lumbar spine. Aust. J. Physiother. 1993, 39, 125–132. [Google Scholar] [CrossRef]
- Glassman, S.D.; Bridwell, K.; Dimar, J.R.; Horton, W.; Berven, S.; Schwab, F. The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976) 2005, 30, 2024–2029. [Google Scholar] [CrossRef] [PubMed]
- Jentzsch, T.; Geiger, J.; Konig, M.A.; Werner, C.M. Hyperlordosis is Associated With Facet Joint Pathology at the Lower Lumbar Spine. Clin. Spine Surg. 2017, 30, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Feng, Q.; Jiang, C.; Zhou, Y.; Huang, Y.; Zhang, M. Relationship between spinal morphology and function and adolescent non-specific back pain: A cross-sectional study. J. Back Musculoskelet. Rehabil. 2017, 30, 625–633. [Google Scholar] [CrossRef] [PubMed]
- Wenig, C.M.; Schmidt, C.O.; Kohlmann, T.; Schweikert, B. Costs of back pain in Germany. Eur. J. Pain 2009, 13, 280–286. [Google Scholar] [CrossRef]
- Bartys, S.; Frederiksen, P.; Bendix, T.; Burton, K. System influences on work disability due to low back pain: An international evidence synthesis. Health Policy 2017, 121, 903–912. [Google Scholar] [CrossRef]
- Pincus, T.; Kent, P.; Bronfort, G.; Loisel, P.; Pransky, G.; Hartvigsen, J. Twenty-five years with the biopsychosocial model of low back pain—Is it time to celebrate? A report from the twelfth international forum for primary care research on low back pain. Spine 2013, 38, 2118–2123. [Google Scholar] [CrossRef]
- Lo, J.; Chan, L.; Flynn, S. A systematic review of the incidence, prevalence, costs, and activity and work limitations of amputation, osteoarthritis, rheumatoid arthritis, back pain, multiple sclerosis, spinal cord injury, stroke, and traumatic brain injury in the United States: A 2019 update. Arch. Phys. Med. Rehabil. 2021, 102, 115–131. [Google Scholar]
- Taimela, S.; Kujala, U.M.; Salminen, J.J.; Viljanen, T. The Prevalence of Low Back Pain Among Children and Adolescents: A Nationwide, Cohort-Based Questionnaire Survey in Finland. Spine 1997, 22, 1132–1136. [Google Scholar] [CrossRef]
- Martínez-Romero, M.T.; Cejudo, A.; Sainz de Baranda, P. Prevalence and characteristics of back pain in children and adolescents from the Region of Murcia (Spain): ISQUIOS programme. Int. J. Environ. Res. Public Health 2022, 19, 946. [Google Scholar] [CrossRef]
- Fabricant, P.D.; Heath, M.R.; Schachne, J.M.; Doyle, S.M.; Green, D.W.; Widmann, R.F. The epidemiology of back pain in American children and adolescents. Spine 2020, 45, 1135–1142. [Google Scholar] [CrossRef]
- Wu, A.; March, L.; Zheng, X.; Huang, J.; Wang, X.; Zhao, J.; Blyth, F.M.; Smith, E.; Buchbinder, R.; Hoy, D. Global low back pain prevalence and years lived with disability from 1990 to 2017: Estimates from the Global Burden of Disease Study 2017. Ann. Transl. Med. 2020, 8, 299. [Google Scholar] [CrossRef] [PubMed]
- Potthoff, T.; de Bruin, E.D.; Rosser, S.; Humphreys, B.K.; Wirth, B. A systematic review on quantifiable physical risk factors for non-specific adolescent low back pain. J. Pediatr. Rehabil. Med. 2018, 11, 79–94. [Google Scholar] [CrossRef] [PubMed]
- Sugai, K.; Michikawa, T.; Takebayashi, T.; Matsumoto, M.; Nakamura, M.; Nishiwaki, Y. Association between visual classification of kyphosis and future ADL decline in community-dwelling elderly people: The Kurabuchi study. Arch. Osteoporos. 2018, 14, 3. [Google Scholar] [CrossRef] [PubMed]
- Decker, S.; Müller, C.; Omar, M.; Krettek, C.; Schwab, F.; Trobisch, P. Sagittal balance of the spine--clinical importance and radiographic assessment. Zeitschrift fur Orthopadie und Unfallchirurgie 2015, 154, 128–133. [Google Scholar] [PubMed]
- Fedorak, C.; Ashworth, N.; Marshall, J.; Paull, H. Reliability of the visual assessment of cervical and lumbar lordosis: How good are we? Spine (Phila Pa 1976) 2003, 28, 1857–1859. [Google Scholar] [CrossRef]
- Korovessis, P.; Vitsas, V.; Syrimpeis, V.; Tsekouras, V. Evolution observation of coronal and sagittal spinal curvatures in school children with non-invasive, non-radiating methods: Scoliometer and Debrunner Kyphometer. Trends Med. 2019, 19, 1–8. [Google Scholar] [CrossRef]
- Stagnara, P.; De Mauroy, J.C.; Dran, G.; Gonon, G.P.; Costanzo, G.; Dimnet, J.; Pasquet, A. Reciprocal angulation of vertebral bodies in a sagittal plane: Approach to references for the evaluation of kyphosis and lordosis. Spine (Phila Pa 1976) 1982, 7, 335–342. [Google Scholar] [CrossRef]
- Patias, P.; Grivas, T.B.; Kaspiris, A.; Aggouris, C.; Drakoutos, E. A review of the trunk surface metrics used as Scoliosis and other deformities evaluation indices. Scoliosis 2010, 5, 12. [Google Scholar] [CrossRef]
- Allier, F.; Monnet, S. Mesure des flèches vertébrales par le télémètre laser. Évaluation de la fiabilité de la mesure de la flèche lombaire. Kinésithérapie la Revue 2013, 13, 41–46. [Google Scholar] [CrossRef]
- Lippold, C.; Segatto, E.; Végh, A.; Drerup, B.; Moiseenko, T.; Danesh, G. Sagittal back contour and craniofacial morphology in preadolescents. Eur. Spine J. 2010, 19, 427–434. [Google Scholar] [CrossRef]
- Greendale, G.A.; Nili, N.S.; Huang, M.H.; Seeger, L.; Karlamangla, A.S. The reliability and validity of three non-radiological measures of thoracic kyphosis and their relations to the standing radiological Cobb angle. Osteoporos. Int. 2011, 22, 1897–1905. [Google Scholar] [CrossRef]
- Livanelioglu, A.; Kaya, F.; Nabiyev, V.; Demirkiran, G.; Fırat, T. The validity and reliability of “Spinal Mouse” assessment of spinal curvatures in the frontal plane in pediatric adolescent idiopathic thoraco-lumbar curves. Eur. Spine J. 2016, 25, 476–482. [Google Scholar] [CrossRef] [PubMed]
- Takacs, M.; Rudner, E.; Kovacs, A.; Orlovits, Z.; Kiss, R.M. The assessment of the spinal curvatures in the sagittal plane of children using an ultrasound-based motion analysing system. Ann. Biomed. Eng. 2015, 43, 348–362. [Google Scholar] [CrossRef] [PubMed]
- Walicka-Cupryś, K.; Wyszyńska, J.; Podgórska-Bednarz, J.; Drzał-Grabiec, J. Concurrent validity of photogrammetric and inclinometric techniques based on assessment of anteroposterior spinal curvatures. Eur. Spine J. 2018, 27, 497–507. [Google Scholar] [CrossRef] [PubMed]
- Barrett, E.; McCreesh, K.; Lewis, J. Intrarater and interrater reliability of the flexicurve index, flexicurve angle, and manual inclinometer for the measurement of thoracic kyphosis. Rehabil. Res. Pract. 2013, 2013, 475870. [Google Scholar] [CrossRef] [PubMed]
- Singla, D.; Veqar, Z.; Hussain, M.E. Photogrammetric Assessment of Upper Body Posture Using Postural Angles: A Literature Review. J. Chiropr. Med. 2017, 16, 131–138. [Google Scholar] [CrossRef] [PubMed]
- D’Amico, M.; Kinel, E.; Roncoletta, P. Normative 3D opto-electronic stereo-photogrammetric posture and spine morphology data in young healthy adult population. PLoS ONE 2017, 12, e0179619. [Google Scholar] [CrossRef]
- Kurzydlo, W.; Stach, B.; Bober, A.; Wodzinska, M.; Dlugosz, M.M. Structured-light 3D scanner in use to assess the human body posture in physical therapy—A pilot study. Folia Med. Crac. 2014, 54, 21–35. [Google Scholar]
- Fortin, C.; Feldman, D.E.; Cheriet, F.; Labelle, H. Clinical methods for quantifying body segment posture: A literature review. Disabil. Rehabil. 2011, 33, 367–383. [Google Scholar] [CrossRef] [PubMed]
- Ohlendorf, D.; Avaniadi, I.; Adjami, F.; Christian, W.; Doerry, C.; Fay, V.; Fisch, V.; Gerez, A.; Goecke, J.; Kaya, U. Standard values of the upper body posture in healthy adults with special regard to age, sex and BMI. Sci. Rep. 2023, 13, 873. [Google Scholar] [CrossRef]
- Ohlendorf, D.; Fisch, V.; Doerry, C.; Schamberger, S.; Oremek, G.; Ackermann, H.; Schulze, J. Standard reference values of the upper body posture in healthy young female adults in Germany: An observational study. BMJ Open 2018, 8, e022236. [Google Scholar] [CrossRef] [PubMed]
- Ohlendorf, D.; Gerez, A.; Porsch, L.; Holzgreve, F.; Maltry, L.; Ackermann, H.; Groneberg, D. Standard reference values of the upper body posture in healthy male adults aged between 41 and 50 years in Germany. Sci. Rep. 2020, 10, 3823. [Google Scholar] [CrossRef] [PubMed]
- Ohlendorf, D.; Krüger, D.; Christian, W.; Ackermann, H.; Keil, F.; Oremek, G.; Maurer-Grubinger, C.; Groneberg, D.A. Standard reference values of the upper body posture in healthy male adults aged between 51 and 60 years in Germany. Sci. Rep. 2022, 12, 6961. [Google Scholar] [CrossRef]
- Ohlendorf, D.; Sosnov, P.; Keller, J.; Wanke, E.M.; Oremek, G.; Ackermann, H.; Groneberg, D.A. Standard reference values of the upper body posture in healthy middle-aged female adults in Germany. Sci. Rep. 2021, 11, 2359. [Google Scholar] [CrossRef] [PubMed]
- Wolf, C.; Betz, U.; Huthwelker, J.; Konradi, J.; Westphal, R.S.; Cerpa, M.; Lenke, L.; Drees, P. Evaluation of 3D vertebral and pelvic position by surface topography in asymptomatic females: Presentation of normative reference data. J. Orthop. Surg. Res. 2021, 16, 703. [Google Scholar] [CrossRef]
- Huthwelker, J.; Konradi, J.; Wolf, C.; Westphal, R.; Schmidtmann, I.; Drees, P.; Betz, U. Reference Values for 3D Spinal Posture Based on Videorasterstereographic Analyses of Healthy Adults. Bioengineering 2022, 9, 809. [Google Scholar] [CrossRef]
- Ribeiro, A.F.M.; Bergmann, A.; Lemos, T.; Pacheco, A.G.; Russo, M.M.; de Oliveira, L.A.S.; de Carvalho Rodrigues, E. Reference values for human posture measurements based on computerized photogrammetry: A systematic review. J. Manip. Physiol. Ther. 2017, 40, 156–168. [Google Scholar] [CrossRef] [PubMed]
- Stolinski, L.; Kozinoga, M.; Czaprowski, D.; Tyrakowski, M.; Cerny, P.; Suzuki, N.; Kotwicki, T. Two-dimensional digital photography for child body posture evaluation: Standardized technique, reliable parameters and normative data for age 7–10 years. Scoliosis Spinal Disord. 2017, 12, 38. [Google Scholar] [CrossRef]
- Ludwig, O.; Hammes, A.; Kelm, J.; Schmitt, E. Assessment of the posture of adolescents in everyday clinical practice: Intra-rater and inter-rater reliability and validity of a posture index. J. Bodyw. Mov. Ther. 2016, 20, 761–766. [Google Scholar] [CrossRef] [PubMed]
- Gong, H.; Sun, L.; Yang, R.; Pang, J.; Chen, B.; Qi, R.; Gu, X.; Zhang, Y.; Zhang, T.-m. Changes of upright body posture in the sagittal plane of men and women occurring with aging–a cross sectional study. BMC Geriatr. 2019, 19, 71. [Google Scholar] [CrossRef] [PubMed]
- Tischer, T.; Oye, S.; Wolf, A.; Feldhege, F.; Jacksteit, R.; Mittelmeier, W.; Bader, R.; Mau-Moeller, A. Measuring lower limb circumference and volume–introduction of a novel optical 3D volumetric measurement system. Biomed. Eng./Biomed. Tech. 2020, 65, 237–241. [Google Scholar] [CrossRef] [PubMed]
- Paul, S.M.; Chamberlin, A.P.; Hatt, C.; Nayak, A.V.; Danoff, J.V. Reliability, validity, and precision of an active stereophotogrammetry system for three-dimensional evaluation of the human torso. Med. Eng. Phys. 2009, 31, 1337–1342. [Google Scholar] [CrossRef] [PubMed]
- Schienkiewitz, A.; Rosario, A.S.; Neuhauser, H. German height references for children aged 0 to under 18 years compared to national and international data. Das Gesundh. 2010, 72, P65. [Google Scholar] [CrossRef]
- Finch, H. Comparison of the performance of nonparametric and parametric MANOVA test statistics when assumptions are violated. Methodology 2005, 1, 27–38. [Google Scholar] [CrossRef]
- Cohen, J. The effect size. In Statistical Power Analysis for the Behavioral Sciences; Routledge: New York, NY, USA, 1988; pp. 77–83. [Google Scholar]
- Kocur, P.; Tomczak, M.; Wiernicka, M.; Goliwąs, M.; Lewandowski, J.; Łochyński, D. Relationship between age, BMI, head posture and superficial neck muscle stiffness and elasticity in adult women. Sci. Rep. 2019, 9, 8515. [Google Scholar] [CrossRef]
- Hesterberg, T. Bootstrap. Wiley Interdiscip. Rev. Comput. Stat. 2011, 3, 497–526. [Google Scholar] [CrossRef]
- Morningstar, M.W.; Pettibon, B.R.; Schlappi, H.; Schlappi, M.; Ireland, T.V. Reflex control of the spine and posture: A review of the literature from a chiropractic perspective. Chiropr. Osteopathy 2005, 13, 16. [Google Scholar] [CrossRef]
- Bruno, A.G.; Anderson, D.E.; D’Agostino, J.; Bouxsein, M.L. The effect of thoracic kyphosis and sagittal plane alignment on vertebral compressive loading. J. Bone Miner. Res. 2012, 27, 2144–2151. [Google Scholar] [CrossRef]
- Drzał-Grabiec, J.; Snela, S.; Rykała, J.; Podgórska, J.; Banaś, A. Changes in the body posture of women occurring with age. BMC Geriatr. 2013, 13, 108. [Google Scholar] [CrossRef] [PubMed]
- Park, M.S.; Moon, S.-H.; Lee, H.-M.; Kim, S.W.; Kim, T.-H.; Lee, S.Y.; Riew, K.D. The effect of age on cervical sagittal alignment: Normative data on 100 asymptomatic subjects. Spine 2013, 38, E458–E463. [Google Scholar] [CrossRef] [PubMed]
- Yukawa, Y.; Kato, F.; Suda, K.; Yamagata, M.; Ueta, T. Age-related changes in osseous anatomy, alignment, and range of motion of the cervical spine. Part I: Radiographic data from over 1200 asymptomatic subjects. Eur. Spine J. 2012, 21, 1492–1498. [Google Scholar] [CrossRef] [PubMed]
- Machino, M.; Yukawa, Y.; Imagama, S.; Ito, K.; Katayama, Y.; Matsumoto, T.; Inoue, T.; Ouchida, J.; Tomita, K.; Ishiguro, N. Age-related and degenerative changes in the osseous anatomy, alignment, and range of motion of the cervical spine: A comparative study of radiographic data from 1016 patients with cervical spondylotic myelopathy and 1230 asymptomatic subjects. Spine 2016, 41, 476–482. [Google Scholar] [CrossRef]
- Arshad, R.; Pan, F.; Reitmaier, S.; Schmidt, H. Effect of age and sex on lumbar lordosis and the range of motion. A systematic review and meta-analysis. J. Biomech. 2019, 82, 1–19. [Google Scholar] [CrossRef]
- Findikcioglu, K.; Findikcioglu, F.; Ozmen, S.; Guclu, T. The impact of breast size on the vertebral column: A radiologic study. Aesthetic Plast. Surg. 2007, 31, 23–27. [Google Scholar] [CrossRef]
- Destatis. Statistisches Bundesamt: Body-Mass-Index (im Durchschnitt und Verteilung der Bevölkerung auf Body-Mass-Index-Gruppe). Available online: https://www.destatis.de (accessed on 31 January 2023).
- Schaffrath Rosario, A.; Kurth, B.-M.; Stolzenberg, H.; Ellert, U.; Neuhauser, H. Body mass index percentiles for children and adolescents in Germany based on a nationally representative sample (KiGGS 2003–2006). Eur. J. Clin. Nutr. 2010, 64, 341–349. [Google Scholar] [CrossRef]
- Schroeder, J.; Schaar, H.; Mattes, K. Spinal alignment in low back pain patients and age-related side effects: A multivariate cross-sectional analysis of video rasterstereography back shape reconstruction data. Eur. Spine J. 2013, 22, 1979–1985. [Google Scholar] [CrossRef]
- Pivotto, L.R.; Navarro, I.J.R.L.; Candotti, C.T. Radiography and photogrammetry-based methods of assessing cervical spine posture in the sagittal plane: A systematic review with meta-analysis. Gait Posture 2021, 84, 357–367. [Google Scholar] [CrossRef]
- Azadinia, F.; Hosseinabadi, M.; Ebrahimi, I.; Mohseni-Bandpei, M.-A.; Ghandhari, H.; Yassin, M.; Behtash, H.; Ganjavian, M.-S. Validity and test–retest reliability of photogrammetry in adolescents with hyperkyphosis. Physiother. Theory Pract. 2022, 38, 3018–3026. [Google Scholar] [CrossRef]
- Traeger, A.C.; Buchbinder, R.; Elshaug, A.G.; Croft, P.R.; Maher, C.G. Care for low back pain: Can health systems deliver? Bull. World Health Organ. 2019, 97, 423. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).