Translation, Cross-Cultural Adaptation and Psychometric Validation of the Greek Version of the Cardiac Rehabilitation Barriers Scale (CRBS-GR): What Are the Barriers in South-East Europe?
Abstract
1. Introduction
2. Methods
2.1. Design
2.2. Translation and Cross-Cultural Adaptation Process
2.3. Psychometric Testing
3. Results
3.1. Translation and Cross-Cultural Adaptation
3.2. Psychometric Validation
3.3. Main Barriers
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Abreu, A.; Pesah, E.; Supervia, M.; Turk-Adawi, K.; Bjarnason-Wehrens, B.; Lopez-Jimenez, F.; Ambrosetti, M.; Andersen, K.; Giga, V.; Vulic, D.; et al. Cardiac rehabilitation availability and delivery in Europe: How does it differ by region and compare with other high-income countries?: Endorsed by the European association of preventive cardiology. Eur. J. Prev. Cardiol. 2019, 26, 1131–1146. [Google Scholar] [CrossRef]
- Bansilal, S.; Castellano, J.M.; Fuster, V. Global burden of CVD: Focus on secondary prevention of cardiovascular disease. Int. J. Cardiol. 2015, 201 (Suppl. 1), S1–S7. [Google Scholar] [CrossRef]
- Townsend, N.; Kazakiewicz, D.; Wright, F.L.; Timmis, A.; Huculeci, R.; Torbica, A.; Gale, C.P.; Achenbach, S.; Weidinger, F.; Vardas, P. Epidemiology of cardiovascular disease in Europe. Nat. Rev. Cardiol. 2022, 19, 133–143. [Google Scholar] [CrossRef]
- Elstat. Deaths/2019. Available online: https://www.statistics.gr/en/statistics/-/publication/SPO09/2019 (accessed on 11 August 2022).
- Vos, T.; Lim, S.S.; Abbafati, C.; Abbas, K.M.; Abbasi, M.; Abbasifard, M.; Abbasi-Kangevari, M.; Abbastabar, H.; Abd-Allah, F.; Abdelalim, A.; et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the global burden of disease study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef]
- European Heart Network; ESC (European Society of Cardiology). Fighting Cardiovascular Disease—A Blueprint for EU Action, Brussels. 2020. Available online: File:///C:/Users/User/Downloads/05748%20CVD%20plan_digital%20edition.pdf (accessed on 22 October 2022).
- WHO. Cardiovascular Diseases. 2022. Available online: https://www.who.int/health-topics/cardiovascular-diseases#tab=tab_1 (accessed on 12 November 2022).
- Ambrosetti, M.; Abreu, A.; Corrà, U.; Davos, C.H.; Hansen, D.; Frederix, I.; Iliou, M.C.; Pedretti, R.F.; Schmid, J.P.; Vigorito, C.; et al. Secondary prevention through comprehensive cardiovascular rehabilitation: From knowledge to implementation. 2020 update. A position paper from the secondary prevention and rehabilitation section of the European association of preventive cardiology. Eur. J. Prev. Cardiol. 2020, 28, 2047487320913379. [Google Scholar] [CrossRef]
- Visseren, F.L.J.; Mach, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Bäck, M.; Benetos, A.; Biffi, A.; Boavida, J.-M.; Capodanno, D.; et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice: Developed by the task force for cardiovascular disease prevention in clinical practice with representatives of the European society of cardiology and 12 medical societies with the special contribution of the European association of preventive cardiology (EAPC). Eur. Heart J. 2021, 42, 3227–3337. [Google Scholar] [CrossRef]
- Salzwedel, A.; Jensen, K.; Rauch, B.; Doherty, P.; Metzendorf, M.-I.; Hackbusch, M.; Völler, H.; Schmid, J.-P.; Davos, C.H. Effectiveness of comprehensive cardiac rehabilitation in coronary artery disease patients treated according to contemporary evidence based medicine: Update of the cardiac rehabilitation outcome study (CROS-II). Eur. J. Prev. Cardiol. 2020, 27, 1756–1774. [Google Scholar] [CrossRef]
- Anderson, L.; Oldridge, N.; Thompson, D.R.; Zwisler, A.D.; Rees, K.; Martin, N.; Taylor, R.S. Exercise-based cardiac rehabilitation for coronary heart disease: Cochrane systematic review and meta-analysis. JACC 2016, 67, R713–R715. [Google Scholar] [CrossRef]
- Sandercock, G.R.; Cardoso, F.; Almodhy, M.; Pepera, G. Cardiorespiratory fitness changes in patients receiving comprehensive outpatient cardiac rehabilitation in the UK: A multicentre study. Heart 2013, 99, 785–790. [Google Scholar] [CrossRef]
- Antoniou, V.; Davos, C.H.; Kapreli, E.; Batalik, L.; Panagiotakos, D.B.; Pepera, G. Effectiveness of home-based cardiac rehabilitation, using wearable sensors, as a multicomponent, cutting-edge intervention: A systematic review and meta-analysis. J. Clin. Med. 2022, 11, 3772. [Google Scholar] [CrossRef]
- Neubeck, L.; Freedman, S.B.; Clark, A.M.; Briffa, T.; Bauman, A.; Redfern, J. Participating in cardiac rehabilitation: A systematic review and meta-synthesis of qualitative data. Eur. J. Prev. Cardiol. 2012, 19, 494–503. [Google Scholar] [CrossRef]
- Ruano-Ravina, A.; Pena-Gil, C.; Abu-Assi, E.; Raposeiras, S.; van ‘t Hof, A.; Meindersma, E.; Bossano Prescott, E.I.; González-Juanatey, J.R. Participation and adherence to cardiac rehabilitation programs. A systematic review. Int. J. Cardiol. 2016, 223, 436–443. [Google Scholar] [CrossRef]
- Santiago de Araújo Pio, C.; Chaves, G.S.S.; Davies, P.; Taylor, R.S.; Grace, S.L. Interventions to promote patient utilisation of cardiac rehabilitation. Cochrane Database Syst. Rev. 2019, 2019, CD007131. [Google Scholar] [CrossRef]
- Sari, D.M.; Wijaya, L.C.G. Cardiac rehabilitation via telerehabilitation in COVID-19 pandemic situation. Egypt Heart J. 2021, 73, 31. [Google Scholar] [CrossRef]
- Besnier, F.; Gayda, M.; Nigam, A.; Juneau, M.; Bherer, L. Cardiac rehabilitation during quarantine in COVID-19 pandemic: Challenges for center-based programs. Arch Phys. Med. Rehabil. 2020, 101, 1835–1838. [Google Scholar] [CrossRef]
- Stefanakis, M.; Batalik, L.; Papathanasiou, J.; Dipla, L.; Antoniou, V.; Pepera, G. Exercise-based cardiac rehabilitation programs in the era of COVID-19: A critical review. Rev. Cardiovasc. Med. Spec. Issue Card. Rehabil. 2021, 22, 270–275. [Google Scholar] [CrossRef]
- Ragupathi, L.; Stribling, J.; Yakunina, Y.; Fuster, V.; McLaughlin, M.A.; Vedanthan, R. Availability, use, and barriers to cardiac rehabilitation in LMIC. Glob. Heart 2017, 12, 323–334.e310. [Google Scholar] [CrossRef]
- Kotseva, K.; De Backer, G.; De Bacquer, D.; Rydén, L.; Hoes, A.; Grobbee, D.; Maggioni, A.; Marques-Vidal, P.; Jennings, C.; Abreu, A.; et al. Lifestyle and impact on cardiovascular risk factor control in coronary patients across 27 countries: Results from the European society of cardiology ESC-EORP EUROASPIRE V registry. Eur. J. Prev. Cardiol. 2019, 26, 824–835. [Google Scholar] [CrossRef]
- Shanmugasegaram, S.; Gagliese, L.; Oh, P.; Stewart, D.E.; Brister, S.J.; Chan, V.; Grace, S.L. Psychometric validation of the cardiac rehabilitation barriers scale. Clin. Rehabil. 2011, 26, 152–164. [Google Scholar] [CrossRef]
- Bullinger, M.; Alonso, J.; Apolone, G.; Leplège, A.; Sullivan, M.; Wood-Dauphinee, S.; Gandek, B.; Wagner, A.; Aaronson, N.; Bech, P.; et al. Translating health status questionnaires and evaluating their quality: The IQOLA project approach. J. Clin. Epidem. 1998, 51, 913–923. [Google Scholar] [CrossRef]
- Bartram, D.; Berberoglu, G.; Grégoire, J.; Hambleton, R.; Muñiz, J.; Van de Vijver, F. ITC guidelines for translating and adapting tests (second edition). Int. J. Test 2018, 18, 101–134. [Google Scholar] [CrossRef]
- Association, W.M. World medical association declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef]
- Martin Bland, J.; Altman, D. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986, 327, 307–310. [Google Scholar] [CrossRef]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef]
- Michopoulos, I.; Douzenis, A.; Kalkavoura, C.; Christodoulou, C.; Michalopoulou, P.; Kalemi, G.; Fineti, K.; Patapis, P.; Protopapas, K.; Lykouras, L. Hospital anxiety and depression scale (HADS): Validation in a Greek general hospital sample. Ann. Gen. Psychiatry 2008, 7, 4. [Google Scholar] [CrossRef]
- Antoniou, V.; Xanthopoulos, A.; Giamouzis, G.; Davos, C.; Batalik, L.; Stavrou, V.; Gourgoulianis, K.I.; Kapreli, E.; Skoularigis, J.; Pepera, G. Efficacy, efficiency and safety of a cardiac telerehabilitation programme using wearable sensors in patients with coronary heart disease: The TELEWEAR-CR study protocol. BMJ Open 2022, 12, e059945. [Google Scholar] [CrossRef] [PubMed]
- Sousa, V.D.; Rojjanasrirat, W. Translation, adaptation and validation of instruments or scales for use in cross-cultural health care research: A clear and user-friendly guideline. J. Eval. Clin. Pract. 2011, 17, 268–274. [Google Scholar] [CrossRef] [PubMed]
- Mokkink, L.B.; Terwee, C.B.; Patrick, D.L.; Alonso, J.; Stratford, P.W.; Knol, D.L.; Bouter, L.M.; de Vet, H.C.W. The COSMIN study reached aninternational consensus on taxonomy, terminology, and definitions of measurement properties for health-related patient-reported outcomes. J. Clin. Epidemiol. 2010, 63, 737–745. [Google Scholar] [CrossRef]
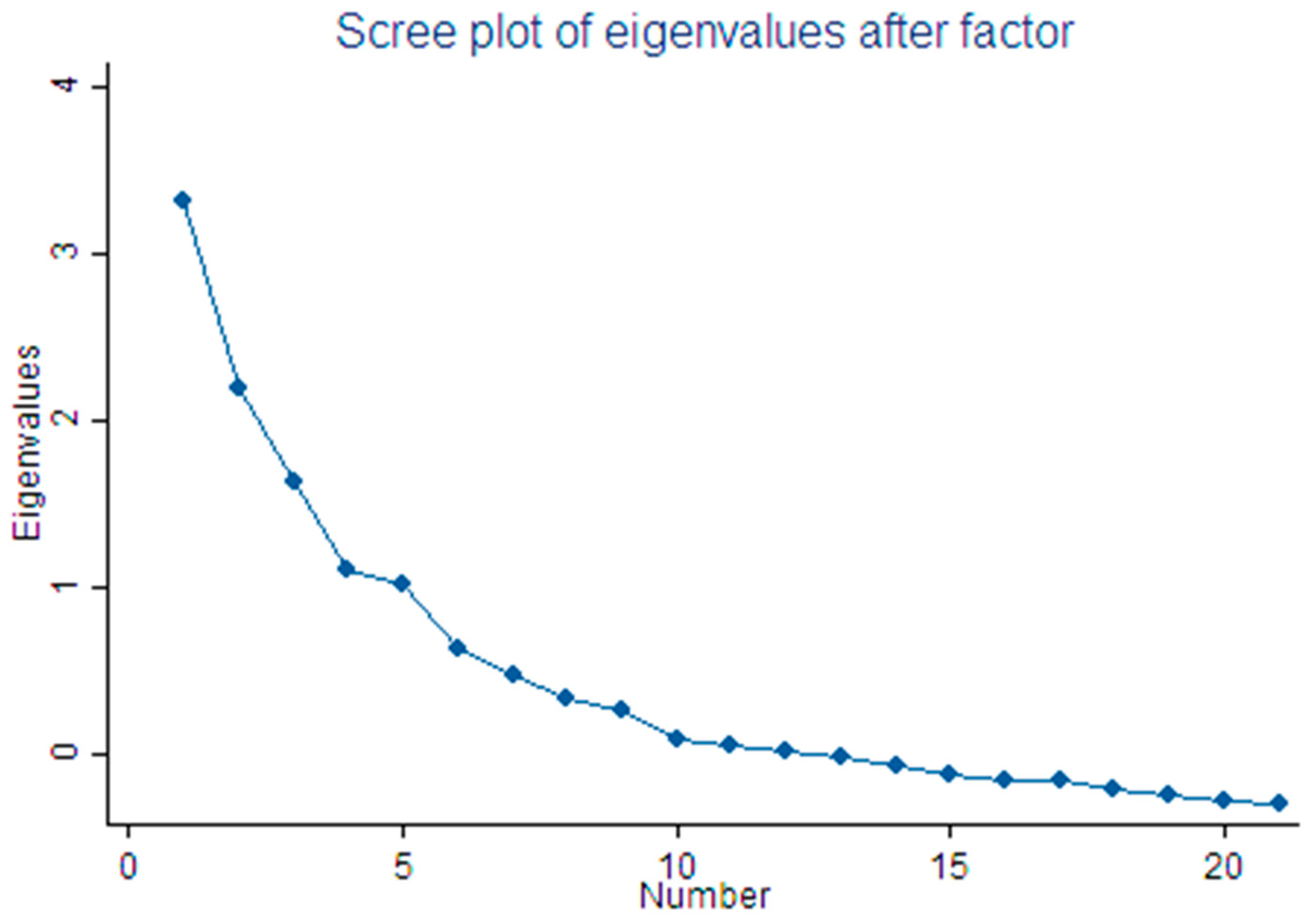
- Kaiser, H.F. The application of electronic computers to factor analysis. Educ. Psychol. Meas. 1960, 20, 141–151. [Google Scholar] [CrossRef]
- Cattell, R.B. The scree test for the number of factors. Multivar. Behav. Res. 1966, 1, 245–276. [Google Scholar] [CrossRef]
- Reymont, R.; Joreskog, K. Applied Factor Analysis in the Natural Sciences; Cambridge University: New York, NY, USA, 1993. [Google Scholar]
- Bland, J.M.; Altman, D.G. Cronbach’s alpha. BMJ Clin. Res. Ed. 1997, 314, 572. [Google Scholar] [CrossRef] [PubMed]
- Streiner, D.L.; Norman, G.R.; Cairney, J. Health Measurement Scales. A Practical Guide to Their Development and Use, 4th ed.; Oxford University Press: New York, NY, USA, 2014. [Google Scholar]
- Horn, J.L. A rationale and test for the number of factors in factor analysis. Psychometrika 1965, 30, 179–185. [Google Scholar] [CrossRef] [PubMed]
- Chai, L.S.; Siop, S.; Putit, Z.; Lim, L.; Gunggu, A.; Tie, S.F. Translation, adaptation, and validation of the malay version of the cardiac rehabilitation barriers scale. J. Nurs. Res. 2020, 28, e64. [Google Scholar] [CrossRef] [PubMed]
- Ghanbari-Firoozabadi, M.; Mirzaei, M.; Vafaii Nasab, M.; Grace, S.L.; Okati-Aliabad, H.; Madadizadeh, F.; Dadras, H.; Amrolahi, N.; Entezari, M.; Sadrbafghi, S.M. Cross-cultural adaptation and psychometric validation of the Persian version of the cardiac rehabilitation barriers scale (CRBS-P). BMJ Open 2020, 10, e034552. [Google Scholar] [CrossRef] [PubMed]
- Winnige, P.; Filakova, K.; Hnatiak, J.; Dosbaba, F.; Bocek, O.; Pepera, G.; Papathanasiou, J.; Batalik, L.; Grace, S.L. Validity and reliability of the cardiac rehabilitation barriers scale in the Czech Republic (CRBS-CZE): Determination of key barriers in east-central Europe. Int. J. Environ. Res. Public Health 2021, 18, 13113. [Google Scholar] [CrossRef]
- Kenis-Coskun, O.; Yagci, I.; Göçmen, S.; Sağdıç, B. Validity and reliability of the Turkish version of “cardiac rehabilitation barriers scale”. Gul. Med. J. 2019, 61, 59. [Google Scholar] [CrossRef]
- Liu, X.; Fowokan, A.; Grace, S.L.; Ding, B.; Meng, S.; Chen, X.; Xia, Y.; Zhang, Y. Translation, cross-cultural adaptation, and psychometric validation of the Chinese/Mandarin cardiac rehabilitation barriers scale (CRBS-C/M). Rehabil. Res. Pract. 2021, 2021, 5511426. [Google Scholar] [CrossRef]
- Ghisi, G.L.M.; Santos, R.Z.D.; Schveitzer, V.; Barros, A.L.; Recchia, T.L.; Oh, P.I.; Benetti, M.; Grace, S.L. Development and validation of the Brazilian Portuguese version of the cardiac rehabilitation barriers scale. Arquivos Brasileiros Cardiologia 2012, 98, 344–351. [Google Scholar] [CrossRef]
- Baek, S.; Park, H.-W.; Lee, Y.; Grace, S.L.; Kim, W.-S. Translation, cross-cultural adaptation and psychometric validation of the Korean-language cardiac rehabilitation barriers scale (CRBS-K). Arm 2017, 41, 858–867. [Google Scholar] [CrossRef]
- Stefanakis, M.; Batalik, L.; Antoniou, V.; Pepera, G. Safety of home-based cardiac rehabilitation: A systematic review. Heart Lung J. Crit. Care 2022, 55, 117–126. [Google Scholar] [CrossRef]
- Nkonde-Price, C.; Reynolds, K.; Najem, M.; Yang, S.-J.; Batiste, C.; Cotter, T.; Lahti, D.; Gin, N.; Funahashi, T. Comparison of home-based vs. center-based cardiac rehabilitation in hospitalization, medication adherence, and risk factor control among patients with cardiovascular disease. JAMA Netw. Open 2022, 5, e2228720. [Google Scholar] [CrossRef] [PubMed]
- Kraal, J.J.; Elske Van Den Akker-Van Marle, M.; Abu-Hanna, A.; Stut, W.; Peek, N.; Kemps, H.M.C. Clinical and cost-effectiveness of home-based cardiac rehabilitation compared to conventional, centre-based cardiac rehabilitation: Results of the FIT@Home study. Eur. J. Prev. Cardiol. 2017, 24, 1260–1273. [Google Scholar] [CrossRef] [PubMed]
- Batalik, L.; Filakova, K.; Sladeckova, M.; Dosbaba, F.; SU, J.J.; Pepera, G. The cost-effectiveness of telehealth exercise-based cardiac rehabilitation intervention: A systematic review. Eur. J. Phys. Rehabil. Med. 2023, 59. [Google Scholar] [CrossRef]
- Batalik, L.; Pepera, G.; Su, J.J. Cardiac telerehabilitation improves lipid profile in the long term: Insights and implications. Int. J. Cardiol. 2022, 367, 117–118. [Google Scholar] [CrossRef] [PubMed]
- Ramachandran, H.J.; Jiang, Y.; Tam, W.W.S.; Yeo, T.J.; Wang, W. Effectiveness of home-based cardiac telerehabilitation as an alternative to Phase 2 cardiac rehabilitation of coronary heart disease: A systematic review and meta-analysis. Eur. J. Prev. Cardiol. 2021, 29, 1017–1043. [Google Scholar] [CrossRef] [PubMed]
| 1. Is the questionnaire, in your opinion, useful for assessing “barriers to cardiac rehabilitation”? (90.66%) 2. Do you think the questionnaire asks about your barriers to cardiac rehabilitation? (89.33%) 3. What do you think about the size of the questionnaire? (92.00%) 4. Are the questions clearly put forward? (87.33%) 5. Is the questionnaire well organized? (91.66%) 6. Did you understand the questions of the questionnaire? (92.33%) 7. Did you face any difficulty while completing the questionnaire? No (89.00%) 8. What do you think about the layout of the questionnaire questions? (88.00%). |
| Characteristic | ||
|---|---|---|
| Age (years) | Mean = 65.27, SD = 10.21 | |
| Gender | Male | 97 (88.2%) |
| Female | 13 (11.8%) | |
| Education level | Primary | 56 (50.9%) |
| Secondary | 34 (30.9%) | |
| Higher | 20 (18.2%) | |
| Distance to center from home | Larissa or ≤50 km | 52 (47.3%) |
| >50 km | 58 (52.7%) | |
| Body mass index | Normal Weight | 36 (32.7%) |
| Overweight | 46 (41.8%) | |
| Obese | 27 (24.6%) | |
| Morbid Obesity | 1 (0.9%) | |
| Hyperlipidemia | Normal | 27 (24.6%) |
| Elevated | 83 (75.5%) | |
| Smoking | Yes | 64 (58.2%) |
| No | 46 (41.8%) | |
| Items | Subscales | |||
|---|---|---|---|---|
| Comorbidities/Functional Status | Logistical Factors | Work Constraints/Lack of Time | Perceived Need/ Healthcare Factors | |
| 9. I find exercise tiring or painful | 0.7309 | |||
| 13. Lack of energy | 0.6944 | |||
| 15. Age (old) | 0.5099 | |||
| 14. Other health issues that prevent me from participating (specify: ) | 0.4641 | |||
| 7. I already practice at home or in my community | −0.4061 | |||
| 21. I prefer to take care of my health on my own and not through participating in groups | 0.4002 | |||
| 1. Distance (e.g., it is not located in your area, too far to travel) | 0.8095 | |||
| 2. Costs (e.g., parking, fuel) | 0.7635 | |||
| 3. Mobility difficulties (e.g., access in a car, Public transport) | 0.5931 | |||
| 8. Bad weather conditions | 0.4233 | |||
| 4. Family obligations | 0.3366 | |||
| 19. I think I got referred but the program did not contact me | 0.7686 | |||
| 20. It took me a long time to catch up and enter the program | 0.7502 | |||
| 11. Time constraints (e.g., very busy) | 0.5062 | |||
| 10. Frequent trips (e.g., holidays, business, home) | 0.4674 | |||
| 17. Many people with cardiac problems do not go and they are fine | 0.4047 | |||
| 12. Work commitments | 0.3774 | |||
| 16. My doctor didn’t think it was so necessary | 0.5572 | |||
| 6. I don’t need cardiac rehabilitation | 0.5133 | |||
| 5. Lack of information about cardiac rehabilitation (e.g., I did not have an update from my doctor) | 0.5116 | |||
| 18. I can handle my heart problem on my own | 0.3322 | |||
| Eigenvalues | 3.308 | 2.190 | 1.630 | 1.092 |
| Variance explained (%) | 35.19 | 23.30 | 17.34 | 11.61 |
| Cumulative variance explained (%) | 35.19 | 58.49 | 75.83 | 87.44 |
| Reliability: Cronbach’s α | 0.70 | 0.74 | 0.68 | 0.56 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Antoniou, V.; Pasias, K.; Loukidis, N.; Exarchou-Kouveli, K.K.; Panagiotakos, D.B.; Grace, S.L.; Pepera, G. Translation, Cross-Cultural Adaptation and Psychometric Validation of the Greek Version of the Cardiac Rehabilitation Barriers Scale (CRBS-GR): What Are the Barriers in South-East Europe? Int. J. Environ. Res. Public Health 2023, 20, 4064. https://doi.org/10.3390/ijerph20054064
Antoniou V, Pasias K, Loukidis N, Exarchou-Kouveli KK, Panagiotakos DB, Grace SL, Pepera G. Translation, Cross-Cultural Adaptation and Psychometric Validation of the Greek Version of the Cardiac Rehabilitation Barriers Scale (CRBS-GR): What Are the Barriers in South-East Europe? International Journal of Environmental Research and Public Health. 2023; 20(5):4064. https://doi.org/10.3390/ijerph20054064
Chicago/Turabian StyleAntoniou, Varsamo, Konstantinos Pasias, Nektarios Loukidis, Kalliopi K. Exarchou-Kouveli, Demosthenes B. Panagiotakos, Sherry L. Grace, and Garyfallia Pepera. 2023. "Translation, Cross-Cultural Adaptation and Psychometric Validation of the Greek Version of the Cardiac Rehabilitation Barriers Scale (CRBS-GR): What Are the Barriers in South-East Europe?" International Journal of Environmental Research and Public Health 20, no. 5: 4064. https://doi.org/10.3390/ijerph20054064
APA StyleAntoniou, V., Pasias, K., Loukidis, N., Exarchou-Kouveli, K. K., Panagiotakos, D. B., Grace, S. L., & Pepera, G. (2023). Translation, Cross-Cultural Adaptation and Psychometric Validation of the Greek Version of the Cardiac Rehabilitation Barriers Scale (CRBS-GR): What Are the Barriers in South-East Europe? International Journal of Environmental Research and Public Health, 20(5), 4064. https://doi.org/10.3390/ijerph20054064








