Determinants of Public Health Personnel Spending in Spain
Abstract
1. Introduction
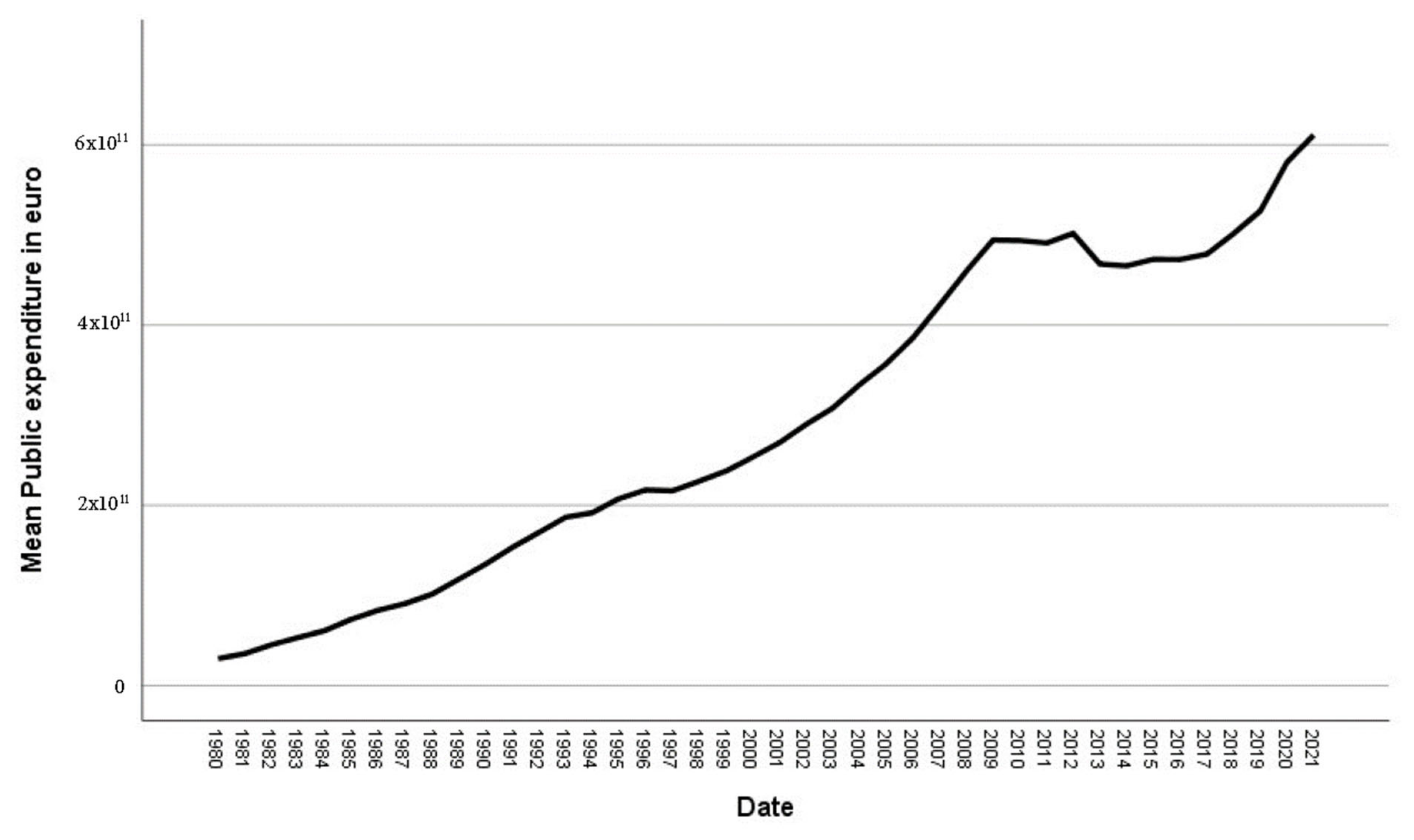
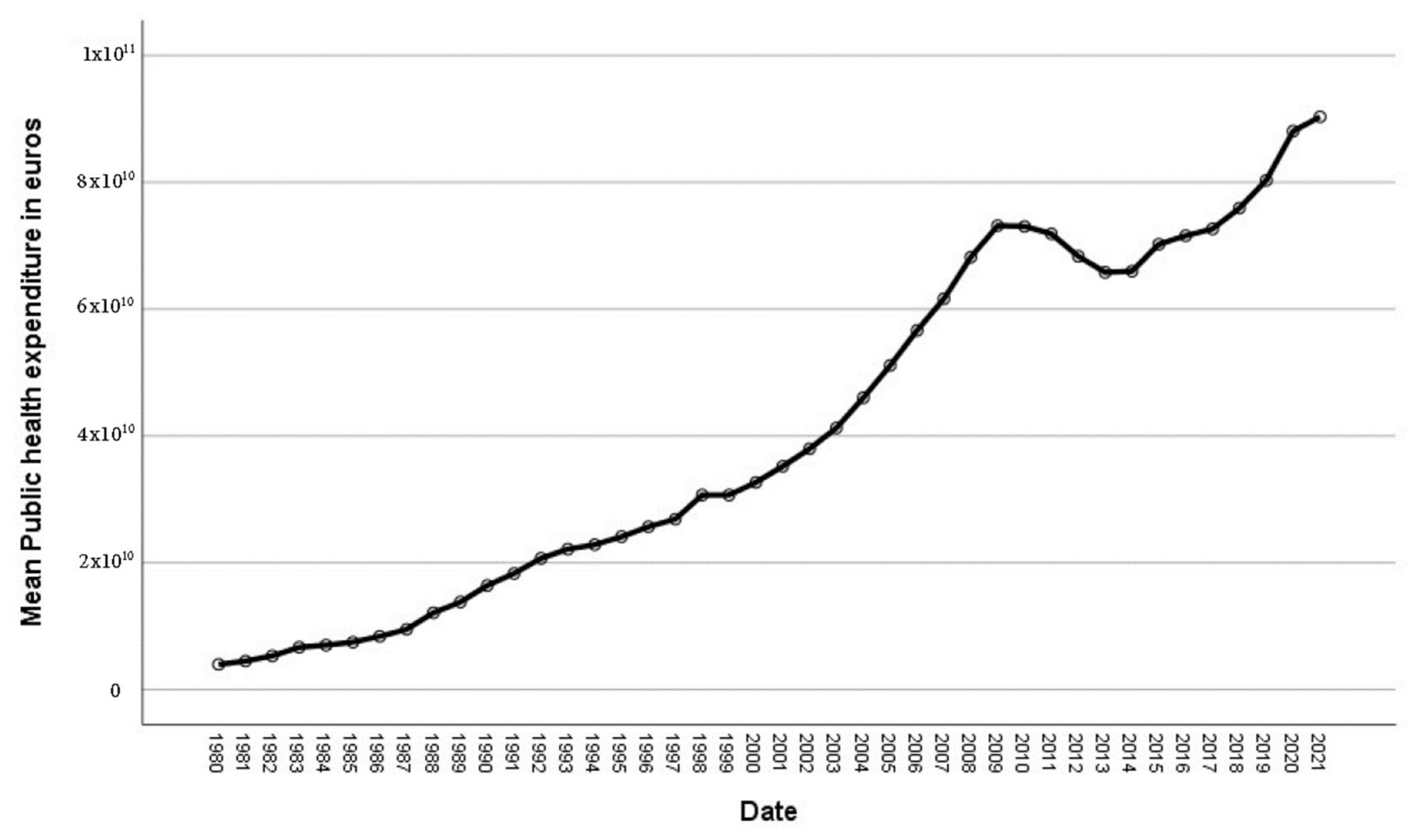
Descriptive Analysis
2. Aims of the Study
3. Methods
Initial Study for Calculating COVID-19 Impact on Spanish GDP
4. Results
5. Discussion
6. Conclusions
6.1. Implications for Health Care Provision and Use
6.2. Implications for Health Policies
6.3. Implications for Further Research
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Organización Mundial de la Salud (WHO). Informe Sobre la Salud en el Mundo 2000. Mejorar el Desempeño de los Sistemas de Salud; OMS: Geneva, Switzerland, 2000; p. 6. [Google Scholar]
- Fernández, A.; Vaquera, M.M. Análisis de la Evolución Histórica de la Sanidad y la Gestión Sanitaria en España. Available online: https://dialnet.unirioja.es/revista/486/V/14 (accessed on 17 August 2022).
- Yamey, G.; Beyeler, N.; Wadge, H.; Jamison, D. Invirtiendo en salud: El argumento económico. Informe del Foro sobre Inversión en Salud de la Cumbre Mundial sobre Innovación para la Salud 2016. Salud Pública Mex. 2017, 59, 321–342. [Google Scholar] [CrossRef] [PubMed]
- Artigas-Lelong, B.; Bennasar-Veny, M. La salud en el siglo XXI: El reto de los cuidados multiculturales. Index Enferm. 2009, 18, 42–46. [Google Scholar] [CrossRef]
- Woodland, L.; Blignault, I.; O’Callaghan, C.; Harris-Roxas, B. A framework for preferred practices in conducting culturally competent health research in a multicultural society. Health Res. Policy Syst. 2021, 19, 24. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez, M.; Freire, M.; Pais, C. El efecto del gasto público sanitario y educativo en la determinación del bienestar de los países de la OCDE: Un modelo con datos de panel. Cuad. Econ. 2018, 41, 104–118. [Google Scholar] [CrossRef]
- Hojman, D. Economic and other determinants of infant and child mortality in small developing countries: The case of Central America and the Caribbean. Appl. Econ. 1996, 28, 281–290. [Google Scholar] [CrossRef] [PubMed]
- Bidani, B.; Ravallion, M. Decomposing social indicators using distributional data. J. Econ. 1997, 77, 125–139. [Google Scholar] [CrossRef]
- Anand, S.; Ravallion, M. Human development in poor countries: On the role of private incomes and public services. J. Econ. Perspect. 1993, 7, 133–150. [Google Scholar] [CrossRef]
- Pérez Gázquez, I.M. Health models and response capacity to epidemiological risks: Towards a universality in terms of access and free services. TECHNO Rev. Int. Technol. Sci. Soc. Rev. 2022, 11, 1–10. [Google Scholar] [CrossRef]
- López-Rodríguez, A.; Abab-Bassols, A.; Esteban-Gonzalo, S. Los Sistemas Sanitarios en los Países de la UE: Características e Indicadores de Salud 2013; Ministerio de Sanidad, Servicios Sociales e Igualdad: Madrid, España, 2014; p. 10. [Google Scholar]
- Kehr, J.; Muinde, J.V.; Prince, R.J. Health for All? Pasts, presents and futures of aspirations for universal healthcare. Soc. Sci. Med. 2023, 319, 115660. [Google Scholar] [CrossRef]
- Ministry of Health, Social Services and Equality. National Health System of Spain. 2012. Available online: https://www.sanidad.gob.es/gl/organizacion/sns/docs/sns2012/SNS012__Ingles.pdf (accessed on 17 August 2022).
- Martín, J.; López del Amo, M. Innovaciones Organizativas y de Gestión en el Sistema Nacional de Salud. In Gestión Hospitalaria; Temes, J.L., Mengíbar, M., Eds.; McGraw Hill España: Madrid, España, 2007; pp. 567–580. [Google Scholar]
- Hinrichs, K. Recent pension reforms in Europe: More challenges, new directions. An overview. Soc. Policy Adm. 2021, 55, 409–422. [Google Scholar] [CrossRef]
- Organization for Economic Cooperation and Development (OECD). State of Health in the EU. 2019. Available online: https://www.oecd.org/spain/Espa%C3%B1a-Perfil-sanitario-nacional-2019-Launch-presentation.pdf (accessed on 22 October 2022).
- Organization for Economic Cooperation and Development (OECD). Health Care Expenditure and Financing. Available online: https://stats.oecd.org/ (accessed on 22 October 2022).
- Vela, E.; Clèries, M.; Vella, V.; Adroher, C.; García-Altés, A. Análisis poblacional del gasto en servicios sanitarios en Cataluña (España): ¿Qué y quién consume más recursos? Gac. Sanit. 2017, 33, 24–31. [Google Scholar] [CrossRef] [PubMed]
- Oliva, J.; Peña-Longobardo, L.; Gonzalez, B.; Barber, P.; Zozaya, N. Crisis económica y salud: Lecciones aprendidas y recomendaciones para el futuro. Cuad. Econ. ICE 2018, 96, 165–196. [Google Scholar] [CrossRef]
- Lopez-Valcarcel, B. Eficiencia y Sostenibilidad en la gestión clínica. In Proceedings of the XXXIV Congreso de la SECA and XXI Congreso de la SEDECA, Córdoba, España, 19–21 October 2023. [Google Scholar]
- Torchia, M.; Calabró, A.; Morner, M. Public-private partnerships in the health care sector: A systematic review of the literature. Public Manag. Rev. 2015, 17, 236–261. [Google Scholar] [CrossRef]
- Ministerio de Sanidad, Servicios Sociales e Igualdad. Presupuestos Iniciales Para Sanidad de las CCAA, la Administración Central y la Seguridad Social. Available online: https://www.msssi.gob.es/estadEstudios/estadisticas/inforRecopilaciones/docs/presupuestosIniciales.pdf (accessed on 5 July 2020).
- Miguel, J.; Belda, C. Los nuevos modelos de gestión de hospitales como alternativa para la sostenibilidad del sistema hospitalario público: Un análisis de eficiencia en gasto sanitario. J. Health Qual. Res. 2019, 34, 131–147. [Google Scholar] [CrossRef] [PubMed]
- Villalobos, J. Análisis del sistema de cuentas de salud 2017. Rev. Agathos. 2019, 19, 56–63. [Google Scholar]
- Blanco, Á.; Urbanos-Garido, R.; Thuissard, I. Evolución de la prestación real media en España por edad y sexo (1998–2008) y su repercusión en las proyecciones de gasto sanitario público. Gac. Sanit. 2013, 27, 220–225. [Google Scholar] [CrossRef]
- Blanco, A.; De Bustos, A. El gasto sanitario público en España: Diez años de Sistema Nacional de Salud. Hacienda Pública Esp. 1996, 3, 3–27. [Google Scholar]
- Urbanos, R.; Blanco, A. Impacto del Envejecimiento en el Gasto Público Sanitario y Sociosanitario Para el Período 2000–2050; Ministerio de Sanidad y Consumo: Madrid, España, 2002; pp. 15–18. [Google Scholar]
- Casado, D.; Puig-Junoy, J.; Puig, R. El Impacto de la Demografía Sobre el Gasto Sanitario Futuro de las CCAA; Fundación Pfizer: Madrid, España, 2009; pp. 31–33. [Google Scholar]
- Jung, N.; Meseguer, J.; Herce, J. Gasto Sanitario y Envejecimiento de la Población en España; Fundación BBVA: Bilbao, España, 2003; pp. 34–37. [Google Scholar]
- Puig-Junoy, J.; Planas, I.; Tur, A. Factores de Crecimiento y Proyecciones del Gasto Sanitario Público Por COMUNIDADES AUTÓNOMAS. Registro Histórico 1991–2003 y Proyecciones 2004–2017; Universitat Pompeu Fabra: Barcelona, España, 2005; pp. 1–3. [Google Scholar]
- Sanfélix-Gimeno, G.; Peiró, S.; Librero, J.; Ausejo-Segura, M.; Suárez-Alemán, C.; Molina-López, T.; Celaya, M.; Castaño-Riera, E. Análisis poblacional por áreas de salud de las variaciones en consumo, precio y gasto de medicamentos cardiovasculares en 8 comunidades autónomas, España, 2005. Rev. Esp. Salud Pública 2010, 84, 389–407. [Google Scholar]
- Organización Mundial de la Salud. Directrices Para Ayudar a los Países a Mantener los Servicios Sanitarios Esenciales Durante la Pandemia COVID-19. Available online: https://www.who.int/es/news-room/detail/30-03-2020-who-releases-guidelines-to-help-countries-maintain-essential-health-services-during-the-covid-19-pandemic (accessed on 6 July 2020).
- Miranda, M. Revisión y reflexión sobre la sanidad pública Española. Enfermería Nefrol. 2014, 17, 85–91. [Google Scholar] [CrossRef]
- Bernal-Delgado, E.; García-Armesto, S.; Oliva, J.; Sánchez, F.; Repullo, J.; Peña-Longardo, L.; Ridao-López, M.; Hernández-Quevedo, C. España. Informe del sistema sanitario. Sist. Sanit. Transic. 2018, 20, 1–179. [Google Scholar]
- Muthuri, R.N.D.K.; Senkubuge, F.; Hongoro, C. An Investigation of Healthcare Professionals’ Motivation in Public and Mission Hospitals in Meru County, Kenya. Healthcare 2020, 8, 530. [Google Scholar] [CrossRef] [PubMed]
- Blázquez-Fernández, C.; Cantarero-Prieto, D.; Pascual-Sáez, M. Políticas públicas de descentralización: ¿Más gasto y mejores resultados salud? Rev. Eval. Programas Políticas Públicas 2016, 1, 49–65. [Google Scholar] [CrossRef]
- Peña-Longobardo, L.; Aranda-Reneo, I.; Oliva-Moreno, J.; Vall-Castello, J. Evaluación de las pérdidas laborales provocadas enfermedades y lesiones en España en el año 2009. Rev. Eval. Programas Políticas Públicas 2016, 6, 66–85. [Google Scholar] [CrossRef]
- Martínez-Pérez, J.; Sanchez-Martínez, F.; Abellán-Perpiñán, J. Esperanza de Vida Ajustada por la Calidad en España: Una aproximación. Rev. Eval. Programas Políticas Públicas 2016, 6, 28–48. [Google Scholar] [CrossRef]
- Santric-Milicevic, M.; Vasic, V.; Terzic-Supic, Z. Do health care workforce, population, and service provision significantly contribute to the total health expenditure? An econometric analysis of Serbia. Hum. Resour. Health 2016, 14, 50. [Google Scholar] [CrossRef] [PubMed]
- Organización Mundial de la Salud. COVID-19: Cronología de la Actuación de la OMS. Available online: https://www.who.int/es/news/item/27-04-2020-who-timeline---covid-19 (accessed on 29 June 2020).
- Spiteri, G.; Fielding, J.; Diercke, M.; Campese, C.; Enouf, V.; Gaymard, A.; Bella, A.; Sognamiglio, P.; Sierra, M.J.; Riutort, A.N.; et al. First cases of coronavirus disease 2019 (COVID-19) in the WHO European Region, 24 January to 21 February 2020. Eurosurveillance 2020, 25, 2000178. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control. Geographical Distribution of 2019-nCov Cases Globally 2020—2 February 2020. Available online: https://www.ecdc.europa.eu/en/geographical-distribution-2019-ncov-cases (accessed on 18 June 2020).
- World Health Organization Regional Office for Europe. Countries 2020. Copenhagen: WHO/Europe. Available online: http://www.euro.who.int/en/countries (accessed on 12 February 2020).
- Torres, R.; Fernández, M.J. La política económica española y el COVID-19. Funcas Cuad. Inf. Econ. 2020, 275, 1–7. [Google Scholar]
- García-Basteiro, A.; Alvarez-Dardet, C.; Arenas, A.; Bengoa, R.; Borrell, C.; Del Val, M.; Franco, M.; Gea-Sánchez, M.; Otero, J.J.G.; Valcárcel, B.G.L.; et al. The need for an independent evaluation of the COVID-19 response in Spain. Lancet 2020, 396, 529–530. [Google Scholar] [CrossRef]
- Cameron, E.; Nuzzo, J.; Bell, J. Global Health Security Index: Building Collective Action and Accountability. Available online: https://www.ghsindex.org/wp-content/uploads/2019/10/2019-Global-Health-Security-Index.pdf (accessed on 21 July 2020).
- Khan, J.; Awan, N.; Islam, M.; Muurlink, O. Healthcare capacity, health expenditure, and civil society as predictors of COVID-19 case fatalities: A global analysis. Front. Public Health 2020, 8, 347. [Google Scholar] [CrossRef]
- Banco de España. Escenarios macroeconómicos de referencia para la economía española tras el COVID-19. Bol. Econ. Articul. Anal. 2020, 1–35. [Google Scholar]
- Boletín Oficial del Estado (BOE). Real Decreto 463/2020, de 14 de marzo, por el que se declara el estado de alarma para la gestión de la situación de crisis sanitaria ocasionada por el COVID-19. Bol. Of. Estado 2020, 67, 25390–25400. [Google Scholar]
- Litvinova, T. Risks of Entrepreneurship amid the COVID-19 Crisis. Risks 2022, 10, 163. [Google Scholar] [CrossRef]
- Statista. Previsión del Impacto Económico en el PIB Español a Marzo de 2020. Available online: https://es.statista.com/estadisticas/1104098/prevision-del-impacto-economico-del-covid-19-en-el-pib-espanol-a-marzo-de-2020/ (accessed on 12 April 2020).
- Instituto Nacional de Estadística (INE). Crecimiento en Volumen. Available online: https://www.ine.es/prensa/pib_tabla_cne.htm (accessed on 10 February 2021).
- Marchildon, G.; Di Matteo, L. Health Care Cost Drivers: The Facts; CIHI Report: Ottawa, ON, Canada, 2011. [Google Scholar]
- Hernandez-Peña, P.; Poullier, J.P.; Van Mosseveld, C.J.; Van de Maele, N.; Cherilova, V.; Indikadahena, C.; Lie, G.; Tan-Torres, T.; Evans, D.B. Health worker remuneration in WHO Member States. Bull. World Health Organ. 2013, 91, 808–815. [Google Scholar] [CrossRef] [PubMed]
- Instituto Nacional de Estadística (INE). PIB y PIB per Cápita. Serie 2000–2018. Available online: https://www.ine.es/dyngs/INEbase/es/operacion.htm?c=Estadistica_C&cid=1254736167628&menu=resultados&idp=1254735576581#!tabs-1254736158133 (accessed on 14 April 2020).
- Ministerio de Sanidad, Consumo y Bienestar Social. Informe Anual del Sistema Nacional de Salud. 2017. Available online: https://www.mscbs.gob.es/estadEstudios/estadisticas/sisInfSanSNS/tablasEstadisticas/InfAnualSNS2017/8_CAP_17.pdf (accessed on 6 July 2020).
- Fondo Monetario Internacional (IMF). Perspectivas de la Economía Mundial: Desaceleración del Crecimiento, Precaria Recuperación; International Monetary Fund, Publication Services: Washington, DC, USA, 2019; pp. 50–52. [Google Scholar]
- Florido, F.; García-Agua, N.; Reyes, A.M.; García, A.J. Crisis, gasto público sanitario y política. Rev. Esp. Salud Publica 2019, 93, e201902007. [Google Scholar]
- World Health Organization (WHO). Global Health Expenditure Database; World Health Organization: Geneva, Sweden, 2014. [Google Scholar]
- Hitiris, T.; Posnett, J. The determinants and effects of health expenditure in developed countries. J. Health Econ. 1992, 11, 173–181. [Google Scholar] [CrossRef]
- Cometto, G.; Scheffler, R.; Liu, J.; Maeda, A.; Tomblin-Murphy, G.; Hunter, D.; Campbell, J. Health workforce needs, demand and shortages to 2030: An overview of forecasted trends in the global health labour market. In Health Employment and Economic Growth: An Evidence Base; Buchan, D.I., Campbell, J., Eds.; World Health Organization: Geneva, Sweden, 2017. [Google Scholar]
- Van Doorslaer, E.; Wagstaff, A.; Bleichrodt, H.; Calonge, S.; Gerdtham, U.G.; Gerfin, M.; Geurts, J.; Gross, L.; Hakkinen, U.; Leu, R.E.; et al. Income-related inequalities in health: Some international comparisons. J. Health Econ. 1997, 16, 93–112. [Google Scholar] [CrossRef]
- Blanco-Moreno, A.; Urbanos-Garrido, R.M.; Thuissard-Vasallo, I.J. Public healthcare expenditure in Spain: Measuring the impact of driving factors. Health Policy 2013, 111, 34–42. [Google Scholar] [CrossRef]
- Braendle, T.; Colombier, C. What drives public health care expenditure growth? Evidence from Swiss cantons, 1970–2012. Health Policy 2016, 120, 1051–1060. [Google Scholar] [CrossRef]
- Serje, J.; Bertram, M.Y.; Brindley, C.; Lauer, J.A. Global health worker salary estimates: An econometric analysis of global earnings data. Cost Eff. Resour. Alloc. 2018, 16, 10. [Google Scholar] [CrossRef]
- Lauer, J.; Soucat, A.; Araujo, E.; Bertram, M.Y.; Edejer, T.; Brindley, C.; Dale, E.; Tan, A. Paying for needed health workers for the SDGs: An analysis of fiscal and financial space. In Health Employment and Economic Growth: An Evidence Base; Buchan, J., Dillon, I., Campbell, J., Eds.; World Health Organization: Geneva, Sweden, 2017. [Google Scholar]


| N | Minimum | Maximum | Mean | STD Deviation | |
|---|---|---|---|---|---|
| Birth rate | 42 | 7.1000 | 15.2200 | 10.208095 | 1.6857715 |
| Death rate | 42 | 7.5200 | 10.4000 | 8.546905 | 0.5247693 |
| Median age of population | 42 | 26.1900 | 49.7800 | 39.110476 | 3.9757717 |
| Life expectancy at birth | 42 | 75.44 | 83.58 | 79.5607 | 2.58854 |
| Population over 65 | 42 | 11.24 | 20.08 | 15.8090 | 2.57171 |
| Annual population variance | 42 | −0.003713 | 0.019343 | 0.00564207 | 0.005842911 |
| Annual health personnel expenditure variation | 42 | −0.078130 | 0.234810 | 0.07753357 | 0.065311194 |
| Annual public spending variation | 41 | −0.067849 | 0.278202 | 0.07825466 | 0.066680494 |
| Annual health spending variation | 41 | −0.049374 | 0.275106 | 0.08127524 | 0.069073167 |
| Annual GDP variation | 41 | −0.102387 | 0.182401 | 0.05227666 | 0.058309309 |
| % Public spending over GDP | 42 | 0.039600 | 0.080000 | 0.05431667 | 0.010557968 |
| Valid N (by list) | 41 |
| Shapiro–Wilk | |||
|---|---|---|---|
| Statistical | gl | Sig. | |
| Birth rate | 0.967 | 41 | 0.284 |
| Death rate | 0.945 | 41 | 0.048 |
| Median population age | 0.951 | 41 | 0.078 |
| Life expectancy at birth | 0.921 | 41 | 0.007 |
| Population over 65 years old | 0.949 | 41 | 0.066 |
| Annual population variation | 0.846 | 41 | 0.000 |
| Annual health personnel spending variation | 0.983 | 41 | 0.776 |
| Annual public expenditure variation | 0.969 | 41 | 0.328 |
| Annual health expenditure variation | 0.963 | 41 | 0.197 |
| Annual GDP variation | 0.954 | 41 | 0.096 |
| % Public spending over GDP | 0.945 | 41 | 0.045 |
| Model | R | R Squared | Adjusted R2 | Standard Estimation Error | Durbin–Watson |
|---|---|---|---|---|---|
| 1 | 0.731 a | 0.534 | 0.522 | 0.044529030 | |
| 2 | 0.738 b | 0.545 | 0.521 | 0.044564984 | |
| 3 | 0.893 c | 0.797 | 0.781 | 0.030139396 | |
| 4 | 0.897 d | 0.804 | 0.782 | 0.030068912 | |
| 5 | 0.897 e | 0.804 | 0.776 | 0.030489495 | |
| 6 | 0.897 f | 0.804 | 0.770 | 0.030909299 | 2.478 |
| Model | Sum of Squares | df | Mean Square | F | Sig. | |
|---|---|---|---|---|---|---|
| 1 | Regression | 0.089 | 1 | 0.089 | 44.652 | 0.000 a |
| Residual | 0.077 | 39 | 0.002 | |||
| Total | 0.166 | 40 | ||||
| 2 | Regression | 0.090 | 2 | 0.045 | 22.758 | 0.000 b |
| Residual | 0.075 | 38 | 0.002 | |||
| Total | 0.166 | 40 | ||||
| 3 | Regression | 0.132 | 3 | 0.044 | 48.532 | 0.000 c |
| Residual | 0.034 | 37 | 0.001 | |||
| Total | 0.166 | 40 | ||||
| 4 | Regression | 0.133 | 4 | 0.033 | 36.863 | 0.000 d |
| Residual | 0.033 | 36 | 0.001 | |||
| Total | 0.166 | 40 | ||||
| Model | Unstandardized Coefficients | Standardized Coefficients | t | Sig. | Statistics of Collinearity | |||
|---|---|---|---|---|---|---|---|---|
| B | Std. Error. | Beta | Tolerance | FIV | ||||
| 4 | (Constant) | −0.041 | 0.039 | −1.053 | 0.299 | |||
| Annual Public Spending Variation | 0.126 | 0.121 | 0.130 | 1.043 | 0.037 | 0.350 | 2.861 | |
| Birth Rate | 0.005 | 0.004 | 0.114 | 1.120 | 0.027 | 0.526 | 1.902 | |
| Annual Health Spending Variation | 0.645 | 0.098 | 0.692 | 6.563 | 0.000 | 0.490 | 2.040 | |
| Annual GDP Variation | 0.097 | 0.090 | 0.088 | 1.083 | 0.028 | 0.827 | 1.209 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Puerto-Casasnovas, E.; Galiana-Richart, J.; Mastrantonio-Ramos, M.P.; López-Muñoz, F.; Rocafort-Nicolau, A. Determinants of Public Health Personnel Spending in Spain. Int. J. Environ. Res. Public Health 2023, 20, 4024. https://doi.org/10.3390/ijerph20054024
Puerto-Casasnovas E, Galiana-Richart J, Mastrantonio-Ramos MP, López-Muñoz F, Rocafort-Nicolau A. Determinants of Public Health Personnel Spending in Spain. International Journal of Environmental Research and Public Health. 2023; 20(5):4024. https://doi.org/10.3390/ijerph20054024
Chicago/Turabian StylePuerto-Casasnovas, Elena, Jorge Galiana-Richart, Maria Paola Mastrantonio-Ramos, Francisco López-Muñoz, and Alfredo Rocafort-Nicolau. 2023. "Determinants of Public Health Personnel Spending in Spain" International Journal of Environmental Research and Public Health 20, no. 5: 4024. https://doi.org/10.3390/ijerph20054024
APA StylePuerto-Casasnovas, E., Galiana-Richart, J., Mastrantonio-Ramos, M. P., López-Muñoz, F., & Rocafort-Nicolau, A. (2023). Determinants of Public Health Personnel Spending in Spain. International Journal of Environmental Research and Public Health, 20(5), 4024. https://doi.org/10.3390/ijerph20054024







