Assessing the Efficacy of a Virtual Assistant in the Remote Cardiac Rehabilitation of Heart Failure and Ischemic Heart Disease Patients: Case-Control Study of Romanian Adult Patients
Abstract
1. Introduction
1.1. Epidemiology of Cardiovascular Disease and the Current Status of Cardiac Rehabilitation
1.2. Virtual Assistants as an Alternative to Classic Recovery Programs
2. Materials and Methods
2.1. Study Design and Objectives
2.2. Profile of Enrolled Patients
2.3. Ethical Considerations
2.4. Initial Assessment and Structuring of the Virtual Environment
2.5. 3-Month Assessment and Collected Parameters
2.6. Virtual Assistant Components
2.7. Statistical Analysis
3. Results
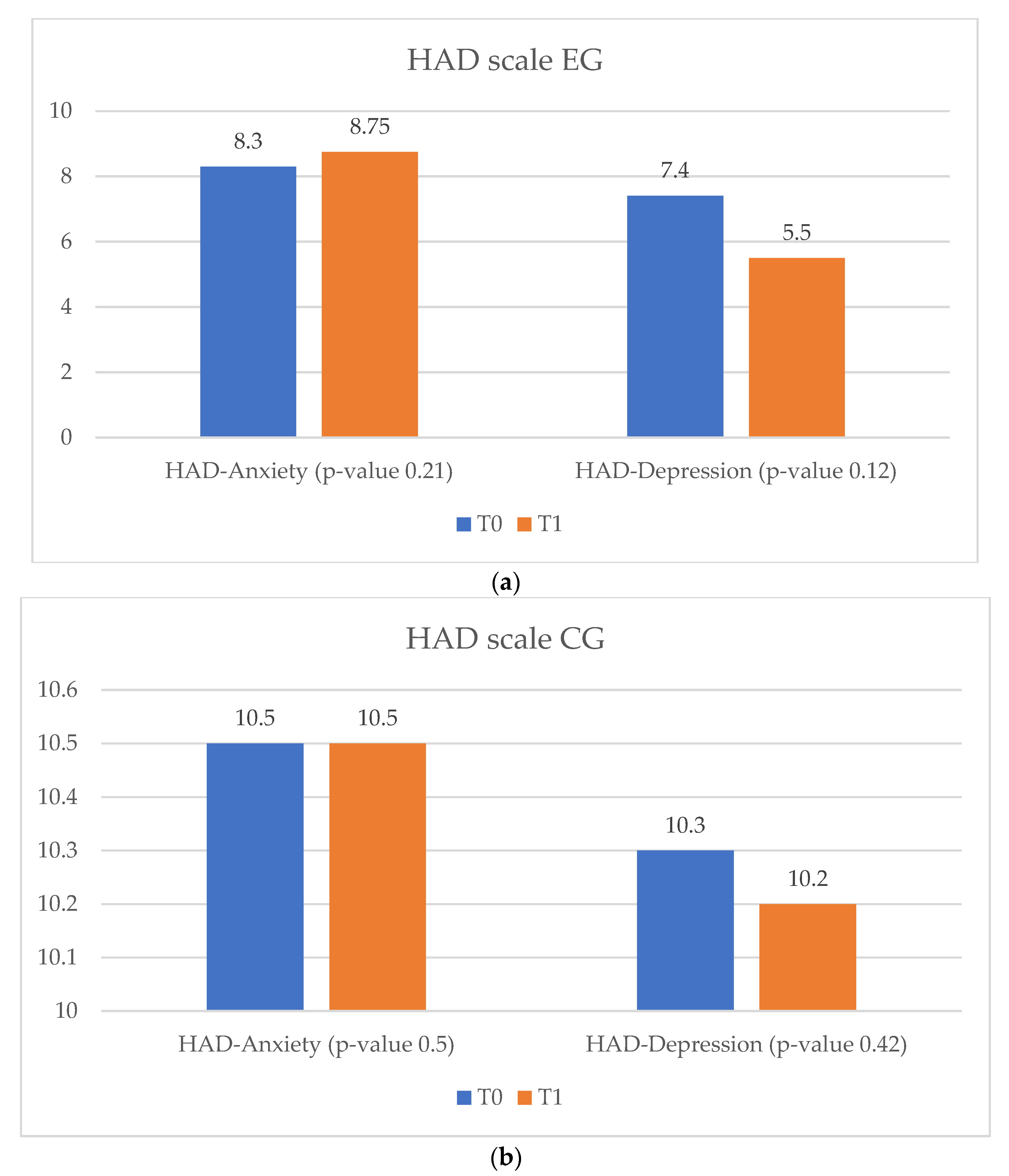
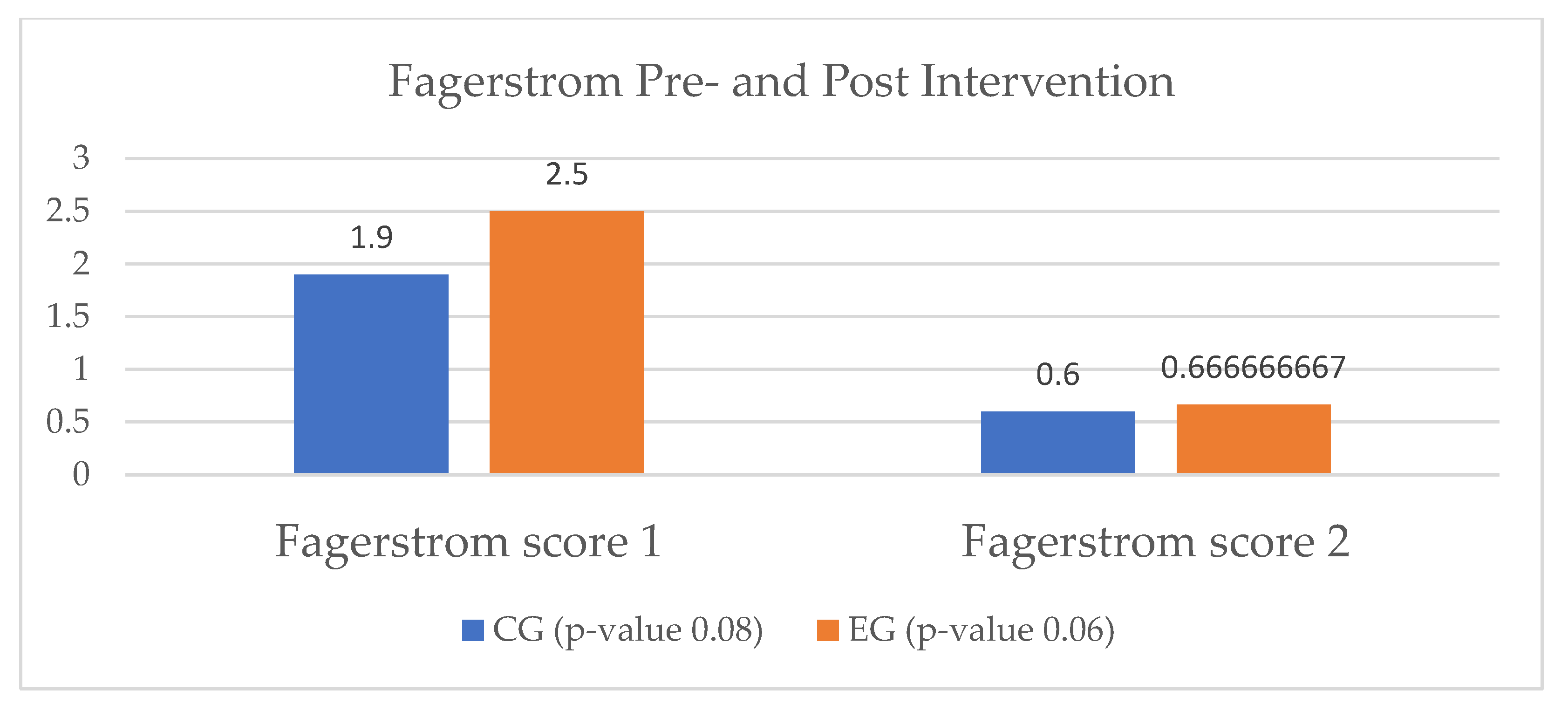
3.1. Heart Failure Participants
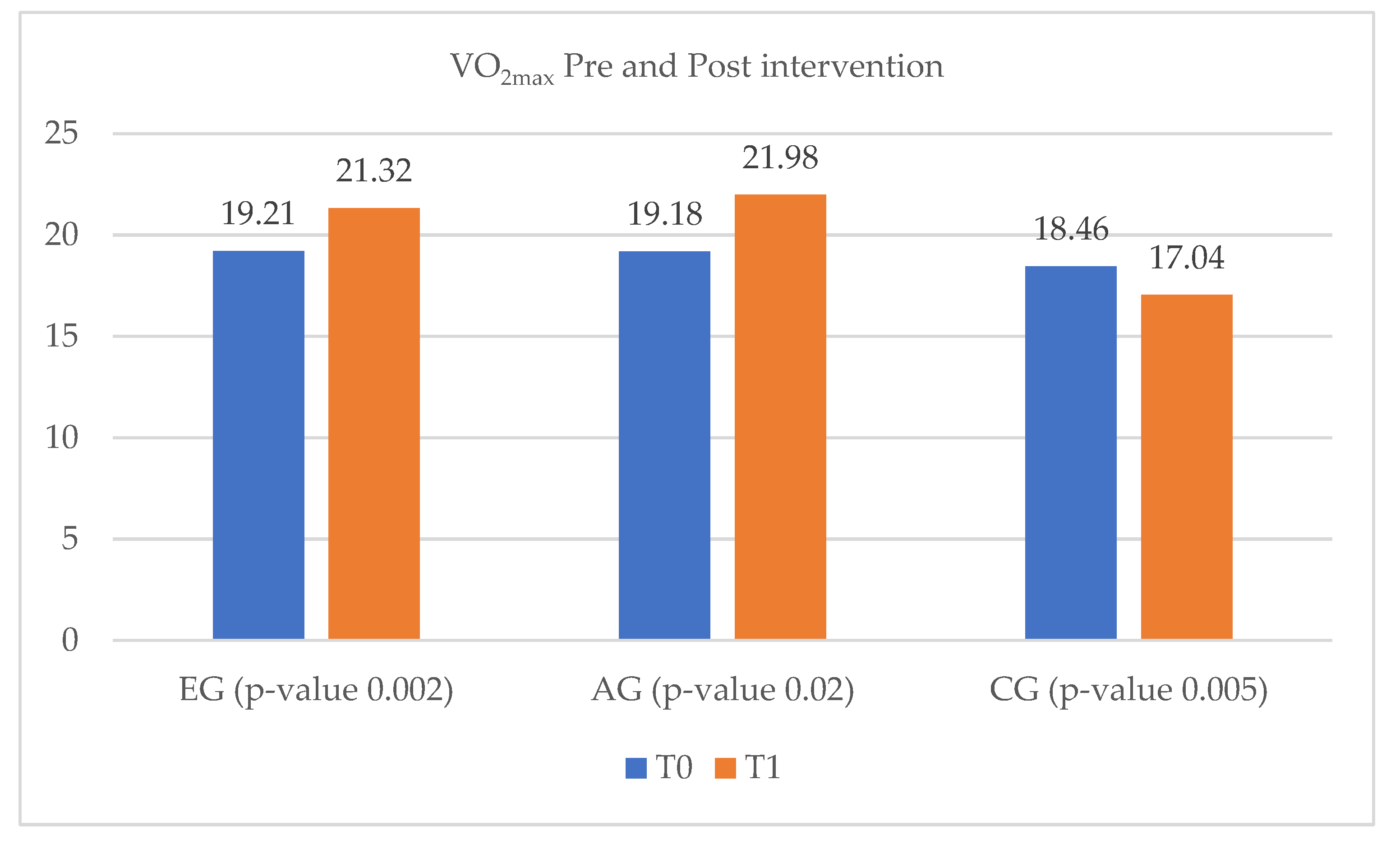
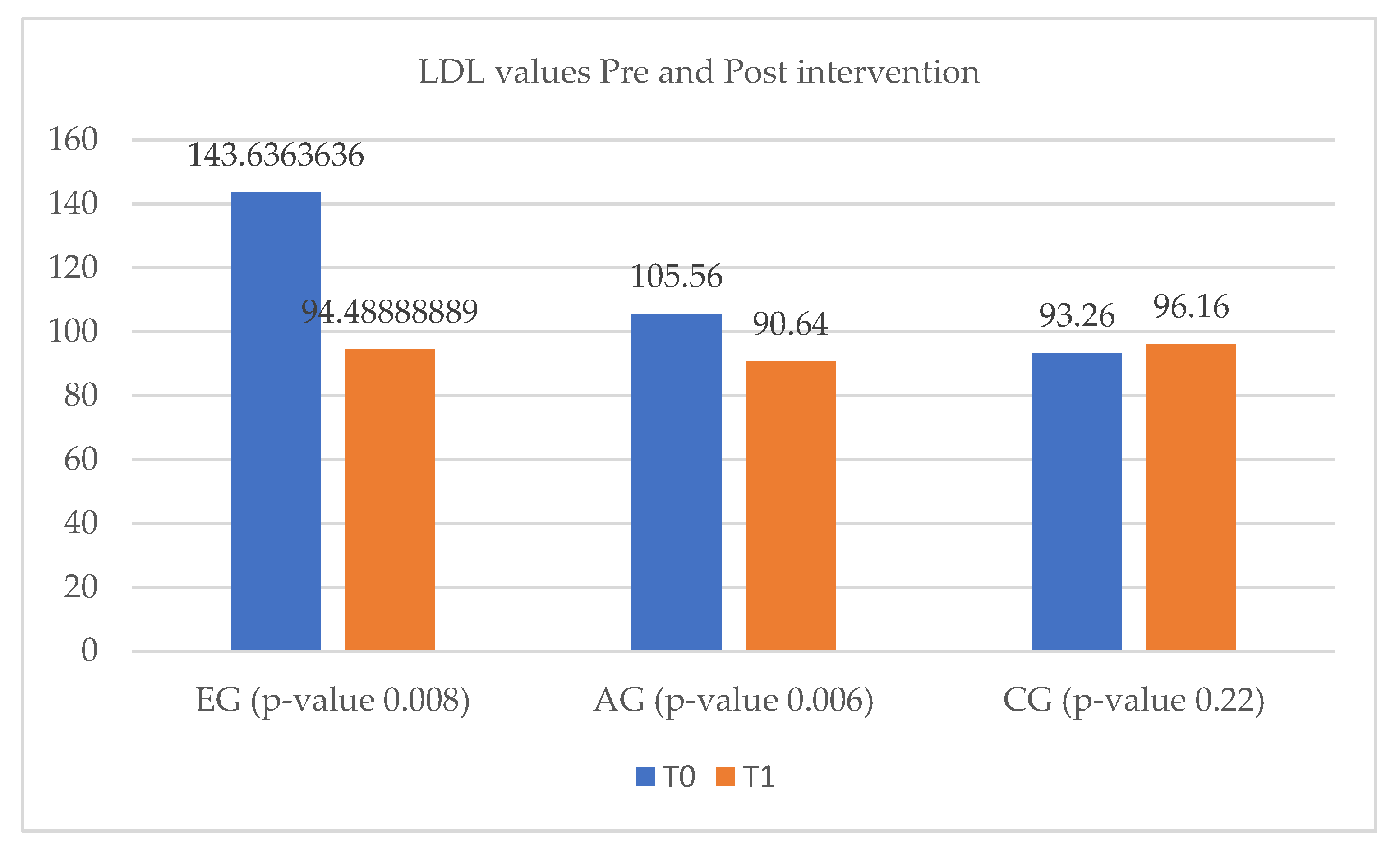
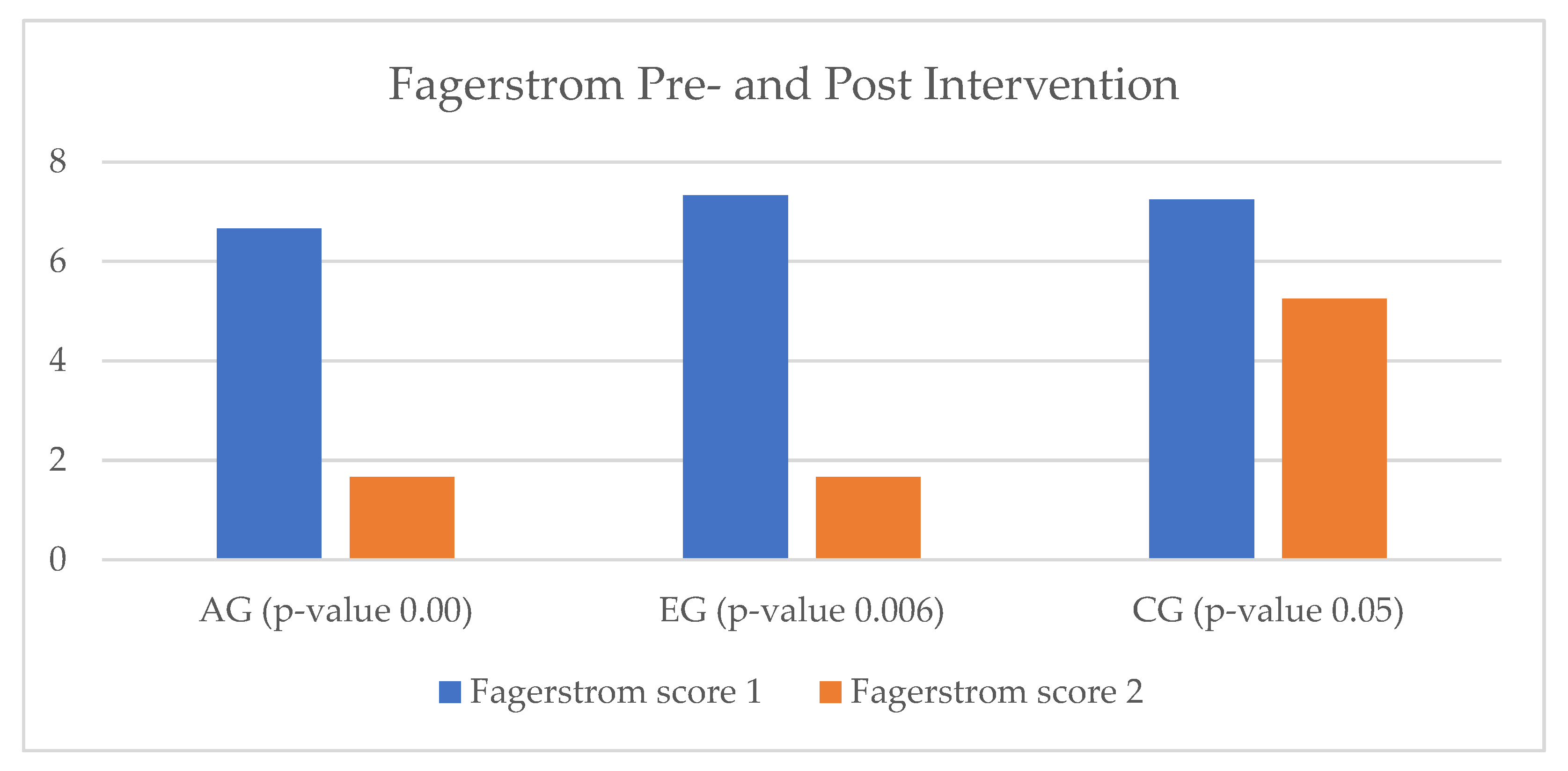
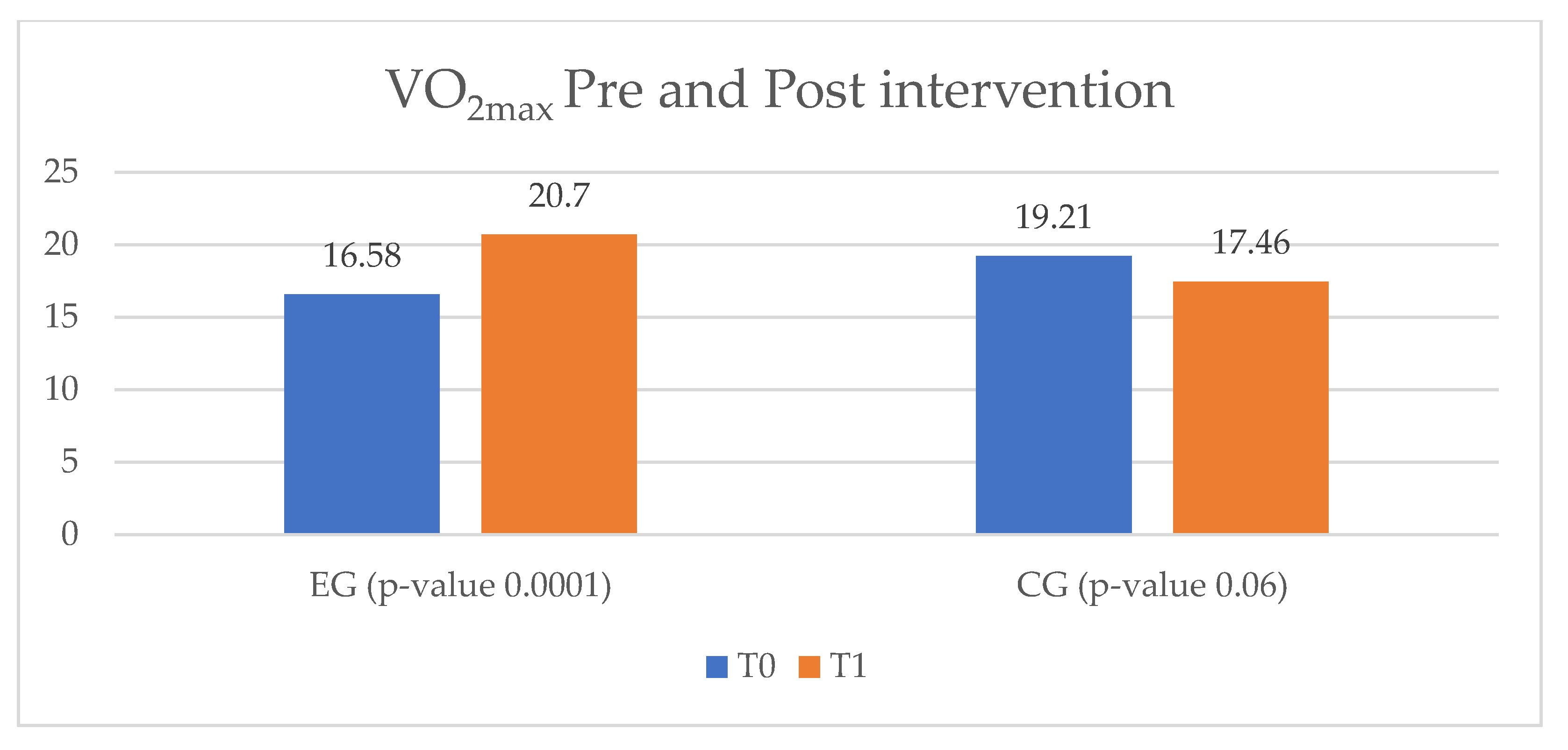
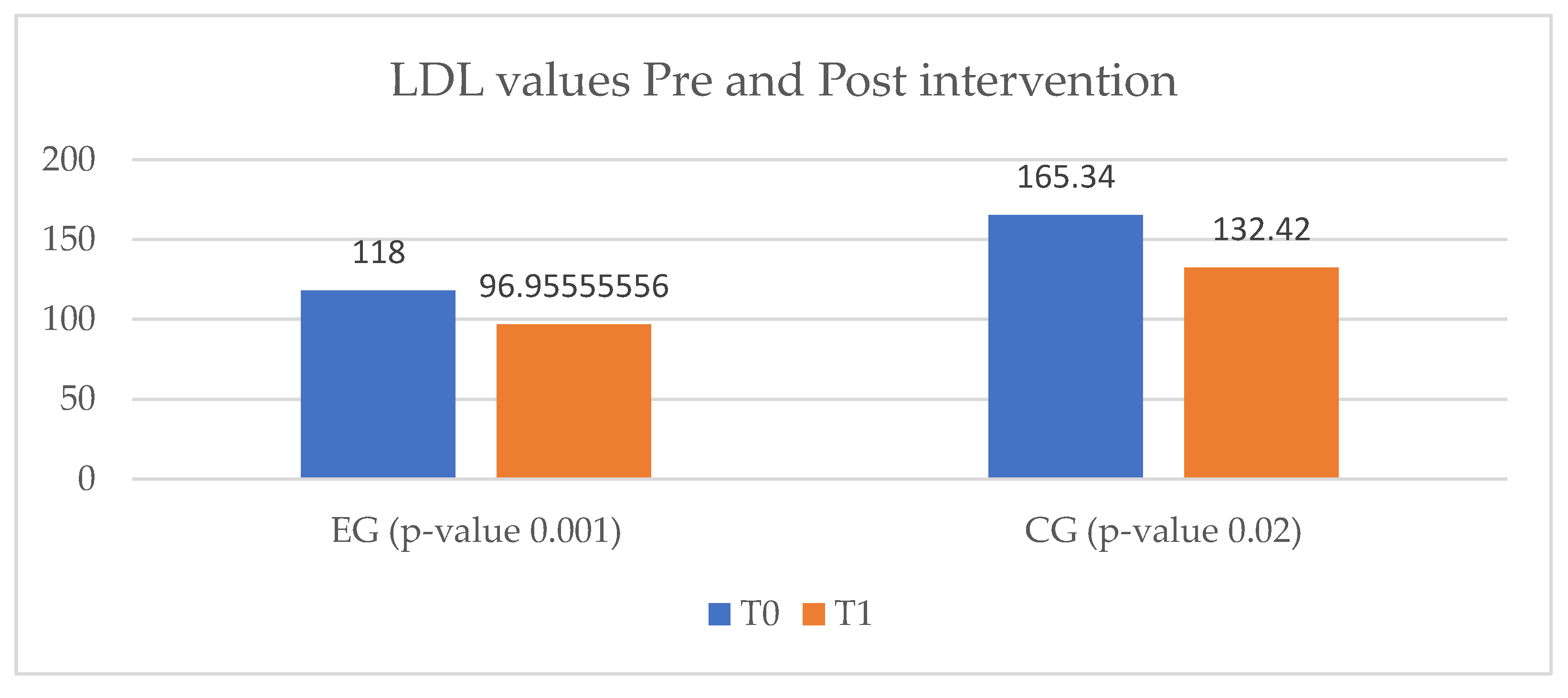
3.2. Ischemic Heart Disease Pilot Results
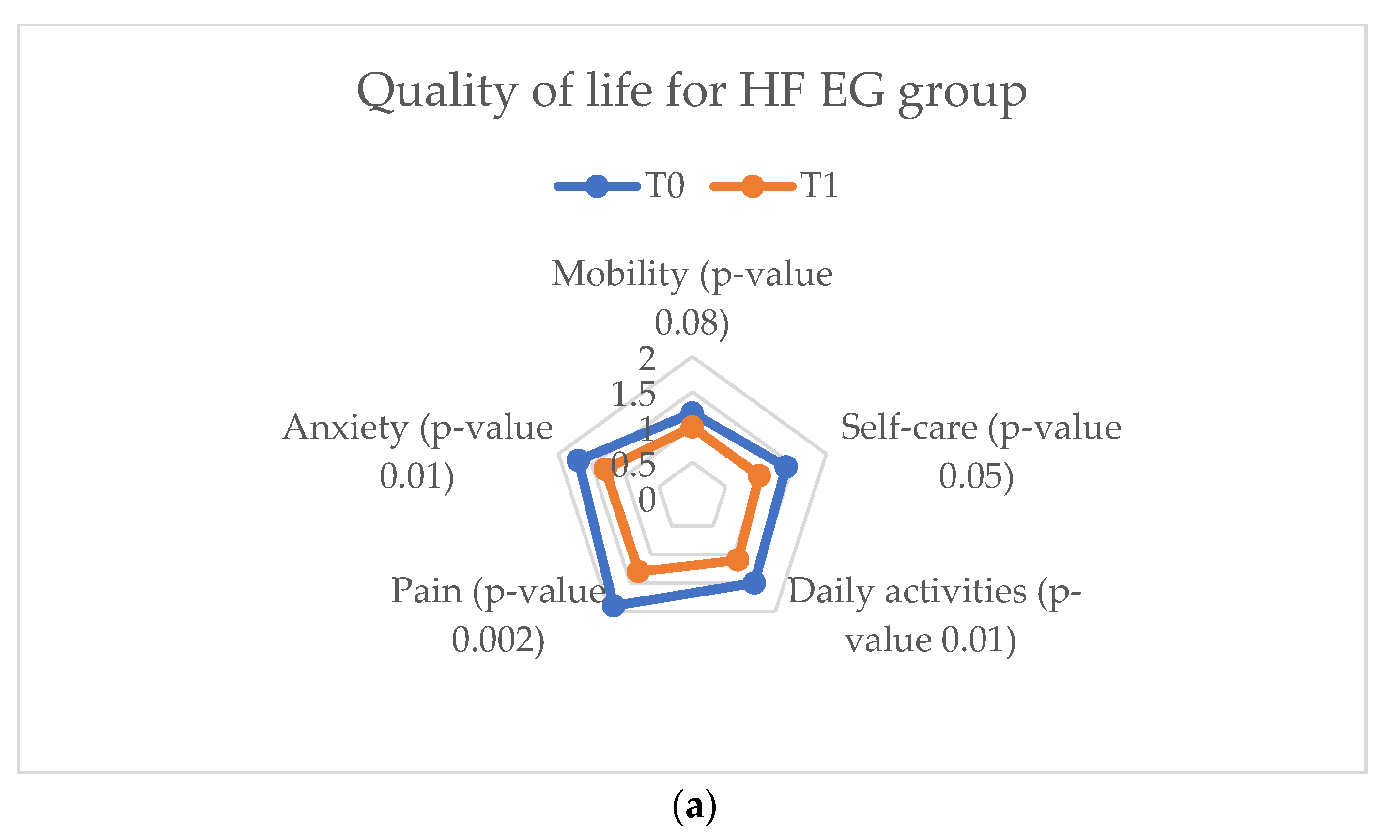
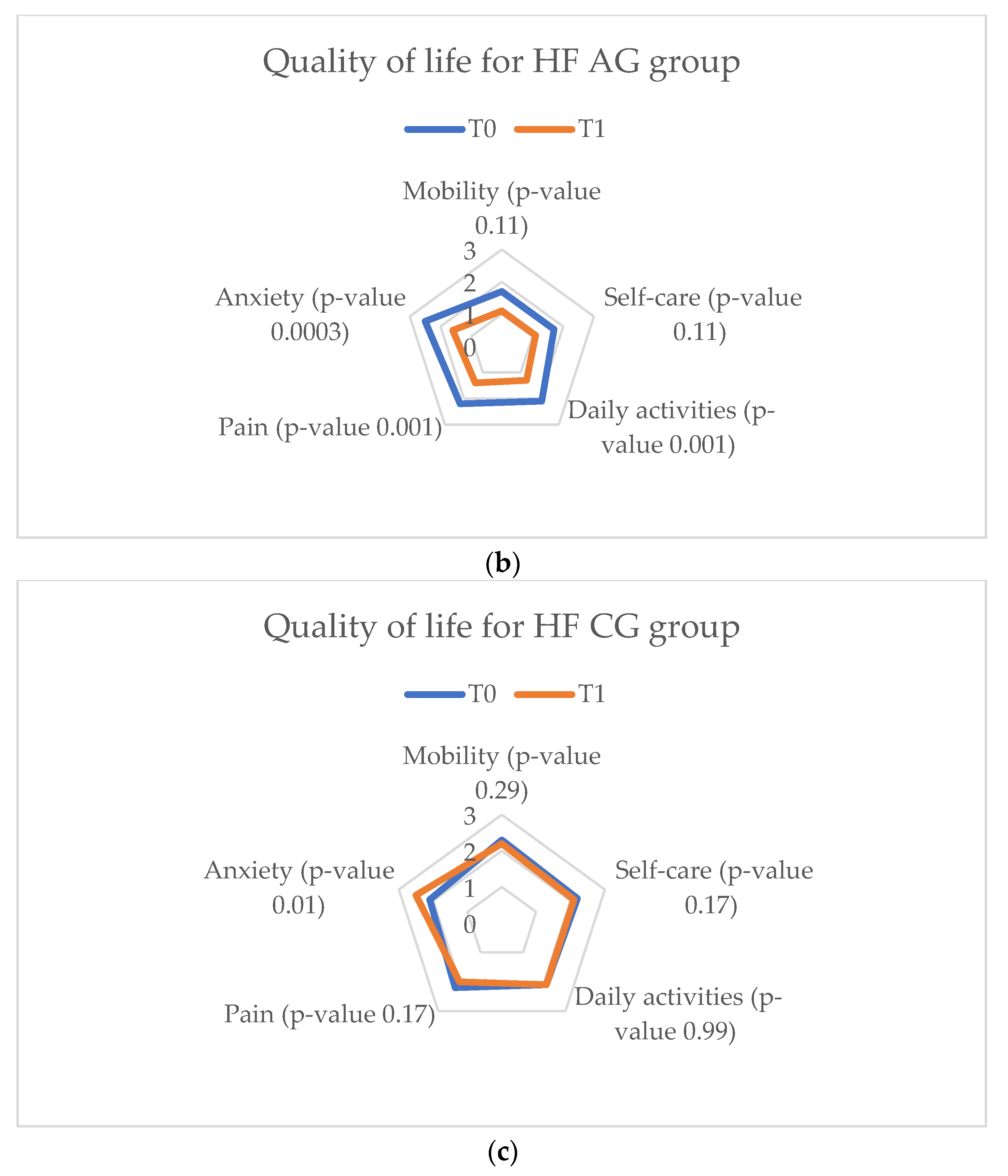
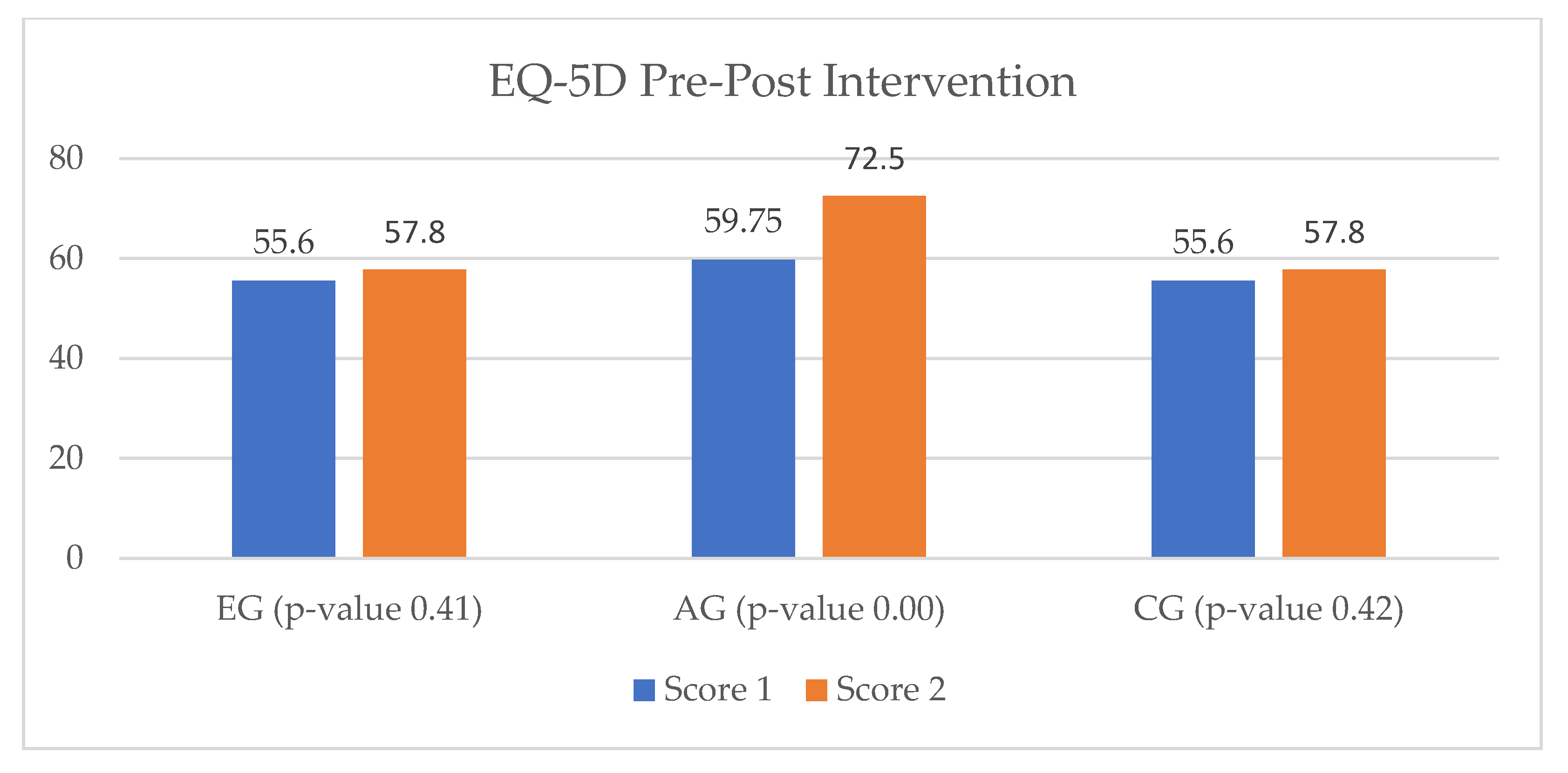
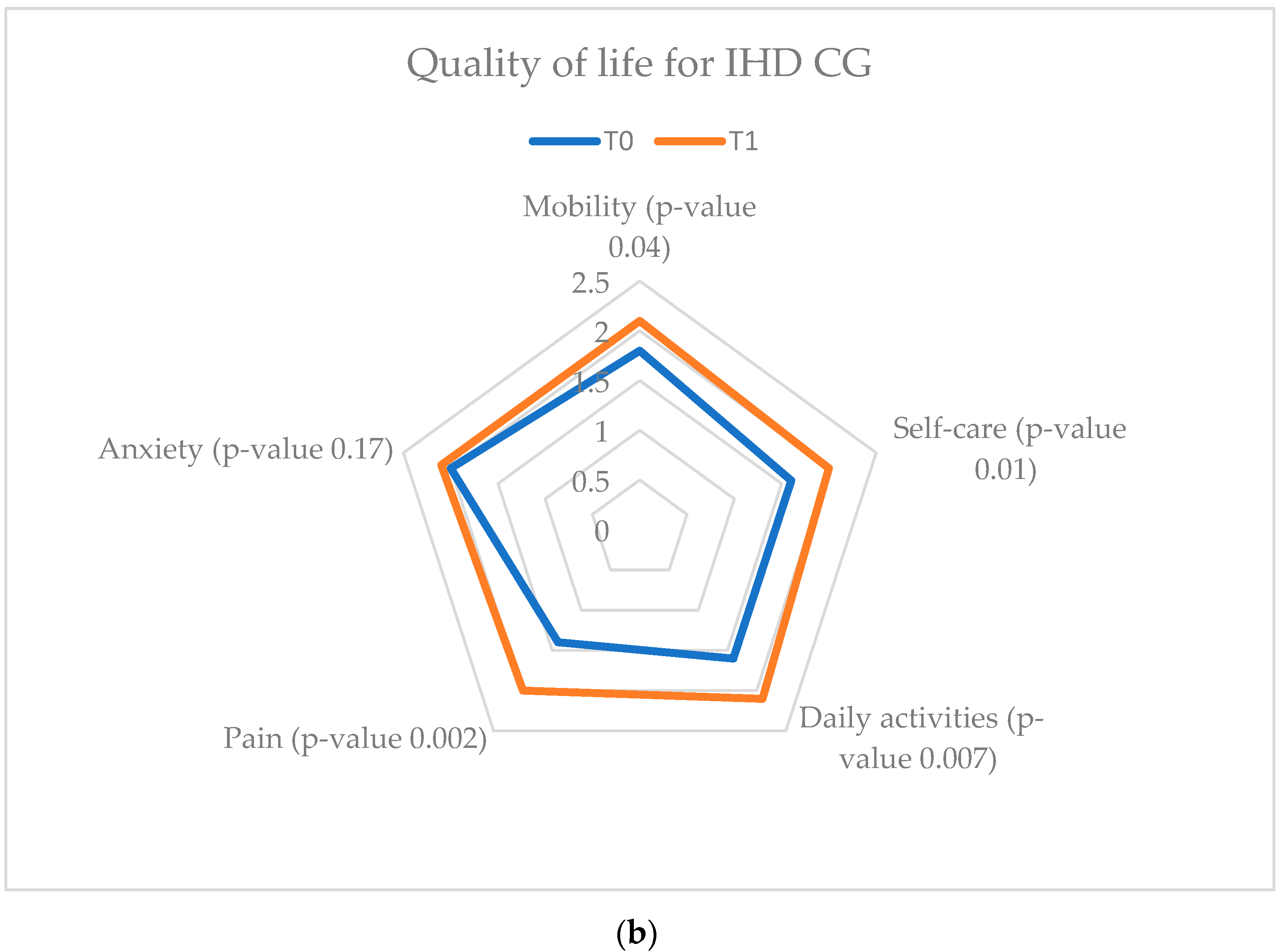
3.3. Quality of Life Assessment
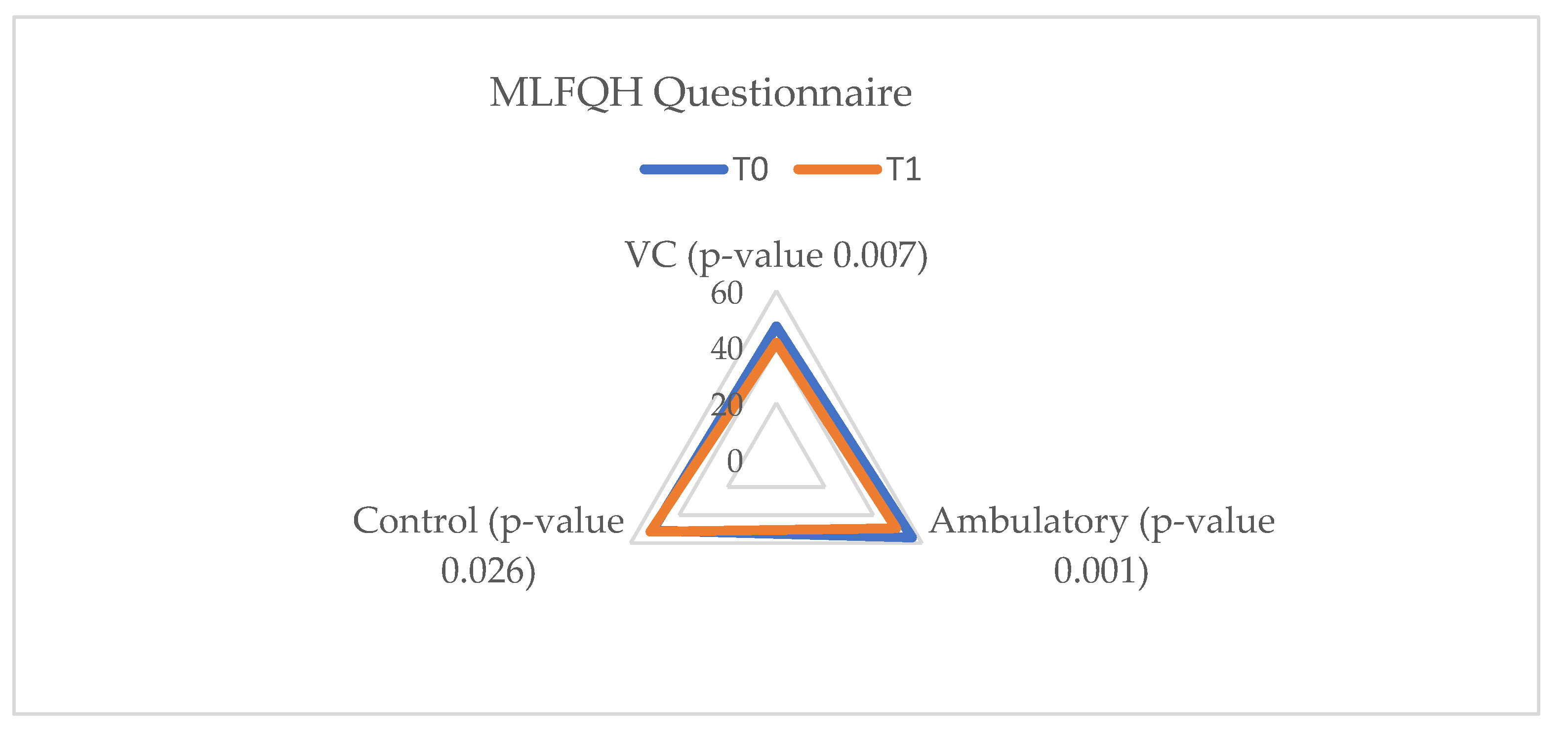
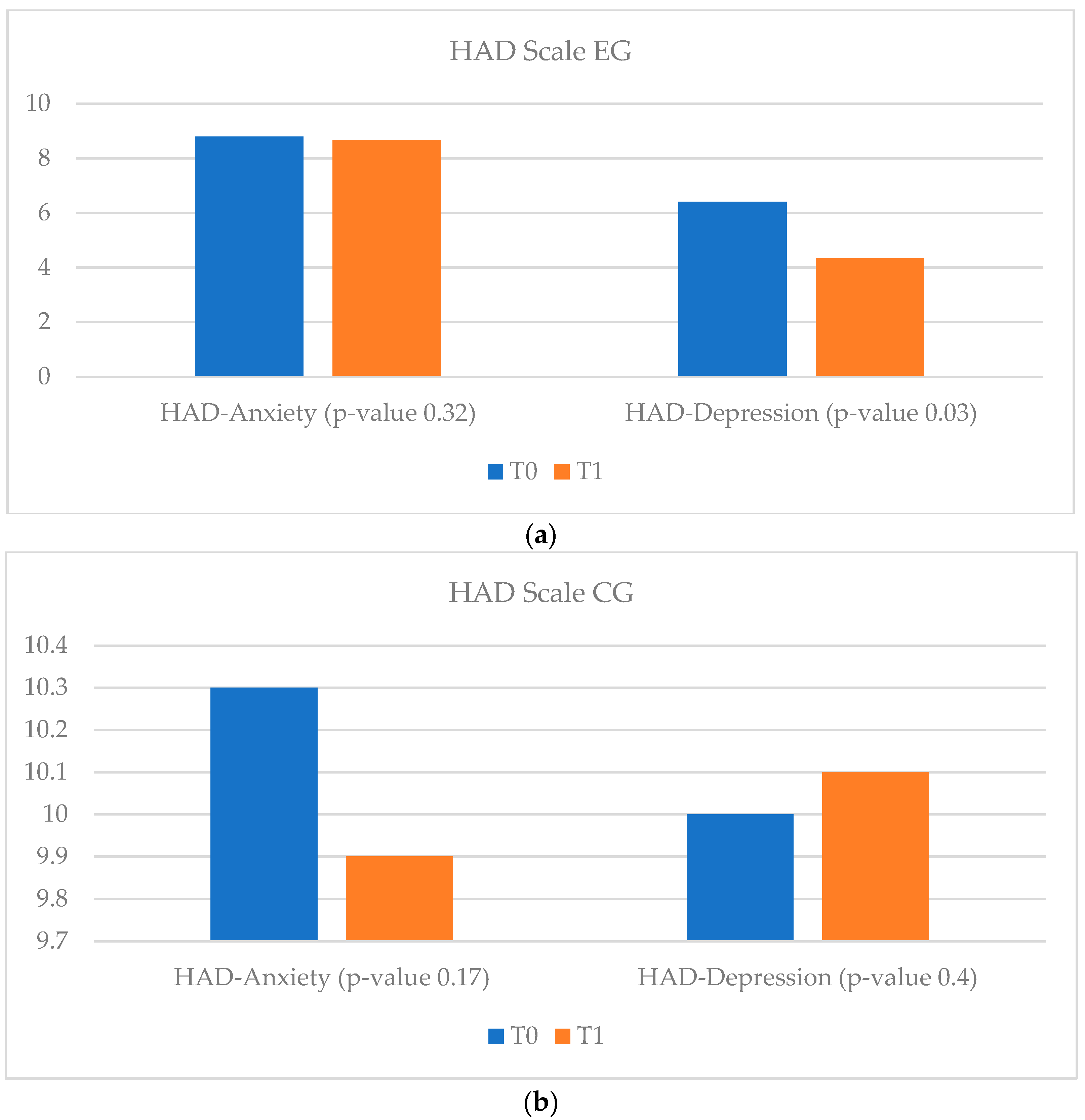
3.3.1. Heart Failure Quality of Life Results
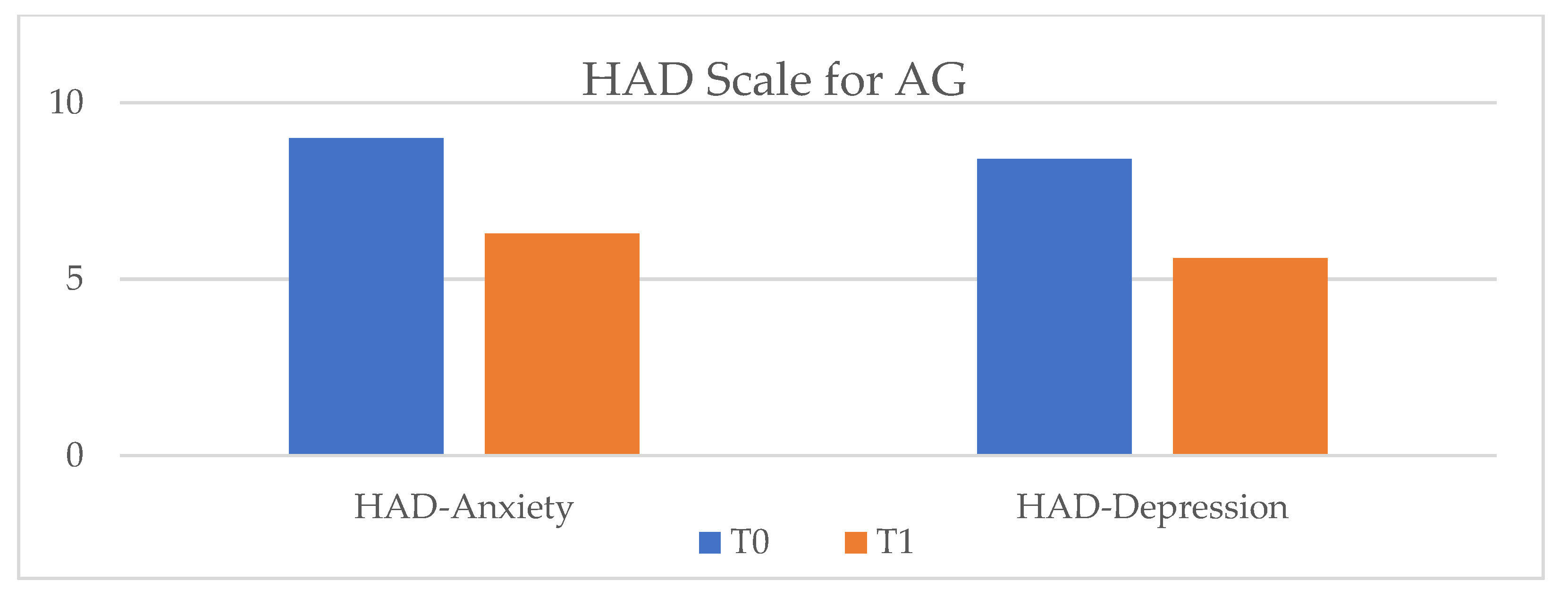
3.3.2. Ischemic Heart Disease Quality of Life Results
3.4. Usefulness of vCare system
4. Discussion
5. Future Perspectives
6. Limitations
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Townsend, N.; Kazakiewicz, D.; Wright, F.L.; Timmis, A.; Huculeci, R.; Torbica, A.; Gale, C.P.; Achenbach, S.; Weidinger, F.; Vardas, P. Epidemiology of cardiovascular disease in Europe. Nat. Rev. Cardiol. 2022, 19, 133–143. [Google Scholar] [CrossRef]
- Roth, G.A.; Abate, D.; Abate, K.H.; Abay, S.M.; Abbafati, C.; Abbasi, N.; Abbastabar, H.; Abd-Allah, F.; Abdela, J.; Abdelalim, A.; et al. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: A systematic analysis for the Global Burden of Disease Study 2017; GBD 2017 Causes of Death Collaborators. Lancet 2018, 392, 1736–1788. [Google Scholar] [CrossRef]
- Timmis, A.; Townsend, N.; Gale, C.; Grobbee, R.; Maniadakis, N.; Flather, M.; Wilkins, E.; Wright, L.; Vos, R.; Bax, J.; et al. European Society of Cardiology: Cardiovascular Disease Statistics 2017. Eur. Heart J. 2018, 39, 508–579. [Google Scholar] [CrossRef]
- Busnatu, S.S.; Pană, M.-A.; Lăcraru, A.E.; Jercălău, C.-E.; Paun, N.; Caprino, M.; Gand, K.; Schlieter, H.; Kyriazakos, S.; Andrei, C.L.; et al. Patient Perception When Transitioning from Classic to Remote Assisted Cardiac Rehabilitation. Diagnostics 2022, 12, 926. [Google Scholar] [CrossRef]
- Visseren, F.L.J.; Mach, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Bäck, M.; Benetos, A.; Biffi, A.; Boavida, J.-M.; Capodanno, D.; et al. ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur. Heart J. 2021, 42, 3227–3337. [Google Scholar] [CrossRef]
- Stefanakis, M.; Batalik, L.; Papathanasiou, J.; Dipla, L.; Antoniou, V.; Pepera, G. Exercise-based cardiac rehabilitation programs in the era of COVID-19: A critical review. Rev. Cardiovasc. Med. 2022, 22, 1143–1155. [Google Scholar] [CrossRef]
- Khera, A.; Baum, S.J.; Gluckman, T.J.; Gulati, M.; Martin, S.S.; Michos, E.D.; Navar, A.M.; Taub, P.R.; Toth, P.P.; Virani, S.S.; et al. Continuity of care and outpatient management for patients with and at high risk for cardiovascular disease during the COVID-19 pandemic: A scientific statement from the American Society for Preventive Cardiology. Am. J. Prev. Cardiol. 2020, 1, 100009. [Google Scholar] [CrossRef]
- Mattioli, A.V.; Puviani, M.B.; Nasi, M.; Farinetti, A. COVID-19 pandemic: The effects of quarantine on cardiovascular risk. Eur. J. Clin. Nutr. 2020, 74, 852–855. [Google Scholar] [CrossRef]
- Doimo, S.; Fabris, E.; Piepoli, M.; Barbati, G.; Antonini-Canterin, F.; Bernardi, G.; Maras, P.; Sinagra, G. Impact of ambulatory cardiac rehabilitation on cardiovascular outcomes: A long-term follow-up study. Eur. Heart J. 2019, 40, 678–685. [Google Scholar] [CrossRef]
- Ibanez, B.; James, S.; Agewall, S.; Antunes, M.J.; Bucciarelli-Ducci, C.; Bueno, H.; Caforio, A.L.P.; Crea, F.; Goudevenos, J.A.; Halvorsen, S.; et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur. Heart J. 2018, 39, 119–177. [Google Scholar] [CrossRef]
- Thomas, R.J.; Beatty, A.; Beckie, T.M.; Brewer, L.C.; Brown, T.M.; Forman, D.E.; Franklin, B.A.; Keteyian, S.J.; Kitzman, D.W.; Regensteiner, J.G.; et al. Home-Based Cardiac Rehabilitation: A Scientific Statement from the American Association of Cardiovascular and Pulmonary Rehabilitation, the American Heart Association, and the American College of Cardiology. Circulation 2019, 140, e69–e89. [Google Scholar] [CrossRef]
- Kim, Y.H.; So, W.-Y. Gender differences in home-based cardiac rehabilitation of post-percutaneous coronary intervention patients. Aging Clin. Exp. Res. 2019, 31, 249–255. [Google Scholar] [CrossRef]
- Afilalo, J. Evaluating and Treating Frailty in Cardiac Rehabilitation. Clin. Geriatr. Med. 2019, 35, 445–457. [Google Scholar] [CrossRef]
- Schopfer, D.; Forman, D.E. Cardiac Rehabilitation in Older Adults. Can. J. Cardiol. 2016, 32, 1088–1096. [Google Scholar] [CrossRef]
- O’Doherty, A.F.; Humphreys, H.; Dawkes, S.; Cowie, A.; Hinton, S.; Brubaker, P.H.; Butler, T.; Nichols, S. How was technology been used to deliver cardiac rehabilitation during the COVID-19 pandemic? An interntional cross-sectional survey of healthcare professionals conducted by the BACPR. BMJ Open 2021, 11, e046051. [Google Scholar] [CrossRef]
- Scherrenberg, M.; Frederix, I.; De Sutter, J.; Dendale, P. Use of cardiac telerehabilitation during COVID-19 pandemic in Belgium. Acta Cardiol. 2021, 76, 773–776. [Google Scholar] [CrossRef]
- Choi, Y.-H.; Paik, N.-J. Mobile Game-based Virtual Reality Program for Upper Extremity Stroke Rehabilitation. J. Vis. Exp. 2018, 133, e56241. [Google Scholar] [CrossRef]
- Laver, K.E.; Lange, B.; George, S.; Deutsch, J.E.; Saposnik, G.; Crotty, M. Virtual reality for stroke rehabilitation. Cochrane Database Syst. Rev. 2017, 2018, CD008349. [Google Scholar] [CrossRef]
- Available online: https://vcare-project.eu/ (accessed on 20 November 2022).
- Bilbao, A.; Escobar, A.; García-Perez, L.; Navarro, G.; Quirós, R. The Minnesota living with heart failure questionnaire: Comparison of different factor structures. Health Qual. Life Outcomes 2016, 14, 23. [Google Scholar] [CrossRef]
- Wu, Y.; Levis, B.; Sun, Y.; He, C.; Krishnan, A.; Neupane, D.; Bhandari, P.M.; Negeri, Z.; Benedetti, A.; Thombs, B.D. Accuracy of the Hospital Anxiety and Depression Scale Depression subscale (HADS-D) to screen for major depression: Systematic review and individual participant data meta-analysis. BMJ 2021, 373, n972. [Google Scholar] [CrossRef]
- Pomerleau, C.S.; Carton, S.M.; Lutzke, M.L.; Flessland, K.A.; Pomerleau, O.F. Reliability of the fagerstrom tolerance questionnaire and the fagerstrom test for nicotine dependence. Addict. Behav. 1994, 19, 33–39. [Google Scholar] [CrossRef]
- Feng, Y.-S.; Kohlmann, T.; Janssen, M.F.; Buchholz, I. Psychometric properties of the EQ-5D-5L: A systematic review of the literature. Qual. Life Res. 2020, 30, 647–673. [Google Scholar] [CrossRef]
- Feng, Y.; Parkin, D.; Devlin, N.J. Assessing the performance of the EQ-VAS in the NHS PROMs programme. Qual. Life Res. 2014, 23, 977–989. [Google Scholar] [CrossRef]
- Rauschenberger, M.; Schrepp, M.; Perez-Cota, M.; Olschner, S.; Thomaschewski, J. Efficient Measurement of the User Experience of Interactive Products. How to use the User Experience Questionnaire (UEQ). Example: Spanish Language Version. Int. J. Interact. Multimedia Artif. Intell. 2013, 2, 39. [Google Scholar] [CrossRef]
- Lewis, J.R. The System Usability Scale: Past, Present, and Future. Int. J. Hum. Comput. Interact. 2018, 34, 577–590. [Google Scholar] [CrossRef]
- Pai, F.-Y.; Huang, K.-I. Applying the Technology Acceptance Model to the introduction of healthcare information systems. Technol. Forecast. Soc. Chang. 2011, 78, 650–660. [Google Scholar] [CrossRef]
- Hansen, D.; Dendale, P.; Coninx, K.; Vanhees, L.; Piepoli, M.F.; Niebauer, J.; Cornelissen, V.; Pedretti, R.; Geurts, E.; Ruiz, G.R.; et al. The European Association of Preventive Cardiology Exercise Prescription in Everyday Practice and Rehabilitative Training (EXPERT) tool: A digital training and decision support system for optimized exercise prescription in cardiovascular disease. Concept, definitions and construction methodology. Eur. J. Prev. Cardiol. 2017, 24, 1017–1031. [Google Scholar] [CrossRef]
- Winnige, P.; Filakova, K.; Hnatiak, J.; Dosbaba, F.; Bocek, O.; Pepera, G.; Papathanasiou, J.; Batalik, L.; Grace, S.L. Validity and Reliability of the Cardiac Rehabilitation Barriers Scale in the Czech Republic (CRBS-CZE): Determination of Key Barriers in East-Central Europe. Int. J. Environ. Res. Public Health 2021, 18, 13113. [Google Scholar] [CrossRef]
- Chen, Y.W.; Wang, C.Y.; Lai, Y.H.; Liao, Y.C.; Wen, Y.K.; Chang, S.T.; Huang, J.L.; Wu, T.J. Home-based cardiac rehabilitation improves quality of life, aerobic capacity, and readmission rates in patients with chronic heart failure. Medicine 2018, 97, e9629. [Google Scholar] [CrossRef]
- Casas, J.; Senft, E.; Gutiérrez, L.F.; Rincón-Rocancio, M.; Múnera, M.; Belpaeme, T.; Cifuentes, C.A. Social Assistive Robots: Assessing the Impact of a Training Assistant Robot in Cardiac Rehabilitation. Int. J. Soc. Robot. 2020, 13, 1189–1203. [Google Scholar] [CrossRef]
- Astley, C.M.; Clarke, R.A.; Cartledge, S.; Beleigoli, A.; Du, H.; Gallagher, C.; Millington, S.; Hendriks, J.M. Remote cardiac rehabilitation services and the digital divide: Implications for elderly populations during the COVID19 pandemic. Eur. J. Cardiovasc. Nurs. 2021, 20, 521–523. [Google Scholar] [CrossRef]
- Robinson, H.; Macdonald, B.; Broadbent, E. The Role of Healthcare Robots for Older People at Home: A Review. Int. J. Soc. Robot. 2014, 6, 575–591. [Google Scholar] [CrossRef]
- Schacksen, C.S.; Henneberg, N.C.; Muthulingam, J.A.; Morimoto, Y.; Sawa, R.; Saitoh, M.; Morisawa, T.; Kagiyama, N.; Takahashi, T.; Kasai, T.; et al. Effects of Telerehabilitation Interventions on Heart Failure Management (2015-2020): Scoping Review. JMIR Rehabil. Assist. Technol. 2021, 8, e29714. [Google Scholar] [CrossRef]
- Owen, O.; O’Carroll, V. The effectiveness of cardiac telerehabilitation in comparison to centre-based cardiac rehabilitation programmes: A literature review. J. Telemed. Telecare 2022. [Google Scholar] [CrossRef]
- Dias, J.F.; Oliveira, V.C.; Borges, P.R.T.; Dutra, F.C.M.S.; Mancini, M.C.; Kirkwood, R.N.; Resende, R.A.; Sampaio, R.F. Effectiveness of exercises by telerehabilitation on pain, physical function and quality of life in people with physical disabilities: A systematic review of randomised controlled trials with GRADE recommendations. Br. J. Sports Med. 2020, 55, 155–162. [Google Scholar] [CrossRef]
- Cordeiro, A.L.L.; Miranda, A.D.S.; de Almeida, H.M.; Santos, P. Quality of Life in Patients with Heart Failure Assisted by Telerehabilitation: A Systematic Review and Meta-Analysis. Int. J. Telerehabilitation 2022, 14, e6456. [Google Scholar] [CrossRef]
- Scherrenberg, M.; Wilhelm, M.; Hansen, D.; Völler, H.; Cornelissen, V.; Frederix, I.; Kemps, H.; Dendale, P. The future is now: A call for action for cardiac telerehabilitation in the COVID-19 pandemic from the secondary prevention and rehabilitation section of the European Association of Preventive Cardiology. Eur. J. Prev. Cardiol. 2021, 28, 524–540. [Google Scholar] [CrossRef]
- Bravo-Escobar, R.; González-Represas, A.; Gómez-González, A.M.; Montiel-Trujillo, A.; Aguilar-Jimenez, R.; Carrasco-Ruíz, R.; Salinas-Sánchez, P. Effectiveness and safety of a home-based cardiac rehabilitation programme of mixed surveillance in patients with ischemic heart disease at moderate cardiovascular risk: A randomised, controlled clinical trial. BMC Cardiovasc. Disord. 2017, 17, 66. [Google Scholar] [CrossRef]
- Spindler, H.; Leerskov, K.; Joensson, K.; Nielsen, G.; Andreasen, J.J.; Dinesen, B. Conventional Rehabilitation Therapy Versus Telerehabilitation in Cardiac Patients: A Comparison of Motivation, Psychological Distress, and Quality of Life. Int. J. Environ. Res. Public Health 2019, 16, 512. [Google Scholar] [CrossRef]


| Inclusion Criteria | Exclusion Criteria |
|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Minnesota Living with Heart Failure | HADS Scale (Anxiety and in-Hospital Depression) | Fagerstrom Test for Nicotine Dependence | EuroQol-5D (EQ5D) | Health Self-Evaluation Scale (EQ-VAS) |
|---|---|---|---|---|
| a self-administered, 21-item disease-specific instrument which assesses the quality of life among patients with heart failure; used only for HF use case [20] | an assessment tool consisting of a 14-item measure designed to assess anxiety and depression symptoms in medical patients, with an emphasis on reducing the impact of physical illness on the total score [21] | a standard assessment tool for the intensity of physical addiction to nicotine; its purpose is to provide an ordinal measure of nicotine dependence related to cigarette smoking [22] | a standard assessment quality of life questionnaire which has five dimensions and a score range from zero (no problems) to four (inability to walk, inability to perform daily activities, extreme pain, or extreme anxiety/depression), or related to their perceived health from zero to one hundred percent, with zero representing the worst possible health and one hundred percent the best possible [23] | a standard self-evaluation scale of a patient’s health, with two endpoints of‚ “The best health you can imagine’’ and‚ “The worst health you can imagine’’; it is used to reflect the patient’s judgement [24] |
| Device | Model |
|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Device | Parameters |
|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| User Experience Questionnaire (UEQ) | System Usability Scale (SUS) | Technology Acceptance Model (TAM) |
|---|---|---|
| was administered to measure classical usability aspects and user experience aspects. It is a questionnaire composed of 26 items built as pairs of contrasting attributes [25] | is a questionnaire that consists of 10 items, with five response options for each item (from “strongly disagree” to “strongly agree”), which allows the subjective evaluation of the usability of the system under examination after the direct interaction of the user with the system [26] | is the most popular model among those proposed to explain and predict the acceptance of a system [27] |
| E-learning | Aerobic Physical Activity | Resistance Training | Medication Intake Support | Vital Stats Control | Smoking Cessation Activity | Anxiety and Depression Reduction | Alcohol Reduction |
|---|---|---|---|---|---|---|---|
| Medical education | Daily number of steps | Strengh training with serious games | Interaction confirming the administration of pharmacological therapy | Vital parameters monitoring | Assessment of the number of cigarettes consumed | Assessment of anxiety and depression status | Assessment of the amount of alcohol consumed |
| Active Days | Adherence | Average Steps per Active Days | Active Weeks | Adherence | Average Accesses per Active Weeks | |
|---|---|---|---|---|---|---|
| Patient1 | 3 | 8% | 211 | 4 | 72% | 3 |
| Patient2 | 7 | 30% | 1467 | 3 | 91% | 2 |
| Patient4 | 22 | 25% | 8632 | 10 | 79% | 6 |
| Patient5 | 1 | 2% | 704 | 2 | 32% | 5 |
| Patient6 | 7 | 6% | 5251 | 13 | 80% | 5 |
| Patient7 | 3 | 4% | 524 | 3 | 31% | 2 |
| Patient8 | 3 | 10% | 474 | 4 | 93% | 3 |
| Patient9 | 35 | 38% | 2545 | 14 | 93% | 10 |
| Patient10 | 20 | 23% | 7863 | 13 | 80% | 5 |
| mean | 10.1 | 16% | 2476 | 6.6 | 71% | 4 |
| std | 12 | 0.1 | 2993 | 4.9 | 0.2 | 3 |
| Active Days | Adherence | Average Steps per Active Days | Active Weeks | Adherence | Average Accesses per Active Weeks | |
|---|---|---|---|---|---|---|
| Patient1 | 1 | 4% | 514 | 3 | 84% | 5 |
| Patient2 | 3 | 13% | 3574 | 3 | 84% | 5 |
| Patient4 | 3 | 6% | 1093 | 4 | 31% | 2 |
| Patient5 | 83 | 91% | 4208 | 15 | 100% | 13 |
| Patient6 | 31 | 34% | 4049 | 11 | 85% | 2 |
| Patient7 | 9 | 22% | 1451 | 6 | 100% | 5 |
| Patient8 | 30 | 33% | 4860 | 5 | 73% | 9 |
| Patient9 | 12 | 27% | 3000 | 3 | 82% | 7 |
| Patient10 | 21 | 30% | 3930 | 4 | 40% | 4 |
| mean | 19.3 | 26% | 2668 | 6.7 | 67.9% | 5.2 |
| std | 29.9 | 0.3 | 1579 | 4.6 | 0.2 | 4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lăcraru, A.-E.; Busnatu, Ș.-S.; Pană, M.-A.; Olteanu, G.; Șerbănoiu, L.; Gand, K.; Schlieter, H.; Kyriazakos, S.; Ceban, O.; Andrei, C.L.; et al. Assessing the Efficacy of a Virtual Assistant in the Remote Cardiac Rehabilitation of Heart Failure and Ischemic Heart Disease Patients: Case-Control Study of Romanian Adult Patients. Int. J. Environ. Res. Public Health 2023, 20, 3937. https://doi.org/10.3390/ijerph20053937
Lăcraru A-E, Busnatu Ș-S, Pană M-A, Olteanu G, Șerbănoiu L, Gand K, Schlieter H, Kyriazakos S, Ceban O, Andrei CL, et al. Assessing the Efficacy of a Virtual Assistant in the Remote Cardiac Rehabilitation of Heart Failure and Ischemic Heart Disease Patients: Case-Control Study of Romanian Adult Patients. International Journal of Environmental Research and Public Health. 2023; 20(5):3937. https://doi.org/10.3390/ijerph20053937
Chicago/Turabian StyleLăcraru, Andreea-Elena, Ștefan-Sebastian Busnatu, Maria-Alexandra Pană, Gabriel Olteanu, Liviu Șerbănoiu, Kai Gand, Hannes Schlieter, Sofoklis Kyriazakos, Octavian Ceban, Cătălina Liliana Andrei, and et al. 2023. "Assessing the Efficacy of a Virtual Assistant in the Remote Cardiac Rehabilitation of Heart Failure and Ischemic Heart Disease Patients: Case-Control Study of Romanian Adult Patients" International Journal of Environmental Research and Public Health 20, no. 5: 3937. https://doi.org/10.3390/ijerph20053937
APA StyleLăcraru, A.-E., Busnatu, Ș.-S., Pană, M.-A., Olteanu, G., Șerbănoiu, L., Gand, K., Schlieter, H., Kyriazakos, S., Ceban, O., Andrei, C. L., & Sinescu, C.-J. (2023). Assessing the Efficacy of a Virtual Assistant in the Remote Cardiac Rehabilitation of Heart Failure and Ischemic Heart Disease Patients: Case-Control Study of Romanian Adult Patients. International Journal of Environmental Research and Public Health, 20(5), 3937. https://doi.org/10.3390/ijerph20053937









