Improving the Management of Children with Fevers by Healers in Native Rural Areas in the South of Ecuador
Abstract
1. Introduction
2. Methods
2.1. Ethical Approval
2.2. Phase 1: Observation
2.2.1. Purposive Sampling Was Used to Recruit the Participants
2.2.2. Procedure
2.3. Phase 2: Planning (Creation of a Plan)
2.4. Phase 3: Action Plan
2.5. Phase 4: Evaluation
3. Results
3.1. Phase 1: Observation
3.1.1. Main Themes
Caring for Children with Fever in Indigenous Communities
“Well, I believe that first (……) the research is done with the mother of the family, from the moment the child has a fever; it’s already 5 days he’s got a fever, what medication or to where she has gone to cure the child, already (….), from the moment the child doesn’t go out or is not active inside the house”(Q1-FG4)
“Suddenly the kid got wet being hot or suddenly he was asleep and woke up and like we say, the air caught him. The air catches him? He gets the air what we call he gets the air or the bad air, the cold; that the cold or the fright……..I clean him and give him some waters”(Q2-FG4)
“I heal with my hands, my hands heal….. I touch the child and see if he’s hot…..I’ve seen they use those thermometers….I cannot see there, I touch the child I feel the head, the belly, the little back.”(Q3-FG2)
“First we apply traditional medicine or ancestral medicine, we give fresh waters; for example mauve, begonia or chamomile waters, we perform a “bajeado” as we call it; the water boils, we place the flowers there, we put the lid on, the fragrance concentrates and you give it with a little bicarbonate.”(Q4-F2)
Alarm Signs in Children with Fever
“What I do is to see if the lips and the tongue are dry because they tell me he is dehydrated, but I also see if the child is run-down sad…”(Q5-FG3)
“You watch the eyes, the tongue; the eyes fall down like small drops inside already, they become pale too, (…..) well let’s say the face is pale like hollow-cheeked and the mouth is totally dry and the tongue too; when this happens it means that the child has an infection or something that is really severe, because if the child is still fine he’s got energy.”(Q6-F5)
Patient Follow-Up
“You buy a little creole chicken egg, better if from the same day just laid…we make crosses with the egg….It’s like I say, it’s a ritual first asking the power from God, who is the one who has given us life first and the earth which is the part of the little animals that we use their live part, because the egg is a live part and that adsorbs gives its life so that that person really takes that life and alleviate.”(Q7-FG7)
“I believe that he’s not going to come very soon so I have to follow him up closely and I have to go to the house all the same as they said to see how the house is if it’s clean how they eat sometimes.”(Q8-FG2)
“For the child to heal the parents must be fine, ……there doesn’t have to be problems with the neighbor…..it’s a balance of the four bodies physical, emotional, spiritual, and mental of the patient, and it involves both the patient and the family environment.”(Q9-FG3)
Referral to the Health System
“I once went to the hospital with a child and they didn’t let me in, they turned me out, that I know nothing, that I should see how the child is and I told them it is a severe infection.”(Q10-FG4)
“Children with high fever start with convulsions then you do have to send them to a health post for them to help because it’s a very dangerous case if the child’s fever doesn’t go down quickly you already have to send him there.”(Q11-FG7)
3.2. Phase 2: Planning (Creation of a Plan)
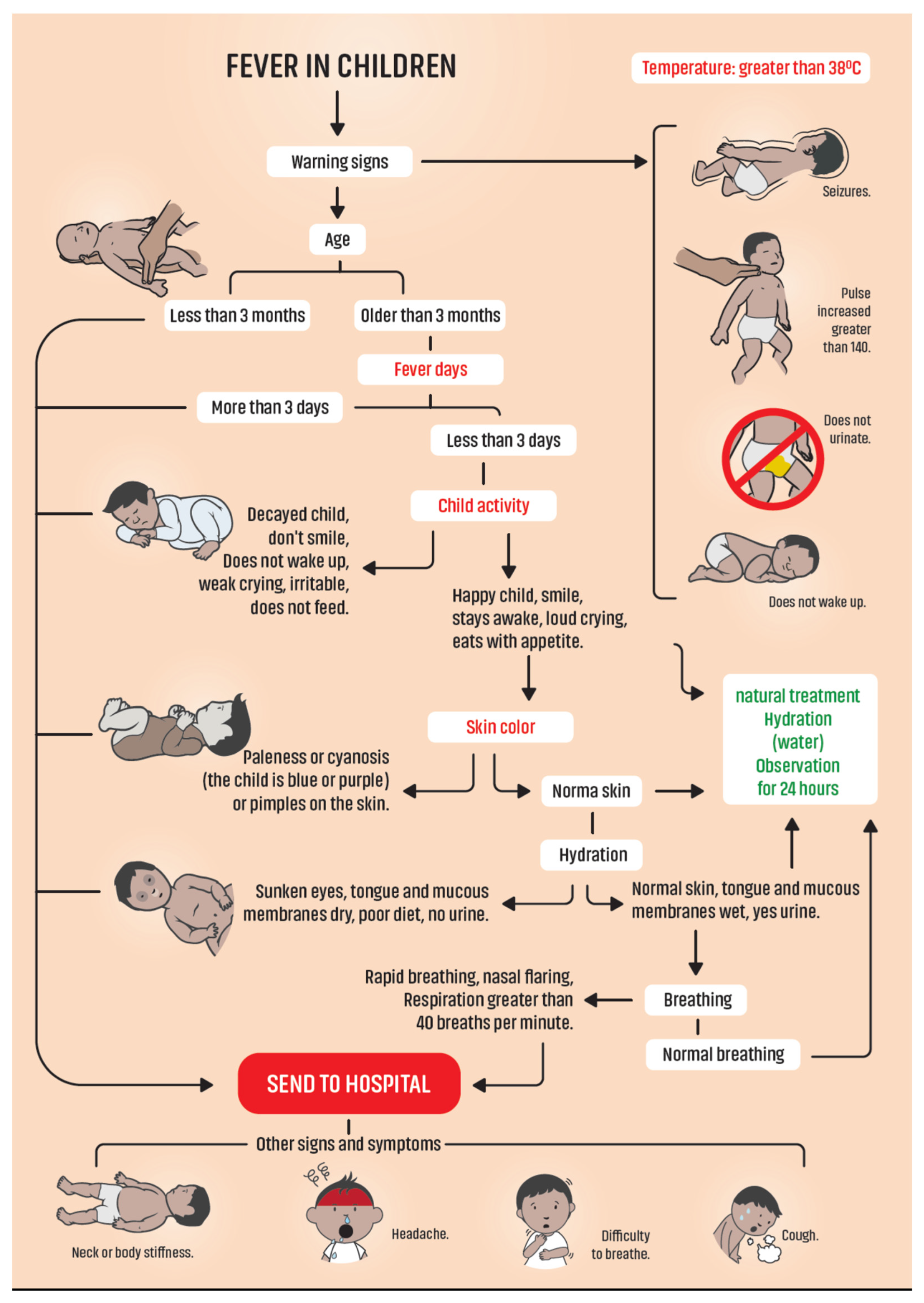
Design of Flowchart in Management of Children with Fever
3.3. Phase 3: Action Plan
- The use of a thermometer and its interpretation;
- Recognition of alarm signs and patient management (steps from the flowchart);
- Patient referral system.
3.4. Phase 4: Evaluation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- United Nations Millennium Development Goals. Available online: https://www.un.org/millenniumgoals/childhealth.shtml (accessed on 25 May 2021).
- García Chong, N.R.; Salvatierra Izaba, B.; Trujillo Olivera, L.E.; Zúñiga Cabrera, M. Mortalidad Infantil, pobreza y marginación en indígenas de los altos de Chiapas, México. Ra Ximhai 2010, 6, 115–130. [Google Scholar] [CrossRef]
- Castro, F.; Benavides Lara, A.; Garcés, A.; Moreno-Velásquez, I.; Odell, C.; Pérez, W.; Ortiz-Panozo, E. Under-5 Mortality in Central America: 1990–2016. Pediatrics 2021, 147, e2020003442. [Google Scholar] [CrossRef]
- Romero-Sandoval, N.; Del Alcázar, D.; Pastor, J.; Martín, M. Ecuadorian infant mortality linked to socioeconomic factors during the last 30 years. Rev. Bras. Saúde Matern. Infant. 2019, 19, 295–301. [Google Scholar] [CrossRef]
- Gracey, M.; King, M. Indigenous health part 1: Determinants and disease patterns. Lancet 2009, 374, 65–75. [Google Scholar] [CrossRef]
- Australian Human Rights Commission. Social determinants and the Health of Indigenous Peoples in Australia—A Human Rights Based Approach. 2007. Available online: http://www.who.int/social_determinants/resources/indigenous_health_adelaide_report_07.pdf (accessed on 16 May 2021).
- Caria, S.; Domínguez, R. Ecuador’s buen vivir: A new ideology for development. Lat. Am. Perspect. 2016, 43, 18–33. [Google Scholar] [CrossRef]
- Hoff, W. Traditional healers and comunnity health. World Health Forum 1992, 13, 182–187. [Google Scholar]
- Makundi, E.A.; Malebo, H.M.; Mhame, P.; Kitua, A.Y.; Warsame, M. Role of traditional healers in the management of severe malaria among children below five years of age: The case of Kilosa and Handeni Districts, Tanzania. Malar J. 2006, 5, 58. [Google Scholar] [CrossRef]
- Okeke, T.A.; Okafor, H.U.; Uzochukwu, B.S. Traditional healers in Nigeria: Perception of cause, treatment and referral practices for severe malaria. J. Biosoc. Sci. 2006, 38, 491–500. [Google Scholar] [CrossRef]
- Gallaher, J.R.; Purcell, L.N.; Banda, W.; Charles, A. The effect of traditional healer intervention prior to allopathic care on pediatric burn mortality in Malawi. Burns 2020, 46, 1952–1957. [Google Scholar] [CrossRef]
- Hooft, A.; Nabukalu, D.; Mwanga-Amumpaire, J.; Gardiner, M.A.; Sundararajan, R. Factors Motivating Traditional Healer versus Biomedical Facility Use for Treatment of Pediatric Febrile Illness: Results from a Qualitative Study in Southwestern Uganda. Am. J. Trop. Med. Hyg. 2020, 103, 501–507. [Google Scholar] [CrossRef]
- Bautista-Valarezo, E.; Duque, V.; Verhoeven, V.; Mejia Chicaiza, J.; Hendrickx, K.; Maldonado-Rengel, R.; Michels, N.R. Perceptions of Ecuadorian indigenous healers on their relationship with the formal health care system: Barriers and opportunities. BMC Complement. Med. Ther. 2021, 21, 65. [Google Scholar] [CrossRef]
- Asamblea Nacional Constituyente. Constitucion Politica de la Republica del Ecuador|Enhanced Reader. Available online: Moz-extension://85d2f2ea-fb72-2246-98be-e376433b0fd7/enhanced-reader.html?openApp&pdf=https%3A%2F%2Fwww.oas.org%2Fjuridico%2Fspanish%2Fmesicic2_ecu_anexo15.pdf (accessed on 26 August 2022).
- Bautista-Valarezo, E.; Vangehuchten, L.; Duque, V. Intercultural health care in Ecuador: An investigation project for the medicine and nursing careers. MediSan 2017, 21, 3111–3122. [Google Scholar]
- Bautista-Valarezo, E.; Duque, V.; Verdugo Sánchez, A.E.; Dávalos-Batallas, V.; Michels, N.R.M.; Hendrickx, K.; Verhoeven, V. Towards an indigenous definition of health: An explorative study to understand the indigenous Ecuadorian people’s health and illness concepts. Int. J. Equity Health 2020, 19, 101. [Google Scholar] [CrossRef]
- Hart, F.; Bond, M. Action Research for Health and Social Care: A Guide to Practice; McGraw-Hill Education: London, UK, 1995. [Google Scholar]
- Zuber-Skerritt, O. Action learning and action research: Paradigm, praxis and programs. In Effective Change Management through Action Research and Action Learning: Concepts, Perspectives, Processes and Applications; Southern Cross University Press: Lismore, Australia, 2001; Volume 1, p. 20. [Google Scholar]
- McNiff, J. Writing Up Your Action Research Project; Taylor & Francis Group: London, UK, 2015. [Google Scholar]
- Walter, M. Participatory Action Research. Social Research Methods; Oxford University Press: Melbourne, Australia, 2009. [Google Scholar]
- Fine, M.; Torre, M.E.; Oswald, A.G.; Avory, S. Critical participatory action research: Methods and praxis for intersectional knowledge production. J. Couns. Psychol. 2021, 68, 344–356. [Google Scholar] [CrossRef]
- Ward, L.; Walter, R. Participatory Action Research (PAR)—To better understand the experiences of nurse academics working in a team. Contemp. Nurse 2021, 57, 269–279. [Google Scholar] [CrossRef]
- Hernández Sampieri, R.; Fernandez Collado, C.; Baptista Lucio, P. Metodología de la Investigación; México, D.F., Ed.; McGraw-Hill Education: London, UK, 2014. [Google Scholar]
- Otani, T. What Is Qualitative Research? J. Pharm. Soc. Jpn. 2017, 137, 653–658. [Google Scholar] [CrossRef]
- Moser, A.; Korstjens, I. Series: Practical guidance to qualitative research. Part 3: Sampling, data collection and analysis. Eur. J. Gen. Pract. 2018, 24, 9–18. [Google Scholar] [CrossRef]
- Cordeiro, L.; Soares, C.B. Action research in the healthcare field: A scoping reviex. JBI Evid. Synth. 2018, 16, 1003–1047. [Google Scholar] [CrossRef]
- Errasti-Ibarrondo, B.; Jordán, J.A.; Díez-Del-Corral, M.P.; Arantzamendi, M. Conducting phenomenological research: Rationalizing the methods and rigour of the phenomenology of practice. J. Adv. Nurs. 2018, 74, 1723–1734. [Google Scholar] [CrossRef]
- Hennink, M.M.; Kaiser, B.N.; Marconi, V.C. Code saturation versus meaning saturation: How many interviews are enough? Qual. Health Res. 2017, 27, 591–608. [Google Scholar] [CrossRef]
- Kwame, A. Integrating Traditional Medicine and Healing into the Ghanaian Mainstream Health System: Voices from Within. Qual. Health Res. 2021, 31, 1847–1860. [Google Scholar] [CrossRef]
- King, M.; Smith, A.; Gracey, M. Indigenous health part 2: The underlying causes of the health gap. Lancet 2009, 374, 76–85. [Google Scholar] [CrossRef]
- Brewster, D.R.; Morris, P.S. Indigenous child health: Are we making progress? J. Paediatr. Child Health 2015, 51, 40–47. [Google Scholar] [CrossRef]
- Fabiani Hurtado, N.R.; Mejía Salas, H. Fiebre sin foco en niños menores de 36 meses tratados en el servicio de emergencias del Hospital del Niño “Dr. Ovidio Aliaga Uría”. Rev. Soc. Boliv. Pediatría 2014, 53, 3–7. [Google Scholar]
- Jaime, B.E.; Martín, J.J.; Baviera, L.C.; Monzón, Á.C.; Hernández, A.H.; Burriel, J.I.; Mérida, M.J.; Fernández, C.P.; Rodríguez, C.C.; Riechmann, E.R.; et al. Non-IgE-mediated cow’s milk allergy: Consensus document of the spanish society of paediatric gastroenterology, hepatology, and nutrition (SEGHNP), the spanish association of paediatric primary care (AEPAP), the spanish society of extra-hospital paediatrics and primary health care (SEPEAP), and the spanish society of paediatric clinical immunology, allergy, and asthma (SEICAP). An. Pediatría 2019, 90, 193-e1. [Google Scholar]
- National Institute for Health and Care Excellence NICE. Fever in under 5s: Assessment and Initial Management; National Institute for Health and Care Excellence NICE: London, UK, 2019. [Google Scholar]
- López, A.; Cataño, N.; López, H.; Velásquez, V. Diversidad cultural de sanadores tradicionales afrocolombianos: Preservación y conciliación de saberes. Aquichan 2011, 11, 287–304. [Google Scholar] [CrossRef]
| Case 1: |
|---|
| A mother brings her 5-year-old child to the doctor, she noticed that the girl started to cough yesterday; she seems to have normal energy and plays well with her brothers, but she feels hot and eats less than normally. |
| Which questions will you ask the mother? |
| Which observations will you make of the child? |
| Which exams will you perform? |
| What do you think is the most likely cause of the problem? |
| Which actions (treatment) will you give? |
| What will you tell the mother? |
| How will you do the follow-up? |
| Case 2: |
| You are asked to give your advice on the case of a 4-year-old boy who has been ill for 5 days now. He is coughing a lot and feels very hot. The mother already gave him a medication for fever but the fever came back after a few hours. The child is very tired and wants to sleep all the time. |
| Which questions will you ask the mother? |
| Which observations will you make in the child? |
| Which exams will you perform? |
| What do you think is the most likely cause of the problem? |
| Which actions (treatment) will you give? |
| What will you tell to the mother? |
| How will you do the follow-up? |
| What is different compared to the first case? |
| Case 3: |
| The mother of a 7-year-old boy calls you to her house, her son suddenly started to vomit an hour ago. He is very irritable and seems a bit confused when you talk to him. He feels hot and is breathing faster than normally. |
| Which questions will you ask the mother? |
| Which observations will you make in the child? |
| Which exams will you perform? |
| What do you think is the most likely cause of the problem? |
| Which actions (treatment) will you give? |
| What will you tell to the mother? |
| How will you do the follow-up? |
| What is different compared to the first case? |
| Have you attended children with fever in the last year? |
|---|
| Yes/No |
| How many children with fever have you attended in the last year? |
| (number) |
| Have you had complications in the care of a child with a fever and what have they been? |
| Yes/No |
| If your answer is yes, what were these? |
| Have you had to transfer any patient to the hospital? |
| Yes/No |
| How the circumstances were for the transfer to the hospital: |
| Transport |
| Acceptance at the hospital |
| Cooperation and collaboration of the hospital staff |
| Communication hospital staff for the midwife or healer |
| Do you think that the flowchart of children with fever is easy to understand and handle? Rate from 1 to 5. Being 1 nothing understandable and nothing useful and 5 very useful |
| 1. I don’t understand and not useful |
| 2. It is understood little and little useful |
| 3. It is understood moderately and is moderately useful |
| 4. It is understood and useful |
| 5. Very useful |
| Characteristic | Healers (N = 65) |
|---|---|
| N (%) | |
| Gender | 46 (70.8) 19 (29.2) |
| Female | |
| Male | |
| Age (years) | |
| <30 | 9 (13.8) |
| 30–49 | 33 (50.8) |
| 50–69 | 21 (32.3) |
| >70 | 2 (3.1) |
| Ethnicity | |
| Kichwa | 54 (83.1) |
| Mestizo | 6 (9.2) |
| Shuar | 5 (7.7) |
| Education | |
| Illiterate | 4 (6.2) |
| Primary | 15 (23.1) |
| High school | 40 (61.5) |
| Higher | 6 (9.2) |
| Healer | |
| Yachay/Uwishin | 9 (13.8) |
| Midwife/parteras | 35 (53.8) |
| Herb-healer (“Hierbateros”), | 14 (21.5) |
| Bonesetter (“sobadores”). | 7 (10.7) |
| Category | Subcategories |
|---|---|
| Caring for children with fever in indigenous communities | Steps in caring for a child with fever. |
| Alarm signs in children with fever | Signs and symptoms Physical examination of the patient |
| Patient follow-up | Healing rituals or treatments |
| Referral to the Health System | Obstacles to referral to the patients |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bautista-Valarezo, E.; Espinosa, M.E.; Arce Guerrero, N.E.; Verhoeven, V.; Hendrickx, K.; Michels, N.R.M. Improving the Management of Children with Fevers by Healers in Native Rural Areas in the South of Ecuador. Int. J. Environ. Res. Public Health 2023, 20, 3923. https://doi.org/10.3390/ijerph20053923
Bautista-Valarezo E, Espinosa ME, Arce Guerrero NE, Verhoeven V, Hendrickx K, Michels NRM. Improving the Management of Children with Fevers by Healers in Native Rural Areas in the South of Ecuador. International Journal of Environmental Research and Public Health. 2023; 20(5):3923. https://doi.org/10.3390/ijerph20053923
Chicago/Turabian StyleBautista-Valarezo, Estefanía, Maria Elena Espinosa, Narciza Eugenia Arce Guerrero, Veronique Verhoeven, Kristin Hendrickx, and Nele R. M. Michels. 2023. "Improving the Management of Children with Fevers by Healers in Native Rural Areas in the South of Ecuador" International Journal of Environmental Research and Public Health 20, no. 5: 3923. https://doi.org/10.3390/ijerph20053923
APA StyleBautista-Valarezo, E., Espinosa, M. E., Arce Guerrero, N. E., Verhoeven, V., Hendrickx, K., & Michels, N. R. M. (2023). Improving the Management of Children with Fevers by Healers in Native Rural Areas in the South of Ecuador. International Journal of Environmental Research and Public Health, 20(5), 3923. https://doi.org/10.3390/ijerph20053923






