Immediate Effect Evaluation of a Robotic Ankle–Foot Orthosis with Customized Algorithm for a Foot Drop Patient: A Quantitative and Qualitative Case Report
Abstract
1. Introduction
2. Materials and Methods
2.1. Participant
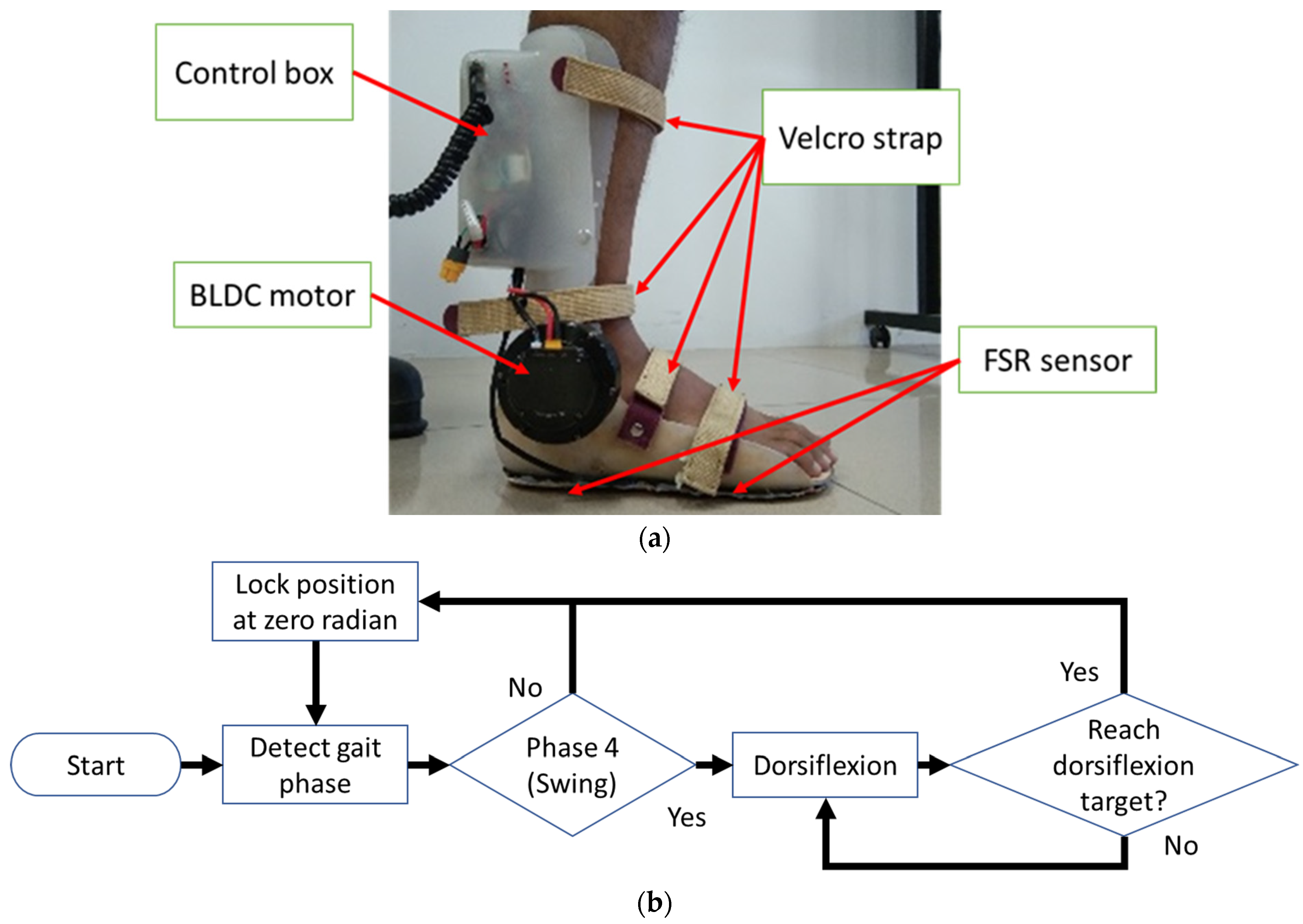
2.2. Customized Robotic AFO
2.3. Data Collection
- -
- The optimal robotic AFO setting is still unknown, so it is necessary to gather further patient information.
- -
- To understand the meaning of the data that researchers from previous studies have obtained, we tested/practiced these results directly on the patient to determine whether there is a gap between theory and practice.
- -
- Understanding the social interactions and feelings between researchers and patients, is to understand the motivation and enthusiasm of both parties to achieve the same goal.
- -
- The data used in the development of the robotic AFO no longer comes from case studies in theory but is also reinforced by data originating from a patient who experienced a stroke.
- Satisfaction category:
- How do you feel when wearing the AFO Robot?
- Are you comfortable standing when using the AFO Robot?
- Are you comfortable sitting when using the AFO Robot?
- Does the AFO Robot affect your balance?
- Do you use energy efficiently while using the AFO Robot?
- Is the AFO Robot comfortable to use?
- Are you satisfied with the appearance of the AFO Robot?
- Does the sound of the AFO robot bother you?
- Will your footwear remain intact when using the AFO Robot?
- Does the AFO robot cover stay intact?
- Can you wear different shoes while using the AFO Robot?
- Are you free while using the AFO Robot?
- Regarding moving using the robotic AFO:
- Can you walk on a flat floor?
- Are you able to sit and stand from the chair?
- Can you walk on a slippery floor?
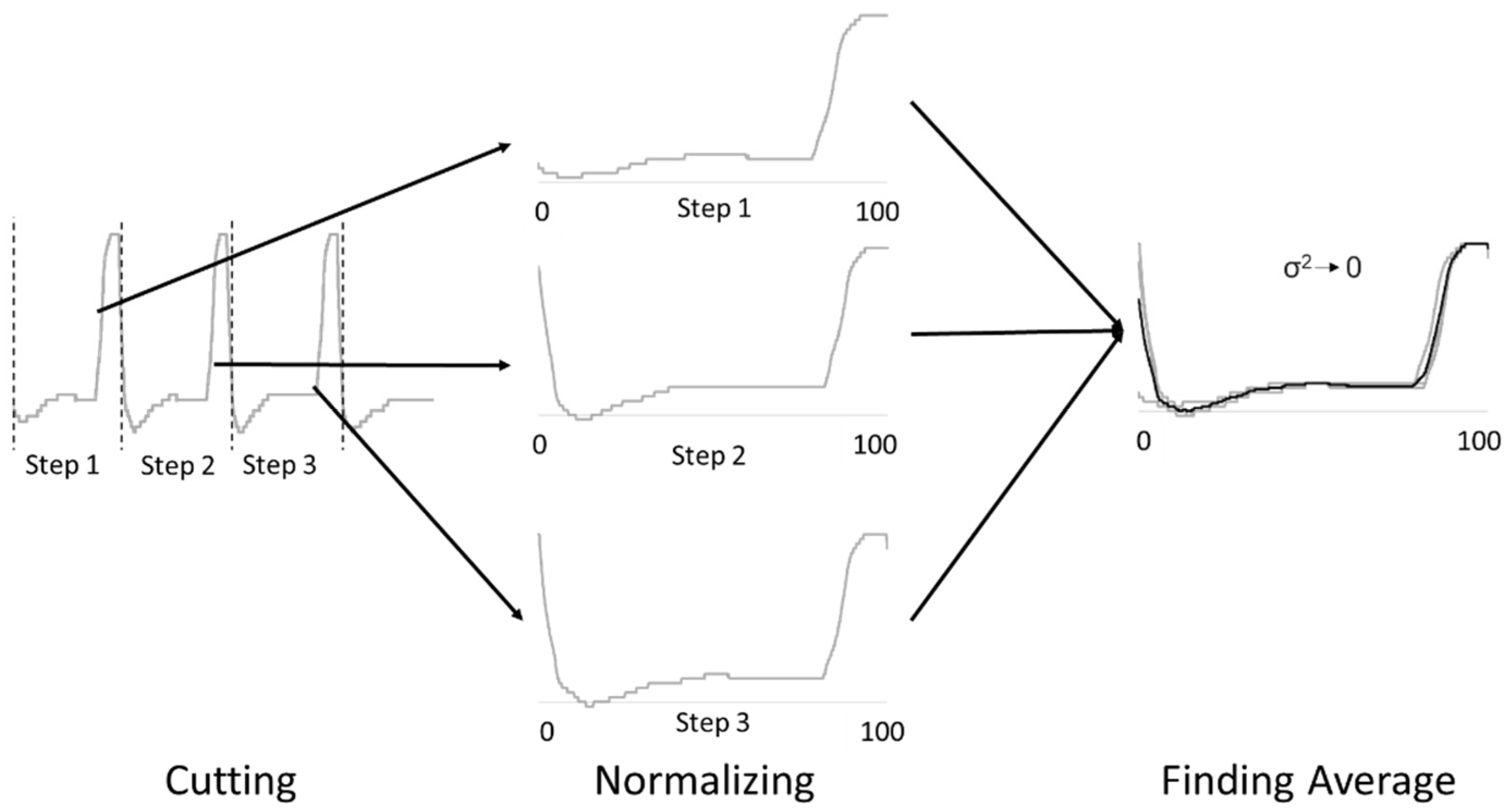
2.4. Data Processing
3. Results
3.1. Spatiotemporal Parameters
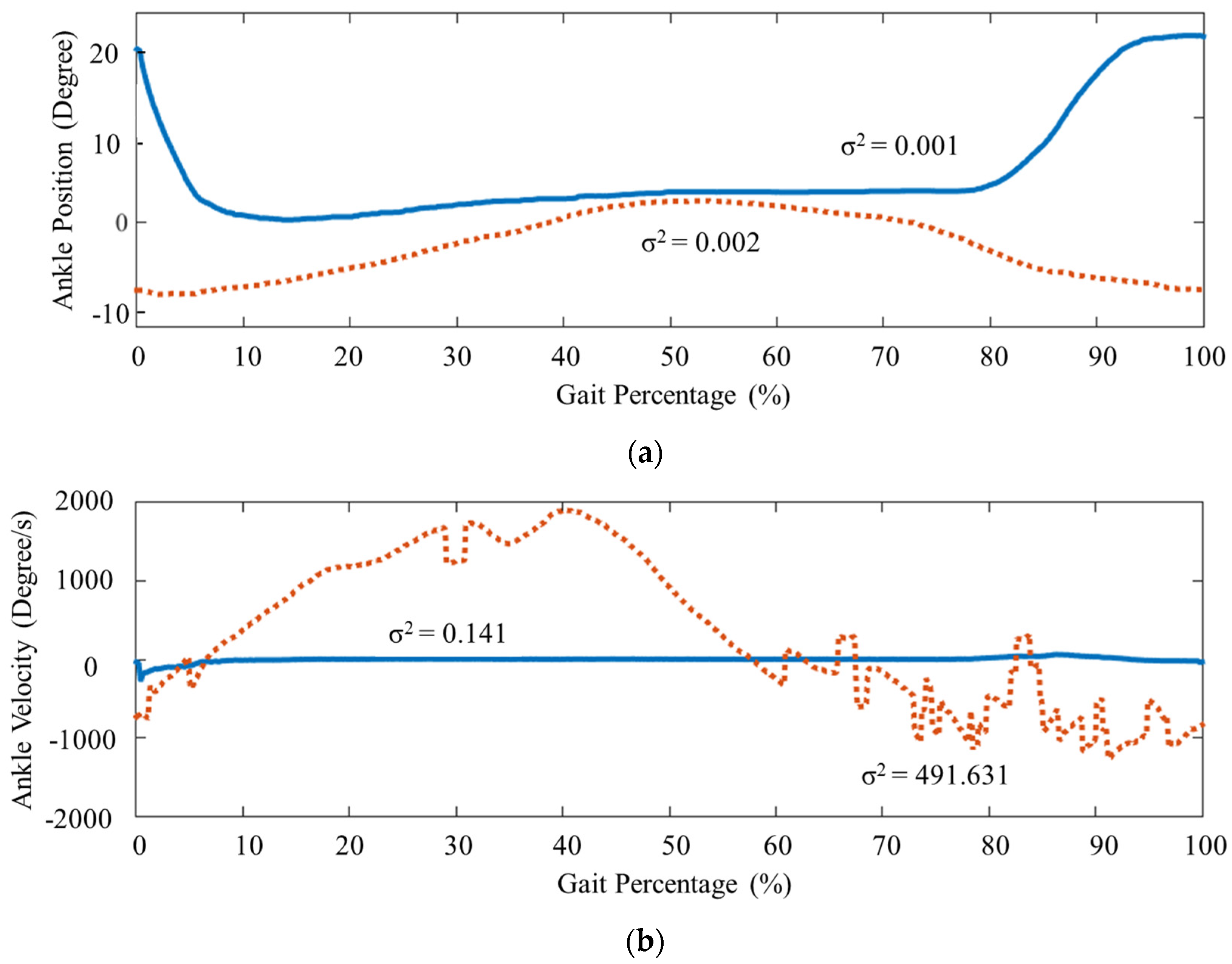
3.2. Ankle Kinematics
3.3. Interview
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Stroke Organizatio. Global Stroke Fact Sheet 2022. Available online: http://ghdx.healthdata.org/gbd-results-tool (accessed on 27 December 2022).
- Nie, P.; Liu, F.; Lin, S.; Guo, J.; Chen, X.; Chen, S.; Yu, L.; Lin, R.; Ms, P.N.; Ms, S.L.; et al. The effects of computer-assisted cognitive rehabilitation on cognitive impairment after stroke: A systematic review and meta-analysis. J. Clin. Nurs. 2021, 31, 1136–1148. [Google Scholar] [CrossRef]
- Anwer, S.; Waris, A.; Gilani, S.O.; Iqbal, J.; Shaikh, N.; Pujari, A.N.; Niazi, I.K. Rehabilitation of Upper Limb Motor Impairment in Stroke: A Narrative Review on the Prevalence, Risk Factors, and Economic Statistics of Stroke and State of the Art Therapies. Healthcare 2022, 10, 190. [Google Scholar] [CrossRef] [PubMed]
- Bae, Y.; Park, D. Immediate Effect of Lower-Leg Kinesio Taping on Ankle Dorsiflexion and Gait Parameters in Chronic Stroke with Foot Drop. J. Stroke Cerebrovasc. Dis. 2022, 31, 106425. [Google Scholar] [CrossRef] [PubMed]
- Srinayanti, Y.; Widianti, W.; Andriani, D.; Firdaus, F.A.; Setiawan, H. Range of Motion Exercise to Improve Muscle Strength among Stroke Patients: A Literature Review. Int. J. Nurs. Health Serv. 2021, 4, 332–343. [Google Scholar] [CrossRef]
- Whittaker, S.L.; Taylor, N.F.; Hill, K.D.; Ekegren, C.L.; Brusco, N.K. Self-managed occupational therapy and physiotherapy for adults receiving inpatient rehabilitation (‘My Therapy’): Protocol for a mixed-methods process evaluation. BMC Health Serv. Res. 2021, 21, 810. [Google Scholar] [CrossRef] [PubMed]
- Adiputra, D.; Nazmi, N.; Bahiuddin, I.; Ubaidillah, U.; Imaduddin, F.; Rahman, M.A.A.; Mazlan, S.A.; Zamzuri, H. A Review on the Control of the Mechanical Properties of Ankle Foot Orthosis for Gait Assistance. Actuators 2019, 8, 10. [Google Scholar] [CrossRef]
- Choo, Y.J.; Chang, M.C. Commonly Used Types and Recent Development of Ankle-Foot Orthosis: A Narrative Review. Healthcare 2021, 9, 1046. [Google Scholar] [CrossRef]
- Zhou, C.; Yang, Z.; Li, K.; Ye, X. Research and Development of Ankle–Foot Orthoses: A Review. Sensors 2022, 22, 6596. [Google Scholar] [CrossRef] [PubMed]
- Raj, R.; Dixit, A.R.; Łukaszewski, K.; Wichniarek, R.; Rybarczyk, J.; Kuczko, W.; Górski, F. Numerical and Experimental Mechanical Analysis of Additively Manufactured Ankle–Foot Orthoses. Materials 2022, 15, 6130. [Google Scholar] [CrossRef]
- Khazaal, A.S.; Aziz, S.J.; Shandookh, A. Development and Manufacturing of Flexible Lightweight Walker for Fractured Foot. IOP Conf. Ser. Mater. Sci. Eng. 2021, 1094, 012128. [Google Scholar] [CrossRef]
- Thalman, C.M.; Debeurre, M.P.; Lee, H. Entrainment during Human Locomotion Using a Soft Wearable Ankle Robot. IEEE Robot. Autom. Lett. 2021, 6, 4265–4272. [Google Scholar] [CrossRef]
- Lu, Y.; Zhang, X.; Ai, Q. Mechanism Design and Analysis of a Multi-DOF Flexible Ankle Rehabilitation Robot. J. Phys. Conf. Ser. 2021, 1884, 012038. [Google Scholar] [CrossRef]
- van der Scheer, J.W.; Goosey-Tolfrey, V.L.; Valentino, S.E.; Davis, G.M.; Ho, C.H. Functional electrical stimulation cycling exercise after spinal cord injury: A systematic review of health and fitness-related outcomes. J. Neuroeng. Rehabil. 2021, 18, 99. [Google Scholar] [CrossRef]
- Alashram, A.R.; Annino, G.; Mercuri, N.B. Changes in spasticity following functional electrical stimulation cycling in patients with spinal cord injury: A systematic review. J. Spinal Cord Med. 2020, 45, 10–23. [Google Scholar] [CrossRef]
- Vasiliauskaite, E.; Ielapi, A.; Beule, M.; Paepegem, W.; Deckers, J.; Vermandel, M.; Forward, M.; Vasiliauskaite, E.; Ielapi, A.; Beule, M.; et al. Disability and Rehabilitation: Assistive Technology A study on the efficacy of AFO stiffness prescriptions. Disabil. Rehabil. Assist. Technol. 2019, 16, 27–39. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.-H.; Choi, I.-R.; Choi, H.-S. Immediate Effects of Ankle–Foot Orthosis Using Wire on Static Balance of Patients with Stroke with Foot Drop: A Cross-Over Study. Healthcare 2020, 8, 116. [Google Scholar] [CrossRef] [PubMed]
- Kadhim, F.M.; Hayal, M.S. Analysis and Evaluating of Flexible Ankle Foot Orthosis for Drop Foot Deformity. Defect Diffus. Forum 2020, 398, 41–47. [Google Scholar] [CrossRef]
- Oba, T.; Kadone, H.; Hassan, M.; Suzuki, K. Robotic Ankle–Foot Orthosis with a Variable Viscosity Link Using MR Fluid. IEEE/ASME Trans. Mechatron. 2019, 24, 495–504. [Google Scholar] [CrossRef]
- Modar, H.; Keisuke, Y.; Hideki, K.; Tomoyuki, U.; Hiromi, M.; Kenji, S. Optimized Design of a Variable Viscosity Link for Robotic AFO. In Proceedings of the 2019 41st Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Berlin, Germany, 23–27 July 2019. Available online: https://ieeexplore.ieee.org/abstract/document/8856773 (accessed on 26 December 2022).
- Zhou, Y.; Liu, L. A Multifunctional Ankle Foot Orthosis Utilizing a Magnetorheological Actuator. IOP Conf. Ser. Mater. Sci. Eng. 2020, 813, 012001. [Google Scholar] [CrossRef]
- Adiputra, D.; Rahman, M.A.A.; Mazlan, S.A. Improving Passive Ankle Foot Orthosis System Using Estimated Ankle Velocity Reference. IEEE Access 2020, 8, 194780–194794. [Google Scholar] [CrossRef]
- Putra, A.P.; Rahmatillah, A.; Rodhiyah, N.K.; Pawana, I.P.A. Computational analysis of ankle-foot orthosis for foot drop case during stance phase in gait cycle. J. Eng. Sci. Technol. 2022, 17, 985–996. [Google Scholar]
- Waterval, N.; Brehm, M.; Harlaar, J.; Nollet, F. Energy cost optimized dorsal leaf ankle-foot-orthoses reduce impact forces on the contralateral leg in people with unilateral plantar flexor weakness. Gait Posture 2021, 92, 71–76. [Google Scholar] [CrossRef] [PubMed]
- Moltedo, M.; Bacek, T.; Serrien, B.; Langlois, K.; Vanderborght, B.; Lefeber, D.; Rodriguez-Guerrero, C. Walking with a powered ankle-foot orthosis: The effects of actuation timing and stiffness level on healthy users. J. Neuroeng. Rehabil. 2020, 17, 98. [Google Scholar] [CrossRef] [PubMed]
- Sanz-Morere, C.B.; Fantozzi, M.; Parri, A.; Giovacchini, F.; Baldoni, A.; Cempini, M.; Crea, S.; Lefeber, D.; Vitiello, N. A Knee–Ankle–Foot Orthosis to Assist the Sound Limb of Transfemoral Amputees. IEEE Trans. Med. Robot. Bionics 2019, 1, 38–48. [Google Scholar] [CrossRef]
- Esposito, E.R.; Schmidtbauer, K.A.; Wilken, J.M. Experimental comparisons of passive and powered ankle-foot orthoses in individuals with limb reconstruction. J. Neuroeng. Rehabil. 2018, 15, 111. [Google Scholar] [CrossRef]
- Inoue, J.; Kimura, R.; Shimada, Y.; Saito, K.; Kudo, D.; Hatakeyama, K.; Watanabe, M.; Maeda, K.; Iwami, T.; Matsunaga, T.; et al. Development of a Gait Rehabilitation Robot Using an Exoskeleton and Functional Electrical Stimulation: Validation in a Pseudo-paraplegic Model. Prog. Rehabil. Med. 2022, 7, 20220001. [Google Scholar] [CrossRef]
- Rahman, M.A.A.; Adiputra, D. Personalized Gait Treatment Using Passive Controllable Ankle Foot Orthosis. IOP Conf. Ser. Mater. Sci. Eng. 2021, 1096, 012002. [Google Scholar] [CrossRef]
- Ballester, B.R.; Ward, N.S.; Brander, F.; Maier, M.; Kelly, K.; Verschure, P.F.M.J. Relationship between intensity and recovery in post-stroke rehabilitation: A retrospective analysis. J. Neurol. Neurosurg. Psychiatry 2021, 93, 226–228. [Google Scholar] [CrossRef]
- Miller, A.; Reisman, D.S.; Billinger, S.A.; Dunning, K.; Doren, S.; Ward, J.; Wright, H.; Wagner, E.; Carl, D.; Gerson, M.; et al. Moderate-intensity exercise versus high-intensity interval training to recover walking post-stroke: Protocol for a randomized controlled trial. Trials 2021, 22, 457. [Google Scholar] [CrossRef]
- Balkman, G.S.; Hafner, B.J.; Rosen, R.E.; Morgan, S.J. Mobility experiences of adult lower limb orthosis users: A focus group study. Disabil. Rehabil. 2022, 44, 7904–7915. [Google Scholar] [CrossRef]
- Choo, Y.J.; Chang, M.C. Effectiveness of an ankle–foot orthosis on walking in patients with stroke: A systematic review and meta-analysis. Sci. Rep. 2021, 11, 15879. [Google Scholar] [CrossRef] [PubMed]
- Ricardo, D.; Raposo, M.R.; Cruz, E.B.; Oliveira, R.; Carnide, F.; Veloso, A.P.; João, F. Effects of Ankle Foot Orthoses on the Gait Patterns in Children with Spastic Bilateral Cerebral Palsy: A Scoping Review. Children 2021, 8, 903. [Google Scholar] [CrossRef] [PubMed]
- Jeon, J.H.; Yang, H.S.; Choi, P.-H.; Ahn, E.J.; Sim, W.S.; Ahn, D.Y.; Kim, J.Y.; Bin Na Lee, S.; Jo, M.; Cho, M.H. Microprocessor-Controlled Prostheses for a Bilateral Transtibial Amputee with Gait Analysis and Satisfaction: A 1-Year Followup Case Report. Int. J. Environ. Res. Public Health 2022, 19, 8279. [Google Scholar] [CrossRef]
- Adiputra, D.; Ubaidillah, U.; Asfari, U.; Waspada, H.S.B.; Humaidi, R.; Prakoso, B.W.; Halisyah, A.N. Robot Ankle Foot Orthosis with Auto Flexion Mode for Foot Drop Training on Post-Stroke Patient in Indonesia. Kinetik 2022, 7, 349–358. [Google Scholar] [CrossRef]
- Adiputra, D.; Rahman, M.A.A.; Bahiuddin, I.; Imaduddin, F.; Nazmi, N. Sensor Number Optimization Using Neural Network for Ankle Foot Orthosis Equipped with Magnetorheological Brake. Open Eng. 2020, 11, 91–101. [Google Scholar] [CrossRef]
- Ren, X.; Lutter, C.; Kebbach, M.; Bruhn, S.; Bader, R.; Tischer, T. Lower extremity joint compensatory effects during the first recovery step following slipping and stumbling perturbations in young and older subjects. BMC Geriatr. 2022, 22, 656. [Google Scholar] [CrossRef] [PubMed]
- Woo, H.; Kong, K.; Rha, D.-W. Lower-Limb-Assisting Robotic Exoskeleton Reduces Energy Consumption in Healthy Young Persons during Stair Climbing. Appl. Bionics Biomech. 2021, 2021, 8833461. [Google Scholar] [CrossRef]
- Kushioka, J.; Sun, R.; Zhang, W.; Muaremi, A.; Leutheuser, H.; Odonkor, C.A.; Smuck, M. Gait Variability to Phenotype Common Orthopedic Gait Impairments Using Wearable Sensors. Sensors 2022, 22, 9301. [Google Scholar] [CrossRef]
- Chen, B.; Zi, B.; Zeng, Y.; Qin, L.; Liao, W.-H. Ankle-foot orthoses for rehabilitation and reducing metabolic cost of walking: Possibilities and challenges. Mechatronics 2018, 53, 241–250. [Google Scholar] [CrossRef]
- Adiputra, D.; Rahman, M.A.A.; Mazlan, S.A.; Nazmi, N.; Shabdin, M.K.; Kobayashi, J.; Ariff, M.H.M. Control Reference Parameter for Stance Assistance Using a Passive Controlled Ankle Foot Orthosis—A Preliminary Study. Appl. Sci. 2019, 9, 4416. [Google Scholar] [CrossRef]
- Baud, R.; Manzoori, A.R.; Ijspeert, A.; Bouri, M. Review of control strategies for lower-limb exoskeletons to assist gait. J. Neuroeng. Rehabil. 2021, 18, 119. [Google Scholar] [CrossRef] [PubMed]
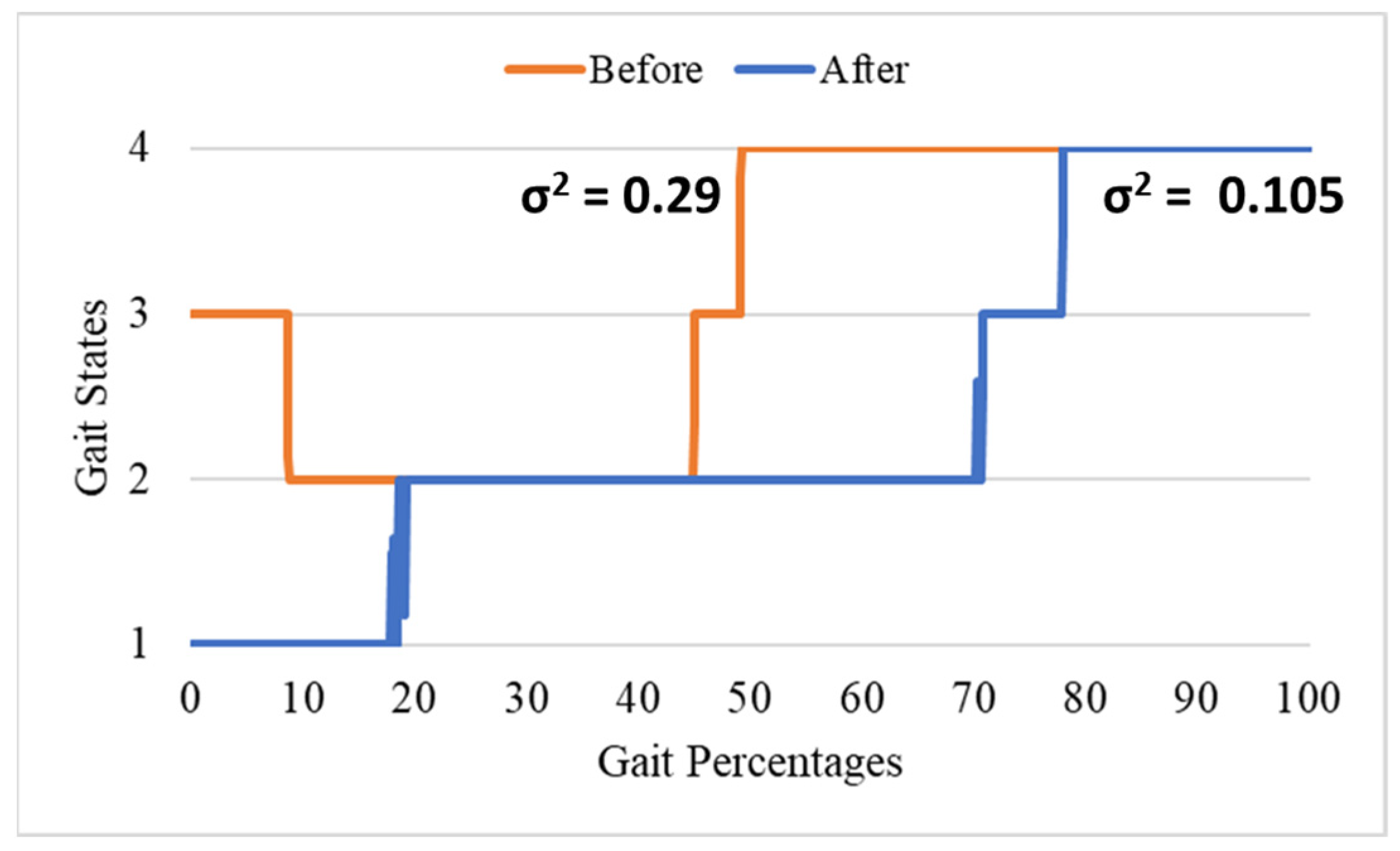
| Gait | P1 | P2 | P3 | P4 | END |
|---|---|---|---|---|---|
| Before | 0.00% | 8.26% | 59.96% | 67.41% | 100.00% |
| After | 0.00% | 10.38% | 75.35% | 81.69% | 100.00% |
| Spatiotemporal Parameter | Unit | Before | σ2 | After | σ2 |
|---|---|---|---|---|---|
| Cadence | Steps/min | 18.14 | 2.17 | 17.97 | 3.52 |
| Stance–swing ratio | Gait % | 60:40 | 147.07 | 75:25 | 31.37 |
| Kinematic Parameter | Unit | Before | σ2 | After | σ2 |
|---|---|---|---|---|---|
| Ankle plantarflexion peak angle at loading response (◦) | Degree | −7.22 | 0.001 | 0.97 | 0.0003 |
| Ankle dorsiflexion peak angle in late stance phase (◦) | Degree | 2.12 | 0.003 | 3.38 | 0.000092 |
| Ankle ROM in stance phase (◦) | Degree | 9.4 | 0.004 | 2.46 | 0.000545 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Adiputra, D.; Asfari, U.; Ubaidillah; Abdul Rahman, M.A.; Harun, A.M. Immediate Effect Evaluation of a Robotic Ankle–Foot Orthosis with Customized Algorithm for a Foot Drop Patient: A Quantitative and Qualitative Case Report. Int. J. Environ. Res. Public Health 2023, 20, 3745. https://doi.org/10.3390/ijerph20043745
Adiputra D, Asfari U, Ubaidillah, Abdul Rahman MA, Harun AM. Immediate Effect Evaluation of a Robotic Ankle–Foot Orthosis with Customized Algorithm for a Foot Drop Patient: A Quantitative and Qualitative Case Report. International Journal of Environmental Research and Public Health. 2023; 20(4):3745. https://doi.org/10.3390/ijerph20043745
Chicago/Turabian StyleAdiputra, Dimas, Ully Asfari, Ubaidillah, Mohd Azizi Abdul Rahman, and Ahmad Mukifza Harun. 2023. "Immediate Effect Evaluation of a Robotic Ankle–Foot Orthosis with Customized Algorithm for a Foot Drop Patient: A Quantitative and Qualitative Case Report" International Journal of Environmental Research and Public Health 20, no. 4: 3745. https://doi.org/10.3390/ijerph20043745
APA StyleAdiputra, D., Asfari, U., Ubaidillah, Abdul Rahman, M. A., & Harun, A. M. (2023). Immediate Effect Evaluation of a Robotic Ankle–Foot Orthosis with Customized Algorithm for a Foot Drop Patient: A Quantitative and Qualitative Case Report. International Journal of Environmental Research and Public Health, 20(4), 3745. https://doi.org/10.3390/ijerph20043745









