Threat Appraisal, Resilience, and Health Behaviors in Recovered COVID-19 Patients: The Serial Mediation of Coping and Meaning-Making
Abstract
1. Introduction
1.1. Threat Appraisal, Resilience, and Health Behaviors
1.2. Coping Strategies and Other Variables
1.3. Coping Strategies and Meaning-Making as Mediators
2. Materials and Methods
2.1. Participants and Procedure
2.2. Procedure
2.3. Measures
2.4. Data Analysis
3. Results
3.1. Sample Characteristics
3.2. Descriptive Statistics and Correlations
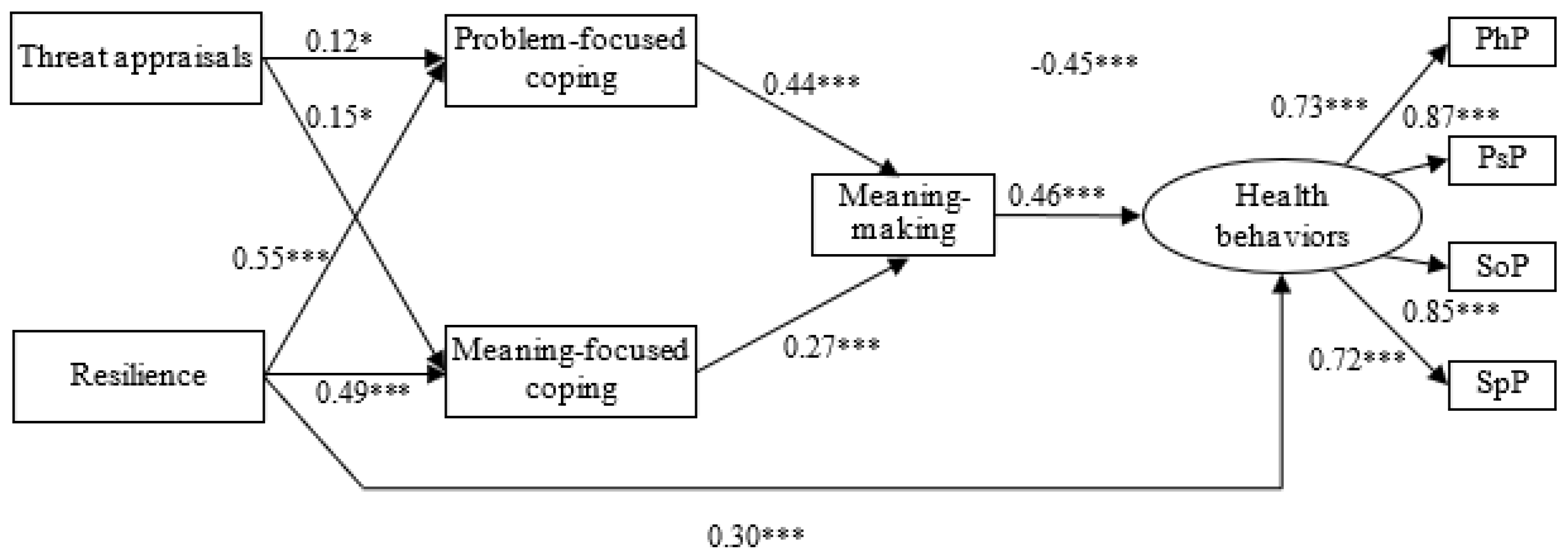
3.3. Serial Mediation Effects
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 11 February 2023).
- Raport zakażeń koronawirusem (SARS-CoV-2). Available online: https://www.gov.pl/web/koronawirus/wykaz-zarazen-koronawirusem-sars-cov-2 (accessed on 11 February 2023).
- Gashi, D.; Gallopeni, F.; Imeri, G.; Shahini, M.; Bahtiri, S. The relationship between Big Five personality traits, coping strategies, and emotional problems through the COVID-19 pandemic. Curr. Psychol 2022. ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Groff, D.; Sun, A.; Ssentongo, A.E.; Ba, D.; Parsons, N.; Poudel, G.R.; Lekoubou, A.; Oh, J.S.; Ericson, J.E.; Ssentongo, P.; et al. Short-term and long-term rates of postacute sequelae of SARS-CoV-2 infection: A systematic review. Infect. Dis. 2021, 4, e2128568. [Google Scholar] [CrossRef] [PubMed]
- Poudel, A.N.; Zhu, S.; Cooper, N.; Roderick, P.; Alwan, N.; Tarrant, C.; Ziauddeen, N.; Yao, G.L. Impact of COVID-19 on health-related quality of life of patients: A structured review. PLoS ONE. 2021, 16, e0259164. [Google Scholar] [CrossRef] [PubMed]
- Salari, N.; Hosseinian-Far, A.; Jalali, R.; Vaisi-Raygani, A.; Rasoulpoor, S.; Mohammadi, M.; Rasoulpoor, S.; Khaledi-Paveh, B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Glob. Health 2020, 16, 57. [Google Scholar] [CrossRef] [PubMed]
- Pei, F.; Wang, Y.; McCloskey, R.J.; Liu, Q. Experiences, life changes, and support systems of recovered COVID-19 patients from practitioners’ perspectives: A qualitative study. Qual. Soc. Work. 2022, 9, 14733250221119440. [Google Scholar] [CrossRef]
- Deng, J.; Zhou, F.; Hou, W.; Silver, Z.; Wong, C.Y.; Chang, O.; Drakos, A.; Zuo, Q.K.; Huang, E. The prevalence of depressive symptoms, anxiety symptoms and sleep disturbance in higher education students during the COVID-19 pandemic: A systematic review and meta-analysis. Psychiatry Res. 2021, 301, 113863. [Google Scholar] [CrossRef]
- Pappa, S.; Ntella, V.; Giannakas, T.; Giannakoulis, V.G.; Papoutsi, E.; Katsaounou, P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav. Immun. 2020, 88, 901–907. [Google Scholar] [CrossRef]
- Vindegaard, N.; Benros, M.E. COVID-19 Pandemic and Mental Health Consequences: Systematic Review of the Current Evidence. Brain Behav. Immun. 2020, 89, 531–542. [Google Scholar] [CrossRef]
- Higgins, V.; Sohaei, D.; Diamandis, E.P.; Prassas, I. COVID-19: From an Acute to Chronic Disease? Potential Long-Term Health Consequences. Crit. Rev. Clin. Lab. Sci. 2021, 58, 297–310. [Google Scholar] [CrossRef] [PubMed]
- Chu, G.M.; Goger, P.; Malaktaris, A.; Lang, A.J. The role of threat appraisal and coping style in psychological response to the COVID-19 pandemic among university students. J. Affect. Disord. Rep. 2022, 8, 100325. [Google Scholar] [CrossRef]
- Shamblaw, A.L.; Rumas, R.L.; Best, M.W. Coping during the COVID-19 pandemic: Relations with mental health and quality of life. Can. Psychol. 2021, 62, 92–100. [Google Scholar] [CrossRef]
- Yoshitake, N.; Omori, M.; Sugawara, M.; Akishinonomiya, K.; Shimada, S. Do health beliefs, personality traits, and interpersonal concerns predict TB prevention behavior among Japanese adults? PLoS ONE. 2019, 14, e0211728. [Google Scholar] [CrossRef]
- Pan, J.Y. A resilience-based and meaning-oriented model of acculturation: A sample of mainland Chinese postgraduate students in Hong Kong. Int. J. Intercult. Relat. 2011, 35, 592–603. [Google Scholar] [CrossRef]
- Constant, A.; Conserve, D.F.; Gallopel-Morvan, K.; Raude, J. Socio-cognitive factors associated with lifestyle changes in response to the COVID-19 epidemic in the general population: Results from a cross-sectional study in France. Front. Psychol. 2020, 11, 579460. [Google Scholar] [CrossRef] [PubMed]
- Lahiri, A.; Iha, S.S.; Chakraborty, A.; Dobe, M.; Dey, A. Role of threat and coping appraisal in protection motivation for adoption of preventive behavior during COVID-19 pandemic. Front. Public Health. 2021, 9, 678566. [Google Scholar] [CrossRef]
- Maloney, E.K.; Lapinski, M.K.; Witte, K. Fear appeals and persuasion: A review and update of extended parallel process model. Soc. Personal. Psychol. Compass. 2011, 5, 206–219. [Google Scholar] [CrossRef]
- Al-Rasheed, M. Protective behavior against COVID-19 among the public in Kuwait: An examination of the Protection Motivation Theory, trust in government, and sociodemographic factors. Soc. Work Public Health. 2020, 35, 546–556. [Google Scholar] [CrossRef] [PubMed]
- Šuriņa, S.; Martinsone, K.; Perepjolkina, V.; Kolesnikova, J.; Vainik, U.; Ruža, A.; Vrublevska, J.; Smirnova, D.; Fountoulakis, K.N.; Rancans, E. Factors related to COVID-19 preventive behaviors: A structural equation model. Front. Psychol. 2021, 12, 676521. [Google Scholar] [CrossRef] [PubMed]
- McGinty, H.L.; Goldenberg, J.L.; Jacobsen, P.B. Relationship of threat appraisal with coping appraisal to fear of cancer recurrence in breast cancer survivors. Psycho-Oncology 2012, 21, 203–210. [Google Scholar] [CrossRef]
- Ireland, J.L. The importance of comping, threat appraisal, and beliefs in understanding and responding to fear of victimization: Applications to a male prisoner sample. Law Hum. Behav. 2011, 35, 306–315. [Google Scholar] [CrossRef]
- Luthar, S.S.; Cichetti, D. The construct of resilience: Implications for interventions and social policies. Dev. Psychoaptol. 2000, 12, 857–885. [Google Scholar] [CrossRef]
- Sturgeon, J.A.; Zautra, A.J. Resilience: A new paradigm for adaptation to chronic pain. Curr. Pain Headache Rep. 2010, 14, 105–112. [Google Scholar] [CrossRef] [PubMed]
- Kermott, C.A.; Johnoson, R.E.; Sood, R.; Jenkins, S.M.; Sood, A. Is higher resilience predictive of lower stress and better mental health among corporate executives? PLoS ONE. 2019, 14, e0218092. [Google Scholar] [CrossRef] [PubMed]
- Gao, J.; Zheng, P.; Jia, Y.; Chen, H.; Mao, Y.; Chen, S.; Wang, Y.; Fu, H.; Dai, J. Mental Health Problems and Social Media Exposure during COVID-19 Outbreak. PLoS ONE 2020, 15, e0231924. [Google Scholar] [CrossRef]
- Smith, J.L.; Hollinger-Smith, L. Savoring, resilience, and psychological well-being in older adults. Aging Ment. Health. 2015, 19, 192–200. [Google Scholar] [CrossRef]
- Markovitz, S.E.; Schrooten, W.; Amtz, A.; Peters, M.L. Resilience as a predictor for emotional response to the diagnosis and surgery in breast cancer patients. Psycho-Oncology 2015, 24, 1639–1645. [Google Scholar] [CrossRef]
- Smith, B.W.; Dalen, J.; Wiggins, K.; Tooley, E.; Christopher, P.; Bernard, J. The brief resilience scale: Assessing the ability to bounce back. Int. J. Behav. Med. 2008, 15, 194–200. [Google Scholar] [CrossRef] [PubMed]
- Endler, N.S.; Parker, J.D.A. Assessment of multidimensional coping: Task, emotion, and avoidance strategies. Psychol. Assess. 1994, 6, 50–60. [Google Scholar] [CrossRef]
- Doron, J.; Trouillet, R.; Maneveau, A.; Neveu, D.; Ninot, G. Coping profiles, perceived stress and health-related behaviors: A cluster analysis approach. Health Promot. Int. 2015, 30, 88–100. [Google Scholar] [CrossRef]
- Krok, D.; Zarzycka, B. Risk perception of COVID-19, meaning-based resources and psychological well-being amongst healthcare personnel: The mediating role of coping. J. Clin. Med. 2020, 9, 3225. [Google Scholar] [CrossRef]
- Penley, J.A.; Tomaka, J.; Wiebe, J.S. The association of coping to physical and psychological health outcomes: A meta-analystic review. J. Behav. Med. 2003, 25, 551–603. [Google Scholar] [CrossRef] [PubMed]
- Tinella, L.; Tinterri, A.; Dipace, A.; Ladogana, M.; Loiodice, I.; Bosco, A. Sociodemographic and digital education factors are associated to general health, coping strategies, and academic outcomes of undergraduate students during the post-pandemic period. Eur. J. Investig. Health Psychol. Educ. 2022, 12, 1334–1348. [Google Scholar] [CrossRef]
- Savitsky, B.; Findling, Y.; Ereli, A.; Hendel, T. Anxiety and coping strategies among nursing students during the covid-19 pandemic. Nurse Educ. Pract. 2020, 46, 102809. [Google Scholar] [CrossRef] [PubMed]
- Tsuno, K. Do personal resilience, coping styles, and social support prevent future psychological distress when experiencing workplace bullying? Evidence from a 1-year prospective study. BMC Psychol. 2022, 10, 310. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Yu, W.; Wu, X.; Wan, H.; Wang, Y.; Lu, G. Psychological resilience and positive coping styles among Chinese undergraduate students: A cross-sectional study. BMC Psychol. 2020, 8, 79. [Google Scholar] [CrossRef] [PubMed]
- Rahmat, H.; Aris, A.; Miskam, H.M.; Rajendran, K.; Mashudi, R. Students’ attitudes and coping strategies relating to online learning during the COVID-19 pandemic: A cross-sectional study. F1000Research 2022, 11, 320. [Google Scholar] [CrossRef]
- Shigeto, A.; Laxman, D.J.; Landy, J.F.; Scheier, L.M. Typologies of coping in young adults in the context of the COVID-19 pandemic. J. Gen. Psychol. 2021, 3, 272–304. [Google Scholar] [CrossRef]
- Marcía, P.; Barranco, M.; Gorbeña, S.; Álvarez-Fuentes, E.; Iraurgi, I. Resilience and coping strategies in relation to mental health outcomes in people with cancer. PLoS ONE. 2021, 16, e0252075. [Google Scholar] [CrossRef]
- Van den Bos, K.; Hewstone, M.; Schut, H.A.W.; de Wit, J.B.F.; Stroebe, M.S. On the scope of social psychology: An introduction. In The Scope of Social Psychology: Theory and Applications; Hewstone, M., Schut, H.A.W., de Wit, J.B.F., Van den Bos, K., Stroebe, M.S., Eds.; Psychology Press: London, UK, 2007; pp. 1–10. [Google Scholar]
- Folkman, S.; Moskowitz, T. Positive affect and meaning-focused coping during significant psychological stress. In The Scope of Social Psychology: Theory and Applications; Hewstone, M., Schut, H.A.W., de Wit, J.B.F., Van den Bos, K., Stroebe, M.S., Eds.; Psychology Press: London, UK, 2007; pp. 193–208. [Google Scholar]
- Park, C.L.; Finkelstein-Fox, L.; Russell, B.S.; Fendrich, M.; Hutchison, M.; Becker, J. Psychological resilience early in the COVID-19 pandemic: Stressors, resources, and coping strategies in a national sample of Americans. Am. Psychol. 2021, 76, 715–728. [Google Scholar] [CrossRef]
- Yıldırım, M.; Arslan, G.; Wong, P.T.P. Meaningful living, resilience, affective balance, and psychological health problems among Turkish young adults during coronavirus pandemic. Curr. Psychol. 2022, 41, 7812–7823. [Google Scholar] [CrossRef] [PubMed]
- Dardas, L.A.; Ahmad, M.M. Coping strategies as mediators and moderators between stress and quality of life among parents of children with autistic disorder. Stress Health. 2015, 31, 5–12. [Google Scholar] [CrossRef]
- Major, B.; Richards, C.; Cooper, M.L.; Cozzarelli, C.; Zubek, J. Personal resilience, cognitive appraisals, and coping: An integrative model of adjustment to abortion. J. Pers. Soc. Psychol. 1998, 74, 735–752. [Google Scholar] [CrossRef]
- Krok, D.; Zarzycka, B.; Telka, E. The Perception of COVID-19, the Light Triad, Harmony and Ethical Sensitivity in Late Adolescents: The Role of Meaning-Making and Stress. ResearchSquare 2022. in review. [Google Scholar]
- Krok, D.; Zarzycka, B.; Telka, E. Risk of contracting COVID-19, personal resources and subjective well-being among healthcare workers: The mediating role of stress and meaning-making. J. Clin. Med. 2021, 10, 132. [Google Scholar] [CrossRef] [PubMed]
- Więsyk, S.M.; Płudowska, M. The mediating role of coping styles in the relations between temperament traits and occupational buronout in bank employees. Med. Stud. 2022, 38, 59–67. [Google Scholar] [CrossRef]
- Ashby, J.S.; Gnilka, P.B. Multidimensional perfectionism and perceived stress: Group differences and test of a coping mediation model. Pers. Individ. Differ. 2017, 119, 106–111. [Google Scholar] [CrossRef]
- Thompson, N.J.; Fiorillo, D.; Rothbaum, B.O.; Ressler, K.J.; Michopoulos, V. Coping strategies as mediators in relation to resilience and posttraumatic stress disorder. J. Affect. Disord. 2018, 225, 153–159. [Google Scholar] [CrossRef] [PubMed]
- de la Fuente, J.; Santos, F.H.; Garzón-Umerenkova, A.; Fadda, S.; Solinas, G.; Pignata, S. Cross-sectional study of resilience, positivity and coping strategies as predictors of engagement-burnout un undergraduate students: Implications for prevention and treatment in mental well-being. Front. Psychiatry. 2021, 12, 596453. [Google Scholar] [CrossRef] [PubMed]
- Aliche, J.C.; Ifeagwazi, C.M.; Onyishi, I.E.; Mefoh, P.C. Presence of meaning in life mediates the relations between social support, posttraumatic growth, and resilience in young adult survivors of a terror attack. J. Loss Trauma. 2019, 24, 736–749. [Google Scholar] [CrossRef]
- Juczynski, Z. Narzędzia Pomiaru w Promocji i Psychologii Zdrowia [Tools for Assessment of Health in Promotion of Health and Psychology]; Polish Psychological Society: Warsaw, Poland, 2001. [Google Scholar]
- Gruszczyńska, E.; Knoll, N. Meaning-focused coping, pain, and affect: A diary study of hospitalized women with rheumatoid arthritis. Qual. Life Res. 2015, 24, 2873–2883. [Google Scholar] [CrossRef]
- Krok, D.; Zarzycka, B. Self-efficacy and psychological well-being in cardiac patients: Moderated mediation by affect and meaning-making. J. Psychol. 2020, 154, 411–425. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.G. Statistical power analyses using G* Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef]
- MacKinnon, D.P.; Lockwood, C.M.; Williams, J. Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivar. Behav. Res. 2004, 39, 99–128. [Google Scholar] [CrossRef]
- Mueller, R.O.; Hancock, G.R. Structural equation modeling. In The Reviewer’s Guide to Quantitative Methods in the Social Sciences; Hancock, G.R., Stapleton, L.M., Mueller, R.O., Eds.; Routledge: London, UK, 2018; pp. 445–456. [Google Scholar]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression Based Approach; The Guilford Press: New York, NY, USA, 2013. [Google Scholar]
- Acar, D.; Kıcali, Ü.Ö. An integrated approach to COVID-19 preventive behaviour intentions: Protection Motivation Theory, information acquisition, and trust. Soc. Work Public Health. 2022, 37, 419–434. [Google Scholar] [CrossRef] [PubMed]
- Floyd, D.L.; Prentice-Dunn, S.; Rogers, R.W. A meta-anaylsis of research on Protection Motivation Theory. J. Appl. Soc. Psychol. 2000, 30, 407–429. [Google Scholar] [CrossRef]
- Maddux, J.E.; Rogers, R.W. Protection motivation and self-efficacy: A revised theory of fear appeals and attitude change. J. Exp. Soc. Psychol. 1983, 19, 469–479. [Google Scholar] [CrossRef]
- Wu, A.Q.; Lau, V.M.C. COVID-19-induced negative emotions and the impacts on personal values and travel behaviors: A threat appraisal perspective. J. Hosp. Tour. Manag. 2022, 51, 143–155. [Google Scholar] [CrossRef]
- Kaplan, S.; Tchetchik, A.; Greenberg, D.; Sapir, I. Transit Use Reduction Following COVID-19: The Effect of Threat Appraisal, Proactive Coping and Institutional Trust. Transp. Res. Part A Policy Pract. 2022, 159, 338–356. [Google Scholar] [CrossRef] [PubMed]
- Jeste, D.V.; Glorioso, D.K.; Depp, C.A.; Lee, E.E.; Daly, R.E.; Jester, D.J.; Palmer, B.W.; Mausbach, B.T. Remotely administered resilience- and wisdom-focused intervention to reduce perceived stress and loneliness: Pilot controlled clinical trial in older adults. Am. J. Geriatr. Psychiatry. 2023, 31, 58–64. [Google Scholar] [CrossRef]
- Faria, D.A.P.; Revoredo, L.S.; Vilar, M.J.; Chaves, M.E.M. Resilience and treatment adhesion in patiens with systemic lupus erythematosus. Open Rheumatol. J. 2014, 8, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Min, J.A.; Lee, N.B.; Lee, C.U.; Lee, C.; Chae, J.H. Low trait anxiety, high resilience, and their interaction as possible predictors for treatment response in patients with depression. J. Affect. Disord. 2012, 137, 61–69. [Google Scholar] [CrossRef] [PubMed]
- Seghal, P.; Ungaro, R.C.; Foltz, C.; Iacoviello, B.; Dubinsky, M.C.; Keefer, L. High levels of psychological resilience associated with less disease activity, better quality of life, and fewer surgeries in inflammatory bowel disease. Inflamm. Bowel Dis. 2021, 27, 791–796. [Google Scholar] [CrossRef]
- Weitzel, E.C.; Löbner, M.; Röhr, S.; Pabst, A.; Reininghaus, U.; Riedel-Heller, S.G. Prevalence of high resilience in old age and association with perceived threat of COVID-19—Results from a representative survey. Int. J. Environ. Res. Public Health. 2021, 18, 7173. [Google Scholar] [CrossRef] [PubMed]
- Skodol, A.E. Personality disorder classification: Stuck in neutral, how to move forward? Curr. Psychiatry Rep. 2014, 16, 480. [Google Scholar] [CrossRef] [PubMed]
- Krüger, M.; Albris, K. Resilience unwanted: Between control and cooperation in disaster response. Secur. Dialogue. 2021, 52, 343–360. [Google Scholar] [CrossRef]
- Dias, C.; Cruz, J.F.; Fonseca, A.M. The relationship between multidimensional competitive anxiety, cognitive threat appraisal, and coping strategies: A multi-sport study. Int. J. Sport Exerc. Psychol. 2012, 10, 52–65. [Google Scholar] [CrossRef]
- Elkayal, M.M.; Shahin, M.A.H.; Hussien, R.M. Psychological distress related to the emerging COVID-19 pandemic and coping strategies among general population in Egypt. J. Egypt. Public. Health. Assoc. 2022, 97, 3. [Google Scholar] [CrossRef]
- Taha, S.; Matheson, K.; Cronin, T.; Anisman, H. Intolerance of Uncertainty, Appraisals, Coping, and Anxiety: The Case of the 2009 H1N1 Pandemic. Br. J. Health Psychol. 2014, 19, 592–605. [Google Scholar] [CrossRef]
- Thompson, S.C. Finding positive meaning in stressful event and coping. Basic Appl. Soc. Psych. 1985, 6, 279–295. [Google Scholar] [CrossRef]
- Szczuka, Z.; Siwa, M.; Abraham, C.; Baban, A.; Brooks, S.; Cipolletta, S.; Danso, E.; Dombrowski, S.U.; Gan, Y.; Gaspar, T.; et al. Handwashing adherence during the COVID-19 pandemic: A longitudinal study based on protection motivation theory. Soc. Sci. Med. 2023, 317, 115569. [Google Scholar] [CrossRef]
- Upenieks, L.; Ellison, C.G. Changes in religiosity and reliance on God during the COVID-19 pandemic: A protective role under conditions of financial strain? Rev. Relig. Res 2023. ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Ziółkowska, N.; Bargiel-Matusiewicz, K.; Gruszczyńska, E. Emotional state of parents of children diagnosed with cancer: Examining religious and meaning-focused coping. Religions 2020, 11, 132. [Google Scholar] [CrossRef]
- Liang, F.; Cao, L. Linking employee resilience with organizational resilience: The roles of coping mechanism and managerial resilience. Psychol. Res. Behav. Manag. 2021, 14, 1063–1075. [Google Scholar] [CrossRef] [PubMed]
- Popa-Velea, O.; Diaconescu, L.; Popescu, M.J.; Truţescu, C. Resilience and active coping style: Effects on the self-reported quality of life in cancer patients. Int. J. Psychiatry Med. 2017, 52, 124–136. [Google Scholar] [CrossRef]
- Tan-Kristanto, S.; Kiropoulos, L.A. Resilience, self-efficacy, coping styles and depressive and anxiety symptoms in those newly diagnosed with multiple sclerosis. Psychol. Health Med. 2015, 20, 635–645. [Google Scholar] [CrossRef]
- Karataş, Z.; Tagay, Ö. The relationship between resilience of the adults affected by the covid pandemic in Turkey and COVID-19 fear, meaning in life, life satisfaction, intolerance of uncertainty and hope. Pers. Individ. Dif. 2021, 172, 110592. [Google Scholar] [CrossRef]
- Eisenbeck, N.; Carreno, D.F.; Wong, P.T.P.; Hicks, J.A.; García María, R.R.; Puga, J.L.; Greville, J.; Testoni, I.; Biancalani, G.; Cepeda López, A.C.; et al. An international study on psychological coping during COVID-19: Towards a meaning-centered coping style. Int. J. Clin. Health Psychol. 2022, 22, 100256. [Google Scholar] [CrossRef]
- Wiener, C.L.; Dodd, M.J. Coping amid uncertainty: An illness trajectory perspective. Sch. Inq. Nurs. Pract. 1993, 7, 17–31. [Google Scholar] [PubMed]
- Guerrero-Torrelles, M.; Monforte-Royo, C.; Rodríguez-Prat, A.; Porta-Sales, J.; Balaguer, A. Understanding meaning in life interventions in patients with advanced disease: A systematic review and realist synthesis. Palliat. Med. 2017, 9, 798–813. [Google Scholar] [CrossRef]
- Elemo, A.S.; Kara, E.; Rostamzadeh, M. The fear of COVID-19 and flourishing: The mediating role of search for meaning and presence of meaning. Curr. Psychol 2022. ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Xie, C.S.; Kim, Y. Post-traumatic growth during COVID-19: The role of perceived social support, personality, and coping strategies. Healthcare 2022, 10, 224. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | ||
|---|---|---|
| Age | M 40.31 | SD 17.19 |
| Body mass index | 26.64 | 3.21 |
| Symptom severity (on a scale from 1 to 10) | 5.78 | 2.34 |
| Time since COVID-19 in months | 6.79 | 4.29 |
| Range of the time since COVID-19 | from 5 days to 18 moths | |
| N | % | |
| Sex | ||
| Male | 129 | 48.5 |
| Female | 137 | 51.5 |
| Hospitalization due to COVID-19 symptoms | 78 | 29.3 |
| Educational attainment | ||
| Basic education | 40 | 15.1 |
| Vocational education | 75 | 28.3 |
| High school education | 101 | 37.9 |
| University education | 50 | 18.7 |
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| - | ||||||||||||
| 0.36 *** | - | |||||||||||
| 0.59 *** | 0.29 *** | - | ||||||||||
| 0.05 | 0.10 | 0.20 ** | - | |||||||||
| 0.46 *** | 0.25 *** | 0.30 *** | 0.03 | - | ||||||||
| 0.30 *** | 0.13 * | 0.27 *** | 0.17 ** | 0.53 *** | - | |||||||
| 0.20 ** | 0.09 | 0.14 * | 0.19 ** | 0.40 *** | 0.63 *** | - | ||||||
| 0.16 ** | 0.13 | 0.18 ** | 0.17 ** | 0.49 *** | 0.73 *** | 0.73 *** | - | |||||
| 0.17 ** | 0.12 | 0.04 | 0.07 | 0.46 *** | 0.59 *** | 0.43 *** | 0.56 *** | - | ||||
| 0.25 ** | 0.07 | 0.16 ** | 0.09 | 0.19 ** | 0.28 *** | 0.36 *** | 0.29 *** | 0.24 *** | - | |||
| 0.35 *** | 0.16 * | 0.36 *** | 0.21 *** | 0.32 *** | 0.37 *** | 0.34 *** | 0.36 *** | 0.40 *** | 0.59 *** | - | ||
| 0.17 ** | 0.18 ** | 0.18 ** | 0.06 | 0.48 *** | 0.42 *** | 0.41 *** | 0.41 *** | 0.43 *** | 0.47 *** | 0.59 *** | - | |
| 0.11 | 0.11 | 0.22 *** | 0.09 | 0.33 *** | 0.39 *** | 0.36 *** | 0.38 *** | 0.39 *** | 0.46 *** | 0.61 *** | 0.54 *** | |
| M | 40.15 | 6.80 | 5.79 | 4.20 | 3.44 | 3.86 | 3.77 | 3.85 | 3.70 | 3.47 | 3.64 | 3.67 | - |
| SD | 17.05 | 4.31 | 2.34 | 0.66 | 0.98 | 0.80 | 0.80 | 0.79 | 0.89 | 0.92 | 0.78 | 0.70 | 3.53 |
| 0.62 |
| Model Pathways | Estimates | Standard Errors | 95% CI | |
|---|---|---|---|---|
| Lower | Upper | |||
| Threat appraisal→Problem- and Meaning-focused coping/Meaning-making→Health behaviors | 0.04 a | 0.02 | 0.01 | 0.07 |
| Resilience→Problem- and Meaning-focused coping/Meaning-making→Health behaviors | 0.15 a | 0.07 | 0.13 | 0.23 |
| Problem-focused coping→Meaning-making→Health behaviors | 0.15 a | 0.04 | 0.08 | 0.24 |
| Meaning-focused coping→Meaning-making→Health behaviors | 0.13 a | 0.04 | 0.06 | 0.21 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Krok, D.; Telka, E.; Szcześniak, M.; Falewicz, A. Threat Appraisal, Resilience, and Health Behaviors in Recovered COVID-19 Patients: The Serial Mediation of Coping and Meaning-Making. Int. J. Environ. Res. Public Health 2023, 20, 3649. https://doi.org/10.3390/ijerph20043649
Krok D, Telka E, Szcześniak M, Falewicz A. Threat Appraisal, Resilience, and Health Behaviors in Recovered COVID-19 Patients: The Serial Mediation of Coping and Meaning-Making. International Journal of Environmental Research and Public Health. 2023; 20(4):3649. https://doi.org/10.3390/ijerph20043649
Chicago/Turabian StyleKrok, Dariusz, Ewa Telka, Małgorzata Szcześniak, and Adam Falewicz. 2023. "Threat Appraisal, Resilience, and Health Behaviors in Recovered COVID-19 Patients: The Serial Mediation of Coping and Meaning-Making" International Journal of Environmental Research and Public Health 20, no. 4: 3649. https://doi.org/10.3390/ijerph20043649
APA StyleKrok, D., Telka, E., Szcześniak, M., & Falewicz, A. (2023). Threat Appraisal, Resilience, and Health Behaviors in Recovered COVID-19 Patients: The Serial Mediation of Coping and Meaning-Making. International Journal of Environmental Research and Public Health, 20(4), 3649. https://doi.org/10.3390/ijerph20043649









