Epidemiological Predictors of Positive SARS-CoV-2 Polymerase Chain Reaction Test in Three Cohorts: Hospitalized Patients, Healthcare Workers, and Military Population, Serbia, 2020
Abstract
1. Introduction
2. Materials and Methods
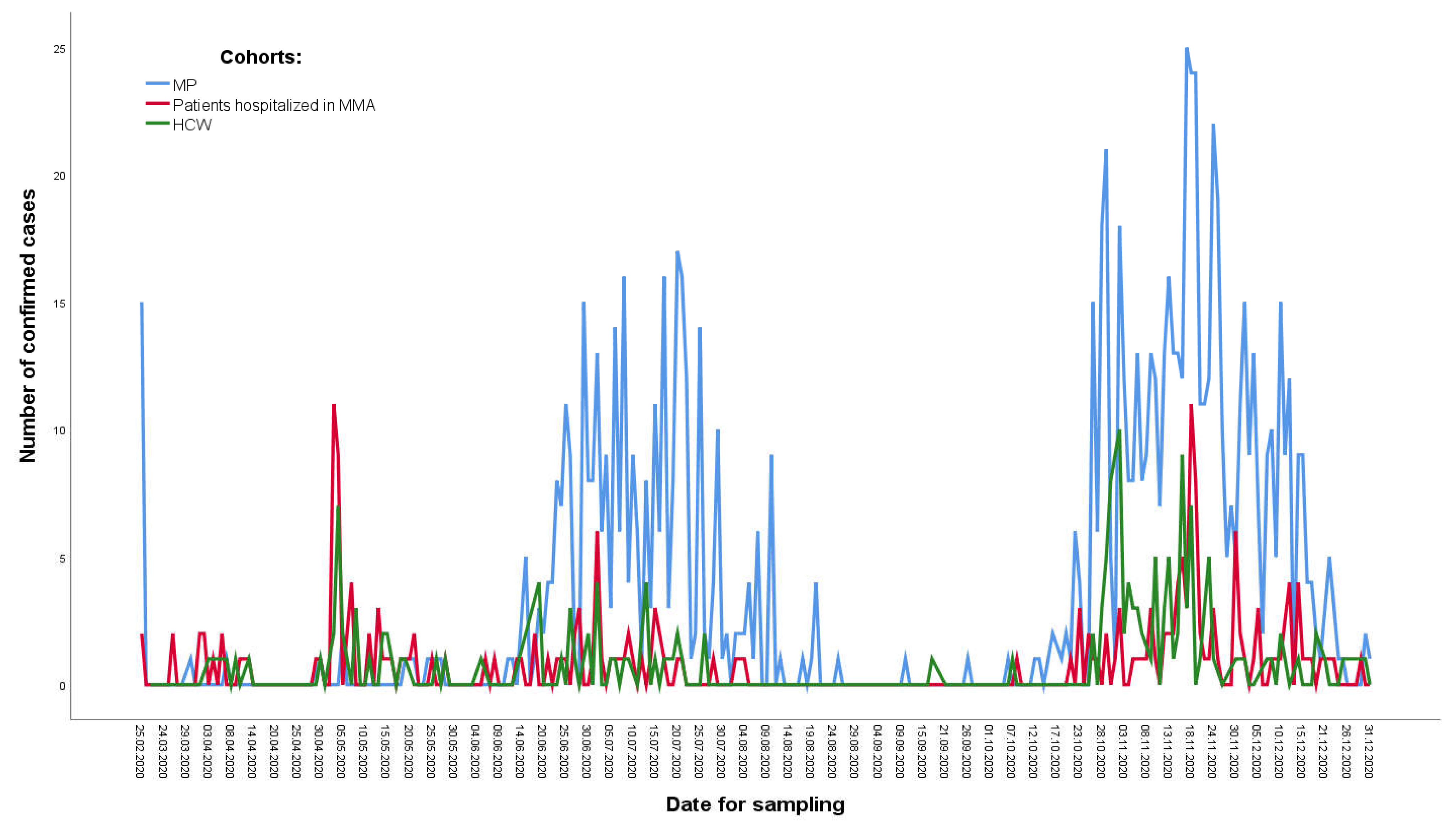
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Coronavirus Disease (COVID-19) Situation Reports. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports (accessed on 28 December 2022).
- Technical Guidance Publications. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance-publications (accessed on 28 December 2022).
- Abbas, M.; Robalo Nunes, T.; Martischang, R.; Zingg, W.; Iten, A.; Pittet, D.; Harbarth, S. Nosocomial Transmission and Outbreaks of Coronavirus Disease 2019: The Need to Protect Both Patients and Healthcare Workers. Antimicrob. Resist. Infect. Control 2021, 10, 7. [Google Scholar] [CrossRef]
- Zhang, M. Estimation of Differential Occupational Risk of COVID-19 by Comparing Risk Factors with Case Data by Occupational Group. Am. J. Ind. Med. 2021, 64, 39–47. [Google Scholar] [CrossRef]
- Escalera-Antezana, J.P.; Mariaca-Cerball, C.A.; Alvarado-Arnez, L.E.; Balderrama-Saavedra, M.A.; Bonilla-Aldana, D.K.; Rodriguez-Morales, A.J. Incidence of SARS-CoV-2/COVID-19 in Military Personnel of Bolivia. BMJ Mil Health 2021, 167, 215–216. [Google Scholar] [CrossRef]
- Segal, D.; Rotschield, J.; Ankory, R.; Kutikov, S.; Moaddi, B.; Verhovsky, G.; Benov, A.; Twig, G.; Glassberg, E.; Fink, N.; et al. Measures to Limit COVID-19 Outbreak Effects Among Military Personnel: Preliminary Data. Mil. Med. 2020, 185, e1624–e1631. [Google Scholar] [CrossRef]
- Professional and Methodological Guidelines to Control the Introduction and Prevention of the Spread of the New Corona Virus SARS-CoV-2 in the Republic of Serbia. Available online: http://demo.paragraf.rs/demo/combined/Old/t/t2020_04/PP_004_2020_002.htm (accessed on 28 December 2022).
- COVID-19. Ministry of Health of Republic of Serbia. Available online: https://covid19.rs/ (accessed on 30 March 2022).
- During the State of Emergency. American Chamber of Commerce in Serbia. Available online: https://www.amcham.rs/combating-covid-19/during-the-state-of-emergency.1112.html (accessed on 30 December 2022).
- Lan, F.-Y.; Filler, R.; Mathew, S.; Buley, J.; Iliaki, E.; Bruno-Murtha, L.A.; Osgood, R.; Christophi, C.A.; Fernandez-Montero, A.; Kales, S.N. COVID-19 Symptoms Predictive of Healthcare Workers’ SARS-CoV-2 PCR Results. PLoS ONE 2020, 15, e0235460. [Google Scholar] [CrossRef]
- Jovanovic, M.; Vukosavljevic, M.; Dincic, D.; Ratkovic, N.; Perisic, N.; Ilic, R.; Lepic, T.; Suljagic, V.; Jadranin, Z.; Lazic, S.; et al. Medical Care of Patients in the Emergency Department of the Military Medical Academy in Belgrade during the Epidemic of COVID-19. VSP 2021, 78, 231–235. [Google Scholar] [CrossRef]
- Li, L.-Q.; Huang, T.; Wang, Y.-Q.; Wang, Z.-P.; Liang, Y.; Huang, T.-B.; Zhang, H.-Y.; Sun, W.; Wang, Y. COVID-19 Patients’ Clinical Characteristics, Discharge Rate, and Fatality Rate of Meta-Analysis. J. Med. Virol. 2020, 92, 577–583. [Google Scholar] [CrossRef]
- Korean Society of Infectious Diseases; Korean Society of Pediatric Infectious Diseases; Korean Society of Epidemiology; Korean Society for Antimicrobial Therapy; Korean Society for Healthcare-Associated Infection Control and Prevention; Korea Centers for Disease Control and Prevention. Report on the Epidemiological Features of Coronavirus Disease 2019 (COVID-19) Outbreak in the Republic of Korea from January 19 to March 2, 2020. J. Korean Med. Sci. 2020, 35, e112. [Google Scholar] [CrossRef]
- Tian, S.; Hu, N.; Lou, J.; Chen, K.; Kang, X.; Xiang, Z.; Chen, H.; Wang, D.; Liu, N.; Liu, D.; et al. Characteristics of COVID-19 Infection in Beijing. J. Infect. 2020, 80, 401–406. [Google Scholar] [CrossRef]
- Stokes, E.K.; Zambrano, L.D.; Anderson, K.N.; Marder, E.P.; Raz, K.M.; El Burai Felix, S.; Tie, Y.; Fullerton, K.E. Coronavirus Disease 2019 Case Surveillance-United States, January 22–May 30, 2020. MMWR Morb. Mortal Wkly. Rep. 2020, 69, 759–765. [Google Scholar] [CrossRef]
- Gebhard, C.; Regitz-Zagrosek, V.; Neuhauser, H.K.; Morgan, R.; Klein, S.L. Impact of Sex and Gender on COVID-19 Outcomes in Europe. Biol. Sex Differ. 2020, 11, 29. [Google Scholar] [CrossRef] [PubMed]
- Balon, B. The Position of Women in the Armed Forces of the Western Balkans; South Eastern and Eastern Europe Clearinghouse for the Control of Small Arms and Light Weapons: Belgrade, Serbia, 2014. [Google Scholar]
- Bradas, S.; Reljanovic, M.; Sekulovic, I. Uticaj Epidemije COVID-19 na Polozaj i Prava Radnica i Radnika u Srbiji [The Impact of the COVID-19 Epidemic on the Position and Rights of Workers in Serbia]; Fondacija Centar za Demokratiju: Belgrade, Serbia, 2020. [Google Scholar]
- Davies, N.G.; Klepac, P.; Liu, Y.; Prem, K.; Jit, M.; CMMID COVID-19 Working Group; Eggo, R.M. Age-Dependent Effects in the Transmission and Control of COVID-19 Epidemics. Nat. Med. 2020, 26, 1205–1211. [Google Scholar] [CrossRef]
- Chinazzi, M.; Davis, J.T.; Ajelli, M.; Gioannini, C.; Litvinova, M.; Merler, S.; Pastore Y Piontti, A.; Mu, K.; Rossi, L.; Sun, K.; et al. The Effect of Travel Restrictions on the Spread of the 2019 Novel Coronavirus (COVID-19) Outbreak. Science 2020, 368, 395–400. [Google Scholar] [CrossRef] [PubMed]
- Online Global Consultation on Contact Tracing for COVID-19, 9–11 June 2020. Available online: https://www.who.int/publications-detail-redirect/online-global-consultation-on-contact-tracing-for-covid-19-9-11-june-2020 (accessed on 30 December 2022).
- Marin-Gomez, F.X.; Fàbregas-Escurriola, M.; Seguí, F.L.; Pérez, E.H.; Camps, M.B.; Peña, J.M.; Comellas, A.R.; Vidal-Alaball, J. Assessing the Likelihood of Contracting COVID-19 Disease Based on a Predictive Tree Model: A Retrospective Cohort Study. PLoS ONE 2021, 16, e0247995. [Google Scholar] [CrossRef] [PubMed]
- Marcus, J.E.; Frankel, D.N.; Pawlak, M.T.; Casey, T.M.; Blackwell, R.S.; Tran, F.V.; Dolan, M.J.; Yun, H.C. COVID-19 Monitoring and Response Among U.S. Air Force Basic Military Trainees-Texas, March-April 2020. MMWR Morb. Mortal Wkly. Rep. 2020, 69, 685–688. [Google Scholar] [CrossRef] [PubMed]
- Tan, K.W.A.; Pong, J.J.J.; Teoh, J.; Wahab, M.T.; Tan, C. COVID-19 Monitoring and Response for Military Bases in Singapore—Perspectives and Lessons from January to June 2020. Mil. Med. 2021. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8690135/ (accessed on 12 January 2023).
- Ebert, T.J.; Dugan, S.; Barta, L.; Gordon, B.; Nguyen-Ho, C.; Pagel, P.S. Clinical Features of COVID-19 Infection in Patients Treated at a Large Veterans Affairs Medical Center. WMJ 2020, 119, 248–252. [Google Scholar] [PubMed]
- Puah, S.H.; Young, B.E.; Chia, P.Y.; Ho, V.K.; Loh, J.; Gokhale, R.S.; Tan, S.Y.; Sewa, D.W.; Kalimuddin, S.; Tan, C.K.; et al. Clinical Features and Predictors of Severity in COVID-19 Patients with Critical Illness in Singapore. Sci. Rep. 2021, 11, 7477. [Google Scholar] [CrossRef]
- Gholami, M.; Fawad, I.; Shadan, S.; Rowaiee, R.; Ghanem, H.; Hassan Khamis, A.; Ho, S.B. COVID-19 and Healthcare Workers: A Systematic Review and Meta-Analysis. Int. J. Infect. Dis. 2021, 104, 335–346. [Google Scholar] [CrossRef]
- Heo, J.; Park, J.A.; Han, D.; Kim, H.-J.; Ahn, D.; Ha, B.; Seog, W.; Park, Y.R. COVID-19 Outcome Prediction and Monitoring Solution for Military Hospitals in South Korea: Development and Evaluation of an Application. J. Med. Internet Res. 2020, 22, e22131. [Google Scholar] [CrossRef]
- Sipetic-Grujicic, S.; Miljus, D.; Soldatovic, I.; Nikolic, A.; Vujcic, I. Prehypertension and Hypertension Prevalence and Risk Factors among Adult Population in Republic of Serbia: A Cross-Sectional Study. VSP 2020, 77, 590–600. [Google Scholar] [CrossRef]
- Ratkovic, N.; Pandrc, M.; Peric, V.; Stojanovic, M.; Rancic, N. Relationship between Plasma High-Sensitivity C-Reactive Protein and Traditional Cardiovascular Risk Factors among Active-Duty Military Personnel in the Republic of Serbia. VSP 2022, 79, 714–723. [Google Scholar] [CrossRef]
- Oxley, T.J.; Mocco, J.; Majidi, S.; Kellner, C.P.; Shoirah, H.; Singh, I.P.; De Leacy, R.A.; Shigematsu, T.; Ladner, T.R.; Yaeger, K.A.; et al. Large-Vessel Stroke as a Presenting Feature of COVID-19 in the Young. N. Engl. J. Med. 2020, 382, e60. [Google Scholar] [CrossRef]
- Taquet, M.; Geddes, J.R.; Husain, M.; Luciano, S.; Harrison, P.J. 6-Month Neurological and Psychiatric Outcomes in 236 379 Survivors of COVID-19: A Retrospective Cohort Study Using Electronic Health Records. Lancet Psychiatry 2021, 8, 416–427. [Google Scholar] [CrossRef]
| Respondents with Positive Test (n = 199) (%) | Respondents with Negative Test (n = 1709) (%) | RR § (95% CI) | ULRA * Crude OR ‡ (95%CI) | ULRA * p | MLRA † Adjusted (95%CI) | MLRA † p | |
|---|---|---|---|---|---|---|---|
| Demographics | |||||||
| Male, n (%) Female, n (%) | 131 (65.8) 68 (34.2) | 1069 (62.6) 640 (37.4) | 10.9/9.6 = 1.14 (0.86–1.50) | 0.86 (0.64–1.18) | 0.365 | / | / |
| Age, median (IQR) | 67 (53–75) | 68 (55–76) | 0.99 (0.99–1.00) | 0.224 | / | / | |
| Exposure risk factors | |||||||
| History of travel in a country with confirmed virus transmission, n (%) | 2 (1.0) | 4 (0.2) | 33.1/10.4 = 3.22 (1.03–10.06) | 4.33 (0.79–23.78) | 0.092 | / | / |
| Treatment in a hospital with COVID-19 cases, n (%) | 40 (20.1) | 153 (9.0) | 20.7/9.3 = 2.23 (1.63–3.06) | 2.56 (1.74–3.76) | <0.001 | 1.51 (0.97–2.36) | 0.067 |
| Contact with known COVID-19 cases within 14 days, n (%) | 52 (26.1) | 176 (10.3) | 22.8/8.8 = 2.60 (1.96–3.46) | 3.08 (2.17–4.38) | <0.001 | 2.56 (1.71–3.83) | <0.001 |
| Clinical signs and symptoms | |||||||
| Fever, n (%) | 116 (58.3) | 688 (40.3) | 14.4/7.5 = 1.92 (1.47–2.51) | 2.07 (1.54–2.79) | <0.001 | 1.89 (1.38–2.59) | <0.001 |
| Sore throat, n (%) | 21 (10.6) | 113 (6.6) | 15.7/10.0 = 1.57 (1.03–2.37) | 1.67 (1.02–2.72) | 0.041 | 1.11 (0.65–1.88) | 0.697 |
| Cough, n (%) | 56 (28.1) | 409 (23.9) | 12.0/9.9 = 1.21 (0.91–1.62) | 1.245 (0.90–1.73) | 0.191 | / | / |
| Headache, n (%) | 33 (16.6) | 176 (10.3) | 15.8/9.8 = 1.61 (1.14–2.28) | 1.73 (1.15–2.60) | 0.008 | 1.35 (0.87–2.09) | 0.176 |
| Myalgia/arthralgia, n (%) | 28 (14.1) | 220 (12.9) | 11.3/10.3 = 1.10 (0.75–1.60) | 1.11 (0.72–1.69) | 0.635 | / | |
| Fatigue, n (%) | 1 (0.5) | 4 (0.2) | 20.0/10.4 = 1.92 (0.33–11.15) | 2.15 (0.24–19.36) | 0.494 | / | / |
| Gastrointestinal symptoms, n (%) | 1 (0.5) | 18 (1.1) | 5.3/10.5 = 0.50 (0.07–3.40) | 0.47 (0.06–3.57) | 0.469 | / | / |
| Pneumonia, n (%) | 51 (25.6) | 284 (16.6) | 15.2/9.4 = 1.62 (1.20–2.17) | 1.73 (1.23–2.44) | 0.002 | 1.46 (1.02–2.09) | 0.041 |
| Comorbidities | |||||||
| No chronic diseases, n (%) | 29 (14.6) | 209 (12.2) | 12.2/10.2 = 1.20 (0.83–1.73) | 1.22 (0.805–1.86) | 0.344 | / | / |
| Chronic cardiac disease, n (%) | 53 (26.6) | 433 (25.5) | 10.9/10.3 = 1.06 (0.79–1.43) | 1.07 (0.77–1.49) | 0.691 | / | / |
| Cardiomyopathy, n (%) | 8 (4.0) | 95 (5.6) | 7.8/10.6 = 0.73 (0.37–1.45) | 0.71 (0.34–1.49) | 0.363 | / | / |
| Hypertension, n (%) | 77 (38.7) | 701 (41.0) | 9.9/10.8 = 0.92 (0.70–1.20) | 0.91 (0.67–1.23) | 0.528 | / | / |
| Chronic pulmonary diseases, n (%) | 22 (11.1) | 192 (11.2) | 10.3/10.4 = 0.98 (0.65–1.50) | 0.98 (0.61–1.57) | 0.940 | / | / |
| Chronic liver diseases, n (%) | 9 (4.5) | 52 (3.0) | 14.8/10.3 = 1.44 (0.77–2.66) | 1.51 (0.73–3.11) | 0.265 | / | / |
| Diabetes mellitus, n (%) | 36 (18.1) | 310 (18.1) | 10.4/10.4 = 1.00 (0.71–1.40) | 0.99 (0.68–1.46) | 0.987 | / | / |
| Neurological diseases, n (%) | 8 (4.0) | 185 (10.8) | 4.1/11.1 = 0.37 (0.19–0.74) | 0.34 (0.17–0.71) | 0.004 | 0.37 (0.18–078) | 0.009 |
| Malignancy, n (%) | 52 (26.1) | 395 (23.1) | 11.6/10.1 = 1.15 (0.86–1.56) | 1.18 (0.84–1.65) | 0.342 | / | / |
| Immunodeficiency, n (%) | 4 (2.0) | 32 (1.9) | 11.1/10.4 = 1.07 (0.42–2.71) | 1.07 (0.38–3.07) | 0.893 | / | / |
| Chronic kidney disease, n (%) | 18 (9.0) | 186 (10.9) | 8.8/10.6 = 0.83 (0.52–1.32) | 0.81 (0.49–1.35) | 0.428 | / | / |
| Characteristics | Respondents with Positive Test (n = 165) (%) | Respondents with Negative Test (n = 871) (%) | RR § (95% CI) | ULRA Crude OR ‡ (95%CI) | ULRA p | MLRA Adjusted OR ‡ (95%CI) | MLRA p |
|---|---|---|---|---|---|---|---|
| Demographics | |||||||
| Male, n (%) Female, n (%) | 61 104 | 290 581 | 17.4/15.2 = 1.14 (0.86–1.53) | 0.85 (0.60–1.20) | 0.361 | / | / |
| Age, median (IQR) | 44 (36–53) | 45 (36–54) | / | 0.99 (0.98–1.01) | 0.618 | / | |
| Exposures risk factors | |||||||
| History of travel in a country with confirmed virus transmission, n (%) | 1 (0.6) | 9 (1.0) | 10.0/16.0 = 0.62 (0.10–4.04) | 0.58 (0.07–4.64) | 0.611 | / | / |
| Treatment in a hospital with COVID-19 cases, n (%) | 51 (30.9) | 311 (35.7) | 14.1/16.9 = 0.83 (0.61–1.13) | 0.81 (0.56–1.15) | 0.237 | / | / |
| Contact with a known COVID-19 case within 14 days, n (%) | 108 (65.5) | 543 (62.3) | 16.6/14.8 = 1.12 (0.83–1.50) | 1.14 (0.81–1.62) | 0.448 | / | / |
| Clinical signs and symptoms | |||||||
| Fever, n (%) | 84 (50.9) | 147 (16.9) | 36.4/10.1 = 3.61 (2.76–4.72) | 5.11 (3.59–7.27) | <0.001 | 2.75 (1.83–4.13) | <0.001 |
| Sore throat, n (%) | 63 (38.2) | 201 (23.1) | 23.9/13.2 = 1.81 (1.36–2.39) | 2.06 (1.45–2.93) | <0.001 | 0.86 (0.56–1.33) | 0.499 |
| Cough, n (%) | 76 (46.1) | 161 (18.5) | 32.1/11.1 = 2.88 (2.20–3.77) | 3.766 (2.65–5.35) | 0.001 | 2.04 (1.32–3.14) | 0.001 |
| Headache, n (%) | 95 (57.6) | 236 (27.1) | 28.7/9.9 = 2.89 (2.18–3.82) | 3.65 (2.59–5.15) | <0.001 | 1.76 (1.15–2.68) | 0.008 |
| Myalgia/arthralgia, n (%) | 88 (53.3) | 196 (22.5) | 31.0/10.2 = 3.03 (2.30–3.98) | 3.94 (2.79–5.56) | <0.001 | 1.58 (1.02–2.45) | 0.039 |
| Fatigue, n (%) | 2 (1.2) | 8 (0.9) | 20.0/15.9 = 1.26 (0.36–4.38) | 1.32 (0.28–6.29) | 0.724 | / | / |
| Gastrointestinal symptoms, n (%) | 5 (3.0) | 3 (0.3) | 62.5/15.6 = 4.02 (2.30–7.00) | 9.04 (2.14–38.21) | 0.003 | 3.38 (0.69–16.44) | 0.132 |
| Pneumonia, n (%) | 2 (1.2) | 5 (0.6) | 28.6/15.8 = 1.80 (0.55–5.87) | 2.14 (0.41–11.05) | 0.370 | / | / |
| Comorbidities | |||||||
| No chronic diseases, n (%) | 115 (69.7) | 555 (63.7) | 17.2/13.7 = 1.26 (0.92–1.71) | 1.31 (0.91–1.88) | 0.142 | / | / |
| Chronic cardiac disease, n (%) | 5 (3.0) | 28 (3.2) | 15.2/16.0 = 0.95 (0.42–2.16) | 0.94 (0.36–2.47) | 0.902 | / | / |
| Cardiomyopathy, n (%) | / | / | 0.0/15.9 = / | / | / | / | / |
| Hypertension, n (%) | 27 (16.4) | 135 (15.5) | 16.7/15.8 = 1.06 (0.72–1.54) | 1.07 (0.68–1.67) | 0.779 | / | / |
| Chronic pulmonary diseases, n (%) | 1 (0.6) | 18 (2.1) | 5.3/16.1 = 0.33 (0.05–2.21) | 0.29 (0.04–2.18) | 0.229 | / | / |
| Chronic liver diseases, n (%) | / | 1 (0.1) | 0.0/15.9 = / | / | 1.000 | / | / |
| Diabetes mellitus, n (%) | 4 (2.4) | 28 (3.2) | 12.5/16.0 = 0.78 (0.31–1.97) | 0.75 (0.26–2.16) | 0.592 | / | / |
| Neurological diseases, n (%) | 1 (0.6) | / | 100.0/15.8 = 6.31 (5.48–7.26) | / | 1.000 | / | / |
| Malignancy, n (%) | 1 (0.6) | 9 (1.0) | 10.0/16.0 = 0.63 (0.10–4.04) | 0.58 (0.07–4.64) | 0.611 | / | / |
| Immunodeficiency, n (%) | / | / | 0.0/15.9 = / | / | 1.000 | / | / |
| Chronic kidney disease, n (%) | / | 1 | 0.0/15.9 = / | / | 1.000 | / | / |
| Characteristics | Respondents with Positive Test (n = 970) (%) | Respondents with Negative Test (n = 2998) (%) | RR § (95% CI) | ULRA Crude OR ‡ (95% CI) | ULRA p | MLRA Adjusted OR ‡ (95% CI) | MLRA p |
|---|---|---|---|---|---|---|---|
| Demographics | |||||||
| Male, n (%) Female, n (%) | 718 252 | 2172 826 | 24.8/23.4 = 1.06 (0.94–1.20) | 0.92 (0.78–1.09) | 0.339 | / | / |
| Age, median (IQR) | 40 (27–51) | 41 (29–51) | / | 0.99 (0.99–1.01) | 0.182 | / | / |
| Exposures risk factors | |||||||
| History of travel in a country with confirmed virus transmission, n (%) | 9 (0.9) | 39 (1.3) | 18.8/24.5 = 0.77 (0.42–1.38) | 0.71 (0.34–1.47) | 0.358 | / | / |
| Treatment in a hospital with COVID-19 cases, n (%) | / | / | / | / | / | / | / |
| Contact with a known COVID-19 case within 14 days, n (%) | 457 (47.1) | 886 (29.6) | 34.0/19.5 = 1.74 (1.56–1.94) | 2.12 (1.83–2.46) | <0.001 | 1.48 (1.25–1.76) | <0.001 |
| Clinical signs and symptoms | |||||||
| Fever, n (%) | 670 (69.1) | 733 (24.4) | 47.8/11.7 = 4.08 (3.62–4.60) | 6.90 (5.88–8.09) | <0.001 | 3.66 (3.04–4.41) | <0.001 |
| Sore throat, n (%) | 369 (38.0) | 576 (19.2) | 39.0/19.9 = 1.96 (1.76–2.19) | 2.58 (2.20–3.02) | <0.001 | 0.93 (0.76–1.13) | 0.443 |
| Cough, n (%) | 501 (51.6) | 614 (20.5) | 44.9/16.4 = 2.74 (2.46–3.04) | 4.15 (3.56–4.84) | <0.001 | 1.91 (1.59–2.30) | <0.001 |
| Headache, n (%) | 519 (53.5) | 712 (23.7) | 42.2/16.5 = 2.56 (2.30–2.85) | 3.70 (3.17–4.30) | <0.001 | 1.24 (1.023–1.50) | 0.028 |
| Myalgia/arthralgia, n (%) | 535 (55.2) | 599 (20.0) | 47.2/15.3 = 3.08 (2.76–3.42) | 4.93 (4.22–5.75) | <0.001 | 2.00 (1.65–2.42) | <0.001 |
| Fatigue, n (%) | 3 (0.3) | 21 (0.7) | 12.5/24.5 = 0.51 (0.18–1.47) | 0.44 (0.13–1.48) | 0.184 | / | / |
| Gastrointestinal symptoms, n (%) | 14 (1.4) | 34 (1.1) | 29.2/24.4 = 1.20 (0.77–1.86) | 1.28 (0.68–2.39) | 0.445 | / | / |
| Pneumonia, n (%) | 6 (0.6) | 22 (0.7) | 21.4/24.5 = 0.88 (0.43–1.78) | 0.84 (0.34–2.08) | 0.710 | / | / |
| Comorbidities | |||||||
| No chronic diseases, n (%) | 693 (71.4) | 2158 (72.0) | 24.3/24.8 = 0.98 (0.87–1.11) | 0.97 (0.83–1.14) | 0.746 | / | / |
| Chronic cardiac disease, n (%) | 28 (2.9) | 67 (2.2) | 29.5/24.3 = 1.21 (0.88–1.66) | 1.30 (0.83–2.03) | 0.250 | / | / |
| Cardiomyopathies, n (%) | / | / | 0.0/24.5 = / | / | / | / | |
| Hypertension, n (%) | 145 (14.9) | 341 (11.4) | 29.8/23.7 = 1.26 (1.08–1.46) | 1.37 (1.11–1.69) | 0.003 | 1.12 (0.88–1.44) | 0.355 |
| Chronic pulmonary diseases, n (%) | 13 (1.3) | 27 (0.9) | 32.5/24.4 = 1.33 (0.85–2.09) | 1.49 (0.77–2.91) | 0.237 | / | / |
| Chronic liver disease, n (%) | / | 2 (0.1) | 0.0/24.5 = / | / | 0.999 | / | / |
| Diabetes mellitus, n (%) | 44 (4.5) | 95 (3.2) | 31.7/24.2 = 1.31 (1.02–1.68) | 1.45 (1.01–2.09) | 0.045 | 0.27 (0.83–1.95) | 0.268 |
| Neurological diseases, n (%) | 4 (0.4) | 7 (0.2) | 36.4/24.4 = 1.49 (0.68–3.26) | 1.77 (0.52–6.06) | 0.363 | / | / |
| Malignancy, n (%) | 16 (1.6) | 73 (2.4) | 18.0/24.6 = 0.73 (0.47–1.14) | 0.67 (0.39–1.16) | 0.154 | / | / |
| Immunodeficiency, n (%) | / | / | 50.0/24.4 = 2.05 (0.51–8.19) | 3.09 (0.19–49.49) | 0.425 | / | / |
| Chronic kidney disease, n (%) | 2 (0.2) | 14 (0.5) | 12.5/24.5 = 0.51 (0.14–1.87) | 0.44 (0.10–1.94) | 0.279 | / | / |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Šuljagić, V.; Đurić-Petković, D.; Lazić, S.; Mladenović, J.; Rakonjac, B.; Opačić, D.; Ljubenović, N.; Milojković, B.; Radojević, K.; Nenezić, I.; et al. Epidemiological Predictors of Positive SARS-CoV-2 Polymerase Chain Reaction Test in Three Cohorts: Hospitalized Patients, Healthcare Workers, and Military Population, Serbia, 2020. Int. J. Environ. Res. Public Health 2023, 20, 3601. https://doi.org/10.3390/ijerph20043601
Šuljagić V, Đurić-Petković D, Lazić S, Mladenović J, Rakonjac B, Opačić D, Ljubenović N, Milojković B, Radojević K, Nenezić I, et al. Epidemiological Predictors of Positive SARS-CoV-2 Polymerase Chain Reaction Test in Three Cohorts: Hospitalized Patients, Healthcare Workers, and Military Population, Serbia, 2020. International Journal of Environmental Research and Public Health. 2023; 20(4):3601. https://doi.org/10.3390/ijerph20043601
Chicago/Turabian StyleŠuljagić, Vesna, Danijela Đurić-Petković, Srđan Lazić, Jovan Mladenović, Bojan Rakonjac, Dolores Opačić, Nenad Ljubenović, Biljana Milojković, Katarina Radojević, Ivana Nenezić, and et al. 2023. "Epidemiological Predictors of Positive SARS-CoV-2 Polymerase Chain Reaction Test in Three Cohorts: Hospitalized Patients, Healthcare Workers, and Military Population, Serbia, 2020" International Journal of Environmental Research and Public Health 20, no. 4: 3601. https://doi.org/10.3390/ijerph20043601
APA StyleŠuljagić, V., Đurić-Petković, D., Lazić, S., Mladenović, J., Rakonjac, B., Opačić, D., Ljubenović, N., Milojković, B., Radojević, K., Nenezić, I., & Rančić, N. (2023). Epidemiological Predictors of Positive SARS-CoV-2 Polymerase Chain Reaction Test in Three Cohorts: Hospitalized Patients, Healthcare Workers, and Military Population, Serbia, 2020. International Journal of Environmental Research and Public Health, 20(4), 3601. https://doi.org/10.3390/ijerph20043601









