Defining the Connotations of Oral Health Literacy Using the Conceptual Composition Method
Abstract
1. Introduction
2. Research Methodology
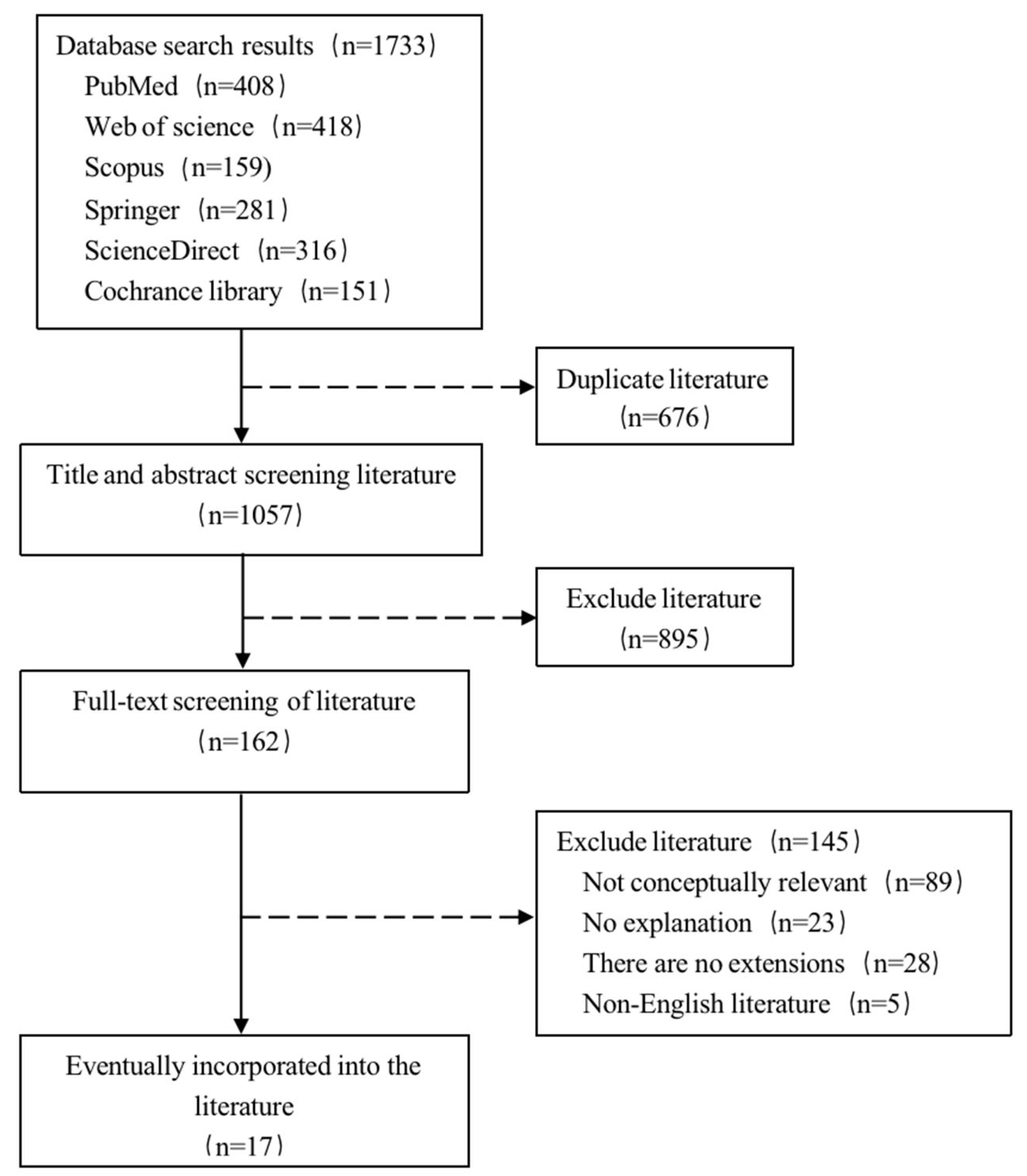
2.1. Search Strategies and Screening Criteria
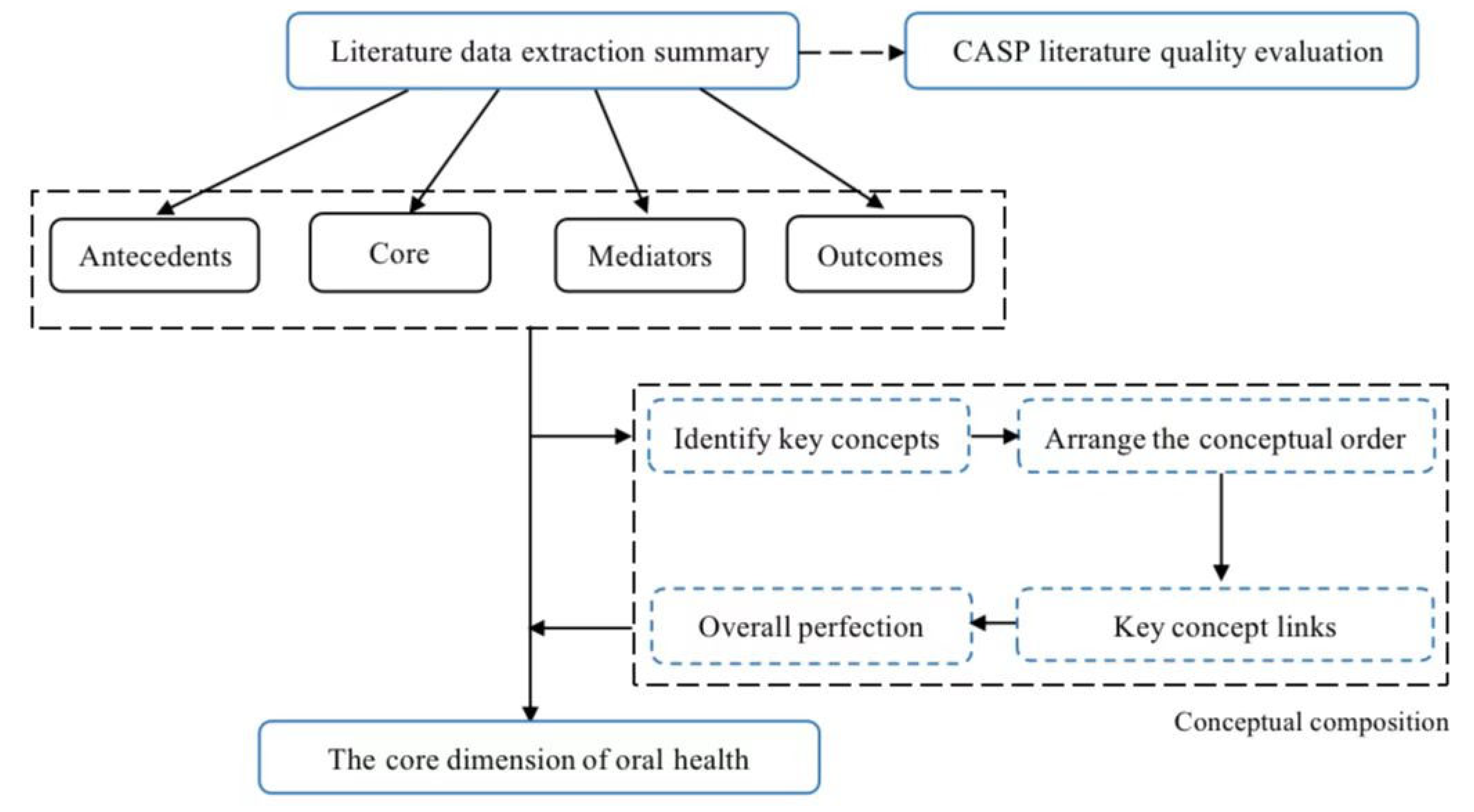
2.2. Conceptual Composition
2.2.1. Clarification of Key Concepts
2.2.2. Order of the Concepts
2.2.3. Links to Key Concepts
2.2.4. Overall Improvement
3. Results
3.1. Basic Information Regarding Inclusion
3.2. Methodological Information Regarding Inclusion
3.3. Antecedents of OHL
3.3.1. Personal Factors
- General characteristics: age, race, gender, education level, income, cultural background, language differences, socioeconomic status, and so on;
- Personality characteristics: attitude, beliefs, psychological characteristics, self-efficacy, a sense of access, and satisfaction with oral health services.
3.3.2. External Factors
- Oral health service providers: communication skills of medical staff;
- Oral medical service system: structure of the oral health service system, social support, patient education, insurance reimbursement, and so on;
- Social factors: community services, social environment, education systems, social activities, government officials, the business sector, public and medical libraries, professional and community groups, and public health actions;
- Personal external factors: family and friends.
3.4. The Core of OHL
3.5. OHL Mediation and Outcomes
3.6. Conceptual Composition Synthesis
3.7. OHL Conceptual Connotations
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Davis, T.C.; Long, S.W.; Jackson, R.H.; Mayeaux, E.J.; George, R.B.; Murphy, P.W.; Crouch, M.A. Rapid Estimate of Adult Literacy in Medicine: A Shortened Screening Instrument. Fam. Med. 1993, 25, 391–395. [Google Scholar]
- Isman, B.; National Institute of Dental and Craniofacial Research (U.S.); Centers for Disease Control and Prevention (U.S.). Healthy People 2010: Oral Health Toolkit; National Institute of Dental and Craniofacial Research: Bethesda, MD, USA, 2000. [Google Scholar]
- Kaur, N.; Kandelman, D.; Nimmon, L.; Potvin, L. Oral Health Literacy: Findings of A Scoping Review. EC Dent. Sci. 2015, 2, 293–306. [Google Scholar]
- Holtzman, J.S.; Atchison, K.A.; Gironda, M.W.; Radbod, R.; Gornbein, J. The association between oral health literacy and failed appointments in adults attending a university-based general dental clinic. Community Dent. Oral Epidemiol. 2014, 42, 263–270. [Google Scholar] [CrossRef]
- Richman, J.A.; Lee, J.Y.; Rozier, R.G.; Gong, D.A.; Pahel, B.T.; Vann, W.F., Jr. Evaluation of a word recognition instrument to test health literacy in dentistry:the REALD-99. J. Public Health Dent. 2007, 67, 99–104. [Google Scholar] [CrossRef]
- Gironda, M.; Der-Martirosian, C.; Messadi, D.; Holtzman, J.; Atchison, K. A brief 20-item dental/medical health literacy screen (REALMD-20). J. Public Health Dent. 2013, 73, 50–55. [Google Scholar] [CrossRef] [PubMed]
- Wanichsaithong, P.; Goodwin, M.; Pretty, I.A. Development and pilot study of an oral health literacy tool for older adults. J. Investig. Clin. Dent. 2019, 10, e12465. [Google Scholar] [CrossRef]
- Macek, M.D.; Haynes, D.; Wells, W.; Bauer-Leffler, S.; Cotten, P.A.; Parker, R.M. Measuring conceptual health knowledge in the context of oral health literacy:preliminary results. J. Public Health Dent. 2010, 70, 197–204. [Google Scholar] [CrossRef]
- Wong, H.; Bridges, S.; Yiu, C.; McGrath, C.; Au, T.; Parthasarathy, D. Validation of the Hong Kong Oral Health Literacy Assessment Task for Paediatric Dentistry (HKOHLAT-P). Intenational J. Paediatr. Dent. 2013, 23, 366–375. [Google Scholar] [CrossRef]
- Service USPH SH The Invisible Barrier: Literacy and Its Relationship with Oral Health. J. Public Health Dent. 2005, 65, 174–182. [CrossRef] [PubMed]
- Lee, J.Y.; Divaris, K.; Baker, A.D.; Rozier, R.G.; Lee, S.Y.D.; Vann, W.F., Jr. Oral health literacy levels among a low-income WIC population. J. Public Health Dent. 2011, 71, 152–160. [Google Scholar] [CrossRef]
- Horn, J.M.; Lee, J.Y.; Divaris, K.; Baker, A.D.; Vann, W.F., Jr. Oral health literacy and knowledge among patients who are pregnant for the first time. J. Am. Dent. Assoc. 2012, 143, 972–980. [Google Scholar]
- McQuistan, M.R.; Qasim, A.; Shao, C.; Straub-Morarend, C.L.; Macek, M.D. Oral health knowledge among elderly patients. J. Am. Dent. Assoc. 2015, 146, 17–26. [Google Scholar] [CrossRef]
- Macek, M.D.; Atchison, K.A.; Chen, H.; Wells, W.; Haynes, D.; Parker, R.M.; Azzo, S. Oral health conceptual knowledge and its relationships with oral health outcomes: Findings from a Multi-site Health Literacy Study. Community Dent. Oral Epidemiol 2017, 45, 323–329. [Google Scholar] [CrossRef]
- Ju, X.; Brennan, D.; Parker, E.; Mills, H.; Kapellas, K.; Jamieson, L. Efficacy of an oral health literacy intervention among Indigenous Australian adults. Community Dent. Oral Epidemiol 2017, 45, 413–426. [Google Scholar] [CrossRef]
- Bridges, S.M.; Parthasarathy, D.S.; Wong, H.M.; Yiu, C.K.; Au, T.K.; McGrath, C.P. The relationship between caregiver functional oral health literacy and child oral health status. Patient Educ. Couns. 2014, 94, 411–416. [Google Scholar] [CrossRef]
- Stein, L.; Bergdahl, M.; Pettersen, K.S.; Bergdahl, J. Effects of the conceptual model of health literacy as a risk: A randomised controlled trial in a clinical dental context. Int. J. Environ. Res. Public Health 2018, 15, 1630. [Google Scholar] [CrossRef]
- Van Wormer, J.J.; Tambe, S.R.; Acharya, A. Oral Health Literacy and Outcomes in Rural Wisconsin Adults. J. Rural Health 2019, 35, 12–21. [Google Scholar] [CrossRef]
- Mohammadi, T.M.; Malekmohammadi, M.; Hajizamani, H.R.; Mahani, S.A. Oral health literacy and its determinants among adults in Southeast Iran. Eur. J. Dent. 2018, 12, 439–442. [Google Scholar] [CrossRef]
- Baskaradoss, J.K. Relationship between oral health literacy and oral health status. BMC Oral Health 2018, 18, 172. [Google Scholar] [CrossRef]
- Márquez-Arrico, C.F.; Almerich-Silla, J.M.; Montiel-Company, J.M. Oral health knowledge in relation to educational level in an adult population in Spain. J. Clin. Exp. Dent. 2019, 11, e1143–e1150. [Google Scholar] [CrossRef]
- Tenani, C.F.; De Checchi, M.H.R.; Bado, F.M.R.; Ju, X.; Jamieson, L.; Mialhe, F.L. Influence of oral health literacy on dissatisfaction with oral health among older people. Gerodontology 2019, 37, 46–52. [Google Scholar] [CrossRef] [PubMed]
- Spivakovsky, S.E.; Katz, R.V. Development of the knowledge related to oral health literacy for Spanish speakers scale. Hisp. Health Care Int. 2020, 18, 198–204. [Google Scholar] [CrossRef] [PubMed]

| Serial Number | Author (Year) | Research Objectives | Target Demographics | Oral Health Literacy (OHL) Definition or Interpretation in Relevant Studies |
|---|---|---|---|---|
| 1 | U.S. Department of Health and Human Services (2000) [2] | Provide guidance, technical tools, and resources for the development of countries, territories, tribes, and communities to help them implement the 2010 Human Health Plan and other oral health plans | General population | OHL is the degree to which an individual has the ability to access, process, and understand basic oral health information and access and understand basic oral health services needed to make appropriate health decisions |
| 2 | Service USPH SH (2005) [10] | Define OHL and provide a framework for studying the relationship between OHL and other intervention points to improve oral health | General population | Individuals can access, process, and understand essential oral health information and access and understand essential oral health services to make appropriate health decisions and take action |
| 3 | Macek et al. (2010) [8] | Measure conceptual health knowledge in the context of OHL | Low-income adults | OHL includes four abilities: word recognition, reading comprehension, communication skills, and conceptual knowledge. Oral health conceptual knowledge includes basic knowledge on oral health and the prevention and management of caries, periodontal disease, and oral cancer |
| 4 | Lee et al. (2011) [11] | Identify OHL levels for low-income women, infants, and children and explore whether there are racial disparities | Low-income women, infants, and children | OHL is the degree to which an individual has the ability to access, process, and understand basic oral health information and access and understand basic oral health services needed to make appropriate health decisions (the definition proposed by Healthy People 2010 in 2000 was adopted) |
| 5 | Horn et al. (2012) [12] | Determine the correlation between OHL levels and oral health knowledge among low-income patients undergoing first-time pregnancies | Low-income patients undergoing first-time pregnancies | Using the definition cited above and proposed by Healthy People 2010 in 2000, it can be concluded that oral health knowledge correlates significantly with OHL levels |
| 6 | Kaur et al. (2015) [3] | (1) How do we assess oral health knowledge?(2) What is the relationship between oral health knowledge, oral health outcomes, and access to and satisfaction with dental health services? (3) What interventions are in place for vulnerable populations with low OHL? | General population | Although not mentioned, the moderators and outcomes of the connotations of the concept of OHL were further explained and extended |
| 7 | McQuistan et al. (2015) [13] | Understand the level of oral health knowledge in older adults aged 65 and older | Seniors (65 and older) | The definition proposed by Healthy People 2010 in 2000 (cited previously) was adopted |
| 8 | Macek et al. (2017) [14] | Extend previous work by using larger study samples and additional outcome variables | Adults | Although not mentioned, the study provides additional support for the effectiveness of the Comprehensive Measure of Oral Health Knowledge (CMOHK). Researchers were encouraged to incorporate knowledge on oral health concepts into their theoretical frameworks, especially regarding beliefs and self-efficacy. Key observational indicators in this study included dental use, self-efficacy, and dental beliefs and attitudes |
| 9 | Ju et al. (2017) [15] | Determine the effect of the OHL intervention on OHL-related outcomes among Australian Aboriginal adults living in rural areas | Aboriginal Australian adults living in rural areas | Although not mentioned, the study was partially successful in the functional, targeted improvement of OHL and the OHL-related outcomes of OHL interventions |
| 10 | Bridges et al. (2014) [16] | Describe the relationship between caregivers and children’s oral health | Children’s caregivers | As described previously, OHL is the degree to which an individual has the ability to access, process, and understand basic oral health information and access and understand basic oral health services needed to make appropriate health decisions (the definition proposed by Healthy People 2010 in 2000 was adopted) |
| 11 | Stein et al. (2018) [17] | Examine the role of the health literacy conceptual model in a clinical stomatology setting | Norwegian-speaking adults | The definition proposed by Healthy People 2010 in 2000 was adopted (cited above) |
| 12 | Van Wormer et al. (2019) [18] | Study the relationship between OHL, sociodemographic factors, and several oral health outcomes when rural adults receive integrated medical and dental care services | Rural adults | The comprehensive conceptual model of health literacy proposed by Sorann et al. was adopted and applied to the context of OHL. This conceptual model synthesized the main health literacy dimensions developed in the previous model (e.g., access to and understanding and application of health information, including the antecedents and consequences of health literacy) |
| 13 | Mohammadi et al. (2018) [19] | Assess adults’ OHL levels and their associated factors | Adults | The level of an individual’s ability to process and understand basic information about oral health and related services (the definition proposed by Healthy People in 2010 was adopted) |
| 14 | Baskaradoss (2018) [20] | Explore the relationship between OHL and oral health | Stomatology patients | Although not mentioned, the study found that subjects with limited levels of OHL had poorer periodontal health. Improving a patient’s OHL level may help improve compliance with physicians’ orders, self-management skills, and overall treatment outcomes |
| 15 | Márquez-Arrico et al. (2019) [21] | Analyze the relationship between oral health knowledge and literacy, oral hygiene habits, eating habits, and oral health-related quality of life among adults in Spain | Adults in Spain | The level of an individual’s ability to process and understand basic information regarding oral health and related services (the definition proposed by Healthy People in 2010 was adopted) |
| 16 | Tenani et al. (2019) [22] | Explore the effects of OHL and its related factors on oral health dissatisfaction among older adults | Senior citizens | Individuals can access, process, and understand essential oral health information and access and understasnd essential oral health services to make appropriate health decisions and take action (2005 National Institute of Dental and Craniofacial Research (NIDCR) definition of OHL) |
| 17 | Spivakovsky et al. (2020) [23] | Introduce the OHL scale for Spanish speakers and understand the factors that affect the oral health of Spanish speakers | Spanish speakers | OHL-related knowledge is influenced by socioeconomic characteristics, beliefs, self-efficacy, previous experiences, etc. and ultimately affects oral health outcomes |
| Serial Number | Author (Year) | Research Methodology |
|---|---|---|
| 1 | U.S. Department of Health and Human Services (2000) [2] | Based on the definition of health literacy and application of that definition to the context of OHL (theoretical construction). |
| 2 | Service USPH SH (2005) [10] | Adoption of the definition proposed by Healthy People 2010 in 2000, explaining and extending it (cross-sectional study) |
| 3 | Macek et al. (2010) [8] | Panel discussions |
| 4 | Lee et al. (2011) [11] | Face-to-face interviews |
| 5 | Horn et al. (2012) [12] | Face-to-face interviews |
| 6 | Kaur et al. (2015) [3] | Scoping review |
| 7 | McQuistan et al. (2015) [13] | Interviews |
| 8 | Macek et al. (2017) [14] | Cross-sectional studies |
| 9 | Ju et al. (2017) [15] | Randomized controlled trials |
| 10 | Bridges et al. (2014) [16] | Face-to-face interviews |
| 11 | Stein et al. (2018) [17] | Randomized controlled trials |
| 12 | Van Wormer et al. (2019) [18] | Cross-sectional studies |
| 13 | Mohammadi et al. (2018) [19] | Cross-sectional studies |
| 14 | Baskaradoss (2018) [20] | Cross-sectional studies |
| 15 | Márquez-Arrico et al. (2019) [21] | Cross-sectional studies |
| 16 | Tenani et al. (2019) [22] | Cross-sectional studies |
| 17 | Spivakovsky et al. (2020) [23] | Theoretical construction |
| Serial Number | Author (Year) | Moderators | Attributes | Mediation | Outcomes |
|---|---|---|---|---|---|
| 1 | U.S. Department of Health and Human Services (2000) [2] | Ability to obtain information, information processing ability, information comprehension skills, information decision-making skills | |||
| 2 | Service USPH SH (2005) [10] | External factors: health service providers, researchers, educators, policymakers, government officials, the business sector, public and medical libraries, professional and community groups | Reading and writing abilities, listening, oral expression ability, information acquisition ability, information processing ability, information comprehension ability, information decision-making ability | Oral health awareness | |
| 3 | Macek et al. (2010) [8] | Text recognition ability, reading comprehension ability, communication skills, decision-making ability Conceptual knowledge: (a) basic knowledge of oral health (b) prevention and management of tooth decay (c) prevention and management of periodontal disease (d) prevention and management of oral cancer | |||
| 4 | Lee et al. (2011) [11] | Personal factors: race | |||
| 5 | Horn et al. (2012) [12] | Personal factors: knowledge External factors: cultural and linguistic differences, insurance reimbursement status | Knowledge | ||
| 6 | Kaur et al. (2015) [3] | Personal factors: oral health knowledge External factors: access to and satisfaction with oral health services | Ability to obtain information, information processing capabilities, information comprehension ability, information decision-making skills | Oral health behaviors | Oral health |
| 7 | McQuistan et al. (2015) [13] | Personal factors: income level, age, education, socioeconomic status, oral hygiene practices | Reading ability, writing skills | Oral health awareness | |
| 8 | Macek et al. (2017) [14] | Personal factors: beliefs, attitudes | Oral conceptual knowledge, self-efficacy | ||
| 9 | Ju et al. (2017) [15] | Race, education level, age, occupation, income, social support, culture, language, self-efficacy, beliefs, motivation, media, oral health education | Vision, hearing, language skills, memory, reasoning skills, knowledge, communication skills | ||
| 10 | Bridges et al. (2014) [16] | External factors: community, public health education, family | Literacy, comprehension ability | ||
| 11 | Stein et al. (2018) [17] | Changes in personal behavior Public health is universal Public health action | Knowledge, communication skills, self-management ability, motivational ability | Gum condition, oral hygiene | |
| 12 | Van Wormer et al. (2019) [18] | Personal factors: education level, oral health information sources, age | Oral hygiene practices | Oral hygiene status | |
| 13 | Mohammadi et al. (2018) [19] | Personal factors: socioeconomic status, ethnicity, annual household income | Quality of life, oral diseases | ||
| 14 | Baskaradoss (2018) [20] | Personal factors: ethnicity, socioeconomic status | Oral health behaviors | Oral health | |
| 15 | Márquez-Arrico et al. (2019) [21] | Personal factors: education level, age, gender | Oral health-related quality of life | ||
| 16 | Tenani et al. (2019) [22] | Socioeconomic variables | Oral health | ||
| 17 | Spivakovsky et al. (2020) [23] | Socioeconomic characteristics, beliefs, self-efficacy, etc. Previous experience | Oral conceptual knowledge, resource utilization capabilities |
| Incorporated Concepts | Weight Coefficients |
|---|---|
| Basic skills | 0.309 |
| Information-related capabilities | 0.225 |
| Oral health maintenance ability | 0.135 |
| Personal factors | 0.129 |
| External factors | 0.084 |
| Oral health behaviors | 0.061 |
| Oral health status | 0.057 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tian, Z.; Wang, Y.; Li, Y.; Lu, J.; Song, L.; Ding, L.; Guo, X.; Zheng, J. Defining the Connotations of Oral Health Literacy Using the Conceptual Composition Method. Int. J. Environ. Res. Public Health 2023, 20, 3518. https://doi.org/10.3390/ijerph20043518
Tian Z, Wang Y, Li Y, Lu J, Song L, Ding L, Guo X, Zheng J. Defining the Connotations of Oral Health Literacy Using the Conceptual Composition Method. International Journal of Environmental Research and Public Health. 2023; 20(4):3518. https://doi.org/10.3390/ijerph20043518
Chicago/Turabian StyleTian, Zhiqiang, Yanjun Wang, Yang Li, Jiao Lu, Li Song, Ling Ding, Xinyu Guo, and Jianzhong Zheng. 2023. "Defining the Connotations of Oral Health Literacy Using the Conceptual Composition Method" International Journal of Environmental Research and Public Health 20, no. 4: 3518. https://doi.org/10.3390/ijerph20043518
APA StyleTian, Z., Wang, Y., Li, Y., Lu, J., Song, L., Ding, L., Guo, X., & Zheng, J. (2023). Defining the Connotations of Oral Health Literacy Using the Conceptual Composition Method. International Journal of Environmental Research and Public Health, 20(4), 3518. https://doi.org/10.3390/ijerph20043518





