Deep Sedation for Dental Care Management in Healthy and Special Health Care Needs Children: A Retrospective Study
Abstract
1. Introduction
2. Materials and Methods
- A.
- Demographic data: age and sex.
- B.
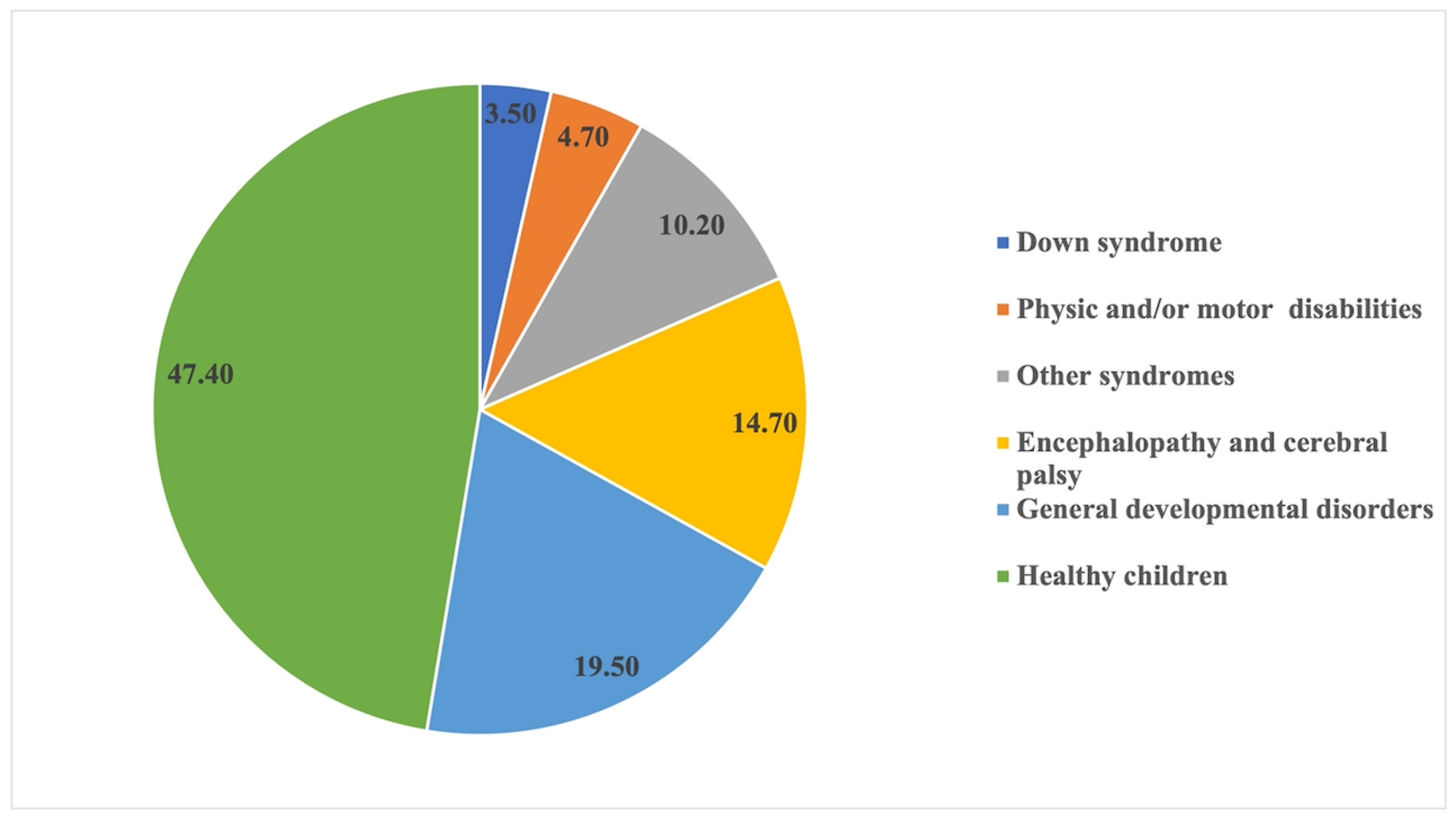
- Systemic health status, differentiating between healthy children and those with SHCN.
- C.
- Reason for sedation.
- D.
- Assessment of oral health status prior to the intervention:
- −
- Hygiene habits. The child was considered to have a hygiene habit when regularly brushing a minimum of twice a day.
- −
- Plaque on visual inspection (Yes or No).
- −
- Calculus on visual inspection (Yes or No).
- −
- Caries and number of teeth affected. Caries was defined as the loss of enamel integrity (ICDAS 3, 4, 5).
- −
- Pulp involvement and number of teeth affected. ICDAS 6 lesions, night pain, radiolucent image on X-rays, and abscesses were considered pulp involvement.
- −
- Root debris on visual inspection and number.
- −
- Teeth lost to dental pathology on visual inspection (number).
- A.
- Treatments carried out.
- −
- Obturation.
- −
- Direct pulp protection.
- −
- Pulpotomy.
- −
- Pulpectomy.
- −
- Endodontics.
- −
- Apexification.
- −
- Calculus removal.
- −
- Scaling and root planing.
- −
- Application of fluoride.
- −
- Exodontias.
- B.
- The number of teeth treated.
- A.
- Attended checkup (Yes or No)
- B.
- Plaque on visual inspection (Yes or No)
- C.
- Need for medication for oral pathology (Yes or No)
- D.
- Improved eating (Yes or No)
- Does the child have frequent pain in the mouth?
- Have they woken at night due to dental pain?
- Has this prevented them from carrying out their usual daily routine?
- Has the child taken medication due to dental problems?
- Does the child have difficulty eating meat?
- Does the child have difficulty eating cold food?
- Does the child have difficulty eating hot food?
- Does the child feel discomfort about the appearance of their teeth?
- When brushing the teeth, does the child complain of pain?
- Does the child have difficulty eating meat?
- Does the child have difficulty eating cold food?
- Does the child have difficulty eating hot food?
- Does the child eat better after the intervention?
- Has the child gained weight during this time?
- Does the child feel discomfort when brushing their teeth?
- Is the child more rested and less irascible?
- Is the child happy with their teeth?
- Has treatment under deep sedation met your expectations?
Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Definition of Special Health Care Needs. Available online: https://www.aapd.org/research/oral-health-policies--recommendations/special-health-care-needs/ (accessed on 14 December 2022).
- Overview. Available online: https://www.aapd.org/research/oral-health-policies--recommendations/behavior-guidance-for-the-pediatric-dental-patient/ (accessed on 14 December 2022).
- AAPD|Use of Anesthesia Providers in the Administration of Office-Based Deep Sedation/General Anesthesia to the Pediatric Dental Patient. Available online: https://www.aapd.org/research/oral-health-policies--recommendations/use-of-anesthesia-providers-in-the-administration-of-office-based-deep-sedationgeneral-anesthesia-to-the-pediatric-dental-patient/ (accessed on 14 December 2022).
- Glassman, P.; Caputo, A.; Dougherty, N.; Lyons, R.; Messieha, Z.; Miller, C.; Peltier, B.; Romer, M. Special Care Dentistry Association Special Care Dentistry Association Consensus Statement on Sedation, Anesthesia, and Alternative Techniques for People with Special Needs. Spec. Care Dent. 2009, 29, 2–8. [Google Scholar] [CrossRef]
- Lim, M.A.W.T.; Borromeo, G.L. The Use of General Anesthesia to Facilitate Dental Treatment in Adult Patients with Special Needs. J. Dent. Anesth. Pain Med. 2017, 17, 91–103. [Google Scholar] [CrossRef]
- Corcuera-Flores, J.-R.; Delgado-Muñoz, J.-M.; Ruiz-Villandiego, J.-C.; Maura-Solivellas, I.; Machuca-Portillo, G. Dental Treatment for Handicapped Patients; Sedation vs General Anesthesia and Update of Dental Treatment in Patients with Different Diseases. Med. Oral Patol. Oral Cir. Bucal 2014, 19, e170–e176. [Google Scholar] [CrossRef]
- Guney, S.E.; Araz, C.; Tirali, R.E.; Cehreli, S.B. Dental Anxiety and Oral Health-Related Quality of Life in Children Following Dental Rehabilitation under General Anesthesia or Intravenous Sedation: A Prospective Cross-Sectional Study. Niger. J. Clin. Pract. 2018, 21, 1304–1310. [Google Scholar] [CrossRef]
- Spera, A.L.; Saxen, M.A.; Yepes, J.F.; Jones, J.E.; Sanders, B.J. Office-Based Anesthesia: Safety and Outcomes in Pediatric Dental Patients. Anesth. Prog. 2017, 64, 144–152. [Google Scholar] [CrossRef]
- Rashewsky, S.; Parameswaran, A.; Sloane, C.; Ferguson, F.; Epstein, R. Time and Cost Analysis: Pediatric Dental Rehabilitation with General Anesthesia in the Office and the Hospital Settings. Anesth. Prog. 2012, 59, 147–153. [Google Scholar] [CrossRef]
- Lee, H.; Milgrom, P.; Huebner, C.E.; Weinstein, P.; Burke, W.; Blacksher, E.; Lantos, J.D. Ethics Rounds: Death After Pediatric Dental Anesthesia: An Avoidable Tragedy? Pediatrics 2017, 140, e20172370. [Google Scholar] [CrossRef]
- Knapp, R.; Gilchrist, F.; Rodd, H.D.; Marshman, Z. Change in Children’s Oral Health-Related Quality of Life Following Dental Treatment under General Anaesthesia for the Management of Dental Caries: A Systematic Review. Int. J. Paediatr. Dent. 2017, 27, 302–312. [Google Scholar] [CrossRef]
- Sischo, L.; Broder, H.L. Oral Health-Related Quality of Life: What, Why, How, and Future Implications. J. Dent. Res. 2011, 90, 1264–1270. [Google Scholar] [CrossRef]
- Park, J.S.; Anthonappa, R.P.; King, N.M.; McGrath, C.P. The Family Impact of Dental General Anaesthesia in Children: A Meta-Analysis. Int. J. Paediatr. Dent. 2018, 29, 149–161. [Google Scholar] [CrossRef]
- Guidry, J.; Bagher, S.; Felemban, O.; Rich, A.; Loo, C. Reasons of Repeat Dental Treatment under General Anaesthesia: A Retrospective Study. Eur. J. Paediatr. Dent. 2017, 18, 313–318. [Google Scholar] [CrossRef]
- Al-Eheideb, A.A.; Herman, N.G. Outcomes of Dental Procedures Performed on Children under General Anesthesia. J. Clin. Pediatr. Dent. 2003, 27, 181–183. [Google Scholar] [CrossRef]
- Al-Ogayyel, S.; Al-Haj Ali, S. Comparison of Dental Treatment Performed under General Anesthesia between Healthy Children and Children with Special Health Care Needs in a Hospital Setting, Saudi Arabia. J. Clin. Exp. Dent. 2018, 10, e963–e969. [Google Scholar] [CrossRef]
- Ciftci, V.; Yazicioglu, İ. A Retrospective Comparison of Dental Treatment under General Anesthesia Provided for Uncooperative Healthy Patients and Patients with Special Health Care Needs. J. Clin. Pediatr. Dent. 2020, 44, 196–201. [Google Scholar] [CrossRef]
- Tahmassebi, J.F.; Achol, L.T.; Fayle, S.A. Analysis of Dental Care of Children Receiving Comprehensive Care under General Anaesthesia at a Teaching Hospital in England. Eur. Arch. Paediatr. Dent. 2014, 15, 353–360. [Google Scholar] [CrossRef]
- Barberia, E.; Arenas, M.; Gómez, B.; Saavedra-Ontiveros, D. An Audit of Paediatric Dental Treatments Carried out under General Anaesthesia in a Sample of Spanish Patients. Community Dent. Health 2007, 24, 55–58. [Google Scholar]
- König, T.; Reicherts, P.; Leha, A.; Hrasky, V.; Wiegand, A. Retrospective Study on Risk Factors for Repeated Dental Treatment of Children under General Anaesthesia. Eur. J. Paediatr. Dent. 2020, 21, 183–186. [Google Scholar] [CrossRef]
- Treuner, A.; Splieth, C.H. Prevención de la caries en la primera infancia. Quintessence Publ. Int. Odontol. 2012, 25, 229–235. [Google Scholar]
- Martignon, S.; Pitts, N.B.; Goffin, G.; Mazevet, M.; Douglas, G.V.A.; Newton, J.T.; Twetman, S.; Deery, C.; Doméjean, S.; Jablonski-Momeni, A.; et al. CariesCare Practice Guide: Consensus on Evidence into Practice. Br. Dent. J. 2019, 227, 353–362. [Google Scholar] [CrossRef]
- Vandenbroucke, J.P.; von Elm, E.; Altman, D.G.; Gøtzsche, P.C.; Mulrow, C.D.; Pocock, S.J.; Poole, C.; Schlesselman, J.J.; Egger, M. STROBE Initiative Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and Elaboration. Int. J. Surg. 2014, 12, 1500–1524. [Google Scholar] [CrossRef]
- Bader, R.M.; Song, G.; Almuhtaseb, E.Y. A Retrospective Study of Paediatric Dental Patients Treated under General Anesthesia. Int. J. Clin. Med. 2013, 4, 18–23. [Google Scholar] [CrossRef]
- Olley, R.C.; Hosey, M.T.; Renton, T.; Gallagher, J. Why Are Children Still Having Preventable Extractions under General Anaesthetic? A Service Evaluation of the Views of Parents of a High Caries Risk Group of Children. Br. Dent. J. 2011, 210, E13. [Google Scholar] [CrossRef]
- Tsai, C.-L.; Tsai, Y.-L.; Lin, Y.-T.; Lin, Y.-T. A Retrospective Study of Dental Treatment under General Anesthesia of Children with or without a Chronic Illness and/or a Disability. Chang Gung Med. J. 2006, 29, 412–418. [Google Scholar]
- Razeghi, S.; Amiri, P.; Mohebbi, S.Z.; Kharazifard, M.J. Impact of Health Promotion Interventions on Early Childhood Caries Prevention in Children Aged 2-5 Years Receiving Dental Treatment Under General Anesthesia. Front. Public Health 2020, 8, 6. [Google Scholar] [CrossRef]
- Elkhadem, A.; Nagi, P.; Abdel-Ghany, M. Pediatric Dentist Accessibility and Post-Operative Complications of Laryngeal Mask Airway versus Nasotracheal Intubation in Full Mouth Rehabilitation under General Anaesthesia: A Randomised Controlled Trial. Egypt. Dent. J. 2020, 66, 17–25. [Google Scholar] [CrossRef]
- Consejería de Salud de la Región de Murcia. Evaluación del Programa de Salud Bucodental Infantil de la Región de Murcia 2014. Available online: http://www.murciasalud.es/publicaciones.php?op=mostrar_publicacion&id=2321&idsec=88 (accessed on 6 November 2022).
- World Health Organization Ending Childhood Dental Caries: WHO Implementation Manual; World Health Organization: Geneva, Switzerland, 2019; ISBN 978-92-4-000005-6.
- Cortiñas-Saenz, M.; Martínez-Gómez, L.; Roncero-Goig, M.; Saez-Cuesta, U.; Ibarra-Martin, M. Results of a Major Ambulatory Oral Surgery Program Using General Inhalational Anesthesia on Disabled Patients. Med. Oral Patol. Oral Cir. Bucal 2009, 14, e605–e611. [Google Scholar] [CrossRef]
- Savanheimo, N.; Vehkalahti, M.M. Preventive Aspects in Children’s Caries Treatments Preceding Dental Care under General Anaesthesia. Int. J. Paediatr. Dent. 2008, 18, 117–123. [Google Scholar] [CrossRef]
- de la Fuente González, D.S. Análisis Del Estado de Salud Oral Y Necesidades de Tratamiento en Dos Grupos de Escolares, Uno Con Discapacidad, en Dos Zonas Periurbanas de la CAM. Ph.D. Thesis, Universidad Complutense de Madrid, Madrid, Spain, 2015. [Google Scholar]
- Schüler, I.M.; Bock, B.; Heinrich-Weltzien, R.; Bekes, K.; Rudovsky, M.; Filz, C.; Ligges, C. Status and Perception of Oral Health in 6–17-Year-Old Psychiatric Inpatients-Randomized Controlled Trial. Clin. Oral Investig. 2017, 21, 2749–2759. [Google Scholar] [CrossRef]
- Shyama, M.; Al-Mutawa, S.A.; Morris, R.E.; Sugathan, T.; Honkala, E. Dental Caries Experience of Disabled Children and Young Adults in Kuwait. Community Dent. Health 2001, 18, 181–186. [Google Scholar]
- Mallineni, S.K.; Yiu, C.K.Y. A Retrospective Review of Outcomes of Dental Treatment Performed for Special Needs Patients under General Anaesthesia: 2-Year Follow-Up. Sci. World J. 2014, 2014, 748353. [Google Scholar] [CrossRef]
- Stanková, M.; Buček, A.; Dostálová, T.; Ginzelová, K.; Pacáková, Z.; Seydlová, M. Patients with Special Needs within Treatment under General Anesthesia—Meta-Analysis. Prague Med. Rep. 2011, 112, 216–225. [Google Scholar] [PubMed]
- American Academy of Pediatric Dentistry. Management of Dental Patients with Special Health Care Needs. In The Reference Manual of Pediatric Dentistry; American Academy of Pediatric Dentistry: Chicago, IL, USA, 2022; pp. 302–309. [Google Scholar]
- Mallineni, S.K.; Yiu, C.K.Y. A Retrospective Audit of Dental Treatment Provided to Special Needs Patients under General Anesthesia During a Ten-Year Period. J. Clin. Pediatr. Dent. 2018, 42, 155–160. [Google Scholar] [CrossRef]
- Schnabl, D.; Schanner, L.L.; Barbieri, F.; Laimer, J.; Bruckmoser, E.; Steiner, R.; Grunert, I. Is Dental General Anaesthesia in Children an Outdated Concept? A Retrospective Analysis. Eur. J. Paediatr. Dent. 2020, 21, 283–286. [Google Scholar] [CrossRef] [PubMed]
- Linas, N.; Decerle, N.; Munoz-Sanchez, M.-L.; Faulks, D.; Collado, V.; Nicolas, E.; Hennequin, M.; Cousson, P.-Y. Long-Term Outcomes of Full Pulpotomy in Permanent Molars for Patients Treated in a Single, Short Session under Special Conditions. J. Endod. 2020, 46, 1597–1604. [Google Scholar] [CrossRef] [PubMed]
- López-Velasco, A.; Puche-Torres, M.; Carrera-Hueso, F.J.; Silvestre, F.-J. General Anesthesia for Oral and Dental Care in Paediatric Patients with Special Needs: A Systematic Review. J. Clin. Exp. Dent. 2021, 13, e303–e312. [Google Scholar] [CrossRef]
- Ferrazzano, G.F.; Sangianantoni, S.; Mitrano, R.L.; Ingenito, A.; Alcidi, B.; Cantile, T. Assessing Changes in Oral Health-Related Quality of Life and Body Growth in 3-5 Years Old Children Following Dental Treatment under General Anaesthesia Due to Severe Dental Caries. Eur. J. Paediatr. Dent. 2019, 20, 214–218. [Google Scholar] [CrossRef]
- Boukhobza, S.; Stamm, T.; Glatthor, J.; Meißner, N.; Bekes, K. Changes in Oral Health-Related Quality of Life among Austrian Preschool Children Following Dental Treatment under General Anaesthesia. Clin. Oral Investig. 2021, 25, 2821–2826. [Google Scholar] [CrossRef]
| Total (100%) | Healthy (47.4%) | SHCN (52.6%) | p-Value | |
|---|---|---|---|---|
| Tooth brushing habit | 20.43% | 17.43% | 23.14% | =0.36 † |
| Plaque | 90.86% | 93.57% | 89.25% | =0.35 † |
| Calculus | 31.30% | 7.33% | 52.89% | <0.001 † |
| Caries | 90.87% | 93.57% | 88.43% | =0.26 † |
| Pulp involvement | 67.83% | 78.90% | 57.85% | =0.001 † |
| Root remains | 13.91% | 10.09% | 17.36% | =0.16 † |
| Missing Teeth | 4.34% | 4.58% | 4.13% | =1 * |
| Number of teeth with caries per child (mean ± SD) | 6.78 ± 4.65 | 7.49 ± 4.68 | 6.13 ± 4.54 | <0.05 ‡ |
| Number of teeth with pulp involvement per child (mean ± SD) | 1.84 ± 2.04 | 2.25 ± 2.01 | 1.47 ± 2.00 | =0.004 ‡ |
| Number of missing teeth per child (mean ± SD) | 0.10 ± 0.84 | 0.045 ± 0.21 | 0.16 ± 1.14 | =0.005 ‡ |
| Total (100%) | Healthy (47.4%) | SHCN (52.6%) | |||||
|---|---|---|---|---|---|---|---|
| % | n | % | N | % | n | p-Value | |
| Fillings | 91.73 | 211 | 95.41 | 104 | 88.43 | 107 | >0.05 † |
| Direct Pulp capping | 1.30 | 3 | 0.91 | 1 | 1.65 | 2 | >0.05 * |
| Pulpectomy | 33.91 | 78 | 55.96 | 61 | 14.05 | 17 | <0.001 † |
| Pulpotomy | 13.04 | 30 | 16.51 | 18 | 9.91 | 12 | >0.05 † |
| Endodontic | 13.04 | 30 | 6.42 | 7 | 19.00 | 23 | <0.05 † |
| MTA apexfication | 1.30 | 3 | 0.91 | 1 | 1.65 | 2 | >0.05 * |
| Calculus removal | 59.13 | 136 | 29.36 | 32 | 85.95 | 104 | <0.001 † |
| Fissure sealants | 40.87 | 94 | 36.70 | 40 | 44.63 | 54 | >0.05 † |
| Scaling and root planing | 0.86 | 2 | 0 | 0 | 1.65 | 2 | >0.05 * |
| Fluoride application | 83.48 | 192 | 73.39 | 80 | 92.56 | 112 | <0.001 † |
| Exodontias | 38.7 | 89 | 31.19 | 34 | 45.45 | 55 | <0.05 † |
| Exodontias due to disease | 30 | 69 | 25.69 | 28 | 33.88 | 41 | >0.05 † |
| Treatment | Healthy (47.4%) | SHCN (52.6%) | p-Value |
|---|---|---|---|
| Fillings | 6.85 ± 4.55 | 4.95 ± 3.72 | <0.05 ¶ |
| Direct pulp capping | 0.027 ± 0.28 | 0.016 ± 0.12 | >0.05 ¶ |
| Pulpectomy | 1.26 ± 1.61 | 0.19 ± 0.52 | <0.001 § |
| Pulpotomy | 0.32 ± 0.84 | 0.20 ± 0.75 | >0.05 ¶ |
| Endodontics | 0.15 ± 0.82 | 0.23 ± 0.53 | >0.05 § |
| MTA apexification | 0.01 ± 0.09 | 0.016 ± 0.13 | >0.05 ¶ |
| Fissure sealants | 0.88 ± 1.54 | 1.80 ± 2.75 | =0.002 ¶ |
| Extractions | 0.64 ± 1.36 | 1.35 ± 2.04 | =0.002 § |
| Extracted due to disease | 0.49 ± 1.19 | 0.81 ± 1.48 | >0.05 ¶ |
| <6 Years (n = 81) | 6–12 Years (n = 129) | >12 Years (n = 20) | p-Value + Cramer’s V | |
|---|---|---|---|---|
| Fillings | 93.80% | 90.69% | 90.00% | >0.05 * |
| Direct pulp capping | 1.23% | 0.77% | 5.00% | >0.05 * |
| Pulpectomy | 61.85% | 27.9% | 0.00% | <0.001 † (V = 0.32) |
| Pulpotomy | 19.70% | 10.85% | 0.00% | =0.037 * (V = 0.17) |
| Endodontic | 0.00% | 15.50% | 50.00% | <0.001 * (V = 0.379) |
| MTA apexfication | 0.00% | 2.32% | 0.00% | >0.05 * |
| Calculus removal | 14.81% | 82.17% | 85.00% | <0.001 † (V = 0.666) |
| Scaling and root planing | 0.00% | 0.00% | 10.00% | =0.006 * (V = 0.312) |
| Fissure sealants | 32.09% | 48.06% | 30.00% | =0.025 † (V = 0.179) |
| Fluoride application | 76.54% | 90.69% | 65.00% | =0.003 * (V = 0.242) |
| Exodontias | 18.51% | 51.16% | 40.00% | <0.001 † (V = 0.309) |
| Treatments | <6 Years | 6–12 Years | >12 Years | p-Value |
|---|---|---|---|---|
| Fillings | 6.88 ± 4.41 | 5.29 ± 3.53 # | 6.05 ± 6.53 | <0.05 |
| Direct pulp capping | 0.04 ± 0.33 | 0.01 ± 0.09 | 0.05 ± 0.22 | =0.305 |
| Pulpectomy | 1.19 ± 1.64 | 0.50 ± 1.01 # | 0.00 ± 0.00 #@ | <0.05 |
| Pulpotomy | 0.40 ± 0.89 | 0.22 ± 0.78 | 0.00 ± 0.00 | =0.06 |
| Endodontics | 0.00 ± 0.00 | 0.19 ± 0.49 # | 0.95 ± 1.82 #@ | <0.05 |
| MTA apexification | 0.00 ± 0.00 | 0.02 ± 0.15 | 0.00 ± 0.00 | =0.306 |
| Fissure sealant | 0.85 ± 1.57 | 1.60 ±2.31 # | 1.90 ± 3.99 | <0.05 |
| Exodontias | 0.30 ± 0.73 | 1.50 ± 2.13 # | 0.85 ± 1.35 | <0.05 |
| Sex (Male/Female) N (57/28) | Age (2–6/7–11/12–18) N (29/40/16) | Health Condition (Healthy/SHCN) N (22/63) | |
|---|---|---|---|
| 1. Does the child have frequent pain in the mouth? | 14/3 † (p = 0.25) | 5/10/2 * (p = 0.62) | 2/15 * (p = 0.22) |
| 2. Have they woken at night due to dental pain? | 12/2 * (p = 0.21) | 5/7/2 * (p = 1.00) | 5/9 * (p = 0.32) |
| 3. Has this prevented them from carrying out their usual daily routine? | 9/1 * (p = 0.16) | 5/4/1 * (p = 0.54) | 4/6 * (p = 0.27) |
| 4. Has the child taken medication due to dental problems? | 19/4 † (p = 0.14) | 9/11/2 * (p = 0.50) | 7/16 † (p = 0.64) |
| 5. Does the child have difficulty eating meat? | 20/8 † (p = 0.85) | 9/15/3 * (p = 0.53) | 6/22 † (p = 0.72) |
| 6. Does the child have difficulty eating cold food? | 14/2 † (p = 0.11) | 5/9/2 * (p = 0.88) | 3/13 * (p = 0.75) |
| 7. Does the child have difficulty eating hot food? | 12/1 * (p = 0.05) | 4/7/2 * (p = 1.00) | 3/10 * (p = 1.00) |
| 8. Does the child feel discomfort about the appearance of their teeth? | 9/2 * (p = 0.49) | 5/5/1 * (p = 0.71) | 5/6 * (p = 0.13) |
| 9. When brushing the teeth, does the child complain of pain? | 18/6 † (p = 0.53) | 10/11/3 * (p = 0.62) | 4/20 † (p = 0.40) |
| Sex (Male/Female) N (57/28) | Age (2–6/7–11/12–18) N (29/40/16) | Health Condition (Healthy/SHCN) N (22/63) | |
|---|---|---|---|
| 1. Does the child have difficulty eating meat? | 15/6 † (p = 1.00) | 4/13/3 * (p = 0.62) | 3/18 † (p = 0.23) |
| 2. Does the child have difficulty eating cold food? | 10/4 * (p = 1.00) | 4/10/0 * (p = 0.08) | 3/11 * (p = 1.00) |
| 3. Does the child have difficulty eating hot food? | 3/1 * (p = 1.00) | 1/3/0 * (p = 0.65) | 2/2 * (p = 0.26) |
| 4. Does the child eat better after the intervention? | 36/12 † (p = 0.11) | 18/22/7 † (p = 0.75) | 11/37 † (p = 0.68) |
| 5. Has the child gained weight during this time? | 15/7 † (p = 1.00) | 9/11/2 * (p = 0.52) | 7/15 † (p = 0.62) |
| 6. Does the child feel discomfort when brushing their teeth? | 9/8 † (p = 0.19) | 5/9/3 * (p = 0.93) | 3/14 * (p = 0.54) |
| 7. Is the child more rested and less irascible? | 27/10 † (p = 0.43) | 13/15/8 † (p = 0.44) | 9/28 † (p = 1.00) |
| 8. Is the child happy with their teeth? | 51/21 * (p = 0.58) | 26/31/14 * (p = 0.54) | 21/51 * (p = 0.57) |
| 9. Has treatment under deep sedation met your expectations? | 55/26 * (p = 1.00) | 27/37/15 * (p = 1.00) | 21/60 * (p = 1.00) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gómez-Ríos, I.; Pérez-Silva, A.; Serna-Muñoz, C.; Ibáñez-López, F.J.; Periago-Bayonas, P.M.; Ortiz-Ruiz, A.J. Deep Sedation for Dental Care Management in Healthy and Special Health Care Needs Children: A Retrospective Study. Int. J. Environ. Res. Public Health 2023, 20, 3435. https://doi.org/10.3390/ijerph20043435
Gómez-Ríos I, Pérez-Silva A, Serna-Muñoz C, Ibáñez-López FJ, Periago-Bayonas PM, Ortiz-Ruiz AJ. Deep Sedation for Dental Care Management in Healthy and Special Health Care Needs Children: A Retrospective Study. International Journal of Environmental Research and Public Health. 2023; 20(4):3435. https://doi.org/10.3390/ijerph20043435
Chicago/Turabian StyleGómez-Ríos, Inmaculada, Amparo Pérez-Silva, Clara Serna-Muñoz, Francisco Javier Ibáñez-López, Paula M. Periago-Bayonas, and Antonio J. Ortiz-Ruiz. 2023. "Deep Sedation for Dental Care Management in Healthy and Special Health Care Needs Children: A Retrospective Study" International Journal of Environmental Research and Public Health 20, no. 4: 3435. https://doi.org/10.3390/ijerph20043435
APA StyleGómez-Ríos, I., Pérez-Silva, A., Serna-Muñoz, C., Ibáñez-López, F. J., Periago-Bayonas, P. M., & Ortiz-Ruiz, A. J. (2023). Deep Sedation for Dental Care Management in Healthy and Special Health Care Needs Children: A Retrospective Study. International Journal of Environmental Research and Public Health, 20(4), 3435. https://doi.org/10.3390/ijerph20043435







