Co-Occurring Conduct Problems and Anxiety: Implications for the Functioning and Treatment of Youth with Oppositional Defiant Disorder
Abstract
1. Introduction
2. Method
2.1. Participants
2.2. Measures
2.2.1. Latent Profile Classification Measures
Parental and Teacher Ratings
Self-Ratings
2.2.2. External Validator Measures
Clinician Ratings
Parental Ratings
Teacher Ratings
Self-Ratings
3. Treatment
4. Statistical Analysis
5. Results
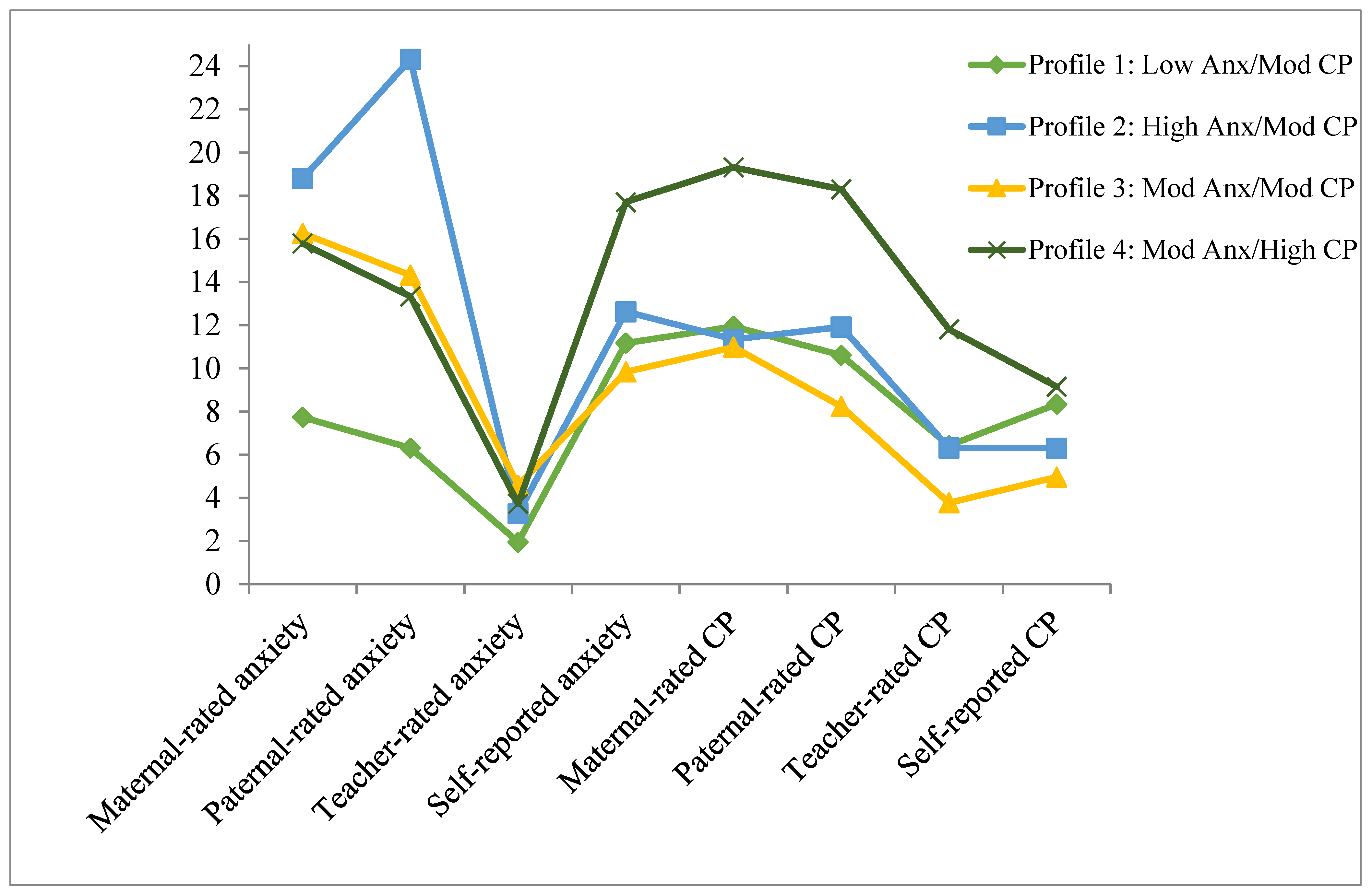
5.1. Latent Profile Classification
5.2. Global Functioning and Treatment Outcomes
5.2.1. Clinician Ratings
5.2.2. Parental Ratings
5.2.3. Teacher Ratings
5.2.4. Self-Ratings
6. Discussion
7. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Burke, J.D.; Rowe, R.; Boylan, K. Functional Outcomes of Child and Adolescent Oppositional Defiant Disorder Symptoms in Young Adult Men. J. Child Psychol. Psychiatry 2014, 55, 264–272. [Google Scholar] [CrossRef] [PubMed]
- Nock, M.K.; Kazdin, A.E.; Hiripi, E.; Kessler, R.C. Lifetime Prevalence, Correlates, and Persistence of Oppositional Defiant Disorder: Results from the National Comorbidity Survey Replication. J. Child Psychol. Psychiatry 2007, 48, 703–713. [Google Scholar] [CrossRef] [PubMed]
- Kaminski, J.W.; Claussen, A.H. Evidence Base Update for Psychosocial Treatments for Disruptive Behaviors in Children. J. Clin. Child Adolesc. Psychol. 2017, 46, 477–499. [Google Scholar] [CrossRef] [PubMed]
- Hawes, D.J.; Price, M.J.; Dadds, M.R. Callous-Unemotional Traits and the Treatment of Conduct Problems in Childhood and Adolescence: A Comprehensive Review. Clin. Child Fam. Psychol. Rev. 2014, 17, 248–267. [Google Scholar] [CrossRef]
- Foster, E.M.; Jones, D.E.; Conduct Problems Prevention Research Group. The High Costs of Aggression: Public Expenditures Resulting from Conduct Disorder. Am. J. Public Health 2005, 95, 1767–1772. [Google Scholar] [CrossRef]
- Roetman, P.J.; Siebelink, B.M.; Vermeiren, R.R.; Colins, O.F. Classes of Oppositional Defiant Disorder Behavior in Clinic-Referred Children and Adolescents: Concurrent Features and Outcomes: Classification Des Comportements Dans Le Trouble Oppositionnel Avec Provocation Chez Des Enfants et Des Adolescents Aiguillés à Une Clinique: Caractéristiques Co-Occurrentes et Résultats. Can. J. Psychiatry 2021, 66, 657–666. [Google Scholar]
- Racz, S.J.; McMahon, R.J.; Gudmundsen, G.; McCauley, E.; Vander Stoep, A. Latent Classes of Oppositional Defiant Disorder in Adolescence and Prediction to Later Psychopathology. Dev. Psychopathol. 2022, 1–19. [Google Scholar] [CrossRef]
- Lavigne, J.V.; Bryant, F.B.; Hopkins, J.; Gouze, K.R. Dimensions of Oppositional Defiant Disorder in Young Children: Model Comparisons, Gender and Longitudinal Invariance. J. Abnorm. Child Psychol. 2015, 43, 423–439. [Google Scholar] [CrossRef]
- Mikolajewski, A.J.; Taylor, J.; Iacono, W.G. Oppositional Defiant Disorder Dimensions: Genetic Influences and Risk for Later Psychopathology. J. Child Psychol. Psychiatry 2017, 58, 702–710. [Google Scholar] [CrossRef]
- Burke, J.D.; Boylan, K.; Rowe, R.; Duku, E.; Stepp, S.D.; Hipwell, A.E.; Waldman, I.D. Identifying the Irritability Dimension of ODD: Application of a Modified Bifactor Model across Five Large Community Samples of Children. J. Abnorm. Psychol. 2014, 123, 841. [Google Scholar] [CrossRef]
- Waldman, I.D.; Rowe, R.; Boylan, K.; Burke, J.D. External Validation of a Bifactor Model of Oppositional Defiant Disorder. Mol. Psychiatry 2018, 26, 1. [Google Scholar] [CrossRef]
- Boylan, K.; Vaillancourt, T.; Boyle, M.; Szatmari, P. Comorbidity of Internalizing Disorders in Children with Oppositional Defiant Disorder. Eur. Child Adolesc. Psychiatry 2007, 16, 484–494. [Google Scholar] [CrossRef]
- Maughan, B.; Rowe, R.; Messer, J.; Goodman, R.; Meltzer, H. Conduct Disorder and Oppositional Defiant Disorder in a National Sample: Developmental Epidemiology. J. Child Psychol. Psychiatry 2004, 45, 609–621. [Google Scholar] [CrossRef]
- Déry, M.; Lapalme, M.; Jagiellowicz, J.; Poirier, M.; Temcheff, C.; Toupin, J. Predicting Depression and Anxiety from Oppositional Defiant Disorder Symptoms in Elementary School-Age Girls and Boys with Conduct Problems. Child Psychiatry Hum. Dev. 2017, 48, 53–62. [Google Scholar] [CrossRef]
- Cunningham, N.R.; Ollendick, T.H. Comorbidity of Anxiety and Conduct Problems in Children: Implications for Clinical Research and Practice. Clin. Child Fam. Psychol. Rev. 2010, 13, 333–347. [Google Scholar] [CrossRef]
- Boden, J.M.; Fergusson, D.M.; Horwood, L.J. Risk Factors for Conduct Disorder and Oppositional/Defiant Disorder: Evidence from a New Zealand Birth Cohort. J. Am. Acad. Child Adolesc. Psychiatry 2010, 49, 1125–1133. [Google Scholar] [CrossRef]
- Drabick, D.A.G.; Gadow, K.D.; Loney, J. Co-Occurring ODD and GAD Symptom Groups: Source-Specific Syndromes and Cross-Informant Comorbidity. J. Clin. Child Adolesc. Psychol. 2008, 37, 314–326. [Google Scholar] [CrossRef]
- Wesselhoeft, R.; Stringaris, A.; Sibbersen, C.; Kristensen, R.V.; Bojesen, A.B.; Talati, A. Dimensions and Subtypes of Oppositionality and Their Relation to Comorbidity and Psychosocial Characteristics. Eur. Child Adolesc. Psychiatry 2018, 28, 351–365. [Google Scholar] [CrossRef]
- Beauchaine, T.P.; Webster-Stratton, C.; Reid, M.J. Mediators, Moderators, and Predictors of 1-Year Outcomes among Children Treated for Early-Onset Conduct Problems: A Latent Growth Curve Analysis. J. Consult. Clin. Psychol. 2005, 73, 371. [Google Scholar] [CrossRef]
- Franco, X.; Saavedra, L.M.; Silverman, W.K. External Validation of Comorbid Patterns of Anxiety Disorders in Children and Adolescents. J. Anxiety Disord. 2007, 21, 717–729. [Google Scholar] [CrossRef]
- Walker, J.L.; Lahey, B.B.; Russo, M.F.; Frick, P.J.; Christ, M.A.G.; McBurnett, K.; Loeber, R.; Stouthamer-Loeber, M.; Green, S.M. Anxiety, Inhibition, and Conduct Disorder in Children: I. Relations to Social Impairment. J. Am. Acad. Child Adolesc. Psychiatry 1991, 30, 187–191. [Google Scholar] [CrossRef] [PubMed]
- Drabick, D.A.G.; Ollendick, T.H.; Bubier, J.L. Co-occurrence of ODD and Anxiety: Shared Risk Processes and Evidence for a Dual-pathway Model. Clin. Psychol. Sci. Pract. 2010, 17, 307–318. [Google Scholar] [CrossRef] [PubMed]
- Sachser, C.; Keller, F.; Goldbeck, L. Complex PTSD as Proposed for ICD-11: Validation of a New Disorder in Children and Adolescents and Their Response to Trauma-Focused Cognitive Behavioral Therapy. J. Child Psychol. Psychiatry Allied Discip. 2017, 58, 160–168. [Google Scholar] [CrossRef] [PubMed]
- Iampietro, M.; Giovannetti, T.; Drabick, D.A.; Kessler, R.K. Empirically Defined Patterns of Executive Function Deficits in Schizophrenia and Their Relation to Everyday Functioning: A Person-Centered Approach. Clin. Neuropsychol. 2012, 26, 1166–1185. [Google Scholar] [CrossRef] [PubMed]
- Andrade, B.F.; Waschbusch, D.A.; King, S.; Thurston, C.; McNutt, L.; Terrio, B.; Northern Partners in Action for Children and Youth, Nova Scotia. Teacher-Classified Peer Social Status: Preliminary Validation and Associations with Behavior Ratings. J. Psychoeduc. Assess. 2005, 23, 279–290. [Google Scholar] [CrossRef]
- Herzhoff, K.; Tackett, J.L. Subfactors of Oppositional Defiant Disorder: Converging Evidence from Structural and Latent Class Analyses. J. Child Psychol. Psychiatry 2016, 57, 18–29. [Google Scholar] [CrossRef]
- Althoff, R.R.; Kuny-Slock, A.V.; Verhulst, F.C.; Hudziak, J.J.; Ende, J. Classes of Oppositional-defiant Behavior: Concurrent and Predictive Validity. J. Child Psychol. Psychiatry 2014, 55, 1162–1171. [Google Scholar] [CrossRef]
- Aebi, M.; Barra, S.; Bessler, C.; Steinhausen, H.-C.; Walitza, S.; Plattner, B. Oppositional Defiant Disorder Dimensions and Subtypes among Detained Male Adolescent Offenders. J. Child Psychol. Psychiatry 2016, 57, 729–736. [Google Scholar] [CrossRef]
- Ollendick, T.H.; Greene, R.W.; Austin, K.E.; Fraire, M.G.; Halldorsdottir, T.; Allen, K.B.; Jarrett, M.A.; Lewis, K.M.; Whitmore Smith, M.; Cunningham, N.R.; et al. Parent Management Training and Collaborative & Proactive Solutions: A Randomized Control Trial for Oppositional Youth. J. Clin. Child Adolesc. Psychol. 2016, 45, 591–604. [Google Scholar] [CrossRef]
- Bögels, S.M.; Brechman-Toussaint, M.L. Family Issues in Child Anxiety: Attachment, Family Functioning, Parental Rearing and Beliefs. Clin. Psychol. Rev. 2006, 26, 834–856. [Google Scholar] [CrossRef]
- Kusche, C.A.; Cook, E.T.; Greenberg, M.T. Neuropsychological and Cognitive Functioning in Children with Anxiety, Externalizing, and Comorbid Psychopathology. J. Clin. Child Psychol. 1993, 22, 172–195. [Google Scholar] [CrossRef]
- Muris, P.; Ollendick, T.H. The Role of Temperament in the Etiology of Child Psychopathology. Clin. Child Fam. Psychol. Rev. 2005, 8, 271–289. [Google Scholar] [CrossRef]
- Raine, A.; Dodge, K.; Loeber, R.; Gatzke-Kopp, L.; Lynam, D.; Reynolds, C.; Stouthamer-Loeber, M.; Liu, J. The Reactive–Proactive Aggression Questionnaire: Differential Correlates of Reactive and Proactive Aggression in Adolescent Boys. Aggress. Behav. 2006, 32, 159–171. [Google Scholar] [CrossRef]
- Cavanagh, M.; Quinn, D.; Duncan, D.; Graham, T.; Balbuena, L. Oppositional Defiant Disorder Is Better Conceptualized as a Disorder of Emotional Regulation. J. Atten. Disord. 2017, 21, 381–389. [Google Scholar] [CrossRef]
- Suveg, C.; Sood, E.; Comer, J.S.; Kendall, P.C. Changes in Emotion Regulation Following Cognitive-Behavioral Therapy for Anxious Youth. J. Clin. Child Adolesc. Psychol. 2009, 38, 390–401. [Google Scholar] [CrossRef]
- Fraire, M.G.; Ollendick, T.H. Anxiety and Oppositional Defiant Disorder: A Transdiagnostic Conceptualization. Clin. Psychol. Rev. 2013, 33, 229–240. [Google Scholar] [CrossRef]
- Reynolds, C.R. Behavior Assessment System for Children; Wiley Online Library: Hoboken, NJ, USA, 2004. [Google Scholar]
- Pelham, W.E.; Evans, S.W.; Gnagy, E.M.; Greenslade, K.E. Teacher Ratings of DSM-III-R Symptoms for the Disruptive Behavior Disorders: Prevalence, Factor Analyses, and Conditional Probabilities in a Special Education Sample. Sch. Psychol. Rev. 1992, 21, 285–299. [Google Scholar] [CrossRef]
- Beck, J.S. Beck Youth Inventories—Second Edition for Children and Adolescents Manual; Psychological Corporation: San Antonio, TX, USA, 2005. [Google Scholar]
- Silverman, W.K.; Albano, A.M. The Anxiety Disorders Interview Schedule for Children (ADIS-C/P); Psychological Corporation: San Antonio, TX, USA, 1996. [Google Scholar]
- Shaffer, D.; Gould, M.S.; Brasic, J.; Ambrosini, P.; Fisher, P.; Bird, H.; Aluwahlia, S. A Children’s Global Assessment Scale (CGAS). Arch. Gen. Psychiatry 1983, 40, 1228–1231. [Google Scholar] [CrossRef]
- Shields, A.; Cicchetti, D. Emotion Regulation among School-Age Children: The Development and Validation of a New Criterion Q-Sort Scale. Dev. Psychol. 1997, 33, 906. [Google Scholar] [CrossRef]
- Brown, K.; Atkins, M.S.; Osborne, M.L.; Milnamow, M. A Revised Teacher Rating Scale for Reactive and Proactive Aggression. J. Abnorm. Child Psychol. 1996, 24, 473–480. [Google Scholar] [CrossRef]
- Gioia, G.A.; Guy, S.C.; Isquith, P.K.; Kenworthy, L. Behavior Rating Inventory of Executive Function; Psychological Assessment Resources: Lutz, FL, USA, 1996. [Google Scholar]
- Barkley, R.A. Defiant Children: A Clinician’s Manual for Parent Training and Assessment; Psychological Corporation: San Antonio, TX, USA, 1997. [Google Scholar]
- Greene, R.W. The Explosive Child: A New Approach for Understanding and Parenting Easily Frustrated," Chronically Inflexible" Children; HarperCollins Publishers: New York, NY, USA, 1998. [Google Scholar]
- Murrihy, R.C.; Drysdale, S.A.; Dedousis-Wallace, A.; Rémond, L.; McAloon, J.; Ellis, D.M.; Halldorsdottir, T.; Greene, R.W.; Ollendick, T.H. Community-Delivered Collaborative and Proactive Solutions and Parent Management Training for Oppositional Youth: A Randomized Trial. Behav. Ther. 2022. [Google Scholar] [CrossRef]
- Muthén, L.K. Mplus User’s Guide; Muthén & Muthén: Los Angeles, CA, USA, 2010. [Google Scholar]
- Akaike, H. Factor Analysis and AIC. Psychometrika 1987, 52, 317–332. [Google Scholar] [CrossRef]
- Schwarz, G. Estimating the Dimension of a Model. Ann. Stat. 1978, 6, 461–464. [Google Scholar] [CrossRef]
- Sclove, S.L. Application of Model-Selection Criteria to Some Problems in Multivariate Analysis. Psychometrika 1987, 52, 333–343. [Google Scholar] [CrossRef]
- Frick, P.J.; Morris, A.S. Temperament and Developmental Pathways to Conduct Problems. J. Clin. Child Adolesc. Psychol. 2004, 33, 54–68. [Google Scholar] [CrossRef]
- Frick, P.J.; Ellis, M. Callous-Unemotional Traits and Subtypes of Conduct Disorder. Clin. Child Fam. Psychol. Rev. 1999, 2, 149–168. [Google Scholar] [CrossRef]
- Gray, J.A. The Psychology of Fear and Stress; CUP Archive: Cambridge, UK, 1987; Volume 5. [Google Scholar]
- Drabick, D.A.G.; Bubier, J.; Chen, D.; Price, J.; Lanza, H.I. Source-Specific Oppositional Defiant Disorder among Inner-City Children: Prospective Prediction and Moderation. J. Clin. Child Adolesc. Psychol. 2011, 40, 23–35. [Google Scholar] [CrossRef]
- De Los Reyes, A.; Augenstein, T.M.; Wang, M.; Thomas, S.A.; Drabick, D.A.G.; Burgers, D.E.; Rabinowitz, J. The Validity of the Multi-Informant Approach to Assessing Child and Adolescent Mental Health. Psychol. Bull. 2015, 141, 858. [Google Scholar] [CrossRef]
- Anderson, S.R.; Ollendick, T.H. Diagnosing Oppositional Defiant Disorder Using the Anxiety Disorders Interview Schedule for DSM-IV: Parent Version and the Diagnostic Interview Schedule for Children. J. Psychopathol. Behav. Assess. 2012, 34, 467–475. [Google Scholar] [CrossRef]
- Nylund, K.; Bellmore, A.; Nishina, A.; Graham, S. Subtypes, Severity, and Structural Stability of Peer Victimization: What Does Latent Class Analysis Say? Child Dev. 2007, 78, 1706–1722. [Google Scholar] [CrossRef]
- Nylund, K.L.; Asparouhov, T.; Muthén, B.O. Deciding on the Number of Classes in Latent Class Analysis and Growth Mixture Modeling: A Monte Carlo Simulation Study. Struct. Equ. Model. 2007, 14, 535–569. [Google Scholar] [CrossRef]
| Categorical Variables | N (%) |
|---|---|
| Gender | |
| Female | 49 (36.6) |
| Male | 85 (63.4) |
| Race | |
| White | 112 (83.6) |
| Non-white | 22 (16.4) |
| Comorbid anxiety disorder | |
| Generalized anxiety disorder | 30 (22.39) |
| Separation anxiety disorder | 16 (11.94) |
| Social phobia | 23 (17.16) |
| Specific phobia | 26 (19.40) |
| Comorbid ADHD | 89 (66.4) |
| Continuous Variables | M (SD) |
| Age in years | 9.67 (1.82) |
| ODD CSR | 5.99 (1.05) |
| CGAS | 59.37 (5.89) |
| Maternal-reported CD symptoms | 1.93 (1.74) |
| Paternal-reported CD symptoms | 1.21 (1.44) |
| Number of Classes | Number of Free Parameters | Log Likelihood | AIC | BIC | ABIC | BLRT |
|---|---|---|---|---|---|---|
| 1 | 16 | −2674.35 | 5380.70 | 5427.07 | 5376.46 | - |
| 2 | 25 | −2644.15 | 5338.30 | 5410.74 | 5331.66 | <0.001 |
| 3 | 34 | −2623.92 | 5315.84 | 5414.37 | 5306.82 | <0.001 |
| 4 | 43 | −2608.53 | 5303.06 | 5427.67 | 5291.65 | 0.0128 |
| Profile 1 Low Anx/Mod CP | Profile 2 High Anx/Mod CP | Profile 3 Mod Anx/Mod CP | Profile 4 Mod Anx/High CP | Pairwise | |||||
|---|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | M | SD | Comparisons | |
| Clinician ratings | |||||||||
| ANX CSR pre | 2.82 | 2.68 | 4.05 | 2.51 | 3.22 | 2.67 | 4.35 | 2.43 | - |
| ODD CSR pre | 5.81 | 1.12 | 6.18 | 1.01 | 5.86 | 1.20 | 6.30 | 1.18 | - |
| ODD CSR post | 3.85 | 2.83 | 3.52 | 2.76 | 3.18 | 2.73 | 4.37 | 3.09 | - |
| ODD CSR 6-month | 3.89 | 3.74 | 3.46 | 3.48 | 3.14 | 2.59 | 4.95 | 2.53 | - |
| ODD CSR 1-year | 3.71 | 3.54 | 3.94 | 4.19 | 2.98 | 3.00 | 6.16 | 2.38 | 4 > 1, 2, 3 |
| CGAS pre | 60.10 | 5.64 | 57.80 | 6.31 | 61.50 | 7.14 | 56.60 | 5.01 | 1, 3 > 4; 3 > 2 |
| CGAS post | 67.18 | 10.41 | 67.41 | 8.77 | 68.99 | 11.63 | 63.89 | 8.96 | - |
| CGAS 6-month | 66.44 | 16.82 | 67.73 | 17.61 | 68.66 | 12.45 | 51.56 | 20.81 | - |
| CGAS 1-year | 66.66 | 11.96 | 65.29 | 17.73 | 72.00 | 15.25 | 57.22 | 15.15 | 1, 3 > 4 |
| Maternal Ratings | |||||||||
| ODD symptoms | 5.42 | 2.05 | 5.74 | 2.03 | 5.63 | 2.01 | 6.43 | 2.31 | - |
| CD symptoms | 1.87 | 1.92 | 1.84 | 1.78 | 1.68 | 1.95 | 2.57 | 2.55 | - |
| Externalizing problems | 71.40 | 11.60 | 72.30 | 9.30 | 69.00 | 10.90 | 85.30 | 10.30 | 4 >1, 2, 3 |
| Aggression | 69.79 | 12.76 | 71.01 | 10.99 | 68.47 | 11.62 | 77.56 | 16.15 | - |
| Lability | 35.10 | 6.87 | 38.60 | 6.14 | 36.60 | 6.07 | 40.2 | 6.98 | 2, 4 > 1 |
| Negative emotionality | 10.25 | 2.28 | 11.64 | 1.98 | 11.17 | 2.19 | 11.78 | 3.02 | - |
| Emotional self-control | 8.45 | 3.56 | 10.90 | 3.56 | 9.94 | 3.54 | 12.30 | 3.27 | 2, 4 > 1; 4 > 3 |
| Proactive aggression | 16.23 | 3.86 | 16.60 | 3.27 | 16.45 | 4.07 | 19.06 | 3.14 | - |
| Reactive aggression | 14.45 | 2.26 | 15.55 | 2.09 | 15.26 | 2.02 | 15.79 | 2.09 | - |
| Executive functioning | 67.55 | 10.63 | 71.36 | 9.74 | 69.25 | 8.96 | 73.54 | 11.73 | - |
| Self-regulation | 41.62 | 7.03 | 43.52 | 6.18 | 42.14 | 7.29 | 43.16 | 10.27 | - |
| Paternal Ratings | |||||||||
| ODD symptoms | 3.89 | 2.59 | 5.35 | 2.87 | 3.56 | 2.46 | 5.71 | 3.88 | 2 > 1, 3; 4 > 3 |
| CD symptoms | 1.04 | 1.54 | 1.78 | 2.42 | .72 | 1.35 | 2.41 | 2.45 | 2 > 3; 4 > 3, 1 |
| Externalizing problems | 65.00 | 8.88 | 71.90 | 11.00 | 62.00 | 10.40 | 81.70 | 13.30 | 4 > 2 > 1, 3 |
| Aggression | 63.10 | 9.72 | 68.60 | 12.30 | 61.40 | 9.92 | 73.50 | 17.90 | 2, 4 > 1, 3 |
| Lability | 33.90 | 7.13 | 38.90 | 6.03 | 35.00 | 7.52 | 40.80 | 11.30 | 2, 4 > 1, 3 |
| Negative emotionality | 9.00 | 2.53 | 11.00 | 2.07 | 8.99 | 2.59 | 10.10 | 4.53 | 2 > 1, 3 |
| Emotional self-control | 7.63 | 3.24 | 10.60 | 3.44 | 8.17 | 3.16 | 10.20 | 4.84 | 2 > 1, 3; 4 > 1 |
| Proactive aggression | 15.00 | 3.18 | 15.80 | 3.16 | 15.00 | 4.55 | 19.30 | 4.71 | 4 > 1, 2, 3 |
| Reactive aggression | 13.59 | 2.85 | 14.91 | 2.81 | 14.02 | 3.18 | 16.02 | 3.46 | - |
| Executive functioning | 64.20 | 12.20 | 70.30 | 10.10 | 65.30 | 11.90 | 72.60 | 15.60 | 2, 4 > 1 |
| Self-regulation | 36.30 | 9.78 | 41.50 | 8.95 | 37.10 | 9.23 | 42.90 | 14.50 | 2 > 1, 3 |
| Teacher Ratings | |||||||||
| Externalizing problems | 59.90 | 16.30 | 59.10 | 18.00 | 53.50 | 15.60 | 72.00 | 17.80 | 4 > 1, 2, 3 |
| Aggression | 61.00 | 19.50 | 59.10 | 22.70 | 53.90 | 16.40 | 67.80 | 22.00 | 4 > 3 |
| School problems | 53.10 | 9.72 | 54.70 | 13.50 | 51.60 | 13.80 | 63.60 | 9.64 | 4 > 1, 2, 3 |
| Social skills | 38.20 | 13.40 | 45.40 | 14.20 | 47.20 | 16.00 | 40.50 | 13.70 | 2, 3 > 1 |
| Learning problems | 48.60 | 10.60 | 52.30 | 15.30 | 49.20 | 12.30 | 60.00 | 13.50 | 4 > 1, 3 |
| Study skills | 42.20 | 11.20 | 45.40 | 14.20 | 48.00 | 12.70 | 36.80 | 10.60 | 3 > 1, 4; 2 > 4 |
| Self-Report | |||||||||
| Proactive aggression | 12.60 | 2.72 | 12.10 | 2.53 | 11.60 | 2.21 | 14.7 | 3.49 | 4 > 1, 2, 3 |
| Reactive aggression | 8.85 | 2.27 | 8.92 | 2.41 | 8.29 | 2.40 | 10.7 | 3.05 | 4 > 1, 2, 3 |
| Self-concept | 40.10 | 11.80 | 42.90 | 10.70 | 44.60 | 11.30 | 34.9 | 13.70 | 2, 3 > 4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Halldorsdottir, T.; Fraire, M.G.; Drabick, D.A.G.; Ollendick, T.H. Co-Occurring Conduct Problems and Anxiety: Implications for the Functioning and Treatment of Youth with Oppositional Defiant Disorder. Int. J. Environ. Res. Public Health 2023, 20, 3405. https://doi.org/10.3390/ijerph20043405
Halldorsdottir T, Fraire MG, Drabick DAG, Ollendick TH. Co-Occurring Conduct Problems and Anxiety: Implications for the Functioning and Treatment of Youth with Oppositional Defiant Disorder. International Journal of Environmental Research and Public Health. 2023; 20(4):3405. https://doi.org/10.3390/ijerph20043405
Chicago/Turabian StyleHalldorsdottir, Thorhildur, Maria G Fraire, Deborah A. G. Drabick, and Thomas H. Ollendick. 2023. "Co-Occurring Conduct Problems and Anxiety: Implications for the Functioning and Treatment of Youth with Oppositional Defiant Disorder" International Journal of Environmental Research and Public Health 20, no. 4: 3405. https://doi.org/10.3390/ijerph20043405
APA StyleHalldorsdottir, T., Fraire, M. G., Drabick, D. A. G., & Ollendick, T. H. (2023). Co-Occurring Conduct Problems and Anxiety: Implications for the Functioning and Treatment of Youth with Oppositional Defiant Disorder. International Journal of Environmental Research and Public Health, 20(4), 3405. https://doi.org/10.3390/ijerph20043405





