Abstract
Conduct problems and anxiety symptoms commonly co-occur among youths with oppositional defiant disorder (ODD); however, how these symptoms influence functioning and treatment outcomes remains unclear. This study examined subtypes based on these co-occurring symptoms in a clinical sample of 134 youths (Mage = 9.67, 36.6% female, 83.6% white) with ODD and the predictive power of these subgroups for youth functioning and psychosocial treatment outcomes. The latent profile analysis (LPA) was used to identify subgroups based on parent- and self-reported conduct problems and anxiety symptoms. Differences among the subgroups in clinician-, parent-, and/or self-reported accounts of symptom severity, school performance, underlying processing known to be impaired across ODD, conduct and anxiety disorders, self-concept, and psychosocial treatment outcomes were examined. Four distinct profiles were identified: (1) Low Anxiety/Moderate Conduct Problems (n = 42); (2) High Anxiety/Moderate Conduct Problems (n = 33); (3) Moderate Anxiety/Moderate Conduct Problems (n = 40); and (4) Moderate Anxiety/High Conduct Problems (n = 19). The Moderate Anxiety/High Conduct Problems group exhibited more severe behavioral problems, greater difficulties with negative emotionality, emotional self-control, and executive functioning; they also demonstrated worse long-term treatment outcomes than the other subgroups. These findings suggest more homogeneous subgroups within and across diagnostic categories may result in a deeper understanding of ODD and could inform nosological systems and intervention efforts.
1. Introduction
Oppositional defiant disorder (ODD) is characterized by a developmentally inappropriate and persistent pattern of irritable mood, defiant behavior, argumentativeness, and hostile behavior towards authority figures [1]. These symptoms lead to social, emotional, and/or academic deficits during childhood, which persist into adulthood if left untreated [2]. The lifetime prevalence of ODD is estimated to be 10.2% [3]. Parent-focused treatments based on behavioral elements, such as positive reinforcement of desirable child behavior, have been identified as evidence-based treatments for ODD [4]. However, one-third to one-half of youths do not respond to these treatments [5]. Given their pervasiveness, resistance to change, and financial burden to society [6], a better understanding of the complex and heterogeneous presentation of oppositional behaviors is necessary to improve the assessment and treatment of ODD. Although the dimensional nature of ODD continues to be studied [7,8,9,10,11,12], an additional avenue to pursue is understanding treatment non-responders and the role of comorbidity and potential underlying processes that contribute to different symptom profiles.
Comorbidity is common among youths diagnosed with ODD [13,14]. Although attention-deficit/hyperactivity disorder (ADHD) has received the most attention, conduct and anxiety disorders are also common among youths with ODD [14,15]. Indeed, clinical studies have shown that >30% of youths with ODD also meet the diagnostic criteria for CD and up to 60% meet the diagnostic criteria for an anxiety disorder [16]. These high comorbidity rates may be indicative of shared psychosocial and biological factors contributing to the disorders [17,18]. However, previous reports on how co-occurring conduct problems and anxiety influence global functioning and treatment responses to psychosocial interventions among youths with ODD have yielded mixed results [18,19,20,21,22]. These inconsistent findings suggest that co-occurring conduct problems and anxiety symptoms may be associated with different profiles of ODD with varying clinical presentations and prognosis [23]. The aim of this study was to extend this literature to a treatment-seeking sample.
The latent profile analysis (LPA) is a person-centered data analytic approach that identifies profiles across the continuum of certain behaviors. A person-centered analytic approach is particularly important in clinical research when exploring heterogeneous populations, such as children with ODD, as it is not assumed that the same processes apply to all individuals, unlike with more traditional, variable-centered analytic approaches. Furthermore, LPAs have the capacity to identify clinically meaningful subgroups from relatively small sample sizes [24,25]. Previous person-centered analyses of ODD have formed subgroups based on oppositional behaviors alone [7,8,19,26,27,28,29]. This research suggests that different dimensions of ODD may be predictive of varying comorbid difficulties later in life (e.g., [7,19]). For instance, one study found that youths with ODD characterized by primarily irritable symptoms were more likely to present with internalizing problems in late adolescence, whereas those primarily characterized by headstrong or hurtful symptoms were more likely to present with substance use [11]. Despite the high levels of comorbidity, to our knowledge, the current study is the first to examine subtypes based on these co-occurring conduct problems and anxiety symptoms in a clinical sample of youths with ODD.
The current study was designed to (1) identify subgroups based on conduct problems and anxiety symptom profiles in a clinical sample of 134 children with ODD using LPA, and (2) examine the predictive power of these subgroups to predict global functioning and treatment outcomes following empirically supported psychosocial interventions [30]. Measures of global functioning were informed by empirical research supporting their inclusion [18,31,32,33,34,35] and potential clinical implications for psychosocial interventions [36]. Specifically, we examined whether the identified subgroups differed on clinician-, parent-, and/or self-reported accounts of symptom severity and presentation (i.e., proactive and reactive aggression); school performance; underlying processing known to be impaired across ODD, CD, and anxiety disorders (i.e., lability, emotional self-control, and executive functioning [37]); self-concept; and treatment outcomes following psychosocial interventions.
2. Method
2.1. Participants
The group of participants comprised 134 7–14 year-old (Meanage = 9.67, SD = 1.82) youths referred for ODD treatment (ClinicalTrials.gov NCT00510120) [30]. Informed consent and assent were obtained from families and participants, respectively. The presence of psychiatric disorders, including ODD, was determined using a semi-structured clinical interview (see below). Children who met full criteria for autism spectrum disorder, a psychotic disorder, CD, or possessed an estimated IQ < 80 were excluded from the study. Although full diagnostic criteria for CD were not met in this study, youths presented with an average of 1.93 maternally reported and 1.21 paternally reported CD symptoms on the Disruptive Behavior Disorders Rating Scale (DBDRS, see below). Participants were recruited from schools, churches, pediatricians, child psychiatrists, and medical clinics.
2.2. Measures
Table S1 in the Supplementary Materials displays the measurements completed by each informant and internal consistency of the subscales. For all the measures, higher scores reflect greater impairment, unless otherwise specified in the description below.
2.2.1. Latent Profile Classification Measures
Parental and Teacher Ratings
The Conduct Problems (9 items; e.g., steals, deceives others) and Anxiety subscales (14 items; e.g., worries, is fearful, tries too hard to please others) of the Behavior Assessment System for Children, Second Edition (BASC-2) [38], were used to assess parent- and teacher-reported conduct problems and anxiety, respectively, in the LPA.
Self-Ratings
The Disruptive Behavior Disorders Rating Scale (DBDRS) [39] was used to assess self-reported symptoms of ODD and CD based on DSM-IV criteria (8 items). A floor effect was observed in self-reported CD symptoms endorsed, with only 18.6% (n = 25) endorsing >1 symptom. Therefore the ODD subscale, which had greater variability in responses, was used in the LPA. The Anxiety subscales of the Beck Youth Inventories, Second Edition (BYI-2) [40], was used to measure self-reported anxiety (20 items; e.g., I worry, I am afraid something bad might happen to me).
2.2.2. External Validator Measures
Clinician Ratings
Diagnostic interview. The Anxiety Disorders Interview Schedule for DSM-IV, Child and Parent Versions (ADIS-C/P) [41], are semi-structured diagnostic interviews in which clinicians assign a clinical severity rating (CSR) on a 9-point scale (0–8, with a rating ≥ 4 suggesting a clinical level of interference). See Supplementary Materials for further description of the administration and psychometric properties of the ADIS C/P. The CSRs derived from the ADIS served as a clinician-rated measure of severity of anxiety disorder, attention-deficit/hyperactivity disorder (ADHD), and ODD prior to and following treatment.
Global functioning. The Child Global Assessment Scale (CGAS) [42] is a 100-point rating scale measuring psychological, social, and school functioning in youths, with lower scores reflecting greater impairment. Participants’ global functioning was assessed prior to and following treatment.
Parental Ratings
ODD and CD symptoms. The ODD and CD subscales of the parent version of the Disruptive Behavior Disorders Rating Scale (DBDRS) [39] were used to measure parent-reported ODD and CD severity. Reflecting DSM-IV symptoms, the ODD scale contains 8 items rated on a four-point Likert scale (0 = never to 3 = very often), whereas the CD scale consists of 15 dichotomous questions in which an item is either endorsed as present or absent by the parent.
Aggression and emotional self-control. Parental ratings on the Aggression and Emotional Self-Control subscales from the BASC-2 [38] were used. The Aggression subscale (11 items; e.g., bullies others, threatens to hurt others) captures general aggressive behaviors towards peers and parents. The Emotional Self-Control subscale assesses difficulties regulating emotions and affect (6 items; e.g., acts out of control, has poor self-control).
Lability. The Lability/Negativity scale (11 items; e.g., exhibits wide mood swings, responds negatively to neutral or friendly overtures by peers) of the Emotion Regulation Checklist (ERC) [43] was used to measure dysregulated negative affect, lability, and inflexibility.
Proactive and reactive aggression. The Proactive Aggression (10 items; e.g., has hurt others to win a game or contest, gets others to gang up on children) and Reactive Aggression subscales (6 items; e.g., gets mad when corrected, blames others when gets into trouble) of the Child Behavior Rating Scale (CBRS) [44] were utilized to assess parental reported proactive (i.e., aggressive behavior intended to harm or coerce another person) and reactive (i.e., defensive response to perceived threat or provocation) aggression.
Executive functioning. The Global Executive Composite (86 items) of the Behavior Rating Inventory of Executive Functioning (BRIEF) [45] was used to assess executive functioning in daily living.
Teacher Ratings
Aggression, school problems, social skills, learning problems, and study skills. Teacher ratings on the Aggression, School Problems, Learning Problems, and Study Skills subscales of the BASC-2 [38] were used to examine aggression, academic problems, and school functioning. Higher scores on the Aggression, School Problems, and Learning Problems subscales indicate greater impairment, whereas lower scores on the Study Skills subscale reflect impaired abilities.
Self-Ratings
Proactive and reactive aggression. A parallel version of the CBRS [44] was administered to assess self-reported proactive and reactive aggression.
Self-concept. The Self-Concept subscale of the BYI-2 [40] was used to assess self-perceived competence and positive self-worth (20 items; e.g., I feel smart, I like myself). Higher scores reflect a more positive self-concept.
3. Treatment
Participants received 12 sessions of Parent Management Training (PMT) [46] or Collaborative & Proactive Solutions (CPS) [47]. The PMT protocol was based on Barkley’s manualized training program [46]. The treatment consists of providing parents with psychoeducation on the causes of defiant, non-compliant behavior and teaching parents how to (1) implement positive attending through the use of “special time”; (2) use attending skills and effective commands to increase compliant behavior; (3) implement a contingency management program; (4) use the time-out procedure. The CPS protocol was based on Greene’s CPS model [47]. The CPS program builds on teaching parents how to solve problems collaboratively and proactively with their child. This involves teaching parents to (1) identify lagging skills and unsolved problems that contribute to defiant, non-compliant behaviors; and (2) techniques to solve these problems with their child. Both treatments have been found effective in treating ODD and have yielded equivalent and positive treatment outcomes [30,48]. Details of the treatment protocols and procedure are described elsewhere [30].
4. Statistical Analysis
The LPA is based on a step-wise procedure to identify profiles [49]. The Akaike Information Criterion (AIC) [50], Bayesian Information Criterion (BIC) [51], sample size adjusted BIC (ABIC) [52], Bootstrap Likelihood Ratio Test (BLRT), and entropy were used to determine the best fitting model. See Supplementary Materials for further details on the LPA, model fit indices, and descriptive statistics of the conduct problems and anxiety symptoms variables included in the LPA (Table S2).
After selecting the best-fitting model, tests of equality of means across latent profiles were conducted to examine whether profiles differed on demographic variables. In this procedure, class membership is held constant and a chi-square statistic for omnibus and pairwise comparisons across latent profiles is provided. If the omnibus tests are significant, the pairwise comparisons are explored. Given the non-normal distribution of several teacher-reported external validators (i.e., learning problems, study skills, and general aggression), non-parametric statistics were used to examine group differences. Raw scores were used for all analyses and α < 0.05 was considered significant. The Full Information Maximum Likelihood estimation was used to address missing data (see Supplementary Materials). Analyses were conducted using Mplus Version 7.1 [49].
5. Results
Table 1 displays demographics and clinical characteristics of the sample.

Table 1.
Demographics and clinical characteristics of the whole sample.
5.1. Latent Profile Classification
LPA was conducted to derive discrete profiles based on conduct problems and anxiety symptoms. Table 2 illustrates the fit indices based on the different models.

Table 2.
Fit indices for LPA Models with 1 to 4 classes.
Although the BIC increased with the three- and four-class models, the sample-size adjusted BIC continued to decrease, as did the AIC, and the BLRT p-value was significant, indicating that the model fit improved with the addition of each class. A five-class model failed to converge owing to local maxima (likely outliers that were unduly influencing class membership) and thus is not presented. As such, a four-class solution best fits the data (BIC = 5427.67, AIC = 5303.06, ABIC = 5291.65; see Figure 1 and Supplementary Materials for symptoms scores in Table S3).
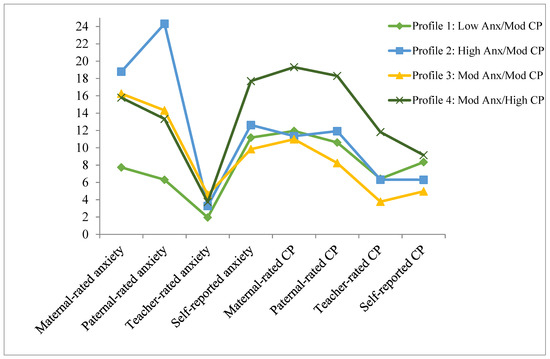
Figure 1.
Average anxiety and conduct problems (CP) for each class in the four-profile model. Note. Anx = anxiety, CP = conduct problems, mod = moderate.
In the four-class solution, Class 1 was characterized by lower levels of anxiety reported across informants relative to the other classes; however, the level of conduct problems was comparable to the other classes (Low Anxiety and Moderate Conduct Problems Class, Low Anx/Mod CP; n = 42). Class 2 was distinctive due to elevated levels of parent-reported anxiety symptoms and moderate conduct problems across informants (High Anxiety and Moderate Conduct Problems Class, High Anx/Mod CP; n = 33). Individuals in Class 3 obtained moderate levels of both conduct problems and anxiety symptoms across informants (Moderate Anxiety and Moderate Conduct Problems Class, Mod Anx/Mod CP; n = 40). Class 4 was characterized by high levels of conduct problems and moderate anxiety symptoms (Moderate Anxiety and High Conduct Problems Class, Mod Anx/High CP; n = 19).
5.2. Global Functioning and Treatment Outcomes
Table 3 displays means, standard deviations, and profile differences for external validators.

Table 3.
Comparison of external validators in the four-profile model.
5.2.1. Clinician Ratings
Prior to treatment, no profile differences in the ODD, anxiety disorder, and ADHD CSRs were noted. However, the two profiles with high symptom severity (High Anx/Mod CP and Mod Anx/High CP) were rated as more impaired overall, as measured using the CGAS, than the other two profiles.
The profiles did not differ in terms of the proportion of youths receiving each kind of treatment (p = 0.73). Comparable treatment outcomes were noted at post-treatment and the 6-month follow-ups across the profiles. However, at the 1-year follow-up, children in the Mod Anx/High CP class had significantly higher levels of ODD symptoms and lower clinician-rated global functioning than the children in the other profiles.
5.2.2. Parental Ratings
The profiles differed on maternal and paternal ratings of lability and emotional self-control, with higher levels of negative emotionality and difficulties regulating emotions and affect among youths in the High Anx/Mod CP and Mod Anx/High CP profiles compared to the Low Anx/Mod CP profile. Children in the Mod Anx/Mod CP profile were also rated by mothers as having greater difficulties with emotional self-control than children in the Low Anx/Mod CP profile.
Youths in the High Anx/Mod CP and Mod Anx/High CP profiles displayed higher levels of ODD and CD symptoms and aggression and displayed greater executive functioning deficits based on paternal reports than youths in the other profiles. Furthermore, higher levels of paternal-reported proactive aggression were noted among youths within the Mod Anx/High CP profile than those in the other profiles.
5.2.3. Teacher Ratings
Teachers rated the youths in the Mod Anx/High CP profile as the most impaired overall, with the highest levels of aggression, school problems, and learning problems, as well as the lowest study skills. Children in the Low Anx/Mod CP profile also had lower social and study skills than youths in the High Anx/Mod CP and Mod Anx/Mod CP profiles.
5.2.4. Self-Ratings
Youths within the Mod Anx/High CP profile reported higher levels of proactive and reactive aggression and lower self-concept than children in the other profiles.
6. Discussion
To the best of our knowledge, this study is the first to examine the differential clinical presentation and treatment outcomes of youths with ODD based on co-occurring conduct problems and anxiety symptoms using a person-centered approach. The LPA revealed four subgroups that differed across various areas of functioning, as well as long-term treatment outcomes.
Overall, children with high levels of conduct problems and moderate levels of anxiety symptoms (i.e., the Mod Anx/High CP subgroup) were the most impaired. Youths within this profile were the only ones that exhibited severe behavioral problems across multiple informants. They were also rated as having greater difficulties associated with negative emotionality, emotional self-control, and executive functioning by at least one informant. Although an initial symptom reduction was observed, children within this profile returned to similar levels of pre-treatment ODD symptoms at the 1-year follow-up, whereas treatment gains were largely maintained in the other profiles. This finding is consistent with other recent person-centered analyses on the poor prognosis of youths with high levels of conduct problems [7,8]. These collective findings suggest that augmented treatment may be necessary for youths in this subgroup if treatment gains are to be sustained over time. This approach may include parallel treatment for the anxiety symptoms or more transdiagnostic approaches that target broader underlying processes such as emotion regulation or executive functioning skills. Future studies should investigate whether adding such components yield better long-term outcomes.
A second profile emerged with comparable levels of anxiety as this impaired profile (i.e., Mod Anx/Mod CP subgroup). However, despite similar levels of anxiety, youths within the Mod Anx/Mod CP subgroup appeared to be higher functioning across multiple areas compared to the Mod Anx/High CP subgroup. Indeed, children within this subgroup displayed lower levels of behavioral problems across informants and were rated as having higher levels of effortful control and better social and study skills compared to children in the Mod Anx/High CP subgroup. Youths within the Mod Anx/Mod CP subgroup showed significant treatment gains that were maintained over time. This finding suggests that targeting behavioral problems for children with this type of symptom presentation is an effective treatment option.
The High Anx/Mod CP profile differed from the other profiles as they exhibited greater levels of anxiety symptoms according to their parents. Although slightly less impaired, youths within this subgroup were similar to the children in the Mod Anx/High CP subgroup. Specifically, children within this profile presented with elevated levels of conduct problems according to their fathers and also reportedly exhibited difficulties with emotion regulation and executive functioning based on parental reports. In terms of strengths, youths in the High Anx/Mod CP subgroup were rated as having higher study skills than children within the other profiles. Additionaly, unlike the Mod Anx/High CP subgroup, children in the High Anx/Mod CP subgroup maintained treatment gains at the 1-year follow-up. Theis finding suggests that current psychosocial treatments are generally effective for youths with this symptom presentation despite some functional deficits, similar to those observed in the multiple problem subgroup.
One profile was defined by low anxiety symptoms (the Low Anx/Mod CP class). Interestingly, youths within this profile were generally comparable in terms of overall functioning and treatment outcomes to the children in the Mod Anx/Mod CP subgroup, with a few exceptions. For instance, youths within this group had lower social and study skills according to their teachers than the Mod Anx/Mod CP profile.
Notably, several theories have been put forth to explain the mixed presentation of comorbid behavioral problems and anxiety among youths [23,53,54,55]. When comparing these theories, the two classes with comparable anxiety levels (i.e., Mod Anx/Mod CP and Mod Anx/High CP) in this study are perhaps most consistent with the dual-pathway model [23]. Specifically, Drabick and colleagues [23] proposed that anxiety mitigates the expression of ODD (i.e., the buffering hypothesis) among youths with low anger/frustration, moderate-to-high fear, high levels of proactive aggression, and age-appropriate levels of effortful control, executive functioning, and social information processing. Alternatively, they suggested anxiety exacerbates (i.e., the multiple-problem hypothesis) the expression of ODD among youths with high anger/frustration, low fear, low effortful control, high levels of reactive aggression, and poor executive functioning and interpersonal competence.
Another interesting finding in this study pertained to informant discrepancies in behavioral ratings. In accordance with previous studies (e.g., [56]), mothers generally provided higher ratings of problematic behaviors across subgroups than other informants. As a result, less variation between groups on external validators was observed based on maternal ratings than other informants. Such discrepancies in ratings have been attributed to the context in which the child is observed, child characteristics, and the rater’s attribution of the child’s behavior [57]. Thus, the addition of other informants yielded important clinical information. For instance, youths in the Mod Anx/High CP subgroup, who exhibited severe behavioral problems in the school setting according to teacher reports, had the worst treatment outcomes. This finding highlights the need to use a multi-informant approach when assessing behavioral problems to obtain a holistic picture of the child’s functioning and to inform treatment options.
Although the study possesses several strengths, such as using a multi-informant person-centered approach and the longitudinal assessment of treatment outcomes, there are several weaknesses. First, youths meeting the diagnostic criteria for CD were excluded from this study. However, many of the youths presented with subthreshold levels of CD symptoms (see Table 1), providing sufficient variability to conduct the LPA. Secondly, subgroups were based on conduct problems and anxiety symptoms, which are understudied but common among youths with ODD. Person-centered studies on how other commonly co-occurring psychiatric symptoms, such as ADHD symptoms, influence functioning and treatment outcomes of youths with ODD remain an important venture for future research. Finally, future studies are also needed to examine the longer-term trajectories of these subtypes. This study did provide some indication of prognosis by tracking participants for one year after treatment completion. However, further follow-up could be informative for prevention and treatment development to examine, for example, whether certain subtypes are more likely to develop depression and/or CD than others.
7. Conclusions
In conclusion, research on how conduct problems and anxiety symptoms influence functioning and treatment outcomes of youths with ODD has been scarce. Using a person-centered approach, we identified subtypes of ODD based on co-occurring conduct problems and anxiety that meaningfully differed in clinical presentation and treatment prognosis. This research highlights the need for determining more homogeneous subgroups within and across diagnostic categories to gain a deeper understanding of ODD, inform future nosological systems, and enhance intervention efforts.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph20043405/s1, Table S1. Assessment measures by informant and internal consistency of the subscales. Table S2. Means, standard deviations, range, and zero-order correlations among classification variables. Table S3. Symptom scores across the four-profile model. References [58,59,60] are cited in Supplementary Materials.
Author Contributions
T.H. and M.G.F. conceived the research question and designed the study in collaboration with T.H.O., T.H. and M.G.F. conducted the literature search. D.A.G.D. and T.H. completed the data analyses. T.H. drafted the initial draft of the manuscript. All authors revised and edited the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
Funding for ODD treatment trial was provided by R01 MH59308 from NIMH and by the Institute for Society, Culture, and Environment at Virginia Tech. THO served as PI for this grant award.
Institutional Review Board Statement
The study was reviewed and approved by the Institutional Review Board at Virginia Tech (#11-774).
Informed Consent Statement
Informed consent and assent was obtained from all families involved in the study. Written informed consent has been obtained from the families to publish research papers using the data acquired during the treatment for ODD.
Data Availability Statement
The data in this study are not publicly available due to patient confidentiality.
Acknowledgments
We express appreciation to graduate student colleagues and research scientists who assisted us with various aspects of this project, including assistance with data reduction, assessment, and treatment of the youths. We would also like to thank the many undergraduate students at Virginia Tech who assisted with data coding, entry, and verification. Finally, we are grateful to the youths and families who participated in this clinical research trial.
Conflicts of Interest
The authors have no conflict of interest to disclose.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Burke, J.D.; Rowe, R.; Boylan, K. Functional Outcomes of Child and Adolescent Oppositional Defiant Disorder Symptoms in Young Adult Men. J. Child Psychol. Psychiatry 2014, 55, 264–272. [Google Scholar] [CrossRef] [PubMed]
- Nock, M.K.; Kazdin, A.E.; Hiripi, E.; Kessler, R.C. Lifetime Prevalence, Correlates, and Persistence of Oppositional Defiant Disorder: Results from the National Comorbidity Survey Replication. J. Child Psychol. Psychiatry 2007, 48, 703–713. [Google Scholar] [CrossRef] [PubMed]
- Kaminski, J.W.; Claussen, A.H. Evidence Base Update for Psychosocial Treatments for Disruptive Behaviors in Children. J. Clin. Child Adolesc. Psychol. 2017, 46, 477–499. [Google Scholar] [CrossRef] [PubMed]
- Hawes, D.J.; Price, M.J.; Dadds, M.R. Callous-Unemotional Traits and the Treatment of Conduct Problems in Childhood and Adolescence: A Comprehensive Review. Clin. Child Fam. Psychol. Rev. 2014, 17, 248–267. [Google Scholar] [CrossRef]
- Foster, E.M.; Jones, D.E.; Conduct Problems Prevention Research Group. The High Costs of Aggression: Public Expenditures Resulting from Conduct Disorder. Am. J. Public Health 2005, 95, 1767–1772. [Google Scholar] [CrossRef]
- Roetman, P.J.; Siebelink, B.M.; Vermeiren, R.R.; Colins, O.F. Classes of Oppositional Defiant Disorder Behavior in Clinic-Referred Children and Adolescents: Concurrent Features and Outcomes: Classification Des Comportements Dans Le Trouble Oppositionnel Avec Provocation Chez Des Enfants et Des Adolescents Aiguillés à Une Clinique: Caractéristiques Co-Occurrentes et Résultats. Can. J. Psychiatry 2021, 66, 657–666. [Google Scholar]
- Racz, S.J.; McMahon, R.J.; Gudmundsen, G.; McCauley, E.; Vander Stoep, A. Latent Classes of Oppositional Defiant Disorder in Adolescence and Prediction to Later Psychopathology. Dev. Psychopathol. 2022, 1–19. [Google Scholar] [CrossRef]
- Lavigne, J.V.; Bryant, F.B.; Hopkins, J.; Gouze, K.R. Dimensions of Oppositional Defiant Disorder in Young Children: Model Comparisons, Gender and Longitudinal Invariance. J. Abnorm. Child Psychol. 2015, 43, 423–439. [Google Scholar] [CrossRef]
- Mikolajewski, A.J.; Taylor, J.; Iacono, W.G. Oppositional Defiant Disorder Dimensions: Genetic Influences and Risk for Later Psychopathology. J. Child Psychol. Psychiatry 2017, 58, 702–710. [Google Scholar] [CrossRef]
- Burke, J.D.; Boylan, K.; Rowe, R.; Duku, E.; Stepp, S.D.; Hipwell, A.E.; Waldman, I.D. Identifying the Irritability Dimension of ODD: Application of a Modified Bifactor Model across Five Large Community Samples of Children. J. Abnorm. Psychol. 2014, 123, 841. [Google Scholar] [CrossRef]
- Waldman, I.D.; Rowe, R.; Boylan, K.; Burke, J.D. External Validation of a Bifactor Model of Oppositional Defiant Disorder. Mol. Psychiatry 2018, 26, 1. [Google Scholar] [CrossRef]
- Boylan, K.; Vaillancourt, T.; Boyle, M.; Szatmari, P. Comorbidity of Internalizing Disorders in Children with Oppositional Defiant Disorder. Eur. Child Adolesc. Psychiatry 2007, 16, 484–494. [Google Scholar] [CrossRef]
- Maughan, B.; Rowe, R.; Messer, J.; Goodman, R.; Meltzer, H. Conduct Disorder and Oppositional Defiant Disorder in a National Sample: Developmental Epidemiology. J. Child Psychol. Psychiatry 2004, 45, 609–621. [Google Scholar] [CrossRef]
- Déry, M.; Lapalme, M.; Jagiellowicz, J.; Poirier, M.; Temcheff, C.; Toupin, J. Predicting Depression and Anxiety from Oppositional Defiant Disorder Symptoms in Elementary School-Age Girls and Boys with Conduct Problems. Child Psychiatry Hum. Dev. 2017, 48, 53–62. [Google Scholar] [CrossRef]
- Cunningham, N.R.; Ollendick, T.H. Comorbidity of Anxiety and Conduct Problems in Children: Implications for Clinical Research and Practice. Clin. Child Fam. Psychol. Rev. 2010, 13, 333–347. [Google Scholar] [CrossRef]
- Boden, J.M.; Fergusson, D.M.; Horwood, L.J. Risk Factors for Conduct Disorder and Oppositional/Defiant Disorder: Evidence from a New Zealand Birth Cohort. J. Am. Acad. Child Adolesc. Psychiatry 2010, 49, 1125–1133. [Google Scholar] [CrossRef]
- Drabick, D.A.G.; Gadow, K.D.; Loney, J. Co-Occurring ODD and GAD Symptom Groups: Source-Specific Syndromes and Cross-Informant Comorbidity. J. Clin. Child Adolesc. Psychol. 2008, 37, 314–326. [Google Scholar] [CrossRef]
- Wesselhoeft, R.; Stringaris, A.; Sibbersen, C.; Kristensen, R.V.; Bojesen, A.B.; Talati, A. Dimensions and Subtypes of Oppositionality and Their Relation to Comorbidity and Psychosocial Characteristics. Eur. Child Adolesc. Psychiatry 2018, 28, 351–365. [Google Scholar] [CrossRef]
- Beauchaine, T.P.; Webster-Stratton, C.; Reid, M.J. Mediators, Moderators, and Predictors of 1-Year Outcomes among Children Treated for Early-Onset Conduct Problems: A Latent Growth Curve Analysis. J. Consult. Clin. Psychol. 2005, 73, 371. [Google Scholar] [CrossRef]
- Franco, X.; Saavedra, L.M.; Silverman, W.K. External Validation of Comorbid Patterns of Anxiety Disorders in Children and Adolescents. J. Anxiety Disord. 2007, 21, 717–729. [Google Scholar] [CrossRef]
- Walker, J.L.; Lahey, B.B.; Russo, M.F.; Frick, P.J.; Christ, M.A.G.; McBurnett, K.; Loeber, R.; Stouthamer-Loeber, M.; Green, S.M. Anxiety, Inhibition, and Conduct Disorder in Children: I. Relations to Social Impairment. J. Am. Acad. Child Adolesc. Psychiatry 1991, 30, 187–191. [Google Scholar] [CrossRef] [PubMed]
- Drabick, D.A.G.; Ollendick, T.H.; Bubier, J.L. Co-occurrence of ODD and Anxiety: Shared Risk Processes and Evidence for a Dual-pathway Model. Clin. Psychol. Sci. Pract. 2010, 17, 307–318. [Google Scholar] [CrossRef] [PubMed]
- Sachser, C.; Keller, F.; Goldbeck, L. Complex PTSD as Proposed for ICD-11: Validation of a New Disorder in Children and Adolescents and Their Response to Trauma-Focused Cognitive Behavioral Therapy. J. Child Psychol. Psychiatry Allied Discip. 2017, 58, 160–168. [Google Scholar] [CrossRef] [PubMed]
- Iampietro, M.; Giovannetti, T.; Drabick, D.A.; Kessler, R.K. Empirically Defined Patterns of Executive Function Deficits in Schizophrenia and Their Relation to Everyday Functioning: A Person-Centered Approach. Clin. Neuropsychol. 2012, 26, 1166–1185. [Google Scholar] [CrossRef] [PubMed]
- Andrade, B.F.; Waschbusch, D.A.; King, S.; Thurston, C.; McNutt, L.; Terrio, B.; Northern Partners in Action for Children and Youth, Nova Scotia. Teacher-Classified Peer Social Status: Preliminary Validation and Associations with Behavior Ratings. J. Psychoeduc. Assess. 2005, 23, 279–290. [Google Scholar] [CrossRef]
- Herzhoff, K.; Tackett, J.L. Subfactors of Oppositional Defiant Disorder: Converging Evidence from Structural and Latent Class Analyses. J. Child Psychol. Psychiatry 2016, 57, 18–29. [Google Scholar] [CrossRef]
- Althoff, R.R.; Kuny-Slock, A.V.; Verhulst, F.C.; Hudziak, J.J.; Ende, J. Classes of Oppositional-defiant Behavior: Concurrent and Predictive Validity. J. Child Psychol. Psychiatry 2014, 55, 1162–1171. [Google Scholar] [CrossRef]
- Aebi, M.; Barra, S.; Bessler, C.; Steinhausen, H.-C.; Walitza, S.; Plattner, B. Oppositional Defiant Disorder Dimensions and Subtypes among Detained Male Adolescent Offenders. J. Child Psychol. Psychiatry 2016, 57, 729–736. [Google Scholar] [CrossRef]
- Ollendick, T.H.; Greene, R.W.; Austin, K.E.; Fraire, M.G.; Halldorsdottir, T.; Allen, K.B.; Jarrett, M.A.; Lewis, K.M.; Whitmore Smith, M.; Cunningham, N.R.; et al. Parent Management Training and Collaborative & Proactive Solutions: A Randomized Control Trial for Oppositional Youth. J. Clin. Child Adolesc. Psychol. 2016, 45, 591–604. [Google Scholar] [CrossRef]
- Bögels, S.M.; Brechman-Toussaint, M.L. Family Issues in Child Anxiety: Attachment, Family Functioning, Parental Rearing and Beliefs. Clin. Psychol. Rev. 2006, 26, 834–856. [Google Scholar] [CrossRef]
- Kusche, C.A.; Cook, E.T.; Greenberg, M.T. Neuropsychological and Cognitive Functioning in Children with Anxiety, Externalizing, and Comorbid Psychopathology. J. Clin. Child Psychol. 1993, 22, 172–195. [Google Scholar] [CrossRef]
- Muris, P.; Ollendick, T.H. The Role of Temperament in the Etiology of Child Psychopathology. Clin. Child Fam. Psychol. Rev. 2005, 8, 271–289. [Google Scholar] [CrossRef]
- Raine, A.; Dodge, K.; Loeber, R.; Gatzke-Kopp, L.; Lynam, D.; Reynolds, C.; Stouthamer-Loeber, M.; Liu, J. The Reactive–Proactive Aggression Questionnaire: Differential Correlates of Reactive and Proactive Aggression in Adolescent Boys. Aggress. Behav. 2006, 32, 159–171. [Google Scholar] [CrossRef]
- Cavanagh, M.; Quinn, D.; Duncan, D.; Graham, T.; Balbuena, L. Oppositional Defiant Disorder Is Better Conceptualized as a Disorder of Emotional Regulation. J. Atten. Disord. 2017, 21, 381–389. [Google Scholar] [CrossRef]
- Suveg, C.; Sood, E.; Comer, J.S.; Kendall, P.C. Changes in Emotion Regulation Following Cognitive-Behavioral Therapy for Anxious Youth. J. Clin. Child Adolesc. Psychol. 2009, 38, 390–401. [Google Scholar] [CrossRef]
- Fraire, M.G.; Ollendick, T.H. Anxiety and Oppositional Defiant Disorder: A Transdiagnostic Conceptualization. Clin. Psychol. Rev. 2013, 33, 229–240. [Google Scholar] [CrossRef]
- Reynolds, C.R. Behavior Assessment System for Children; Wiley Online Library: Hoboken, NJ, USA, 2004. [Google Scholar]
- Pelham, W.E.; Evans, S.W.; Gnagy, E.M.; Greenslade, K.E. Teacher Ratings of DSM-III-R Symptoms for the Disruptive Behavior Disorders: Prevalence, Factor Analyses, and Conditional Probabilities in a Special Education Sample. Sch. Psychol. Rev. 1992, 21, 285–299. [Google Scholar] [CrossRef]
- Beck, J.S. Beck Youth Inventories—Second Edition for Children and Adolescents Manual; Psychological Corporation: San Antonio, TX, USA, 2005. [Google Scholar]
- Silverman, W.K.; Albano, A.M. The Anxiety Disorders Interview Schedule for Children (ADIS-C/P); Psychological Corporation: San Antonio, TX, USA, 1996. [Google Scholar]
- Shaffer, D.; Gould, M.S.; Brasic, J.; Ambrosini, P.; Fisher, P.; Bird, H.; Aluwahlia, S. A Children’s Global Assessment Scale (CGAS). Arch. Gen. Psychiatry 1983, 40, 1228–1231. [Google Scholar] [CrossRef]
- Shields, A.; Cicchetti, D. Emotion Regulation among School-Age Children: The Development and Validation of a New Criterion Q-Sort Scale. Dev. Psychol. 1997, 33, 906. [Google Scholar] [CrossRef]
- Brown, K.; Atkins, M.S.; Osborne, M.L.; Milnamow, M. A Revised Teacher Rating Scale for Reactive and Proactive Aggression. J. Abnorm. Child Psychol. 1996, 24, 473–480. [Google Scholar] [CrossRef]
- Gioia, G.A.; Guy, S.C.; Isquith, P.K.; Kenworthy, L. Behavior Rating Inventory of Executive Function; Psychological Assessment Resources: Lutz, FL, USA, 1996. [Google Scholar]
- Barkley, R.A. Defiant Children: A Clinician’s Manual for Parent Training and Assessment; Psychological Corporation: San Antonio, TX, USA, 1997. [Google Scholar]
- Greene, R.W. The Explosive Child: A New Approach for Understanding and Parenting Easily Frustrated," Chronically Inflexible" Children; HarperCollins Publishers: New York, NY, USA, 1998. [Google Scholar]
- Murrihy, R.C.; Drysdale, S.A.; Dedousis-Wallace, A.; Rémond, L.; McAloon, J.; Ellis, D.M.; Halldorsdottir, T.; Greene, R.W.; Ollendick, T.H. Community-Delivered Collaborative and Proactive Solutions and Parent Management Training for Oppositional Youth: A Randomized Trial. Behav. Ther. 2022. [Google Scholar] [CrossRef]
- Muthén, L.K. Mplus User’s Guide; Muthén & Muthén: Los Angeles, CA, USA, 2010. [Google Scholar]
- Akaike, H. Factor Analysis and AIC. Psychometrika 1987, 52, 317–332. [Google Scholar] [CrossRef]
- Schwarz, G. Estimating the Dimension of a Model. Ann. Stat. 1978, 6, 461–464. [Google Scholar] [CrossRef]
- Sclove, S.L. Application of Model-Selection Criteria to Some Problems in Multivariate Analysis. Psychometrika 1987, 52, 333–343. [Google Scholar] [CrossRef]
- Frick, P.J.; Morris, A.S. Temperament and Developmental Pathways to Conduct Problems. J. Clin. Child Adolesc. Psychol. 2004, 33, 54–68. [Google Scholar] [CrossRef]
- Frick, P.J.; Ellis, M. Callous-Unemotional Traits and Subtypes of Conduct Disorder. Clin. Child Fam. Psychol. Rev. 1999, 2, 149–168. [Google Scholar] [CrossRef]
- Gray, J.A. The Psychology of Fear and Stress; CUP Archive: Cambridge, UK, 1987; Volume 5. [Google Scholar]
- Drabick, D.A.G.; Bubier, J.; Chen, D.; Price, J.; Lanza, H.I. Source-Specific Oppositional Defiant Disorder among Inner-City Children: Prospective Prediction and Moderation. J. Clin. Child Adolesc. Psychol. 2011, 40, 23–35. [Google Scholar] [CrossRef]
- De Los Reyes, A.; Augenstein, T.M.; Wang, M.; Thomas, S.A.; Drabick, D.A.G.; Burgers, D.E.; Rabinowitz, J. The Validity of the Multi-Informant Approach to Assessing Child and Adolescent Mental Health. Psychol. Bull. 2015, 141, 858. [Google Scholar] [CrossRef]
- Anderson, S.R.; Ollendick, T.H. Diagnosing Oppositional Defiant Disorder Using the Anxiety Disorders Interview Schedule for DSM-IV: Parent Version and the Diagnostic Interview Schedule for Children. J. Psychopathol. Behav. Assess. 2012, 34, 467–475. [Google Scholar] [CrossRef]
- Nylund, K.; Bellmore, A.; Nishina, A.; Graham, S. Subtypes, Severity, and Structural Stability of Peer Victimization: What Does Latent Class Analysis Say? Child Dev. 2007, 78, 1706–1722. [Google Scholar] [CrossRef]
- Nylund, K.L.; Asparouhov, T.; Muthén, B.O. Deciding on the Number of Classes in Latent Class Analysis and Growth Mixture Modeling: A Monte Carlo Simulation Study. Struct. Equ. Model. 2007, 14, 535–569. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).