A 1-Week Comprehensive Foam Rolling Intervention Program Can Improve Knee Pain but Not Muscle Function and Range of Motion in Patients with Total Knee Arthroplasty
Abstract
:1. Introduction
2. Materials and Methods
2.1. Experimental Design
2.2. Participants
2.3. Regular Physical Therapy Intervention
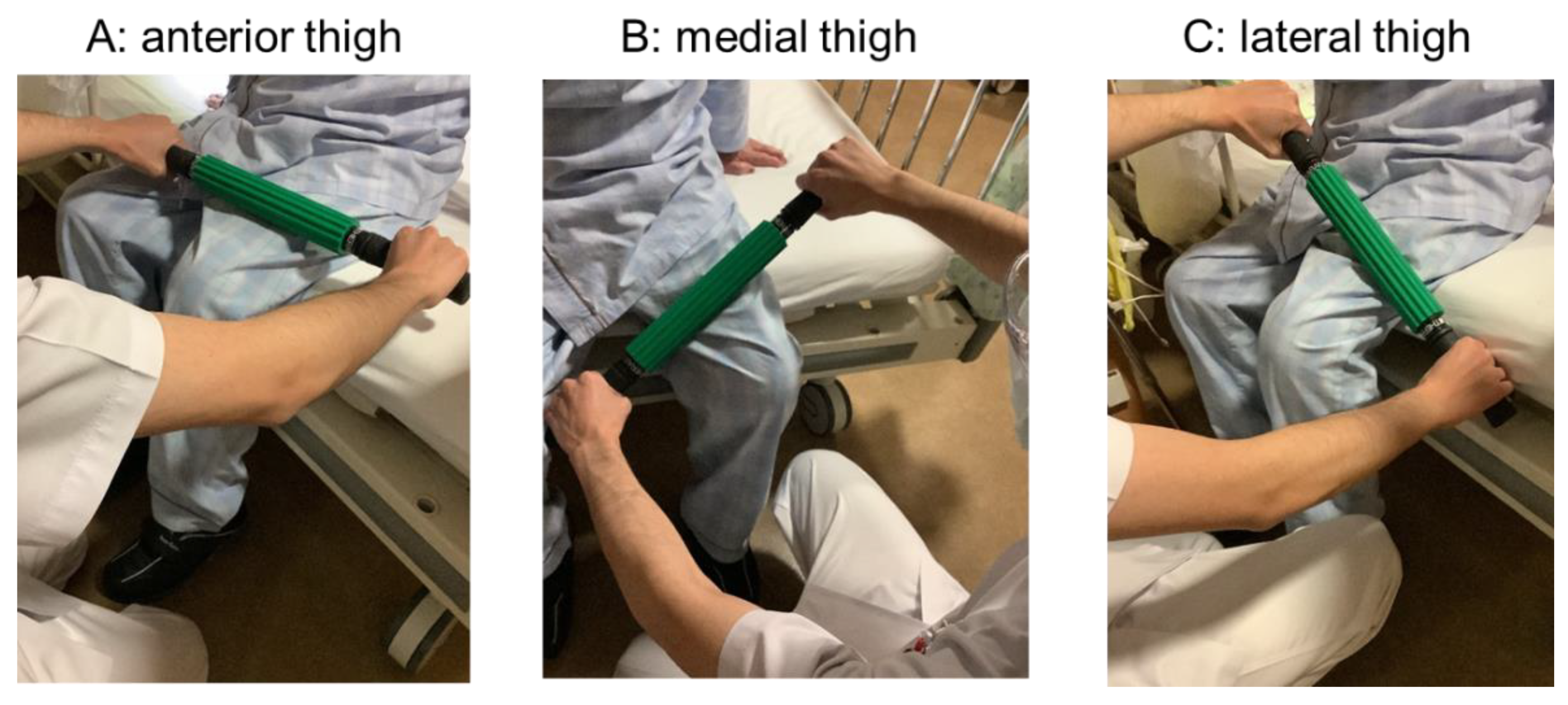
2.4. FR Exercise
2.5. Knee Flexion and Extension ROM Measurement
2.6. Pain Measurement
2.7. Walking Measurements
2.8. Balance Measurements
2.9. Muscle Strength Measurement
2.10. Statistical Analysis
3. Results
4. Discussion
5. Limitation
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Milner, C.E. Is gait normal after total knee arthroplasty? Systematic review of the literature. J. Orthop. Sci. Off. J. Jpn. Orthop. Assoc. 2009, 14, 114–120. [Google Scholar] [CrossRef] [PubMed]
- Furu, M.; Ito, H.; Nishikawa, T.; Nankaku, M.; Kuriyama, S.; Ishikawa, M.; Nakamura, S.; Azukizawa, M.; Hamamoto, Y.; Matsuda, S. Quadriceps strength affects patient satisfaction after total knee arthroplasty. J. Orthop. Sci. Off. J. Jpn. Orthop. Assoc. 2016, 21, 38–43. [Google Scholar] [CrossRef] [PubMed]
- Foroughi, N.; Smith, R.; Vanwanseele, B. The association of external knee adduction moment with biomechanical variables in osteoarthritis: A systematic review. Knee 2009, 16, 303–309. [Google Scholar] [CrossRef] [PubMed]
- Scranton, P.E., Jr. Management of knee pain and stiffness after total knee arthroplasty. J. Arthroplast. 2001, 16, 428–435. [Google Scholar] [CrossRef]
- Daluga, D.; Lombardi, A.V., Jr.; Mallory, T.H.; Vaughn, B.K. Knee manipulation following total knee arthroplasty. Analysis of prognostic variables. J. Arthroplast. 1991, 6, 119–128. [Google Scholar] [CrossRef] [PubMed]
- Mauerhan, D.R.; Mokris, J.G.; Ly, A.; Kiebzak, G.M. Relationship between length of stay and manipulation rate after total knee arthroplasty. J. Arthroplast. 1998, 13, 896–900. [Google Scholar] [CrossRef] [PubMed]
- Witvrouw, E.; Bellemans, J.; Victor, J. Manipulation under anaesthesia versus low stretch device in poor range of motion after TKA. Knee Surg. Sports Traumatol. Arthrosc. Off. J. ESSKA 2013, 21, 2751–2758. [Google Scholar] [CrossRef]
- Nakamura, M.; Yasaka, K.; Kiyono, R.; Onuma, R.; Yahata, K.; Sato, S.; Konrad, A. The Acute Effect of Foam Rolling on Eccentrically-Induced Muscle Damage. Int. J. Environ. Res. Public Health 2020, 18, 75. [Google Scholar] [CrossRef]
- Konrad, A.; Nakamura, M.; Tilp, M.; Donti, O.; Behm, D.G. Foam Rolling Training Effects on Range of Motion: A Systematic Review and Meta-Analysis. Sports Med. 2022, 52, 2523–2535. [Google Scholar] [CrossRef]
- Kiyono, R.; Onuma, R.; Yasaka, K.; Sato, S.; Yahata, K.; Nakamura, M. Effects of 5-Week Foam Rolling Intervention on Range of Motion and Muscle Stiffness. J. Strength Cond. Res. 2020, 36, 1890–1895. [Google Scholar] [CrossRef]
- Kasahara, K.; Konrad, A.; Yoshida, R.; Murakami, Y.; Sato, S.; Aizawa, K.; Koizumi, R.; Thomas, E.; Nakamura, M. Comparison between 6-week foam rolling intervention program with and without vibration on rolling and non-rolling sides. Eur. J. Appl. Physiol. 2022, 122, 2061–2070. [Google Scholar] [CrossRef] [PubMed]
- Ikutomo, H.; Nagai, K.; Tagomori, K.; Miura, N.; Okamura, K.; Okuno, T.; Nakagawa, N.; Masuhara, K. Effects of foam rolling on hip pain in patients with hip osteoarthritis: A retrospective propensity-matched cohort study. Physiother. Theory Pract. 2022, 38, 995–1002. [Google Scholar] [CrossRef] [PubMed]
- Ughreja, R.A.; Venkatesan, P.; Balebail Gopalakrishna, D.; Singh, Y.P. Effectiveness of myofascial release on pain, sleep, and quality of life in patients with fibromyalgia syndrome: A systematic review. Complement. Ther. Clin. Pract. 2021, 45, 101477. [Google Scholar] [CrossRef] [PubMed]
- Weerapong, P.; Hume, P.A.; Kolt, G.S. The mechanisms of massage and effects on performance, muscle recovery and injury prevention. Sports Med. 2005, 35, 235–256. [Google Scholar] [CrossRef]
- Lo, C.W.T.; Tsang, W.W.N.; Yan, C.H.; Lord, S.R.; Hill, K.D.; Wong, A.Y.L. Risk factors for falls in patients with total hip arthroplasty and total knee arthroplasty: A systematic review and meta-analysis. Osteoarthr. Cartil. 2019, 27, 979–993. [Google Scholar] [CrossRef]
- Kampitak, W.; Tanavalee, A.; Ngarmukos, S.; Amarase, C.; Songthamwat, B.; Boonshua, A. Comparison of Adductor Canal Block Versus Local Infiltration Analgesia on Postoperative Pain and Functional Outcome after Total Knee Arthroplasty: A Randomized Controlled Trial. Malays. Orthop. J. 2018, 12, 7–14. [Google Scholar] [CrossRef]
- Reiner, M.M.; Glashüttner, C.; Bernsteiner, D.; Tilp, M.; Guilhem, G.; Morales-Artacho, A.; Konrad, A. A comparison of foam rolling and vibration foam rolling on the quadriceps muscle function and mechanical properties. Eur. J. Appl. Physiol. 2021, 121, 1461–1471. [Google Scholar] [CrossRef]
- Matsuda, S.; Kawahara, S.; Okazaki, K.; Tashiro, Y.; Iwamoto, Y. Postoperative alignment and ROM affect patient satisfaction after TKA. Clin. Orthop. Relat. Res. 2013, 471, 127–133. [Google Scholar] [CrossRef]
- Hawker, G.A.; Mian, S.; Kendzerska, T.; French, M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res. 2011, 63 (Suppl. S11), S240–S252. [Google Scholar] [CrossRef]
- Davut, S.; Huzmeli, I.; Hallaceli, H.; Kalacı, A. Does Total Knee Arthroplasty Positively Affect Body Static-Dynamic Balance and Fall Risk Parameters in Patients with Satisfactory Functional Scores? Cureus 2022, 14, e30207. [Google Scholar] [CrossRef]
- Pinto-Ramos, J.; Moreira, T.; Costa, F.; Tavares, H.; Cabral, J.; Costa-Santos, C.; Barroso, J.; Sousa-Pinto, B. Handheld dynamometer reliability to measure knee extension strength in rehabilitation patients-A cross-sectional study. PLoS ONE 2022, 17, e0268254. [Google Scholar] [CrossRef]
- Seo, S.S.; Kim, O.G.; Seo, J.H.; Kim, D.H.; Kim, Y.G.; Park, B.Y. Comparison of the Effect of Continuous Femoral Nerve Block and Adductor Canal Block after Primary Total Knee Arthroplasty. Clin. Orthop. Surg. 2017, 9, 303–309. [Google Scholar] [CrossRef] [PubMed]
- Dubljanin Raspopović, E.; Meissner, W.; Zaslansky, R.; Kadija, M.; Tomanović Vujadinović, S.; Tulić, G. Associations between early postoperative pain outcome measures and late functional outcomes in patients after knee arthroplasty. PLoS ONE 2021, 16, e0253147. [Google Scholar] [CrossRef] [PubMed]
- Danoff, J.R.; Goel, R.; Sutton, R.; Maltenfort, M.G.; Austin, M.S. How Much Pain Is Significant? Defining the Minimal Clinically Important Difference for the Visual Analog Scale for Pain After Total Joint Arthroplasty. J. Arthroplast. 2018, 33, S71–S75.e2. [Google Scholar] [CrossRef] [PubMed]
- Schroeder, A.N.; Best, T.M. Is self myofascial release an effective preexercise and recovery strategy? A literature review. Curr. Sports Med. Rep. 2015, 14, 200–208. [Google Scholar] [CrossRef]
- Cheatham, S.W.; Kolber, M.J.; Cain, M.; Lee, M. The effects of self-myofascial release using a foam roll or roller massager on joint range of motion, muscle recovery, and performance: A systematic review. Int. J. Sports Phys. Ther. 2015, 10, 827–838. [Google Scholar]
- Konrad, A.; Nakamura, M.; Behm, D.G. The Effects of Foam Rolling Training on Performance Parameters: A Systematic Review and Meta-Analysis including Controlled and Randomized Controlled Trials. Int. J. Environ. Res. Public Health 2022, 19, 11638. [Google Scholar] [CrossRef]

| FR Group | Control Group | |||||
|---|---|---|---|---|---|---|
| PRE | POST | Δ Change | PRE | POST | Δ Change | |
| Knee flexion ROM (°) | 97.0 ± 10.5 | 106.3 ± 9.5 * | 9.3 ± 4.7 | 102.0 ± 10.8 | 111.0 ± 7.1 * | 9.0 ± 4.5 |
| d= | 0.96 | p < 0.01 | d= | 1.04 | p < 0.01 | |
| Knee extension ROM (°) | −4.0 ± 3.9 | −3.0 ± 3.7 * | 1.0 ± 0.5 | −7.3 ± 5.6 | −5.3 ± 4.0 * | 2.0 ± 1 |
| d= | 0.27 | p < 0.01 | d= | 0.43 | p < 0.01 | |
| Pain score at rest (mm) | 9.9 ± 11.7 | 1.3 ± 3.0 * | −8.6 ± 4.3 | 17.1 ± 20.2 | 5.3 ± 13.6 * | −11.8 ± 5.9 |
| d= | −1.21 | p < 0.01 | d= | −0.72 | p < 0.01 | |
| Pain score at stretching (mm) | 38.4 ± 18.3 | 12.4 ± 19.7 * | −26 ± 13 | 30.2 ± 13.9 | 17.7 ± 15.8 * | −12.47 ± 6.2 |
| d= | −1.42 | p < 0.01 | d= | −0.87 | p < 0.01 | |
| Knee extension strength (N/kg) | 1.2 ± 0.4 | 1.5 ± 0.5 * | 0.36 ± 0.2 | 1.2 ± 0.5 | 1.6 ± 0.5 * | 0.3 ± 0.2 |
| d= | 0.79 | p < 0.01 | d= | 0.63 | p < 0.01 | |
| 10-m walking test (s) | 14.2 ± 5.5 | 11.4 ± 3.5 * | −2.8 ± 1.4 | 14.9 ± 5.0 | 12.5 ± 2.8 * | −2.4 ± 1.2 |
| d= | −0.65 | p < 0.01 | d= | −0.64 | p < 0.01 | |
| TUG (s) | 17.2 ± 6.0 | 12.8 ± 3.5 * | −4.5 ± 2.2 | 20.0 ± 4.6 | 14.2 ± 3.7 * | −5.9 ± 2.9 |
| d= | −0.97 | p < 0.01 | d= | −1.47 | p < 0.01 | |
| One-leg standing time (s) | 4.9 ± 5.5 | 6.7 ± 5.1 * | 1.7 ± 0.9 | 4.9 ± 5.8 | 8.4 ± 8.3 * | 3.5 ± 1.7 |
| d= | 0.34 | p < 0.01 | d= | 0.51 | p < 0.01 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yokochi, M.; Nakamura, M.; Iwata, A.; Kaneko, R.; Watanabe, S.; Konrad, A.; Yamada, N. A 1-Week Comprehensive Foam Rolling Intervention Program Can Improve Knee Pain but Not Muscle Function and Range of Motion in Patients with Total Knee Arthroplasty. Int. J. Environ. Res. Public Health 2023, 20, 3351. https://doi.org/10.3390/ijerph20043351
Yokochi M, Nakamura M, Iwata A, Kaneko R, Watanabe S, Konrad A, Yamada N. A 1-Week Comprehensive Foam Rolling Intervention Program Can Improve Knee Pain but Not Muscle Function and Range of Motion in Patients with Total Knee Arthroplasty. International Journal of Environmental Research and Public Health. 2023; 20(4):3351. https://doi.org/10.3390/ijerph20043351
Chicago/Turabian StyleYokochi, Masanobu, Masatoshi Nakamura, Ayaka Iwata, Ryota Kaneko, Shiho Watanabe, Andreas Konrad, and Noboru Yamada. 2023. "A 1-Week Comprehensive Foam Rolling Intervention Program Can Improve Knee Pain but Not Muscle Function and Range of Motion in Patients with Total Knee Arthroplasty" International Journal of Environmental Research and Public Health 20, no. 4: 3351. https://doi.org/10.3390/ijerph20043351
APA StyleYokochi, M., Nakamura, M., Iwata, A., Kaneko, R., Watanabe, S., Konrad, A., & Yamada, N. (2023). A 1-Week Comprehensive Foam Rolling Intervention Program Can Improve Knee Pain but Not Muscle Function and Range of Motion in Patients with Total Knee Arthroplasty. International Journal of Environmental Research and Public Health, 20(4), 3351. https://doi.org/10.3390/ijerph20043351










