Exploring Radiologists’ Burnout in the COVID-19 Era: A Narrative Review
Abstract
:1. Introduction
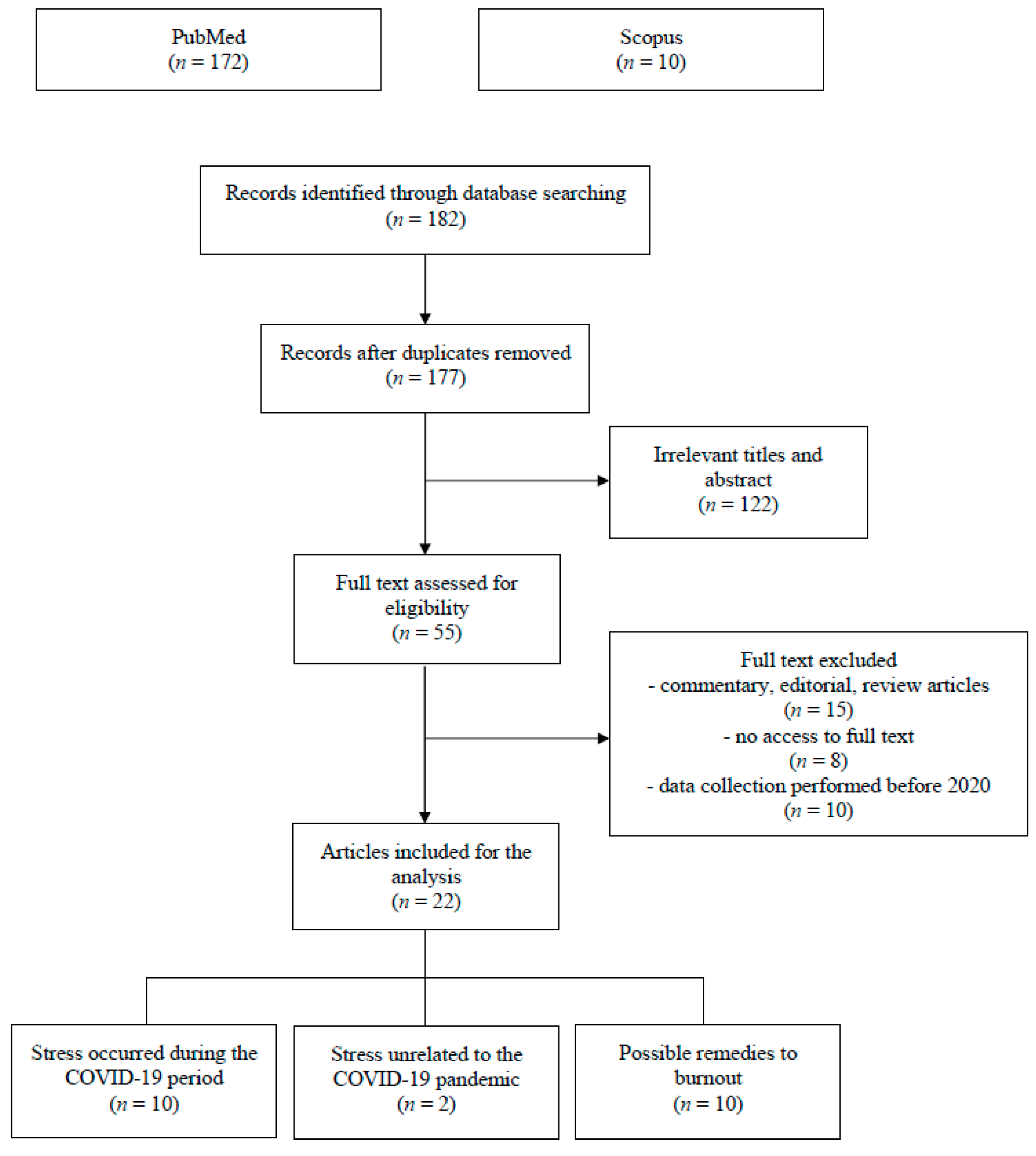
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Maslach, C.; Leiter, M.P. Understanding the Burnout Experience: Recent Research and Its Implications for Psychiatry. World Psychiatry 2016, 15, 103–111. [Google Scholar] [CrossRef] [PubMed]
- Guenette, J.P.; Smith, S.E. Burnout: Prevalence and Associated Factors Among Radiology Residents in New England with Comparison Against United States Resident Physicians in Other Specialties. AJR Am. J. Roentgenol. 2017, 209, 136–141. [Google Scholar] [CrossRef] [PubMed]
- Zha, N.; Patlas, M.N.; Neuheimer, N.; Duszak, R., Jr. Prevalence of Burnout Among Canadian Radiologists and Radiology Trainees. Can. Assoc. Radiol. J. 2018, 69, 367–372. [Google Scholar] [CrossRef]
- Kumar, S. Burnout and Doctors: Prevalence, Prevention and Intervention. Healthcare 2016, 4, 37. [Google Scholar] [CrossRef] [PubMed]
- Higgins, M.C.S.S.; Higgins, M.C.S.; Nguyen, M.-T.; Kosowsky, T.; Unan, L.; Mete, M.; Rowe, S.; Marchalik, D. Burnout, Professional Fulfillment, Intention to Leave, and Sleep-Related Impairment Among Faculty Radiologists in the United States: An Epidemiologic Study. J. Am. Coll. Radiol. 2021, 18, 1359–1364. [Google Scholar] [CrossRef] [PubMed]
- Spieler, B.; Baum, N. Burnout: A Mindful Framework for the Radiologist. Curr. Probl. Diagn. Radiol. 2022, 51, 155–161. [Google Scholar] [CrossRef]
- Taranu, S.M.; Ilie, A.C.; Turcu, A.-M.; Stefaniu, R.; Sandu, I.A.; Pislaru, A.I.; Alexa, I.D.; Sandu, C.A.; Rotaru, T.-S.; Alexa-Stratulat, T. Factors Associated with Burnout in Healthcare Professionals. Int. J. Environ. Res. Public Health 2022, 19, 14701. [Google Scholar] [CrossRef]
- Scapicchio, C.; Gabelloni, M.; Barucci, A.; Cioni, D.; Saba, L.; Neri, E. A Deep Look into Radiomics. Radiol. Med. 2021, 126, 1296–1311. [Google Scholar] [CrossRef]
- Nardone, V.; Reginelli, A.; Grassi, R.; Boldrini, L.; Vacca, G.; D’Ippolito, E.; Annunziata, S.; Farchione, A.; Belfiore, M.P.; Desideri, I.; et al. Delta Radiomics: A Systematic Review. Radiol. Med. 2021, 126, 1571–1583. [Google Scholar] [CrossRef]
- Vicini, S.; Bortolotto, C.; Rengo, M.; Ballerini, D.; Bellini, D.; Carbone, I.; Preda, L.; Laghi, A.; Coppola, F.; Faggioni, L. A Narrative Review on Current Imaging Applications of Artificial Intelligence and Radiomics in Oncology: Focus on the Three Most Common Cancers. Radiol. Med. 2022, 127, 819–836. [Google Scholar] [CrossRef]
- Aiello, M. Is Radiomics Growing towards Clinical Practice? J. Pers. Med. 2022, 12, 1373. [Google Scholar] [CrossRef]
- Saini, A.; Breen, I.; Pershad, Y.; Naidu, S.; Knuttinen, M.G.; Alzubaidi, S.; Sheth, R.; Albadawi, H.; Kuo, M.; Oklu, R. Radiogenomics and Radiomics in Liver Cancers. Diagnostics 2018, 9, 4. [Google Scholar] [CrossRef]
- Peng, Y.-C.; Lee, W.-J.; Chang, Y.-C.; Chan, W.P.; Chen, S.-J. Radiologist Burnout: Trends in Medical Imaging Utilization under the National Health Insurance System with the Universal Code Bundling Strategy in an Academic Tertiary Medical Centre. Eur. J. Radiol. 2022, 157, 110596. [Google Scholar] [CrossRef]
- Ratwani, R.M.; Wang, E.; Fong, A.; Cooper, C.J. A Human Factors Approach to Understanding the Types and Sources of Interruptions in Radiology Reading Rooms. J. Am. Coll. Radiol. 2016, 13, 1102–1105. [Google Scholar] [CrossRef] [PubMed]
- Khalifa, S.A.M.; Swilam, M.M.; El-Wahed, A.A.A.; Du, M.; El-Seedi, H.H.R.; Kai, G.; Masry, S.H.D.; Abdel-Daim, M.M.; Zou, X.; Halabi, M.F.; et al. Beyond the Pandemic: COVID-19 Pandemic Changed the Face of Life. Int. J. Environ. Res. Public Health 2021, 18, 5645. [Google Scholar] [CrossRef] [PubMed]
- Fandrejewska, A.; Chmielarz, W.; Zborowski, M. The Impact of the COVID-19 Pandemic on the Perception of Globalization and Consumer Behavior. Sustainability 2022, 14, 9575. [Google Scholar] [CrossRef]
- Choi, Y.; Kim, H.-J.; Lee, Y. Economic Consequences of the COVID-19 Pandemic: Will It Be a Barrier to Achieving Sustainability? Sustainability 2022, 14, 1629. [Google Scholar] [CrossRef]
- Anastasi, E.; Manganaro, L.; Guiducci, E.; Ciaglia, S.; Dolciami, M.; Spagnoli, A.; Alessandri, F.; Angeloni, A.; Vestri, A.; Catalano, C.; et al. Association of Serum Krebs von Den Lungen-6 and Chest CT as Potential Prognostic Factors in Severe Acute Respiratory Syndrome SARS-CoV-2: A Preliminary Experience. Radiol. Med. 2022, 127, 725–732. [Google Scholar] [CrossRef] [PubMed]
- Somma, F.; Negro, A.; D’Agostino, V.; Piscitelli, V.; Pace, G.; Tortora, M.; Tortora, F.; Gatta, G.; Caranci, F. COVID-19 and Low Back Pain: Previous Infections Lengthen Recovery Time after Intradiscal Ozone Therapy in Patients with Herniated Lumbar Disc. Radiol. Med. 2022, 127, 673–680. [Google Scholar] [CrossRef]
- Novelli, F.; Pinelli, V.; Chiaffi, L.; Carletti, A.M.; Sivori, M.; Giannoni, U.; Chiesa, F.; Celi, A. Prognostic Significance of Peripheral Consolidations at Chest X-Ray in Severe COVID-19 Pneumonia. Radiol. Med. 2022, 127, 602–608. [Google Scholar] [CrossRef]
- Gabelloni, M.; Faggioni, L.; Cioni, D.; Mendola, V.; Falaschi, Z.; Coppola, S.; Corradi, F.; Isirdi, A.; Brandi, N.; Coppola, F.; et al. Extracorporeal Membrane Oxygenation (ECMO) in COVID-19 Patients: A Pocket Guide for Radiologists. Radiol. Med. 2022, 127, 369–382. [Google Scholar] [CrossRef]
- Rizzo, S.; Catanese, C.; Puligheddu, C.; Epistolio, S.; Ramelli, G.; Frattini, M.; Pereira Mestre, R.; Nadarajah, N.; Rezzonico, E.; Magoga, F.; et al. CT Evaluation of Lung Infiltrates in the Two Months Preceding the Coronavirus Disease 19 Pandemic in Canton Ticino (Switzerland): Were There Suspicious Cases before the Official First Case? Radiol. Med. 2022, 127, 360–368. [Google Scholar] [CrossRef] [PubMed]
- Filograna, L.; Manenti, G.; Ampanozi, G.; Calcagni, A.; Ryan, C.P.; Floris, R.; Thali, M.J. Potentials of Post-Mortem CT Investigations during SARS-CoV-2 Pandemic: A Narrative Review. Radiol. Med. 2022, 127, 383–390. [Google Scholar] [CrossRef] [PubMed]
- Caruso, D.; Zerunian, M.; Polici, M.; Pucciarelli, F.; Guido, G.; Polidori, T.; Rucci, C.; Bracci, B.; Tremamunno, G.; Laghi, A. Diagnostic Performance of CT Lung Severity Score and Quantitative Chest CT for Stratification of COVID-19 Patients. Radiol. Med. 2022, 127, 309–317. [Google Scholar] [CrossRef] [PubMed]
- Borghesi, A.; Golemi, S.; Scrimieri, A.; Nicosia, C.M.C.; Zigliani, A.; Farina, D.; Maroldi, R. Chest X-ray versus Chest Computed Tomography for Outcome Prediction in Hospitalized Patients with COVID-19. Radiol. Med. 2022, 127, 305–308. [Google Scholar] [CrossRef] [PubMed]
- Dalpiaz, G.; Gamberini, L.; Carnevale, A.; Spadaro, S.; Mazzoli, C.A.; Piciucchi, S.; Allegri, D.; Capozzi, C.; Neziri, E.; Bartolucci, M.; et al. Clinical Implications of Microvascular CT Scan Signs in COVID-19 Patients Requiring Invasive Mechanical Ventilation. Radiol. Med. 2022, 127, 162–173. [Google Scholar] [CrossRef]
- Masselli, G.; Almberger, M.; Tortora, A.; Capoccia, L.; Dolciami, M.; D’Aprile, M.R.; Valentini, C.; Avventurieri, G.; Bracci, S.; Ricci, P. Role of CT Angiography in Detecting Acute Pulmonary Embolism Associated with COVID-19 Pneumonia. Radiol. Med. 2021, 126, 1553–1560. [Google Scholar] [CrossRef]
- Cellini, F.; Di Franco, R.; Manfrida, S.; Borzillo, V.; Maranzano, E.; Pergolizzi, S.; Morganti, A.G.; Fusco, V.; Deodato, F.; Santarelli, M.; et al. Palliative Radiotherapy Indications during the COVID-19 Pandemic and in Future Complex Logistic Settings: The NORMALITY Model. Radiol. Med. 2021, 126, 1619–1656. [Google Scholar] [CrossRef]
- Caruso, D.; Pucciarelli, F.; Zerunian, M.; Ganeshan, B.; De Santis, D.; Polici, M.; Rucci, C.; Polidori, T.; Guido, G.; Bracci, B.; et al. Chest CT Texture-Based Radiomics Analysis in Differentiating COVID-19 from Other Interstitial Pneumonia. Radiol. Med. 2021, 126, 1415–1424. [Google Scholar] [CrossRef]
- Borghesi, A.; Sverzellati, N.; Polverosi, R.; Balbi, M.; Baratella, E.; Busso, M.; Calandriello, L.; Cortese, G.; Farchione, A.; Iezzi, R.; et al. Impact of the COVID-19 Pandemic on the Selection of Chest Imaging Modalities and Reporting Systems: A Survey of Italian Radiologists. Radiol. Med. 2021, 126, 1258–1272. [Google Scholar] [CrossRef]
- Cardobi, N.; Benetti, G.; Cardano, G.; Arena, C.; Micheletto, C.; Cavedon, C.; Montemezzi, S. CT Radiomic Models to Distinguish COVID-19 Pneumonia from Other Interstitial Pneumonias. Radiol. Med. 2021, 126, 1037–1043. [Google Scholar] [CrossRef] [PubMed]
- Moroni, C.; Cozzi, D.; Albanesi, M.; Cavigli, E.; Bindi, A.; Luvarà, S.; Busoni, S.; Mazzoni, L.N.; Grifoni, S.; Nazerian, P.; et al. Chest X-Ray in the Emergency Department during COVID-19 Pandemic Descending Phase in Italy: Correlation with Patients’ Outcome. Radiol. Med. 2021, 126, 661–668. [Google Scholar] [CrossRef] [PubMed]
- Özel, M.; Aslan, A.; Araç, S. Use of the COVID-19 Reporting and Data System (CO-RADS) Classification and Chest Computed Tomography Involvement Score (CT-IS) in COVID-19 Pneumonia. Radiol. Med. 2021, 126, 679–687. [Google Scholar] [CrossRef]
- Ippolito, D.; Giandola, T.; Maino, C.; Pecorelli, A.; Capodaglio, C.; Ragusi, M.; Porta, M.; Gandola, D.; Masetto, A.; Drago, S.; et al. Acute Pulmonary Embolism in Hospitalized Patients with SARS-CoV-2-Related Pneumonia: Multicentric Experience from Italian Endemic Area. Radiol. Med. 2021, 126, 669–678. [Google Scholar] [CrossRef] [PubMed]
- Cereser, L.; Girometti, R.; Da Re, J.; Marchesini, F.; Como, G.; Zuiani, C. Inter-Reader Agreement of High-Resolution Computed Tomography Findings in Patients with COVID-19 Pneumonia: A Multi-Reader Study. Radiol. Med. 2021, 126, 577–584. [Google Scholar] [CrossRef]
- Bianchi, A.; Mazzoni, L.N.; Busoni, S.; Pinna, N.; Albanesi, M.; Cavigli, E.; Cozzi, D.; Poggesi, A.; Miele, V.; Fainardi, E.; et al. Assessment of Cerebrovascular Disease with Computed Tomography in COVID-19 Patients: Correlation of a Novel Specific Visual Score with Increased Mortality Risk. Radiol. Med. 2021, 126, 570–576. [Google Scholar] [CrossRef]
- Grassi, R.; Belfiore, M.P.; Montanelli, A.; Patelli, G.; Urraro, F.; Giacobbe, G.; Fusco, R.; Granata, V.; Petrillo, A.; Sacco, P.; et al. COVID-19 Pneumonia: Computer-Aided Quantification of Healthy Lung Parenchyma, Emphysema, Ground Glass and Consolidation on Chest Computed Tomography (CT). Radiol. Med. 2021, 126, 553–560. [Google Scholar] [CrossRef]
- Palmisano, A.; Scotti, G.M.; Ippolito, D.; Morelli, M.J.; Vignale, D.; Gandola, D.; Sironi, S.; De Cobelli, F.; Ferrante, L.; Spessot, M.; et al. Chest CT in the Emergency Department for Suspected COVID-19 Pneumonia. Radiol. Med. 2021, 126, 498–502. [Google Scholar] [CrossRef]
- Caruso, D.; Polici, M.; Zerunian, M.; Pucciarelli, F.; Polidori, T.; Guido, G.; Rucci, C.; Bracci, B.; Muscogiuri, E.; De Dominicis, C.; et al. Quantitative Chest CT Analysis in Discriminating COVID-19 from Non-COVID-19 Patients. Radiol. Med. 2021, 126, 243–249. [Google Scholar] [CrossRef]
- Shaw, B.; Daskareh, M.; Gholamrezanezhad, A. The Lingering Manifestations of COVID-19 during and after Convalescence: Update on Long-Term Pulmonary Consequences of Coronavirus Disease 2019 (COVID-19). Radiol. Med. 2021, 126, 40–46. [Google Scholar] [CrossRef]
- Salvatore, C.; Roberta, F.; Angela, L.; Cesare, P.; Alfredo, C.; Giuliano, G.; Giulio, L.; Giuliana, G.; Maria, R.G.; Paola, B.M.; et al. Clinical and Laboratory Data, Radiological Structured Report Findings and Quantitative Evaluation of Lung Involvement on Baseline Chest CT in COVID-19 Patients to Predict Prognosis. Radiol. Med. 2021, 126, 29–39. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.; Adil, S.F.; Alkhathlan, H.Z.; Tahir, M.N.; Saif, S.; Khan, M.; Khan, S.T. COVID-19: A Global Challenge with Old History, Epidemiology and Progress So Far. Molecules 2020, 26, 39. [Google Scholar] [CrossRef] [PubMed]
- Helmy, Y.A.; Fawzy, M.; Elaswad, A.; Sobieh, A.; Kenney, S.P.; Shehata, A.A. The COVID-19 Pandemic: A Comprehensive Review of Taxonomy, Genetics, Epidemiology, Diagnosis, Treatment, and Control. J. Clin. Med. Res. 2020, 9, 1225. [Google Scholar] [CrossRef] [PubMed]
- Moazzam, M.; Sajid, M.I.; Shahid, H.; Butt, J.; Bashir, I.; Jamshaid, M.; Shirazi, A.N.; Tiwari, R.K. Understanding COVID-19: From Origin to Potential Therapeutics. Int. J. Environ. Res. Public Health 2020, 17, 5904. [Google Scholar] [CrossRef] [PubMed]
- Kao, Y.-S.; Lin, K.-T. A Meta-Analysis of the Diagnostic Test Accuracy of CT-Based Radiomics for the Prediction of COVID-19 Severity. Radiol. Med. 2022, 127, 754–762. [Google Scholar] [CrossRef]
- Pecoraro, M.; Cipollari, S.; Marchitelli, L.; Messina, E.; Del Monte, M.; Galea, N.; Ciardi, M.R.; Francone, M.; Catalano, C.; Panebianco, V. Cross-Sectional Analysis of Follow-up Chest MRI and Chest CT Scans in Patients Previously Affected by COVID-19. Radiol. Med. 2021, 126, 1273–1281. [Google Scholar] [CrossRef] [PubMed]
- Ierardi, A.M.; Gaibazzi, N.; Tuttolomondo, D.; Fusco, S.; La Mura, V.; Peyvandi, F.; Aliberti, S.; Blasi, F.; Cozzi, D.; Carrafiello, G.; et al. Deep Vein Thrombosis in COVID-19 Patients in General Wards: Prevalence and Association with Clinical and Laboratory Variables. Radiol. Med. 2021, 126, 722–728. [Google Scholar] [CrossRef] [PubMed]
- Barra, S.; Guarnieri, A.; di Monale E Bastia, M.B.; Marcenaro, M.; Tornari, E.; Belgioia, L.; Magrini, S.M.; Ricardi, U.; Corvò, R. Short Fractionation Radiotherapy for Early Prostate Cancer in the Time of COVID-19: Long-Term Excellent Outcomes from a Multicenter Italian Trial Suggest a Larger Adoption in Clinical Practice. Radiol. Med. 2021, 126, 142–146. [Google Scholar] [CrossRef]
- Laghi, A.; Tamburi, V.; Polici, M.; Anibaldi, P.; Marcolongo, A.; Caruso, D. Management Decisions of an Academic Radiology Department during COVID-19 Pandemic: The Important Support of a Business Analytics Software. Eur. Radiol. 2022, 32, 7048–7055. [Google Scholar] [CrossRef]
- Ayyala, R.S.; Garver, K.A.; Callahan, M.J. Wellness in Pediatric Radiology: Lessons Learned in a Time of Pandemic. Pediatr. Radiol. 2020, 50, 898–899. [Google Scholar] [CrossRef] [PubMed]
- Gerasia, R.; Mamone, G.; Amato, S.; Cucchiara, A.; Gallo, G.S.; Tafaro, C.; Fiorello, G.; Caruso, C.; Miraglia, R. COVID-19 Safety Measures at the Radiology Unit of a Transplant Institute: The Non-COVID-19 Patient’s Confidence with Safety Procedures. Radiol. Med. 2022, 127, 426–432. [Google Scholar] [CrossRef] [PubMed]
- Caliandro, M.; Fabiana, G.; Surgo, A.; Carbonara, R.; Ciliberti, M.P.; Bonaparte, I.; Caputo, S.; Fiorentino, A. Impact on Mental Health of the COVID-19 Pandemic in a Radiation Oncology Department. Radiol. Med. 2022, 127, 220–224. [Google Scholar] [CrossRef] [PubMed]
- Amanullah, S.; Ramesh Shankar, R. The Impact of COVID-19 on Physician Burnout Globally: A Review. Healthcare 2020, 8, 421. [Google Scholar] [CrossRef]
- Gualano, M.R.; Sinigaglia, T.; Lo Moro, G.; Rousset, S.; Cremona, A.; Bert, F.; Siliquini, R. The Burden of Burnout among Healthcare Professionals of Intensive Care Units and Emergency Departments during the COVID-19 Pandemic: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 8172. [Google Scholar] [CrossRef] [PubMed]
- Ulbrichtova, R.; Svihrova, V.; Tatarkova, M.; Svihra, J., Jr.; Novak, M.; Hudeckova, H. Prevalence of Burnout Syndrome in COVID-19 and Non-COVID-19 Units in University Hospital: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 12664. [Google Scholar] [CrossRef] [PubMed]
- Elghazally, S.A.; Alkarn, A.F.; Elkhayat, H.; Ibrahim, A.K.; Elkhayat, M.R. Burnout Impact of COVID-19 Pandemic on Health-Care Professionals at Assiut University Hospitals, 2020. Int. J. Environ. Res. Public Health 2021, 18, 5368. [Google Scholar] [CrossRef]
- Claponea, R.M.; Pop, L.M.; Iorga, M.; Iurcov, R. Symptoms of Burnout Syndrome among Physicians during the Outbreak of COVID-19 Pandemic-A Systematic Literature Review. Healthcare 2022, 10, 979. [Google Scholar] [CrossRef]
- Conti, C.; Fontanesi, L.; Lanzara, R.; Rosa, I.; Doyle, R.L.; Porcelli, P. Burnout Status of Italian Healthcare Workers during the First COVID-19 Pandemic Peak Period. Healthcare 2021, 9, 510. [Google Scholar] [CrossRef]
- Franzoi, I.G.; Granieri, A.; Sauta, M.D.; Agnesone, M.; Gonella, M.; Cavallo, R.; Lochner, P.; Bragazzi, N.L.; Naldi, A. Anxiety, Post-Traumatic Stress, and Burnout in Health Professionals during the COVID-19 Pandemic: Comparing Mental Health Professionals and Other Healthcare Workers. Healthcare 2021, 9, 635. [Google Scholar] [CrossRef]
- Haravuori, H.; Junttila, K.; Haapa, T.; Tuisku, K.; Kujala, A.; Rosenström, T.; Suvisaari, J.; Pukkala, E.; Laukkala, T.; Jylhä, P. Personnel Well-Being in the Helsinki University Hospital during the COVID-19 Pandemic-A Prospective Cohort Study. Int. J. Environ. Res. Public Health 2020, 17, 7905. [Google Scholar] [CrossRef]
- Coppola, F.; Faggioni, L.; Neri, E.; Grassi, R.; Miele, V. Impact of the COVID-19 Outbreak on the Profession and Psychological Wellbeing of Radiologists: A Nationwide Online Survey. Insights Imaging 2021, 12, 23. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Healthcare Interventions: Explanation and Elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef] [PubMed]
- Ayyala, R.S.; Baird, G.; Bloom, D.A.; McDaniel, J.D.; Lampl, B. Evaluation of Stress and Anxiety Caused by the Coronavirus Disease 2019 (COVID-19) Pandemic in Pediatric Radiology. Pediatr. Radiol. 2021, 51, 1589–1596. [Google Scholar] [CrossRef]
- Demirjian, N.L.; Fields, B.K.K.; Song, C.; Reddy, S.; Desai, B.; Cen, S.Y.; Salehi, S.; Gholamrezanezhad, A. Impacts of the Coronavirus Disease 2019 (COVID-19) Pandemic on Healthcare Workers: A Nationwide Survey of United States Radiologists. Clin. Imaging 2020, 68, 218–225. [Google Scholar] [CrossRef] [PubMed]
- Elshami, W.; Akudjedu, T.N.; Abuzaid, M.; David, L.R.; Tekin, H.O.; Cavli, B.; Issa, B. The Radiology Workforce’s Response to the COVID-19 Pandemic in the Middle East, North Africa and India. Radiography 2021, 27, 360–368. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.L.; Chen, R.C.; Teo, I.; Chaudhry, I.; Heng, A.L.; Da Zhuang, K.; Tan, H.K.; Tan, B.S. A Survey of Anxiety and Burnout in the Radiology Workforce of a Tertiary Hospital during the COVID-19 Pandemic. J. Med. Imaging Radiat. Oncol. 2021, 65, 139–145. [Google Scholar] [CrossRef]
- Huang, L.; Wang, Y.; Liu, J.; Ye, P.; Cheng, B.; Xu, H.; Qu, H.; Ning, G. Factors Associated with Resilience Among Medical Staff in Radiology Departments During The Outbreak of 2019 Novel Coronavirus Disease (COVID-19): A Cross-Sectional Study. Med. Sci. Monit. 2020, 26, e925669. [Google Scholar] [CrossRef]
- Huang, L.; Wang, Y.; Liu, J.; Ye, P.; Chen, X.; Xu, H.; Guo, Y.; Qu, H.; Ning, G. Short Report: Factors Determining Perceived Stress among Medical Staff in Radiology Departments during the COVID-19 Outbreak. Psychol. Health Med. 2021, 26, 56–61. [Google Scholar] [CrossRef]
- Milch, H.S.; Grimm, L.J.; Plimpton, S.R.; Tran, K.; Markovic, D.; Dontchos, B.N.; Destounis, S.; Dialani, V.; Dogan, B.E.; Sonnenblick, E.B.; et al. COVID-19 and Breast Radiologist Wellness: Impact of Gender, Financial Loss, and Childcare Need. J. Am. Coll. Radiol. 2021, 18, 1017–1026. [Google Scholar] [CrossRef]
- Oprisan, A.; Baettig-Arriagada, E.; Baeza-Delgado, C.; Martí-Bonmatí, L. Prevalencia Y Factores de Desgaste Profesional En Radiólogos Durante La Pandemia COVID-19. Radiología 2022, 64, 119–127. [Google Scholar] [CrossRef]
- Woerner, A.; Chick, J.F.B.; Monroe, E.J.; Ingraham, C.R.; Pereira, K.; Lee, E.; Hage, A.N.; Makary, M.S.; Shin, D.S. Interventional Radiology in the Coronavirus Disease 2019 Pandemic: Impact on Practices and Wellbeing. Acad. Radiol. 2021, 28, 1209–1218. [Google Scholar] [CrossRef] [PubMed]
- Aggarwal, A.; Lazarow, F.; Anzai, Y.; Elsayed, M.; Ghobadi, C.; Al Dandan, O.; Griffith, B.; Straus, C.M.; Kadom, N. Maximizing Value While Volumes Are Increasing. Curr. Probl. Diagn. Radiol. 2021, 50, 451–453. [Google Scholar] [CrossRef] [PubMed]
- Belfi, L.M.; Jordan, S.G.; Chetlen, A.; Deitte, L.A.; Frigini, L.A.; Methratta, S.T.; Robbins, J.; Woods, R.; Benefield, T.; Jay, A.K. Self-Care and Storytelling for Radiologists: A Feasibility Study. Curr. Probl. Diagn. Radiol. 2022, 51, 445–449. [Google Scholar] [CrossRef] [PubMed]
- Brown, B.P. Why Wellness Fails. J. Am. Coll. Radiol. 2021, 18, 166–169. [Google Scholar] [CrossRef] [PubMed]
- Buch, K.A.; Daye, D.; Wood, M.J.; Alvarez, C.; del Carmen, M.G.; Mehta, D.H.; Bredella, M.A. Wellness Program Implementation in an Academic Radiology Department: Determination of Need, Organizational Buy-In, and Outcomes. J. Am. Coll. Radiol. 2021, 18, 663–668. [Google Scholar] [CrossRef]
- Fishman, M.D.C.; Reddy, S.P. Coaching: A Primer for the Radiologist. J. Am. Coll. Radiol. 2021, 18, 1192–1197. [Google Scholar] [CrossRef]
- Glover, A.M.; Whitman, G.J.; Shin, K. Ergonomics in Radiology: Improving the Work Environment for Radiologists. Curr. Probl. Diagn. Radiol. 2022, 51, 680–685. [Google Scholar] [CrossRef]
- McGrath, A.L.; Dodelzon, K.; Awan, O.A.; Said, N.; Bhargava, P. Optimizing Radiologist Productivity and Efficiency: Work Smarter, Not Harder. Eur. J. Radiol. 2022, 155, 110131. [Google Scholar] [CrossRef]
- Oliveira, A.; Gowda, V.; Jordan, S.G. It Takes a Village: A Multimodal Approach to Addressing Radiologist Burnout. Curr. Probl. Diagn. Radiol. 2022, 51, 289–292. [Google Scholar] [CrossRef]
- Parikh, J.R.; Bender, C.E. How Radiology Leaders Can Address Burnout. J. Am. Coll. Radiol. 2021, 18, 679–684. [Google Scholar] [CrossRef]
- Patel, R.; Link, T.M. Abbreviated Musculoskeletal MRI Protocols: Counterpoint-Worsened Patient Care and Radiologist Burnout. AJR Am. J. Roentgenol. 2021, 216, 35–36. [Google Scholar] [CrossRef] [PubMed]
- Deshmukh, S.; Shmelev, K.; Vassiliades, L.; Kurumety, S.; Agarwal, G.; Horowitz, J.M. Imposter Phenomenon in Radiology: Incidence, Intervention, and Impact on Wellness. Clin. Imaging 2022, 82, 94–99. [Google Scholar] [CrossRef] [PubMed]
- Felice, F.D.; De Felice, F.; D’Angelo, E.; Ingargiola, R.; Iacovelli, N.A.; Alterio, D.; Franco, P.; Bonomo, P.; Merlotti, A.; Bacigalupo, A.; et al. A Snapshot on Radiotherapy for Head and Neck Cancer Patients during the COVID-19 Pandemic: A Survey of the Italian Association of Radiotherapy and Clinical Oncology (AIRO) Head and Neck Working Group. Radiol. Med. 2021, 126, 343–347. [Google Scholar] [CrossRef] [PubMed]
- Giorgi, G.; Lecca, L.I.; Alessio, F.; Finstad, G.L.; Bondanini, G.; Lulli, L.G.; Arcangeli, G.; Mucci, N. COVID-19-Related Mental Health Effects in the Workplace: A Narrative Review. Int. J. Environ. Res. Public Health 2020, 17, 7857. [Google Scholar] [CrossRef]
- D’Ettorre, G.; Ceccarelli, G.; Santinelli, L.; Vassalini, P.; Innocenti, G.P.; Alessandri, F.; Koukopoulos, A.E.; Russo, A.; d’Ettorre, G.; Tarsitani, L. Post-Traumatic Stress Symptoms in Healthcare Workers Dealing with the COVID-19 Pandemic: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 601. [Google Scholar] [CrossRef]
- Yassin, A.H.; Spector, J.T.; Mease, L.; Shumate, A.; Hill, R.; Lincoln, J.E.; Baker, M.G. Workplace Determinants of Depression, Anxiety, and Stress in U.S. Mariners during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 16628. [Google Scholar] [CrossRef]
- Bodner, A.; Ruhl, L.; Barr, E.; Shridhar, A.; Skakoon-Sparling, S.; Card, K.G. The Impact of Working from Home on Mental Health: A Cross-Sectional Study of Canadian Worker’s Mental Health during the Third Wave of the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 11588. [Google Scholar] [CrossRef]
- Kim, S.; Son, H.-G.; Lee, S.; Park, H.; Jeong, K.-H. A Study on the Relationship between Depression Change Types and Suicide Ideation before and after COVID-19. Healthcare 2022, 10, 1610. [Google Scholar] [CrossRef]
- Di Corrado, D.; Muzii, B.; Magnano, P.; Coco, M.; La Paglia, R.; Maldonato, N.M. The Moderated Mediating Effect of Hope, Self-Efficacy and Resilience in the Relationship between Post-Traumatic Growth and Mental Health during the COVID-19 Pandemic. Healthcare 2022, 10, 1091. [Google Scholar] [CrossRef]
- Andreassi, S.; Monaco, S.; Salvatore, S.; Sciabica, G.M.; De Felice, G.; Petrovska, E.; Mariani, R. To Work or Not to Work, That Is the Question: The Psychological Impact of the First COVID-19 Lockdown on the Elderly, Healthcare Workers, and Virtual Workers. Healthcare 2021, 9, 1754. [Google Scholar] [CrossRef]
- Lohela-Karlsson, M.; Condén Mellgren, E. Health Consequences of the COVID-19 Pandemic among Health-Care Workers: A Comparison between Groups Involved and Not Involved in COVID-19 Care. Healthcare 2022, 10, 2540. [Google Scholar] [CrossRef]
- Esquivel-Chirino, C.; Valero-Princet, Y.; Gaitán-Cepeda, L.A.; Hernández-Hernández, C.; Hernández, A.M.; Laparra-Escareño, H.; Ventura-Gallegos, J.L.; Montes-Sánchez, D.; Lopéz-Macay, A.; Hernández-Sánchez, F.; et al. The Effects of COVID-19 on Healthcare Workers and Non-Healthcare Workers in Mexico: 14 Months into the Pandemic. Medicina 2021, 57, 1353. [Google Scholar] [CrossRef] [PubMed]
- McFadden, P.; Neill, R.D.; Moriarty, J.; Gillen, P.; Mallett, J.; Manthorpe, J.; Currie, D.; Schroder, H.; Ravalier, J.; Nicholl, P.; et al. A Cross-Sectional Examination of the Mental Wellbeing, Coping and Quality of Working Life in Health and Social Care Workers in the UK at Two Time Points of the COVID-19 Pandemic. Epidemiologia 2021, 2, 227–242. [Google Scholar] [CrossRef]
- Capone, V.; Borrelli, R.; Marino, L.; Schettino, G. Mental Well-Being and Job Satisfaction of Hospital Physicians during COVID-19: Relationships with Efficacy Beliefs, Organizational Support, and Organizational Non-Technical Skills. Int. J. Environ. Res. Public Health 2022, 19, 3734. [Google Scholar] [CrossRef]
- Doraiswamy, S.; Cheema, S.; Maisonneuve, P.; Abraham, A.; Weber, I.; An, J.; Lowenfels, A.B.; Mamtani, R. Knowledge and Anxiety about COVID-19 in the State of Qatar, and the Middle East and North Africa Region—A Cross Sectional Study. Int. J. Environ. Res. Public Health. 2021, 18, 6439. [Google Scholar] [CrossRef]
- Aldossari, M.; Chaudhry, S. Women and Burnout in the Context of a Pandemic. Gend. Work. Organ. 2021, 28, 826–834. [Google Scholar] [CrossRef]
- Wu, Y.; Wang, J.; Luo, C.; Hu, S.; Lin, X.; Anderson, A.E.; Bruera, E.; Yang, X.; Wei, S.; Qian, Y. A Comparison of Burnout Frequency Among Oncology Physicians and Nurses Working on the Frontline and Usual Wards During the COVID-19 Epidemic in Wuhan, China. J. Pain Symptom Manag. 2020, 60, e60–e65. [Google Scholar] [CrossRef] [PubMed]
- Giovagnoni, A.; Gandolfo, N.; Miele, V. Women in Radiology: The SIRM Believes in Equal Opportunity. Radiol. Med. 2022, 127, 225–227. [Google Scholar] [CrossRef] [PubMed]
- Lesslie, M.D.; Parikh, J.R. Multidisciplinary Tumor Boards: An Opportunity for Radiologists to Demonstrate Value. Acad. Radiol. 2017, 24, 107–110. [Google Scholar] [CrossRef]
- Neri, E.; Gabelloni, M.; Bäuerle, T.; Beets-Tan, R.; Caruso, D.; D’Anastasi, M.; Dinkel, J.; Fournier, L.S.; Gourtsoyianni, S.; Hoffmann, R.-T.; et al. Involvement of Radiologists in Oncologic Multidisciplinary Team Meetings: An International Survey by the European Society of Oncologic Imaging. Eur. Radiol. 2021, 31, 983–991. [Google Scholar] [CrossRef]
- Granata, V.; Faggioni, L.; Grassi, R.; Fusco, R.; Reginelli, A.; Rega, D.; Maggialetti, N.; Buccicardi, D.; Frittoli, B.; Rengo, M.; et al. Structured Reporting of Computed Tomography in the Staging of Colon Cancer: A Delphi Consensus Proposal. Radiol. Med. 2022, 127, 21–29. [Google Scholar] [CrossRef]
- Neri, E.; Granata, V.; Montemezzi, S.; Belli, P.; Bernardi, D.; Brancato, B.; Caumo, F.; Calabrese, M.; Coppola, F.; Cossu, E.; et al. Structured Reporting of X-Ray Mammography in the First Diagnosis of Breast Cancer: A Delphi Consensus Proposal. Radiol. Med. 2022, 127, 471–483. [Google Scholar] [CrossRef] [PubMed]
- Faggioni, L.; Coppola, F.; Ferrari, R.; Neri, E.; Regge, D. Usage of Structured Reporting in Radiological Practice: Results from an Italian Online Survey. Eur. Radiol. 2017, 27, 1934–1943. [Google Scholar] [CrossRef] [PubMed]
- Ganeshan, D.; Duong, P.-A.T.; Probyn, L.; Lenchik, L.; McArthur, T.A.; Retrouvey, M.; Ghobadi, E.H.; Desouches, S.L.; Pastel, D.; Francis, I.R. Structured Reporting in Radiology. Acad. Radiol. 2018, 25, 66–73. [Google Scholar] [CrossRef]
- Cao, D.J.; Hurrell, C.; Patlas, M.N. Current Status of Burnout in Canadian Radiology. Can. Assoc. Radiol. J. 2022, 74, 37–43. [Google Scholar] [CrossRef]
- Zerunian, M.; Pucciarelli, F.; Caruso, D.; Polici, M.; Masci, B.; Guido, G.; De Santis, D.; Polverari, D.; Principessa, D.; Benvenga, A.; et al. Artificial Intelligence Based Image Quality Enhancement in Liver MRI: A Quantitative and Qualitative Evaluation. Radiol. Med. 2022, 127, 1098–1105. [Google Scholar] [CrossRef] [PubMed]
- Matsoukas, S.; Scaggiante, J.; Schuldt, B.R.; Smith, C.J.; Chennareddy, S.; Kalagara, R.; Majidi, S.; Bederson, J.B.; Fifi, J.T.; Mocco, J.; et al. Accuracy of Artificial Intelligence for the Detection of Intracranial Hemorrhage and Chronic Cerebral Microbleeds: A Systematic Review and Pooled Analysis. Radiol. Med. 2022, 127, 1106–1123. [Google Scholar] [CrossRef]
- Palmisano, A.; Vignale, D.; Boccia, E.; Nonis, A.; Gnasso, C.; Leone, R.; Montagna, M.; Nicoletti, V.; Bianchi, A.G.; Brusamolino, S.; et al. AI-SCoRE (artificial Intelligence-SARS CoV2 Risk Evaluation): A Fast, Objective and Fully Automated Platform to Predict the Outcome in COVID-19 Patients. Radiol. Med. 2022, 127, 960–972. [Google Scholar] [CrossRef]
- Gurgitano, M.; Angileri, S.A.; Rodà, G.M.; Liguori, A.; Pandolfi, M.; Ierardi, A.M.; Wood, B.J.; Carrafiello, G. Interventional Radiology Ex-Machina: Impact of Artificial Intelligence on Practice. Radiol. Med. 2021, 126, 998–1006. [Google Scholar] [CrossRef]
- Coppola, F.; Faggioni, L.; Regge, D.; Giovagnoni, A.; Golfieri, R.; Bibbolino, C.; Miele, V.; Neri, E.; Grassi, R. Artificial Intelligence: Radiologists’ Expectations and Opinions Gleaned from a Nationwide Online Survey. Radiol. Med. 2021, 126, 63–71. [Google Scholar] [CrossRef]
- Granata, V.; Fusco, R.; Catalano, O.; Setola, S.V.; di Castelguidone, E.D.L.; Piccirillo, M.; Palaia, R.; Grassi, R.; Granata, F.; Izzo, F.; et al. Multidetector Computer Tomography in the Pancreatic Adenocarcinoma Assessment: An Update. Infect. Agents Cancer 2016, 11, 57. [Google Scholar] [CrossRef] [PubMed]
- Granata, V.; Fusco, R.; Costa, M.; Picone, C.; Cozzi, D.; Moroni, C.; La Casella, G.V.; Montanino, A.; Monti, R.; Mazzoni, F.; et al. Preliminary Report on Computed Tomography Radiomics Features as Biomarkers to Immunotherapy Selection in Lung Adenocarcinoma Patients. Cancers 2021, 13, 3992. [Google Scholar] [CrossRef]
- Fusco, R.; Granata, V.; Mazzei, M.A.; Meglio, N.D.; Roscio, D.D.; Moroni, C.; Monti, R.; Cappabianca, C.; Picone, C.; Neri, E.; et al. Quantitative Imaging Decision Support (QIDS) Tool Consistency Evaluation and Radiomic Analysis by Means of 594 Metrics in Lung Carcinoma on Chest CT Scan. Cancer Control 2021, 28, 1073274820985786. [Google Scholar] [CrossRef] [PubMed]
- Granata, V.; Fusco, R.; Setola, S.V.; Galdiero, R.; Picone, C.; Izzo, F.; D’Aniello, R.; Miele, V.; Grassi, R.; Grassi, R.; et al. Lymphadenopathy after BNT162b2 COVID-19 Vaccine: Preliminary Ultrasound Findings. Biology 2021, 10, 214. [Google Scholar] [CrossRef]
- COVIDSurg Collaborative Preoperative Nasopharyngeal Swab Testing and Postoperative Pulmonary Complications in Patients Undergoing Elective Surgery during the SARS-CoV-2 Pandemic. Br. J. Surg. 2021, 108, 88–96. [CrossRef] [PubMed]
- D’Agostino, V.; Caranci, F.; Negro, A.; Piscitelli, V.; Tuccillo, B.; Fasano, F.; Sirabella, G.; Marano, I.; Granata, V.; Grassi, R.; et al. A Rare Case of Cerebral Venous Thrombosis and Disseminated Intravascular Coagulation Temporally Associated to the COVID-19 Vaccine Administration. J. Pers. Med. 2021, 11, 285. [Google Scholar] [CrossRef] [PubMed]
- COVIDSurg Collaborative Effect of COVID-19 Pandemic Lockdowns on Planned Cancer Surgery for 15 Tumour Types in 61 Countries: An International, Prospective, Cohort Study. Lancet Oncol. 2021, 22, 1507–1517. [CrossRef] [PubMed]
- Fusco, R.; Setola, S.V.; Raiano, N.; Granata, V.; Cerciello, V.; Pecori, B.; Petrillo, A. Analysis of a Monocentric Computed Tomography Dosimetric Database Using a Radiation Dose Index Monitoring Software: Dose Levels and Alerts before and after the Implementation of the Adaptive Statistical Iterative Reconstruction on CT Images. Radiol. Med. 2022, 127, 733–742. [Google Scholar] [CrossRef]
- Mungmunpuntipantip, R.; Wiwanitkit, V. COVID-19, Intradiscal Ozone Therapy and Back Pain: A Correspondence. Radiol. Med. 2022, 127, 1179. [Google Scholar] [CrossRef]
- Masci, G.M.; Iafrate, F.; Ciccarelli, F.; Pambianchi, G.; Panebianco, V.; Pasculli, P.; Ciardi, M.R.; Mastroianni, C.M.; Ricci, P.; Catalano, C.; et al. Tocilizumab Effects in COVID-19 Pneumonia: Role of CT Texture Analysis in Quantitative Assessment of Response to Therapy. Radiol. Med. 2021, 126, 1170–1180. [Google Scholar] [CrossRef]
- Lombardi, A.F.; Afsahi, A.M.; Gupta, A.; Gholamrezanezhad, A. Severe Acute Respiratory Syndrome (SARS), Middle East Respiratory Syndrome (MERS), Influenza, and COVID-19, beyond the Lungs: A Review Article. Radiol. Med. 2021, 126, 561–569. [Google Scholar] [CrossRef] [PubMed]
- Agostini, A.; Borgheresi, A.; Carotti, M.; Ottaviani, L.; Badaloni, M.; Floridi, C.; Giovagnoni, A. Third-Generation Iterative Reconstruction on a Dual-Source, High-Pitch, Low-Dose Chest CT Protocol with Tin Filter for Spectral Shaping at 100 kV: A Study on a Small Series of COVID-19 Patients. Radiol. Med. 2021, 126, 388–398. [Google Scholar] [CrossRef] [PubMed]
- Gaia, C.; Maria Chiara, C.; Silvia, L.; Chiara, A.; Maria Luisa, D.C.; Giulia, B.; Silvia, P.; Lucia, C.; Alessandra, T.; Annarita, S.; et al. Chest CT for Early Detection and Management of Coronavirus Disease (COVID-19): A Report of 314 Patients Admitted to Emergency Department with Suspected Pneumonia. Radiol. Med. 2020, 125, 931–942. [Google Scholar] [CrossRef] [PubMed]
- Cartocci, G.; Colaiacomo, M.C.; Lanciotti, S.; Andreoli, C.; De Cicco, M.L.; Brachetti, G.; Pugliese, S.; Capoccia, L.; Tortora, A.; Scala, A.; et al. Correction to: Chest CT for Early Detection and Management of Coronavirus Disease (COVID-19): A Report of 314 Patients Admitted to Emergency Department with Suspected Pneumonia. Radiol. Med. 2021, 126, 642. [Google Scholar] [CrossRef]
- Coppola, F.; Faggioni, L.; Gabelloni, M.; De Vietro, F.; Mendola, V.; Cattabriga, A.; Cocozza, M.A.; Vara, G.; Piccinino, A.; Lo Monaco, S.; et al. Human, All Too Human? An All-Around Appraisal of the “Artificial Intelligence Revolution” in Medical Imaging. Front. Psychol. 2021, 12, 710982. [Google Scholar] [CrossRef]
- Neri, E.; Coppola, F.; Miele, V.; Bibbolino, C.; Grassi, R. Artificial Intelligence: Who Is Responsible for the Diagnosis? Radiol. Med. 2020, 125, 517–521. [Google Scholar] [CrossRef]
- Mezrich, J.L. Demystifying Medico-Legal Challenges of Artificial Intelligence Applications in Molecular Imaging and Therapy. PET Clin. 2022, 17, 41–49. [Google Scholar] [CrossRef]
- Lang, M.; Bernier, A.; Knoppers, B.M. Artificial Intelligence in Cardiovascular Imaging: “Unexplainable” Legal and Ethical Challenges? Can. J. Cardiol. 2022, 38, 225–233. [Google Scholar] [CrossRef]
- Laptev, V.A.; Ershova, I.V.; Feyzrakhmanova, D.R. Medical Applications of Artificial Intelligence (Legal Aspects and Future Prospects). Laws 2021, 11, 3. [Google Scholar] [CrossRef]
- Prakash, S.; Balaji, J.N.; Joshi, A.; Surapaneni, K.M. Ethical Conundrums in the Application of Artificial Intelligence (AI) in Healthcare—A Scoping Review of Reviews. J. Pers. Med. 2022, 12, 1914. [Google Scholar] [CrossRef]
- Triberti, S.; Durosini, I.; Pravettoni, G. A “Third Wheel” Effect in Health Decision Making Involving Artificial Entities: A Psychological Perspective. Front Public Health 2020, 8, 117. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, M.; van der Pol, C.B.; Patlas, M.N.; Udare, A.; Chung, A.D.; Rubino, J. Optimizing the Radiologist Work Environment: Actionable Tips to Improve Workplace Satisfaction, Efficiency, and Minimize Burnout. Radiol. Med. 2021, 126, 1255–1257. [Google Scholar] [CrossRef] [PubMed]
- Granata, V.; Fusco, R.; De Muzio, F.; Cutolo, C.; Mattace Raso, M.; Gabelloni, M.; Avallone, A.; Ottaiano, A.; Tatangelo, F.; Brunese, M.C.; et al. Radiomics and Machine Learning Analysis Based on Magnetic Resonance Imaging in the Assessment of Colorectal Liver Metastases Growth Pattern. Diagnostics 2022, 12, 1115. [Google Scholar] [CrossRef] [PubMed]
- Gabelloni, M.; Di Nasso, M.; Morganti, R.; Faggioni, L.; Masi, G.; Falcone, A.; Neri, E. Application of the ESR iGuide Clinical Decision Support System to the Imaging Pathway of Patients with Hepatocellular Carcinoma and Cholangiocarcinoma: Preliminary Findings. Radiol. Med. 2020, 125, 531–537. [Google Scholar] [CrossRef]
- Fan, Y.; Zhao, Z.; Wang, X.; Ai, H.; Yang, C.; Luo, Y.; Jiang, X. Radiomics for Prediction of Response to EGFR-TKI Based on Metastasis/brain Parenchyma (M/BP)-Interface. Radiol. Med. 2022, 127, 1342–1354. [Google Scholar] [CrossRef]
- Dallan, I.; Seccia, V.; Faggioni, L.; Castelnuovo, P.; Montevecchi, F.; Casani, A.P.; Tschabitscher, M.; Vicini, C. Anatomical Landmarks for Transoral Robotic Tongue Base Surgery: Comparison between Endoscopic, External and Radiological Perspectives. Surg. Radiol. Anat. 2013, 35, 3–10. [Google Scholar] [CrossRef]
- Chmielewski, J.; Łoś, K.; Łuczyński, W. Mindfulness in Healthcare Professionals and Medical Education. Int. J. Occup. Med. Environ. Health 2021, 34, 1–14. [Google Scholar] [CrossRef]
- Ebuoma, L.O.; Severs, F.J.; Sedgwick, E.L.; Roark, A.A.; Ortiz-Perez, T.; Sepulveda, K.A.; Benveniste, A.P. Benefits of Professional Coaching for Radiologists. J. Am. Coll. Radiol. 2017, 14, 976–979. [Google Scholar] [CrossRef]
- Kruskal, J.B.; Shanafelt, T. Radiologist Well-Being and Professional Fulfillment in the COVID-19 Era: Fostering Posttraumatic Growth. J. Am. Coll. Radiol. 2021, 18, 1198–1207. [Google Scholar] [CrossRef]
| Authors [Reference Number] | Year | Country | Qualification | Age (Years) | Professional Experience (Years) | Gender Distribution | Survey Duration | Main Findings |
|---|---|---|---|---|---|---|---|---|
| Ayyala et al. [63] | 2021 | North America | Physician members of the Society for Pediatric Radiology | Median 48 (range 33–70) | Median 14 (range 1–45) | Female 53%, male 46% | From 27 April 2020 to 22 May 2020 | Response rate 21% 69% of respondents felt more isolated from a lack of regular interaction with colleagues 53% of respondents indicated that it is challenging to work remotely while overseeing home schooling for children In comparison to men, women reported overall higher work-related stress and anxiety (p = 0.02), higher feelings of guilt from radiology staff (i.e., technologists and nurses) being more exposed to COVID-19 (p = 0.02) and higher levels of stress providing for dependents (p = 0.04) |
| Coppola et al. [61] | 2021 | Italy | Members of the Italian Society of Medical and Interventional Radiology (SIRM) | Under 35 (18.7%) 36–65 (68.2%) Over 65 (13%) (“hot regions”) Under 35 (16.3%) 36–65 (70.8%) Over 65 (12.8%) (other regions) | Resident (10.7%) Post-doc fellow, PhD student or outpatient specialist (1.2%) Research fellow (0.4%) Associate or full professor (1.3%) Staff radiologist (52.2%) Medical director (8.5%) Private consultant (25.7%) (“hot regions”) Resident (9.8%) Post-doc fellow, PhD student or outpatient specialist (1.4%) Research fellow (1.2%) Associate or full professor (1.4%) Staff radiologist (52.6%) Medical director (10.8%) Private consultant (21.8%) (other regions) | Female 50.7%, male 49.3% (“hot regions”) Female 51.3%, male 48.7% (other regions) | From 4 May 2020 to 11 May 2020* | Response rate 20.1% More than 60% of respondents estimated a workload reduction greater than 50%, with a higher prevalence among private workers in hot regions (72.7% vs. 66.5% elsewhere, p = 0.1010) More than 40% were moderately or severely worried that their professional activity could be damaged, and most residents believed that their training had been affected More than 50% of respondents had increased emotional stress at work, including moderate or severe symptoms due to sleep disturbances, feeling like living in slow motion and having negative thoughts, those latter being more likely in single-living respondents from hot regions [log OR 0.7108 (CI95% 0.3445 ÷ 1.0770), p = 0.0001] |
| Demirjian et al. [64] | 2020 | USA | Radiologists | Mean 45 (SD 11) | Radiologist/attending radiologists (80%) In training (residents) (16%) In training (fellows) (4%) Other (0.4%) | Female 47% male 53% nonbinary 0.2% prefer not to say 0.7% | From 3 April 2020 for 8 days | 61% of respondents rated their level of anxiety with regard to COVID-19 as 7 out of 10 or greater, and higher scores were positively correlated the standardized number of COVID-19 cases in a respondent’s state (RR = 1.11, CI95% 1.02–1.21, p = 0.01) Citing the stressor of “personal health” was a strong predictor of higher anxiety scores (RR 1.23, CI95% 1.13–1.34, p < 0.01) Participants who reported needing no coping methods were more likely to self-report lower anxiety scores (RR 0.4, CI95% 0.3–0.53, p < 0.01) |
| Elshami et al. [65] | 2021 | Middle East, North Africa, India | Radiographers (92.5%) radiologists (2.3%) advanced practitioners (1.4%) radiology residents (1.0%) radiology assistants (0.9%) radiology nurses (0.9%) others (1.0%) | 18–29 (49.7%) 30–39 (27.9%) 40–49 (17.8%) 50–59 (4.2%) 60+ (0.3%) | Less than 5 (38.1%) 6–10 (24.6%) 11–15 (14.0%) 16–20 (11.0%) 20+ (12.4%) | Female 49.1% male 50.9% | From 22 May 2020 to 2 June 2020 | Respondents reported experiences of work-related stress (42.9%), high COVID-19 fear score (83.3%) and anxiety (10%) during the COVID-19 pandemic 79.5% of respondents strongly agreed or agreed that PPE was adequately available at work during the pandemic It is important to provide training and regular mental health support and evaluations for healthcare professionals, including radiology workers, during similar future pandemics |
| Huang HL et al. [66] | 2021 | Singapore | Doctors (21.7%) nurses (2.2%) allied health professionals (58.9%) others (17.2%) | Mean 38.6 (SD 12.4) | N/A | Female 62.8% male 37.2% | From 12 March 2020 to 20 July 2020 | During the COVID-19 pandemic, a proportion of radiological staff reported significant burnout and anxiety, although less compared to the larger hospital cohort (17.8% vs. 23.9%, p = 0.068) and 6.7% vs. 13.2%, p = 0.013) Measures to prevent longer than usual work hours and increase feelings of enthusiasm and pride in one’s job may further reduce the prevalence of anxiety problems and burnout in radiology departments |
| Huang L et al. [67] | 2020 | China | Doctors (38.0%) technicians (41.7%) nurses (20.3%) | Median 33 (range 28–43) | Median 10 (range 5–21) | Female 52.0% male 48.0% | From 7 February 2020 to 9 February 2020 | Effective response rate 97.8%. The resilience level of the medical staff in the radiology departments during the COVID-19 pandemic was generally low, particularly regarding toughness More attention should be paid to resilience influence factors such as high perceived stress, female gender, lack of understanding of COVID-19 and protective measures, and lack of protective materials, and targeted interventions should be undertaken to improve the resilience level of the medical staff in the radiology departments during the outbreak of COVID-19 |
| Huang L et al. [68] | 2020 | China | Doctors, technicians, nurses | Median 33 (range 28–43) | Median 10 (range 5–21) | Female 52.0% male 48.0% | From 7 February 2020 to 9 February 2020 | Medical staff in radiology departments faces a higher risk of infection and a heavier workload during the COVID-19 pandemic Risk factors for perceived stress were female gender, existing anxiety, and fears of being infected at work, an uncontrollable outbreak, and not being able to pay rent or mortgage |
| Milch et al. [69] | 2021 | USA (97%), Canada (1%), other countries (1%) | Members of the SBI (Society of Breast Imaging) and the National Consortium of Breast Centers (NCBC) | 31–40 (19%) 41–50 (26%) 51–60 (34%) 61–70 (20%) 71+ (2%) | <5 (11%) 5–10 (18%) 11–20 (19%) 20+ (52%) | Female 79% male 21% | From 29 June 2020 to 18 September 2020 | Overall response rate 18%. Anxiety was reported by 68% of respondents, followed by sadness (41%), sleep problems (36%), anger (25%), and depression (23%) A higher psychological distress score correlated with female gender (OR 1.9, p = 0.001), younger age (OR 0.8 per SD; p = 0.005), and a higher financial loss score (OR 1.4, p < 0.0001) Participants whose practices had not initiated wellness efforts specific to COVID-19 (54%) had higher psychological distress scores (OR 1.4, p = 0.03) Of those with children at home, 38% reported increased childcare needs, higher in women than men (40% vs. 29%, p < 0.001). A total of 37% reported that childcare needs had adversely affected their jobs, which correlated with higher psychological distress scores (OR 2.2–3.3, p < 0.05) |
| Oprisan et al. [70] | 2021 | Spain | Mean 40.39 (SD 10.8) | 0–4 (20.3%) 5–9 (25%) 10–19 (29.1%) 20–29 (18.9%) > 30 (6.7%) | Female 58.7% male 41.3% | From April to August 2020 | The prevalence of burnout syndrome increased during the COVID-19 pandemic (49.3% vs. 33.6%, p = 0.002) No risk factors or protective factors that were valid both before and after the pandemic were identified No correlations were identified between sociodemographic or work-related characteristics and burnout syndrome | |
| Woerner et al. [71] | 2021 | USA (77.5%) India (9.7%) UK (5.9%) Saudi Arabia (2%) Spain (1%) Chile (1%) other (3%) | Interventional radiologists (Society of Interventional Radiology, SIR) | N/A | 78.9% interventional radiologists 21% interventional radiologists in training | Female 15.9% male 83.9% | From 28 November 2020 to 23 December 2020 | The COVID-19 pandemic induced practice alterations and high rates of self-reported anxiety in interventional radiology Female gender, increased call coverage, and lack of adequate or timely departmental adjustments were associated with increased anxiety levels |
| Authors [Reference Number] | Year | Objective |
|---|---|---|
| Aggarwal et al. [72] | 2021 | To discuss several strategies for mitigating high volumes, including abbreviated MRI protocols, 24/7 radiologist coverage, reading room assistants, and other strategies to tackle radiologist burnout |
| Belfi et al. [73] | 2022 | To investigate the process of storytelling as a self-care practice for radiologists |
| Brown et al. [74] | 2021 | To introduce wholeness, rather than wellness, to address the symptoms of burnout To focus radiologist as member of health care teams, rather than an individual, as a solution to the problem |
| Buch et al. [75] | 2021 | To implement a wellness program in an academic radiology department to prevent burnout and to assess initial outcomes, with special focus on the challenges related to the COVID-19 pandemic |
| Fishman et al. [76] | 2021 | To evaluate coaching as a method to combat burnout |
| Glover et al. [77] | 2022 | To evaluate how optimizing radiologist’s work environment to improve overall quality of life and wellness |
| McGrath et al. [78] | 2022 | To enhance radiologists’ productivity and efficiency through optimization of institutional infrastructure, reading room and workstation, user-level interactions with personal devices, and advances in artificial intelligence |
| Oliveira et al. [79] | 2022 | To evaluate key techniques at the individual, peer, and institutional levels to offer a multifaceted approach to ameliorating radiologist burnout |
| Parikh et al. [80] | 2021 | To describe common misperceptions that may contribute to radiology practice leaders not addressing burnout and to explore practical skills that leaders should develop to effectively address burnout |
| Patel et al. [81] | 2021 | To abbreviate musculoskeletal MRI protocols |
| Parikh et al. [80] | 2021 | To evaluate the major stressors affecting breast radiologists |
| Deshmukh et al. [82] | 2022 | To investigate imposter phenomenon, and assess correlation with burnout, in radiologists. To pilot an intervention aimed at addressing imposter phenomenon through improvisational theater techniques |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gabelloni, M.; Faggioni, L.; Fusco, R.; De Muzio, F.; Danti, G.; Grassi, F.; Grassi, R.; Palumbo, P.; Bruno, F.; Borgheresi, A.; et al. Exploring Radiologists’ Burnout in the COVID-19 Era: A Narrative Review. Int. J. Environ. Res. Public Health 2023, 20, 3350. https://doi.org/10.3390/ijerph20043350
Gabelloni M, Faggioni L, Fusco R, De Muzio F, Danti G, Grassi F, Grassi R, Palumbo P, Bruno F, Borgheresi A, et al. Exploring Radiologists’ Burnout in the COVID-19 Era: A Narrative Review. International Journal of Environmental Research and Public Health. 2023; 20(4):3350. https://doi.org/10.3390/ijerph20043350
Chicago/Turabian StyleGabelloni, Michela, Lorenzo Faggioni, Roberta Fusco, Federica De Muzio, Ginevra Danti, Francesca Grassi, Roberta Grassi, Pierpaolo Palumbo, Federico Bruno, Alessandra Borgheresi, and et al. 2023. "Exploring Radiologists’ Burnout in the COVID-19 Era: A Narrative Review" International Journal of Environmental Research and Public Health 20, no. 4: 3350. https://doi.org/10.3390/ijerph20043350
APA StyleGabelloni, M., Faggioni, L., Fusco, R., De Muzio, F., Danti, G., Grassi, F., Grassi, R., Palumbo, P., Bruno, F., Borgheresi, A., Bruno, A., Catalano, O., Gandolfo, N., Giovagnoni, A., Miele, V., Barile, A., & Granata, V. (2023). Exploring Radiologists’ Burnout in the COVID-19 Era: A Narrative Review. International Journal of Environmental Research and Public Health, 20(4), 3350. https://doi.org/10.3390/ijerph20043350











