Association of Affiliate Stigma with Parenting Stress and Its Moderators among Caregivers of Children with Attention-Deficit/Hyperactivity Disorder
Abstract
1. Introduction
1.1. Parenting Stress in Caregivers of Children with Attention-Deficit/Hyperactivity Disorder
1.2. Affiliate Stigma in Caregivers of CADHD
1.3. Study Aims
2. Materials and Methods
2.1. Participants and Procedure
2.2. Measures
2.2.1. Parenting Stress Index, Fourth Edition Short Form
2.2.2. Affiliate Stigma Scale
2.2.3. Parent Form of the Swanson, Nolan, and Pelham Scale, Version IV
2.2.4. Demographic Characteristics
2.3. Statistical Analysis
3. Results
4. Discussion
4.1. Parenting Stress and AS
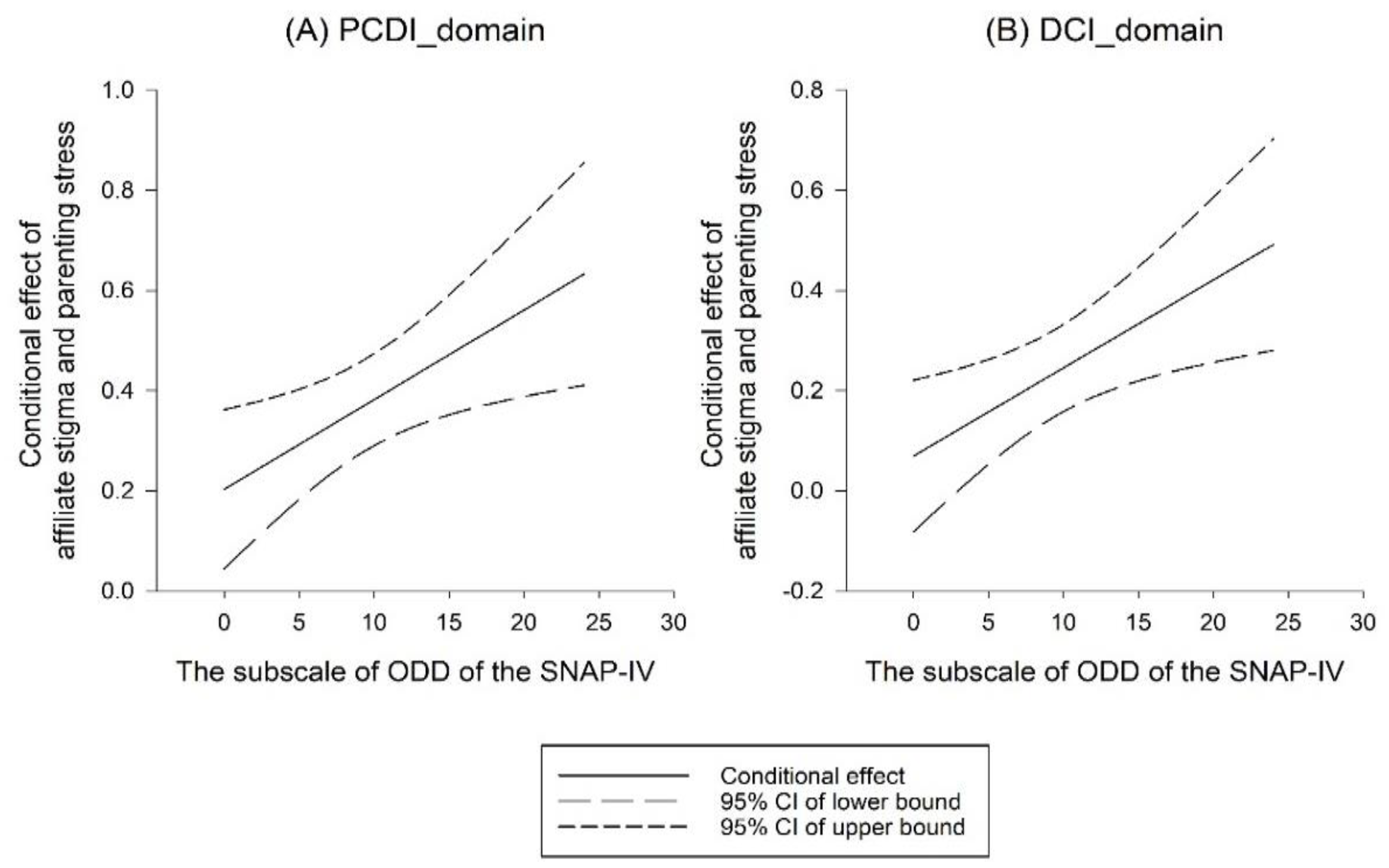
4.2. Moderating Effect of ODD Symptoms
4.3. Implications for Practice
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sayal, K.; Prasad, V.; Daley, D.; Ford, T.; Coghill, D. ADHD in children and young people: Prevalence, care pathways, and service provision. Lancet Psychiatry 2018, 5, 175–186. [Google Scholar] [CrossRef] [PubMed]
- Perez Algorta, G.; Kragh, C.A.; Arnold, L.E.; Molina, B.S.G.; Hinshaw, S.P.; Swanson, J.M.; Hechtman, L.; Copley, L.M.; Lowe, M.; Jensen, P.S. Maternal ADHD symptoms, personality, and parenting Stress: Differences between mothers of children with ADHD and mothers of comparison children. J. Atten. Disord. 2018, 22, 1266–1277. [Google Scholar] [CrossRef]
- Wiener, J.; Biondic, D.; Grimbos, T.; Herbert, M. Parenting stress of parents of adolescents with attention-deficit hyperactivity disorder. J. Abnorm. Child. Psychol. 2016, 44, 561–574. [Google Scholar] [CrossRef] [PubMed]
- Cussen, A.; Sciberras, E.; Ukoumunne, O.C.; Efron, D. Relationship between symptoms of attention-deficit/hyperactivity disorder and family functioning: A community-based study. Eur. J. Pediatr. 2012, 171, 271–280. [Google Scholar] [CrossRef] [PubMed]
- Theule, J.; Wiener, J.; Tannock, R.; Jenkins, J.M. Parenting stress in families of children with ADHD: A meta-analysis. J. Emot. Behav. Disord. 2013, 21, 3–17. [Google Scholar] [CrossRef]
- Leitch, S.; Sciberras, E.; Post, B.; Gerner, B.; Rinehart, N.; Nicholson, J.M.; Evans, S. Experience of stress in parents of children with ADHD: A qualitative study. Int. J. Qual. Stud. Health Well-Being 2019, 14, 1690091. [Google Scholar] [CrossRef]
- Abidin, R.R. Parenting Stress Index, 4th ed.; Psychological Assessment Resources: Lutz, FL, USA, 2012. [Google Scholar]
- Graziano, P.A.; McNamara, J.P.; Geffken, G.R.; Reid, A. Severity of children’s ADHD symptoms and parenting stress: A multiple mediation model of self-regulation. J. Abnorm. Child Psychol. 2011, 39, 1073–1083. [Google Scholar] [CrossRef] [PubMed]
- Breen, M.J.; Barkley, R.A. Child psychopathology and parenting stress in girls and boys having attention deficit disorder with hyperactivity. J. Pediatr. Psychol. 1988, 13, 265–280. [Google Scholar] [CrossRef] [PubMed]
- McLuckie, A.; Landers, A.L.; Rowbotham, M.; Landine, J.; Schwartz, M.; Ng, D. Are parent- and teacher-reported executive function difficulties associated with parenting stress for Children diagnosed with ADHD? J. Atten. Disord. 2021, 25, 22–32. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.J.; Kim, J. Effect of maternal anxiety on parenting stress of fathers of children with ADHD. J. Korean Med. Sci. 2022, 37, e89. [Google Scholar] [CrossRef]
- Muñoz-Silva, A.; Lago-Urbano, R.; Sanchez-Garcia, M.; Carmona-Márquez, J. Child/adolescent’s ADHD and parenting stress: The mediating role of family impact and conduct problems. Front. Psychol. 2017, 8, 2252. [Google Scholar] [CrossRef]
- Podolski, C.-L.; Nigg, J.T. Parent stress and coping in relation to child ADHD severity and associated child disruptive behavior problems. J. Clin. Child. Psychol. 2001, 30, 503–513. [Google Scholar] [CrossRef]
- Theule, J.; Wiener, J.; Rogers, M.A.; Marton, I. Predicting parenting stress in families of children with ADHD: Parent and contextual factors. J. Child. Fam. Stud. 2011, 20, 640–647. [Google Scholar] [CrossRef]
- Charbonnier, E.; Caparos, S.; Trémolière, B. The role of mothers’ affiliate stigma and child’s symptoms on the distress of mothers with ADHD children. J. Ment. Health 2019, 28, 282–288. [Google Scholar] [CrossRef]
- Mak, W.W.; Cheung, R.Y. Affiliate stigma among caregivers of people with intellectual disability or mental illness. J. Appl. Res. Intellect. Disabil. 2008, 21, 532–545. [Google Scholar] [CrossRef]
- Mak, W.W.; Cheung, R.Y. Psychological distress and subjective burden of caregivers of people with mental illness: The role of affiliate stigma and face concern. Commun. Ment. Health J. 2012, 48, 270–274. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.-L.; Chang, C.-C.; Chen, Y.-M.; Liu, T.-L.; Hsiao, R.C.; Chou, W.-J.; Yen, C.-F. Association between affiliate stigma and depression and its moderators in caregivers of children with attention-deficit/hyperactivity disorder. J. Affect Disord. 2021, 279, 59–65. [Google Scholar] [CrossRef]
- Chang, C.-C.; Chen, Y.-M.; Liu, T.-L.; Hsiao, R.C.; Chou, W.-J.; Yen, C.-F. Affiliate stigma and related factors in family caregivers of children with attention-deficit/hyperactivity disorder. Int. J. Environ. Res. Public Health 2020, 17, 576. [Google Scholar] [CrossRef]
- Chou, W.-J.; Liu, T.-L.; Hsiao, R.C.; Chen, Y.-M.; Chang, C.-C.; Yen, C.-F. Application and perceived effectiveness of complementary and alternative intervention strategies for attention-deficit/hyperactivity disorder: Relationships with affiliate stigma. Int. J. Environ. Res. Public Health 2020, 17, 1505. [Google Scholar] [CrossRef]
- Chou, W.-J.; Liu, T.-L.; Hsiao, R.C.; Chen, Y.-M.; Chang, C.-C.; Yen, C.-F. Caregiver-attributed etiologies of children’s attention-deficit/hyperactivity disorder: A study in Taiwan. Int. J. Environ. Res. Public Health 2020, 17, 1652. [Google Scholar] [CrossRef]
- Chang, C.-C.; Chen, Y.-M.; Hsiao, R.C.; Chou, W.-J.; Yen, C.-F. Did affiliate stigma predict affective and behavioral outcomes in caregivers and their children with attention-deficit/hyperactivity disorder? Int. J. Environ. Res. Public Health 2021, 18, 7532. [Google Scholar] [CrossRef] [PubMed]
- Mikami, A.Y.; Chong, G.K.; Saporito, J.M.; Na, J.J. Implications of parental affiliate stigma in families of children with ADHD. J. Clin. Child Adolesc. Psychol. 2015, 44, 595–603. [Google Scholar] [CrossRef] [PubMed]
- Maughan, B.; Rowe, R.; Messer, J.; Goodman, R.; Meltzer, H. Conduct disorder and oppositional defiant disorder in a national sample: Developmental epidemiology. J. Child. Psychol. Psychiatry 2004, 45, 609–621. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, Y.P.; Wu, C.F.; Chou, W.J.; Yen, C.F. Multidimensional correlates of parental self-efficacy in managing adolescent internet use among parents of adolescents with attention-deficit/hyperactivity disorder. Int. J. Environ. Res. Public Health 2020, 17, 5768. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Potvin, S.; Pelletier, J.; Grot, S.; Hébert, C.; Barr, A.M.; Lecomte, T. Cognitive deficits in individuals with methamphetamine use disorder: A meta-analysis. Addict. Behav. 2018, 80, 154–160. [Google Scholar] [CrossRef]
- Wollman, S.C.; Hauson, A.O.; Hall, M.G.; Connors, E.J.; Allen, K.E.; Stern, M.J.; Stephan, R.A.; Kimmel, C.L.; Sarkissians, S.; Barlet, B.D.; et al. Neuropsychological functioning in opioid use disorder: A research synthesis and meta-analysis. Am. J. Drug Alcohol Abuse 2019, 45, 11–25. [Google Scholar] [CrossRef]
- Rehm, J.; Hasan, O.S.M.; Black, S.E.; Shield, K.D.; Schwarzinger, M. Alcohol use and dementia: A systematic scoping review. Alzheimers Res. Ther. 2019, 11, 1. [Google Scholar] [CrossRef]
- Khalil, M.; Hollander, P.; Raucher-Chéné, D.; Lepage, M.; Lavigne, K.M. Structural brain correlates of cognitive function in schizophrenia: A meta-analysis. Neurosci. Biobehav. Rev. 2022, 132, 37–49. [Google Scholar] [CrossRef]
- Weng, Y. Taiwanese Version of the Parenting Stress Index–Short Form; Psychological Publishing Corporation: Taipei, Taiwan, 2011. [Google Scholar]
- Chang, C.-C.; Su, J.-A.; Tsai, C.-S.; Yen, C.-F.; Liu, J.-H.; Lin, C.-Y. Rasch analysis suggested three unidimensional domains for Affiliate Stigma Scale: Additional psychometric evaluation. J. Clin. Epidemiol. 2015, 68, 674–683. [Google Scholar] [CrossRef]
- Swanson, J.M.; Kraemer, H.C.; Hinshaw, S.P.; Arnold, L.E.; Conners, C.K.; Abikoff, H.B.; Clevenger, W.; Davies, M.; Elliott, G.R.; Greenhill, L.L. Clinical relevance of the primary findings of the MTA: Success rates based on severity of ADHD and ODD symptoms at the end of treatment. J. Am. Acad. Child Adolesc. Psychiatry 2001, 40, 168–179. [Google Scholar] [CrossRef] [PubMed]
- Gau, S.S.F.; Shang, C.Y.; Liu, S.K.; Lin, C.H.; Swanson, J.M.; Liu, Y.C.; Tu, C.L. Psychometric properties of the Chinese version of the Swanson, Nolan, and Pelham, version IV scale–parent form. Int. J. Methods Psychiatr. Res. 2008, 17, 35–44. [Google Scholar] [CrossRef]
- Baron, R.M.; Kenny, D.A. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J. Pers. Soc. Psychol. 1986, 51, 1173. [Google Scholar] [CrossRef]
- Kim, H.-Y. Statistical notes for clinical researchers: Assessing normal distribution (2) using skewness and kurtosis. Restor. Dent. Endod. 2013, 38, 52–54. [Google Scholar] [CrossRef]
- Senaviratna, N.; Cooray, T. Diagnosing multicollinearity of logistic regression model. Asian J. Probab. Statist. 2019, 5, 1–9. [Google Scholar] [CrossRef]
- Chang, C.C.; Chen, Y.M.; Hsiao, R.C.; Chou, W.J.; Yen, C.F. Affiliate stigma in caregivers of children with attention-deficit/hyperactivity disorder: The roles of stress-coping orientations and parental child-rearing styles. Int. J. Environ. Res. Public Health 2021, 18, 9004. [Google Scholar] [CrossRef] [PubMed]
- Harrison, C.; Sofronoff, K. ADHD and parental psychological distress: Role of demographics, child behavioral characteristics, and parental cognitions. J. Am. Acad. Child. Adolesc. Psychiatry 2002, 41, 703–711. [Google Scholar] [CrossRef]
- Manti, F.; Giovannone, F.; Sogos, C. Parental stress of preschool children with generalized anxiety or oppositional defiant disorder. Front. Pediatr. 2019, 7, 415. [Google Scholar] [CrossRef] [PubMed]
- Ross, C.N.; Blanc, H.M.; McNeil, C.B.; Eyberg, S.M.; Hembree-Kigin, T.L. Parenting stress in mothers of young children with oppositional defiant disorder and other severe behavior problems. Child Study J. 1998, 28, 93–110. [Google Scholar]
- Grimmett, M.A.; Dunbar, A.S.; Williams, T.; Clark, C.; Prioleau, B.; Miller, J.S. The process and implications of diagnosing oppositional defiant disorder in African American males. Prof. Counselor 2016, 6, 147–160. [Google Scholar] [CrossRef]
- Fadus, M.C.; Ginsburg, K.R.; Sobowale, K.; Halliday-Boykins, C.A.; Bryant, B.E.; Gray, K.M.; Squeglia, L.M. Unconscious bias and the diagnosis of disruptive behavior disorders and ADHD in African American and Hispanic Youth. Acad. Psychiatry 2020, 44, 95–102. [Google Scholar] [CrossRef]
- Beltrán, S.; Sit, L.; Ginsburg, K.R. A call to revise the diagnosis of oppositional defiant disorder—Diagnoses are for helping, not harming. JAMA Psychiatry 2021, 78, 1181–1182. [Google Scholar] [CrossRef]
- Poulton, A.S. Time to redefine the diagnosis of oppositional defiant disorder. J. Paediatr. Child Health 2011, 47, 332–334. [Google Scholar] [CrossRef]
- Singh, A.; Yeh, C.J.; Verma, N.; Das, A.K. Overview of attention deficit hyperactivity disorder in young children. Health Psychol. Res. 2015, 3, 2115. [Google Scholar] [CrossRef]
- Rappley, M.D. Clinical practice. Attention deficit-hyperactivity disorder. N. Engl. J. Med. 2005, 352, 165–173. [Google Scholar] [CrossRef]
- Loeber, R.; Burke, J.D.; Lahey, B.B.; Winters, A.; Zera, M. Oppositional defiant and conduct disorder: A review of the past 10 years, part I. J. Am. Acad. Child Adolesc. Psychiatry 2000, 39, 1468–1484. [Google Scholar] [CrossRef]
- Nguyen, P.; Hinshaw, S. Understanding the stigma associated with ADHD: Hope for the future? ADHD Rep. 2020, 28, 1–10. [Google Scholar] [CrossRef]
- Montoya, A.; Colom, F.; Ferrin, M. Is psychoeducation for parents and teachers of children and adolescents with ADHD efficacious? A systematic literature review. Eur. Psychiatry 2011, 26, 166–175. [Google Scholar] [CrossRef] [PubMed]
- McCleary, L. Parenting adolescents with attention deficit hyperactivity disorder: Analysis of the literature for social work practice. Health Soc. Work 2002, 27, 285–292. [Google Scholar] [CrossRef]
- Daley, D.; Van der Oord, S.; Ferrin, M.; Cortese, S.; Danckaerts, M.; Doepfner, M.; Van den Hoofdakker, B.J.; Coghill, D.; Thompson, M.; Asherson, P. Practitioner review: Current best practice in the use of parent training and other behavioural interventions in the treatment of children and adolescents with attention deficit hyperactivity disorder. J. Child Psychol. Psychiatry 2018, 59, 932–947. [Google Scholar] [CrossRef]
- Lavigne, J.V.; LeBailly, S.A.; Gouze, K.R.; Cicchetti, C.; Jessup, B.W.; Arend, R.; Pochyly, J.; Binns, H.J. Predictor and moderator effects in the treatment of oppositional defiant disorder in pediatric primary care. J. Pediatr. Psychol. 2008, 33, 462–472. [Google Scholar] [CrossRef][Green Version]
| n (%) | Mean (SD) | Range | |
|---|---|---|---|
| Caregiver factors | |||
| Sex | |||
| Female | 168 (78.9) | ||
| Male | 45 (21.1) | ||
| Age (years) | 44.63 (6.11) | 30–69 | |
| Years of education (years) | 14.15 (3.02) | 6–24 | |
| Affiliate stigma | 37.84 (10.78) | 22–72 | |
| Children factors | |||
| Sex | |||
| Boy | 181 (85.0) | ||
| Girl | 32 (15.0) | ||
| Age (years) | 12.88 (2.15) | 10–18 | |
| Inattention | 13.18 (5.90) | 1–27 | |
| Hyperactivity/impulsivity | 9.01 (5.89) | 0–26 | |
| Oppositional defiance | 9.57 (6.03) | 0–24 | |
| Parenting stress | |||
| Parental distress | 32.54 (9.20) | 12–57 | |
| Parent–child dysfunctional interaction | 30.29 (8.52) | 12–52 | |
| Difficult child | 31.90 (8.65) | 11–54 |
| Parental Distress | Parent–Child Dysfunctional Interaction | Difficult Child | |
|---|---|---|---|
| B (se) | B (se) | B (se) | |
| Caregivers’ sex a | −1.297 (1.386) | 2.131 (1.208) | 1.348 (1.150) |
| Caregivers’ age | −0.027 (0.098) | 0.119 (0.085) | 0.052 (0.081) |
| Caregivers’ education | 0.068 (0.190) | −0.322 (0.165) | −0.068 (0.157) |
| Children’s sex b | 1.104 (1.592) | 0.478 (1.387) | −0.666 (1.321) |
| Children’s age | −0.231 (0.284) | 0.172 (0.248) | −0.035 (0.236) |
| Children’s inattention | 0.247 (0.118) * | 0.147 (0.103) | 0.201 (0.098) * |
| Children’s hyperactivity/impulsivity | −0.033 (0.136) | −0.105 (0.118) | −0.028 (0.113) |
| Children’s oppositional defiance | 0.165 (0.122) | 0.286 (0.106) ** | 0.669 (0.101) *** |
| Affiliate stigma | 0.340 (0.054) *** | 0.371 (0.047) *** | 0.235 (0.045) *** |
| R2 | 0.256 | 0.342 | 0.421 |
| Adjusted R2 | 0.223 | 0.312 | 0.395 |
| F | 7.780 *** | 11.698 *** | 16.400 *** |
| Parental Distress | Parent–Child Dysfunctional Interaction | Difficult Child | |
|---|---|---|---|
| B (se) | B (se) | B (se) | |
| Caregivers’ age | −0.029 (0.098) | 0.119 (0.084) | 0.057 (0.080) |
| Caregivers’ education | 0.065 (0.190) | −0.354 (0.163) * | −0.094 (0.156) |
| Children’s sex | 1.099 (1.596) | 0.574 (1.369) | −0.548 (1.303) |
| Children’s age | −0.242 (0.286) | 0.119 (0.245) | −0.066 (0.234) |
| Caregivers’ sex | −1.299 (1.389) | 2.566 (1.204) * | 1.839 (1.147) |
| Children’s inattention | 0.128 (0.346) | 0.196 (0.103) | 0.556 (0.302) |
| Children’s hyperactivity/impulsivity | −0.035 (0.136) | −0.155 (0.118) | −0.079 (0.112) |
| Children’s oppositional defiance | 0.170 (0.123) | −0.398 (0.289) | −0.106 (0.290) |
| Affiliate stigma | 0.298 (0.128) * | 0.203 (0.081) * | 0.155 (0.111) |
| Inattention X Affiliate stigma | 0.003 (0.009) | −0.008 (0.007) | |
| Oppositional defiance X Affiliate stigma | 0.018 (0.007) * | 0.020 (0.007) ** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, P.-Y.; Chou, W.-J.; Hsiao, R.C.; Liu, T.-L.; Yen, C.-F. Association of Affiliate Stigma with Parenting Stress and Its Moderators among Caregivers of Children with Attention-Deficit/Hyperactivity Disorder. Int. J. Environ. Res. Public Health 2023, 20, 3192. https://doi.org/10.3390/ijerph20043192
Lin P-Y, Chou W-J, Hsiao RC, Liu T-L, Yen C-F. Association of Affiliate Stigma with Parenting Stress and Its Moderators among Caregivers of Children with Attention-Deficit/Hyperactivity Disorder. International Journal of Environmental Research and Public Health. 2023; 20(4):3192. https://doi.org/10.3390/ijerph20043192
Chicago/Turabian StyleLin, Pei-Yun, Wen-Jiun Chou, Ray C. Hsiao, Tai-Ling Liu, and Cheng-Fang Yen. 2023. "Association of Affiliate Stigma with Parenting Stress and Its Moderators among Caregivers of Children with Attention-Deficit/Hyperactivity Disorder" International Journal of Environmental Research and Public Health 20, no. 4: 3192. https://doi.org/10.3390/ijerph20043192
APA StyleLin, P.-Y., Chou, W.-J., Hsiao, R. C., Liu, T.-L., & Yen, C.-F. (2023). Association of Affiliate Stigma with Parenting Stress and Its Moderators among Caregivers of Children with Attention-Deficit/Hyperactivity Disorder. International Journal of Environmental Research and Public Health, 20(4), 3192. https://doi.org/10.3390/ijerph20043192







