Sleep Architecture and Sleep-Related Breathing Disorders of Seafarers on Board Merchant Ships: A Polysomnographic Pilot Field Study on the High Seas
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Patient and Public Involvement Statement
2.3. Methods
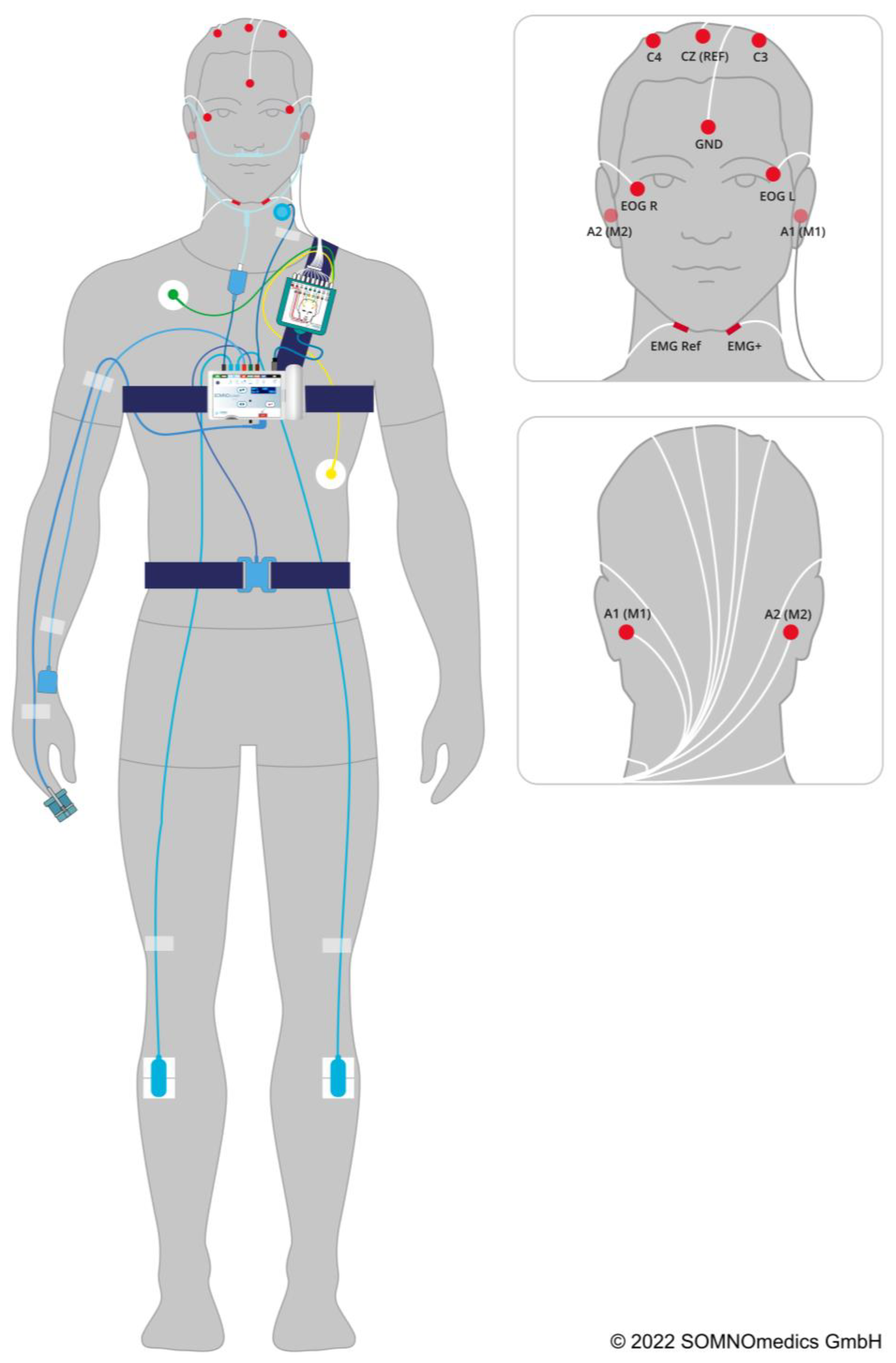
2.3.1. Polysomnography
2.3.2. Pupillometry
2.3.3. Questionnaires
2.4. Statistical Analysis
3. Results
3.1. Quality of Polysomnography on Board Merchant Ships
3.2. Demographics. Comparison of Watchkeepers and Day Workers
3.3. Prevalence of Sleep Disordered-Breathing in Seafarers
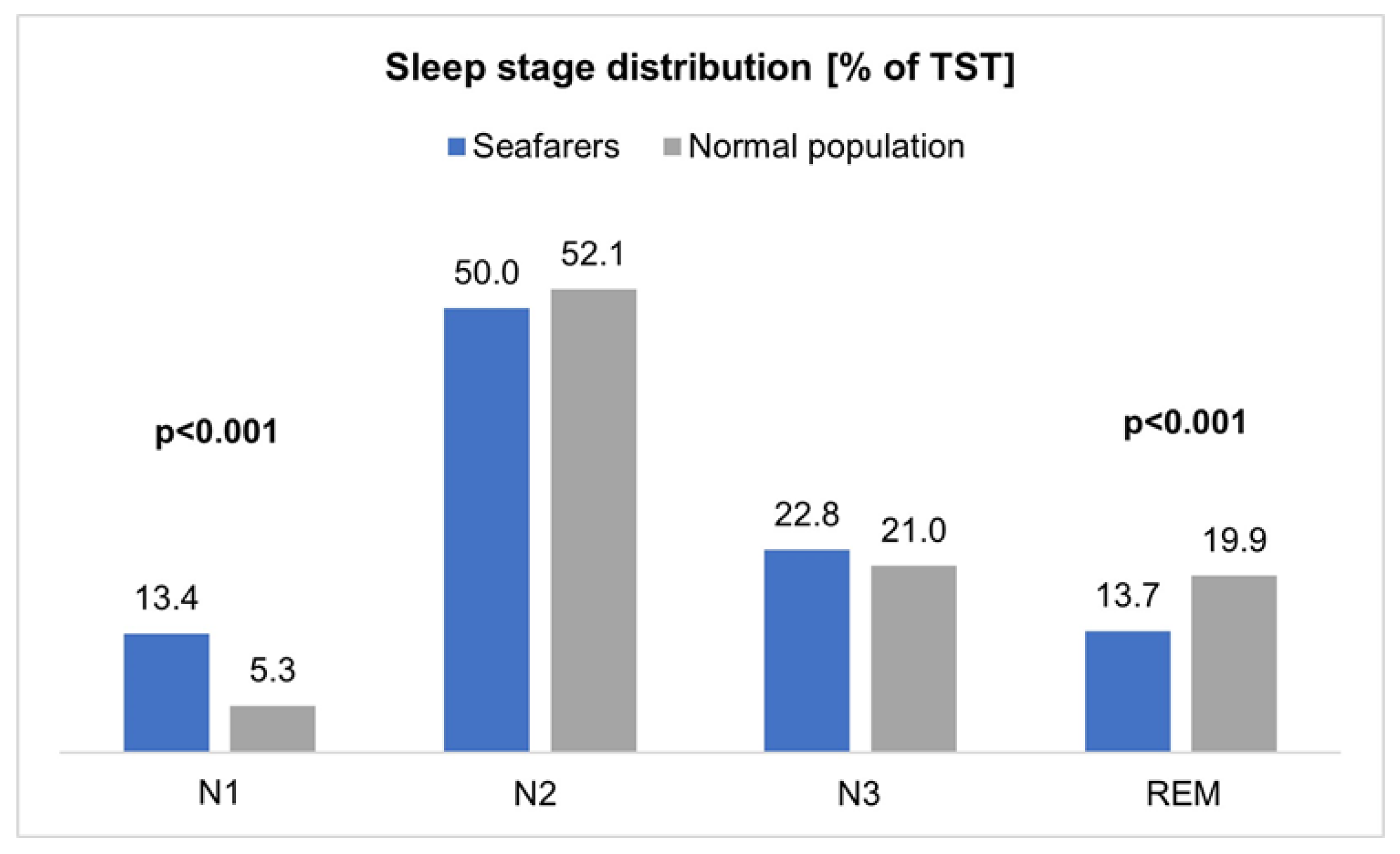
3.4. Comparison of the Objective Sleep Quality of Seafarers with the Normal Population
3.5. The Influence of Age, Seafaring Experience and Length of Stay on Board on Sleepiness and Sleep Behavior
3.6. Correlation of Sleepiness on Board Measured with ESS, Pupillometry and PSG
4. Discussion
4.1. Quality of Polysomnography on Board Merchant Ships
4.2. Comparison of Watchkeepers and Day Workers
4.3. Prevalence of Sleep-Disordered Breathing in Seafarers
4.4. Comparison of the Objective Sleep Quality of Seafarers with the Normal Population
4.5. Influence of Age, Seafaring Experience, and Length of Stay on Board on Sleepiness and Sleep Behavior
4.6. Correlation of Sleepiness on Board Measured with ESS, Pupillometry and PSG
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Oldenburg, M.; Baur, X.; Schlaich, C. Occupational Risks and Challenges of Seafaring. J. Occup. Health 2010, 52, 249–256. [Google Scholar] [CrossRef] [PubMed]
- Matsangas, P.; Shattuck, N.L. Habitability in Berthing Compartments and Well-Being of Sailors Working on U.S. Navy Surface Ships. Hum. Factors: J. Hum. Factors Ergon. Soc. 2020, 63, 462–473. [Google Scholar] [CrossRef]
- Lützhöft, M.; Dahlgren, A.; Kircher, A.; Msc, B.T.; Gillberg, M. Fatigue at sea in Swedish shipping-a field study. Am. J. Ind. Med. 2010, 53, 733–740. [Google Scholar] [CrossRef] [PubMed]
- Oldenburg, M.; Jensen, H.-J. Sleepiness of day workers and watchkeepers on board at high seas: A cross-sectional study. BMJ Open 2019, 9, e028449. [Google Scholar] [CrossRef]
- Shattuck, N.L.; Matsangas, P. Does the quality of life differ for shift workers compared to day workers? Chrono. Int. 2020, 37, 1299–1303. [Google Scholar] [CrossRef]
- Oldenburg, M.; Jensen, H.-J. Stress and Strain among Seafarers Related to the Occupational Groups. Int. J. Environ. Res. Public Health 2019, 16, 1153. [Google Scholar] [CrossRef]
- Baumler, R.; De Klerk, Y.; Manuel, M.E.; Carballo Piñeiro, L. A Culture of Adjustment, Evaluating the Implementation of the Current Maritime Regulatory Framework on Rest and Work Hours (EVREST); World Maritime University: Malmö, Sweden, 2020. [Google Scholar]
- Shattuck, N.L.; Matsangas, P. Eating behaviors in sailors of the United States Navy: Meal-to-sleep intervals. Nutr. Health 2020, 27, 260106020960878. [Google Scholar] [CrossRef]
- Kerkamm, F.; Dengler, D.; Eichler, M.; Materzok-Köppen, D.; Belz, L.; Neumann, F.A.; Zyriax, B.C.; Harth, V.; Oldenburg, M. Measurement Methods of Fatigue, Sleepiness, and Sleep Behaviour Aboard Ships: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 19, 120. [Google Scholar] [CrossRef]
- Mayer, G.; Arzt, M.; Braumann, B. S3-Leitlinie Nicht erholsamer Schlaf/Schlafstörungen—Kapitel “Schlafbezogene Atmungsstörungen”. Somnologie 2016, 20, 97–180. [Google Scholar] [CrossRef]
- van Leeuwen, W.M.A.; Kircher, A.; Dahlgren, A.; Lützhöft, M.; Barnett, M.; Kecklund, G.; Åkerstedt, T. Sleep, Sleepiness, and Neurobehavioral Performance While on Watch in a Simulated 4 Hours on/8 Hours off Maritime Watch System. Chrono. Int. 2013, 30, 1108–1115. [Google Scholar] [CrossRef] [PubMed]
- Jay, S.M.; Dawson, D.; Lamond, N. Train Drivers’ Sleep Quality and Quantity during Extended Relay Operations. Chrono. Int. 2006, 23, 1241–1252. [Google Scholar] [CrossRef]
- Signal, T.L.; Gander, P.H.; Berg, M.V.D.; Graeber, R.C. In-Flight Sleep of Flight Crew During a 7-hour Rest Break: Implications for Research and Flight Safety. Sleep 2013, 36, 109–115. [Google Scholar] [CrossRef]
- Phillips, R. Sleep, watchkeeping and accidents: A content analysis of incident at sea reports. Transp. Res. Part F Traffic Psychol. Behav. 2000, 3, 229–240. [Google Scholar] [CrossRef]
- Robb, G.; Sultana, S.; Ameratunga, S.; Jackson, R. A systematic review of epidemiological studies investigating risk factors for work-related road traffic crashes and injuries. Inj. Prev. 2008, 14, 51–58. [Google Scholar] [CrossRef]
- Techera, U.; Hallowell, M.; Stambaugh, N.; Littlejohn, R. Causes and Consequences of Occupational Fatigue: Meta-Analysis and Systems Model. J. Occup. Environ. Med. 2016, 58, 961–973. [Google Scholar] [CrossRef]
- Williamson, A.; Lombardi, D.A.; Folkard, S.; Stutts, J.; Courtney, T.K.; Connor, J.L. The link between fatigue and safety. Accid. Anal. Prev. 2011, 43, 498–515. [Google Scholar] [CrossRef]
- Oldenburg, M. Risk of cardiovascular diseases in seafarers. Int. Marit. Health 2014, 65, 53–57. [Google Scholar] [CrossRef]
- Sagaro, G.; Battineni, G.; Di Canio, M.; Amenta, F. Self-Reported Modifiable Risk Factors of Cardiovascular Disease among Seafarers: A Cross-Sectional Study of Prevalence and Clustering. J. Pers. Med. 2021, 11, 512. [Google Scholar] [CrossRef]
- Eriksson, H.P.; Forsell, K.; Andersson, E. Mortality from cardiovascular disease in a cohort of Swedish seafarers. Int. Arch. Occup. Environ. Health 2019, 93, 345–353. [Google Scholar] [CrossRef] [PubMed]
- Von Katzler, R.; Zyriax, B.C.; Jagemann, B.; Westenhoefer, J.; Jensen, H.J.; Harth, V.; Oldenburg, M. Lifestyle behaviour and prevalence of cardiovascular risk factors—A pilot study comparing Kiribati and European seafarers. BMC Public Health 2019, 19, 855. [Google Scholar] [CrossRef]
- Roberts, S.E.; Jaremin, B. Cardiovascular disease mortality in British merchant shipping and among British seafarers ashore in Britain. Int. Marit. Health 2010, 62, 107–116. [Google Scholar]
- Heinzer, R.; Vat, S.; Marques-Vidal, P.; Marti-Soler, H.; Andries, D.; Tobback, N.; Mooser, V.; Preisig, M.; Malhotra, A.; Waeber, G.; et al. Prevalence of sleep-disordered breathing in the general population: The HypnoLaus study. Lancet Respir. Med. 2015, 3, 310–318. [Google Scholar] [CrossRef] [PubMed]
- Berry, R.B.; Budhiraja, R.; Gottlieb, D.J.; Gozal, D.; Iber, C.; Kapur, V.K.; Marcus, C.L.; Mehra, R.; Parthasarathy, S.; Quan, S.F.; et al. Rules for Scoring Respiratory Events in Sleep: Update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J. Clin. Sleep Med. 2012, 8, 597–619. [Google Scholar] [CrossRef]
- AASM. International Classification of Sleep Disorders, 3rd ed.; American Academy of Sleep Medicine: Darien, IL, USA, 2014. [Google Scholar]
- Weeß, H.-G. Diagnostische Methoden. In Praxis der Schlafmedizin: Diagnostik, Differenzialdiagnostik und Therapie bei Erwachsenen und Kindern, 3rd ed.; Stuck, B.A., Maurer, J.T., Schlarb, A.A., Schredl, M., Weeß, H.G., Eds.; Springer: Berlin/Heidelberg, Germany, 2017; Volume 3, pp. 23–85. [Google Scholar]
- Johns, M.W. A New Method for Measuring Daytime Sleepiness: The Epworth Sleepiness Scale. Sleep 1991, 14, 540–545. [Google Scholar] [CrossRef] [PubMed]
- Johns, M.W. Reliability and Factor Analysis of the Epworth Sleepiness Scale. Sleep 1992, 15, 376–381. [Google Scholar] [CrossRef]
- Johns, M.W. The Epworth Sleepiness Scale—About the ESS. Available online: https://epworthsleepinessscale.com/about-the-ess/ (accessed on 8 August 2021).
- Boulos, M.I.; Jairam, T.; Kendzerska, T.; Im, J.; Mekhael, A.; Murray, B.J. Normal polysomnography parameters in healthy adults: A systematic review and meta-analysis. Lancet Respir. Med. 2019, 7, 533–543. [Google Scholar] [CrossRef]
- Iber, C.; Ancoli-Israel, S.; Chesson, A.; Quan, S.F. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology, and Technical Specifications, 1st ed.; American Academy of Sleep Medicine: Westchester, IL, USA, 2007. [Google Scholar]
- Tan, H.-L.; Kheirandish-Gozal, L.; Gozal, D. Pediatric Home Sleep Apnea Testing: Slowly Getting There! Chest 2015, 148, 1382–1395. [Google Scholar] [CrossRef] [PubMed]
- D’Rozario, A.L.; Dungan, G.C.; Banks, S.; Liu, P.Y.; Wong, K.K.H.; Killick, R.; Grunstein, R.R.; Kim, J.W. An automated algorithm to identify and reject artefacts for quantitative EEG analysis during sleep in patients with sleep-disordered breathing. Sleep Breath. 2014, 19, 607–615. [Google Scholar] [CrossRef]
- DGAUM. S2k-Leitlinie Gesundheitliche Aspekte und Gestaltung von Nacht- und Schichtarbeit. Available online: https://www.awmf.org/uploads/tx_szleitlinien/002-030l_S2k_Gesundheitliche-Aspekte-Gestaltung-Nacht-und-Schichtarbeit_2020-03.pdf (accessed on 23 April 2021).
- Skarpsno, E.S.; Mork, P.J.; Nilsen, T.I.L.; Holtermann, A. Sleep positions and nocturnal body movements based on free-living accelerometer recordings: Association with demographics, lifestyle, and insomnia symptoms. Nat. Sci. Sleep 2017, 9, 267–275. [Google Scholar] [CrossRef]
- De Koninck, J.; Gagnon, P.; Lallier, S. Sleep Positions in the Young Adult and Their Relationship with the Subjective Quality of Sleep. Sleep 1983, 6, 52–59. [Google Scholar] [CrossRef]
- Franklin, K.A.; Lindberg, E. Obstructive sleep apnea is a common disorder in the population—A review on the epidemiology of sleep apnea. J. Thorac. Dis. 2015, 7, 1311–1322. [Google Scholar] [CrossRef]
- Heinzer, R.; Marti-Soler, H.; Haba-Rubio, J. Prevalence of sleep apnoea syndrome in the middle to old age general population. Lancet Respir. Med. 2016, 4, e5–e6. [Google Scholar] [CrossRef] [PubMed]
- Pougnet, R.; Pougnet, L.; Loddé, B.; Canals, L.; Bell, S.; Lucas, D.; Dewitte, J.-D. Consumption of addictive substances in mariners. Int. Marit. Health 2014, 65, 199–204. [Google Scholar] [CrossRef]
- Dashti, H.S.; Scheer, F.A.; Jacques, P.F.; Lamon-Fava, S.; Ordovás, J.M. Short Sleep Duration and Dietary Intake: Epidemiologic Evidence, Mechanisms, and Health Implications. Adv. Nutr. Int. Rev. J. 2015, 6, 648–659. [Google Scholar] [CrossRef]
- Neumann, F.A.; Belz, L.; Dengler, D.; Harth, V.; von Münster, T.; Westenhöfer, J.; Oldenburg, M.; Zyriax, B.-C. Eating behaviour and weight development of European and Asian seafarers during stay on board and at home. J. Occup. Med. Toxicol. 2021, 16, 41. [Google Scholar] [CrossRef] [PubMed]
- Alshaer, H.; Hummel, R.; Mendelson, M.; Marshal, T.; Bradley, T.D. Objective Relationship Between Sleep Apnea and Frequency of Snoring Assessed by Machine Learning. J. Clin. Sleep Med. 2019, 15, 463–470. [Google Scholar] [CrossRef] [PubMed]
- Mäkelä, J.P.; Savolainen, S. Obstructive Sleep Apnea in Loudly Snoring Army Conscripts. Mil. Med. 2007, 172, 879–881. [Google Scholar] [CrossRef]
- Shahid, A.; Wilkinson, K.; Marcu, S.; Shapiro, C.M. STOP, THAT and One Hundred Other Sleep Scales; Springer Science & Business Media: New York, NY, USA, 2012. [Google Scholar]
- Hirshkowitz, M.; Whiton, K.; Albert, S.M.; Alessi, C.; Bruni, O.; DonCarlos, L.; Hazen, N.; Herman, J.; Katz, E.S.; Kheirandish-Gozal, L.; et al. National sleep foundation’s sleep time duration recommendations: Methodology and results summary. Sleep Health 2015, 1, 40–43. [Google Scholar] [CrossRef]
- Maurer, J.T.; Weeß, H.-G.; Schredl, M. Physiologische Grundlagen des normalen und gestörten Schlafes. In Praxis der Schlafmedizin: Diagnostik, Differenzialdiagnostik und Therapie bei Erwachsenen und Kindern, 3rd ed.; Stuck, B.A., Maurer, J.T., Schlarb, A.A., Schredl, M., Weeß, H.G., Eds.; Springer: Berlin/Heidelberg, Germany, 2017; Volume 3. [Google Scholar]
- Lofaso, F.; Coste, A.; Gilain, L.; Harf, A.; Guilleminault, C.; Goldenberg, F. Sleep Fragmentation as a Risk Factor for Hypertension in Middle-aged Nonapneic Snorers. Chest 1996, 109, 896–900. [Google Scholar] [CrossRef]
- Bonnet, M.H.; Doghramji, K.; Roehrs, T.; Stepanski, E.J.; Sheldon, S.H.; Walters, A.S.; Wise, M.; Chesson, A.L., Jr. The Scoring of Arousal in Sleep: Reliability, Validity, and Alternatives. J. Clin. Sleep Med. 2007, 3, 133–145. [Google Scholar] [CrossRef]
- Shrivastava, D.; Jung, S.; Saadat, M.; Sirohi, R.; Crewson, K. How to interpret the results of a sleep study. J. Community Hosp. Intern. Med. Perspect. 2014, 4, 24983. [Google Scholar] [CrossRef]
- Huang, C.-Y.; Yu, C.-C. Different diagnostic criteria for periodic leg movements in patients with obstructive sleep apnea after continuous positive airway pressure titration. Neuropsychiatr. Dis. Treat. 2019, 15, 2129–2136. [Google Scholar] [CrossRef]
- Glovinsky, P.B.; Spielman, A.J.; Carroll, P.; Weinstein, L.; Ellman, S.J. Sleepiness and REM Sleep Recurrence: The Effects of Stage 2 and REM Sleep Awakenings. Psychophysiology 1990, 27, 552–559. [Google Scholar] [CrossRef]
- Nykamp, K.; Rosenthal, L.; Folkerts, M.; Roehrs, T.; Guido, P.; Roth, T. The effects of REM sleep deprivation on the level of sleepiness/alertness. Sleep 1998, 21, 609–614. [Google Scholar] [CrossRef]
- Jaipurkar, R.; Mahapatra, S.; Bobdey, S.; Banerji, C. Work–rest pattern, alertness and performance assessment among naval personnel deployed at sea: A cross sectional study. Med. J. Armed Forces India 2019, 75, 158–163. [Google Scholar] [CrossRef] [PubMed]
- Sunde, E.; Bratveit, M.; Pallesen, S.; Moen, B.E. Noise and sleep on board vessels in the Royal Norwegian Navy. Noise Health 2016, 18, 85–92. [Google Scholar] [CrossRef]
- Harris, E.; Taylor, M.K.; Drummond, S.; Larson, G.E.; Potterat, E.G. Assessment of Sleep Disruption and Sleep Quality in Naval Special Warfare Operators. Mil. Med. 2015, 180, 803–808. [Google Scholar] [CrossRef]
- Espinoza, H.; Thornton, A.T.; Sharp, D.; Antic, R.; McEvoy, R.D. Sleep Fragmentation and Ventilatory Responsiveness to Hypercapnia. Am. Rev. Respir. Dis. 1991, 144, 1121–1124. [Google Scholar] [CrossRef] [PubMed]
- Series, F.; Roy, N.; Marc, I. Effects of sleep deprivation and sleep fragmentation on upper airway collapsibility in normal subjects. Am. J. Respir. Crit. Care Med. 1994, 150, 481–485. [Google Scholar] [CrossRef] [PubMed]
- Vold, M.L.; Aasebø, U.; Wilsgaard, T.; Melbye, H. Low oxygen saturation and mortality in an adult cohort: The Tromsø study. BMC Pulm. Med. 2015, 15, 9. [Google Scholar] [CrossRef]
- Vold, M.L.; Aasebø, U.; Hjalmarsen, A.; Melbye, H. Predictors of oxygen saturation ≤95% in a cross-sectional population based survey. Respir. Med. 2012, 106, 1551–1558. [Google Scholar] [CrossRef] [PubMed]
- Hystad, S.W.; Eid, J. Sleep and Fatigue Among Seafarers: The Role of Environmental Stressors, Duration at Sea and Psychological Capital. Saf. Health Work 2016, 7, 363–371. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, K.; Kobayashi, F.; Hori, R.; Arita, A.; Sasanabe, R.; Shiomi, T. Association between pupillometric sleepiness measures and sleep latency derived by MSLT in clinically sleepy patients. Environ. Health Prev. Med. 2013, 18, 361–367. [Google Scholar] [CrossRef] [PubMed]
- Aurora, R.N.; Caffo, B.; Crainiceanu, C.; Punjabi, N.M. Correlating Subjective and Objective Sleepiness: Revisiting the Association Using Survival Analysis. Sleep 2011, 34, 1707–1714. [Google Scholar] [CrossRef]
| Start of TIB | Number | Percentage | |
|---|---|---|---|
| Watchkeepers (n = 11) | midnight–4 a.m. | 3 | 27.3 |
| 4 a.m.–8 a.m. | 2 | 18.2 | |
| 8 p.m.–midnight | 6 | 54.5 | |
| Day workers (n = 8) | 8 p.m.–midnight | 8 | 100.0 |
| Impedance Quality n (%) | Signal Quality n (%) | |
|---|---|---|
| Good | 11 (57.9) | 19 (100.0) |
| Sufficient | 8 (42.1) | 0 (0) |
| Poor | 0 (0) | 0 (0) |
| n (%) | Mean | SD | Minimum | Maximum | |
|---|---|---|---|---|---|
| Resp. artifacts [%TIB] | 2 (10.5) | 30.5 | 40.1 | 2.1 | 58.8 |
| O2-artifacts [%TIB] | 7 (36.8) | 6.7 | 6.3 | 0.1 | 16.9 |
| HR-artifacts [%TIB] | 3 (15.8) | 0.2 | 0.1 | 0.1 | 0.2 |
| Total (n = 19) | Watchkeepers (n = 11) | Day Workers (n = 8) | |
|---|---|---|---|
| Demographic and lifestyle parameters | |||
| Age, mean (min–max) | 42.2 (25–61) | 41.6 (25–61) | 43.1 (27–60) |
| Nationality, n (%) | |||
| European | 5 (26.3) | 3 (27.3) | 2 (25.0) |
| Non-European | 14 (73.7) | 8 (72.7) | 6 (75.0) |
| Officers, n (%) | 6 (31.6) | 4 (36.4) | 2 (25.0) |
| Non-Officers, n (%) | 13 (68.4) | 7 (63.6) | 6 (75.0) |
| Length of stay on board [d], mean (SD) | 115.1 (65.0) | 106.1 (65.1) | 127.4 (67.3) |
| BMI [kg/m2], mean (SD) | 27.2 (4.4) | 27.3 (4.1) | 27.2 (5.0) |
| BMI ≥ 25, n (%) | 11 (57.9) | 7 (63.6) | 4 (50.0) |
| Smoking (current or former), n (%) | 10 (52.6) | 6 (54.5) | 4 (50.0) |
| Subjectively disturbed on board by: | |||
| Noise, n (%) | 10 (52.6) | 5 (45.5) | 5 (62.5) |
| Vibration, n (%) | 10 (52.6) | 5 (45.5) | 5 (62.5) |
| Ship movement, n (%) | 7 (36.8) | 4 (36.4) | 3 (37.5) |
| Subjective Sleep Parameters | Total (n = 19) | Watchkeepers (n = 11) | Day Workers (n = 8) | p-Value |
|---|---|---|---|---|
| Snoring, n (%) | 13 (86.7) | 8 (88.9) | 5 (83.3) | 1.000 3 |
| Sleep problems, n (%) | 6 (31.6) | 4 (36.4) | 2 (25.0) | 1.000 3 |
| Sleepiness | ||||
| ESS, median (min–max) | 6 (3–12) | 6 (3–11) | 9 (3–12) | 0.536 2 |
| ESS > 5, n (%) | 11 (61.1) | 7 (63.6) | 4 (57.1) | 1.000 3 |
| ESS > 10 (EDS), n (%) | 3 (16.7) | 1 (9.1) | 2 (28.6) | 0.528 3 |
| rPUI, mean (SD) | 1.2 (0.7) | 1.1 (0.8) | 1.4 (0.7) | 0.690 1 |
| rPUI, n (%) | ||||
| Normal (<1.02) | 5 (55.6) | 3 (50.0) | 2 (66.7) | |
| Conspicuous (≥1.02–<1.53) | 1 (11.1) | 1 (16.7) | 0 (0.0) | |
| Unift for duty (≥1.53) | 3 (33.3) | 2 (33.3) | 1 (33.3) |
| Total (n = 19) | Watchkeepers (n = 11) | Day Workers (n = 8) | p-Value | |
|---|---|---|---|---|
| Objective sleep quality | ||||
| TIB [min], mean (SD) | 391.0 (81.5) | 359.3 (83.1) | 434.7 (58.8) | 0.043 1 |
| TST [min], mean (SD) | 323.2 (89.5) | 283.3 (90.3) | 377.9 (55.1) | 0.018 1 |
| WASO [min], mean (SD) | 38.2 (21.6) | 41.9 (25.2) | 33.1 (15.6) | 0.394 1 |
| Sleep efficiency [%], mean (SD) | 81.9 (10.3) | 78.3 (11.5) | 87.0 (5.7) | 0.065 1 |
| Sleep onset latency (SOL) [min], mean (SD) | 20.9 (26.8) | 21.7 (29.9) | 19.9 (23.9) | 0.840 2 |
| Deep sleep latency (N3 latency) [min], mean (SD) | 42.3 (36.5) | 46.8 (40.4) | 36.3 (32.0) | 0.442 2 |
| REM latency [min] | 112.9 (59.4) | 113.6 (74.2) | 111.9 (34.6) | 0.946 1 |
| Sleep stage duration [%TST], mean (SD) | ||||
| N1 | 13.4 (7.3) | 14.6 (6.0) | 11.9 (8.9) | 0.446 1 |
| N2 | 50.0 (11.9) | 48.2 (12.3) | 52.6 (11.5) | 0.437 1 |
| N3 | 22.8 (11.2) | 23.5 (9.0) | 22.0 (14.3) | 0.787 1 |
| REM | 13.7 (5.7) | 13.8 (6.7) | 13.5 (4.5) | 0.930 1 |
| Sleep stage transition index [n/h], mean (SD) | 21.6 (11.1) | 25.0 (12.3) | 17.1 (4.5) | 0.041 2 |
| Arousal index [n/h], mean (SD) | 29.4 (18.7) | 32.6 (18.4) | 24.9 (19.3) | 0.388 1 |
| Wake number index [n/h], mean (SD) | 7.9 (7.2) | 10.2 (8.8) | 5.0 (2.1) | 0.016 2 |
| #wake respiratory index [n/h], mean (SD) | 3.4 (7.4) | 4.9 (9.5) | 1.4 (2.3) | 0.351 2 |
| PLMS index [n/h], mean (SD) | 4.0 (7.2) | 3.1 (3.2) | 5.3 (10.8) | 0.600 2 |
| Body position change index [n/h], mean (SD) | 2.8 (1.8) | 3.0 (2.1) | 2.5 (1.5) | 0.840 2 |
| Respiratory analysis | ||||
| AHI [n/h], mean (SD) | 18.2 (20.0) | 17.8 (20.0) | 18.9 (21.2) | 0.904 2 |
| AHI [n/h], n (%) | ||||
| <5 | 5 (26.3) | 3 (27.3) | 2 (25.0) | |
| 5–14 | 5 (26.3) | 3 (27.3) | 2 (25.0) | |
| 15–29 | 6 (31.6) | 3 (27.3) | 3 (37.5) | |
| ≥30 | 3 (15.8) | 2 (18.2) | 1 (12.5) | |
| RDI [n/h], mean (SD) | 20.7 (20.3) | 21.8 (20.7) | 19.3 (21.1) | 0.778 2 |
| Obstructive apnea index [n/h], mean (SD) | 11.6 (19.3) | 11.2 (19.9) | 12.2 (19.9) | 0.840 2 |
| Mixed apnea index [n/h], mean (SD) | 0.8 (2.6) | 1.3 (3.4) | 0.09 (0.2) | 0.310 2 |
| Central apnea index [n/h], mean (SD) | 0.5 (1.5) | 0.8 (2.0) | 0.06 (0.1) | 0.442 2 |
| Snoring duration [min], mean (SD) | 27.7 (34.2) | 19.34 (21.0) | 39.3 (46.0) | 0.657 2 |
| Oxygen saturation | ||||
| Desaturation index [n/h], mean (SD) | 12.0 (18.7) | 11.4 (19.7) | 12.8 (18.4) | 0.657 2 |
| Minimum SpO2 [%], mean (SD) | 82.5 (7.9) | 83.1 (8.5) | 81.6 (7.5) | 0.702 1 |
| Mean SpO2 [%], mean (SD) | 94.7 (2.4) | 94.6 (2.7) | 95.0 (2.1) | 0.717 2 |
| Sleep position | ||||
| Sleep position [%TST], mean (SD) | ||||
| Supine position | 63.5 (30.8) | 62.7 (35.1) | 64.6 (26.0) | 0.968 2 |
| Non-supine position | 36.5 (30.8) | 37.4 (35.1) | 35.4 (26.0) | 0.968 2 |
| RDI [%TST], mean (SD) | ||||
| in supine position | 29.4 (26.7) | 30.1 (26.5) | 28.6 (28.7) | 0.904 2 |
| in non-supine position | 5.7 (8.2) | 5.6 (9.9) | 5.8 (5.6) | 0.310 2 |
| AHI Severity, n (%) | AHI ≥ 5 | AHI ≥ 15 | AHI ≥ 30 | AHI ≥ 5 + ESS > 10 1 |
|---|---|---|---|---|
| 14 (73.7) | 9 (47.4) | 3 (15.8) | 3 (16.7) |
| Seafarers (Males, n = 19) | Reference Parameters 1 (Males) | p-Value 2 | |
|---|---|---|---|
| Mean (95% CI) | Mean (95% CI) | ||
| TST [min] | 323.2 (280.0–366.3) | 374.6 (357.3–392.0) | 0.022 |
| SE [%] | 81.9 (77.0–86.9) | 84.3 (82.0–86.6) | 0.329 |
| WASO [min] | 38.2 (27.8–48.6) | 51.8 (42.1–61.4) | 0.013 |
| Sleep onset latency (SOL) [min] | 20.9 (8.0–33.9) | 14.7 (13.0–16.4) | 0.324 |
| REM latency [min] | 112.9 (84.3–141.5) | 92.5 (85.8–99.2) | 0.152 |
| Arousal index [n/h] | 29.4 (20.4–38.4) | 14.5 (12.6–16.5) | 0.003 |
| AHI [n/h] | 18.2 (8.6–27.9) | 5.2 (4.2–6.1) | 0.011 |
| Mean SpO2 [%] | 94.7 (93.6–95.9) | 94.7 (94.3–95.1) | 0.947 |
| Minimum SpO2 [%] | 82.5 (78.7–86.3) | 87.9 (86.6–89.2) | 0.008 |
| PLMS index [n/h] | 4.0 (0.5–7.8) | 2.1 (1.3–3.0) | 0.266 |
| (a) | |||||||
| AHI | RDI | #Wake Resp. Index | Obstr. Apnea Index | TIB | TST | Supine Position | |
| Age | r = 0.537 p = 0.018 | r = 0.504 p = 0.028 | r = 0.481 p = 0.037 | r = 0.474 p = 0.040 | r = 0.542 p = 0.016 | r = 0.489 p = 0.034 | r = 0.002 p = 0.994 |
| Seafaring experience (in years) | r = 0.509 p = 0.026 | r = 0.515 p = 0.024 | r = 0.508 p = 0.026 | r = 0.480 p = 0.037 | r = 0.537 p = 0.018 | r = 0.536 p = 0.018 | r = −0.124 p = 0.614 |
| Length of stay on board | r = 0.191 p = 0.433 | r = 0.181 p = 0.459 | r = 0.128 p = 0.600 | r = 0.126 p = 0.608 | r = −0.520 p = 0.022 | r = −0.443 p = 0.058 | r = 0.639 p = 0.003 |
| (b) | |||||||
| ESS | rPUI | ||||||
| Age | r = −0.078 p = 0.757 | r = −0.333 p = 0.381 | |||||
| Seafaring experience (in years) | r = −0.233 p = 0.352 | r = −0.238 p = 0.537 | |||||
| Length of stay on board | r = 0.156 p = 0.536 | r = 0.323 p = 0.397 | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kerkamm, F.; Dengler, D.; Eichler, M.; Materzok-Köppen, D.; Belz, L.; Neumann, F.A.; Zyriax, B.-C.; Harth, V.; Oldenburg, M. Sleep Architecture and Sleep-Related Breathing Disorders of Seafarers on Board Merchant Ships: A Polysomnographic Pilot Field Study on the High Seas. Int. J. Environ. Res. Public Health 2023, 20, 3168. https://doi.org/10.3390/ijerph20043168
Kerkamm F, Dengler D, Eichler M, Materzok-Köppen D, Belz L, Neumann FA, Zyriax B-C, Harth V, Oldenburg M. Sleep Architecture and Sleep-Related Breathing Disorders of Seafarers on Board Merchant Ships: A Polysomnographic Pilot Field Study on the High Seas. International Journal of Environmental Research and Public Health. 2023; 20(4):3168. https://doi.org/10.3390/ijerph20043168
Chicago/Turabian StyleKerkamm, Fiona, Dorothee Dengler, Matthias Eichler, Danuta Materzok-Köppen, Lukas Belz, Felix Alexander Neumann, Birgit-Christiane Zyriax, Volker Harth, and Marcus Oldenburg. 2023. "Sleep Architecture and Sleep-Related Breathing Disorders of Seafarers on Board Merchant Ships: A Polysomnographic Pilot Field Study on the High Seas" International Journal of Environmental Research and Public Health 20, no. 4: 3168. https://doi.org/10.3390/ijerph20043168
APA StyleKerkamm, F., Dengler, D., Eichler, M., Materzok-Köppen, D., Belz, L., Neumann, F. A., Zyriax, B.-C., Harth, V., & Oldenburg, M. (2023). Sleep Architecture and Sleep-Related Breathing Disorders of Seafarers on Board Merchant Ships: A Polysomnographic Pilot Field Study on the High Seas. International Journal of Environmental Research and Public Health, 20(4), 3168. https://doi.org/10.3390/ijerph20043168









