Utility of Telehealth Platforms Applied to Burns Management: A Systematic Review
Abstract
1. Introduction
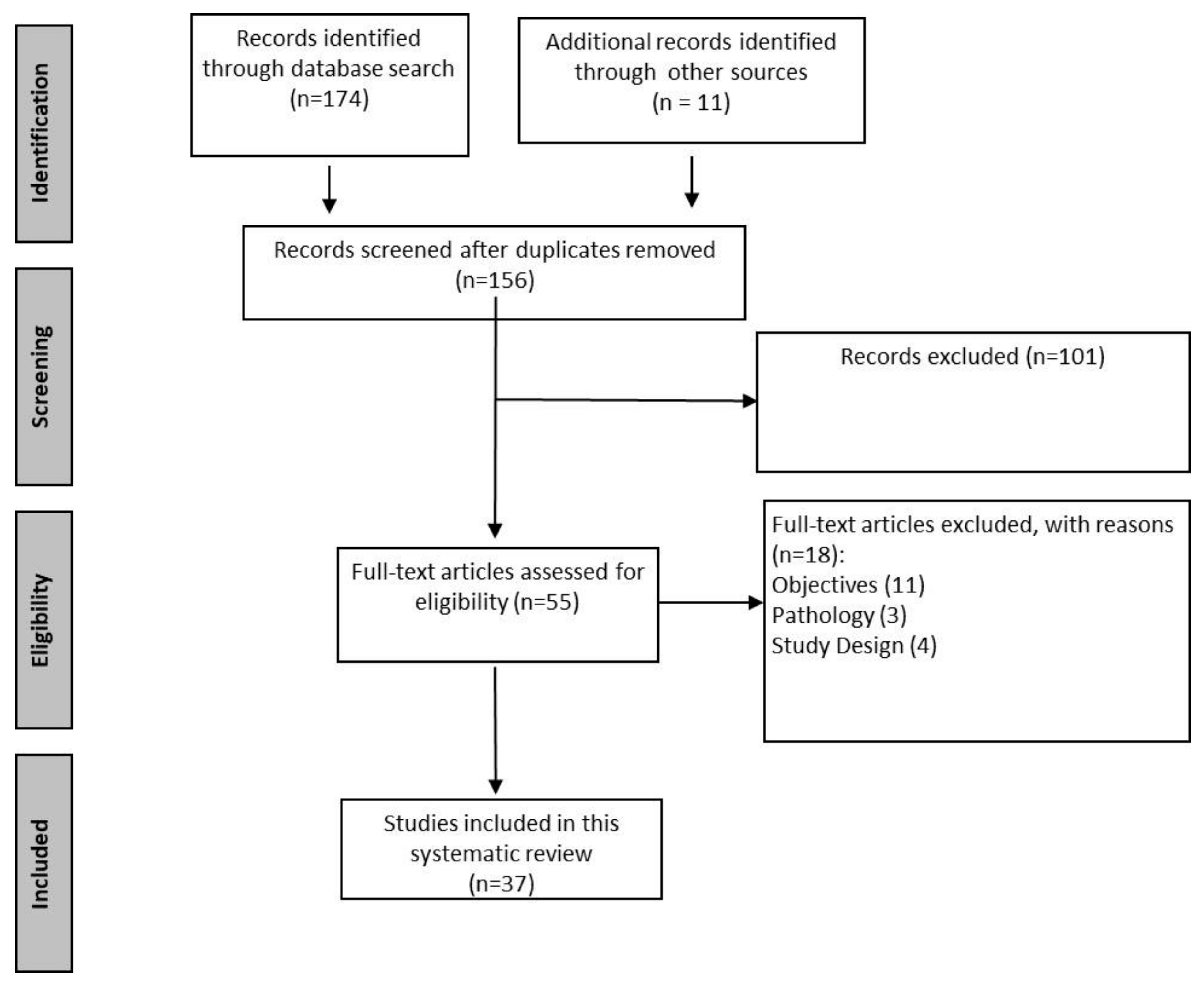
2. Materials and Methods
2.1. Search Strategy
2.2. Selection Criteria
2.3. Data Extraction
2.4. Synthesis
- P (population): patients requiring treatment of their burns with a high degree of specialisation, particularly in tertiary hospitals;
- I (intervention): TH;
- C (comparison): conventional treatment versus treatment using TH;
- O (outcomes): the cost-benefit impact of TH in burn patients, as well as the clinical effectiveness of implementing any TH strategy;
- S (study design): any.
3. Results
3.1. Clinical Results in the Management of Acute Burns
3.2. Clinical Results in the Follow-Up of Burn Patients
3.3. Results in Cost Evaluation
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Norris, A. Essentials of Telemedicine and Telecare; Wiley: Chichester, UK, 2001; ISBN 978-0-471-53151-7. [Google Scholar]
- Wallace, D.L.L.; Hussain, A.; Khan, N.; Wilson, Y.T.T. A Systematic Review of the Evidence for Telemedicine in Burn Care: With a UK Perspective. Burns 2012, 38, 465–480. [Google Scholar] [CrossRef] [PubMed]
- Butler, D.P. The 21st Century Burn Care Team. Burns 2013, 39, 375–379. [Google Scholar] [CrossRef] [PubMed]
- Kelly, J.; Nikkhah, D.; Wek, C.; Dheansa, B. Changing Management Models in Burn Care. Br. J. Healthc. Manag. 2013, 19, 585–589. [Google Scholar] [CrossRef]
- Blom, L.; Laflamme, L.; Alvesson, H.M. Expectations of Medical Specialists about Image-Based Teleconsultation—A Qualitative Study on Acute Burns in South Africa. PLoS ONE 2018, 13, e0194278. [Google Scholar] [CrossRef]
- Ajami, S.; Arzani-Birgani, A. Fast Resuscitation and Care of the Burn Patients by Telemedicine: A Review. J. Res. Med. Sci. 2014, 19, 562–566. [Google Scholar]
- Lewis, E.R.; Thomas, C.A.; Wilson, M.L.; Mbarika, V.W.A. Telemedicine in Acute-Phase Injury Management: A Review of Practice and Advancements. Telemed. e-Health 2012, 18, 434–445. [Google Scholar] [CrossRef]
- Wallace, D.L.L.; Jones, S.M.M.; Milroy, C.; Pickford, M.A.A. Telemedicine for Acute Plastic Surgical Trauma and Burns. J. Plast. Reconstr. Aesthet. Surg. 2008, 61, 31–36. [Google Scholar] [CrossRef]
- Mock, C.; Peck, M.; Krug, E.; Haberal, M. Confronting the Global Burden of Burns: A WHO Plan and a Challenge. Burns 2009, 35, 615–617. [Google Scholar] [CrossRef]
- World Health Organization. Fact Sheet about Burns. Available online: https://www.who.int/news-room/fact-sheets/detail/burns (accessed on 1 September 2022).
- Paul, M.A.; Kamali, P.; Ibrahim, A.M.S.; Medin, C.; Lee, B.T.; Lin, S.J. Initial Assessment, Treatment, and Follow-Up of Minor Pediatric Burn Wounds in Four Patients Remotely: A Preliminary Communication. Telemed. J. E. Health. 2018, 24, 379–385. [Google Scholar] [CrossRef]
- Cai, L.Z.; Caceres, M.; Dangol, M.K.; Nakarmi, K.; Rai, S.M.; Chang, J.; Gibran, N.S.; Pham, T.N. Accuracy of Remote Burn Scar Evaluation via Live Video-Conferencing Technology. Burns 2016, 16, 4–11. [Google Scholar] [CrossRef]
- Urrutia, G.; Bonfill, X. Declaración PRISMA: Una Propuesta Para Mejorar La Publicación de Revisiones Sistemáticas y Metaanálisis. Med. Clin. Barc. 2010, 135, 507–511. [Google Scholar] [CrossRef]
- Goldet, G.; Howick, J. Understanding GRADE: An Introduction. J. Evid. Based. Med. 2013, 6, 50–54. [Google Scholar] [CrossRef]
- Saffle, J.R.; Edelman, L.; Theurer, L.; Morris, S.E.; Cochran, A. Telemedicine Evaluation of Acute Burns Is Accurate and Cost-Effective. J. Trauma—Inj. Infect. Crit. Care 2009, 67, 358–365. [Google Scholar] [CrossRef]
- Pham, C.; Collier, Z.; Gillenwater, J. Changing the Way We Think About Burn Size Estimation. J. Burn Care Res. 2018, 40, 1–11. [Google Scholar] [CrossRef]
- Burgess, J.; Watt, K.; Kimble, R.M.; Cameron, C.M. Combining Technology and Research to Prevent Scald Injuries (the Cool Runnings Intervention): Randomized Controlled Trial. J. Med. Internet Res. 2018, 20, e10361. [Google Scholar] [CrossRef]
- Wibbenmeyer, L.; Kluesner, K.; Wu, H.; Eid, A.; Heard, J.; Mann, B.; Pauley, A.; Peek-Asa, C. Video-Enhanced Telemedicine Improves the Care of Acutely Injured Burn Patients in a Rural State. J. Burn Care Res. 2016, 37, e531–e538. [Google Scholar] [CrossRef]
- Wallace, D.L.; Smith, R.W.; Pickford, M.A. A Cohort Study of Acute Plastic Surgery Trauma and Burn Referrals Using Telemedicine. J. Telemed. Telecare 2007, 13, 282–287. [Google Scholar] [CrossRef]
- Boccara, D.; Bekara, F.; Soussi, S.; Legrand, M.; Chaouat, M.; Mimoun, M.; Serror, K. Ongoing Development and Evaluation of a Method of Telemedicine: Burn Care Management with a Smartphone. J. Burn Care Res. 2018, 39, 580–584. [Google Scholar] [CrossRef]
- Saffle, J.R.; Edelman, L.; Morris, S.E. Regional Air Transport of Burn Patients: A Case for Telemedicine? J. Trauma—Inj. Infect. Crit. Care 2004, 57, 57–64. [Google Scholar] [CrossRef]
- Mohr, N.M.; Harland, K.K.; Chrischilles, E.A.; Bell, A.; Shane, D.M.; Ward, M.M. Emergency Department Telemedicine Is Used for More Severely Injured Rural Trauma Patients, but Does Not Decrease Transfer: A Cohort Study. Acad. Emerg. Med. 2017, 24, 177–185. [Google Scholar] [CrossRef]
- Hop, M.J.; Moues, C.M.; Bogomolova, K.; Nieuwenhuis, M.K.; Oen, I.M.M.H.; Middelkoop, E.; Breederveld, R.S.; Van Baar, M.E. Photographic Assessment of Burn Size and Depth: Reliability and Validity. J. Wound Care 2014, 23, 144–152. [Google Scholar] [CrossRef] [PubMed]
- Shokrollahi, K.; Sayed, M.; Dickson, W.; Potokar, T. Mobile Phones for the Assessment of Burns: We Have the Technology. Emerg. Med. J. 2007, 24, 753–755. [Google Scholar] [CrossRef] [PubMed]
- Parvizi, D.; Giretzlehner, M.; Dirnberger, J.; Owen, R.; Haller, H.L.; Schintler, M.V.; Wurzer, P.; Lumenta, D.B.; Kamolz, L.P. The Use of Telemedicine in Burn Care: Development of a Mobile System for TBSA Documentation and Remote Assessment. Ann. Burn. Fire Disasters 2014, 27, 94–100. [Google Scholar]
- Kiser, M.; Beijer, G.; Mjuweni, S.; Muyco, A.; Cairns, B.; Charles, A. Photographic Assessment of Burn Wounds: A Simple Strategy in a Resource-Poor Setting. Burns 2013, 39, 155–161. [Google Scholar] [CrossRef]
- Smith, A.C.; Scuffham, P.; Wootton, R. The Costs and Potential Savings of a Novel Telepaediatric Service in Queensland. BMC Health Serv. Res. 2007, 7, 35. [Google Scholar] [CrossRef]
- Gacto-Sánchez, P.; Molina-Morales, J.; Rodríguez-Vela, F.; Moreno-Conde, J.; Sendin-Martin, M.; Parra-Calderon, C.; Gomez-Cía, T.; Pereyra-Rodriguez, J.J. Diagnostic Accuracy of a Telemedicine Tool for Acute Burns Diagnosis. Burns 2020, 46, 1799–1804. [Google Scholar] [CrossRef]
- Basaran, A.; Ozlu, O.; Das, K. Telemedicine in Burn Patients: Reliability and Patient Preference. Burns 2021, 47, 1873–1877. [Google Scholar] [CrossRef]
- Garber, R.N.; Garcia, E.; Goodwin, C.W.; Deeter, L.A. Pictures Do Influence the Decision to Transfer: Outcomes of a Telemedicine Program Serving an Eight-State Rural Population. J. Burn Care Res. Off. Publ. Am. Burn Assoc. 2020, 41, 690–694. [Google Scholar] [CrossRef]
- Carmichael, H.; Dyamenahalli, K.; Duffy, P.S.; Lambert Wagner, A.; Wiktor, A.J. Triage and Transfer to a Regional Burn Center-Impact of a Mobile Phone App. J. Burn Care Res. Off. Publ. Am. Burn Assoc. 2020, 41, 971–975. [Google Scholar] [CrossRef]
- Liu, Y.M.; Mathews, K.; Vardanian, A.; Bozkurt, T.; Schneider, J.C.; Hefner, J.; Schulz, J.T.; Fagan, S.P.; Goverman, J. Urban Telemedicine: The Applicability of Teleburns in the Rehabilitative Phase. J. Burn Care Res. 2017, 38, e235–e239. [Google Scholar] [CrossRef]
- Hickey, S.; Gomez, J.; Meller, B.; Schneider, J.C.; Cheney, M.; Nejad, S.; Schulz, J.; Goverman, J. Interactive Home Telehealth and Burns: A Pilot Study. Burns 2017, 43, 1318–1321. [Google Scholar] [CrossRef]
- Garcia, D.I.; Howard, H.R.; Cina, R.A.; Patel, S.; Ruggiero, K.; Treiber, F.A.; Lesher, A.P. Expert Outpatient Burn Care in the Home through Mobile Health Technology Denise. J. Burn Care Res. 2018, 39, 680–684. [Google Scholar] [CrossRef]
- Nguyen, L.T.; Massman, N.J.; Franzen, B.J.; Ahrenholz, D.H.; Sorensen, N.W.; Mohr, W.J.; Solem, L.D. Telemedicine Follow-up of Burns: Lessons Learned from the First Thousand Visits. J. Burn Care Rehabil. 2004, 25, 485–490. [Google Scholar] [CrossRef]
- Redlick, F.; Roston, B.; Gomez, M.; Fish, J.S. An Initial Experience with Telemedicine in Follow-up Burn Care. J. Burn Care Rehabil. 2002, 23, 110–115. [Google Scholar] [CrossRef]
- Smith, A.C.; Kimble, R.; Mill, J.; Bailey, D.; O’Rourke, P.; Wootton, R. Diagnostic Accuracy of and Patient Satisfaction with Telemedicine for the Follow-up of Paediatric Burns Patients. J. Telemed. Telecare 2004, 10, 193–198. [Google Scholar] [CrossRef]
- Vyas, K.S.; Hambrick, H.R.; Shakir, A.; Morrison, S.D.; Tran, D.C.; Pearson, K.; Vasconez, H.C.; Mardini, S.; Gosman, A.A.; Dobke, M.; et al. A Systematic Review of the Use of Telemedicine in Plastic and Reconstructive Surgery and Dermatology. Ann. Plast. Surg. 2017, 78, 681–736. [Google Scholar] [CrossRef]
- Hoseini, F.; Ayatollahi, H.; Salehi, S.H. A Systematized Review of Telemedicine Applications in Treating Burn Patients. Med. J. Islam. Repub. Iran 2016, 30, 459. [Google Scholar]
- Wiktor, A.J.; Madsen, L.; Carmichael, H.; Smith, T.; Zanyk, S.; Amani, H.; Wagner, A.L. Multiregional Utilization of a Mobile Device App for Triage and Transfer of Burn Patients. J. Burn Care Res. 2018, 39, 858–862. [Google Scholar] [CrossRef]
- Martinez, R.; Rogers, A.D.; Numanoglu, A.; Rode, H. The Value of WhatsApp Communication in Paediatric Burn Care. Burns 2018, 44, 947–955. [Google Scholar] [CrossRef]
- Russell, K.W.; Saffle, J.R.; Theurer, L.; Cochran, A.L. Transition from Grant Funding to a Self-Supporting Burn Telemedicine Program in the Western United States. Am. J. Surg. 2015, 210, 1037–1044. [Google Scholar] [CrossRef]
- Turk, E.; Karagulle, E.; Aydogan, C.; Oguz, H.; Tarim, A.; Karakayali, H.; Haberal, M. Use of Telemedicine and Telephone Consultation in Decision-Making and Follow-up of Burn Patients: Initial Experience from Two Burn Units. Burns 2011, 37, 415–419. [Google Scholar] [CrossRef] [PubMed]
- McWilliams, T.; Hendricks, J.; Twigg, D.; Wood, F.; Giles, M. Telehealth for Paediatric Burn Patients in Rural Areas: A Retrospective Audit of Activity and Cost Savings. Burns 2016, 42, 1487–1493. [Google Scholar] [CrossRef] [PubMed]
- Head, W.T.; Garcia, D.; Mukherjee, R.; Kahn, S.; Lesher, A. Virtual Visits for Outpatient Burn Care During the COVID-19 Pandemic. J. Burn Care Res. Off. Publ. Am. Burn Assoc. 2022, 43, 300–305. [Google Scholar] [CrossRef] [PubMed]
- Smith, A.C.; Kimble, R.M.; O’Brien, A.; Mill, J.; Wootton, R. A Telepaediatric Burns Service and the Potential Travel Savings for Families Living in Regional Australia. J. Telemed. Telecare 2007, 13, 76–79. [Google Scholar] [CrossRef]
- Hasselberg, M.; Wallis, L.; Blessing, P.; Laflamme, L. A Smartphone-Based Consultation System for Acute Burns—Methodological Challenges Related to Follow-up of the System. Glob. Health Action 2017, 10, 1328168. [Google Scholar] [CrossRef]
- Thomas, E.E.; Haydon, H.M.; Mehrotra, A.; Caffery, L.J.; Snoswell, C.L.; Banbury, A.; Smith, A.C. Building on the Momentum: Sustaining Telehealth beyond COVID-19. J. Telemed. Telecare 2022, 28, 301–308. [Google Scholar] [CrossRef]
- Saigí-Rubió, F.; Borges do Nascimento, I.J.; Robles, N.; Ivanovska, K.; Katz, C.; Azzopardi-Muscat, N.; Novillo Ortiz, D. The Current Status of Telemedicine Technology Use Across the World Health Organization European Region: An Overview of Systematic Reviews. J. Med. Internet Res. 2022, 24, e40877. [Google Scholar] [CrossRef]
| Study Type | Patient Intervention | Clinical Results | Cost Evaluation | GRADE | |
|---|---|---|---|---|---|
| MANAGEMENT OF ACUTE BURNS | |||||
| Ajami et al. (2014) Iran [6] | Systematic review | A review of 30 articles on fast resuscitation and care of burn patients using TH (from 1999 to 2012). | TH proves to be adequate and effective for acute emergency management (rapid resuscitation and patient care), preventing the burn from progressing and becoming infected, and plays a relevant role in improving access to the required experience, increasing professional confidence. It is a useful tool in triage and planning for the treatment of patients. | It can reduce excessive triage for air or ground transportation, saving time and costs. For patients with major burns, TH helped accelerate the preparation of appropriate critical care and justified the costs and risks of air travel. Patients with minor burns were quickly identified for inexpensive ground transportation. | A |
| Pham et al. (2018) USA [16] | Systematic review | A review of 26 articles analysing burn size estimation (TBSA) (from 1982 to 2017). | Up to 77% of burn victims inappropriately transferred to burn centres from referring hospitals caused by improper use of TBSA. Few studies with limited sample sizes argue that TBSA misestimations significantly affect fluid resuscitation volume; although, the findings suggest that small burns (<20% TBSA) are overestimated and overresuscitated—the opposite of larger burns. | TBSA misestimation is associated with an increased incidence of inappropriate transfers to burn centres and the associated costs. The results suggest that TH could reduce referrals subject to TBSA modification errors, thereby reducing unnecessary costs. | A |
| Lewis et al. (2012) USA [7] | Systematic review | A review of 31 articles in the emerging field of TH in the management of acute-phase injuries (6 of them related to burn injuries) (from 2004 to 2010). | Focusing on the acute context, mHealth tools provide useful and beneficial plugins for clinical decision-making and support reductions in mortality and morbidity. Especially in rural and resource-poor areas, TH supports better health outcomes and better quality of care. | Although the results of these integrative modalities demonstrated high sensitivity and specificity, high reliability, simplicity, and cost-effectiveness, there are still barriers to the use of TH that limit its wider adoption. The limitations of its adoption include poor infrastructure, limited availability of equipment, and insufficient access to professional training and education. | A |
| Burgess et al. (2018) Australia [17] | 2-group, parallel, single-blinded RCT | “Cool Runnings” app intervention for improving knowledge about risks of hot beverage scalds and of burn first aid in mothers of young children. Participants were women aged 18 years and above with at least one child aged 5–12 months at time of enrolment. In total, 498 participants were recruited via social media and enrolled. At the 6-month follow-up, 244 participants completed the post-test questionnaire. | Intervention group participants achieved significantly greater improvement in overall knowledge post-test than control group participants on both primary outcome measures. These results show that only eight people needed to be exposed to this intervention to improve inadequate overall knowledge to adequate knowledge in one additional person. Participants who remained in the study demonstrated a higher level of education. | Given the low cost and large reach of smartphone apps to deliver content to and engage with targeted populations, smartphone apps can be used for widespread injury prevention campaigns and public health campaigns generally. However, it is important to acknowledge that a change in knowledge does not necessarily reflect a change in behaviour. | B |
| Wibbenmeyer et al. (2016) USA [18] | Cohort study. Multicentre | Implementation of the addition of video-enhanced TH to the current telephone burn transfer programme in a rural state. Over a 2-year period (2012–2014), 282 patients were enrolled in the study, (59.4% of all burn patients transferred from outside hospitals). | The referring staff was correct in their burn assessment 20% of the time. Video assessment improved the ChargeRN BSA burned and resulted in more accurate fluid resuscitation (p = 0.03), changes in both transportation mode (p = 0.042), and disposition decisions (p = 0.2). The majority of the referring staff found that video-enhanced TH helped them communicate with the burn staff more effectively (3.4 ± 0.37, scale 1–4). This study reports the successful implementation of a video-enhanced TH pilot project in a rural state. | Non-quantitative study. The low cost of the system, coupled with changes in disposition and transportation suggest a significant decrease in healthcare costs associated with the addition of video to a telephone-only transfer programme. | C |
| Saffle et al. (2009) USA [15] | Cohort study. Multicentre | During the TELE period (from 2005 to 2007), 80 patients were referred, of whom 70 were seen acutely by TH, compared with 28 referrals before instituting TH (PRE-TELE). | Only 31 patients seen by TH received emergency air transport (44.3%), compared with 100% of PRE-TELE patients (p < 0.05). TELE patients transported by air had somewhat larger burn sizes (9.0% vs. 6.5% TBSA; p = NS) and longer lengths of stay (13.0 days vs. 8.0 days; p = NS) than PRE-TELE patients. It demonstrated an improved triage accuracy with face-to-face equivalent TH assessment and proved significantly better than referring clinicians. | TH assessment helped accelerate the provision of appropriate critical care for severely burned patients and justify the expense and risks of air travel. Patients with minor burns were either quickly identified for inexpensive ground transportation or received definitive local care at great cost savings, all without an apparent increase in misclassification. | C |
| Wallace et al. (2007) UK [19] | Cohort study. Multicentre | During a 12-week prospective study, 11 units with the TH system and 10 units without it regularly made referrals to the Queen Victoria Hospital (QVH). There were 389 referrals from the TH-equipped units and 607 telephone referrals from the non-TH units. | The TH system was used for 246 of the 389 referrals (63%) made from TH-equipped units. It did not document burn size estimation and no clinical outcomes were reported; although, subgroup analysis showed a significantly improved accuracy of triage for minor burns. | No cost savings analysis. | C |
| Boccara et al. (2017) France [20] | Retrospective study | This retrospective study included 323 patients who were initially assessed by digital images via smartphone, implemented between 2011 and 2016. This procedure only involved patients burned in a small portion of the body surface (i.e., ≤15%), between 15 and 75 years old, and who did not present significant comorbidity. | The initial diagnosis regarding the need for a surgical procedure was accurate in 94.4% (305/323) of the cases. Eleven patients (3.4%) were transferred unnecessarily as they ultimately did not require surgery, and seven patients (2.2%) were ultimately transferred even though the need for surgery was not initially established at the time that the images were viewed. The overall error rate was 5.6% (18/323). This could equally be a result of burn progression rather than incorrect evaluation of the initial image. The delay in treatment did not adversely affect life-threatening, functional, or aesthetic prognoses. | Out of the 222 patients not hospitalised on an emergency basis, only seven ultimately underwent surgery for a straightforward excision–skin graft. This low error rate (3.2%) and the lack of observed injury supported the development of photograph-based opinions. The cost savings and the freeing-up of the burn centre resources were very substantial during this period, thanks to this TH system. | D |
| Saffle et al. (2004) USA [21] | Retrospective study | In total, 225 acutely burned patients from 2000 to 2001 who were transported to the facility by air from referring hospitals in nine states. They wanted to study whether TH evaluation before transport could have significantly altered initial treatment decisions. | Out of the 225 patients, only 60% were classified as air-transport appropriate. The mean burn size calculated by burn centre physicians was 19.7% TBSA, whereas that calculated by referring physicians was 29%. In 92 cases, over- or underestimation of burn size by referring physicians was as much as 560%. TH evaluation before transport might have significantly altered transport decisions or care. | Some patients obviously met more than one of these criteria. The TH group had shorter lengths of hospital stay than the other patients (13.5 ± 2 days vs. 24.2 ± 3 days, p < 0.05) and, correspondingly, lower hospital charges. Air transport charges exceeded hospital charges in 21 cases. | D |
| Mohr et al. (2017) USA [22] | Cohort study | In total, 2837 patients were treated to describe patient-level factors associated with TH consultation in an emergency department (ED) and to measure the association between TH consultation and interhospital transfer from 2008 to 2014. | No differences were observed in clinical outcomes. TH was consulted for 11% of all trauma patients in TH-capable EDs. Factors associated with TH consultation included a higher Injury Severity Score. Adjusting for the severity of illness, injury mechanism, and type of injury, TH use was not associated with interhospital transfer (adjusted odds ratio = 1.28, 95% confidence interval = 0.94 to 1.75). | No cost analysis. | C |
| Wallace et al. (2008) UK [8] | Cohort study | Study conducted in different phases. (1) Ten-week retrospective evaluation of the TH system with 973 referrals from 53 different sites. (2) Twelve-week prospective cohort study to investigate changes in patient management from TH-assisted referrals compared to telephone-only referrals. In total, 996 referrals were received from over 60 different sites. | (1) In total, 452 patients were referred from the sites with TH, and TH was used for 42% of these patients. Referring clinicians were pleased with the TH system, finding it easy to use and helpful in the referral process. They also expressed an improvement in the clarity of information. (2) Of 389 referrals, the TH system was used for 243 (63%). A significant difference was noted in the management of patients with and without the availability of TH. Significantly fewer patients needed to come for further assessment and more patients could be directly booked for definitive care in a Day Surgery Unit (10.5%). A decrease in the number of occasions when the QVH was unable to accept a referral due to a lack of capacity was observed compared to telephone advice only. | The authors found no evidence of cost savings for the QVH trust and only anecdotal patient cost savings. The capital outlay was significant (£70,000) for the installation of the computer network lines, equipment, and software. | C |
| Hop et al. (2014) The Netherlands [23] | Cohort study | This study examined the reliability and validity of using 50 randomly selected photographs taken on day 0–1 post-burn by seven burn experts and eight referring physicians to assess both burn size and depth from one general hospital. | Experts (ICCs of 0.83 and 0.87), but not referring physicians (ICCs of 0.68 and 0.78), could assess burn size from photographs both reliably and validly. Neither experts (0.38 and 0.28) nor referring physicians (0.24 and 0.13) could assess burn depth either reliably or validly, or the indication for surgery. The agreement between assessors regarding referral indication was low. | No cost analysis. Future research should also address the actual impact and cost-effectiveness of the introduction of TH, e.g., the prevention of unnecessary referrals, in a clinical trial. | C |
| Cai et al. (2016) Nepal/USA [12] | Cohort study | A prospective study conducted with 17 individuals with healed burn scars in Nepal. Three independent observers (one physically present and two remote observers in the United States) assessed 85 burn scars to test the reliability of the Patient and Observer Scar Assessment Scale (POSAS) using live videoconferencing. | The single-rater reliability of the POSAS was acceptable (ICC > 0.70) in overall opinion, thickness, pliability, and surface area. The average rater reliability for three observers was acceptable (ICC > 0.70) for all parameters except for vascularity. When comparing patients’ and observers’ overall opinion scores, the patients’ scores were consistently worse. | No cost analysis. This study demonstrated that an off-the-shelf camera smartphone is sufficient to transmit a reliable video-feed of burn scars from Nepal to the US. Videoconferencing offers an acceptable low-cost solution applicable to most resource-limited healthcare environments. | D |
| Shokrollahi et al. (2007) UK [24] | Case-control | An investigation into the accuracy of assessment of TBSA and depth in 31 patients with minor burns using a basic camera-equipped mobile phone, assessed at the Welsh Centre for Burns and Plastic Surgery. | It demonstrated a good correlation of burn size (correlation coefficient r = 0.91) estimation, though only for small burn sizes (<5%TBSA (mean 1.2%)). Using the images, assessors could reliably differentiate full-thickness burns from partial-thickness burns in almost all cases (94%, n = 29). | No cost analysis. Within minutes, an emergency department was able to transmit accurate images to the centre, enabling good decisions to be made related to the appropriateness of transfer, interim dressings, and fluid resuscitation, with profound implications for the quality of patient care as well as cost. | D |
| Parvizi et al. (2014) Austria [25] | Cross-sectional study | At two international burn meetings, a survey containing three pictures of burn patients was conducted. Eighty specialists were asked to give a burn extent estimation. The same burn pictures were transferred to a computer system and the TBSA in % was calculated by the BurnCase 3D software and the estimations were compared. | The majority of respondents were specialists (32), residents (27), and nursing staff (21). The preferred methods for burn extent estimation were the Rule of Nines (38%), the Rule of Palm (37%), and the Lund-Browder chart (18%). The analysis showed very high deviations of TBSA across the participants, even in the group of experts. In comparison to a computer-aided method, the authors found a massive overestimation of up to 230%. | No cost analysis. BurnCase 3D brought an objective extent estimation that could have a true impact on the quality of treatment in burns. In acute burn care, TH had great potential to help guide decisions regarding triage and transfer based on TBSA, burn depth, patient age, and injury mechanism. | D |
| Kiser et al. (2013) Malawi/USA [26] | Cohort study | In the burn unit at Kamuzu Central Hospital (KCH), Malawi, 39 burn patients (50 wounds) were clinically assisted and also photographed by an experienced clinician over a 2-month period in 2011. Then, these photographs were reviewed by two blinded burn clinicians after 4–6 weeks. The correlation between clinical assessment and photographic evaluation was calculated using the Kappa score and Pearson’s correlation coefficient. | Pearson’s correlation coefficients for TBSA agreement between clinical examination and photograph review by experts 1 and 2 were 0.96 and 0.93 (p < 0.001), respectively. Pearson’s correlation coefficients comparing experts 1 and 2 to the gold standard were the proportion of full-thickness burn (0.88 and 0.81, p < 0.001), and epithelialised superficial burn (0.89 and 0.55, p < 0.001). Kappa scores were significant for wound evolution (0.57 and 0.64, p < 0.001), and prognosis (0.80 and 0.80, p < 0.001). | No cost analysis. Burn assessment with digital photography was a valid and affordable alternative to direct clinical examination, alleviating access issues to burn care in developing countries. | C |
| Smith et al. (2007) Australia [27] | Case-control | Over a 5-year period, a novel telepaediatric service (videoconferencing) was set up for selected regional hospitals in Queensland. In total, 1499 consultations were conducted for a broad range of paediatric subspecialities including burns. | No clinical results | Total cost of providing 1499 consultations was AUD 955,996, but the estimated cost without this service at the hospital was AUD 1,553,264; thus, telepaediatric services resulted in a net saving of approximately AUD 600,000 to the health service provider. TM was cheaper than conventional outpatient service after 774 consultations. The state reimburses the patients’ travel expenses. | D |
| Gacto-Sánchez et al. (2020) Spain [28] | Cross-sectional study | Diagnostic test validation study made by TH (through an App designed for this project) to 202 patients with acute burns between July 1 and 23 October 2018. | All images were valid for diagnosis. Quality evaluation was “very good” (52%) and good (43%). The intra-observer concordance was k = 0.94 (95% CI: 0.90 0.97). Interobserver concordance: k = 0.95 (95% CI: 0.910.99). The results highlight a very high sensitivity (99.40%) and specificity (100%). | The TH detected that 83.17% of the patients attending the BU could have been managed on as outpatient basis. 49.44 min for tele-response report (95% CI 45.89-52.67; range 2-138) vs. 243.60 min to assist the patient at the BU (95% CI 224.05-266.75; range 19-1620). The study optimizes the use of resources (urgency consultations, medicalized transportation) (non-data presented). | D |
| Basaran et al. (2020) Turkey [29] | Cross-sectional study | Study of reliability of TH assessment of burn patients and preference of patients to use TH. | TH examination resulted in an agreement in terms of burn depth, decision of hospitalisation, and a high concordance for TBSA evaluation between face-to-face examination and TH group. | Although WhatsApp is a reliable method, the majority of patients preferred a face-to-face follow-up. | D |
| Garber et al. (2020) USA [30] | Cross-sectional study | 155 burn patients from rural areas were referred by telephone to provide initial triage and the need or not to transfer to the reference hospital, compared to the decision based solely on the telephone conversation. | In total, 24.5% of patient images changed the initial decision transfer, and 75.5% confirmed the initial care plan. Of the cases that required a change of plan, 60.5% were they went down to outpatient care, and 39.5% went up to transfer. | They saved between USD 150,000 to USD 180,000 in air freight costs alone. The authors do not calculate the additional cost of hospitalisation that the patient would have incurred. | D |
| Carmichael-et al. (2020) USA [31] | Retrospective study | To assess the efficacy of a mobile app in the triage decisions of burn patients. | The Burn mobile app can be used to improve triage decisions in patients with intermediate-size burns measuring 1–10% TBSA. The Burn mobile app can be used in a HIPPA-compliant manner. | The cost savings to the system and patients were estimated to be nearly USD 100 per patient. | D |
| FOLLOW-UP OF BURN PATIENTS | |||||
| Liu et al. (2017) USA [32] | Retrospective study | A retrospective review was performed on 29 patients enrolled in 73 virtual visits through the TH/rehabilitation programme between 2013 and 2014. | Videoconferencing between a burn centre and rehabilitation hospital streamlined patient care and reduced healthcare costs, while maintaining quality of care and patient satisfaction. | Total savings of USD 101,110 in transportation costs were achieved by eliminating 146 ambulance transfers. The reduced time of virtual visits resulted in savings of 6.8 days in outpatient management. Early discharge was facilitated, and savings of 80 bed days were estimated. The rehabilitation hospital saved an average of 2.5 days by eliminating travel. No unplanned readmissions from the rehabilitation hospital to the burn hospital were observed during the study. The patient satisfaction surveys showed 100% satisfaction, especially related to the trips saved. The rehabilitation centre had reduced interruptions, thereby improving its efficiency. | D |
| Hickey et al. (2017) USA [33] | Retrospective study | A review of 31 burn patients participating in Interactive Home Telehealth (IHT) visits for follow-up burn care using videoconferencing over the course of 15 months (from 2015 to 2016). | There were no unplanned readmissions and no complications. Of 31 total patients, burn surgeons treated 26, physiatrists treated 4, and psychiatrists treated 6, with a mean length of time for the IHT consultation of 10.8 min, 17.2 min, and 30 min, respectively. Of the 34 encounters with burn surgeons, 23 (67.7%) were supplemented with high-resolution images. | The average roundtrip travel distance saved was 188 miles (range 4–822 miles). The average roundtrip travel time saved was 201 min (range 20–564 min). Five connectivity issues were reported, none of which prevented the completion of the visit. | D |
| Garcia et al. (2018) USA [34] | Case-control | The authors retrospectively reviewed clinical outcomes and usability in paediatric partial thickness burn patients treated using the TeleBurn App (32) through text and image messaging, videoconferencing, and instructional videos, compared to standard therapy alone (35), between 2016 and 2017. | Most of the patients (74%) who were offered the app used it as their primary source of follow-up care. This group had no wound infections or unexpected returns to a clinic or hospital. Both the TeleBurn App and standard therapy groups had similar burn severity, age, and burn mechanism. Mean healing time was shorter in the app group (11.6 ± 4.7 days) vs. standard therapy (14.3 ± 5.4 (p = 0.03)) with fewer clinical encounters (0.93 ± 0.6) vs. standard therapy (3.3 ± 1.0 (p = 0.001)). Adherence to completion of therapy in patients using the app was 80% vs. 64% with standard therapy. | No cost analysis. While understudied, the cost of distributing and licencing an app-based care model would likely be significantly lower than the cost of former TH hub-and-spoke models used in burn care. | D |
| Nguyen et al. (2004) USA [35] | Cohort study | Evaluation of 1000 burn follow-up visits with 294 patients via TH over a 5-year period to identify the barriers and benefits specific to burn care. Travel costs and financial data were evaluated. | No clinical outcome analysed. Psychology, therapy, and surgical care were delivered during the virtual visits. Subjective improvement in local liaison and quality care. The benefits of TH included a decrease in travel, improved continuity of care, and increased access to specialised consultants. | Total costs for the 1000 TH follow-up visits were USD 145,522, averaging USD 146 per visit. TH burn visits were a cost-effective clinical alternative for the patient. In contrast, TH could be a financial burden to healthcare systems and inefficient for healthcare providers. | C |
| Redlick et al. (2002) Canada [36] | Cohort study | This study evaluated (1) patient and (2) physician satisfaction with 14 teleconsultations (video/audio communication) in follow-up burn care and assessed the costs and benefits of these teleconsultations in 1999. | (1) In total, 67% of patients felt that talking to the specialist and asking the specialist questions in their teleconsultation was much easier than a face-to-face visit, whereas 33% of patients found that teleconsultations were equal to an in-person visit. The patients indicated that they were very satisfied with their appointments and that the teleconsultations were much better than traveling to out-of-town specialists. (2) The consulting physician reported that patients presented with the same types of problems as those seen in regular practice. The consulting physician was also very satisfied because they saved the patients and burn care team time and money and allowed the burn care team to plan surgeries and rehabilitation strategies more efficiently. The only reported difficulty was with discussing personal issues with patients during teleconsultations. | (1) On average, the patients’ teleconsultations were completed in only 2.7 h. This time investment was significantly shorter than the estimated trip of more than two days to the burn unit (p < 0.0001). The average expense per patient was CAD 16.66 for a teleconsultation, which was significantly less than the estimated average cost per patient of CAD 615.74 for an out-of-town consultation (p < 0.01). (2) The average time was 19.5 min. The average cost of a teleconsultation was CAD 57.09 in specialist fees and CAD 11.12 in telecommunication fees (19.5 min at CAD 0.57 per minute). | C |
| Smith et al. (2004) Australia [37] | Cohort study | This study compared the use of videoconferencing for the assessment of burns with conventional, face-to-face (FTF) assessments. A total of 35 children with a previous burn injury were studied. | This study confirms that the quality of information collected during a videoconference appointment is comparable to that collected during a traditional, FTF appointment for a follow-up burns consultation. | No cost analysis. | C |
| ACUTE BURN MANAGEMENT AND FOLLOW-UP | |||||
| Wallace et al. (2012) UK [2] | Systematic review | A review of the findings of 24 articles in burn care to assess the evidence for the use of TH in acute burn care and outpatient treatment (from 1993 to 2010). Mostly case series studies. | The studies suggested that TH in the management of acute burns was feasible (TBSA evaluation, emergency triage, and need for interventions) and might be as good as face-to-face evaluation, aiding clinical decision-making. However, comparative studies showing TH superiority or equality were lacking. Further education was needed to familiarise professionals with technology. | Dependent on the country (healthcare system and burn infrastructure) and who pays. Greater patient convenience and substantially fewer costs and less time (more satisfied). The initial cost was higher for the medical care provider. | A |
| Vyas et al. (2017) USA [38] | Systematic review | A review of the findings of 23 articles about the use of TH in plastic and reconstructive surgery, and dermatology, five of which were on burn management (from 2010 to 2017). | All 23 articles reported TH benefits, which frequently related to better post-operative monitoring, greater access to rural settings without affecting the quality of care provided, and cost savings. TH improved the coordination of care and management of burn wounds, facilitated interprofessional collaboration over time and space, and saved a significant number of unnecessary referrals. Greater commitment, standardisation, and regulation were required. Privacy and security remained unresolved concerns. | Although the studies suggested that TH could produce cost savings and better results, larger and more general studies were needed. | A |
| Hoseini et al. (2016) Iran [39] | Systematic review | A review of 32 articles about TH applications in the treatment of burn patients (from 2000 to March 2016). | TH could help reduce possible errors in the categorisation of the burned patient. Remote monitoring had been shown to be successful in patients residing in distant areas. There was still resistance from doctors as well as legal challenges. Teleconsultation also led to success for outpatient injuries, though the potential for committing decision-making errors should not be underestimated. Numerous studies showed that the results of the burn size estimation and evaluation via imaging and TH were very close to the results from face-to-face evaluation and diagnosis. | The conventional technique showed a considerable percentage of unnecessary transfers. According to several findings, the use of TH to assess burns resulted in savings of money and time, increased productivity, reduced referrals, and unnecessary transportation, with the correct and most efficient method for patient transfer and treatment being chosen. | A |
| Wiktor et al. (2018) USA [40] | Retrospective multicentre study | A retrospective review was conducted of referrals from 2016 to 2017 at three regional burn centres utilising the Burn App to facilitate triage of patients by allowing referring providers to send encrypted photos, thus enhancing the telephone consultation process. | A total of 2011 consults were placed using the mobile phone app from 294 different referring facilities spanning seven states. Overall Burn App utilisation among enrolled referring centres was 45% (range 39–48%). Most patients were referred to outpatient clinics for continued burn care (59%), 22% were admitted, and 18% received care at local facilities. The application seemed to be a useful tool for patient triage. | As telehealth and technology were more readily utilised, the question of whether or not a platform such as the Burn App improved triage decisions, affected patient care, and ultimately reduced costs still required further study. | D |
| Martínez et al. (2018) South Africa [41] | Retrospective study | A review was conducted of all consultations using WhatsApp over an 18-month period, received by the burn centre’s two senior medical practitioners from 2015 to 2016. | 838 communications and 1562 different clinical consultations were described; 486 (58%) intrahospital and 352 (42%) between centres. Most of the images received were of adequate quality for the evaluation of depth, focus, colour, and clinical relevance. The use of WhatsApp in daily burn care processes significantly improved the quality of paediatric referrals to specialised burn services. Unnecessary referrals and outpatient visits were reduced, continuing medical education was facilitated, and care for large burns was improved through more effective communication. | Outpatient visits were significantly reduced during the study period. It was estimated that up to 160 unnecessary admissions were also avoided as a result of better triage that translated into considerable cost savings for the institution and better distribution of resources. | D |
| Russell et al. (2015) USA [42] | Retrospective study | This retrospective review from 2005 to 2014 evaluated burn TH visits and financial reimbursement during (2005–2007) and after (2008–2014) a Technology Opportunities Program (TOP) grant to a regional burn centre. | In 2005, it had 12 TH visits, which increased to 458 in 2014. It was possible to demonstrate that evaluation of burn extent and depth via video was essentially equivalent to face-to-face examination. Patient and provider satisfaction was extremely high. During the 26 months that the TOP grant was active, consultations at the burn centre almost tripled, air transports decreased from 100% to 44% of consults, and burn severity of those patients transported increased. | Over 3 years, they admitted 42 patients after initial TH evaluation that generated more than USD 4 million in hospital revenue. A separate sampling of 24% of teleburn visits from 2010 to 2011 showed that these visits directly resulted in USD 4.2 million in revenue to the University of Utah. This success has resulted in expanded institutional efforts in TH. Furthermore, because of the profitability of the teleburn enterprise, the hospital has assumed responsibility for operating costs, including equipment upgrades, and now budgets these as operating costs for the TH programme. | D |
| Turk et al. (2011) Turkey [43] | Cohort study | This study investigated the use of TH in decision-making and follow-up of 187 burn patients, in 2003 and up to 2009, all of whom had teleconsultations (audiovisual) with the same burn surgeon at the Ankara Burn Referral Centre. | Over a 66-month period, 525 televisits with 187 patients were carried out. As a result, 21 patients (11.2%) were transferred to the referral centre in Ankara. The mean TBSA was 23.3 ± 17.8%. The mean hospital stay was 16.4 ± 13.4 days. In total, 157 patients were discharged after successful burn therapy (84%). Nine (4.8%) died owing to multiorgan failure and sepsis. The number of deceased patients, televisits, and transferred patients decreased over time. | No cost analysis. However, TH was said to be appropriate and cost-effective for the treatment and follow-up of patients in burn units by personnel with limited experience. The potential benefits of TH included reductions in patient travel costs, continuity of care, and access to specialised health consultations in remote areas. | C |
| McWilliams et al. (2016) Australia [44] | Retrospective audit study | From 2005 to 2013, 904 patients were referred to the paediatric Burns Telehealth Service in Western Australia. This is a retrospective chart audit of avoided transfers and bed days, and the avoided associated costs to the tertiary burn unit and patient travel funding. | No clinical outcomes. | Over an 8-year period, the audit identified 4905 avoided inpatient bed days, 1763 avoided follow-up review transfers, and 364 avoided acute patient transfers for a total of 1312 paediatric burn patients because of this telehealth service. The paper presented the derivation of these outcomes and an estimation of their cost savings in 2012–2013 of AUD 1.89 million. | D |
| Head et al. (2022) USA [45] | Cohort study | To assess the efficacy and cost savings of virtual visits for acute, outpatient burn care in the home setting during a 6-month timeframe of the COVID-19 pandemic. | There were no significant differences in burn % TBSA, depth, cause, number of unplanned readmissions, number of unplanned reoperations, or complications. | Virtual visits offer significant cost savings for the patient and can be as effective as traditional face-to-face visits in the outpatient burn care setting. | C |
| Smith et al. (2007) Australia [46] | Retrospective study | Review of the first 1000 burns consultations conducted by the telepaediatric service over a 6-year timeframe. | No clinical outcomes. | Assuming that each consultation required a return journey, and the paediatric patients were accompanied by a parent or carer, the total distance saved would be over 1.4 million km. | D |
| Study Type | Number of Articles Selected |
|---|---|
| Systematic review | 6 |
| Randomised control trial | 1 |
| Cohort study | 13 |
| Retrospective study | 10 |
| Cross-sectional study | 4 |
| Case-control study | 3 |
| TOTAL | 37 articles |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
García-Díaz, A.; Vilardell-Roig, L.; Novillo-Ortiz, D.; Gacto-Sánchez, P.; Pereyra-Rodríguez, J.J.; Saigí-Rubió, F. Utility of Telehealth Platforms Applied to Burns Management: A Systematic Review. Int. J. Environ. Res. Public Health 2023, 20, 3161. https://doi.org/10.3390/ijerph20043161
García-Díaz A, Vilardell-Roig L, Novillo-Ortiz D, Gacto-Sánchez P, Pereyra-Rodríguez JJ, Saigí-Rubió F. Utility of Telehealth Platforms Applied to Burns Management: A Systematic Review. International Journal of Environmental Research and Public Health. 2023; 20(4):3161. https://doi.org/10.3390/ijerph20043161
Chicago/Turabian StyleGarcía-Díaz, Antonio, Lluís Vilardell-Roig, David Novillo-Ortiz, Purificación Gacto-Sánchez, José Juan Pereyra-Rodríguez, and Francesc Saigí-Rubió. 2023. "Utility of Telehealth Platforms Applied to Burns Management: A Systematic Review" International Journal of Environmental Research and Public Health 20, no. 4: 3161. https://doi.org/10.3390/ijerph20043161
APA StyleGarcía-Díaz, A., Vilardell-Roig, L., Novillo-Ortiz, D., Gacto-Sánchez, P., Pereyra-Rodríguez, J. J., & Saigí-Rubió, F. (2023). Utility of Telehealth Platforms Applied to Burns Management: A Systematic Review. International Journal of Environmental Research and Public Health, 20(4), 3161. https://doi.org/10.3390/ijerph20043161








