Time to Lift up COVID-19 Restrictions? Public Support towards Living with the Virus Policy and Associated Factors among Hong Kong General Public
Abstract
:1. Introduction
1.1. COVID-19 in Hong Kong and the Call for a LWV Policy
1.2. Factors Associated with Attitudes towards COVID-19 Policy
1.3. Resilient Coping and Support towards the LWV Policy
1.4. Self-Efficacy and Support towards the LWV Policy
1.5. Emotional Distress and Support towards the LWV Policy
2. Materials and Methods
2.1. Participants and Data Collection
2.2. Measurements
2.2.1. Background Information
2.2.2. Level of Support towards the LWV Policy
2.2.3. Resilient Coping
2.2.4. Self-Efficacy
2.2.5. Emotional Distress Related to COVID-19
2.2.6. Previous COVID-19 Infection
2.3. Statistical Analysis
3. Results
3.1. Descriptive Statistics
3.2. Correlation Analysis
3.3. Factors of Supportive Attitude towards the LWV Policy
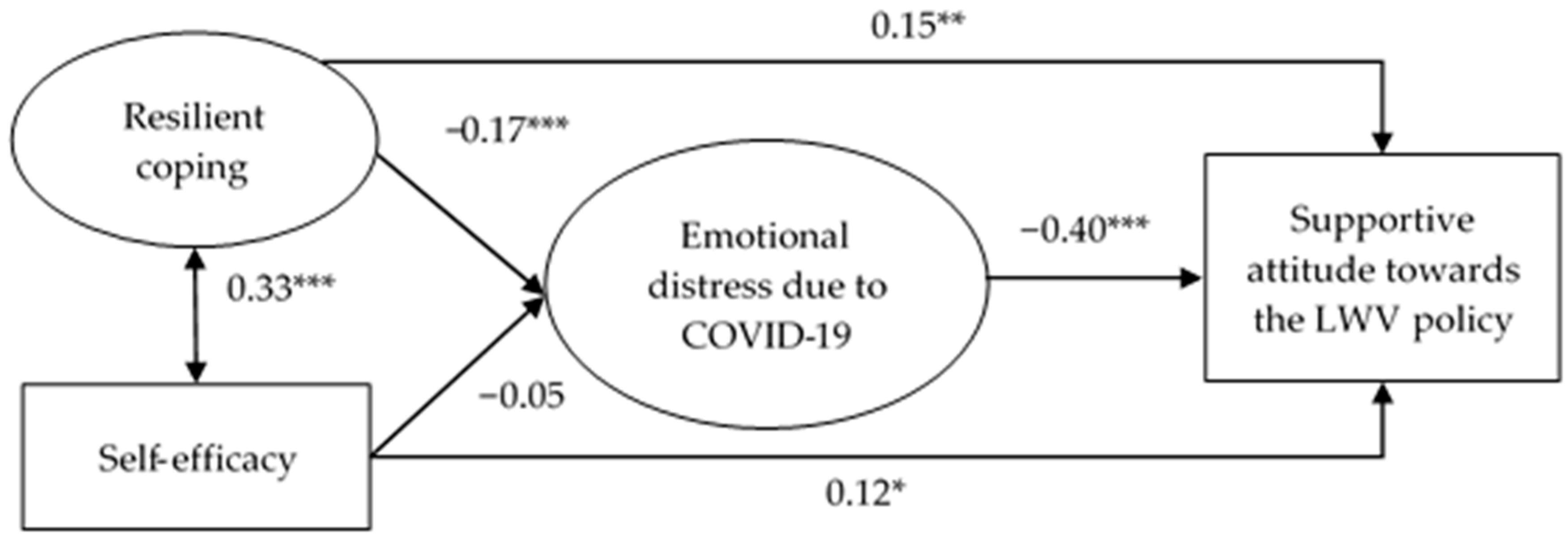
3.4. Structural Equation Model for Support towards the LWV Policy
3.5. Invariance Testing by Previous COVID-19 Infection Status
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Makridis, C.; Hartley, J. The Cost of COVID-19: A Rough Estimate of the 2020 US GDP Impact (6 April 2020). Spec. Ed. Policy Brief 2020. [Google Scholar]
- Nussbaumer-Streit, B.; Mayr, V.; Dobrescu, A.I.; Chapman, A.; Persad, E.; Klerings, I.; Wagner, G.; Siebert, U.; Ledinger, D.; Zachariah, C.; et al. Quarantine alone or in combination with other public health measures to control COVID-19: A rapid review. Cochrane Database Syst. Rev. 2020, 9, CD013574. [Google Scholar] [PubMed]
- Allen, D.W. COVID-19 Lockdown Cost/Benefits: A Critical Assessment of the Literature. Int. J. Econ. Bus. 2022, 29, 1–32. [Google Scholar] [CrossRef]
- Miles, D.K.; Stedman, M.; Heald, A.H. “Stay at Home, Protect the National Health Service, Save Lives”: A cost benefit analysis of the lockdown in the United Kingdom. Int. J. Clin. Practice 2021, 75, e13674. [Google Scholar] [CrossRef]
- Miles, D.; Stedman, M.; Heald, A. Living with COVID-19: Balancing Costs Against Benefits in the Face of the Virus. Natl. Inst. Econ. Review 2020, 253, R60–R76. [Google Scholar] [CrossRef]
- Haktanir, A.; Can, N.; Seki, T.; Kurnaz, M.F.; Dilmaç, B. Do we experience pandemic fatigue? Current state, predictors, and prevention. Curr. Psychol. 2021, 41, 7314–7325. [Google Scholar] [CrossRef]
- World Health Organization; Regional Office for Europe. Pandemic Fatigue: Reinvigorating the Public to Prevent COVID-19: Policy Framework for Supporting Pandemic Prevention and Management: Revised Version November 2020; World Health Organization: Copenhagen, Denmark, 2020. [Google Scholar]
- The Lancet Infectious Diseases. The COVID-19 exit strategy-why we need to aim low. Lancet Infect. Dis. 2021, 21, 297. [Google Scholar] [CrossRef]
- Marziano, V.; Guzzetta, G.; Mammone, A.; Riccardo, F.; Poletti, P.; Trentini, F.; Manica, M.; Siddu, A.; Bella, A.; Stefanelli, P.; et al. The effect of COVID-19 vaccination in Italy and perspectives for living with the virus. Nat. Commun. 2021, 12, 7272. [Google Scholar] [CrossRef]
- O’Leary, P.; Tsui, M.-S. Dealing and Living with OMICRON in the Pandemic: What Did We Learn and What Should We Do? Int. Soc. Work. 2022, 65, 201–202. [Google Scholar] [CrossRef]
- Raboisson, D.; Lhermie, G. Living With COVID-19: A Systemic and Multi-Criteria Approach to Enact Evidence-Based Health Policy. Front. Public Health 2020, 8, 294. [Google Scholar] [CrossRef]
- Lee, A.; Thornley, S.; Morris, A.J.; Sundborn, G. Should countries aim for elimination in the COVID-19 pandemic? BMJ 2020, 370, m3410. [Google Scholar] [CrossRef]
- Centre for Health Protection. Statistics on Cases Tested Positive for SARS-CoV-2 Virus. 2022. Available online: https://chp-dashboard.geodata.gov.hk/covid-19/en.html (accessed on 29 January 2023).
- Burki, T. Hong Kong’s fifth COVID-19 wave-the worst yet. Lancet Infect. Dis. 2022, 22, 455–456. [Google Scholar] [CrossRef]
- South China Morning Post. Hong Kong at the Tipping Point: ‘Frank Words’, Dire Warnings Prompted City Leader’s Rethink of tough Anti-Covid Measures. 2022. Available online: https://www.scmp.com/news/hong-kong/health-environment/article/3170886/hong-kong-tipping-point-frank-words-dire-warnings (accessed on 29 January 2023).
- YouGov. COVID-19: Level of Support for Actions Governments Could Take 2022. Available online: https://yougov.co.uk/topics/international/articles-reports/2020/03/17/level-support-actions-governments-could-take (accessed on 29 January 2023).
- Wright, L.; Steptoe, A.; Fancourt, D. What predicts adherence to COVID-19 government guidelines? Longitudinal analyses of 51,000 UK adults. medRxiv 2020. [Google Scholar] [CrossRef]
- Prati, G. Intention to receive a vaccine against SARS-CoV-2 in Italy and its association with trust, worry and beliefs about the origin of the virus. Health Educ. Res. 2020, 35, 505–511. [Google Scholar] [CrossRef]
- YouGov. COVID-19: Government Handling and Confidence in Health Authorities. 2021. Available online: https://yougov.co.uk/topics/international/articles-reports/2020/03/17/perception-government-handling-covid-19 (accessed on 29 January 2023).
- The Lancet. COVID-19: Learning from experience. Lancet 2020, 395, 1011. [Google Scholar] [CrossRef]
- Lazarus, J.V.; Ratzan, S.; Palayew, A.; Billari, F.C.; Binagwaho, A.; Kimball, S.; Larson, H.J.; Melegaro, A.; Rabin, K.; White, T.M.; et al. COVID-SCORE: A global survey to assess public perceptions of government responses to COVID-19 (COVID-SCORE-10). PLoS ONE 2020, 15, e0240011. [Google Scholar] [CrossRef]
- Mallinas, S.R.; Maner, J.K.; Ashby Plant, E. What factors underlie attitudes regarding protective mask use during the COVID-19 pandemic? Personal. Individ. Differ. 2021, 181, 111038. [Google Scholar] [CrossRef]
- Paul, E.; Steptoe, A.; Fancourt, D. Attitudes towards vaccines and intention to vaccinate against COVID-19: Implications for public health communications. Lancet Reg. Health 2021, 1, 100012. [Google Scholar] [CrossRef]
- Wang, X. Factors associated with public support for a lockdown measure in China during the COVID-19 pandemic. Asian J. Soc. Psychol. 2022, 25, 658–673. [Google Scholar] [CrossRef]
- Pummerer, L.; Böhm, R.; Lilleholt, L.; Winter, K.; Zettler, I.; Sassenberg, K. Conspiracy Theories and Their Societal Effects During the COVID-19 Pandemic. Soc. Psychol. Pers. Sci. 2021, 13, 49–59. [Google Scholar] [CrossRef]
- Blendon, R.J.; Koonin, L.M.; Benson, J.M.; Cetron, M.S.; Pollard, W.E.; Mitchell, E.W.; Weldon, K.; Herrmann, M.J. Public Response to Community Mitigation Measures for Pandemic Influenza. Emerg. Infect. Dis. 2008, 14, 778–786. [Google Scholar] [CrossRef] [PubMed]
- Peretti-Watel, P.; Verger, P.; Launay, O. The French general population’s attitudes toward lockdown against COVID-19: A fragile consensus. BMC Public Health 2020, 20, 1920. [Google Scholar] [CrossRef] [PubMed]
- Gerace, A.; Rigney, G.; Anderson, J.R. Predicting attitudes towards easing COVID-19 restrictions in the United States of America: The role of health concerns, demographic, political, and individual difference factors. PLoS ONE 2022, 17, e0263128. [Google Scholar] [CrossRef] [PubMed]
- Lei, Y.; Wang, J.; Yue, Y.; Zhou, H.; Yin, W. Rethinking the relationships of vulnerability, resilience, and adaptation from a disaster risk perspective. Nat. Hazards 2014, 70, 609–627. [Google Scholar] [CrossRef]
- Luthar, S.S.; Cicchetti, D. The construct of resilience: Implications for interventions and social policies. Dev. Psychopathol. 2001, 12, 857–885. [Google Scholar] [CrossRef]
- Polk, L.V. Toward a Middle-Range Theory of Resilience. Adv. Nurs. Sci. 1997, 19, 1–13. [Google Scholar] [CrossRef]
- Ruiz-Robledillo, N.; De Andrés-García, S.; Pérez-Blasco, J.; González-Bono, E.; Moya-Albiol, L. Highly resilient coping entails better perceived health, high social support and low morning cortisol levels in parents of children with autism spectrum disorder. Res. Dev. Disabil. 2014, 35, 686–695. [Google Scholar] [CrossRef]
- Friesen, K.A.; Weiss, J.A.; Howe, S.J.; Kerns, C.M.; McMorris, C.A. Mental Health and Resilient Coping in Caregivers of Autistic Individuals during the COVID-19 Pandemic: Findings from the Families Facing COVID Study. J. Autism Dev. Disord. 2021, 52, 3027–3037. [Google Scholar] [CrossRef]
- Tsehay, M.; Belete, A.; Necho, M. Factors Associated with Psychological Distress and Brief Resilient Coping Level During the COVID-19 Pandemic Among Health-Care Professionals in Dessie, Ethiopia. Psychol. Res. Behav. Manag. 2020, 13, 1213–1221. [Google Scholar] [CrossRef]
- Bandura, A.; Freeman, W.H.; Lightsey, R. Self-Efficacy: The Exercise of Control; Springer: Berlin/Heidelberg, Germany, 1999. [Google Scholar]
- Avery, E.J.; Kim, M.; Park, S. Self-Efficacy and Other Considerations in Performance of Risk-Reducing Behaviors during a Major Disease Outbreak. J. Health Commun. 2021, 26, 112–120. [Google Scholar] [CrossRef]
- Sheeran, P.; Maki, A.; Montanaro, E.; Avishai-Yitshak, A.; Bryan, A.; Klein, W.M.P.; Miles, E.; Rothman, A.J. The impact of changing attitudes, norms, and self-efficacy on health-related intentions and behavior: A meta-analysis. Health Psychol. 2016, 35, 1178–1188. [Google Scholar] [CrossRef]
- Mo, P.K.H.; Fong, V.W.I.; Song, B.; Di, J.; Wang, Q.; Wang, L. Association of Perceived Threat, Negative Emotions, and Self-Efficacy With Mental Health and Personal Protective Behavior Among Chinese Pregnant Women During the COVID-19 Pandemic: Cross-sectional Survey Study. J. Med. Internet Res. 2021, 23, e24053. [Google Scholar] [CrossRef]
- Yıldırım, M.; Güler, A. COVID-19 severity, self-efficacy, knowledge, preventive behaviors, and mental health in Turkey. Death Stud. 2022, 46, 979–986. [Google Scholar] [CrossRef]
- Taylor, S.; Landry, C.A.; Paluszek, M.M.; Rachor, G.S.; Asmundson, G.J. Worry, avoidance, and coping during the COVID-19 pandemic: A comprehensive network analysis. J. Anxiety Disord. 2020, 76, 102327. [Google Scholar] [CrossRef]
- Boyraz, G.; Legros, D.N.; Tigershtrom, A. COVID-19 and traumatic stress: The role of perceived vulnerability, COVID-19-related worries, and social isolation. J. Anxiety Disord. 2020, 76, 102307. [Google Scholar] [CrossRef]
- Sinclair, V.G.; Wallston, K.A. The Development and Psychometric Evaluation of the Brief Resilient Coping Scale. Assessment 2004, 11, 94–101. [Google Scholar] [CrossRef]
- Fung, S.-F. Validity of the Brief Resilience Scale and Brief Resilient Coping Scale in a Chinese Sample. Int. J. Environ. Res. Public Health 2020, 17, 1265. [Google Scholar] [CrossRef]
- Chen, G.; Gully, S.M.; Eden, D. Validation of a New General Self-Efficacy Scale. Organ. Res. Methods 2001, 4, 62–83. [Google Scholar] [CrossRef]
- Di, W.; Nie, Y.; Chua, B.; Chye, S.; Teo, T. Developing a Single-Item General Self-Efficacy Scale: An Initial Study; Research Square: Durham, NC, USA, 2021. [Google Scholar]
- Gu, J.; Zhong, Y.; Hao, Y.; Zhou, D.; Tsui, H.; Hao, C.; Gao, Q.; Ling, W.; Lau, J.T.F. Preventive Behaviors and Mental Distress in Response to H1N1 Among University Students in Guangzhou, China. Asia Pac. J. Public Health 2015, 27, NP1867–NP1879. [Google Scholar] [CrossRef]
- Liu, Y.; Rocklöv, J. The effective reproduction number for the omicron SARS-CoV-2 variant of concern is several times higher than Delta. J. Travel Med. 2022, 29, taac037. [Google Scholar] [CrossRef]
- Prati, G.; Mancini, A.D. The psychological impact of COVID-19 pandemic lockdowns: A review and meta-analysis of longitudinal studies and natural experiments. Psychol. Med. 2021, 51, 201–211. [Google Scholar] [CrossRef] [PubMed]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [PubMed]
- Habersaat, K.B.; Betsch, C.; Danchin, M.; Sunstein, C.R.; Böhm, R.; Falk, A.; Brewer, N.T.; Omer, S.B.; Scherzer, M.; Sah, S.; et al. Ten considerations for effectively managing the COVID-19 transition. Nat. Hum. Behav. 2020, 4, 677–687. [Google Scholar] [CrossRef] [PubMed]
- Kaim, A.; Jaffe, E.; Siman-Tov, M.; Khairish, E.; Adini, B. Impact of a Brief Educational Intervention on Knowledge, Perceived Knowledge, Perceived Safety, and Resilience of the Public During COVID-19 Crisis. Int. J. Environ. Res. Public Health 2020, 17, 5971. [Google Scholar] [CrossRef] [PubMed]
- Sippel, L.M.; Pietrzak, R.H.; Charney, D.S.; Mayes, L.C.; Southwick, S.M. How does social support enhance resilience in the trauma-exposed individual? Ecol. Soc. 2015, 20, 1–10. [Google Scholar] [CrossRef]
- Bandura, A. Health Promotion by Social Cognitive Means. Health Educ. Behav. 2004, 31, 143–164. [Google Scholar] [CrossRef]
- Census and Statistics Department HKSAR. Population by Sex and Age Group. 2022. Available online: https://www.census2021.gov.hk/en/index.html (accessed on 29 January 2023).
- Lau, J.T.F.; Tsui, H.Y.; Wang, Q.S. Effects of two telephone survey methods on the level of reported risk behaviours. Sex. Transm. Infect. 2003, 79, 325–331. [Google Scholar] [CrossRef]
- Yang, X.; She, R.; Lau, M.M.C.; Lau, J.T. Anticipated socio-political developments and related personal responses as structural determinants of mental health problems: A population-based study. Int. J. Soc. Psychiatry 2020, 66, 58–66. [Google Scholar] [CrossRef]
| Overall | Supportive Attitude towards the LWV Policy | |||
|---|---|---|---|---|
| Supportive | Unsupportive | p Value | ||
| N (%) | n (%) | n (%) | ||
| Overall | 500 (100.0) | 198 (39.6) | 302 (60.4) | |
| Background factors | ||||
| Gender | 0.092 | |||
| Female | 337 (67.0) | 124 (62.6) | 211 (69.9) | |
| Male | 165 (33.0) | 74 (37.4) | 91 (30.1) | |
| Age groups (years) | 0.003 | |||
| 18–30 | 71 (14.2) | 40 (20.2) | 31 (10.3) | |
| 31–60 | 262 (52.4) | 103 (52.0) | 159 (52.6) | |
| >60 | 167 (33.4) | 55 (27.8) | 112 (37.1) | |
| Educational level | <0.001 | |||
| Below college | 365 (74.8) | 127 (65.5) | 238 (81.0) | |
| College or above | 123 (25.2) | 67 (34.5) | 56 (19.0) | |
| Marital status | 0.021 | |||
| Others | 151 (30.5) | 71 (36.4) | 80 (26.7) | |
| Married | 344 (69.5) | 124 (63.6) | 220 (73.3) | |
| Employment status | 0.033 | |||
| Full-time | 208 (41.6) | 100 (50.5) | 108 (35.8) | |
| Part-time | 41 (8.2) | 11 (5.6) | 30 (9.9) | |
| Retired | 114 (22.8) | 41 (20.7) | 73 (24.2) | |
| Under-employed | 27 (5.4) | 10 (5.1) | 17 (5.6) | |
| Homemaker | 94 (18.8) | 30 (15.2) | 64 (21.2) | |
| Others | 16 (3.2) | 6 (3.0) | 10 (3.3) | |
| Chronic disease status | 0.459 | |||
| No/unknown | 321 (64.2) | 131 (66.2) | 190 (62.9) | |
| Yes | 179 (35.8) | 67 (33.8) | 112 (37.1) | |
| COVID-19 ever infection | 0.002 | |||
| No/Don’t know/Refused to answer | 416 (83.2) | 152 (76.8) | 264 (87.4) | |
| Yes | 84 (16.8) | 46 (23.2) | 38 (12.6) | |
| Range | Mean, SD | 1 | 2 | 3 | |
|---|---|---|---|---|---|
| 1. Resilient coping | 4–20 | 15.5, 2.6 | - | ||
| 2. Self-efficacy | 1–5 | 3.9, 0.7 | 0.49 *** | - | |
| 3. Emotional distress due to COVID-19 | 2–10 | 4.4, 2.4 | −0.18 *** | −0.04 | - |
| ORc (95% CI) | ORa (95% CI) | |
|---|---|---|
| Resilient coping | 1.16 (1.07, 1.25) *** | 1.18 (1.08, 1.28) *** |
| Self-efficacy | 1.43 (1.09, 1.87) * | 1.54 (1.16, 2.07) ** |
| Emotional distress due to COVID-19 | 0.87 (0.81, 0.94) ** | 0.89 (0.82, 0.97) ** |
| Previous COVID-19 Infection = No | Previous COVID-19 Infection = Yes | Wald Test | ||||||
|---|---|---|---|---|---|---|---|---|
| β | p | β | p | Estimate | p | Invariance | Model Fit | |
| Structural path | ||||||||
| Resilient coping → Emotional distress due to COVID-19 | −0.13 | <0.001 | −0.14 | 0.805 | 0.17 | 0.682 | Supported | χ2/df = 196.93/172 = 1.15 (p = 0.093); CFI = 0.99; TLI = 0.99; RMSEA = 0.02 |
| Self-efficacy → Emotional distress due to COVID-19 | −0.11 | <0.001 | −0.06 | 0.842 | 0.42 | 0.519 | Supported | χ2/df = 199.20/174 = 1.15 (p = 0.092); CFI = 0.99; TLI = 0.99; RMSEA = 0.02 |
| Resilient coping → Supportive attitude towards the LWV policy | −0.07 | 0.004 | −0.06 | 0.299 | 0.31 | 0.580 | Supported | χ2/df = 234.48/174 = 1.35 (p = 0.002); CFI = 0.98; TLI = 0.98; RMSEA = 0.04 |
| Self-efficacy → Supportive attitude towards the LWV policy | 0.35 | <0.001 | 0.14 | 0.286 | 0.89 | 0.346 | Supported | χ2/df = 260.78/176 = 1.48 (p < 0.001); CFI = 0.98; TLI = 0.97; RMSEA = 0.05 |
| Emotional distress due to COVID-19 → Supportive attitude towards the LWV policy | −0.42 | <0.001 | −0.23 | 0.832 | 0.14 | 0.704 | Supported | χ2/df = 196.93/172 = 1.15 (p = 0.093); CFI = 0.99; TLI = 0.99; RMSEA = 0.02 |
| Indirect path | ||||||||
| Resilient coping → Emotional distress due to COVID-19 → Supportive attitude towards the LWV policy | 0.05 | 0.001 | 0.03 | 0.350 | 0.01 | 0.913 | Supported | χ2/df = 196.93/172 = 1.15 (p = 0.093); CFI = 0.99; TLI = 0.99; RMSEA = 0.01 |
| Self-efficacy → Emotional distress due to COVID-19 → Supportive attitude towards the LWV policy | 0.05 | <0.001 | 0.01 | 0.397 | 1.04 | 0.309 | Supported | χ2/df = 199.20/174 = 1.15 (p = 0.092); CFI = 0.99; TLI = 0.99; RMSEA = 0.02 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mo, P.K.H.; Yu, Y.; Lau, M.M.C.; Ling, R.H.Y.; Lau, J.T.F. Time to Lift up COVID-19 Restrictions? Public Support towards Living with the Virus Policy and Associated Factors among Hong Kong General Public. Int. J. Environ. Res. Public Health 2023, 20, 2989. https://doi.org/10.3390/ijerph20042989
Mo PKH, Yu Y, Lau MMC, Ling RHY, Lau JTF. Time to Lift up COVID-19 Restrictions? Public Support towards Living with the Virus Policy and Associated Factors among Hong Kong General Public. International Journal of Environmental Research and Public Health. 2023; 20(4):2989. https://doi.org/10.3390/ijerph20042989
Chicago/Turabian StyleMo, Phoenix K. H., Yanqiu Yu, Mason M. C. Lau, Rachel H. Y. Ling, and Joseph T. F. Lau. 2023. "Time to Lift up COVID-19 Restrictions? Public Support towards Living with the Virus Policy and Associated Factors among Hong Kong General Public" International Journal of Environmental Research and Public Health 20, no. 4: 2989. https://doi.org/10.3390/ijerph20042989
APA StyleMo, P. K. H., Yu, Y., Lau, M. M. C., Ling, R. H. Y., & Lau, J. T. F. (2023). Time to Lift up COVID-19 Restrictions? Public Support towards Living with the Virus Policy and Associated Factors among Hong Kong General Public. International Journal of Environmental Research and Public Health, 20(4), 2989. https://doi.org/10.3390/ijerph20042989










