Knowledge, Attitude, and Practice towards COVID-19 among Patients Attending Phuentsholing Hospital, Bhutan: A Cross-Sectional Study
Abstract
1. Introduction
2. Methods
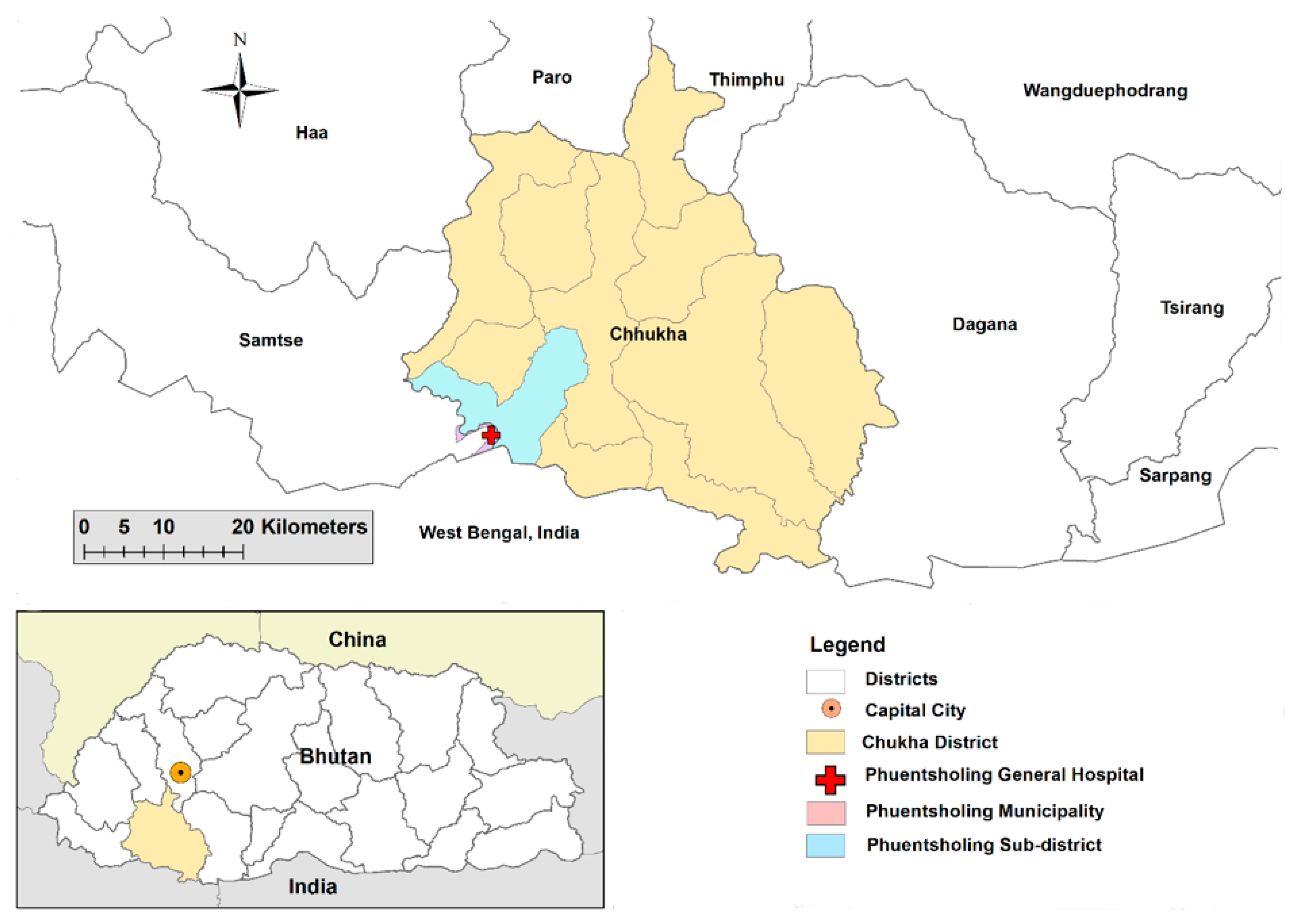
2.1. Study Design and Participants
2.2. Sampling and Participant Recruitment
2.3. Data Collection Instruments
2.4. Data Processing and Analysis
3. Results
3.1. Socio-Demographic Characteristics of Study Participants and Source of Information on COVID-19
3.2. Knowledge
3.3. Attitude
3.4. Practice
3.5. Correlates of Good Knowledge, Positive Attitude, and Good Practice
4. Discussion
4.1. Conclusions
4.2. Limitations and Strengths of the Study
4.3. Practical and Theoretical Implications of the Work
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wang, C.; Horby, P.W.; Hayden, F.G.; Gao, G.F. A novel coronavirus outbreak of global health concern. Lancet 2020, 395, 470–473. [Google Scholar] [CrossRef]
- Pal, M.; Berhanu, G.; Desalegn, C.; Kandi, V. Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2): An Update. Cureus 2020, 12, e7423. [Google Scholar] [CrossRef]
- World Health Organization. WHO Coronavirus Disease (COVID-19) Dashboard [Internet]. 2022. Available online: https://covid19.who.int/ (accessed on 2 February 2021).
- Ghahramani, S.; Lankarani, K.B.; Yousefi, M.; Heydari, K.; Shahabi, S.; Azmand, S. A Systematic Review and Meta-Analysis of Burnout Among Healthcare Workers During COVID-19. Front. Psychiatry 2021, 12, 758849. [Google Scholar] [CrossRef]
- Galanis, P.; Vraka, I.; Fragkou, D.; Bilali, A.; Kaitelidou, D. Nurses’ burnout and associated risk factors during the COVID-19 pandemic: A systematic review and meta-analysis. J. Adv. Nurs. 2021, 77, 3286–3302. [Google Scholar] [CrossRef]
- Events: European Comission. The COVID-19 Pandemic Crisis and the Impact on Health Systems: Curbing the Pandemic and Improving Health Outcomes in Low and Middle Income Countries [Internet]. Available online: https://ec.europa.eu/international-partnerships/events/covid-19-pandemic-crisis-and-impact-health-systems-curbing-pandemic-and-improving-health_en (accessed on 2 February 2021).
- Singanayagam, A.; Hakki, S.; Dunning, J.; Madon, K.J.; Crone, M.A.; Koycheva, A.; Derqui-Fernandez, N.; Barnett, J.L.; Whitfield, M.G.; Varro, R.; et al. Community transmission and viral load kinetics of the SARS-CoV-2 delta (B.1.617.2) variant in vaccinated and unvaccinated individuals in the UK: A prospective, longitudinal, cohort study. Lancet Infect. Dis. 2022, 22, 183–195. [Google Scholar]
- Stokel-Walker, C. What do we know about covid vaccines and preventing transmission? BMJ 2022, 376, o298. [Google Scholar] [CrossRef]
- Tsheten, T.; Lowe, C.; Wangdi, K.; Kelly, M.; Mationg, M.L.; Williams, G.M.; McManus, D.P.; Gray, D.J. COVID-19 continues its rampage in children and in unvaccinated communities due to the Delta and Omicron variants-Infectious Diseases & Tropical Medicine. Infect. Dis. Trop. Med. 2022, 8, e810. [Google Scholar] [CrossRef]
- Tachfouti, N.; Slama, K.; Berraho, M.; Nejjari, C. The impact of knowledge and attitudes on adherence to tuberculosis treatment: A case-control study in a Moroccan region. Pan Afr. Med. J. 2012, 12, 52. [Google Scholar]
- Zhong, B.L.; Luo, W.; Li, H.M.; Zhang, Q.Q.; Liu, X.G.; Li, W.T.; Li, Y. Knowledge, attitudes, and practices towards COVID-19 among chinese residents during the rapid rise period of the COVID-19 outbreak: A quick online cross-sectional survey. Int. J. Biol. Sci. 2020, 16, 1745–1752. [Google Scholar] [CrossRef]
- Qazi, A.; Qazi, J.; Naseer, K.; Zeeshan, M.; Hardaker, G.; Maitama, J.Z.; Haruna, K. Analyzing situational awareness through public opinion to predict adoption of social distancing amid pandemic COVID-19. J. Med. Virol. 2020, 92, 849–855. [Google Scholar] [CrossRef]
- Azlan, A.A.; Hamzah, M.R.; Sern, T.J.; Ayub, S.H.; Mohamad, E. Public knowledge, attitudes and practices towards COVID-19: A cross-sectional study in Malaysia. PLoS ONE 2020, 15, e0233668. [Google Scholar]
- Della Polla, G.; Pelullo, C.P.; Napolitano, F.; Lambiase, C.; De Simone, C.; Angelillo, I.F. Knowledge, attitudes, and practices towards infectious diseases related to travel of community pharmacists in italy. Int. J. Environ. Res. Public Health 2020, 17, 2147. [Google Scholar] [CrossRef]
- Yap, J.; Lee, V.J.; Yau, T.Y.; Ng, T.P.; Tor, P.C. Knowledge, attitudes and practices towards pandemic influenza among cases, close contacts, and healthcare workers in tropical Singapore: A cross-sectional survey. BMC Public Health 2010, 10, 442. [Google Scholar] [CrossRef]
- Akalu, Y.; Ayelign, B.; Molla, M.D. Knowledge, Attitude and Practice Towards COVID-19 Among Chronic Disease Patients at Addis Zemen Hospital, Northwest Ethiopia. Infect. Drug Resist. 2020, 13, 1949–1960. [Google Scholar]
- Ferdous, M.Z.; Islam, M.S.; Sikder, M.T.; Mosaddek, A.S.M.; Zegarra-Valdivia, J.A.; Gozal, D. Knowledge, attitude, and practice regarding COVID-19 outbreak in Bangladesh: An onlinebased cross-sectional study. PLoS ONE 2020, 15, e0239254. [Google Scholar]
- Islam, S.; Emran, G.I.; Rahman, E.; Banik, R.; Sikder, T.; Smith, L.; Hossain, S. Knowledge, attitudes and practices associated with the COVID-19 among slum dwellers resided in Dhaka City: A Bangladeshi interview-based survey. J. Public Health 2021, 43, 13–25. [Google Scholar] [CrossRef]
- Ministry of Health RG of, B. Public Notification. 2022. Available online: https://www.facebook.com/photo.php?fbid=587966853156151&set=a.370886901530815&type=3 (accessed on 29 December 2022).
- Tsheten, T.; Wangchuk, S.; Wangmo, D.; Clements, A.C.; Gray, D.J.; Wangdi, K. COVID-19 Response and Lessons Learned on Dengue Control in Bhutan. J. Med. Entomol. 2021, 58, 502–504. [Google Scholar] [CrossRef]
- Penjor, K.; Zangpo, T.; Clements, A.C.; Gray, D.J.; Wangdi, K. Has COVID19 derailed Bhutan′s national malaria elimination goal? A commentary. Malar J. 2021, 20, 20. [Google Scholar] [CrossRef]
- Lhendup, K.; Tsheten, T.; Rinzin, T.; Wangdi, K. Risk Factors of Symptomatic COVID-19 in Samtse District, Bhutan. Front. Public Health 2022, 10, 857084. [Google Scholar] [CrossRef]
- Kumar, S.; Preetha, G. Health promotion: An effective tool for global health. Indian J. Community Med. 2012, 37, 5. [Google Scholar] [CrossRef]
- Girum, T.; Lentiro, K.; Geremew, M.; Migora, B.; Shewamare, S. Global strategies and effectiveness for COVID-19 prevention through contact tracing, screening, quarantine, and isolation: A systematic review. Trop. Med. Health 2020, 48, 91. [Google Scholar] [CrossRef]
- National Statistic Bureau. Population and housing census of Bhutan, National Report. 2017. Available online: https://www.amisdubhoutan.fr/page02zq/PHCB2017_national.pdf (accessed on 2 February 2021).
- Olum, R.; Chekwech, G.; Wekha, G.; Nassozi, D.R.; Bongomin, F. Coronavirus Disease-2019: Knowledge, Attitude, and Practices of Health Care Workers at Makerere University Teaching Hospitals, Uganda. Front. Public Health 2020, 8, 181. [Google Scholar] [CrossRef]
- Goni, M.D.; Naing, N.N.; Hasan, H.; Wan-Arfah, N.; Deris, Z.Z.; Arifin, W.N.; Hussin, T.M.A.R.; Abdulrahman, A.S.; Baaba, A.A.; Arshad, M.R. Development and validation of knowledge, attitude and practice questionnaire for prevention of respiratory tract infections among Malaysian Hajj pilgrims. BMC Public Health 2020, 20, 189. [Google Scholar] [CrossRef]
- Al-Hanawi, M.K.; Angawi, K.; Alshareef, N.; Qattan, A.M.; Helmy, H.Z.; Abudawood, Y.; Alqurashi, M.; Kattan, W.M.; Kadasah, N.A.; Chirwa, G.C.; et al. Knowledge, Attitude and Practice Toward COVID-19 Among the Public in the Kingdom of Saudi Arabia: A Cross-Sectional Study. Front. Public Health 2020, 8, 217. [Google Scholar] [CrossRef]
- Yousaf, M.A.; Noreen, M.; Saleem, T.; Yousaf, I. A Cross-Sectional Survey of Knowledge, Attitude, and Practices (KAP) Toward Pandemic COVID-19 Among the General Population of Jammu and Kashmir, India. Soc. Work Public Health 2020, 35, 569–578. [Google Scholar] [CrossRef]
- Christy, J.S.; Kaur, K.; Gurnani, B.; Hess, O.M.; Narendran, K.; Venugopal, A.; Anuja, J.; Manohar, D.; Raman, R.; Venkatesh, R. Knowledge, attitude and practise toward COVID-19 among patients presenting to five tertiary eye care hospitals in South India-A multicentre questionnaire-based survey. Indian J. Ophthalmol. 2020, 68, 2385. [Google Scholar]
- Sah, G.S.; Shrestha, G.; Dhakal, A.; Mulmi, R.; Sapkota, A.; Poudel, S. Knowledge, Attitudes, and Practices of Cancer Patients Towards COVID-19: A Cross-Sectional Study in Central Nepal. Cancer Manag. Res. 2020, 12, 10173–10180. [Google Scholar] [CrossRef]
- Padmanaban, S.; Rajendran, P.; Davis, P.; Velayutham, P. Knowledge, attitude and practices towards COVID-19 among higher education students in India: A cross sectional study. J. Public Health 2021, 30, 1661–1673. [Google Scholar] [CrossRef]
- Devkota, H.R.; Sijali, T.R.; Bogati, R.; Clarke, A.; Adhikary, P.; Karkee, R. How Does Public Knowledge, Attitudes, and Behaviors Correlate in Relation to COVID-19? A Community-Based Cross-Sectional Study in Nepal. Front. Public Health 2021, 8, 589372. [Google Scholar] [CrossRef]
- Gebretsadik, D.; Gebremichael, S.; Belete, M.A. Knowledge, Attitude and Practice Toward COVID-19 Pandemic Among Population Visiting Dessie Health Center for COVID-19 Screening, Northeast Ethiopia. Infect. Drug Resist. 2021, 14, 905–915. [Google Scholar] [CrossRef]
- Ayouni, I.; Maatoug, J.; Dhouib, W.; Zammit, N.; Fredj, S.B.; Ghammam, R.; Ghannem, H. Effective public health measures to mitigate the spread of COVID-19: A systematic review. BMC Public Health 2021, 21, 1015. [Google Scholar] [CrossRef]
- Olawade, D.; Wada, O.; Odetayo, A.; Akeju, O.; Asaolu, F.; Owojori, G. COVID-19 vaccine hesitancy among Nigerian youths: Case study of students in Southwestern Nigeria. J. Educ. Health Promot. 2022, 11, 244. [Google Scholar] [CrossRef]
- Biancovilli, P.; Makszin, L.; Jurberg, C. Misinformation on social networks during the novel coronavirus pandemic: A quali-quantitative case study of Brazil. BMC Public Health 2021, 21, 1200. [Google Scholar]
- de Carvalho, V.D.H.; Nepomuceno, T.C.C.; Poleto, T.; Costa, A.P.C.S. The COVID-19 Infodemic on Twitter: A Space and Time Topic Analysis of the Brazilian Immunization Program and Public Trust. Trop. Med. Infect. Dis. 2022, 7, 425. [Google Scholar] [CrossRef]
- Njoga, E.O.; Mshelbwala, P.P.; Abah, K.O.; Awoyomi, O.J.; Wangdi, K.; Pewan, S.B.; Oyeleye, F.A.; Galadima, H.B.; Alhassan, S.A.; Okoli, C.E.; et al. COVID-19 Vaccine Hesitancy and Determinants of Acceptance among Healthcare Workers, Academics and Tertiary Students in Nigeria. Vaccines 2022, 10, 626. [Google Scholar] [CrossRef]
- Sato, R. COVID-19 Vaccine Hesitancy and Trust in Government in Nigeria. Vaccines 2022, 10, 1008. [Google Scholar] [CrossRef]
- Bajos, N.; Spire, A.; Silberzan, L.; Sireyjol, A.; Jusot, F.; Meyer, L.; Franck, J.E.; Warszawski, J.; Bagein, G.; Counil, E.; et al. When Lack of Trust in the Government and in Scientists Reinforces Social Inequalities in Vaccination Against COVID-19. Front. Public Health 2022, 10, 2005. [Google Scholar]
- Abdelhafiz, A.S.; Mohammed, Z.; Ibrahim, M.E.; Ziady, H.H.; Alorabi, M.; Ayyad, M.; Sultan, E.A. Knowledge, Perceptions, and Attitude of Egyptians Towards the Novel Coronavirus Disease (COVID-19). J. Community Health 2020, 45, 881–890. [Google Scholar]
- Lee, M.; Kang, B.A.; You, M. Knowledge, attitudes, and practices (KAP) toward COVID-19: A cross-sectional study in South Korea. BMC Public Health 2021, 21, 295. [Google Scholar] [CrossRef]
- Kasemy, Z.A.; Bahbah, W.A.; Zewain, S.K.; Haggag, M.G.; Alkalash, S.H.; Zahran, E.; Desouky, D.E. Knowledge, Attitude and Practice toward COVID-19 among Egyptians. J. Epidemiol. Glob. Health 2020, 10, 378. [Google Scholar] [CrossRef]
- Banik, R.; Rahman, M.; Sikder, M.; Rahman, Q.M.; Pranta, M.U.R. Knowledge, attitudes, and practices related to the COVID-19 pandemic among Bangladeshi youth: A web-based cross-sectional analysis. J. Public Health 2021, 31, 165. [Google Scholar]
- Dolkar, S. Govt. Distributes Free Hand Sanitizers to the Public in Thimphu. BBS. 2020. Available online: http://www.bbs.bt/news/?p=129353 (accessed on 12 December 2021).
- Tashi, S. Facemasks and Hand Sanitizers Run Out Due to COVID-2019 Scare. Business Bhutan. 2020. Available online: https://businessbhutan.bt/facemasks-and-hand-sanitizers-run-out-due-to-covid-2019-scare/ (accessed on 12 December 2021).
- Dorji, T.; Wangmo, K.; Wangchuk, T.; Wangdi, K. Knowledge, Attitude, and Practice Toward COVID-19 Among Sherubtse College Students in Bhutan: A Web-Based Cross-Sectional Study. Front. Public Health 2021, 9, 721493. [Google Scholar] [CrossRef]
- World Health Organization. Promote Hand Hygiene to Save Lives and Combat COVID-19. Available online: https://www.who.int/southeastasia/news/detail/04-05-2020-promote-hand-hygiene-to-save-lives-and-combat-covid-19 (accessed on 12 December 2021).
- Qutob, N.; Awartani, F. Knowledge, attitudes and practices (KAP) towards COVID-19 among Palestinians during the COVID-19 outbreak: A cross-sectional survey. PLoS ONE 2021, 16, e0244925. [Google Scholar] [CrossRef]
- Erfani, A.; Shahriarirad, R.; Ranjbar, K.; Mirahmadizadeh, A.; Moghadami, M. Knowledge, Attitude and Practice toward the Novel Coronavirus (COVID-19) Outbreak: A Population-Based Survey in Iran. Bull Wold Health Organ 2020, 30, 10–2471. [Google Scholar] [CrossRef]
- Hossain, M.A.; Jahid, M.I.K.; Hossain, K.M.A.; Walton, L.M.; Uddin, Z.; Haque, M.O.; Kabir, M.F.; Arafat, S.Y.; Sakel, M.; Faruqui, R.; et al. Knowledge, attitudes, and fear of COVID-19 during the Rapid Rise Period in Bangladesh. PLoS ONE 2020, 15, e0239646. [Google Scholar] [CrossRef]
- Wangchuk, T.; Kinga, K.; Wangdi, U.; Tshering, U.; Wangdi, K. Hand Hygiene, Face Mask Use, and Associated Factors during the COVID-19 Pandemic among the Students of Mongar High-er Secondary School, Bhutan: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2023, 20, 1058. [Google Scholar] [CrossRef]
- Asaad, A.; El Sokkary, R.; Alzamanan, M.; El Shafei, M. Knowledge and attitudes towards Middle East respiratory sydrome-coronavirus (MERS-CoV) among health care workers in south-western Saudi Arabia. East. Mediterr. Health J. 2020, 26, 435–442. [Google Scholar] [CrossRef]
- Siddiquea, B.N.; Shetty, A.; Bhattacharya, O.; Afroz, A.; Billah, B. Global epidemiology of COVID-19 knowledge, attitude and practice: A systematic review and meta-analysis. BMJ Open 2021, 11, e051447. [Google Scholar] [CrossRef]
- Yesuf, M.; Abdu, M. Knowledge, attitude, prevention practice, and associated factors toward COVID-19 among preparatory school students in Southwest Ethiopia, 2021. PLoS ONE 2022, 17, e0262907. [Google Scholar] [CrossRef]
- Kanyangarara, M.; Hamapumbu, H.; Mamini, E.; Lupiya, J.; Stevenson, J.C.; Mharakurwa, S.; Chaponda, M.; Thuma, P.E.; Gwanzura, L.; Munyati, S.; et al. Malaria knowledge and bed net use in three transmission settings in southern Africa. Malar. J. 2018, 17, 41. [Google Scholar] [CrossRef]
- Vandamme, E. Concepts and Challenges in the Use of Knowledge-Attitude-Practice Surveys: Literature Review. 2009. Available online: https://www.semanticscholar.org/paper/Concepts-and-challenges-in-the-use-of-surveys%3A-Vandamme/e33554a49ddc6facc637e5f768fcb1e474efc053 (accessed on 17 December 2022).


| Characteristics | Number | Percent |
|---|---|---|
| Sex | ||
| Male | 200 | 45.4 |
| Female | 241 | 54.6 |
| Age groups(years) | ||
| 18–25 | 121 | 27.4 |
| 26–35 | 153 | 34.7 |
| 36–45 | 82 | 18.6 |
| >45 | 85 | 19.3 |
| Ethnicity | ||
| Ngalong | 80 | 18.1 |
| Sharchokpa | 146 | 33.2 |
| Lhotshampa | 180 | 40.8 |
| Khengpa | 24 | 5.4 |
| Others ethnicity | 11 | 2.5 |
| Highest level of education | ||
| Cannot read and write | 68 | 15.4 |
| MNFE * | 26 | 5.9 |
| Primary | 22 | 5.0 |
| Higher secondary | 196 | 44.4 |
| Higher education (Diploma, degree, or higher) | 129 | 29.3 |
| Occupation | ||
| Civil servant | 120 | 27.2 |
| Private/corporate/business | 129 | 29.3 |
| Homemaker | 44 | 9.9 |
| Student | 43 | 9.8 |
| Farmer | 68 | 15.4 |
| Others ** | 37 | 8.4 |
| Question Theme (%) * | Responses | N (%) |
|---|---|---|
| Transmission (59.2%) | Dirty hands | 196 (47.2) |
| Touching dirty surfaces | 125 (30.1) | |
| Spread via droplets from coughing of an infected person | 336 (81.0) | |
| Symptoms (61.4%) | Fever | 349 (86.4) |
| Dry cough | 285 (70.5) | |
| Shortness of breath | 310 (76.7) | |
| Feeling tired | 197 (48.8) | |
| Sore throat | 200 (49.5) | |
| Prevention (67.1%) | Washing hands regularly | 376 (87.4) |
| Cleaning hands with hand sanitizer | 339 (78.8) | |
| Wearing mask | 357 (83.0) | |
| Not touching face | 205 (47.5) | |
| Covering mouth when coughing | 323 (75.1) | |
| Staying home | 307 (71.4) | |
| Doing enough exercise | 126 (29.3) | |
| Avoiding going to a crowded place | 324 (75.4) | |
| Knowledge | ||
| Good knowledge | 244 (55.3%) | |
| Mean ± SD | 14.7 ± 6.5 | |
| Range (min–max) | 0–24 |
| Practice Questions | Always/ Usually (%) | |
|---|---|---|
| P1. Do you cover your mouth when sneezing or coughing? | 394 (89.8) | |
| P2. Do you wash your hands regularly? | 417 (94.6) | |
| P3. Do you use soap while you wash your hands? | 411 (93.2) | |
| P4. Do you clean your hands with a hand sanitizer? | 306 (69.4) | |
| P5. While COVID-19 is still a problem in our city, do you wear a mask when you are sick? | 383 (86.9) | |
| P6. While COVID-19 is still a problem in our city, do people in your family wear a mask at home? | 205 (46.5) | |
| P7. During the COVID-19 crisis, do people in your family wear a mask when leaving home? | 414 (93.9) | |
| Practice related to information and place of visit during COVID-19 Pandemic | ||
| P8. During the COVID-19 crisis, which websites do you usually rely on for correct information? | Prime Minister’s Office (Facebook) | 255 (57.8) |
| Ministry of Health, Bhutan (Facebook) | 253 (57.4) | |
| Information shared in social media groups | 45 (10.2) | |
| Friends, colleagues, or relatives | 62 (14.1) | |
| WHO website | 141 (32.0) | |
| P9. During the COVID-19 crisis, where do you usually go? | Hospital | 255 (57.8) |
| Market | 88 (19.9) | |
| Flu clinic | 191 (43.3) | |
| Hangout with family/friend | 31 (7.0) | |
| Have lunch, or dinner with family/friends | 36 (8.2) | |
| Do not leave the house | 156 (35.4) | |
| Practice score | N (%) | |
| Good | 369 (83.7%) | |
| Mean ± SD | 24.7 ± 4.8 | |
| Range (min–max) | 0–30 | |
| Note: Scoring system: always = 4, usually = 3, sometimes = 2, rarely = 1, never/don’t know = 0. | ||
| Characteristics | Knowledge | Attitude | Practice | ||||
|---|---|---|---|---|---|---|---|
| AOR (95% CI) | p Value | AOR (95% CI) | p Value | AOR (95% CI) | p Value | ||
| Sex | |||||||
| Male | Ref | Ref | Ref | ||||
| Female | 1.59 (0.995, 2.540) | 0.052 | 1.29 (0.835, 2.008) | 0.249 | 0.74 (0.353, 1.561) | 0.432 | |
| Age groups (years) | |||||||
| 18–25 | Ref | Ref | |||||
| 26–35 | 1.52 (0.806, 2.865) | 0.196 | 1.42 (0.785, 2.555) | 0.248 | 0.11 (0.026, 0.484) | 0.003 | |
| 36–45 | 1.06 (0.521, 2.158) | 0.871 | 1.25 (0.637, 2.449) | 0.518 | 0.27 (0.057, 1.306) | 0.104 | |
| >45 | 0.92 (0.419, 2.010) | 0.831 | 0.94 (0.441, 2.003) | 0.873 | 0.12 (0.026, 0.588) | 0.009 | |
| Ethnicity | |||||||
| Ngalong | Ref | Ref | Ref | ||||
| Sharchokpa | 1.28 (0.677, 2.436) | 0.445 | 0.50 (0.271, 0.934) | 0.029 | 0.45 (0.128, 1.601) | 0.219 | |
| Lhotshampa | 0.88 (0.477, 1.636) | 0.693 | 0.60 (0.327, 1.105) | 0.101 | 0.46 (0.136, 1.547) | 0.209 | |
| Khengpa | 0.78 (0.286, 2.118) | 0.624 | 0.70 (0.261, 1.857) | 0.469 | 1.36 (0.188, 9.810) | 0.762 | |
| Other ethnicities | 1.75 (0.336, 9.119) | 0.506 | 0.51 (0.136, 1.913) | 0.318 | 0.08 (0.010, 0.646) | 0.018 | |
| Education | |||||||
| Illiterate | Ref | Ref | Ref | ||||
| MNFE | 3.82 (1.199, 12.141) | 0.023 | 1.87 (0.569, 6.115) | 0.304 | 1.97 (0.495, 7.862) | 0.336 | |
| Primary | 1.68 (0.486, 5.781) | 0.414 | 1.98 (0.595, 6.570) | 0.266 | 4.43 (0.938, 20.922) | 0.06 | |
| Secondary | 3.50 (1.425, 8.619) | 0.006 | 3.53 (1.454, 8.555) | 0.005 | 11.50 (3.439, 38.486) | <0.001 | |
| Higher education | 9.23 (3.438, 24.797) | <0.001 | 2.97 (1.154, 7.660) | 0.024 | 12.31 (2.952, 51.318) | 0.001 | |
| Occupation | |||||||
| Civil servants | Ref | Ref | Ref | ||||
| Private/business | 0.62 (0.344, 1.124) | 0.116 | 0.96 (0.566, 1.627) | 0.879 | 8.81 (1.615, 41.455) | 0.011 | |
| Homemaker | 0.49 (0.219, 1.091) | 0.08 | 1.04 (0.488, 2.214) | 0.92 | 1.07 (0.298, 3.823) | 0.919 | |
| Student | 0.61 (0.250, 1.513) | 0.29 | 2.48 (1.010, 6.097) | 0.048 | 0.17 (0.031, 0.942) | 0.042 | |
| Others * | 0.41 (0.162, 1.011) | 0.053 | 1.24 (0.517, 2.977) | 0.63 | 0.27 (0.071, 1.011) | 0.052 | |
| Farmer | 0.32 (0.124, 0.834) | 0.02 | 0.34 (0.132, 0.869) | 0.024 | 0.32 (0.093, 1.073) | 0.065 | |
| Domain | N (%) | Correlation | |
|---|---|---|---|
| Knowledge category | Knowledge | Attitude | |
| Poor knowledge < 60% | 197 (44.7) | ||
| Good knowledge ≥ 60% | 244 (55.3) | ||
| Attitude Category | |||
| Negative attitude < 60% | 217 (49.2) | ||
| Good attitude ≥ 60% | 224 (50.8) | r = 0.228 p value < 0.001 | |
| Practice category | |||
| Poor practice < 60% | 72 (16.3) | ||
| Positive practice ≥ 60% | 369 (83.7) | r = 0.220 p value < 0.001 | r = 0.338 p value < 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gyeltshen, K.; Phuntsho, S.; Wangdi, K. Knowledge, Attitude, and Practice towards COVID-19 among Patients Attending Phuentsholing Hospital, Bhutan: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2023, 20, 2942. https://doi.org/10.3390/ijerph20042942
Gyeltshen K, Phuntsho S, Wangdi K. Knowledge, Attitude, and Practice towards COVID-19 among Patients Attending Phuentsholing Hospital, Bhutan: A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2023; 20(4):2942. https://doi.org/10.3390/ijerph20042942
Chicago/Turabian StyleGyeltshen, Kinley, Sangay Phuntsho, and Kinley Wangdi. 2023. "Knowledge, Attitude, and Practice towards COVID-19 among Patients Attending Phuentsholing Hospital, Bhutan: A Cross-Sectional Study" International Journal of Environmental Research and Public Health 20, no. 4: 2942. https://doi.org/10.3390/ijerph20042942
APA StyleGyeltshen, K., Phuntsho, S., & Wangdi, K. (2023). Knowledge, Attitude, and Practice towards COVID-19 among Patients Attending Phuentsholing Hospital, Bhutan: A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 20(4), 2942. https://doi.org/10.3390/ijerph20042942






