Central Sensitization and Chronic Pain Personality Profile: Is There New Evidence? A Case-Control Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
- Radiological and clinical diagnosis of knee OA based on the American College of Rheumatology (ACR) criteria, affecting at least one knee with a minimum of 3 months of symptom duration prior to screening.
- Male or female (nonchildbearing potential) at least 45 years old.
- A minimum of 4 out of 10 on the numerical rating scale (item 5 of Brief Pain Inventory) at screening and/or a requirement for the use of an analgesic for the knee pain.
- Clinical evidence of pain or altered sensations spread beyond the knee joint by manual palpation in the baseline rheumatologist assessment.
- At least 3 tender points in the extended version of the Arendt–Nielsen peripatellar map (excluding points 3, 7, and 8, which are part of the joint itself). A tender point is defined as a point showing a pressure pain threshold below 4 kg/cm2 [34].
- A pain score of 4 points or more in an 11-point verbal scale during a 2 s, 4 kg/cm2 pressure stimulation on the anterior surface of the tibial bone.
- Presence of temporal summation (increase of more than 1 point in an 11-point verbal scale after 10 repeated pressure stimulation at 1 s interstimulus intervals) on the most sensitive site of the peripatellar region [11].
- Diagnosis of FM following the ACR criteria [34].
- History of widespread nonarticular pain with insidious onset primary over 3 months.
- One year minimum of disease evolution.
- Absence of comorbid chronic fatigue syndrome.
- No history of rheumatic disorder, no history of functional pain or physical widespread pain.
- No history of Axis I or II psychiatric illness and no history of neurological disease.
2.2. Procedure
2.3. Assessment
- Novelty-seeking (NS), defined as the inclination to respond impulsively to novel stimuli with active avoidance of frustration.
- Harm-avoidance (HA) as the tendency to inhibit responses to aversive stimuli leading to avoidance of punishment.
- Reward dependence (RD) as the predisposition to answer to signals of reward.
- Persistence (PS) as the tendency to perseverance despite frustration and fatigue.
- Self-directedness (SD), which refers to the ability to control, regulate, and adapt behavior to fit the situation.
- Cooperativeness (CO), which is related to acceptance of other people.
- Self-transcendence (ST), which is viewed as the identification with everything conceived as essential and consequential parts of a unified whole.
- Exploratory excitability (NS1), impulsiveness (NS2), extravagance (NS3), and disorderliness (NS4).
- HA: Anticipatory worry (HA1), fear of uncertainty (HA2), shyness with strangers (HA3), and fatigability (HA4).
- RD: Sentimentality (RD1), openness to warm (RD2), attachment (RD3), and dependence (RD4).
- PS: Eagerness of effort (PS1), work-hardened (PS2), ambitious (PS3), and perfectionist (PS4).
- Responsibility (SD1), purposefulness (SD2), resourcefulness (SD3), self-acceptance (SD4), and enlightened second nature (SD5).
- CO: Social acceptance (C1), empathy (C2), helpfulness (C3), compassion (C4), pure-hearted conscience (C5).
- ST: Self-forgetful (ST1), transpersonal identification (ST2), and spiritual acceptance (ST3).
2.4. Data Analysis
3. Results
OA Patients versus Controls and FM Patients versus OA-noCS Patients
4. Discussion
- The sample size is small, especially for the OA-CS group. Given the size of the sample, we were not able to carry out an analysis that differentiates between gender and age.
- External validity is limited by the sample size, even though the sample is very specific and restrictive, with the inclusion/exclusion criteria. For example, FM patients showed no chronic fatigue, which is a very common characteristic.
- The FM group was not divided into potential subgroups of patients according to severity; for example, there are few studies that show evidence in this field. Thus, it is complicated to find previous studies to compare our results with others.
- The effects of other symptoms of central sensitization that may be present in these patients, such as migraine, irritable bowel syndrome, or low back pain, have not been studied in OA groups due to the small sample size.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Friedman, H.S.; Kern, M.L. Personality, well-being, and health. Annu. Rev. Psychol. 2014, 65, 719–742. [Google Scholar] [CrossRef]
- Nave, C.S. Long-Term Stability of Personality: Implications for Behavior. UC Riverside. 2011. Available online: https://escholarship.org/uc/item/5t79c15j (accessed on 26 September 2020).
- Weston, S.J.; Jackson, J.J. Identification of the healthy neurotic: Personality traits predict smoking after disease onset. J. Res. Personal. 2015, 54, 61–69. [Google Scholar] [CrossRef]
- Giurea, A.; Fraberger, G.; Kolbitsch, P.; Lass, R.; Schneider, E.; Kubista, B.; Windhager, R. The Impact of Personality Traits on the Outcome of Total Knee Arthroplasty. BioMed Res. Int. 2016, 2016, 5282160. [Google Scholar] [CrossRef]
- Van der Steeg, A.F.W.; De Vries, J.; van der Ent, F.W.C.; Roukema, J.A. Personality predicts quality of life six months after the diagnosis and treatment of breast disease. Ann. Surg. Oncol. 2007, 14, 678–685. [Google Scholar] [CrossRef]
- WHO. Chronic Rheumatic Conditions. World Health Organization. Available online: http://www.who.int/chp/topics/rheumatic/en/ (accessed on 26 September 2020).
- NFA. Fibromyalgia Prevalence. 2019. Available online: https://fmaware.net/fibromyalgia-prevalence/ (accessed on 26 September 2020).
- Woolf, C.J. Central sensitization: Implications for the diagnosis and treatment of pain. Pain 2011, 152, S2–S15. [Google Scholar] [CrossRef]
- Arendt-Nielsen, L.; Graven-Nielsen, T. Central sensitization in fibromyalgia and other musculoskeletal disorders. Curr. Pain Headache Rep. 2003, 7, 355–361. [Google Scholar] [CrossRef]
- Staud, R.; Smitherman, M.L. Peripheral and central sensitization in fibromyalgia: Pathogenetic role. Curr. Pain Headache Rep. 2002, 6, 259–266. [Google Scholar] [CrossRef]
- Siracusa, R.; Paola, R.D.; Cuzzocrea, S.; Impellizzeri, D. Fibromyalgia: Pathogenesis, mechanisms, diagnosis and treatment options update. Int. J. Mol. Sci. 2021, 22, 3891. [Google Scholar] [CrossRef]
- Arendt-Nielsen, L.; Nie, H.; Laursen, M.B.; Laursen, B.S.; Madeleine, P.; Simonsen, O.H.; Graven-Nielsen, T. Sensitization in patients with painful knee osteoarthritis. Pain 2010, 149, 573–581. [Google Scholar] [CrossRef]
- Lluch, E.; Torres, R.; Nijs, J.; Van Oosterwijck, J. Evidence for central sensitization in patients with osteoarthritis pain: A systematic literature review. Eur. J. Pain 2014, 18, 1367–1375. [Google Scholar] [CrossRef]
- O’Neill, T.W.; Felson, D.T. Mechanisms of Osteoarthritis (OA) Pain. Curr. Osteoporos. Rep. 2018, 16, 611–616. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Fontanals, A.; Portell, M.; García-Blanco, S.; Poca-Dias, V.; García-Fructuoso, F.; López-Ruiz, M.; Gutiérrez-Rosado, T.; Gomà-i-Freixanet, M.; Deus, J. Vulnerability to psychopathology and dimensions of personality in patients with fibromyalgia. Clin. J. Pain 2017, 33, 991–997. [Google Scholar] [CrossRef] [PubMed]
- Yunus, M.B.; Ahles, T.A.; Aldag, J.C.; Masi, A.T. Relationship of clinical features with psychological status in primary fibromyalgia. Arthritis Rheumatol. 1991, 34, 15–21. [Google Scholar] [CrossRef]
- Garcia-Fontanals, A.; García-Blanco, S.; Portell, M.; Pujol, J.; Poca-Dias, V.; García-Fructuoso, F.; López-Ruiz, M.; Gutiérrez-Rosado, T.; Gomà-i-Freixanet, M.; Deus, J. Cloninger’s psychobiological model of personality and psychological distress in fibromyalgia. Int. J. Rheum. Dis. 2016, 19, 852–863. [Google Scholar] [CrossRef]
- Gencay-Can, A.; Can, S.S. Temperament and character profile of patients with fibromyalgia. Rheumatol. Int. 2012, 32, 3957–3961. [Google Scholar] [CrossRef]
- Leombruni, P.; Zizzi, F.; Miniotti, M.; Colonna, F.; Castelli, L.; Fusaro, E.; Torta, R. Harm avoidance and self-directedness characterize fibromyalgic patients and the symptom severity. Front. Psychol. 2016, 7, 579. [Google Scholar] [CrossRef]
- Galvez-Sánchez, C.M.; Duschek, S.; Reyes del Paso, G.A. Psychological impact of fibromyalgia: Current perspectives. Psychol. Res. Behav. Manag. 2019, 12, 117–127. [Google Scholar] [CrossRef]
- Conrad, R.; Wegener, I.; Geiser, F.; Kleiman, A. Temperament, character, and personality disorders in chronic pain. Curr. Pain Headache Rep. 2013, 17, 318. [Google Scholar] [CrossRef]
- Gong, L.; Dong, J.-Y. Patient’s personality predicts recovery after total knee arthroplasty: A retrospective study. J. Orthop. Sci. 2014, 19, 263–269. [Google Scholar] [CrossRef]
- ÇiDem, M.; Rezvanï, A.; Karacan, İ. Assessment of Affective Temperament in Knee Osteoarthritis Patients and Its Effects on Physical Therapy Response. Turk. Klin. J. Med. Sci. 2011, 31, 1372–1376. [Google Scholar] [CrossRef]
- Malmgren-Olsson, E.-B.; Bergdahl, J. Temperament and character personality dimensions in patients with nonspecific musculoskeletal disorders. Clin. J. Pain 2006, 22, 625–631. [Google Scholar] [CrossRef]
- Naylor, B.; Boag, S.; Gustin, S.M. New evidence for a pain personality? A critical review of the last 120 years of pain and personality. Scand. J. Pain 2017, 17, 58–67. [Google Scholar] [CrossRef]
- Weisberg, J.N. Personality and personality disorders in chronic pain. Curr. Rev. Pain 2000, 4, 60–70. [Google Scholar] [CrossRef]
- Timmermans, G.; Sternbach, R.A. Factors of human chronic pain: An analysis of personality and pain reaction variables. Science 1974, 184, 806–808. [Google Scholar] [CrossRef]
- Cloninger, C.R.; Przybeck, T.R.; Svrakic, D.M. The Temperament and Character Inventory-Revised; Washington University: St. Louis, MO, USA, 1999. [Google Scholar]
- Gutierrez-Zotes, A.; Labad, J.; Martorell, L.; Gaviria, A.; Bayón, C.; Vilella, E.; Cloninger, C.R. The revised Temperament and Character Inventory: Normative data by sex and age from a Spanish normal randomized sample. PeerJ 2015, 3, e1481. [Google Scholar] [CrossRef]
- Komasi, S.; Rezaei, F.; Hemmati, A.; Rahmani, K.; Amianto, F.; Miettunen, J. Comprehensive meta-analysis of associations between temperament and character traits in Cloninger’s psychobiological theory and mental disorders. J. Int. Med. Res. 2022, 50, 3000605211070766. [Google Scholar] [CrossRef]
- Graven-Nielsen, T.; Arendt-Nielsen, L. Assessment of mechanisms in localized and widespread musculoskeletal pain. Nat. Rev. Rheumatol. 2010, 6, 599–606. [Google Scholar] [CrossRef]
- Imamura, M.; Imamura, S.T.; Kaziyama, H.H.S.; Targino, R.A.; Hsing, W.T.; de Souza, L.P.M.; Cutait, M.M.; Fregni, F.; Camanho, G.L. Impact of nervous system hyperalgesia on pain, disability, and quality of life in patients with knee osteoarthritis: A controlled analysis. Arthritis. Rheumatol. 2008, 59, 1424–1431. [Google Scholar] [CrossRef]
- Nijs, J.; Van Houdenhove, B.; Oostendorp, R.A.B. Recognition of central sensitization in patients with musculoskeletal pain: Application of pain neurophysiology in manual therapy practice. Man. Ther. 2010, 15, 135–141. [Google Scholar] [CrossRef]
- Wolfe, F.; Smythe, H.A.; Yunus, M.B.; Bennett, R.M.; Bombardier, C.; Goldenberg, D.L.; Tugwell, P.; Campbell, S.M.; Abeles, M.; Clark, P.; et al. The American College of Rheumatology 1990 criteria for the classification of fibromyalgia. report of the multicenter criteria committee. Arthritis Rheumatol. 1990, 33, 160–172. [Google Scholar] [CrossRef]
- Torres, X.; Bailles, E.; Valdes, M.; Gutierrez, F.; Peri, J.-M.; Arias, A.; Gomez, E.; Collado, A. Personality does not distinguish people with fibromyalgia but identifies subgroups of patients. Gen. Hosp. Psychiatry 2013, 35, 640–648. [Google Scholar] [CrossRef]
- Fisher, E.; Law, E.; Dudeney, J.; Palermo, T.M.; Stewart, G.; Eccleston, C. Psychological therapies for the management of chronic and recurrent pain in children and adolescents. Cochrane Database Syst. Rev. 2018, 9, CD003968. [Google Scholar] [CrossRef]
- Zhou, M. The role of personality in patients with knee Osteoarthritis. Arthritis Rheumatol. 2018, 70 (Suppl. S10), 1360. [Google Scholar]
- Clark, J.R.; Nijs, J.; Smart, K.; Holmes, P.; Yeowell, G.; Goodwin, P.C. Prevalence of extreme trait sensory profiles and personality types in nonspecific chronic low back pain with predominant central sensitization: Secondary analysis of an international observational study. Pain Physician 2019, 22, E181–E190. [Google Scholar] [CrossRef]
- San-Antolín, M.; Rodríguez-Sanz, D.; Becerro-de-Bengoa-Vallejo, R.; Losa-Iglesias, M.E.; Casado-Hernández, I.; López-López, D.; Calvo-Lobo, C. Central sensitization and catastrophism symptoms are associated with chronic myofascial pain in the gastrocnemius of athletes. Pain Med. 2020, 21, 1616–1625. [Google Scholar] [CrossRef]

| Groups | |||||
|---|---|---|---|---|---|
| Factors | OA | OA-CS | OA-noCS | FM | Control |
| N | 46 | 15 | 31 | 47 | 22 |
| Gender (women %) | 71.7 | 84.2 | 65.9 | 100 | 59.3 |
| Age ((SD)) | 66.67 (7.78) | 66.37 (8.77) | 66.8 (7.39) | 46.47 (7.92) | 62.92 (7.39) |
| Months after diagnosis ( ± SD) | 55.28 (63.34) | 50.58 (54.09) | 57.46 (67.71) | 84.38 (54.14) | - |
| Educational level (%) | |||||
| Uneducated | 6.7 | 10.5 | 4.9 | 0 | 0 |
| Primary education | 21.7 | 26.3 | 19.5 | 10.6 | 26.9 |
| Secondary education | 15 | 10.6 | 17.1 | 21.3 | 12.1 |
| General education | 5 | 10.5 | 2.4 | 12.8 | 7.4 |
| Vocational education and training and/or Higher education | 31.7 | 36.8 | 29.3 | 17 | 30.6 |
| Bachelor and/or University Degree | 20 | 5.3 | 26.8 | 38.3 | 23 |
| Drug use (%) | |||||
| Painkiller | 50 | 16 | 34 | 16 | 0 |
| Non-steroidal Anti-inflammatory drugs (NSAIDs) | 51 | 16 | 35 | 17 | 2 |
| Antiepileptic drugs | 2 | 0 | 2 | 4 | 3 |
| Antidepressant drugs | 14.9 | 15.8 | 19.5 | 85.7 | 7.4 |
| Questionnaires | |||||
| FIQ | - | - | 65.99 (14.01) | - | |
| Mini-Mental: 27.61 (2.68) | 26.82 (3.17) | 28 (2.36) | - | 27.5 (2.45) | |
| Group | ||||||
|---|---|---|---|---|---|---|
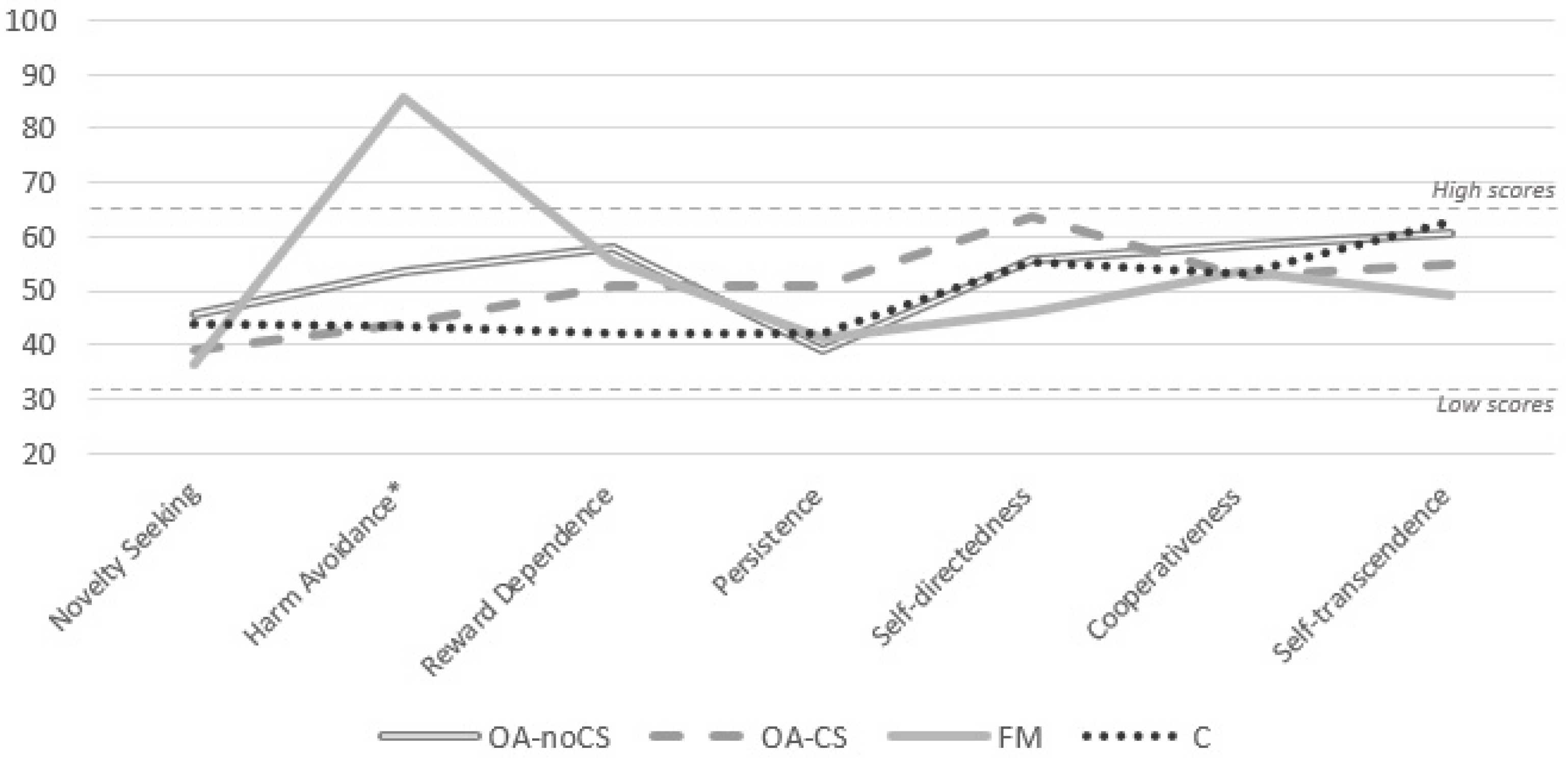
| TCI-R Dimensions | OA-noCS (n = 15) Mean (SD) | OA-CS (n = 31) Mean (SD) | FM (n = 47) Mean (SD) | C (n = 22) Mean (SD) | K–W Test p | Cronbach’s Alpha |
| Novelty-seeking | 45.58 (27.53) | 39.00 (29.25) | 36.21 (22.33) | 43.68 (24.25) | 0.379 | 0.43 |
| Harm-avoidance * | 53.61 (30.30) | 43.80 (30.44) | 85.85 (15.17) | 43.27 (30.29) | <0.001 * | 0.77 |
| Reward dependence | 57.94 (22.80) | 51.13 (24.62) | 55.15 (27.89) | 42.09 (32.94) | 0.227 | 0.64 |
| Persistence | 39.03 (28.15) | 50.8 (32.94) | 41.13 (30.58) | 42.05 (26.07) | 0.675 | 0.77 |
| Self-directedness | 55.71 (28.03) | 63.67 (31.40) | 45.98 (30.27) | 55.36 (29.63) | 0.178 | 0.74 |
| Cooperativeness | 58.55 (30.84) | 52.87 (32.39) | 53.74 (27.88) | 52.95 (29.05) | 0.817 | 0.71 |
| Self-transcendence | 60.71 (30.03) | 54.87 (35.32) | 49.26 (30.07) | 62.91 (32.82) | 0.275 | 0.78 |
| Group | |||||
|---|---|---|---|---|---|
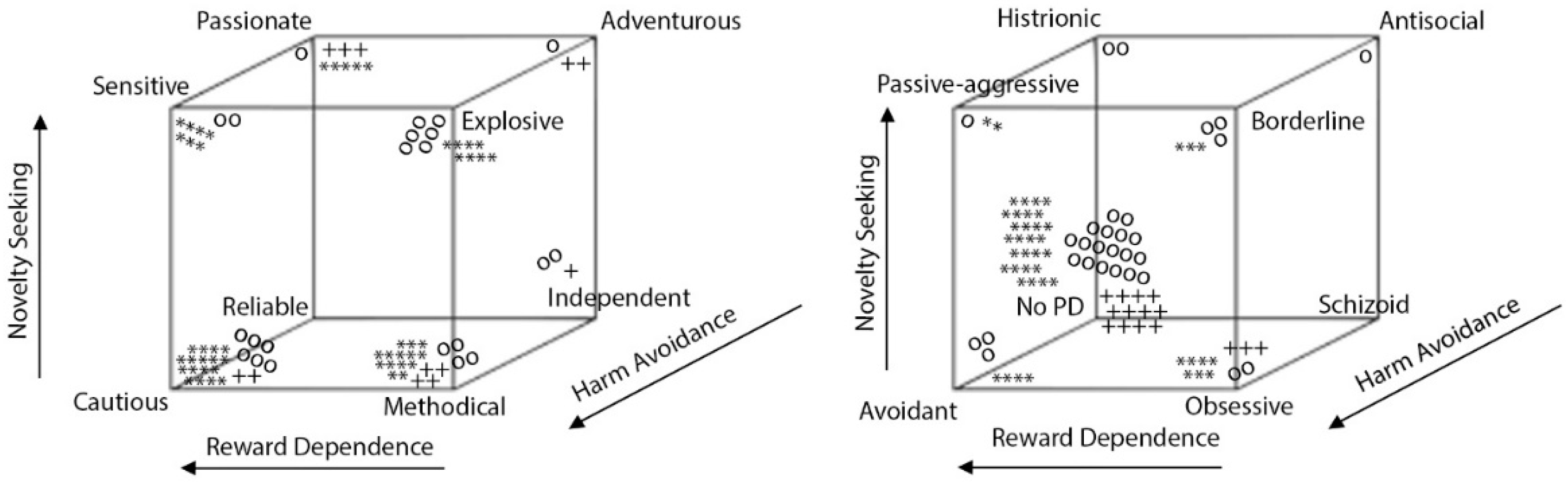
| TCI-R Temperamental Profile | OA (n = 46) n (%) | OA-CS (n = 15) n (%) | OA-noCS (n = 31) n (%) | FM (n = 47) n (%) | C (n = 22) n (%) |
| Methodical | 8 (17.4) | 4 (26.7) | 4 (12.9) | 14 (29.8) | 3 (13.6) |
| Cautious | 8 (17.4) | 2 (13.3) | 6 (19.4) | 17 (36.2) | 3 (13.6) |
| Explosive | 6 (13) | 0 | 6 (19.4) | 8 (17.0) | 2 (9.1) |
| Sensitive | 2 (4.3) | 0 | 2 (6.5) | 7 (14.9) | 1 (4.5) |
| Passionate | 8 (17.4) | 3 (20) | 5 (16.1) | 1 (2.1) | 4 (18.2) |
| Independent | 3 (6.5) | 1 (6.7) | 2 (6.5) | 0 | 8 (36.4) |
| Adventurous | 3 (6.5) | 2 (13.3) | 1 (3.2) | 0 | 0 |
| Reliable | 8 (17.4) | 3 (20) | 5 (16.1) | 0 | 1 (4.5) |
| Chi-square = 61.116, p < 0.001. | |||||
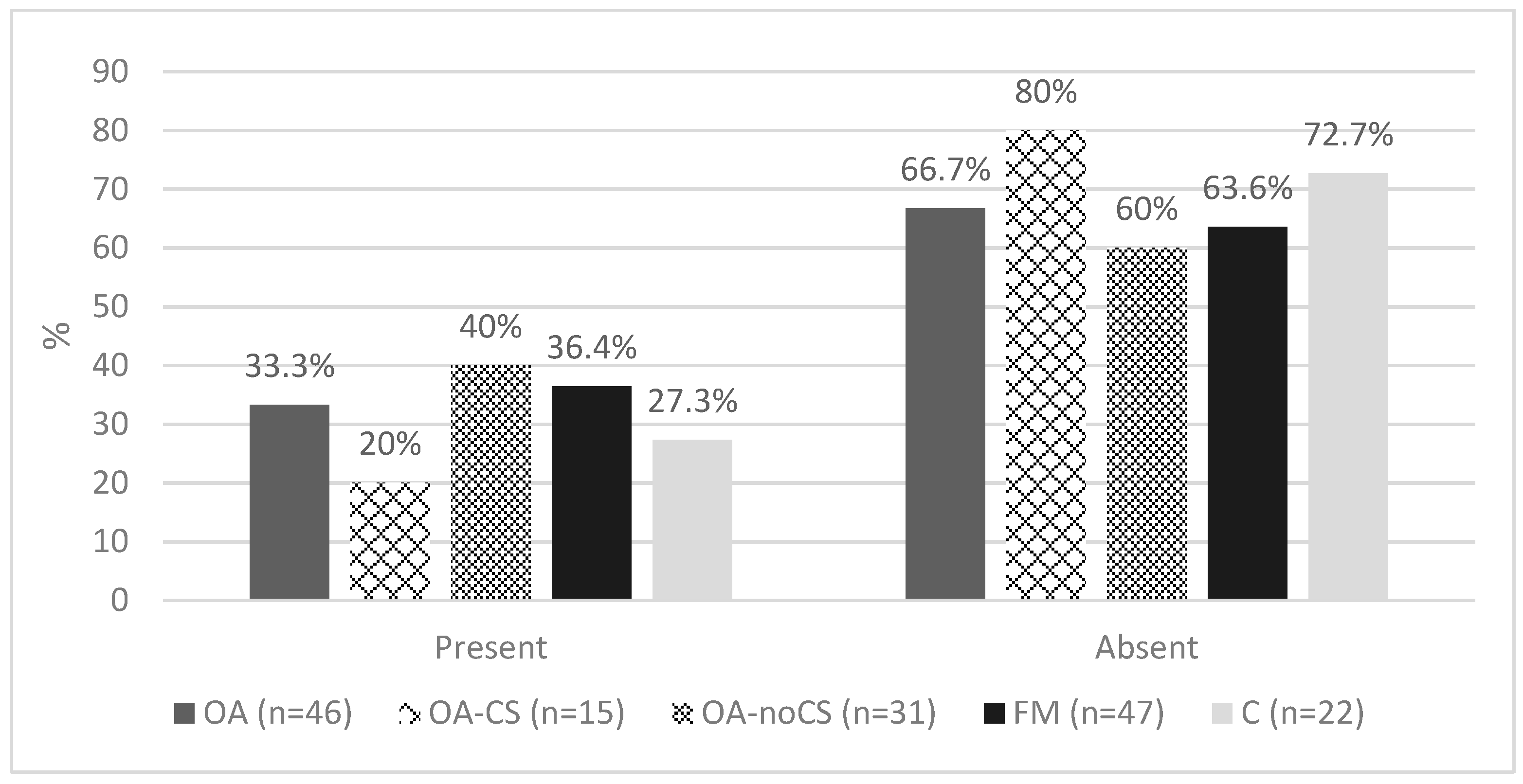
| TCI-R Personality Disorders | OA (n = 46) n(%) | OA-CS (n = 15) n(%) | OA-noCS (n = 31) n(%) | FM (n = 47) n(%) | C (n = 22) n(%) |
| Absent | 30 (66.7) | 12 (80) | 18 (60) | 28 (63.6) | 16 (72.7) |
| Obsessive | 5 (11.1) | 3 (20) | 2 (6.7) | 7 (15.9) | 1 (4.5) |
| Avoidant | 3 (6.7) | 0 | 3 (10) | 4 (9.1) | 0 |
| Borderline | 3 (6.7) | 0 | 3 (10) | 3 (6.8) | 2 (9.1) |
| Passive–aggressive | 1 (2.2) | 0 | 1 (3.3) | 2 (4.5) | 0 |
| Histrionic | 2 (4.4) | 0 | 2 (6.7) | 0 | 0 |
| Antisocial | 1 (2.2) | 0 | 1 (3.3) | 0 | 3 (13.6) |
| Chi-square = 24.261, p = 0.147 | |||||
| OA vs. C | |||
|---|---|---|---|
| ORadj (95% CI) | (ORadj − 1) × 100 | p | |
| Reward Dependence (RD) | 1.079 (1.079–1.153) | 7.9% (7.9–15.3%) | 0.024 |
| FM vs. OA-noCS | |||
| ORadj (95% CI) | (ORadj − 1) × 100 | p | |
| Harm Avoidance (HA) | 1.332 (1.042–1.702) | 33.2% (4.2–70.2%) | 0.022 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lopez-Ruiz, M.; Doreste Soler, A.; Pujol, J.; Losilla, J.-M.; Ojeda, F.; Blanco-Hinojo, L.; Martínez-Vilavella, G.; Gutiérrez-Rosado, T.; Monfort, J.; Deus, J. Central Sensitization and Chronic Pain Personality Profile: Is There New Evidence? A Case-Control Study. Int. J. Environ. Res. Public Health 2023, 20, 2935. https://doi.org/10.3390/ijerph20042935
Lopez-Ruiz M, Doreste Soler A, Pujol J, Losilla J-M, Ojeda F, Blanco-Hinojo L, Martínez-Vilavella G, Gutiérrez-Rosado T, Monfort J, Deus J. Central Sensitization and Chronic Pain Personality Profile: Is There New Evidence? A Case-Control Study. International Journal of Environmental Research and Public Health. 2023; 20(4):2935. https://doi.org/10.3390/ijerph20042935
Chicago/Turabian StyleLopez-Ruiz, Marina, Andrea Doreste Soler, Jesus Pujol, Josep-Maria Losilla, Fabiola Ojeda, Laura Blanco-Hinojo, Gerard Martínez-Vilavella, Teresa Gutiérrez-Rosado, Jordi Monfort, and Joan Deus. 2023. "Central Sensitization and Chronic Pain Personality Profile: Is There New Evidence? A Case-Control Study" International Journal of Environmental Research and Public Health 20, no. 4: 2935. https://doi.org/10.3390/ijerph20042935
APA StyleLopez-Ruiz, M., Doreste Soler, A., Pujol, J., Losilla, J.-M., Ojeda, F., Blanco-Hinojo, L., Martínez-Vilavella, G., Gutiérrez-Rosado, T., Monfort, J., & Deus, J. (2023). Central Sensitization and Chronic Pain Personality Profile: Is There New Evidence? A Case-Control Study. International Journal of Environmental Research and Public Health, 20(4), 2935. https://doi.org/10.3390/ijerph20042935








