Circadian and Seasonal Pattern of Arrhythmic Events in Arrhythmogenic Cardiomyopathy Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population and Clinical Assessment
2.2. Statistical Analysis
3. Results
3.1. Study Population
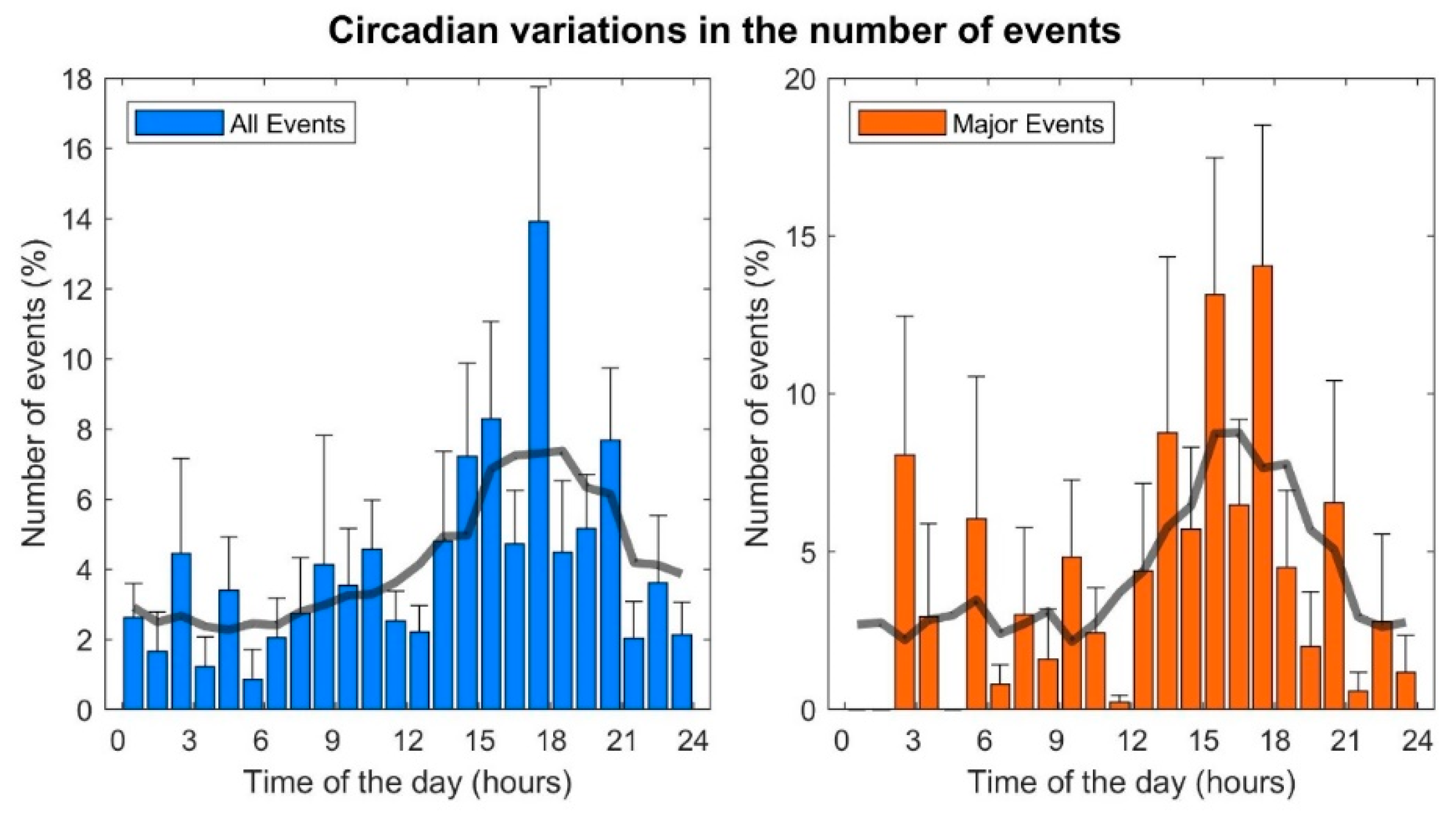
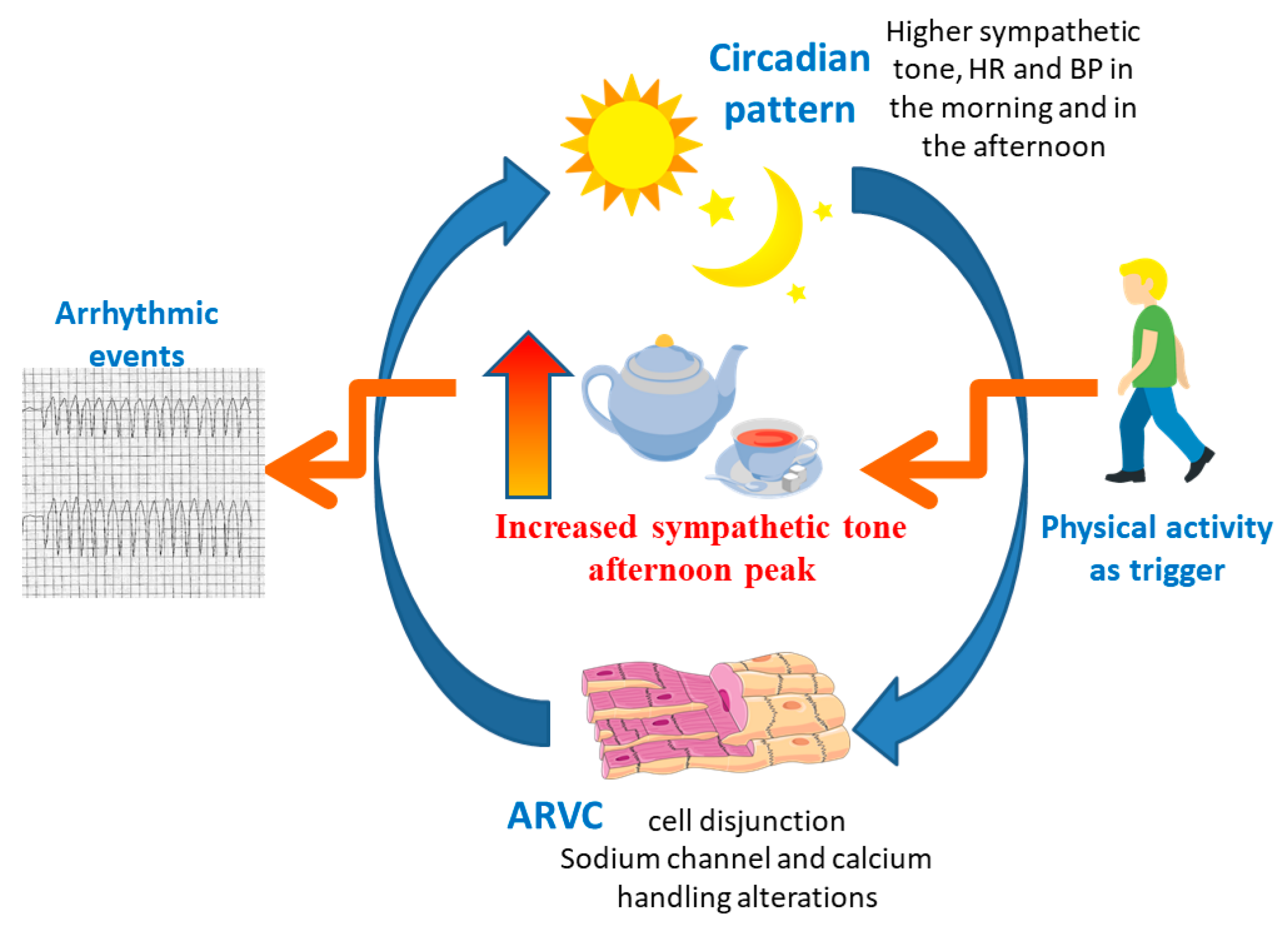
3.2. Circadian Pattern
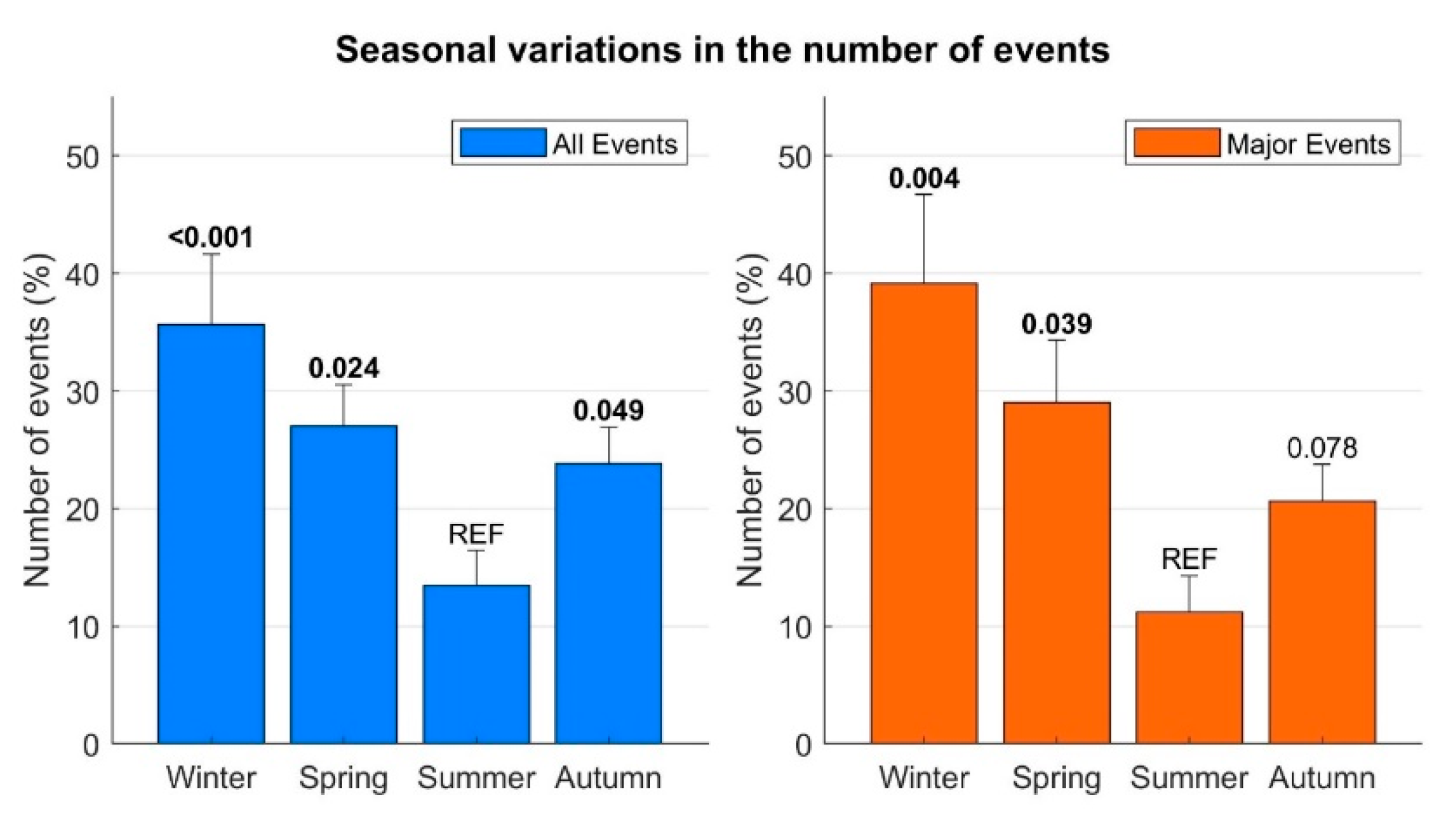
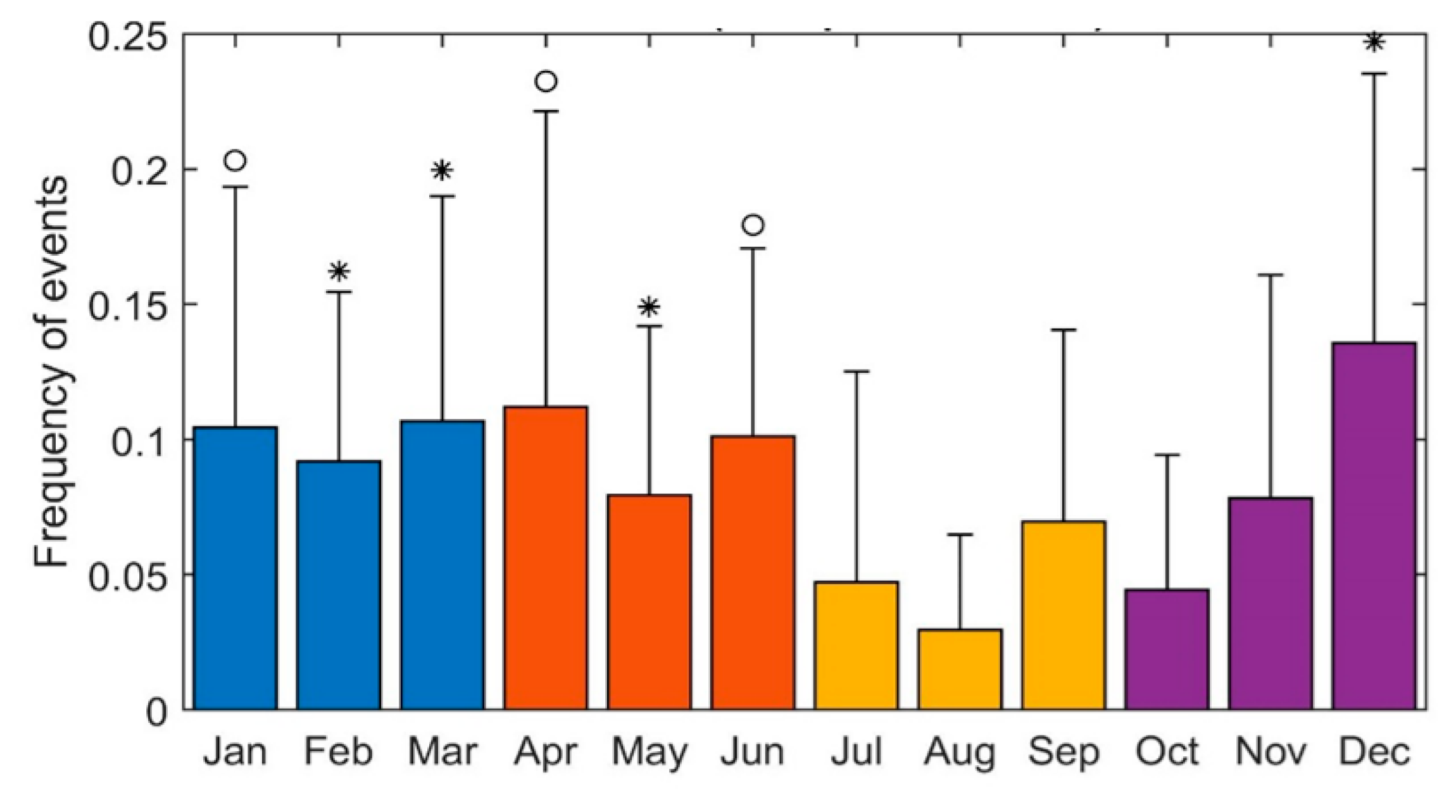
3.3. Seasonal Variation
4. Discussion
4.1. Circadian and Seasonal Determinants of Biological Internal Clocks
- Arrhythmic events in ARVC are significantly more frequent in the afternoon, around 6 pm;
- Arrhythmic events occur more frequently during the winter and less frequently in the summer.
4.2. Circadian Distribution of the Arrhythmic Events in ARVC
4.3. Seasonal Distribution of the Arrhythmic Events in ARVC Patients
4.4. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Marcus, F.I.; McKenna, W.J.; Sherrill, D.; Basso, C.; Bauce, B.; Bluemke, D.A.; Calkins, H.; Corrado, D.; Cox, M.G.; Daubert, J.P.; et al. Diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia: Proposed Modification of the Task Force Criteria. Eur. Heart J. 2010, 31, 806–814. [Google Scholar] [CrossRef]
- Tabib, A.; Miras, A.; Taniere, P.; Loire, R. Undetected cardiac lesions cause unexpected sudden cardiac death during occasional sport activity. A report of 80 cases A report on 80 cases. Eur. Heart J. 1999, 20, 900–903. [Google Scholar] [CrossRef] [PubMed]
- Ruwald, A.-C.; Marcus, F.; Estes, N.M.; Link, M.; McNitt, S.; Polonsky, B.; Calkins, H.; Towbin, J.A.; Moss, A.J.; Zareba, W. Association of competitive and recreational sport participation with cardiac events in patients with arrhythmogenic right ventricular cardiomyopathy: Results from the North American multidisciplinary study of arrhythmogenic right ventricular cardiomyopathy. Eur. Heart J. 2015, 36, 1735–1743. [Google Scholar] [CrossRef]
- Chung, F.-P.; Li, H.-R.; Chong, E.; Pan, C.-H.; Lin, Y.-J.; Chang, S.-L.; Lo, L.-W.; Hu, Y.-F.; Tuan, T.-C.; Chao, T.-F.; et al. Seasonal variation in the frequency of sudden cardiac death and ventricular tachyarrhythmia in patients with arrhythmogenic right ventricular dysplasia/cardiomyopathy: The effect of meteorological factors. Heart Rhythm 2013, 10, 1859–1866. [Google Scholar] [CrossRef]
- Anand, K.; Aryana, A.; Cloutier, D.; Hee, T.; Esterbrooks, D.; Mooss, A.N.; Mohiuddin, S.M. Circadian, Daily, and Seasonal Distributions of Ventricular Tachyarrhythmias in Patients With Implantable Cardioverter-Defibrillators. Am. J. Cardiol. 2007, 100, 1134–1138. [Google Scholar] [CrossRef]
- Müller, D.; Lampe, F.; Wegscheider, K.; Schultheiss, H.-P.; Behrens, S. Annual distribution of ventricular tachycardias and ventricular fibrillation. Am. Heart J. 2003, 146, 1061–1065. [Google Scholar] [CrossRef] [PubMed]
- Willich, S.N.; Levy, D.; Rocco, M.B.; Tofler, G.H.; Stone, P.H.; Muller, J.E. Circadian variation in the incidence of sudden cardiac death in the framingham heart study population. Am. J. Cardiol. 1987, 60, 801–806. [Google Scholar] [CrossRef]
- Muller, E.J.; Ludmer, P.L.; Willich, S.N.; Tofler, G.H.; Aylmer, G.; Klangos, I.; Stone, P.H. Circadian variation in the frequency of sudden cardiac death. Circulation 1987, 75, 131–138. [Google Scholar] [CrossRef]
- Kiernan, T.J.; Weivoda, P.L.; Somers, V.K.; Ommen, S.R.; Gersh, B.J. Circadian Rhythm of Appropriate Implantable Cardioverter Defibrillator Discharges in Patients with Hypertrophic Cardiomyopathy. Pacing Clin. Electrophysiol. 2008, 31, 1253–1258. [Google Scholar] [CrossRef]
- Maron, B.J.; Semsarian, C.; Shen, W.-K.; Link, M.S.; Epstein, A.E.; Estes, N.M.; Almquist, A.; Giudici, M.C.; Haas, T.S.; Hodges, J.S.; et al. Circadian patterns in the occurrence of malignant ventricular tachyarrhythmias triggering defibrillator interventions in patients with hypertrophic cardiomyopathy. Heart Rhythm 2009, 6, 599–602. [Google Scholar] [CrossRef] [PubMed]
- O’Mahony, C.; Lambiase, P.D.; Rahman, S.M.; Cardona, M.; Calcagnino, M.; Quarta, G.; Tsovolas, K.; Al-Shaikh, S.; McKenna, W.; Elliott, P. The relation of ventricular arrhythmia electrophysiological characteristics to cardiac phenotype and circadian patterns in hypertrophic cardiomyopathy. Europace 2011, 14, 724–733. [Google Scholar] [CrossRef]
- Corrado, D.; Perazzolo Marra, M.; Zorzi, A.; Beffagna, G.; Cipriani, A.; Lazzari, M.; Migliore, F.; Pilichou, K.; Rampazzo, A.; Rigato, I.; et al. Diagnosis of arrhythmogenic cardiomyopathy: The Padua criteria. Int. J. Cardiol. 2020, 319, 106–114. [Google Scholar] [CrossRef]
- Towbin, J.A.; McKenna, W.J.; Abrams, D.; Ackerman, M.J.; Calkins, H.; Darrieux, F.; Daubert, J.P.; De Chillou, C.; DePasquale, E.C.; Desai, M.Y.; et al. 2019 HRS expert consensus statement on evaluation, risk stratification, and management of arrhythmogenic cardiomyopathy. Heart Rhythm 2019, 16, e301–e372. [Google Scholar] [CrossRef]
- Vischer, A.S.; Castelletti, S.; Syrris, P.; Bastiaenen, R.; Miles, C.; Akdis, D.; Denhaerynck, K.; Jacoby, D.; Saguner, A.M.; Krahn, A.D.; et al. Risk score for the exclusion of arrhythmic events in arrhythmogenic right ventricular cardiomyopathy at first presentation. Int. J. Cardiol. 2019, 290, 100–105. [Google Scholar] [CrossRef] [PubMed]
- Castelletti, S.; Vischer, A.S.; Syrris, P.; Crotti, L.; Spazzolini, C.; Ghidoni, A.; Parati, G.; Jenkins, S.; Kotta, M.-C.; McKenna, W.J.; et al. Desmoplakin missense and non-missense mutations in arrhythmogenic right ventricular cardiomyopathy: Genotype-phenotype correlation. Int. J. Cardiol. 2017, 249, 268–273. [Google Scholar] [CrossRef] [PubMed]
- Lang, R.M.; Badano, L.P.; Mor-Avi, V.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.A.; Foster, E.; Goldstein, S.A.; Kuznetsova, T.; et al. Recommendations for Cardiac Chamber Quantification by Echocardiography in Adults: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. 2015, 16, 233–271. [Google Scholar] [CrossRef]
- Chellappa, S.; Vujovic, N.; Williams, J.S.; Scheer, F.A. Impact of Circadian Disruption on Cardiovascular Function and Disease. Trends Endocrinol. Metab. 2019, 30, 767–779. [Google Scholar] [CrossRef]
- Rubart, M. Mechanisms of sudden cardiac death. J. Clin. Investig. 2005, 115, 2305–2315. [Google Scholar] [CrossRef] [PubMed]
- Rana, S.; Prabhu, S.D.; Young, M.E. Chronobiological Influence Over Cardiovascular Function. Circ. Res. 2020, 126, 258–279. [Google Scholar] [CrossRef]
- Takigawa, M.; Noda, T.; Shimizu, W.; Miyamoto, K.; Okamura, H.; Satomi, K.; Suyama, K.; Aihara, N.; Kamakura, S.; Kurita, T. Seasonal and circadian distributions of ventricular fibrillation in patients with Brugada syndrome. Heart Rhythm 2008, 5, 1523–1527. [Google Scholar] [CrossRef]
- Miyake, C.Y.; Asaki, S.Y.; Webster, G.; Czosek, R.J.; Atallah, J.; Avasarala, K.; Rao, S.O.; Thomas, P.E.; Kim, J.J.; Valdes, S.O.; et al. Circadian Variation of Ventricular Arrhythmias in Catecholaminergic Polymorphic Ventricular Tachycardia. JACC Clin. Electrophysiol. 2017, 3, 1308–1317. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.-H.; Nam, G.-B.; Baek, S.; Choi, H.O.; Kim, K.H.; Choi, K.-J.; Joung, B.; Pak, H.-N.; Lee, M.-H.; Kim, S.S.; et al. Circadian and Seasonal Variations of Ventricular Tachyarrhythmias in Patients with Early Repolarization Syndrome and Brugada Syndrome: Analysis of Patients with Implantable Cardioverter Defibrillator. J. Cardiovasc. Electrophysiol. 2012, 23, 757–763. [Google Scholar] [CrossRef] [PubMed]
- Elliott, P.M.; Anastasakis, A.; Asimaki, A.; Basso, C.; Bauce, B.; Brooke, M.A.; Calkins, H.; Corrado, D.; Duru, F.; Green, K.J.; et al. Definition and treatment of arrhythmogenic cardiomyopathy: An updated expert panel report. Eur. J. Heart Fail. 2019, 21, 955–964. [Google Scholar] [CrossRef]
- Mayosi, B.M.; Fish, M.; Shaboodien, G.; Mastantuono, E.; Kraus, S.; Wieland, T.; Kotta, M.-C.; Chin, A.; Laing, N.; Ntusi, N.B.; et al. Identification of Cadherin 2 (CDH2) Mutations in Arrhythmogenic Right Ventricular Cardiomyopathy. Circ. Cardiovasc. Genet. 2017, 10, e001605. [Google Scholar] [CrossRef] [PubMed]
- McKenna, W.J.; Caforio, A.L. Myocardial Inflammation and Sudden Death in the Inherited Cardiomyopathies. Can. J. Cardiol. 2022, 38, 427–438. [Google Scholar] [CrossRef] [PubMed]
- Cerrone, M.; Remme, C.A.; Tadros, R.; Bezzina, C.R.; Delmar, M. Beyond the One Gene–One Disease Paradigm. Circulation 2019, 140, 595–610. [Google Scholar] [CrossRef]
- van Opbergen, C.J.M.; Delmar, M.; van Veen, T.A.B. Potential new mechanisms of pro-arrhythmia in arrhythmogenic cardiomyopathy: Focus on calcium sensitive pathways. Neth. Heart J. 2017, 25, 157–169. [Google Scholar] [CrossRef]
- Paul, M.; Wichter, T.; Kies, P.; Gerss, J.; Wollmann, C.; Rahbar, K.; Eckardt, L.; Breithardt, G.; Schober, O.; Schulze-Bahr, E.; et al. Cardiac Sympathetic Dysfunction in Genotyped Patients with Arrhythmogenic Right Ventricular Cardiomyopathy and Risk of Recurrent Ventricular Tachyarrhythmias. J. Nucl. Med. 2011, 52, 1559–1565. [Google Scholar] [CrossRef]
- Gasperetti, A.; A James, C.; Cerrone, M.; Delmar, M.; Calkins, H.; Duru, F. Arrhythmogenic right ventricular cardiomyopathy and sports activity: From molecular pathways in diseased hearts to new insights into the athletic heart mimicry. Eur. Heart J. 2020, 42, 1231–1243. [Google Scholar] [CrossRef]
- Quyyumi, A.A. Circadian rhythms in cardiovascular disease. Am. Heart J. 1990, 120, 726–733. [Google Scholar] [CrossRef]
- Kaplan, S.R.; Gard, J.J.; Protonotarios, N.; Tsatsopoulou, A.; Spiliopoulou, C.; Anastasakis, A.; Squarcioni, C.P.; McKenna, W.J.; Thiene, G.; Basso, C.; et al. Remodeling of myocyte gap junctions in arrhythmogenic right ventricular cardiomyopathy due to a deletion in plakoglobin (Naxos disease). Heart Rhythm 2004, 1, 3–11. [Google Scholar] [CrossRef]
- Degaute, J.P.; van de Borne, P.; Linkowski, P.; Van Cauter, E. Quantitative analysis of the 24-hour blood pressure and heart rate patterns in young men. Hypertension 1991, 18, 199–210. [Google Scholar] [CrossRef]
- Arvidsson, D.; Eriksson, U.; Lönn, S.L.; Sundquist, K. Neighborhood Walkability, Income, and Hour-by-Hour Physical Activity Patterns. Med. Sci. Sports Exerc. 2013, 45, 698–705. [Google Scholar] [CrossRef]
- Berglind, D.; Tynelius, P. Objectively measured physical activity patterns, sedentary time and parent-reported screen-time across the day in four-year-old Swedish children. BMC Public Health 2017, 18, 69. [Google Scholar] [CrossRef]
- Hansen, B.H.; Holme, I.; Anderssen, S.A.; Kolle, E. Patterns of Objectively Measured Physical Activity in Normal Weight, Overweight, and Obese Individuals (20–85 Years): A Cross-Sectional Study. PLoS ONE 2013, 8, e53044. [Google Scholar] [CrossRef] [PubMed]
- Šimaitytė, M.; Petrėnas, A.; Kravčenko, J.; Kaldoudi, E.; Marozas, V. Objective evaluation of physical activity pattern using smart devices. Sci. Rep. 2019, 9, 2006. [Google Scholar] [CrossRef] [PubMed]
- Stuber, T.; Eigenmann, C.; Delacrétaz, E. Seasonal Variations of Ventricular Arrhythmia Clusters in Defibrillator Recipients. Pacing Clin. Electrophysiol. 2006, 29, 816–820. [Google Scholar] [CrossRef] [PubMed]
- Phillips, D.P.; Jarvinen, J.R.; Abramson, I.S.; Phillips, R.R. Cardiac Mortality Is Higher Around Christmas and New Year’s Than at Any Other Time. Circulation 2004, 110, 3781–3788. [Google Scholar] [CrossRef]
- Arntz, H.-R.; Willich, S.; Schreiber, C.; Brüggemann, T.; Stern, R.; Schultheiß, H.-P. Diurnal, weekly and seasonal variation of sudden death. Population-based analysis of 24061 consecutive cases. Eur. Heart J. 2000, 21, 315–320. [Google Scholar] [CrossRef]
- Kloner, R.A.; Poole, W.K.; Perritt, R.L. When Throughout the Year Is Coronary Death Most Likely to Occur? Circulation 1999, 100, 1630–1634. [Google Scholar] [CrossRef]
- Spencer, F.A.; Goldberg, R.J.; Becker, R.C.; Gore, J.M. Seasonal Distribution of Acute Myocardial Infarction in the Second National Registry of Myocardial Infarction. J. Am. Coll. Cardiol. 1998, 31, 1226–1233. [Google Scholar] [CrossRef]
- Ornato, J.P.; Peberdy, M.A.; Chandra, N.C.; Bush, D.E. Seasonal Pattern of Acute Myocardial Infarction in the National Registry of Myocardial Infarction. J. Am. Coll. Cardiol. 1996, 28, 1684–1688. [Google Scholar] [CrossRef]
- Wang, H.; Sekine, M.; Chen, X.; Kagamimori, S. A study of weekly and seasonal variation of stroke onset. Int. J. Biometeorol. 2002, 47, 13–20. [Google Scholar] [CrossRef]
- Mehta, R.H.; Manfredini, R.; Hassan, F.; Sechtem, U.; Bossone, E.; Oh, J.K.; Cooper, J.V.; Smith, D.E.; Portaluppi, F.; Penn, M.; et al. Chronobiological Patterns of Acute Aortic Dissection. Circulation 2002, 106, 1110–1115. [Google Scholar] [CrossRef]
- Maeda, S.; Takahashi, Y.; Nogami, A.; Yamauchi, Y.; Osaka, Y.; Shirai, Y.; Ihara, K.; Yokoyama, Y.; Suzuki, M.; Okishige, K.; et al. Seasonal, weekly, and circadian distribution of ventricular fibrillation in patients with J-wave syndrome from the J-PREVENT registry. J. Arrhythmia 2015, 31, 268–273. [Google Scholar] [CrossRef]
- Fares, A. Winter cardiovascular diseases phenomenon. North Am. J. Med. Sci. 2013, 5, 266–279. [Google Scholar] [CrossRef]
- Altizer, S.; Dobson, A.; Hosseini, P.; Hudson, P.; Pascual, M.; Rohani, P. Seasonality and the dynamics of infectious diseases. Ecol. Lett. 2006, 9, 467–484. [Google Scholar] [CrossRef]
- Basso, C.; Thiene, G.; Corrado, D.; Angelini, A.; Nava, A.; Valente, M. Arrhythmogenic Right Ventricular Cardiomyopathy: Dysplasia, dystrophy, or myocarditis? Circulation 1996, 94, 983–991. [Google Scholar] [CrossRef]
- Bauce, B.; Basso, C.; Rampazzo, A.; Beffagna, G.; Daliento, L.; Frigo, G.; Malacrida, S.; Settimo, L.; Danieli, G.; Thiene, G.; et al. Clinical profile of four families with arrhythmogenic right ventricular cardiomyopathy caused by dominant desmoplakin mutations. Eur. Heart J. 2005, 26, 1666–1675. [Google Scholar] [CrossRef]
- Thiene, G.; Nava, A.; Corrado, D.; Rossi, L.; Pennelli, N. Right Ventricular Cardiomyopathy and Sudden Death in Young People. N. Engl. J. Med. 1988, 318, 129–133. [Google Scholar] [CrossRef]
- Thiene, G.; Corrado, D.; Nava, A.; Rossi, L.; Poletti, A.; Boffa, G.M.; Daliento, L.; Pennelli, N. Right ventricular cardiomyopathy: Is there evidence of an inflammatory aetiology? Eur. Heart J. 1991, 12, 22–25. [Google Scholar] [CrossRef] [PubMed]
- Bowles, E.N.; Ni, J.; Marcus, F.; A Towbin, J. The detection of cardiotropic viruses in the myocardium of patients with arrhythmogenic right ventricular dysplasia/cardiomyopathy. J. Am. Coll. Cardiol. 2002, 39, 892–895. [Google Scholar] [CrossRef] [PubMed]
- Calabrese, F.; Basso, C.; Carturan, E.; Valente, M.; Thiene, G. Arrhythmogenic right ventricular cardiomyopathy/dysplasia: Is there a role for viruses? Cardiovasc. Pathol. 2006, 15, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Grumbach, I.M.; Heim, A.; Vonhof, S.; Stille-Siegener, M.; Mall, G.; Gonska, B.D.; Kreuzer, H.; Andreas, S.; Figulla, H.R. Coxsackievirus Genome in Myocardium of Patients with Arrhythmogenic Right Ventricular Dysplasia/Cardiomyopathy. Cardiology 1998, 89, 241–245. [Google Scholar] [CrossRef]
- Matsumori, A.; Kawai, C. Coxsackie virus B3 perimyocarditis in BALB/c mice: Experimental model of chronic perimyocarditis in the right ventricle. J. Pathol. 1980, 131, 97–106. [Google Scholar] [CrossRef]
- Heim, A.; Grumbach, I.; Stille-Siegener, M.; Figulla, H. Detection of enterovirus RNA in the myocardium of a patient with arrhythmogenic right ventricular cardiomyopathy by in situ hybridization. Clin. Infect. Dis. 1997, 25, 1471–1472. [Google Scholar] [CrossRef] [PubMed]
- Campuzano, O.; Alcalde, M.; Iglesias, A.; Barahona-Dussault, C.; Sarquella-Brugada, G.; Benito, B.; Arzamendi, D.; Flores, J.; Leung, T.K.; Talajic, M.; et al. Arrhythmogenic right ventricular cardiomyopathy: Severe structural alterations are associated with inflammation. J. Clin. Pathol. 2012, 65, 1077–1083. [Google Scholar] [CrossRef] [PubMed]
- Patrianakos, A.; Protonotarios, N.; Nyktari, E.; Pagonidis, K.; Tsatsopoulou, A.; Parthenakis, F.; Vardas, P. Arrhythmogenic right ventricular cardiomyopathy/dysplasia and troponin release. Myocarditis or the “hot phase” of the disease? Int. J. Cardiol. 2012, 157, e26–e28. [Google Scholar] [CrossRef]
- Tanawuttiwat, T.; Sager, S.J.; Hare, J.M.; Myerburg, R.J. Myocarditis and ARVC/D: Variants or mimics? Heart Rhythm 2013, 10, 1544–1548. [Google Scholar] [CrossRef] [PubMed]
- Jordan, A.N.; Lyne, J.; De Silva, R.; Wong, T. Myocarditic Appearance of Arrhythmogenic Right Ventricular Cardiomyopathy. Circulation 2010, 122, e556–e557. [Google Scholar] [CrossRef]
- Poller, W.; Haas, J.; Klingel, K.; Kühnisch, J.; Gast, M.; Kaya, Z.; Escher, F.; Kayvanpour, E.; Degener, F.; Opgen-Rhein, B.; et al. Familial Recurrent Myocarditis Triggered by Exercise in Patients With a Truncating Variant of the Desmoplakin Gene. J. Am. Heart Assoc. 2020, 9, e015289. [Google Scholar] [CrossRef]
- Piriou, N.; Marteau, L.; Kyndt, F.; Serfaty, J.M.; Toquet, C.; Le Gloan, L.; Warin-Fresse, K.; Guijarro, D.; Le Tourneau, T.; Conan, E.; et al. Familial screening in case of acute myocarditis reveals inherited arrhythmogenic left ventricular cardiomyopathies. ESC Heart Fail. 2020, 7, 1520–1533. [Google Scholar] [CrossRef]
- Ammirati, E.; Raimondi, F.; Piriou, N.; Infirri, L.S.; Mohiddin, S.A.; Mazzanti, A.; Shenoy, C.; Cavallari, U.A.; Imazio, M.; Aquaro, G.D.; et al. Acute Myocarditis Associated With Desmosomal Gene Variants. JACC Heart Fail. 2022, 10, 714–727. [Google Scholar] [CrossRef] [PubMed]
- Chatterjee, D.; Fatah, M.; Akdis, D.; Spears, D.A.; Koopmann, T.T.; Mittal, K.; Rafiq, M.A.; Cattanach, B.M.; Zhao, Q.; Healey, J.S.; et al. An autoantibody identifies arrhythmogenic right ventricular cardiomyopathy and participates in its pathogenesis. Eur. Heart J. 2018, 39, 3932–3944. [Google Scholar] [CrossRef] [PubMed]
- Caforio, A.L.; Re, F.; Avella, A.; Marcolongo, R.; Baratta, P.; Seguso, M.; Gallo, N.; Plebani, M.; Izquierdo-Bajo, A.; Cheng, C.-Y.; et al. Evidence From Family Studies for Autoimmunity in Arrhythmogenic Right Ventricular Cardiomyopathy. Circulation 2020, 141, 1238–1248. [Google Scholar] [CrossRef] [PubMed]
- Asimaki, A.; Tandri, H.; Huang, H.; Halushka, M.K.; Gautam, S.; Basso, C.; Thiene, G.; Tsatsopoulou, A.; Protonotarios, N.; McKenna, W.J.; et al. A New Diagnostic Test for Arrhythmogenic Right Ventricular Cardiomyopathy. N. Engl. J. Med. 2009, 360, 1075–1084. [Google Scholar] [CrossRef]
- Dubash, A.D.; Kam, C.Y.; Aguado, B.A.; Patel, D.M.; Delmar, M.; Shea, L.D.; Green, K.J. Plakophilin-2 loss promotes TGF-β1/p38 MAPK-dependent fibrotic gene expression in cardiomyocytes. J. Cell Biol. 2016, 212, 425–438. [Google Scholar] [CrossRef]
- Padrón-Barthe, L.; Domínguez, F.; Garcia-Pavia, P.; Lara-Pezzi, E. Animal models of arrhythmogenic right ventricular cardiomyopathy: What have we learned and where do we go? Insight for therapeutics. Basic Res. Cardiol. 2017, 112, 50. [Google Scholar] [CrossRef]
- Pilichou, K.; Remme, C.A.; Basso, C.; Campian, M.E.; Rizzo, S.; Barnett, P.; Scicluna, B.P.; Bauce, B.; Hoff, M.J.V.D.; De Bakker, J.M.; et al. Myocyte necrosis underlies progressive myocardial dystrophy in mouse dsg2-related arrhythmogenic right ventricular cardiomyopathy. J. Exp. Med. 2009, 206, 1787–1802. [Google Scholar] [CrossRef]
- Lubos, N.; Van Der Gaag, S.; Gerçek, M.; Kant, S.; Leube, R.E.; Krusche, C.A. Inflammation shapes pathogenesis of murine arrhythmogenic cardiomyopathy. Basic Res. Cardiol. 2020, 115, 42. [Google Scholar] [CrossRef]
- Chelko, S.; Asimaki, A.; Lowenthal, J.; Bueno-Beti, C.; Bedja, D.; Scalco, A.; Amat-Alarcon, N.; Andersen, P.; Judge, D.P.; Tung, L.; et al. Therapeutic Modulation of the Immune Response in Arrhythmogenic Cardiomyopathy. Circulation 2019, 140, 1491–1505. [Google Scholar] [CrossRef]

| # Patient | Diagnostic Criteria * | # Patient | Diagnostic Criteria * | ||
|---|---|---|---|---|---|
| Major | Minor | Major | Minor | ||
| 1 | 2 (e, f) | 1 (a) | 52 | 4 (a, b, e, f) | |
| 2 | 2 (e, f) | 1 (c) | 53 | 2 (a, e) | |
| 3 | 3 (a, e, f) | 1 (c) | 54 | 2 (e, f) | 1 (d) |
| 4 | 4 (a, c, e, f) | 1 (d) | 55 | 3 (a, e, f) | |
| 5 | 2 (e, f) | 56 | 1 (c) | 2 (e, f) | |
| 6 | 3 (c, e, f) | 1 (a) | 57 | 3 (a, e, f) | 2 (c, d) |
| 7 | 2 (c, f) | 58 | 2 (a, c) | 1 (d) | |
| 8 | 3 (a, c, f) | 1 (e) | 59 | 2 (e, f) | |
| 9 | 2 (e, f) | 60 | 2 (e, f) | 1 (a) | |
| 10 | 3 (a, e, f) | 61 | 2 (e, f) | ||
| 11 | 2 (a, f) | 62 | 2 (e, f) | ||
| 12 | 2 (a, f) | 63 | 3 (a, c, e) | ||
| 13 | 2 (e, f) | 64 | 2 (e, f) | 1 (c) | |
| 14 | 2 (a, c) | 2 (e, d) | 65 | 3 (a, c, e) | |
| 15 | 3 (a, c, e) | 1 (d) | 66 | 2 (c, e) | 2 (a, d) |
| 16 | 3 (a, d, f) | 1 (c) | 67 | 2 (d, f) | 2 (a, e) |
| 17 | 5 (a, b, c, e, f) | 1 (d) | 68 | 2 (c, f) | 1 (d) |
| 18 | 2 (a, f) | 2 (d, e) | 69 | 2 (c, f) | 2 (a, e) |
| 19 | 3 (c, e, f) | 70 | 2 (e, f) | 2 (c, d) | |
| 20 | 2 (e, f) | 71 | 2 (e, f) | 1 (c) | |
| 21 | 3 (c, d, f) | 2 (a, e) | 72 | 3 (c, d, e) | 1 (a) |
| 22 | 2 (d, f) | 2 (c, e) | 73 | 2 (a, f) | |
| 23 | 3 (a, d, f) | 1 (e) | 74 | 3 (a, e, f) | |
| 24 | 3 (a, d, f) | 1 (e) | 75 | 3 (c, e, f) | |
| 25 | 2 (e, f) | 1 (c) | 76 | 2 (a, f) | 1 (d) |
| 26 | 2 (d, f) | 3 (a, c, e) | 77 | 4 (a, c, e, f) | |
| 27 | 2 (a, f) | 1 (e) | 78 | 3 (a, e, f) | |
| 28 | 2 (e, f) | 1 (a) | 79 | 3 (a, e, f) | 1 (c) |
| 29 | 2 (e, f) | 1 (d) | 80 | 3 (a, c, f) | |
| 30 | 2 (a, f) | 1 (e) | 81 | 3 (a, c, f) | |
| 31 | 2 (a, d, f) | 1 (e) | 82 | 2 (a, e) | |
| 32 | 3 (a, e, f) | 1 (c) | 83 | 4 (a, c, e, f) | |
| 33 | 3 (a, e, f) | 1 (c) | 84 | 2 (c, e) | 1 (a) |
| 34 | 1 (f) | 3 (c, d, e) | 85 | 3 (a, c, e) | |
| 35 | 3 (c, e, f) | 86 | 2 (a, c) | 1 (d) | |
| 36 | 2 (c, f) | 87 | 1 (f) | 2 (c, d) | |
| 37 | 2 (c, f) | 88 | 2 (a, e) | 2 (c, d) | |
| 38 | 3 (c, d, f) | 1 (e) | 89 | 3 (a, c, f) | 1 (e) |
| 39 | 3 (c, e, f) | 1 (a) | 90 | 2 (c, e) | |
| 40 | 1 (f) | 3 (a, d, e) | 91 | 2 (e, f) | |
| 41 | 2 (e, f) | 1 (a) | 92 | 3 (a, c, e) | |
| 42 | 2 (c, e) | 1 (d) | 93 | 2 (a, e) | 1 (c) |
| 43 | 2 (c, f) | 2 (a, e) | 94 | 4 (b, c, e, f) | 1 (a) |
| 44 | 5 (a, c, d, e, f) | 95 | 2 (e, f) | 1 (c) | |
| 45 | 2 (a, f) | 1 (d) | 96 | 2 (a, e) | |
| 46 | 2 (a, f) | 1 (c) | 97 | 2 (e, f) | |
| 47 | 2 (e, f) | 2 (c, d) | 98 | 3 (a, c, f) | 2 (d, e) |
| 48 | 3 (a, e, f) | 1 (c) | 99 | 4 (a, c, e, f) | |
| 49 | 2 (a, e) | 1 (d) | 100 | 3 (a, e, f) | |
| 50 | 3 (a, e, f) | 101 | 2 (a, f) | 1 (e) | |
| 51 | 1 (f) | 2 (e, d) | 102 | 3 (a, c, f) | 2 (d, e) |
| Study Population 102 | ||
|---|---|---|
| Male/female | 55 (54%) | 47 (46%) |
| Caucasian/other | 96(94%) | 6 (6%) |
| Age at diagnosis/age at ICD implantation | 40 ± 14 | 41 ± 15 |
| Proband/family member | 75 (74%) | 27 (26%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Castelletti, S.; Orini, M.; Vischer, A.S.; McKenna, W.J.; Lambiase, P.D.; Pantazis, A.; Crotti, L. Circadian and Seasonal Pattern of Arrhythmic Events in Arrhythmogenic Cardiomyopathy Patients. Int. J. Environ. Res. Public Health 2023, 20, 2872. https://doi.org/10.3390/ijerph20042872
Castelletti S, Orini M, Vischer AS, McKenna WJ, Lambiase PD, Pantazis A, Crotti L. Circadian and Seasonal Pattern of Arrhythmic Events in Arrhythmogenic Cardiomyopathy Patients. International Journal of Environmental Research and Public Health. 2023; 20(4):2872. https://doi.org/10.3390/ijerph20042872
Chicago/Turabian StyleCastelletti, Silvia, Michele Orini, Annina S. Vischer, William J. McKenna, Pier D. Lambiase, Antonios Pantazis, and Lia Crotti. 2023. "Circadian and Seasonal Pattern of Arrhythmic Events in Arrhythmogenic Cardiomyopathy Patients" International Journal of Environmental Research and Public Health 20, no. 4: 2872. https://doi.org/10.3390/ijerph20042872
APA StyleCastelletti, S., Orini, M., Vischer, A. S., McKenna, W. J., Lambiase, P. D., Pantazis, A., & Crotti, L. (2023). Circadian and Seasonal Pattern of Arrhythmic Events in Arrhythmogenic Cardiomyopathy Patients. International Journal of Environmental Research and Public Health, 20(4), 2872. https://doi.org/10.3390/ijerph20042872










