Prevalence and Factors Associated with Eating Disorders in Military First Line of Defense against COVID-19: A Cross-Sectional Study during the Second Epidemic Wave in Peru
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design, Population, and Sample
2.1.1. Instruments and Variables
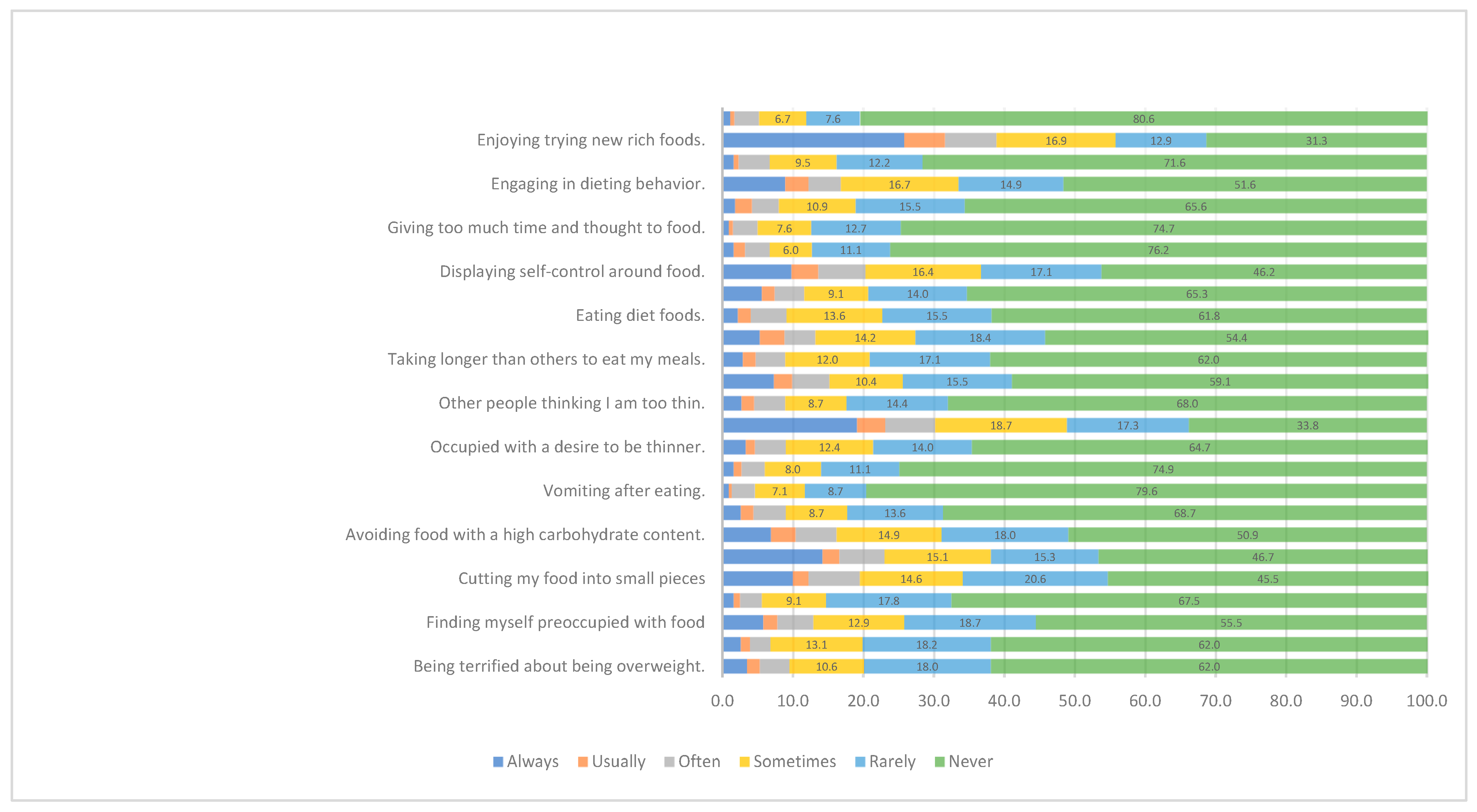
- Eating Disorder symptomatology was the outcome, measured with the Eating Attitudes Test-26 (EAT-26). This test consists of 26 self-report questions assessing general eating behavior and 5 additional questions assessing risk behaviors [28,29,30]. EAT-26 allows the detection of probable eating disorder such as anorexia nervosa, bulimia nervosa and binge eating disorder [31]. Each question has 6 response options with different scoring: 0 points (never, rarely, sometimes); 1 point (often); 2 points (very often); 3 points (always) [28,29]. The total score is the sum of the responses to the 26 items, with question 26 being scored inversely. The higher the score, the higher the risk of anorexia nervosa (AN) or bulimia nervosa (BN) [28,29]. The instrument has 3 subscales: (a) diet, with 13 items on avoidance of fattening foods and concerns about thinness; (b) bulimia and food preoccupation, with 6 items on bulimic behaviors and thoughts about food; and c) oral control, with 7 items on self-control of intake and external pressure to gain weight [28,29]. We used the Spanish version of EAT-26 validated by Gandarillas et al. [32]. The instrument used (EAT-26) has 88.9% sensitivity and 97.7% specificity [33]. The EAT-26 is a useful instrument for assessing risk of eating disorder, but it does not provide a definitive diagnosis [34]. A score of 20 or more obtained from the EAT-26 was considered as positive eating disorder symptomatology, which requires further clinical evaluation by mental health professionals [35]. For this study, the Cronbach’s alpha coefficient was 0.93.
- Insomnia was measured with the Insomnia Severity Index (ISI). It consists of seven self-report items that measure the perceived severity of insomnia through a Likert-type scale from 0 to 4 points and a final score from 0 to 28 points. Higher scores reflect a greater degree of insomnia, with a cut-off point of 8 points [36]. It has been validated in older adults [37] and the general Spanish-speaking population [38]. For this study, the Cronbach’s alpha coefficient was 0.88.
- Food Insecurity was measured with the Household Food Insecurity Assessment Scale (HFIAS). It consists of nine items on a Likert scale of 1 to 3 points (1, seldom; 2, sometimes; 3, frequently). It has excellent psychometric properties in the Latin American population [39]. It has three domains: (1) anxiety and uncertainty about food supply in the household, (2) food quality and insufficient food intake and (3) physical consequences [39]. Mild IA has a score of 2–3 on the first item, 1–3 on the second item or 1 on the third or fourth item [39]. Moderate IA is defined as a score of 2–3 on the third or fourth item, or 1–2 on the fifth or sixth item [39]. Severe IA is defined as a score of 3 on the fifth or sixth item, or 1–3 on factors seven and eight and nine [39]. For this study, the Cronbach’s alpha coefficient was 0.87.
- Physical Activity was measured with the short version of the International Physical Activity Questionnaire (IPAQ-S). This questionnaire includes 9 items and assesses reported physical activity during the last 7 days. It allows obtaining a weighted estimate of total physical activity from the activities reported per week to classify physical activity into: intense, moderate, mild or inactive [40]. It has been validated in Hispanic communities and applied to Latin American populations [41]. For this study, the Cronbach’s alpha coefficient was 0.64.
- Resilience was measured with the Connor-Davidson Resilience Scale (CD-RISC). This questionnaire consists of 10 questions with a Likert scale of 0–4 points (0 “not at all”, 1 “rarely”, 2 “sometimes”, 3 “often”, 4 “almost always”) [42]. It presents adequate internal consistency and validity in multiple occupational groups, health personnel and general adult populations [43,44,45]. It uses a score of less than 30 to define high resilience and less than 30 for low resilience [42,43,44,45]. For this study, the Cronbach’s alpha coefficient was 0.97.
- Fear of COVID-19 was measured with the Fear of COVID-19 Scale. This questionnaire consists of 7 items with a Likert scale of 1–5 points (1 “strongly disagree”, 2 “disagree”, 3 “neither agree nor disagree”, 4 “agree”, 5 “strongly agree”) that evaluate the degree of fear of COVID-19, whereby a higher score indicates a greater fear of COVID-19 [46]. It has excellent psychometric properties and is considered a solid instrument for evaluation in different languages [47]. It has been validated in Latin and Spanish-speaking populations [48,49]. A cut-off point of 16.5 points has been validated to define fear of COVID [50]. For this study, the Cronbach’s alpha coefficient was 0.94.
- Burnout Syndrome was measured with the Maslach Burnout Inventory. It consists of 22 items with a Likert scale of 0–7 points organized in three dimensions that evaluate emotional exhaustion (9 items), depersonalization (5 items) and personal fulfillment (8 items) [51]. It has been validated in the Latin population [52] with adequate validity and reliability properties (Cronbach’s alpha, 0.87; sensitivity, 86.6%; specificity, 89%) [53]. For this study, the Cronbach’s alpha coefficient was 0.91.
- Anxiety was measured with the Generalized Anxiety Disorder-7 Scale (GAD-7). This instrument consists of 7 questions with a Likert scale of 0–3 points (0 “no day”, 1 “several days”, 2 “more than half of the days, 3 “almost every day”) [54]. It assesses anxiety symptoms during the prior 2 weeks, according to DSM-IV criteria [55]. Scores are grouped into no anxiety (0–4 points), mild anxiety (5–9 points), moderate anxiety (10–14 points) and severe anxiety (15–21 points). Its psychometric properties are optimal (Cronbach’s alpha, 0.93; sensitivity, 86.8%; and specificity, 93.4%) [54]. For this study, the Cronbach’s alpha coefficient was 0.93.
- Depression was measured with the Patient Health Questionnaire-9 (PHQ-9): This questionnaire evaluates the presence of depressive symptoms during the prior 2 weeks and is based on DSM-IV criteria [56]. It presents 9 items and uses a Likert scale from 0 to 3 points to evaluate four response options (0 “never”, 1 “several days”, 2 “more than half of the days”, 3 “almost every day”) and has a final score range between 0 to 27 points. It has been validated in the Peruvian population and shows excellent internal consistency (Cronbach’s alpha: 0.87) [57]. For this study, the Cronbach’s alpha coefficient was 0.92.
- Post-traumatic stress disorder was measured with the PTSD Checklist-Civilian Version (PCL-C): This instrument is made up of 17 questions with a Likert scale of 1–5, which measure symptoms of post-traumatic stress disorder, based on the DSM-IV criteria and the rubric of the National Center for PTSD [58,59]. It comprises the domains of trauma re-experiencing (domain B), trauma avoidance and blunting (domain C) and hyperactivity (domain D) [58,59]. It presents a score from 17 to 85 points, with 43 points being the cut-off point to define PTSD [58,59]. It has been validated in Latin populations [60], demonstrating adequate psychometric properties in its internal validity [59]. In the military population, it has been found to have adequate internal consistency and convergent and discriminant validity [61]. For this study, the Cronbach’s alpha coefficient was 0.95.
- General, occupational and psychosocial data: age in years, gender (male, female), single marital status (no, yes), religion (none, Catholic, non-Catholic), children (no, yes), report of frequent alcohol and tobacco consumption (no, yes), report of comorbidities (arterial hypertension, diabetes), body mass index (underweight, normal, overweight, obese), work time (1 to 6 months, 7 to 12 months, 13 to 18 months, 19 months or more), reported personal prior mental health history (no, yes), reported family prior mental health history (no, yes), sought help for mental health problem during COVID pandemic (no, yes), reliance on government to handle COVID (no, yes).
2.1.2. Procedures
2.1.3. Statistical Analysis
2.1.4. Ethical Aspects
3. Results
3.1. General Characteristics
3.2. Factors Associated with Eating Disorder Symptoms
3.3. Factors Associated with Eating Disorder Symptoms in Simple and Multiple Regression Analysis
4. Discussion
4.1. Main Findings
4.2. Prevalence of Eating Disorder Symptoms
4.3. Factors Associated with Eating Disorder Symptoms
4.4. Public Health Implications of Findings
4.5. Limitations and Strengths
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Psychiatry.Org—What Are Eating Disorders? Available online: https://psychiatry.org:443/patients-families/eating-disorders/what-are-eating-disorders (accessed on 14 June 2022).
- Balasundaram, P.; Santhanam, P. Eating Disorders. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Arditte Hall, K.A.; Bartlett, B.A.; Iverson, K.M.; Mitchell, K.S. Military-Related Trauma Is Associated with Eating Disorder Symptoms in Male Veterans. Int. J. Eat. Disord. 2017, 50, 1328–1331. [Google Scholar] [CrossRef] [PubMed]
- Arditte Hall, K.A.; Bartlett, B.A.; Iverson, K.M.; Mitchell, K.S. Eating Disorder Symptoms in Female Veterans: The Role of Childhood, Adult, and Military Trauma Exposure. Psychol. Trauma Theory Res. Pract. Policy 2018, 10, 345–351. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, K.S.; Masheb, R.; Smith, B.N.; Kehle-Forbes, S.; Hardin, S.; Vogt, D. Eating Disorder Measures in a Sample of Military Veterans: A Focus on Gender, Age, and Race/Ethnicity. Psychol. Assess. 2021, 33, 1226–1238. [Google Scholar] [CrossRef] [PubMed]
- Qian, J.; Wu, Y.; Liu, F.; Zhu, Y.; Jin, H.; Zhang, H.; Wan, Y.; Li, C.; Yu, D. An Update on the Prevalence of Eating Disorders in the General Population: A Systematic Review and Meta-Analysis. Eat. Weight Disord. 2022, 27, 415–428. [Google Scholar] [CrossRef]
- Bartlett, B.A.; Mitchell, K.S. Eating Disorders in Military and Veteran Men and Women: A Systematic Review. Int. J. Eat. Disord. 2015, 48, 1057–1069. [Google Scholar] [CrossRef]
- Carhuapoma-Yance, M.; Apolaya-Segura, M.; Valladares-Garrido, M.J.; Failoc-Rojas, V.E.; Díaz-Vélez, C. Human development and COVID-19 lethality rate: Ecological study in America. Rev. Cuerpo Med. Hosp. HNAAA 2021, 14, 362–366. [Google Scholar] [CrossRef]
- Vasquez-Elera, L.E.; Failoc-Rojas, V.E.; Martinez-Rivera, R.N.; Morocho-Alburqueque, N.; Temoche-Rivas, M.S.; Valladares-Garrido, M.J. Self-Medication in Hospitalized Patients with COVID-19: A Cross-Sectional Study in Northern Peru. Germs 2022, 12, 46–53. [Google Scholar] [CrossRef]
- León-Jiménez, F.; Vives-Kufoy, C.; Failoc-Rojas, V.E.; Valladares-Garrido, M.J. Mortalidad En Pacientes Hospitalizados Por COVID-19. Estudio Prospectivo En El Norte Del Perú, 2020. Rev. Méd. Chile 2021, 149, 1459–1466. [Google Scholar] [CrossRef]
- Ponce, V.V.; Garrido, M.V.; Peralta, C.I.; Astudillo, D.; Malca, J.T.; Manrique, E.O.; Quispe, E.T. Factores Asociados al Afrontamiento Psicológico Frente a La COVID-19 Durante El Periodo de Cuarentena. Rev. Cub. Med. Mil. 2020, 49, 0200870. [Google Scholar]
- Changes of Symptoms of Eating Disorders (ED) and Their Related Psychological Health Issues during the COVID-19 Pandemic: A Systematic Review and Meta-Analysis|J Eat Dis|Full Text. Available online: https://jeatdisord.biomedcentral.com/articles/10.1186/s40337-022-00550-9 (accessed on 14 June 2022).
- Rodgers, R.F.; Lombardo, C.; Cerolini, S.; Franko, D.L.; Omori, M.; Fuller-Tyszkiewicz, M.; Linardon, J.; Courtet, P.; Guillaume, S. The Impact of the COVID-19 Pandemic on Eating Disorder Risk and Symptoms. Int. J. Eat. Disord. 2020, 53, 1166–1170. [Google Scholar] [CrossRef]
- Monteleone, P. Eating Disorders in the Era of the COVID-19 Pandemic: What Have We Learned? Int. J. Environ. Res. Public Health 2021, 18, 12381. [Google Scholar] [CrossRef] [PubMed]
- Baenas, I.; Etxandi, M.; Munguía, L.; Granero, R.; Mestre-Bach, G.; Sánchez, I.; Ortega, E.; Andreu, A.; Moize, V.L.; Fernández-Real, J.-M.; et al. Impact of COVID-19 Lockdown in Eating Disorders: A Multicentre Collaborative International Study. Nutrients 2022, 14, 100. [Google Scholar] [CrossRef] [PubMed]
- Valladares-Garrido, M.J.; Picón-Reátegui, C.K.; Zila-Velasque, J.P.; Grados-Espinoza, P. Prevalence and Factors Associated with Insomnia in Military Personnel: A Retrospective Study during the Second COVID-19 Epidemic Wave in Peru. Healthcare 2022, 10, 1199. [Google Scholar] [CrossRef] [PubMed]
- Savarese, G.; Milano, W.D.; Carpinelli, L. Eating Disorders (EDs) and the COVID-19 Pandemic: A Pilot Study on the Impact of Phase II of the Lockdown. BioMed 2022, 2, 110–116. [Google Scholar] [CrossRef]
- Mejia, C.R.; Liendo-Venegas, D.; García-Gamboa, F.; Mejía-Rodríguez, M.A.; Valladares-Garrido, M.J. Factors Associated with the Perception of Inadequate Sanitary Control in 12 Latin American Countries during the COVID-19 Pandemic. Front. Public Health 2022, 10, 934087. [Google Scholar] [CrossRef]
- Kasiak, P.S.; Adamczyk, N.; Jodczyk, A.M.; Kaproń, A.; Lisowska, A.; Mamcarz, A.; Śliż, D. COVID-19 Pandemic Consequences among Individuals with Eating Disorders on a Clinical Sample in Poland—A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 8484. [Google Scholar] [CrossRef]
- Bray, B.; Bray, C.; Bradley, R.; Zwickey, H. Binge Eating Disorder Is a Social Justice Issue: A Cross-Sectional Mixed-Methods Study of Binge Eating Disorder Experts’ Opinions. Int. J. Environ. Res. Public Health 2022, 19, 6243. [Google Scholar] [CrossRef]
- World Health Organization; Pan American Health Organization. Impact of COVID-19 on Human Resources for Health and Policy Response: The Case of Plurinational State of Bolivia, Chile, Colombia, Ecuador and Peru: Overview of Findings from Five Latin American Countries; World Health Organization: Geneva, Switzerland, 2021; ISBN 978-92-4-003900-1. [Google Scholar]
- Bouskill, K.E.; Fitzke, R.E.; Saba, S.K.; Ring, C.; Davis, J.P.; Lee, D.S.; Pedersen, E.R. Stress and Coping among Post-9/11 Veterans During COVID-19: A Qualitative Exploration. J. Vet. Stud. 2022, 8, 134–146. [Google Scholar] [CrossRef]
- Las Fuerzas Armadas del Perú y su lucha contra la COVID-19. Available online: https://www.gob.pe/institucion/ccffaa/informes-publicaciones/2049105-las-fuerzas-armadas-del-peru-y-su-lucha-contra-la-covid-19 (accessed on 14 June 2022).
- The Effects of COVID-19 on the Mental Health of the Peruvian Police and Armed Forces. Available online: https://www.ejgm.co.uk/article/the-effects-of-covid-19-on-the-mental-health-of-the-peruvian-police-and-armed-forces-10839 (accessed on 14 June 2022).
- Díaz-Vélez, C.; Failoc-Rojas, V.E.; Valladares-Garrido, M.J.; Colchado, J.; Carrera-Acosta, L.; Becerra, M.; Paico, D.M.; Ocampo-Salazar, E.T. SARS-CoV-2 Seroprevalence Study in Lambayeque, Peru. June–July 2020. PeerJ 2021, 9, e11210. [Google Scholar] [CrossRef]
- Díaz-Vélez, C.; Urrunaga-Pastor, D.; Romero-Cerdán, A.; Peña-Sánchez, E.R.; Fernández Mogollon, J.L.; Cossio Chafloque, J.D.; Marreros Ascoy, G.C.; Benites-Zapata, V.A. Risk Factors for Mortality in Hospitalized Patients with COVID-19 from Three Hospitals in Peru: A Retrospective Cohort Study. F1000Research 2021, 10, 224. [Google Scholar] [CrossRef]
- Pietrzak, R.H.; Tsai, J.; Southwick, S.M. Association of Symptoms of Posttraumatic Stress Disorder With Posttraumatic Psychological Growth Among US Veterans During the COVID-19 Pandemic. JAMA Netw. Open 2021, 4, e214972. [Google Scholar] [CrossRef] [PubMed]
- Constaín, G.A.; Ricardo Ramírez, C.; Rodríguez-Gázquez, M.d.L.Á.; Alvarez Gómez, M.; Marín Múnera, C.; Agudelo Acosta, C. Diagnostic validity and usefulness of the Eating Attitudes Test-26 for the assessment of eating disorders risk in a Colombian female population. Aten. Primaria 2014, 46, 283–289. [Google Scholar] [CrossRef] [PubMed]
- Constaín, G.A.; Rodríguez-Gázquez, M.d.L.Á.; Ramírez Jiménez, G.A.; Gómez Vásquez, G.M.; Mejía Cardona, L.; Cardona Vélez, J. Diagnostic validity and usefulness of the Eating Attitudes Test-26 for the assessment of eating disorders risk in a Colombian male population. Aten. Primaria 2017, 49, 206–213. [Google Scholar] [CrossRef] [PubMed]
- Noma, S.; Nakai, Y.; Hamagaki, S.; Uehara, M.; Hayashi, A.; Hayashi, T. Comparison between the SCOFF Questionnaire and the Eating Attitudes Test in Patients with Eating Disorders. Int. J. Psychiatry Clin. Pract. 2006, 10, 27–32. [Google Scholar] [CrossRef] [PubMed]
- Eating Attitudes Test-26 (EAT-26). Available online: https://novopsych.com.au/assessments/diagnosis/eating-attitudes-test-26-eat-26/ (accessed on 8 July 2022).
- Trastornos del Comportamiento Alimentario: Prevalencia de Casos en Mujeres Adolescentes de la Comunidad de Madrid. Available online: https://psiquiatria.com/trastornos_de_alimentacion/trastornos-del-comportamiento-alimentario-prevalencia-de-casos-en-mujeres-adolescentes-de-la-comunidad-de-madrid/ (accessed on 28 June 2022).
- Jacobi, C.; Hayward, C.; de Zwaan, M.; Kraemer, H.C.; Agras, W.S. Coming to Terms with Risk Factors for Eating Disorders: Application of Risk Terminology and Suggestions for a General Taxonomy. Psychol. Bull. 2004, 130, 19–65. [Google Scholar] [CrossRef]
- Al-Jumayan, A.A.; Al-Eid, N.A.; AlShamlan, N.A.; AlOmar, R.S. Prevalence and Associated Factors of Eating Disorders in Patrons of Sport Centers in Saudi Arabia. J. Fam. Community Med. 2021, 28, 94–102. [Google Scholar] [CrossRef]
- Aparicio-Martinez, P.; Perea-Moreno, A.-J.; Martinez-Jimenez, M.P.; Redel-Macías, M.D.; Pagliari, C.; Vaquero-Abellan, M. Social Media, Thin-Ideal, Body Dissatisfaction and Disordered Eating Attitudes: An Exploratory Analysis. Int. J. Environ. Res. Public Health 2019, 16, 4177. [Google Scholar] [CrossRef]
- Bastien, C.H.; Vallières, A.; Morin, C.M. Validation of the Insomnia Severity Index as an Outcome Measure for Insomnia Research. Sleep Med. 2001, 2, 297–307. [Google Scholar] [CrossRef]
- Sierra, J.C.; Guillén-Serrano, V.; Santos-Iglesias, P. Insomnia Severity Index: Some indicators about its reliability and validity on an older adults sample. Rev. Neurol. 2008, 47, 566–570. [Google Scholar]
- Fernandez-Mendoza, J.; Rodriguez-Muñoz, A.; Vela-Bueno, A.; Olavarrieta-Bernardino, S.; Calhoun, S.L.; Bixler, E.O.; Vgontzas, A.N. The Spanish Version of the Insomnia Severity Index: A Confirmatory Factor Analysis. Sleep Med. 2012, 13, 207–210. [Google Scholar] [CrossRef]
- Household Food Insecurity Access Scale (HFIAS) for Measurement of Food Access: Indicator Guide|Food and Nutrition Technical Assistance III Project (FANTA). Available online: https://www.fantaproject.org/monitoring-and-evaluation/household-food-insecurity-access-scale-hfias (accessed on 8 July 2022).
- Mantilla Toloza, S.C.; Gómez-Conesa, A. El Cuestionario Internacional de Actividad Física. Un instrumento adecuado en el seguimiento de la actividad física poblacional. Rev. Iberoam. Fisioter. Kinesiol. 2007, 10, 48–52. [Google Scholar] [CrossRef]
- Cancela Carral, J.M.; Lago Ballesteros, J.; Ayán Pérez, C.; Mosquera Morono, M.B. Análisis de Fiabilidad y Validez de Tres Cuestionarios de Autoinforme Para Valorar La Actividad Física Realizada Por Adolescentes Españoles. Gac. Sanit. 2016, 30, 333–338. [Google Scholar] [CrossRef] [PubMed]
- Campbell-Sills, L.; Stein, M.B. Psychometric Analysis and Refinement of the Connor-Davidson Resilience Scale (CD-RISC): Validation of a 10-Item Measure of Resilience. J. Trauma. Stress 2007, 20, 1019–1028. [Google Scholar] [CrossRef] [PubMed]
- Blanco, V.; Guisande, M.A.; Sánchez, M.T.; Otero, P.; Vázquez, F.L. Spanish Validation of the 10-Item Connor-Davidson Resilience Scale (CD-RISC 10) with Non-Professional Caregivers. Aging Ment. Health 2019, 23, 183–188. [Google Scholar] [CrossRef] [PubMed]
- Soler Sánchez, M.I.; Meseguer de Pedro, M.; García Izquierdo, M. Propiedades psicométricas de la versión española de la escala de resiliencia de 10 ítems de Connor-Davidson (CD-RISC 10) en una muestra multiocupacional. Rev. Latinoam. De Psicol. 2016, 48, 159–166. [Google Scholar] [CrossRef]
- Notario-Pacheco, B.; Solera-Martínez, M.; Serrano-Parra, M.D.; Bartolomé-Gutiérrez, R.; García-Campayo, J.; Martínez-Vizcaíno, V. Reliability and Validity of the Spanish Version of the 10-Item Connor-Davidson Resilience Scale (10-Item CD-RISC) in Young Adults. Health Qual. Life Outcomes 2011, 9, 63. [Google Scholar] [CrossRef]
- Ahorsu, D.K.; Lin, C.-Y.; Imani, V.; Saffari, M.; Griffiths, M.D.; Pakpour, A.H. The Fear of COVID-19 Scale: Development and Initial Validation. Int. J. Ment. Health Addict. 2020, 20, 1537–1545. [Google Scholar] [CrossRef]
- Alimoradi, Z.; Lin, C.-Y.; Ullah, I.; Griffiths, M.D.; Pakpour, A.H. Item Response Theory Analysis of the Fear of COVID-19 Scale (FCV-19S): A Systematic Review. Psychol. Res. Behav. Manag. 2022, 15, 581–596. [Google Scholar] [CrossRef]
- Huarcaya-Victoria, J.; Villarreal-Zegarra, D.; Podestà, A.; Luna-Cuadros, M.A. Psychometric Properties of a Spanish Version of the Fear of COVID-19 Scale in General Population of Lima, Peru. Int. J. Ment. Health Addict. 2022, 20, 249–262. [Google Scholar] [CrossRef]
- Martínez-Lorca, M.; Martínez-Lorca, A.; Criado-Álvarez, J.J.; Armesilla, M.D.C.; Latorre, J.M. The Fear of COVID-19 Scale: Validation in Spanish University Students. Psychiatry Res. 2020, 293, 113350. [Google Scholar] [CrossRef]
- Nikopoulou, V.A.; Holeva, V.; Parlapani, E.; Karamouzi, P.; Voitsidis, P.; Porfyri, G.N.; Blekas, A.; Papigkioti, K.; Patsiala, S.; Diakogiannis, I. Mental Health Screening for COVID-19: A Proposed Cutoff Score for the Greek Version of the Fear of COVID-19 Scale (FCV-19S). Int. J. Ment. Health Addict. 2022, 20, 907–920. [Google Scholar] [CrossRef] [PubMed]
- Confiabilidad y Validez Factorial Del Maslach Burnout Inventory Versión Human Services Survey En Una Muestra de Asistentes Sociales Chilenos. Available online: https://www.psicologiacientifica.com/maslach-burnout-inventory-confiabilidad/ (accessed on 4 July 2022).
- Validación Del Cuestionario Maslach Burnout Inventory-Student Survey (MBI-SS) En Contexto Académico Colombiano*. Available online: http://www.scielo.org.co/scielo.php?script=sci_arttext&pid=S2011-30802016000100002 (accessed on 5 July 2022).
- Millán de Lange, A.C.; D’Aubeterre López, M.E. Propiedades Psicométricas Del Maslach Burnout Inventory-GS En Una Muestra Multiocupacional Venezolana. Rev. Psicol. (PUCP) 2012, 30, 103–128. [Google Scholar] [CrossRef]
- García-Campayo, J.; Zamorano, E.; Ruiz, M.A.; Pardo, A.; Pérez-Páramo, M.; López-Gómez, V.; Freire, O.; Rejas, J. Cultural Adaptation into Spanish of the Generalized Anxiety Disorder-7 (GAD-7) Scale as a Screening Tool. Health Qual. Life Outcomes 2010, 8, 8. [Google Scholar] [CrossRef] [PubMed]
- Franco-Jimenez, R.A.; Nuñez-Magallanes, A.; Franco-Jimenez, R.A.; Nuñez-Magallanes, A. Propiedades Psicométricas Del GAD-7, GAD-2 y GAD-Mini En Universitarios Peruanos. Propósitos Represent. 2022, 10. [Google Scholar] [CrossRef]
- Baader, M.T.; Molina, F.J.L.; Venezian, B.S.; Rojas, C.C.; Farías, S.R.; Fierro-Freixenet, C.; Backenstrass, M.; Mundt, C. Validación y Utilidad de La Encuesta PHQ-9 (Patient Health Questionnaire) En El Diagnóstico de Depresión En Pacientes Usuarios de Atención Primaria En Chile. Rev. Chil. Neuro-Psiquiatr. 2012, 50, 10–22. [Google Scholar] [CrossRef]
- Villarreal-Zegarra, D.; Copez-Lonzoy, A.; Bernabé-Ortiz, A.; Melendez-Torres, G.J.; Bazo-Alvarez, J.C. Valid Group Comparisons Can Be Made with the Patient Health Questionnaire (PHQ-9): A Measurement Invariance Study across Groups by Demographic Characteristics. PLoS ONE 2019, 14, e0221717. [Google Scholar] [CrossRef]
- Weathers, F.W.; Bovin, M.J.; Lee, D.J.; Sloan, D.M.; Schnurr, P.P.; Kaloupek, D.G.; Keane, T.M.; Marx, B.P. The Clinician-Administered PTSD Scale for DSM–5 (CAPS-5): Development and Initial Psychometric Evaluation in Military Veterans. Psychol. Assess. 2018, 30, 383–395. [Google Scholar] [CrossRef]
- Gelaye, B.; Zheng, Y.; Medina-Mora, M.E.; Rondon, M.B.; Sánchez, S.E.; Williams, M.A. Validity of the Posttraumatic Stress Disorders (PTSD) Checklist in Pregnant Women. BMC Psychiatry 2017, 17, 179. [Google Scholar] [CrossRef]
- Miles, J.N.V.; Marshall, G.N.; Schell, T.L. Spanish and English Versions of the PTSD Checklist—Civilian Version (PCL-C): Testing for Differential Item Functioning. J. Trauma. Stress 2008, 21, 369–376. [Google Scholar] [CrossRef]
- Wilkins, K.C.; Lang, A.J.; Norman, S.B. Synthesis of the Psychometric Properties of the PTSD Checklist (PCL) Military, Civilian, and Specific Versions. Depress. Anxiety 2011, 28, 596–606. [Google Scholar] [CrossRef]
- Masheb, R.M.; Ramsey, C.M.; Marsh, A.G.; Decker, S.E.; Maguen, S.; Brandt, C.A.; Haskell, S.G. DSM-5 Eating Disorder Prevalence, Gender Differences, and Mental Health Associations in United States Military Veterans. Int. J. Eat. Disord. 2021, 54, 1171–1180. [Google Scholar] [CrossRef] [PubMed]
- Górska, P.; Górna, I.; Miechowicz, I.; Przysławski, J. Changes in Life Situations during the SARS-CoV-2 Virus Pandemic and Their Impact on Eating Behaviors for Residents of Europe, Australia as Well as North and South America. Nutrients 2021, 13, 3570. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Aranda, F.; Munguía, L.; Mestre-Bach, G.; Steward, T.; Etxandi, M.; Baenas, I.; Granero, R.; Sánchez, I.; Ortega, E.; Andreu, A.; et al. COVID Isolation Eating Scale (CIES): Analysis of the Impact of Confinement in Eating Disorders and Obesity—A Collaborative International Study. Eur. Eat. Disord. Rev. 2020, 28, 871–883. [Google Scholar] [CrossRef]
- Shattuck, N.L.; Matsangas, P. Eating Behaviors in Sailors of the United States Navy: Meal-to-Sleep Intervals. Nutr. Health 2021, 27, 3–8. [Google Scholar] [CrossRef] [PubMed]
- Reyes-Olavarría, D.; Latorre-Román, P.Á.; Guzmán-Guzmán, I.P.; Jerez-Mayorga, D.; Caamaño-Navarrete, F.; Delgado-Floody, P. Positive and Negative Changes in Food Habits, Physical Activity Patterns, and Weight Status during COVID-19 Confinement: Associated Factors in the Chilean Population. Int. J. Environ. Res. Public Health 2020, 17, 5431. [Google Scholar] [CrossRef] [PubMed]
- Özcan, B.A.; Uslu, B.; Okudan, B.; Alphan, M.E. Evaluation of the Relationships between Burnout, Eating Behavior and Quality of Life in Academicans. Prog. Nutr. 2021, 23. [Google Scholar] [CrossRef]
- Verhavert, Y.; De Martelaer, K.; Van Hoof, E.; Van Der Linden, E.; Zinzen, E.; Deliens, T. The Association between Energy Balance-Related Behavior and Burn-Out in Adults: A Systematic Review. Nutrients 2020, 12, E397. [Google Scholar] [CrossRef]
- Lauder, T.D.; Williams, M.V.; Campbell, C.S.; Davis, G.D.; Sherman, R.A. Abnormal Eating Behaviors in Military Women. Med. Sci. Sports Exerc. 1999, 31, 1265–1271. [Google Scholar] [CrossRef]
- Hage, T.W.; Isaksson Rø, K.; Rø, Ø. Burnout among Staff on Specialized Eating Disorder Units in Norway. J. Eat. Disord. 2021, 9, 138. [Google Scholar] [CrossRef]
- Vaught, A.S.; Piazza, V.; Raines, A.M. Prevalence of Eating Disorders and Comorbid Psychopathology in a US Sample of Treatment-Seeking Veterans. Int. J. Eat. Disord. 2021, 54, 2009–2014. [Google Scholar] [CrossRef]
- Forman-Hoffman, V.L.; Mengeling, M.; Booth, B.M.; Torner, J.; Sadler, A.G. Eating Disorders, Post-Traumatic Stress, and Sexual Trauma in Women Veterans. Mil. Med. 2012, 177, 1161–1168. [Google Scholar] [CrossRef] [PubMed]
- Herman, A.M.; Pilcher, N.; Duka, T. Deter the Emotions: Alexithymia, Impulsivity and Their Relationship to Binge Drinking. Addict. Behav. Rep. 2020, 12, 100308. [Google Scholar] [CrossRef] [PubMed]
- Rijkers, C.; Schoorl, M.; van Hoeken, D.; Hoek, H.W. Eating Disorders and Posttraumatic Stress Disorder. Curr. Opin. Psychiatry 2019, 32, 510–517. [Google Scholar] [CrossRef]
- Elran-Barak, R.; Goldschmidt, A.B. Differences in Severity of Eating Disorder Symptoms between Adults with Depression and Adults with Anxiety. Eat. Weight Disord. 2021, 26, 1409–1416. [Google Scholar] [CrossRef]
- Sander, J.; Moessner, M.; Bauer, S. Depression, Anxiety and Eating Disorder-Related Impairment: Moderators in Female Adolescents and Young Adults. Int. J. Environ. Res. Public Health 2021, 18, 2779. [Google Scholar] [CrossRef] [PubMed]
- Elran-Barak, R. Analyses of Posts Written in Online Eating Disorder and Depression/Anxiety Moderated Communities: Emotional and Informational Communication before and during the COVID-19 Outbreak. Internet Interv. 2021, 26, 100438. [Google Scholar] [CrossRef]
- Rolland, B.; Haesebaert, F.; Zante, E.; Benyamina, A.; Haesebaert, J.; Franck, N. Global Changes and Factors of Increase in Caloric/Salty Food Intake, Screen Use, and Substance Use During the Early COVID-19 Containment Phase in the General Population in France: Survey Study. JMIR Public Health Surveill. 2020, 6, e19630. [Google Scholar] [CrossRef]
- Saadat, S.H.; Shahrezagamasaei, M.; Hatef, B.; Shahyad, S. Comparison of COVID-19 Anxiety, Health Anxiety, and Cognitive Emotion Regulation Strategies in Militaries and Civilians during COVID-19 Outbreaks. Health Educ. Health Promot. 2021, 9, 99–104. [Google Scholar]
- Huete Cordova, M.A. Trastorno de Conducta Alimentaria Durante La Pandemia Del SARS-CoV-2. Rev. Neuro-Psiquiatr. 2022, 85, 66–71. [Google Scholar] [CrossRef]
- Hart, L.M.; Jorm, A.F.; Paxton, S.J. Mental Health First Aid for Eating Disorders: Pilot Evaluation of a Training Program for the Public. BMC Psychiatry 2012, 12, 98. [Google Scholar] [CrossRef]
- Interpretation—EAT-26: Eating Attitudes Test & Eating Disorder Testing. Available online: https://www.eat-26.com/interpretation/ (accessed on 8 July 2022).
- Gewirtz-Meydan, A.; Spivak-Lavi, Z. Profiles of Sexual Disorders and Eating Disorder Symptoms: Associations With Body Image. J. Sex. Med. 2021, 18, 1364–1373. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | n (%) | |
|---|---|---|
| Age (years) * | 22 (19–32) | |
| Gender | ||
| Female | 25 (4.6) | |
| Male | 525 (95.5) | |
| Single | ||
| No | 147 (26.7) | |
| Yes | 403 (73.3) | |
| Religion | ||
| None | 82 (14.9) | |
| Catholic | 379 (68.9) | |
| Non-Catholic | 89 (16.2) | |
| Children | 150 (27.3) | |
| Alcoholism | 97 (17.6) | |
| Smoking | 37 (6.7) | |
| Comorbidity | ||
| Hypertension | 53 (9.6) | |
| Diabetes | 10 (1.8) | |
| BMI (categorized) † | ||
| Underweight/Normal | 323 (59.6) | |
| Overweight | 182 (33.6) | |
| Obesity | 37 (6.8) | |
| Personal mental health history | ||
| No | 543 (98.7) | |
| Yes | 7 (1.3) | |
| Family mental health history | ||
| No | 525 (95.5) | |
| Yes | 25 (4.6) | |
| Seeking mental health help | ||
| No | 504 (91.6) | |
| Yes | 46 (8.4) | |
| Trust in government to handle COVID-19 | ||
| Yes | 299 (54.4) | |
| No | 251 (45.6) | |
| Labor time† | ||
| 1 to 6 months | 138 (25.7) | |
| 7 to 12 months | 85 (15.8) | |
| 13 to 18 months | 116 (21.6) | |
| 19 months or more | 198 (36.9) | |
| Insomnia | ||
| No | 424 (77.1) | |
| Yes | 126 (22.9) | |
| Food insecurity | ||
| No | 282 (51.3) | |
| Yes | 268 (48.7) | |
| Physical activity | ||
| Low | 64 (11.6) | |
| Moderate | 39 (7.1) | |
| High | 447 (81.3) | |
| Resilience | ||
| Low | 311 (56.6) | |
| High | 239 (43.5) | |
| Fear of COVID-19 † | ||
| No | 424 (80.8) | |
| Yes | 101 (19.2) | |
| Burnout Syndrome | ||
| No | 499 (90.7) | |
| Yes | 51 (9.3) | |
| Anxiety | ||
| No | 430 (78.2) | |
| Yes | 120 (21.8) | |
| Depression | ||
| No | 387 (70.4) | |
| Yes | 163 (29.6) | |
| Suicidal risk † | ||
| No | 442 (86.0) | |
| Yes | 72 (14.0) | |
| Post-traumatic stress disorder | ||
| No | 509 (92.6) | |
| Yes | 41 (7.5) | |
| Eating disorder symptoms | ||
| No | 494 (89.8) | |
| Yes | 56 (10.2) | |
| Variables | Eating Disorder Symptoms | p * | ||
|---|---|---|---|---|
| No (n = 494) | Yes (n = 56) | |||
| n (%) | n (%) | |||
| Age (years) *** | 22 (19–32) | 22 (19–32) | 0.626 ** | |
| Gender | 0.325 | |||
| Female | 21 (84.0) | 4 (16.0) | ||
| Male | 473 (90.1) | 52 (9.9) | ||
| Single | 0.758 | |||
| No | 133 (90.5) | 14 (9.5) | ||
| Yes | 361 (89.6) | 42 (10.4) | ||
| Religion | 0.728 | |||
| None | 73 (89.0) | 9 (11.0) | ||
| Catholic | 339 (89.5) | 40 (10.6) | ||
| Non-Catholic | 82 (92.1) | 7 (7.9) | ||
| Children | 135 (90.0) | 15 (10.0) | 0.931 | |
| Alcoholism | 86 (88.7) | 11 (11.3) | 0.678 | |
| Smoking | 30 (81.1) | 7 (18.9) | 0.069 | |
| Comorbidity | ||||
| Hypertension | 48 (90.6) | 5 (9.4) | 0.850 | |
| Diabetes | 8 (80.0) | 2 (20.0) | 0.300 | |
| BMI (categorized) | 0.281 | |||
| Underweight/Normal | 296 (91.6) | 27 (8.4) | ||
| Overweight | 159 (87.4) | 23 (12.6) | ||
| Obesity | 34 (91.9) | 3 (8.1) | ||
| Personal mental health history | 0.105 | |||
| No | 489 (90.1) | 54 (9.9) | ||
| Yes | 5 (71.4) | 2 (28.6) | ||
| Family mental health history | 0.295 | |||
| No | 470 (89.5) | 55 (10.5) | ||
| Yes | 24 (96.0) | 1 (4.0) | ||
| Seeking mental health help | 0.728 | |||
| No | 452 (89.7) | 52 (10.3) | ||
| Yes | 42 (91.3) | 4 (8.7) | ||
| Trust in government to handle COVID-19 | 0.330 | |||
| Yes | 272 (91.0) | 27 (9.0) | ||
| No | 222 (88.5) | 29 (11.6) | ||
| Labor time | 0.022 | |||
| 1 to 6 months | 132 (95.7) | 6 (4.4) | ||
| 7 to 12 months | 71 (83.5) | 14 (16.5) | ||
| 13 to 18 months | 105 (90.5) | 11 (9.5) | ||
| 19 months or more | 174 (87.9) | 24 (12.1) | ||
| Insomnia | <0.001 | |||
| No | 393 (92.7) | 31 (7.3) | ||
| Yes | 101 (80.2) | 25 (19.8) | ||
| Food insecurity | 0.935 | |||
| No | 253 (89.7) | 29 (10.3) | ||
| Yes | 241 (89.9) | 27 (10.1) | ||
| Physical activity | 0.856 | |||
| Low | 57 (89.1) | 7 (10.9) | ||
| Moderate | 36 (92.3) | 3 (7.7) | ||
| High | 401 (89.7) | 46 (10.3) | ||
| Resilience | 0.448 | |||
| Low | 282 (90.7) | 29 (9.3) | ||
| High | 212 (88.7) | 27 (11.3) | ||
| Fear of COVID-19 | <0.001 | |||
| No | 394 (92.9) | 30 (7.1) | ||
| Yes | 77 (76.2) | 24 (23.8) | ||
| Burnout Syndrome | 0.005 | |||
| No | 454 (91.0) | 45 (9.0) | ||
| Yes | 40 (78.4) | 11 (21.6) | ||
| Anxiety | <0.001 | |||
| No | 397 (92.3) | 33 (7.7) | ||
| Yes | 97 (80.8) | 23 (19.2) | ||
| Depression | 0.009 | |||
| No | 356 (92.0) | 31 (8.0) | ||
| Yes | 138 (84.7) | 25 (15.3) | ||
| Suicidal risk | 0.810 | |||
| No | 397 (89.8) | 45 (10.2) | ||
| Yes | 64 (88.9) | 8 (11.1) | ||
| Post-traumatic stress disorder | <0.001 | |||
| No | 467 (91.8) | 42 (8.3) | ||
| Yes | 27 (65.9) | 14 (34.2) | ||
| Characteristics | Eating Disorder Symptoms | ||||||
|---|---|---|---|---|---|---|---|
| Simple Regression | Multiple Regression | ||||||
| PR | CI 95% | p * | PR | CI 95% | p * | ||
| Age (years) | 1.01 | 0.98–1.03 | 0.535 | ||||
| Gender | |||||||
| Female | Ref. | ||||||
| Male | 0.62 | 0.24–1.58 | 0.315 | ||||
| Single | |||||||
| No | Ref. | ||||||
| Yes | 1.09 | 0.62–1.94 | 0.759 | ||||
| Religion | |||||||
| None | Ref. | ||||||
| Catholic | 0.96 | 0.49–1.90 | 0.911 | ||||
| Non-Catholic | 0.72 | 0.28–1.84 | 0.488 | ||||
| Children | 0.98 | 0.56–1.71 | 0.931 | ||||
| Alcoholism | 1.14 | 0.61–2.13 | 0.677 | ||||
| Smoking | 1.98 | 0.90–4.37 | 0.091 | ||||
| Comorbidity | |||||||
| Hypertension | 0.92 | 0.38–2.20 | 0.851 | ||||
| Diabetes | 2.00 | 0.56–7.10 | 0.283 | ||||
| BMI (categorized) | |||||||
| Underweight/Normal | Ref. | ||||||
| Overweight | 1.51 | 0.89–2.56 | 0.124 | ||||
| Obesity | 0.97 | 0.31–3.05 | 0.958 | ||||
| Personal mental health history | |||||||
| No | Ref. | ||||||
| Yes | 2.87 | 0.87–9.53 | 0.085 | ||||
| Family mental health history | |||||||
| No | Ref. | ||||||
| Yes | 0.38 | 0.05–2.65 | 0.330 | ||||
| Seeking mental health help | |||||||
| No | Ref. | ||||||
| Yes | 0.84 | 0.32–2.23 | 0.730 | ||||
| Trust in government to handle COVID-19 | |||||||
| Yes | Ref. | ||||||
| No | 1.28 | 0.78–2.10 | 0.331 | ||||
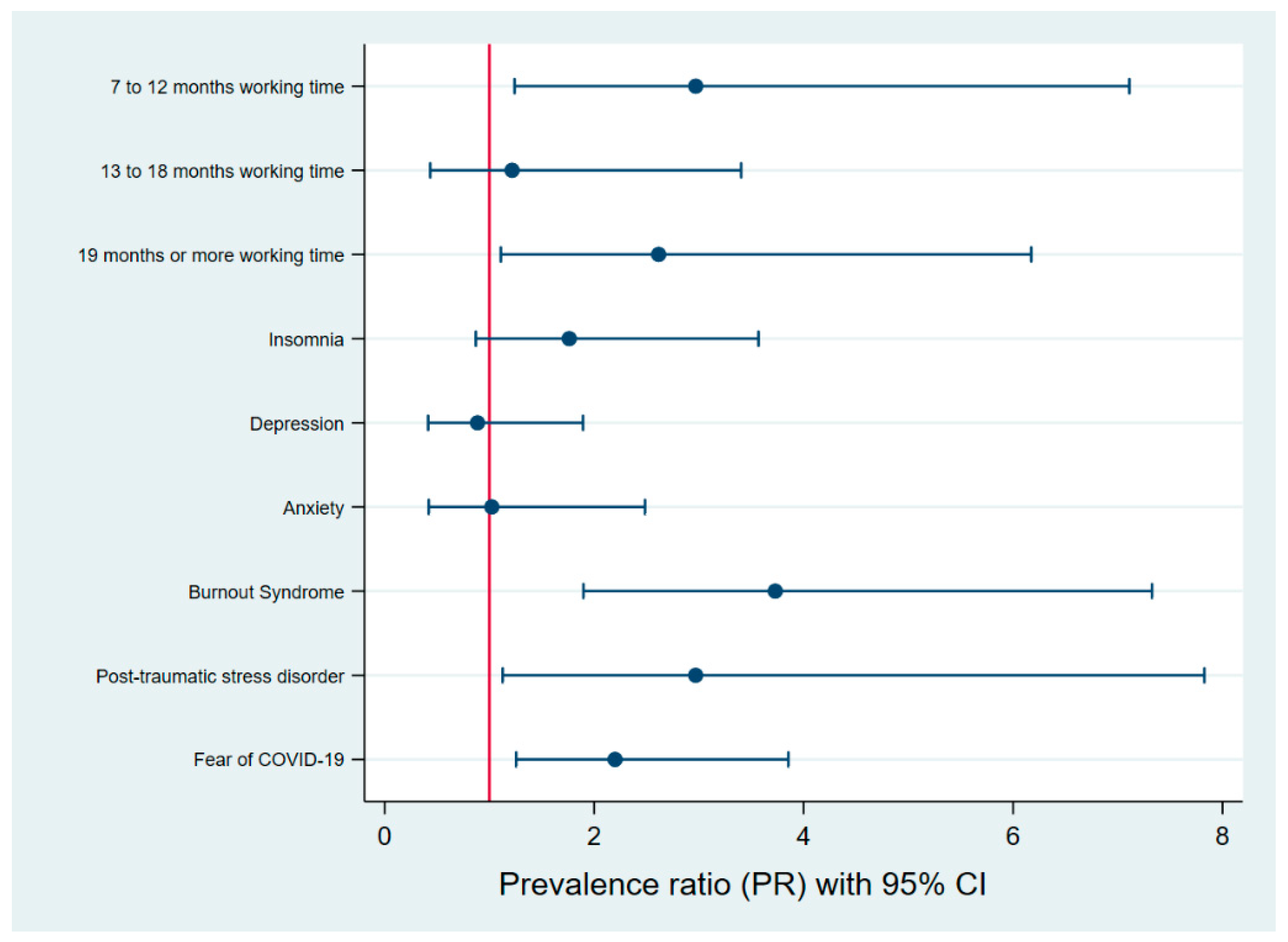
| Labor time | |||||||
| 1 to 6 months | Ref. | Ref. | |||||
| 7 to 12 months | 3.79 | 1.51–9.49 | 0.004 | 2.97 | 1.24–7.11 | 0.015 | |
| 13 to 18 months | 2.18 | 0.83–5.72 | 0.113 | 1.22 | 0.44–3.40 | 0.708 | |
| 19 months or more | 2.79 | 1.17–6.65 | 0.012 | 2.62 | 1.11–6.17 | 0.028 | |
| Insomnia | |||||||
| No | Ref. | Ref. | |||||
| Yes | 2.71 | 1.67–4.42 | <0.001 | 1.76 | 0.87–3.57 | 0.115 | |
| Food insecurity | |||||||
| No | Ref. | ||||||
| Yes | 0.98 | 0.60–1.61 | 0.935 | ||||
| Physical activity | |||||||
| Low | Ref. | ||||||
| Moderate | 0.70 | 0.19–2.56 | 0.594 | ||||
| High | 0.94 | 0.44–1.99 | 0.874 | ||||
| Resilience | |||||||
| Low | Ref. | ||||||
| High | 1.21 | 0.74–1.99 | 0.449 | ||||
| Fear of COVID-19 | |||||||
| No | Ref. | Ref. | |||||
| Yes | 3.36 | 2.05–5.49 | <0.001 | 2.20 | 1.26–3.85 | 0.006 | |
| Burnout Syndrome | |||||||
| No | Ref. | Ref. | |||||
| Yes | 2.39 | 1.32–4.33 | 0.004 | 3.73 | 1.90–7.33 | <0.001 | |
| Anxiety | |||||||
| No | Ref. | Ref. | |||||
| Yes | 2.50 | 1.53–4.09 | <0.001 | 1.02 | 0.42–2.49 | 0.960 | |
| Depression | |||||||
| No | Ref. | Ref. | |||||
| Yes | 1.91 | 1.17–3.14 | 0.010 | 0.89 | 0.42–1.89 | 0.756 | |
| Suicidal risk | |||||||
| No | Ref. | ||||||
| Yes | 1.09 | 0.54–2.22 | 0.809 | ||||
| Post-traumatic stress disorder | |||||||
| No | Ref. | Ref. | |||||
| Yes | 4.14 | 2.47–6.92 | <0.001 | 2.97 | 1.13–7.83 | 0.028 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Valladares-Garrido, M.J.; León-Figueroa, D.A.; Picón-Reátegui, C.K.; García-Vicente, A.; Valladares-Garrido, D.; Failoc-Rojas, V.E.; Pereira-Victorio, C.J. Prevalence and Factors Associated with Eating Disorders in Military First Line of Defense against COVID-19: A Cross-Sectional Study during the Second Epidemic Wave in Peru. Int. J. Environ. Res. Public Health 2023, 20, 2848. https://doi.org/10.3390/ijerph20042848
Valladares-Garrido MJ, León-Figueroa DA, Picón-Reátegui CK, García-Vicente A, Valladares-Garrido D, Failoc-Rojas VE, Pereira-Victorio CJ. Prevalence and Factors Associated with Eating Disorders in Military First Line of Defense against COVID-19: A Cross-Sectional Study during the Second Epidemic Wave in Peru. International Journal of Environmental Research and Public Health. 2023; 20(4):2848. https://doi.org/10.3390/ijerph20042848
Chicago/Turabian StyleValladares-Garrido, Mario J., Darwin A. León-Figueroa, Cinthia Karina Picón-Reátegui, Abigaíl García-Vicente, Danai Valladares-Garrido, Virgilio E. Failoc-Rojas, and César Johan Pereira-Victorio. 2023. "Prevalence and Factors Associated with Eating Disorders in Military First Line of Defense against COVID-19: A Cross-Sectional Study during the Second Epidemic Wave in Peru" International Journal of Environmental Research and Public Health 20, no. 4: 2848. https://doi.org/10.3390/ijerph20042848
APA StyleValladares-Garrido, M. J., León-Figueroa, D. A., Picón-Reátegui, C. K., García-Vicente, A., Valladares-Garrido, D., Failoc-Rojas, V. E., & Pereira-Victorio, C. J. (2023). Prevalence and Factors Associated with Eating Disorders in Military First Line of Defense against COVID-19: A Cross-Sectional Study during the Second Epidemic Wave in Peru. International Journal of Environmental Research and Public Health, 20(4), 2848. https://doi.org/10.3390/ijerph20042848







