PEEP-ZEEP Compared with Bag Squeezing and Chest Compression in Mechanically Ventilated Cardiac Patients: Randomized Crossover Clinical Trial
Abstract
1. Introduction
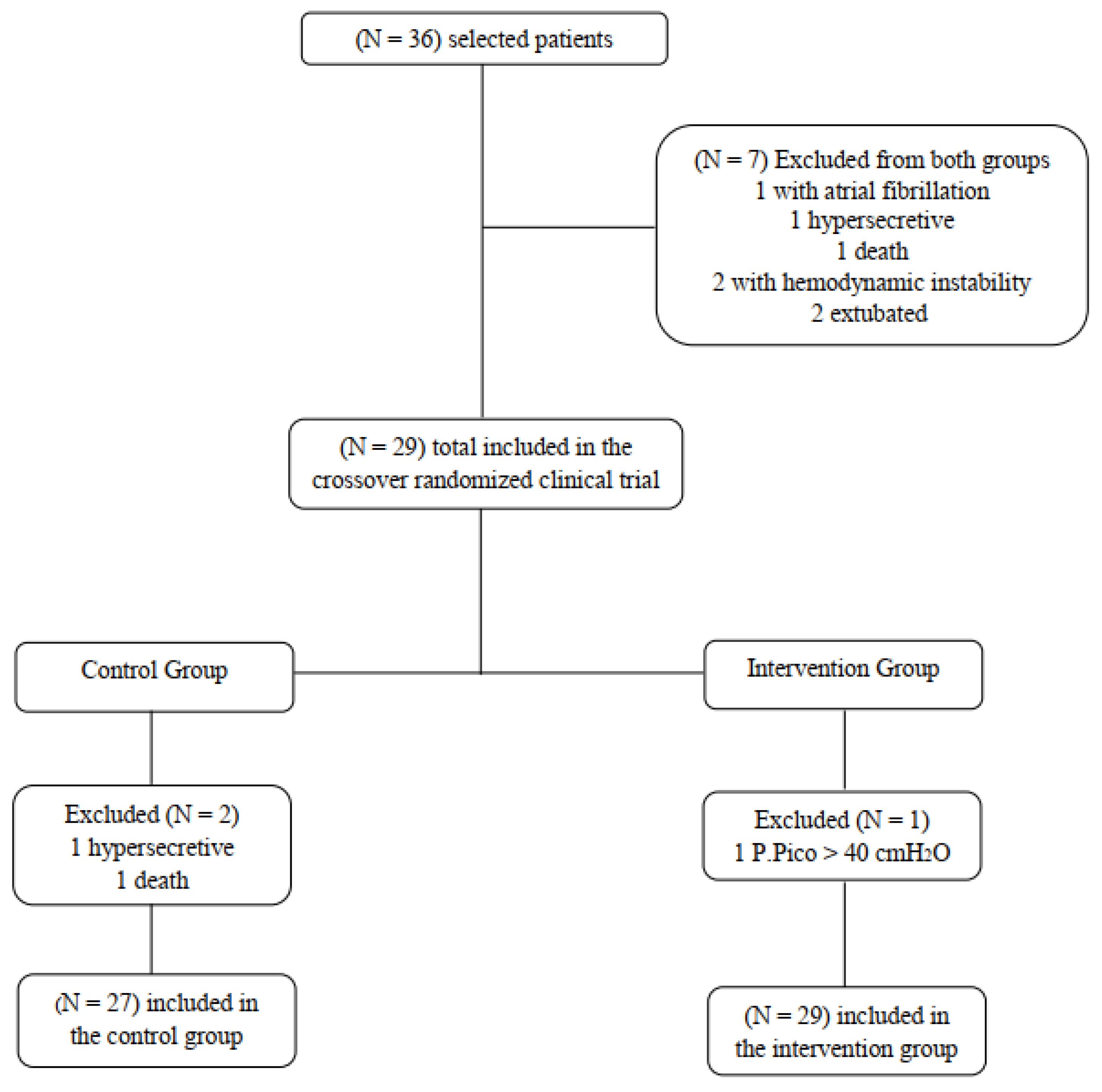
2. Methods
Statistical Analysis
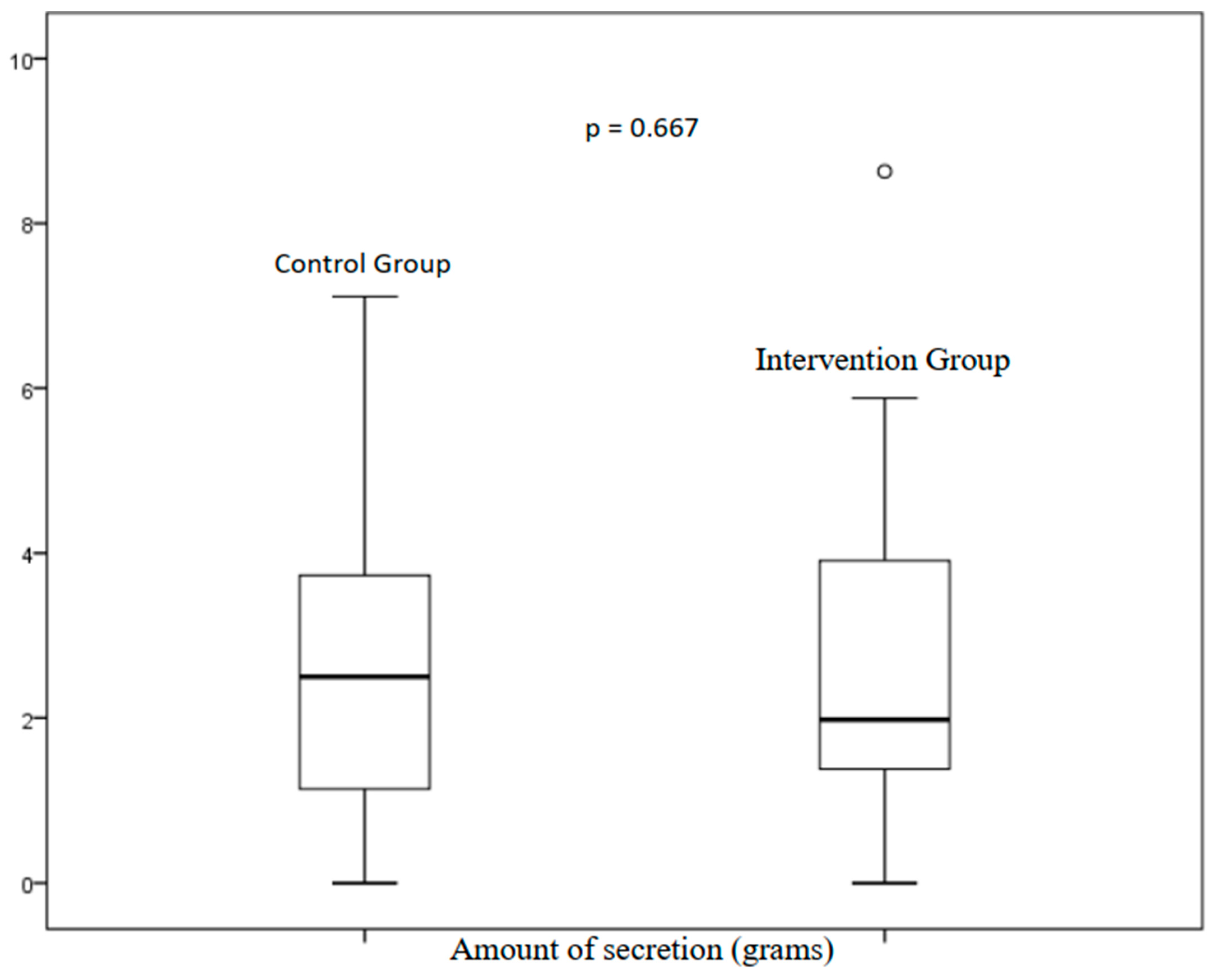
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Barbas, C.S.V.; Ísola, A.M.; de Carvalho Farias, A.M.; Cavalcanti, A.B.; Gama, A.M.C.; Duarte, A.C.M.; Vianna, A.; Neto, A.S.; de Arruda Bravim, B.; Pinheiro, B.V.; et al. Diretrizes Brasileiras de Ventilação Mecânica; Associação de Medicina Intensiva Brasileira (AMIB): Sao Paulo, Brazil; Sociedade Brasileira de Pneumologia e Tisiologia (SBPT): Brasilia, Brazil, 2013. [Google Scholar]
- Ciccarelli, M.; Dawson, D.; Falcao-Pires, I.; Giacca, M.; Hamdani, N.; Heymans, S.; Hooghiemstra, A.; Leeuwis, A.; Hermkens, D.; Tocchetti, C.G.; et al. Reciprocal organ interactions during heart failure: A position paper from the ESC Working Group on Myocardial Function. Cardiovasc. Res. 2021, 117, 2416–2433. [Google Scholar] [CrossRef] [PubMed]
- Rohde, L.E.P.; Montera, M.W.; Bocchi, E.A.; Clausell, N.O.; de Albuquerque, D.C.; Rassi, S.; Colafranceschi, A.S.; de Freitas Junior, A.F.; Ferraz, A.S.; Biolo, A.; et al. Diretriz Brasileira de Insuficiência Cardíaca Crônica e Aguda Diretrizes. Arq. Bras. Cardiol. 2018, 111, 436–539. [Google Scholar] [PubMed]
- Jiang, X.; Cheng, X.; Zhang, W. Unilateral cardiogenic pulmonary edema caused by acute mitral valve prolapse. Medicine 2021, 100, e24622. [Google Scholar] [CrossRef] [PubMed]
- Carolina, A.; Oliveira, O.; Lorena, D.M. Effects of manual chest compression on expiratory flow bias during the positive end-expiratory pressure-zero end-expiratory pressure maneuver in patients on mechanical ventilation. J. Bras. Pneumol. 2019, 45, 1–9. [Google Scholar]
- Dennis, D.; Jacob, W.; Budgeon, C. Ventilator versus Manual Hyperinflation in Clearing Sputum in Ventilated Intensive Care Unit Patients. Anaesth. Intensiv. Care 2012, 40, 142–149. [Google Scholar] [CrossRef] [PubMed]
- Carlos, L.; Júnior, S. Efeitos da compressão torácica manual versus a manobra de PEEP-ZEEP na complacência do sistema respiratório e na oxigenação de pacientes submetidos à ventilação mecânica invasiva. Rev. Bras. Ter. Intensiv. 2009, 21, 155–161. [Google Scholar]
- Schulz, K.F.; Altman, D.G.; Moher, D.; Consort Group. Withdrawn: Consort 2010 statement: Updated guidelines for reporting parallel group randomised trials. Int. J. Surg. 2010, 152, 726–732. [Google Scholar] [CrossRef]
- Favretto, D.O.; Cristina, R.; Pereira, D.C.; Rita, S.; Canini, S.; Garbin, L.M.; Martins, F.T.M.; Dalri, M.C.B. Endotracheal suction in intubated critically ill adult patients undergoing mechanical ventilation: A systematic review. Rev. Lat.-Am. Enferm. 2012, 20, 997–1007. [Google Scholar] [CrossRef] [PubMed]
- Lobo, D.M.L.; Cavalcante, L.A.; Mont’Alverne, D.G.B. Applicability of bag squeezing and zeep maneuvers in mechanically ventilated patients. Rev. Bras. Ter. Intensiv. 2010, 22, 186–191. [Google Scholar] [CrossRef]
- Dias, C.M.; Siqueira, M.; Regina, T.; Gontijo, L.C. Bronchial hygiene technique with manual hyperinflation and thoracic compression: Effectiveness and safety. Rev. Bras. Ter. Intensive 2011, 23, 190–198. [Google Scholar] [CrossRef]
- Volpe, M.S.; Guimara, F.S. Airway Clearance Techniques for Mechanically Ventilated Patients: Insights for Optimization. Respir. Care 2020, 65, 1174–1188. [Google Scholar] [CrossRef] [PubMed]
- Précoma, D.B.; Oliveira, G.M.M.d.; Simão, A.F.; Dutra, O.P.; Coelho, O.R.; Izar, M.C.d.O.; Póvoa, R.M.d.S.; Giuliano, I.d.C.B.; Filho, A.C.d.A.; Machado, C.A.; et al. Atualização da Diretriz de Prevenção Cardiovascular da Sociedade Brasileira de Cardiologia—2019 Atualização. Arq. Bras. Cardiol. 2019, 113, 787–891. [Google Scholar] [PubMed]
- Parsanathan, R.; Jain, S.K. Novel Invasive and Noninvasive Cardiac-Specific Biomarkers in Obesity and Cardiovascular Diseases. Metab. Syndr. Relat. Disord. 2020, 18, 10–30. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, A.C.C.; Sousa, J.M.A. Cardiopatia isquêmica. Rev. Bras. Hipertens. 2001, 8, 297–305. [Google Scholar]
- Herbst-rodrigues, M.V.; Carvalho, V.O.; Otávio, J.; Auler, C.; Ignez, M.; Feltrim, Z. PEEP-ZEEP technique: Cardiorespiratory repercussions in mechanically ventilated patients submitted to a coronary artery bypass graft surgery. J. Cardiothorac. Surg. 2011, 6, 108. [Google Scholar] [CrossRef] [PubMed]
- Asmann, C.B.; Vieira, P.J.C.; Kutchak, F.; Rieder, M.M.; Forgiarini, S.G.I.; Junior Forgiarini, L.A. Hiperinsuflação pulmonar com ventilador mecânico versus aspiração traqueal isolada na higiene brônquica de pacientes submetidos à ventilação mecânica. Rev. Bras. Ter. Intensive 2016, 28, 27–32. [Google Scholar]
- Lemes, D.A.; Zin, W.A.; Guimarães, F.S. Hyperinflation using pressure support ventilation improves secretion clearance and respiratory mechanics in ventilated patients with pulmonary infection: A randomised crossover trial. Aust. J. Physiother. 2009, 55, 249–254. [Google Scholar] [CrossRef] [PubMed]
- Volpe, M.S.; Naves, J.M.; Ribeiro, G.G.; Ruas, G.; Tucci, R. Effects of manual hyperinflation, clinical practice versus expert recommendation, on displacement of mucus simulant: A laboratory study. PLoS ONE 2018, 13, e0191787. [Google Scholar] [CrossRef] [PubMed]
- Khalil, N.S.; Ismaeel, M.S.; Askar, A.H.; Sayed, M.S. Effects of manual hyperinflation with rib cage compression and endotracheal suctioning on arterial blood gas parameters in mechanically ventilated patients at a university hospital, Egypt. Egypt. J. Bronchol. 2021, 15, 47. [Google Scholar] [CrossRef]
- Ortiz, T.D.A.; Forti, G.; Volpe, M.S.; Roberto, C.; Carvalho, R.; Brito, M. Experimental study on the efficiency and safety of the manual hyperinflation maneuver as a secretion clearance technique. J. Bras. Pneumol. 2013, 39, 205–213. [Google Scholar] [CrossRef] [PubMed]
| Variable | N = 36 (%) |
|---|---|
| Age * | 70.3 ± 10.6 |
| Sex | |
| Female | 15 (10.4) |
| Male | 21 (14.6) |
| BMI | |
| Underweight | 4 (2.8) |
| Normal | 12 (8.3) |
| Overweight | 7 (4.9) |
| Obesity | 12 (8.3) |
| Risk factors | |
| Smoking | 14 (9.7) |
| Hypertension | 29 (20.1) |
| Diabetes mellitus | 17 (11.8) |
| Dyslipidemia | 26 (18.1) |
| Reason for hospitalization | |
| Ischemic heart disease | 15 (10.4) |
| Dilated cardiomyopathy | 2 (1.4) |
| Valve disease | 6 (4.2) |
| PAD | 3 (2.1) |
| Decompensated heart failure | 1 (0.7) |
| Others | 5 (3.5) |
| Associated diseases | |
| Ischemic heart disease | 4 (2.8) |
| Kidney disease | 15 (10.4) |
| CAD | 8 (5.6) |
| Arrhythmias | 7 (4.9) |
| Others | 20 (13.9) |
| Cardiac surgery | |
| Total postoperative | 4 (2.8) |
| Complications during hospitalization | |
| Cardiopulmonary arrest | 14 (9.7) |
| Arrhythmias | 10 (6.9) |
| Respiratory failure | 9 (6.3) |
| Cardiogenic shock | 5 (3.5) |
| APE | 6 (4.2) |
| Others | 16 (11.1) |
| MV days * | 5.3 ± 3.1 |
| Drug class used | |
| Vasoactive drug | 17 (11.8) |
| Sedatives | 15 (10.4) |
| Antibiotics | 32 (22.2) |
| Anticoagulants | 6 (4.2) |
| Others | 3 (2.1) |
| Variable | N = 36 (%) | |
|---|---|---|
| VM Mode | Control Group | Intervention Group |
| PCV | 13 (41.9) | 12 (40.0) |
| VCV | 5 (16.1) | 5 (16.7) |
| PSV | 11 (35.5) | 9 (30) |
| IPPV | 2 (6.5) | 4 (13.3) |
| Ventilation adjustment | ||
| PEEP * | 6.9 ± 1.3 | 6.7 ± 1.1 |
| FiO2 * | 35.1 ± 13.2 | 35.3 ± 12.9 |
| Control Group (N = 27) | Intervention Group (N = 29) | Group | Time | G*M | |||
|---|---|---|---|---|---|---|---|
| Variable | Before | After | Before | After | p Value | ||
| SBP (mmHg) * | 121 ± 3.6 | 129.1 ± 4.2 | 119.2 ± 4.7 | 126.2 ± 6.2 | 0.592 | 0.083 | 0.845 |
| DBP (mmHg) * | 64.7 ± 2.5 | 72.2 ± 3.8 | 64.7 ± 2.7 | 69.5 ± 3.3 | 0.631 | 0.024 | 0.609 |
| MAP (mmHg) * | 82 ± 2.1 | 90 ± 3.1 | 79.9 ± 2.4 | 87.9 ± 4 | 0.428 | 0.004 | 0.998 |
| HR (bpm) * | 92 ± 4.5 | 94.4 ± 3.6 | 92.8 ± 4.3 | 98.9 ± 3.7 | 0.386 | 0.173 | 0.299 |
| SpO2 (%) * | 97.3 ± 0.4 | 97.6 ± 0.4 | 96.5 ± 0.5 | 96.8 ± 0.6 | 0.210 | 0.394 | 0.903 |
| RR (bpm) * | 22 ± 0.8 | 22.4 ± 0.9 | 21 ± 0.7 | 22.8 ± 0.6 | 0.798 | 0.041 | 0.154 |
| Control Group (N = 27) | Intervention Group (N = 29) | Group | Moment | G*M | |||
|---|---|---|---|---|---|---|---|
| Variable | Before | After | Before | After | p Value | ||
| TV * | 425.19 ± 11.9 | 443.1 ± 14.3 | 410.7 ± 11.7 | 442.5 ± 18.9 | 0.384 | 0.052 | 0.479 |
| PPeak * | 20.9 ± 0.9 | 19.7 ± 0.9 | 21.4 ± 1.1 | 20.8 ± 1.0 | 0.202 | 0.011 | 0.333 |
| P Plateau * | 18.5 ± 0.9 | 18.9 ± 0. 8 | 18.3 ± 0.9 | 18.4 ± 0.8 | 0.640 | 0.644 | 0.787 |
| DP * | 11.50 ± 0.7 | 11.52 ± 7.6 | 11.4 ± 0.9 | 12 ± 0.8 | 0.701 | 0.518 | 0.531 |
| Cst * | 36.5 ± 2. 8 | 36.3 ± 2.6 | 37.3 ± 3.7 | 35.2 ± 3.7 | 0.963 | 0.373 | 0.597 |
| Cdyn * | 26.9 ± 1.9 | 33.8 ± 2.7 | 30.3 ± 3.6 | 29.4 ± 4.4 | 0.902 | 0.122 | 0.004 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Oliveira, T.F.; Peringer, V.S.; Forgiarini Junior, L.A.; Eibel, B. PEEP-ZEEP Compared with Bag Squeezing and Chest Compression in Mechanically Ventilated Cardiac Patients: Randomized Crossover Clinical Trial. Int. J. Environ. Res. Public Health 2023, 20, 2824. https://doi.org/10.3390/ijerph20042824
de Oliveira TF, Peringer VS, Forgiarini Junior LA, Eibel B. PEEP-ZEEP Compared with Bag Squeezing and Chest Compression in Mechanically Ventilated Cardiac Patients: Randomized Crossover Clinical Trial. International Journal of Environmental Research and Public Health. 2023; 20(4):2824. https://doi.org/10.3390/ijerph20042824
Chicago/Turabian Stylede Oliveira, Taís Flores, Vinicius Serra Peringer, Luiz Alberto Forgiarini Junior, and Bruna Eibel. 2023. "PEEP-ZEEP Compared with Bag Squeezing and Chest Compression in Mechanically Ventilated Cardiac Patients: Randomized Crossover Clinical Trial" International Journal of Environmental Research and Public Health 20, no. 4: 2824. https://doi.org/10.3390/ijerph20042824
APA Stylede Oliveira, T. F., Peringer, V. S., Forgiarini Junior, L. A., & Eibel, B. (2023). PEEP-ZEEP Compared with Bag Squeezing and Chest Compression in Mechanically Ventilated Cardiac Patients: Randomized Crossover Clinical Trial. International Journal of Environmental Research and Public Health, 20(4), 2824. https://doi.org/10.3390/ijerph20042824







