Influence of COVID-19-Related Interventions on the Number of Inpatients with Acute Viral Respiratory Infections: Using Interrupted Time Series Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data
- (1)
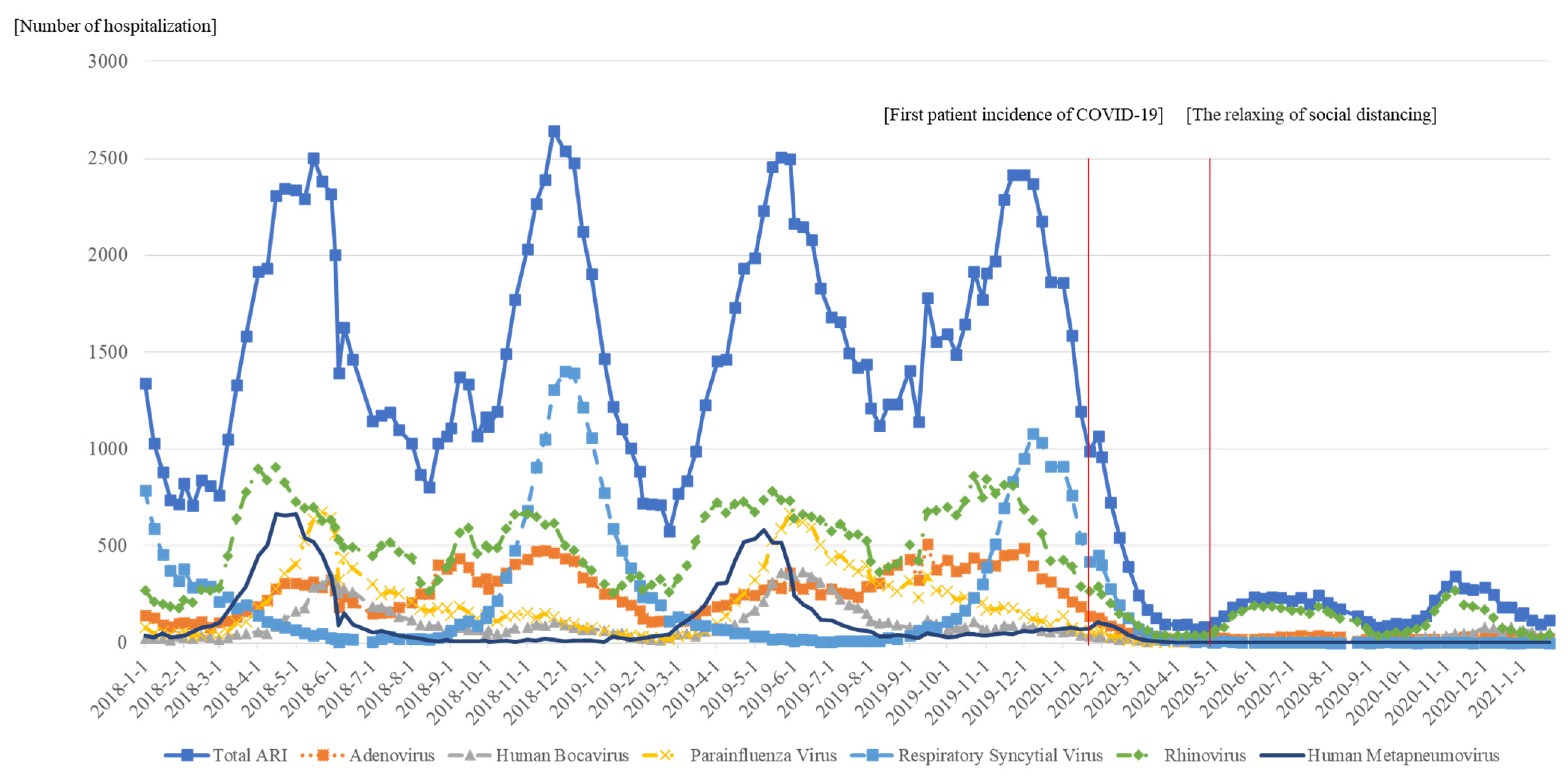
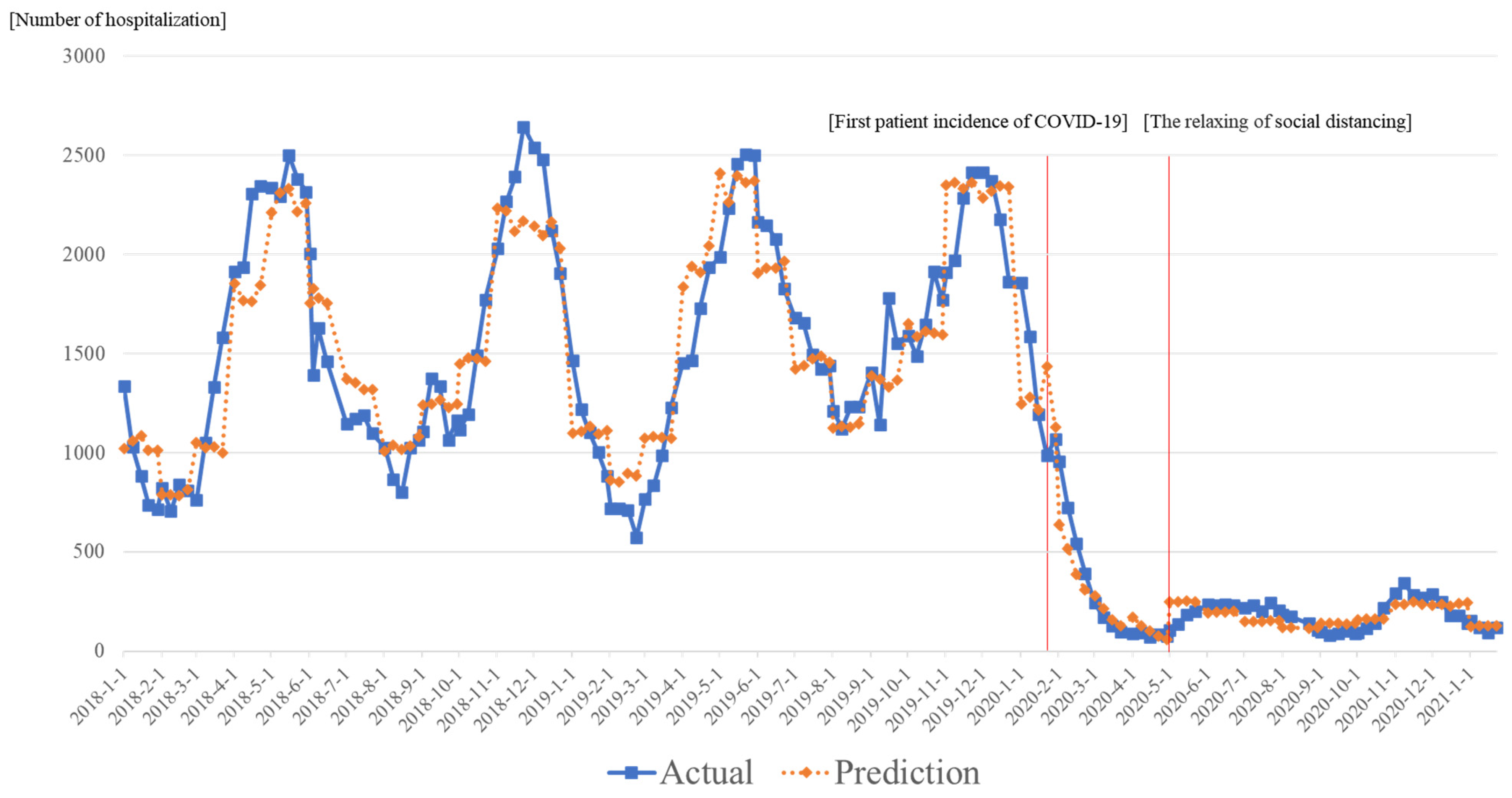
- Period 1: Week 1 of January 2018 to Week 3 of January 2020. (Before the first incident of COVID-19.)
- (2)
- Period 2: Week 4 of January 2020 to Week 4 of April 2020. (After the first incident of COVID-19 and during the implementation of the social distancing policy.)
- (3)
- Period 3: Week 1 of May 2020 to Week 4 of January 2021. (The relaxing of the social distancing policy.)
2.2. Study Variables
2.3. Statistical Analysis
3. Results
4. Discussion
4.1. Finding
4.2. Interpretations
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19. 2020. Available online: https://bit.ly/3EWpZ4g (accessed on 28 September 2021).
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef] [PubMed]
- WHO. WHO Coronavirus (COVID-19) Dashboard. 2020. Available online: https://covid19.who.int/ (accessed on 28 September 2021).
- Her, M. How is COVID-19 affecting South Korea? What is our current strategy? Disaster Med. Public Health Prep. 2020, 14, 684–686. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.-A. Social Distancing and Public Health Guidelines at Workplaces in Korea: Responses to Coronavirus Disease-19. Saf. Health Work 2020, 11, 275–283. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Ko, Y.; Kim, Y.-J.; Jung, E. The impact of social distancing and public behavior changes on COVID-19 transmission dynamics in the Republic of Korea. PLoS ONE 2020, 15, e0238684. [Google Scholar] [CrossRef] [PubMed]
- KCDC. Overview of Social Distancing System. 2021. Available online: http://ncov.mohw.go.kr/en/socdisBoardView.do?brdId=19&brdGubun=191&dataGubun=191&ncvContSeq=&contSeq=&board_id= (accessed on 10 July 2021).
- Lee, H.; Lee, H.; Song, K.H.; Kim, E.S.; Park, J.S.; Jung, J.; Kim, H.B. Impact of public health interventions on seasonal influenza activity during the COVID-19 outbreak in Korea. Clin. Infect. Dis. 2021, 73, e132–e140. [Google Scholar] [CrossRef]
- Feng, S.; Shen, C.; Xia, N.; Song, W.; Fan, M.; Cowling, B.J. Rational use of face masks in the COVID-19 pandemic. Lancet Respir. Med. 2020, 8, 434–436. [Google Scholar] [CrossRef]
- Ahmed, F.; Zviedrite, N.; Uzicanin, A. Effectiveness of workplace social distancing measures in reducing influenza transmission: A systematic review. BMC Public Health 2018, 18, 518. [Google Scholar] [CrossRef]
- Rashid, H.; Ridda, I.; King, C.; Begun, M.; Tekin, H.; Wood, J.G.; Booy, R. Evidence compendium and advice on social distancing and other related measures for response to an influenza pandemic. Paediatr. Respir. Rev. 2015, 16, 119–126. [Google Scholar] [CrossRef]
- Lee, W.R.; Kim, L.H.; Lee, G.M.; Cheon, J.; Kwon, Y.D.; Noh, J.W.; Yoo, K.B. Effect of COVID-19-Related Interventions on the Incidence of Infectious Eye Diseases: Analysis of Nationwide Infectious Disease Incidence Monitoring Data. Int. J. Public Health 2022, 67, 1605211. [Google Scholar] [CrossRef]
- Hatoun, J.; Correa, E.T.; Donahue, S.M.A.; Vernacchio, L. Social distancing for COVID-19 and diagnoses of other infectious diseases in children. Pediatrics 2020, 146, e2020006460. [Google Scholar] [CrossRef]
- Park, S.; Michelow, I.C.; Choe, Y.J. Shifting patterns of respiratory virus activity following social distancing measures for coronavirus disease 2019 in South Korea. J. Infect. Dis. 2021, 224, 1900–1906. [Google Scholar] [CrossRef]
- Kuitunen, I.; Artama, M.; Mäkelä, L.; Backman, K.; Heiskanen-Kosma, T.; Renko, M. Effect of social distancing due to the COVID-19 pandemic on the incidence of viral respiratory tract infections in children in Finland during early 2020. Pediatr. Infect. Dis. J. 2020, 39, e423–e427. [Google Scholar] [CrossRef] [PubMed]
- KCDC. Infectious Disease Potal. 2021. Available online: https://www.kdca.go.kr/npt/biz/npp/iss/influenzaStatisticsMain.do (accessed on 28 September 2021).
- KCDC. Infectious Disease Monitoring System. 2020. Available online: http://www.cdc.go.kr/contents.es?mid=a20301110300 (accessed on 28 September 2021).
- Mäkinen, T.M.; Juvonen, R.; Jokelainen, J.; Harju, T.H.; Peitso, A.; Bloigu, A.; Silvennoinen-Kassinen, S.; Leinonen, M.; Hassi, J. Cold temperature and low humidity are associated with increased occurrence of respiratory tract infections. Respir. Med. 2009, 103, 456–462. [Google Scholar] [CrossRef] [PubMed]
- Pönkä, A. Absenteeism and respiratory disease among children and adults in Helsinki in relation to low-level air pollution and temperature. Environ. Res. 1990, 52, 34–46. [Google Scholar] [CrossRef] [PubMed]
- Pica, N.; Bouvier, N.M. Environmental factors affecting the transmission of respiratory viruses. Curr. Opin. Virol. 2012, 2, 90–95. [Google Scholar] [CrossRef]
- Paynter, S. Humidity and respiratory virus transmission in tropical and temperate settings. Epidemiol. Infect. 2015, 143, 1110–1118. [Google Scholar] [CrossRef]
- Wagner, A.K.; Soumerai, S.B.; Zhang, F.; Ross-Degnan, D. Segmented regression analysis of interrupted time series studies in medication use research. J. Clin. Pharm. Ther. 2002, 27, 299–309. [Google Scholar] [CrossRef]
- Bogard, M. Marginal Effects vs Odds Ratio. Econom Sense. 2016. Available online: http://econometricsense.blogspot.com/2016/03/marginal-effects-vs-odds-ratios_11.html (accessed on 20 September 2021).
- Chiu, N.-C.; Chi, H.; Tai, Y.-L.; Peng, C.-C.; Tseng, C.-Y.; Chen, C.-C.; Tan, B.F.; Lin, C.-Y. Impact of wearing masks, hand hygiene, and social distancing on influenza, enterovirus, and all-cause pneumonia during the coronavirus pandemic: Retrospective national epidemiological surveillance study. J. Med. Internet Res. 2020, 22, e21257. [Google Scholar] [CrossRef]
- Chu, D.K.; Akl, E.A.; Duda, S.; Solo, K.; Yaacoub, S.; Schünemann, H.J. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: A systematic review and meta-analysis. Lancet 2020, 395, 1973–1987. [Google Scholar] [CrossRef]
- Cowling, B.J.; Ali, S.T.; Ng, T.W.; Tsang, T.K.; Li, J.C.M.; Fong, M.W.; Liao, Q.; Kwan, M.Y.W.; Lee, S.L.; Chiu, S.S. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: An observational study. Lancet Public Health 2020, 5, e279–e288. [Google Scholar] [CrossRef]
- Murillo-Zamora, E.; Guzmán-Esquivel, J.; Sánchez-Piña, R.A.; Cedeño-Laurent, G.; Delgado-Enciso, I.; Mendoza-Cano, O. Physical distancing reduced the incidence of influenza and supports a favorable impact on SARS-CoV-2 spread in Mexico. J. Infect. Dev. Ctries. 2020, 14, 953–956. [Google Scholar] [CrossRef] [PubMed]
- Akhtar, J.; Garcia, A.L.; Saenz, L.; Kuravi, S.; Shu, F.; Kota, K. Can face masks offer protection from airborne sneeze and cough droplets in close-up, face-to-face human interactions?—A quantitative study. Phys. Fluids 2020, 32, 127112. [Google Scholar] [CrossRef] [PubMed]
- Bandiera, L.; Pavar, G.; Pisetta, G.; Otomo, S.; Mangano, E.; Seckl, J.R.; Digard, P.; Molinari, E.; Menolascina, F.; Viola, I.M. Face coverings and respiratory tract droplet dispersion. R. Soc. Open Sci. 2020, 7, 201663. [Google Scholar] [CrossRef] [PubMed]
- Jefferson, T.; Del Mar, C.B.; Dooley, L.; Ferroni, E.; Al-Ansary, L.A.; Bawazeer, G.; Driel, M.L.; Jones, M.A.; Thorning, S.; Beller, E.M.; et al. Physical interventions to interrupt or reduce the spread of respiratory viruses. Cochrane Database Syst. Rev. 2020, 11, CD006207. [Google Scholar] [CrossRef]
- Islam, N.; Sharp, S.; Chowell, G.; Shabnam, S.; Kawachi, I.; Lacey, B.; Massaro, J.M.; D’Agostino, R.B.; White, M. Physical distancing interventions and incidence of coronavirus disease 2019: Natural experiment in 149 countries. BMJ 2020, 370, m2743. [Google Scholar] [CrossRef]
- Coroiu, A.; Moran, C.; Campbell, T.; Geller, A.C. Barriers and facilitators of adherence to social distancing recommendations during COVID-19 among a large international sample of adults. PLoS ONE 2020, 15, e0239795. [Google Scholar] [CrossRef]
- Jang, W.M.; Jang, D.H.; Lee, J.Y. Social distancing and transmission-reducing practices during the 2019 coronavirus disease and 2015 Middle East respiratory syndrome coronavirus outbreaks in Korea. J. Korean Med. Sci. 2020, 35, e220. [Google Scholar] [CrossRef]
- Kim, H.M.; Lee, H.; Lee, N.; Kim, E.-J. COVID-19 Impact on Influenza and Respiratory Virus-es Surveillance. 2020. Available online: https://www.kdca.go.kr/filepath/boardDownload.es?bid=0031&list_no=711404&seq=1 (accessed on 30 September 2021).
- Jeon, I.S.; Cho, W.J.; Lee, J.; Kim, H.M. Epidemiology and clinical severity of the hospitalized children with viral croup. Pediatr. Infect Vaccine 2018, 25, 8–16. [Google Scholar] [CrossRef]
- Lim, Y.K.; Kweon, O.J.; Kim, H.R.; Kim, T.-H.; Lee, M.-K. Clinical features, epidemiology, and climatic impact of genotype-specific human metapneumovirus infections: Long-term surveillance of hospitalized patients in South Korea. Clin. Infect. Dis. 2020, 70, 2683–2694. [Google Scholar] [CrossRef]
- Cheon, J.M.; Yang, Y.J.; Yoon, Y.S.; Lee, E.-S.; Lee, J.-H.; Huh, Y.; Mun, J.-W.; Jhung, C.-H.; Hyun, B.-R. Influence of fine particulate dust particulate matter 10 on respiratory virus infection in the Republic of Korea. Korean J. Fam. Pract. 2019, 9, 454–459. [Google Scholar] [CrossRef]
- Kasdan, D.O.; Campbell, J.W. Dataveillant collectivism and the coronavirus in Korea: Values, biases, and socio-cultural foundations of containment efforts. Adm. Theory Prax. 2020, 42, 604–613. [Google Scholar] [CrossRef]
| Total Acute Respiratory Infection | Adenovirus | Human Bocavirus | Parainfluenza Virus | Respiratory Syncytial Virus | Rhinovirus | Human Metapneumovirus | |
|---|---|---|---|---|---|---|---|
| Time | 0.002 ** | 0.003 *** | 0.003 *** | 0.004 *** | 0 | 0.003 *** | 0.001 |
| Intervention 1 | 0.398 | 0.031 | 0.252 | 0.341 | 0.23 | 0.3 | 1.787 *** |
| Time after i = Intervention 1 | −0.262 *** | −0.198 *** | −0.208 *** | −0.32 *** | −0.158 *** | −0.278 *** | −0.506 *** |
| Intervention 2 | 1.174 *** | 0.209 | −0.972 *** | −0.525 | 0.66 | 2.231 *** | −0.086 |
| Time after i = Intervention 2 | 0.263 *** | 0.196 *** | 0.315 *** | 0.342 *** | 0.017 | 0.264 *** | 0.545 *** |
| Temperature | −0.001 | −0.007 | 0.024 | 0.022 | −0.074 *** | 0.015 | 0.019 |
| Humidity | 0.003 | 0.004 | −0.003 | 0.01 ** | 0.021 *** | 0 | 0.005 |
| February | −0.252 * | −0.353 *** | −0.276 * | −0.248 | −0.419 ** | 0.046 | 0.612 *** |
| March | −0.056 | −0.207 | −0.045 | −0.08 | −0.781 *** | 0.487 ** | 1.397 *** |
| April | 0.525 *** | 0.357 ** | 0.581 * | 1.06 *** | −1.014 *** | 0.882 *** | 2.392 *** |
| May | 0.724 *** | 0.637 *** | 1.595 *** | 1.802 *** | −1.495 *** | 0.636 *** | 2.317 *** |
| June | 0.473 * | 0.46 ** | 1.663 *** | 1.565 *** | −2.216 *** | 0.453 * | 1.079 * |
| July | 0.166 | 0.333 | 1.058 ** | 1.01 ** | −2.115 *** | 0.283 | 0.097 |
| August | −0.088 | 0.683 ** | 0.359 | 0.616 | −1.651 ** | −0.103 | −0.826 |
| September | 0.081 | 0.813 *** | 0.313 | 0.623 * | −0.716 | 0.256 | −0.949 * |
| October | 0.253 | 0.738 *** | 0.316 | 0.635 ** | −0.086 | 0.573 *** | −0.704 * |
| November | 0.643 *** | 0.877 *** | 0.61 *** | 0.657 *** | 0.61 ** | 0.827 *** | −0.354 |
| December | 0.632 *** | 0.715 *** | 0.626 *** | 0.4 * | 0.577 *** | 0.51 *** | 0.001 |
| Acute Respiratory Infection | The Effects on Fourth Week of April 2020 (Compared to Third Week of January 2020) | The Effects on First Week of July 2020 (Compared to Third Week of January 2020) | The Effects on First Week of January 2021 (Compared to Third Week of January 2020) |
|---|---|---|---|
| Difference (95% CI) | Difference (95% CI) | Difference (95% CI) | |
| Total acute respiratory infection | −1394.0 (−1493.7–−1294.3) | −1300.1 (−1386.9–−1213.3) | −1298.3 (−1376.4–−1220.4) |
| Adenovirus | −225.9 (−243.8–−208.1) | −223.4 (−241.3–−205.5) | −224.5 (−242.3–−206.7) |
| Human bocavirus | −88.2 (−96.0–−80.3) | −88.3 (−95.8–−80.7) | 32.5 (5.3–59.8) |
| Parainfluenza virus | −175.1 (−194.8–−155.3) | −175.6 (−195.3–−156.0) | −174.3 (−193.6–−155.0) |
| Respiratory syncytial virus | −205.5 (−242.6–−168.4) | −217.9 (−255.3–−180.6) | −232.7 (−275.1–−190.3) |
| Rhinovirus | −449.9 (−482.0–−417.8) | −369.3 (−399.0–−339.5) | −389.2 (−418.7–−359.7) |
| Human metapneumovirus | −125.8 (−147.7–−104.0) | −125.7 (−147.4–−104.1) | −124.6 (−145.8–−103.4) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Noh, J.-W.; Lee, W.-R.; Kim, L.-H.; Cheon, J.; Kwon, Y.D.; Yoo, K.-B. Influence of COVID-19-Related Interventions on the Number of Inpatients with Acute Viral Respiratory Infections: Using Interrupted Time Series Analysis. Int. J. Environ. Res. Public Health 2023, 20, 2808. https://doi.org/10.3390/ijerph20042808
Noh J-W, Lee W-R, Kim L-H, Cheon J, Kwon YD, Yoo K-B. Influence of COVID-19-Related Interventions on the Number of Inpatients with Acute Viral Respiratory Infections: Using Interrupted Time Series Analysis. International Journal of Environmental Research and Public Health. 2023; 20(4):2808. https://doi.org/10.3390/ijerph20042808
Chicago/Turabian StyleNoh, Jin-Won, Woo-Ri Lee, Li-Hyun Kim, Jooyoung Cheon, Young Dae Kwon, and Ki-Bong Yoo. 2023. "Influence of COVID-19-Related Interventions on the Number of Inpatients with Acute Viral Respiratory Infections: Using Interrupted Time Series Analysis" International Journal of Environmental Research and Public Health 20, no. 4: 2808. https://doi.org/10.3390/ijerph20042808
APA StyleNoh, J.-W., Lee, W.-R., Kim, L.-H., Cheon, J., Kwon, Y. D., & Yoo, K.-B. (2023). Influence of COVID-19-Related Interventions on the Number of Inpatients with Acute Viral Respiratory Infections: Using Interrupted Time Series Analysis. International Journal of Environmental Research and Public Health, 20(4), 2808. https://doi.org/10.3390/ijerph20042808







