Age-Friendly Community Interventions for Health and Social Outcomes: A Scoping Review
Abstract
1. Introduction
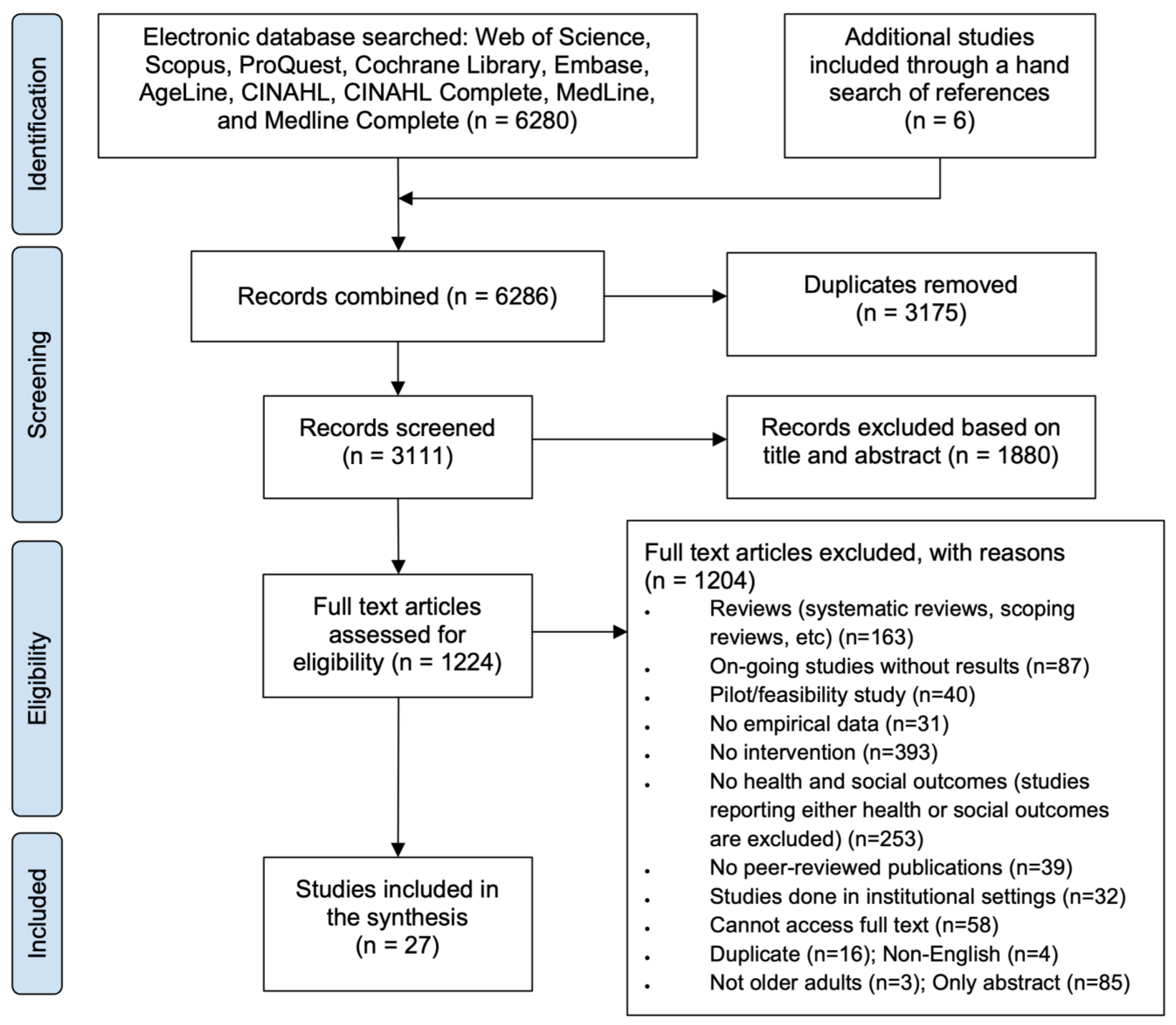
2. Materials and Methods
2.1. Research Design
2.2. Research Question
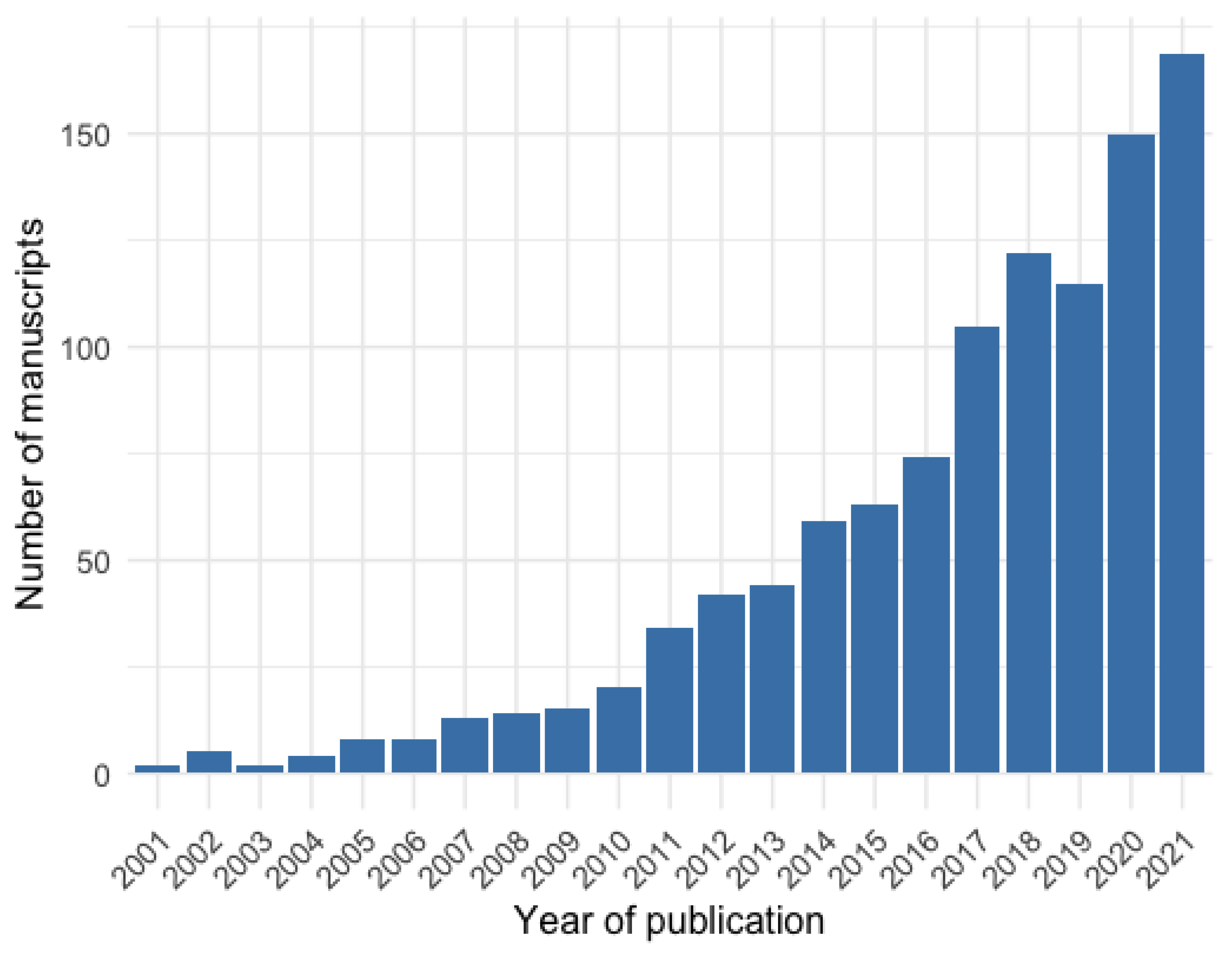
2.3. Search Strategy
2.4. Study Selection
3. Results
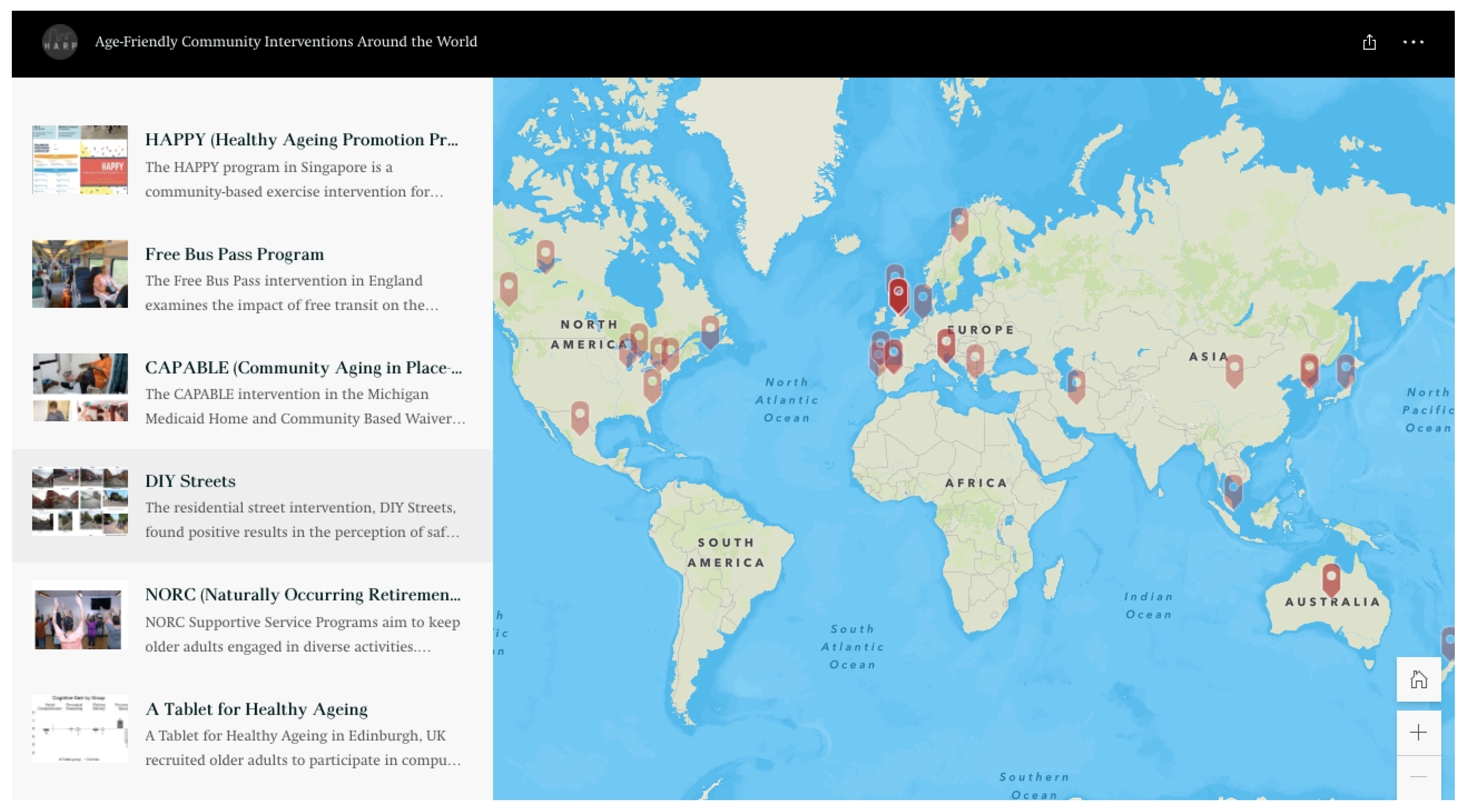
3.1. Summary of Selected Studies
3.2. Physical Activity Interventions
3.3. Educational Interventions
3.4. Multi-Domain Interventions
3.5. Other Interventions
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Database | Search String |
|---|---|
| Web of Science | ((TI = “age friendly” OR TI = “age friendliness” OR TI = “elder friendly” OR TI = “healthy aging” OR TI = “aging-in-place” OR TI = “urban aging” OR TI = “active aging” OR TI = “healthy ageing” OR TI = “ageing-in-place” OR TI = “urban ageing” OR TI = “active ageing”) AND (TI = intervention * OR TI = initiative * OR TI = policies OR TI = policy OR TI = framework *) AND (TI = “older adult” OR TI = senior * OR TI = aged OR TI = elder * OR TI = geriatric *) AND (TI = outcome * OR TI = evaluation * OR TI = impact * OR TI = effect * OR TI = benefit * OR TI = evidence *)) OR ((AB = “age friendly” OR AB = “age friendliness” OR AB = “elder friendly” OR AB = “healthy aging” OR AB = “aging-in-place” OR AB = “urban aging” OR AB = “active aging” OR AB = “healthy ageing” OR AB = “ageing-in-place” OR AB = “urban ageing” OR AB = “active ageing”) AND (AB = intervention * OR AB = initiative * OR AB = policies OR AB = policy OR AB = framework *) AND (AB = “older adult” OR AB = senior * OR AB = aged OR AB = elder * OR AB = geriatric *) AND (AB = outcome * OR AB = evaluation * OR AB = impact * OR AB = effect * OR AB = benefit * OR AB = evidence *)) OR ((AK = “age friendly” OR AK = “age friendliness” OR AK = “elder friendly” OR AK = “healthy aging” OR AK = “aging-in-place” OR AK = “urban aging” OR AK = “active aging” OR AK = “healthy ageing” OR AK = “ageing-in-place” OR AK = “urban ageing” OR AK = “active ageing”) AND (AK = intervention * OR AK = initiative * OR AK = policies OR AK = policy OR AK = framework *) AND (AK = “older adult” OR AK = senior * OR AK = aged OR AK = elder * OR AK = geriatric *) AND (AK = outcome * OR AK = evaluation * OR AK = impact * OR AK = effect * OR AK = benefit * OR AK = evidence *)) |
| PubMed | ((“age friendly”[Title/Abstract] OR “age friendliness”[Title/Abstract] OR “elder friendly”[Title/Abstract] OR “healthy aging”[Title/Abstract] OR “aging-in-place”[Title/Abstract] OR “urban aging”[Title/Abstract] OR “active aging”[Title/Abstract] OR “healthy ageing”[Title/Abstract] OR “ageing-in-place”[Title/Abstract] OR “urban ageing”[Title/Abstract] OR “active ageing”[Title/Abstract]) AND (“intervention *”[Title/Abstract] OR “initiative *”[Title/Abstract] OR “policies”[Title/Abstract] OR “policy”[Title/Abstract] OR “framework *”[Title/Abstract]) AND (“older adult”[Title/Abstract] OR “senior *”[Title/Abstract] OR “aged”[Title/Abstract] OR “elder *”[Title/Abstract] OR “geriatric *”[Title/Abstract]) AND (“outcome *”[Title/Abstract] OR “evaluation *”[Title/Abstract] OR “impact *”[Title/Abstract] OR “effect *”[Title/Abstract] OR “benefit *”[Title/Abstract] OR “evidence *”[Title/Abstract])) |
| Scopus | TITLE-ABS(“age friendly” OR “age friendliness” OR “elder friendly” OR “healthy aging” OR “aging-in-place” OR “urban aging” OR “active aging” OR “healthy ageing” OR “ageing-in-place” OR “urban ageing” OR “active ageing”) AND TITLE-ABS(intervention * OR initiative * OR policies OR policy OR framework *) AND TITLE-ABS(“older adult” OR senior * OR aged OR elder * OR geriatric *) AND TITLE-ABS(outcome * OR evaluation * OR impact * OR effect * OR benefit * OR evidence *) |
| ProQuest | ti(“age friendly” OR “age friendliness” OR “elder friendly” OR “healthy aging” OR “aging-in-place” OR “urban aging” OR “active aging” OR “healthy ageing” OR “ageing-in-place” OR “urban ageing” OR “active ageing”) AND ti(intervention? OR initiative? OR policies OR policy OR framework?) AND ti(“older adult” OR senior? OR aged OR elder?? OR geriatric) AND ti(outcome? OR evaluation? OR impact? OR effect??? OR benefit? OR evidence *) (ab(“age friendly” OR “age friendliness” OR “elder friendly” OR “healthy aging” OR “aging-in-place” OR “urban aging” OR “active aging” OR “healthy ageing” OR “ageing-in-place” OR “urban ageing” OR “active ageing”) AND ab(intervention? OR initiative? OR policies OR policy OR framework?) AND ab(“older adult” OR senior? OR aged OR elder?? OR geriatric) AND ab(outcome? OR evaluation? OR impact? OR effect??? OR benefit? OR evidence *)) |
| Ebscohost AgeLine, CINAHL, CINAHL Complete, Medline, Medline Complete | (“age friendly” OR “age friendliness” OR “elder friendly” OR “healthy aging” OR “aging-in-place” OR “urban aging” OR “active aging” OR “healthy ageing” OR “ageing-in-place” OR “urban ageing” OR “active ageing”) AND (intervention * OR initiative * OR policies OR policy OR framework *) AND (“older adult” OR senior * OR aged OR elder * OR geriatric *) AND (outcome * OR evaluation * OR impact * OR effect * OR benefit * OR evidence *) |
| Embase | (‘age friendly’:ab,ti OR ‘age friendliness’:ab,ti OR ‘elder friendly’:ab,ti OR ‘healthy aging’:ab,ti OR ‘aging-in-place’:ab,ti OR ‘urban aging’:ab,ti OR ‘active aging’:ab,ti OR ‘healthy ageing’:ab,ti OR ‘ageing-in-place’:ab,ti OR ‘urban ageing’:ab,ti OR ‘active ageing’:ab,ti) AND (intervention *:ab,ti OR initiative *:ab,ti OR policies:ab,ti OR policy:ab,ti OR framework *:ab,ti) AND (‘older adult’:ab,ti OR senior *:ab,ti OR aged:ab,ti OR elder *:ab,ti OR geriatric *:ab,ti) AND (outcome *:ab,ti OR evaluation *:ab,ti OR impact *:ab,ti OR effect *:ab,ti OR benefit *:ab,ti OR evidence *:ab,ti) |
| Cochrane Library | (“age friendly” OR “age friendliness” OR “elder friendly” OR “healthy aging” OR “aging-in-place” OR “urban aging” OR “active aging” OR “healthy ageing” OR “ageing-in-place” OR “urban ageing” OR “active ageing”):ab AND (intervention * OR initiative * OR policies OR policy OR framework *):ab AND (“older adult” OR senior * OR aged OR elder * OR geriatric *):ab AND (outcome * OR evaluation * OR impact * OR effect * OR benefit * OR evidence *):ab (“age friendly” OR “age friendliness” OR “elder friendly” OR “healthy aging” OR “aging-in-place” OR “urban aging” OR “active aging” OR “healthy ageing” OR “ageing-in-place” OR “urban ageing” OR “active ageing”):ti AND (intervention * OR initiative * OR policies OR policy OR framework *):ti AND (“older adult” OR senior * OR aged OR elder * OR geriatric *):ti AND (outcome * OR evaluation * OR impact * OR effect * OR benefit * OR evidence *):ti |
| Author (Year) | Intervention | Outcome (1) | Outcome (2) | Outcome (3) | Outcome (4) | Outcome (5) | Outcome (6) |
|---|---|---|---|---|---|---|---|
| Physical Activity Interventions | |||||||
| Ericson et al. (2018) | Resistance training program [P] | Increase in mean sense of coherence (SOC-13): 72.4 (pre), 72.9 (post) | Increase in mean health-related quality of life (SOC-13 (MCS): 52.0 (pre), 54.5 (post); (PCS): 53.9 (pre), 54.1 (post)) | Increase in mean hope (HOPE): 43.9 (pre) 47.1 * (post) | Change in mean affect (PANAS (positive): 18.6 (pre), 18.9 (post); (negative): 10.3 (pre), 7.9 * (post)) | ||
| Liao et al. (2019) | Tai Chi program with background music [P] | Increase in mean physical domain (WHOQOL-BREF): 40.40 (pre), 52.89 ***(post) | Increase in mean psychological domain (WHOQOL-BREF): 44.72 (pre), 54.05 *** (post) | Increase in mean social domain (WHOQOL-BREF): 46.39 (pre), 57.40 *** (post) | Increase in mean environmental domain (WHOQOL-BREF): 45.02 (pre), 52.67 ***(post) | ||
| Martins et al. (2020) | Exercise program [P] | Increase in functional abilities: hand strength *, 4-stage balance test ***, step test *, 30 s sit-to-stand *, timed up-and-go (n.s.) | Increase in self-efficiency for exercise (n.s.) | Improved participation performance (PAPM) *** | |||
| McKay et al. (2018) | Physical activity program [P] | Increase in physical activity at 3 months (+1.6 days/week ***) and 6 months (+1.4 days/week ***) in younger group (60–74 years); increase in physical activity at 3 months (+1 days/week ***) in older group | Decrease in % reporting mobility limitation at 3 months (−15% ***) and 6 months (−12% ***) in younger group (60–74 years); decrease in % reporting mobility limitation at 3 months (−14% *) in older group (>75 years) | Decrease in sitting time at 3 months (−0.5 *) and 6 months (−0.4) in younger group; decrease in sitting time at 3 months (−0.2) and 6 months (−1.1 ***) in older group | Decrease in social exclusion at 3 months (+0.6 ***) and 6 months (+0.4 *) in younger group; no significant result in older group | Decrease in loneliness at 3 months (−0.4 ***) and 6 months (−0.3 ***) in younger group; decrease in loneliness at 3 months (−0.5 ***) and 6 months (−0.4 ***) in older group | Increase in happiness at 3 months (+0.2 ***) and 6 months (+0.1 ***) in younger group; increase in happiness at 3 months (+0.2 ***) and 6 months (+0.2 ***) in older group |
| McNamara et al. (2016) | Healthy aging activity program [P] | Increase in leisure activities (including health-related activities): 72% (pre), 77% (post) | Increase in social engagement: 70% (pre), 72% (post) | ||||
| Merchant et al. (2021) | Peer-led, dual-task exercise program [P] | Reduction in prevalence of depressive symptoms (Euroqol−5D domain): 30% ** | Decrease in prevalence of fragility (FRAIL): 50–75% ** | Decrease in prevalence of 1 or more falls: 66.66% (2/3) ** | Decrease in social isolation (LSNS-6): 10% ** | ||
| Noh et al. (2020) | Exercise program [P] | Increase in mean physical health (skeletal muscle mass: 21.13 (pre), 21.47 *** (post); BMI: 23.32 (pre), 22.90 *** (post); body fat percentage: 32.09 (pre), 31.35 *** (post); waist circumference: 80.27 (pre), 78.63 *** (post); hip circumference: 95.05 (pre), 95.81 * (post); grip strength: 21.69 (pre), 23.35 *** (post); abdominal muscle strength: 14.62 (pre), 21.19 *** (post); flexibility: 14.09 (pre), 18.79 *** (post)) | Decrease in prevalence of mean mental health symptoms (emotion (depression): 48.38 (pre), 43.57 * (post); emotion (anxiety): 51.71 (pre), 48.10 (post); emotion (phobic anxiety): 49.19 (pre), 46.10 * (post); emotion (panic attack): 51.43 (pre), 46.90 (post); emotion (agoraphobia): 47.38 (pre), 46.00 * (post); emotion (obsessive-compulsive): 49.76 (pre), 46.52 (post)) | Decrease in prevalence of mean mental health symptoms (cont.) (emotion (obsession): 52.00 (pre), 48.29 (post); emotion (obsessive-compulsive personality trait): 46.90 (pre), 45.52 (post); emotion (PTSD): 49.05 (pre), 46.14 (post); emotion (aggression): 46.52 (pre), 44.86 (post); emotion (somatization): 51.00 (pre), 46.14 (post)) | Decrease in prevalence of mental health symptoms (cont.) (adaptation to reality (manic episode): 51.71 (pre), 50.14 (post); adaptation to reality (paranoia): 46.38 (pre), 45.86 (post); adaptation to reality (schizophrenia): 48.81 (pre), 47.14 (post)) | Decrease in prevalence of mental health symptoms (cont.) (others (suicide): 45.76 (pre), 44.67 (post); others (addiction): 46.76 (pre), 47.10 (post); others (sleep problem): 53.95 (pre), 50.57 * (post); others (stress vulnerability): 51.71 (pre), 48.10 * (post); others (self-regulation problem): 51.19 (pre), 45.86 * (post)) | Decrease in negative social behaviors (emotion (social desirability): 54.00 (pre), 51.90 (post); emotion (inconsistency): 50.05 (pre), 51.90 (post); others (interpersonal sensitivity): 52.24 (pre), 49.00 (post)) |
| Douka et al. (2019) | Greek traditional dance program [P] | Improvement in attention in both healthy and MCI groups (S4viac ***, S4viti ***) | Improvement in verbal fluency for MCI group (Verflx *, Verfls ***, Verfmo ***) | Improvement in executive functions (FUCAS *) | Improvement in anxiety for healthy * and MCI * groups | Increase in physical condition (arm curl ***, chair stand ***, back scratch+, 2 min step *, timed up-and-go ***, sit and reach ***, balance on one leg ***) | Increase in quality of life (healthy: 62.63 (pre), 64.88+ (post); MCI: 61.25 (pre), 65 * (post)) |
| Educational Interventions | |||||||
| Dumitrache et al. (2017) | Cognitive stimulation, crafts, and exercise workshops [E] | Increase in mean cognitive performance (MEC/MMSE: 27.29 *** (pre), 30.50 *** (post); CDT: 5.62 ***(pre), 7.17 ** (post)) | Increase in mean health (WHOQOL-BREF (general): 3.38 (pre), 3.45 (post); (physical): 25.17 (pre), 25.30 (post); (psychological): 21.49 (pre), 21.91 ***(post)) | Increase in mean quality of life (General QL): 3.28 (pre), 3.31 (post) | Social relationship mean remains constant (WHOQOL-BREF): 10.88 (pre), 10.88 (post) | Improved mean environment (WHOQOL-BREF): 25.10 (pre), 21.61 ***(post) | |
| Fernández-Ballesteros et al. (2012) | University programs [E] | Increase in mean cognitive functioning (digit-symbol): 44.36 (pre), 45.54 *** (post) | Decrease in mean illness reported (objective (illness reported): 0.79 (pre), 0.77 *** (post)) | Increase in mean general health (subjective: 3.05 (pre), 3.06 (post); compared with others: 3.61 (pre), 3.64 (post)) | Change in mean affect (positive affect, increase: 3.01 (pre), 3.15 *** (post); negative affect, decrease: 1.71 (pre), 1.65 ** (post); balance, increase: 1.84 (pre), 2.07 (post)) | Increase in mean social relationships (social networks): 7.84 (pre), 7.85 (post) | Change in mean activity (information-seeking, increase: 3.34 (pre), 3.35 *** (post); social, increase: 2.29 (pre), 2.39 *** (post); productivity, decrease: 2.28 (pre), 2.24 *** (post)) |
| Gough et al. (2017) | Peer-led education series [E] | Increase in awareness of brain health and resilience (FoH information): 50.0% (pre), 96.3% *** (post) | Increase in FoH information application 38.3% (pre), 92.6% (post) | Increase in awareness of interventions to promote cognitive and mental health: 32.1% (pre), 100% *** (post) | Increase in ability to name four or more evidence-based brain health and resilience interventions: 23.1% (pre), 90.0% *** (post) | Increased confidence in goal setting to promote personal health and well-being: 82.0% (pre), 92.3% * (post) | Improved attitude towards aging (average self-perception score): 3.08/5 (pre), 4.08/5 * (post) |
| Mendoza-Nunez et al. (2018) | Healthy aging education program [E] | Increase in health behavior (health care: 7.7 (pre), 8.2 * (post); self-esteem: 8.3 (pre), 8.4 (post); healthy food: 7.9 (pre), 8.1 (post); physical exercise: 8.0 (pre), 8.5 (post)) | Increase in healthy lifestyle (sleep hygiene: 7.4 (pre), 8.2 * (post); body hygiene: 8.4 (pre), 8.9 (post); healthy environment: 8.4 (pre), 8.5 (post)) | Increase in self-perception of aging (where having a positive self-perception (score ≤ 44) and negative self-perception (score ≥ 59): 51 (pre), 40 *** (post) | |||
| Oetzel et al. (2020) | Peer education program [E] | Increase in self-rated health: +4.47 (average treatment effect on the treated, ATT) | Increase in health-related quality of life: +2.66 (ATT) | Increase in perceived support: 0.35 * (ATT) | Increase in desired support: 0.03 (ATT) | Increase in tribal identity: 0.36 * (ATT) | Decrease in loneliness: 0.05 (ATT) |
| Rabiei et al. (2013) | Family-based empowerment program [E] | Decrease in mean perceived threat (SF-36 (public health): 20.81 (pre), 14.33 ***(post); (physical problems): 21.25 (pre), 10.71 ***(post); (mental health): 35.55 (pre), 19.70 ***(post); (pain): 24.82 (pre), 13.57 ***(post); (general health): 21.04 (pre), 12.06 (post)) | Decrease in mean perceived threat (SF-36 (playing role): 23.98 (pre), 14.95 ***(post); (social performance): 25.27 (pre), 15.50 ***(post); (power and energy): 18.91 (pre), 11.15 ***(post); (life quality): 17.30 (pre), 10.92 ***(post)) | ||||
| Shinkai et al. (2016) | Health education program [E] | Increase in life-space mobility (men: 80.8% (pre), 86.9% (post); women: 63.7% (pre), 74.3% (post)) | Increase in instrumental ADL (men: 72.9% (pre), 80.8% (post); women: 66.5% (pre), 76.3% (post)) | Increase in mean intellectual activity (men: 64.2% (pre), 64.7% (post); women: 49.0% (pre), 57.2% (post)) | Increase in social role (men: 55.0% (pre), 58.8% (post); women: 51.5% (pre), 58.3% (post)) | ||
| Tagliabue et al. (2018) | Multi-domain cognitive training [E] | Increase in global cognitive functioning (MoCA) | Non-significant changes in verbal and visuo-spatial memory (forward digit span *, backward digit span, forward Corsi span, backward Corsi span, short story test, recall of ROCF) | Non-significant changes in visuo-constructional abilities (copy of ROCF) | Increase in executive functions on most tests (semantic verbal fluency *, phonological verbal fluency, Stroop test (time) **, Stroop test (errors) *) | Increase in measures of attention (TMT); increase in non-verbal reasoning (Raven’s Matrices) + | Positive influence on mood: 57.53%; positive influence on socialization: 41.89% |
| Multi-domain Interventions | |||||||
| Castle et al. (2008) | Senior living enhancement program (SLEP) [M] | Decrease in reported participation in regular activity (item 1a): 55% (pre), 68% * (post); increase in physical activity 1 or more times weekly (item 1b): 45% (pre), 55% * (post) | Increase in lack of knowledge pertaining to participants’ blood glucose level, LDL cholesterol level, and systolic blood pressure level (item 2a, 7, and 10a): 33% (pre), 52% *(post), 33% (pre), 53% (post), and 85% (pre), 86% * (post); increase in reported glucose level as ideal (<110) or moderate high (11–129), and systolic blood pressure as ideal (under 140) (item 2b and 10b): 14% (pre), 36% * (post), 51% (pre), 52% * (post) | Increase in engagement with preventative care (item 5a (sigmoidoscopy or colonoscopy in past 5 years): 42% (pre), 52% * (post); item 5b (skin examination in past year): 9% (pre), 25% (post); item 5c (fecal occult blood in past year): 30% (pre), 43% * (post); item 5d (PSA test in past year): 42% (pre), 58% * (post); item 5e (mammogram in past 1–2 years): 52% (pre), 66% (post); item 5f (PAP test in past 1–2 years): 38% (pre), 49% (post); item 6a (flu shot in past year): 55% (pre), 75% * (post); item 6b (pneumonia shot in past 10 years): 63% (pre), 74% * (post)) | Improved smoking habits (item 3): 82% (pre), 84% * (post) | Decrease in the experience of muscle weakness or reduced muscle strength (item 9): 71% (pre), 61% * (post) | Increase in social activities outside the home (item 4a): 34% (pre), 60% (post); increase in strong social ties with friends/family: 70% (pre), 77% (post) |
| Park et al. (2011) | Health education and exercise program [M] | Decrease in mean blood pressure (systolic): 134.6 (pre), 122.3 **(post); (diastolic): 77.9 (pre), 77.0 (post) | Increase in mean physical activity (MET-min/week (vigorous intensity): 1180.0 (pre), 2248.9 (post); (moderate intensity): 475.5 (pre), 1275.3 (post); (walking): 1534.3 (pre), 1915.5 (post); (total physical activity): 2825.9 (pre), 4938.1 *(post)) | Change in health-related quality of life (SF-36 (physical functioning): 80.3 (pre), 85.0 (post); (role-physical): 75.3 (pre), 79.5 (post); (bodily pain): 69.4 (pre), 66.1 (post); (general health): 51.7 (pre), 68.9 ** (post); (vitality): 57.9 (pre), 72.6 *(post); (mental health): 70.3 (pre), 81.7 * (post)) | Increase in mean self-care behavior: 60.6 (pre), 67.6 * (post) | Increase in self-efficacy for exercise: 625.6 (pre), 643.3 (post) | Increase in mean health-related quality of life (SF-36 (social functioning): 65.0 (pre), 73.3 * (post); (role-emotional): 84.3 (pre), 87.9 (post)) |
| Rainero et al. (2021) | Multi-center health promotion program [M] | Decrease in depressed mood * | Increase in positive nutritional habits ** | No significant changes in physical and cognitive function, nor sleep. | No change in quality of life or social function | ||
| Author (Year) | Intervention | Health Outcomes | Social Outcomes |
|---|---|---|---|
| Physical Activity Interventions | |||
| Haynes et al. (2021) | Physical activity and fall-prevention program [P] | The CHaNGE trial found an increase in reported physical activity, an increase in motivation and goal-setting behaviors, and an improvement for some participants in fitness and strength. Additionally, weight loss and increased fall prevention awareness or skills were also considered benefits of the program. The participants’ participation in the trial was measured using Fitbit technology, and many participants agreed that the accountability factor, in relation to tracking technology, increased their engagement in the intervention. | The trial found no change in social participation due to the intervention; however, “...one third of those who expressed a preference said they would like more interaction with their community group” (p. 299). Because the trial did not implement a social piece into their intervention, the participants relied on established connections as encouragement to engage in physical activity. The respondents who did engage in these established connections throughout the intervention reported a higher sense of security, companionship, mutual support, encouragement, and community. |
| VanRavenstein et al. (2018) | Physical activity program [P] | The participants within this program had differing responses dependent upon where they lived, as the intervention was provided in two separate senior living apartment complexes. The group which engaged in social behaviors throughout the intervention reported higher rates of engagement with the exercise and continuation of exercise post-program than the group that did not have regular socialization habits. The group which reported little socialization had a significant number of participants struggling with depression. This appeared to not be improved with the intervention. | A key aspect in this intervention was the participants’ relationship with socialization and their willingness to engage with other residents in the study. The group which actively participated in socialization practices had a different outlook on exercise and saw it as a fun activity and a way to encourage community. |
| Educational Interventions | |||
| Morse et al. (2018) | Comedy improvisation course [E] | In the “Humor Doesn’t Retire” Program, respondents reported mood change, and more specifically a decrease in depressive symptoms. Other outcomes included in the study findings were “...enhanced mental flexibility and cognitive acuity following the program, accompanied by a willingness to accept the unexpected and react spontaneously” (p. 4). | The participants in this program cited many reasons as to why they engaged in this social intervention, with some attending to improve their social or communication skills as a way of self-development, while others attended due to their interest in the activities or desire to have fun. The study found that increased social participation/connection and decreased isolation were common themes amongst the respondent interviews. |
| Sims-Gould et al. (2020) | Health promotion program [E] | This study followed multiple Active Aging Grant (AAG) funded organizations and their implementation of health promotion programs within community settings. Participants from multiple organizations reported physical activity in the programs as “…beneficial, enjoyable, and at times, life altering” (p. 6). Despite each site having different physical activity programs, the older adults’ engagement and enjoyment of the program appeared to provide positive results. | Social activity and connectedness varied between the sites but were still reported to be positive by respondents. The social outcomes of this study included increased social connectedness for both the participants and the facilitators, as well as a decrease in social isolation and loneliness. |
| Multi-domain Interventions | |||
| Greenfield et al. (2015) | Naturally occurring retirement community (NORC) support programs [M] | Through this study, the participants were able to access both preventative and supportive services to improve their overall health and well-being. Many participants in the study found these services to be vital in their ability to age-in-place in a healthy manner. | The NORC study revealed that older adults’ involvement in NORC programs is not just determined by their utilization level, but rather by their relationship with the NORC program as a whole. Some of the characteristics of high involvement included a close relationship with staff, lifelong histories, and a desire to ‘give back’ to the program. |
| Orellana et al. (2020) | Day centers for older adults [M] | Day centers for older adults were found to provide services which allowed participants to continue to age-in-place without requiring the individual to engage in a traditional residential care model. Due to the wide range of services and activities offered, many participants in this study reported an increase in mental well-being/health, physical well-being/health, as well as increased hygiene. | This study followed participants who were already established in day centers; therefore, social connectedness was based on the individual’s social engagement both in and out of the program. Social participation/involvement, feelings of dignity/control, quality of life, and feelings of security were all found to be common themes amongst those who attend day centers. |
References
- United Nations. World Population Ageing 2020 Highlights; United Nations: Geneva, Switzerland, 2020.
- Prince, M.J.; Wu, F.; Guo, Y.; Gutierrez Robledo, L.M.; O’Donnell, M.; Sullivan, R.; Yusuf, S. The Burden of Disease in Older People and Implications for Health Policy and Practice. Lancet 2015, 385, 549–562. [Google Scholar] [CrossRef] [PubMed]
- Harper, S. Economic and Social Implications of Aging Societies. Science 2014, 346, 587–591. [Google Scholar] [CrossRef]
- Jain, R.; Dupas, P. The Effects of India’s COVID-19 Lockdown on Critical Non-COVID Health Care and Outcomes: Evidence from Dialysis Patients. Soc. Sci. Med. 2022, 296, 114762. [Google Scholar] [CrossRef] [PubMed]
- Steinman, M.A.; Perry, L.; Perissinotto, C.M. Meeting the Care Needs of Older Adults Isolated at Home During the COVID-19 Pandemic. JAMA Intern. Med. 2020, 180, 819. [Google Scholar] [CrossRef] [PubMed]
- Stenholm, S.; Westerlund, H.; Salo, P.; Hyde, M.; Pentti, J.; Head, J.; Kivimäki, M.; Vahtera, J. Age-Related Trajectories of Physical Functioning in Work and Retirement: The Role of Sociodemographic Factors, Lifestyle and Disease. J. Epidemiol. Community Health 2014, 68, 503–509. [Google Scholar] [CrossRef]
- Rantakokko, M.; Mänty, M.; Rantanen, T. Mobility Decline in Old Age. Exerc. Sport Sci. Rev. 2013, 41, 19–25. [Google Scholar] [CrossRef]
- Metz, D.H. Mobility of Older People and Their Quality of Life. Transp. Policy 2000, 7, 149–152. [Google Scholar] [CrossRef]
- Musich, S.; Wang, S.S.; Ruiz, J.; Hawkins, K.; Wicker, E. The Impact of Mobility Limitations on Health Outcomes among Older Adults. Geriatr. Nurs. 2018, 39, 162–169. [Google Scholar] [CrossRef]
- Greenfield, E.A. Using Ecological Frameworks to Advance a Field of Research, Practice, and Policy on Aging-in-Place Initiatives. Gerontologist 2012, 52, 1–12. [Google Scholar] [CrossRef]
- World Health Organization. Global Age-Friendly Cities: A Guide; WHO: Geneva, Switzerland, 2007.
- Courtin, E.; Knapp, M. Social Isolation, Loneliness and Health in Old Age: A Scoping Review. Health Soc. Care Community 2017, 25, 799–812. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping Studies: Towards a Methodological Framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- MacQueen, K.M.; McLellan, E.; Metzger, D.S.; Kegeles, S.; Strauss, R.P.; Scotti, R.; Blanchard, L.; Trotter, R.T. What Is Community? An Evidence-Based Definition for Participatory Public Health. Am. J. Public Health 2001, 91, 1929–1938. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization Official Records of the World Health Organization No 2. Summary Report on Proceedings Minutes and Final Acts of the International Health Conference Held in New York from 19 June to 22 July 1946; WHO: Geneva, Switzerland, 1948.
- Dijkers, M.P.J.M.; Whiteneck, G.; El-Jaroudi, R. Measures of Social Outcomes in Disability Research. Arch. Phys. Med. Rehabil. 2000, 81, S63–S80. [Google Scholar] [CrossRef] [PubMed]
- Santini, Z.I.; Jose, P.E.; York Cornwell, E.; Koyanagi, A.; Nielsen, L.; Hinrichsen, C.; Meilstrup, C.; Madsen, K.R.; Koushede, V. Social Disconnectedness, Perceived Isolation, and Symptoms of Depression and Anxiety among Older Americans (NSHAP): A Longitudinal Mediation Analysis. Lancet Public Health 2020, 5, e62–e70. [Google Scholar] [CrossRef] [PubMed]
- Ericson, H.; Skoog, T.; Johansson, M.; Wåhlin-Larsson, B. Resistance Training Is Linked to Heightened Positive Motivational State and Lower Negative Affect among Healthy Women Aged 65–70. J. Women Aging 2018, 30, 366–381. [Google Scholar] [CrossRef] [PubMed]
- Haynes, A.; Sherrington, C.; Wallbank, G.; Lester, D.; Tong, A.; Merom, D.; Rissel, C.; Tiedemann, A. “Someone’s Got My Back”: Older People’s Experience of the Coaching for Healthy Ageing Program for Promoting Physical Activity and Preventing Falls. J. Aging Phys. Act. 2021, 29, 296–307. [Google Scholar] [CrossRef]
- Liao, S.J.; Chong, M.C.; Tan, M.P.; Chua, Y.P. Tai Chi with Music Improves Quality of Life among Community-Dwelling Older Persons with Mild to Moderate Depressive Symptoms: A Cluster Randomized Controlled Trial. Geriatr. Nurs. 2019, 40, 154–159. [Google Scholar] [CrossRef]
- Martins, A.C.; Guia, D.; Saraiva, M.; Pereira, T. Effects of A “Modified” Otago Exercise Program on the Functional Abilities and Social Participation of Older Adults Living in the Community-The AGA@4life Model. Int. J. Environ. Res. Public Health 2020, 17, 1258. [Google Scholar] [CrossRef]
- McKay, H.; Nettlefold, L.; Bauman, A.; Hoy, C.; Gray, S.M.; Lau, E.; Sims-Gould, J. Implementation of a Co-Designed Physical Activity Program for Older Adults: Positive Impact When Delivered at Scale 11 Medical and Health Sciences 1117 Public Health and Health Services. BMC Public Health 2018, 18, 1289. [Google Scholar] [CrossRef]
- McNamara, B.; Rosenwax, L.; Lee, E.A.; Same, A. Evaluation of a Healthy Ageing Intervention for Frail Older People Living in the Community. Australas. J. Ageing 2016, 35, 30–35. [Google Scholar] [CrossRef]
- Merchant, R.A.; Tsoi, C.T.; Tan, W.M.; Lau, W.; Sandrasageran, S.; Arai, H. Community-Based Peer-Led Intervention for Healthy Ageing and Evaluation of the “HAPPY” Program. J. Nutr. Health Aging 2021, 25, 520–527. [Google Scholar] [CrossRef] [PubMed]
- Noh, E.; Kim, J.; Kim, M.; Yi, E. Effectiveness of SaBang-DolGi Walking Exercise Program on Physical and Mental Health of Menopausal Women. Int. J. Environ. Res. Public Health 2020, 17, 6935. [Google Scholar] [CrossRef] [PubMed]
- VanRavenstein, K.; Davis, B.H. When More Than Exercise Is Needed to Increase Chances of Aging in Place: Qualitative Analysis of a Telehealth Physical Activity Program to Improve Mobility in Low-Income Older Adults. JMIR Aging 2018, 1, e11955. [Google Scholar] [CrossRef] [PubMed]
- Douka, S.; Zilidou, V.I.; Lilou, O.; Tsolaki, M. Greek Traditional Dances: A Way to Support Intellectual, Psychological, and Motor Functions in Senior Citizens at Risk of Neurodegeneration. Front. Aging Neurosci. 2019, 11, 6. [Google Scholar] [CrossRef] [PubMed]
- Dumitrache, C.G.; Rubio, L.; Bedoya, I.; Rubio-Herrera, R. Promoting Active Aging in Rural Settings: An Intervention Program Implemented in Orense, Spain. Univ. Psychol. 2017, 16, 1–12. [Google Scholar] [CrossRef]
- Fernández-Ballesteros, R.; Caprara, M.; Schettini, R.; Bustillos, A.; Mendoza-Nunez, V.; Orosa, T.; Kornfeld, R.; Rojas, M.; López, M.D.; Santacreu, L.M.; et al. Effects of University Programs for Older Adults: Changes in Cultural and Group Stereotype, Self-Perception of Aging, and Emotional Balance. Educ. Gerontol. 2013, 39, 119–131. [Google Scholar] [CrossRef]
- Gough, A.; Cassidy, K.-L. Toward Psychosocial Health in Age-Friendly Communities: The Fountain of Health Peer-Led Education Series. Ment. Health Prev. 2017, 8, 14–19. [Google Scholar] [CrossRef]
- Mendoza-Nunez, V.M.; Sarmiento-Salmoran, E.; Marin-Cortes, R.; Martinez-Maldonado, M.D.; Ruiz-Ramos, M. Influence of the Self-Perception of Old Age on the Effect of a Healthy Aging Program. J. Clin. Med. 2018, 7, 106. [Google Scholar] [CrossRef]
- Morse, L.A.; Xiong, L.; Ramirez-Zohfeld, V.; Anne, S.; Barish, B.; Lindquist, L.A. Humor Doesn’t Retire: Improvisation as a Health-Promoting Intervention for Older Adults. Arch. Gerontol. Geriatr. 2018, 75, 1–5. [Google Scholar] [CrossRef]
- Oetzel, J.G.; Cameron, M.P.; Simpson, M.L.; Reddy, R.; Nock, S.; Greensill, H.; Meha, P.; Johnston, K.; Harding, T.; Shelford, P.; et al. Kaumātua Mana Motuhake: Peer Education Intervention to Help Māori Elders during Later-Stage Life Transitions. BMC Geriatr. 2020, 20, 186. [Google Scholar] [CrossRef]
- Rabiei, L.; Mostafavi, F.; Masoudi, R.; Hassanzadeh, A. The Effect of Family-Based Intervention on Empowerment of the Elders. J. Educ. Health Promot. 2013, 2, 24. [Google Scholar] [CrossRef] [PubMed]
- Shinkai, S.; Yoshida, H.; Taniguchi, Y.; Murayama, H.; Nishi, M.; Amano, H.; Nofuji, Y.; Seino, S.; Fujiwara, Y. Public Health Approach to Preventing Frailty in the Community and Its Effect on Healthy Aging in Japan. Geriatr. Gerontol. Int. 2016, 16, 87–97. [Google Scholar] [CrossRef] [PubMed]
- Sims-Gould, J.; Franke, T.; Lusina-Furst, S.; McKay, H.A. Community Health Promotion Programs for Older Adults: What Helps and Hinders Implementation. Health Sci. Rep. 2020, 3, e144. [Google Scholar] [CrossRef] [PubMed]
- Tagliabue, C.F.; Guzzetti, S.; Gualco, G.; Boccolieri, G.; Boccolieri, A.; Smith, S.; Daini, R. A Group Study on the Effects of a Short Multi-Domain Cognitive Training in Healthy Elderly Italian People. BMC Geriatr. 2018, 18, 321. [Google Scholar] [CrossRef]
- Castle, N. Service Enriched Housing and the Senior Living Enhancement Program. J. Hous. Elder. 2008, 22, 263–278. [Google Scholar] [CrossRef]
- Greenfield, E.A.; Fedor, J.P. Characterizing Older Adults’ Involvement in Naturally Occurring Retirement Community (NORC) Supportive Service Programs. J. Gerontol. Soc. Work 2015, 58, 449–468. [Google Scholar] [CrossRef]
- Orellana, K.; Manthorpe, J.; Tinker, A. Day Centres for Older People—Attender Characteristics, Access Routes and Outcomes of Regular Attendance: Findings of Exploratory Mixed Methods Case Study Research. BMC Geriatr. 2020, 20, 158. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.H.; Song, M.; Cho, B.L.; Lim, J.Y.; Song, W.; Kim, S.H. The Effects of an Integrated Health Education and Exercise Program in Community-Dwelling Older Adults with Hypertension: A Randomized Controlled Trial. Patient Educ. Couns. 2011, 82, 133–137. [Google Scholar] [CrossRef]
- Rainero, I.; Summers, M.J.; Monter, M.; Bazzani, M.; Giannouli, E.; Aumayr, G.; Burin, D.; Provero, P.; Vercelli, A.E. The My Active and Healthy Aging ICT Platform Prevents Quality of Life Decline in Older Adults: A Randomised Controlled Study. Age Ageing 2021, 50, 1261–1267. [Google Scholar] [CrossRef]
- Ballesteros, S.; Peter, C.; Waterworth, E.L.; Waterworth, J.A. The Role of ICT and Networking in Healthy Ageing. In PETRA 2012, Proceedings of the 5th International Conference on PErvasive Technologies Related to Assistive Environments, Heraklion, Greece, 6–8 June 2012; UNED: Madrid, Spain, 2012. [Google Scholar]
- Reinhard, E.; Courtin, E.; van Lenthe, F.J.; Avendano, M. Public Transport Policy, Social Engagement and Mental Health in Older Age: A Quasi-Experimental Evaluation of Free Bus Passes in England. J. Epidemiol. Community Health 2018, 72, 361–368. [Google Scholar] [CrossRef]
- Sánchez-González, D.; Rojo-Pérez, F.; Rodríguez-Rodríguez, V.; Fernández-Mayoralas, G.; Sanchez-Gonzalez, D.; Rojo-Perez, F.; Rodriguez-Rodriguez, V.; Fernandez-Mayoralas, G.; Sánchez-González, D.; Rojo-Pérez, F.; et al. Environmental and Psychosocial Interventions in Age-Friendly Communities and Active Ageing: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 8305. [Google Scholar] [CrossRef] [PubMed]
- Owusu-Addo, E.; Ofori-Asenso, R.; Batchelor, F.; Mahtani, K.; Brijnath, B. Effective Implementation Approaches for Healthy Ageing Interventions for Older People: A Rapid Review. Arch. Gerontol. Geriatr. 2021, 92, 104263. [Google Scholar] [CrossRef] [PubMed]
- Breysse, J.; Dixon, S.; Wilson, J.; Szanton, S. Aging Gracefully in Place: An Evaluation of the Capability of the CAPABLE© Approach. J. Appl. Gerontol. 2021, 41, 718–728. [Google Scholar] [CrossRef]
- Szanton, S.L.; Leff, B.; Li, Q.; Breysse, J.; Spoelstra, S.; Kell, J.; Purvis, J.; Xue, Q.; Wilson, J.; Gitlin, L.N. CAPABLE Program Improves Disability in Multiple Randomized Trials. J. Am. Geriatr. Soc. 2021, 69, 3631–3640. [Google Scholar] [CrossRef]
- Andrews, G.J.; Gavin, N.; Begley, S.; Brodie, D. Assisting Friendships, Combating Loneliness: Users’ Views on a ‘Befriending’ Scheme. Ageing Soc. 2003, 23, 349–362. [Google Scholar] [CrossRef]
- Luck, R. Dialogue in Participatory Design. Des. Stud. 2003, 24, 523–535. [Google Scholar] [CrossRef]
- Haggis, C.; Sims-Gould, J.; Winters, M.; Gutteridge, K.; McKay, H.A. Sustained Impact of Community-Based Physical Activity Interventions: Key Elements for Success. BMC Public Health 2013, 13, 892. [Google Scholar] [CrossRef] [PubMed]
- James, H.; Buffel, T. Co-Research with Older People: A Systematic Literature Review. Ageing Soc. 2022, 1–27. [Google Scholar] [CrossRef]
- Kwan, B.M.; McGinnes, H.L.; Ory, M.G.; Estabrooks, P.A.; Waxmonsky, J.A.; Glasgow, R.E. RE-AIM in the Real World: Use of the RE-AIM Framework for Program Planning and Evaluation in Clinical and Community Settings. Front. Public Health 2019, 7, 345. [Google Scholar] [CrossRef] [PubMed]
- Chase, J.-A.D. Interventions to Increase Physical Activity Among Older Adults: A Meta-Analysis. Gerontologist 2015, 55, 706–718. [Google Scholar] [CrossRef] [PubMed]
- Menec, V.H.; Means, R.; Keating, N.; Parkhurst, G.; Eales, J. Conceptualizing Age-Friendly Communities. Can. J. Aging 2011, 30, 479–493. [Google Scholar] [CrossRef] [PubMed]
- Menec, V.H. Conceptualizing Social Connectivity in the Context of Age-Friendly Communities. J. Hous. Elder. 2017, 31, 99–116. [Google Scholar] [CrossRef]
- Fakoya, O.A.; McCorry, N.K.; Donnelly, M. Loneliness and Social Isolation Interventions for Older Adults: A Scoping Review of Reviews. BMC Public Health 2020, 20, 129. [Google Scholar] [CrossRef] [PubMed]
- Breheny, M.; Stephens, C. ‘I Sort of Pay Back in My Own Little Way’: Managing Independence and Social Connectedness through Reciprocity. Ageing Soc. 2009, 29, 1295–1313. [Google Scholar] [CrossRef]
- Beck, K.L.; Weeks, L.E.; Montelpare, W.J.; MacDonald, D.J. Identifying Important Factors for Older Adults’ Physical Activity Participation across Individual/Group, Structured/Unstructured Contexts. Eur. J. Ageing 2016, 13, 209–218. [Google Scholar] [CrossRef] [PubMed]
- Dacey, M.; Baltzell, A.; Zaichkowsky, L. Older Adults’ Intrinsic and Extrinsic Motivation toward Physical Activity. Am. J. Health Behav. 2008, 32, 570–582. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Decade of Healthy Ageing: Baseline Report; WHO: Geneva, Switzerland, 2020. [Google Scholar]
| Group 1 | Group 2 | Group 3 | Group 4 |
|---|---|---|---|
| age-friendly age-friendliness elder friendly healthy aging aging-in-place urban aging active aging healthy ageing ageing-in-place urban ageing active ageing | intervention * initiative * policies policy framework * | older adult senior * aged elder * geriatric * | outcome * evaluation * impact * effect * benefit * evidence * |
| Inclusion Criteria | Exclusion Criteria | |
|---|---|---|
| Study focus | Studies that examine interventions, policies, and initiatives | Studies that do not examine interventions |
| Study context | Studies conducted in community settings | Studies conducted in institutional settings |
| Outcomes of interest | Both health and social outcomes | Studies that do not include any health or social outcomes; also studies that report either health or social outcomes only |
| Types of study | Peer-reviewed journal publications; empirical studies that employed quantitative/qualitative data | Systematic reviews, scoping reviews, books, book chapters, book reviews, commentaries, opinions, abstracts, conference proceedings, dissertation/theses, study protocols, pilot/feasibility studies |
| Geographic scope | All countries | |
| Temporal scope | Publications from January 2001 to October 2021 | Publications prior to January 2001 |
| Study population | People aged 60 and above |
| Authors (Year) | Country | Population (N) | Study Design | Intervention | Health Outcomes | Social Outcomes | Main Findings |
|---|---|---|---|---|---|---|---|
| Physical Activity Interventions | |||||||
| Ericson et al. (2018) [18] | Sweden | People aged 65+ (N = 32) w: 32, m: 0 | Randomized control trial | Resistance training program [P] | Coherence, health-related quality of life | Hope, negative affect | Resistance training amongst female older adults improved hope and contributed to a decrease in negative affects. This intervention appeared to be positively linked with psychological benefits. |
| Haynes et al. (2021) [19] | Australia | People aged 60+ (N = 32) w: 22, m: 10 | Qualitative | Physical activity and fall-prevention program [P] | Physical activity, motivation, goal-setting, fitness, strength, weight loss, fall prevention | Sense of security, companionship, mutual support, encouragement, community | The healthy aging program reported increased physical activity levels and positivity related to physical activity. Social connections encouraged motivation but were not a primary outcome. |
| Liao et al. (2019) [20] | China | People aged 60+ (N = 112) w: 69, m: 43 | Randomized control trial | Tai Chi program with background music [P] | Physical/psychological domains | Social/environmental domains | Tai Chi with music appeared to improve the quality of life for older adults. Physical, social, psychological, and environmental factors also experienced an increased improvement after the intervention. |
| Martins et al. (2020) [21] | Portugal | People aged 65+ (N = 34) w: 26, m: 8 | Non-randomized cluster trial | Exercise program [P] | Functional abilities | Participation, self-efficacy | The strength and balance exercise program improved physical/functional abilities and self-efficacy for exercise. The intervention also serves to improve social participation and reduce the risk of falls. |
| McKay et al. (2018) [22] | Canada | People aged 60+ (N = 534) w: 411, m: 123 | Type 2 hybrid effectiveness implementation | Physical activity program [P] | Physical activity, mobility limitations, sitting time | Social exclusion, loneliness, happiness | The physical activity program contributed to increased mobility, strength, and physical activity. An additional effect of this intervention was a decrease in social exclusion. |
| McNamara et al. (2016) [23] | Australia | People aged 55+ (N = 32) w: 24, m: 8 | Mixed-methods study | Healthy aging activity program [P] | Leisure activities | Social engagement | The healthy aging activity program reported increased social functioning, mental well-being, household/leisure activities, and overall enjoyment and confidence when participating in the intervention. |
| Merchant et al. (2021) [24] | Singapore | People aged 60+ (N = 569) n/a | Non-randomized cluster trial | Peer-led, dual-task exercise program [P] | Depressive symptoms, frailty, falls | Isolation | The Healthy Aging Promotion Program, a peer and professionally led intervention, promoted increased cognition, physical functioning, balance, perception of health, and a decrease in falls and social isolation. |
| Noh et al. (2020) [25] | South Korea | People aged 50+ (N = 40) only women | Randomized control trial | Healthy aging program workshop [P] | Physical/mental health | Social behaviors | The SaBang-DolGi walking exercise program improved mental/physical well-being and vitality amongst menopausal women. |
| VanRavenstein et al. (2018) [26] | United States | People aged 55+ (N = 21) w: 19, m: 2 | Qualitative | Physical activity program [P] | Depressive symptoms, exercise | Social participation, community | The telehealth exercise program delivered to two separate community groups produced differing results. One group improved in social connectedness and physical activity, and the other described isolation and depression to be distressing. |
| Douka et al. (2019) [27] | Greece | People aged 60+ (N = 60) w: 45, m: 15 | Program evaluation (pre/post) | Greek traditional dance program [E] | Attention, verbal frequency, executive function, anxiety, physical condition | Quality of life | The Greek traditional dance program improved the cognitive and physical condition as well as the quality of life for both healthy older adults and older adults with mild cognitive impairment. |
| Educational Interventions | |||||||
| Dumitrache et al. (2017) [28] | Spain | People aged 65+ (N = 86) w: 61, m: 25 | Cross-sectional | Cognitive stimulation, crafts, and exercise workshops [E] | Cognition, overall health | Quality of life, social connectedness, environment | The health promotion program, which was comprised of exercise workshops, crafts, and cognitive stimulation, improved cognition, and the perception of psychological health and leisure activity opportunities. |
| Fernández-Ballesteros et al. (2013) [29] | Spain | People aged 55+ (N = 95) w: 42, m: 53 | Evaluation study | University program [E] | Self-perception of aging, wellbeing | Social relationships, activity, negative and positive affects | The university program intervention reported maintaining activity, overall health, cognitive functioning, and an increase in positive affects amongst older adults. |
| Gough et al. (2017) [30] | Canada | People aged 50+ (N = 51) w: 39, m: 12 | Observational study | Peer-led education series [E] | Brain health, information application, awareness of interventions, health-related goal setting | Self-perception | The peer-led health education program led to an increase in engagement with lifestyle and health interventions amongst older adults. Additionally, this intervention improved attitudes towards aging and goal-setting behaviors. |
| Mendoza-Nunez et al. (2018) [31] | Mexico | People aged 60+ (N = 64) w: 52, m: 12 | Pre/post | Healthy aging program workshop [E] | Healthy lifestyle | Self-perception | The healthy aging programming added to improved physiological health in older adults, and self-perception remained constant. |
| Morse et al. (2018) [32] | United States | People aged 55+ (N = 10) w: 9, m: 1 | Qualitative | Comedy improvisation course [E] | Depressive symptoms, mental flexibility, cognitive acuity | Self-development, social skills, communication skills, connection, loneliness | The benefits of the improvisation course included an increased sense of comfort, positivity, self-development/awareness, feelings of acceptance, and improved problem-solving capabilities. |
| Oetzel et al. (2020) [33] | New Zealand | Average age of participants 70 (N = 180) w: 122, m: 58 | Pre/post | Peer education program [E] | Health, health-related quality of life | Support, tribal identity, loneliness | The peer-led education program led to improved social connectedness, connection with supportive services, and a sense of identity within the participant’s tribe. |
| Rabiei et al. (2013) [34] | Iran | People aged 55+ (N = 64) w: 33, m: 31 | Semi-experimental study | Family-based empowerment program [E] | Physical/mental health | Roles, social functioning, quality of life | The family-based empowerment program was found to increase quality of life amongst older adults and self-esteem, while self-efficacy remained constant. |
| Shinkai et al. (2016) [35] | Japan | People aged 70+ (N = 686) n/a | Program evaluation (longitudinal) | Health education program [E] | Life-space mobility, instrumental ADL, intellectual activity | Social role | The multicomponent health education and integration program contributed to improved functional health and extended life expectancy. |
| Sims-Gould et al. (2020) [36] | Canada | People aged 65+ (N = 26) w: 18, m: 9 | Qualitative | Health promotion program [E] | Physical activity | Social connectedness, isolation/loneliness | The health promotion program encouraged physical activity and social connections, while addressing loneliness and isolation. |
| Tagliabue et al. (2018) [37] | Italy | People aged 60+ (N = 84) w: 55, m: 29 | Non-randomized cluster trial | Multi-domain cognitive training [E] | Cognitive functioning, memory, executive function, attention | Mood, socialization | The multi-domain cognitive training program reported an improvement in older adults in cognitive functioning and non-verbal reasoning. In addition, improved everyday life, mood, and socialization were also cited as benefits of the program. |
| Multi-domain Interventions | |||||||
| Castle et al. (2008) [38] | United States | People aged 60+ (N = 823) n/a | Program evaluation (longitudinal) | Senior living enhancement program (SLEP) [M] | Physical activity, body function, habits, care, depressive symptoms | Social activities outside the home | The Senior Living Enhancement Program saw improvements in a majority of the “10 Keys to Healthy Aging” including physical activity, general health, and social connectivity. |
| Greenfield and Fedor (2015) [39] | United States | People aged 60+ (N = 35) w: 25, m: 10 | Natural experiment | Naturally occurring retirement community (NORC) supportive service programs [M] | Overall health, well-being | Social connectedness, volunteerism | The NORC supportive service programs found that positive results in health and social outcomes were indicated by the older adult’s relationship with the program, rather than solely their utilization of the program. |
| Orellana et al. (2020) [40] | United Kingdom | People aged 60+ (N = 23) w: 18, m: 5 | Qualitative | Day centers for older adults [M] | Mental well-being/health, physical well-being/health, hygiene | Social participation/involvement, feelings of dignity/control, quality of life, feelings of security | Day centers for community-dwelling older adults had a positive impact on social participation and meaningful occupation. |
| Park et al. (2011) [41] | South Korea | People aged 65+ (N = 45) w: 27, m: 18 | Randomized control trial | Health education and exercise program [M] | Blood pressure, physical activity, health-related quality of life | Self-care, self-efficacy, quality of life (social) | The health education and exercise program improved systolic blood pressure, self-efficacy, mental/physical health, vitality, and social functioning in older adults with hypertension. |
| Rainero et al. (2021) [42] | Italy, Australia, Spain, Germany, Austria, Japan | People aged 60+ (N = 201) w: 148, m: 53 | Randomized control study | Multi-center health promotion program [M] | Depressive symptoms, nutrition, physical/cognitive function, sleep | Social function, quality of life | The multi-domain ICT healthy aging intervention allowed participants in the intervention to maintain their quality of life with no decrease. In addition, participants had improved mood and nutritional habits. |
| Other Interventions | |||||||
| Ballesteros et al. (2012) [43] | Spain, Sweden, Greece | People aged 65+ (N = 29) n/a | Randomized control trial | Online social network platform with technology training [O] | Cognition, depressive symptoms, mobility and performance | Affection, behavioral confirmation, social status, comfort, stimulation | The ICT intervention had a positive impact on cognitive functioning, feelings of achievement, being treated with positive regard, independence, and self-realization. |
| Reinhard et al. (2018) [44] | United Kingdom | People aged 60+ (N = 18,453) w: 9564, m: 8124 | Natural experiment | Free bus pass [O] | Public transport use, depressive symptoms | Loneliness, volunteering, social contacts | The free bus pass contributed to reductions in depressive symptoms and feelings of loneliness among older people. It also promoted more regular contact with friends and children. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hong, A.; Welch-Stockton, J.; Kim, J.Y.; Canham, S.L.; Greer, V.; Sorweid, M. Age-Friendly Community Interventions for Health and Social Outcomes: A Scoping Review. Int. J. Environ. Res. Public Health 2023, 20, 2554. https://doi.org/10.3390/ijerph20032554
Hong A, Welch-Stockton J, Kim JY, Canham SL, Greer V, Sorweid M. Age-Friendly Community Interventions for Health and Social Outcomes: A Scoping Review. International Journal of Environmental Research and Public Health. 2023; 20(3):2554. https://doi.org/10.3390/ijerph20032554
Chicago/Turabian StyleHong, Andy, Jessie Welch-Stockton, Ja Young Kim, Sarah L. Canham, Valerie Greer, and Michelle Sorweid. 2023. "Age-Friendly Community Interventions for Health and Social Outcomes: A Scoping Review" International Journal of Environmental Research and Public Health 20, no. 3: 2554. https://doi.org/10.3390/ijerph20032554
APA StyleHong, A., Welch-Stockton, J., Kim, J. Y., Canham, S. L., Greer, V., & Sorweid, M. (2023). Age-Friendly Community Interventions for Health and Social Outcomes: A Scoping Review. International Journal of Environmental Research and Public Health, 20(3), 2554. https://doi.org/10.3390/ijerph20032554








