Implant Survival in Patients with Chronic Kidney Disease: A Case Report and Systematic Review of the Literature
Abstract
1. Introduction
2. Materials and Methods
2.1. Screening of Scientific Products
2.2. Inclusion and Exclusion Criteria
2.3. Screening Process
2.4. Data Analysis
3. Results
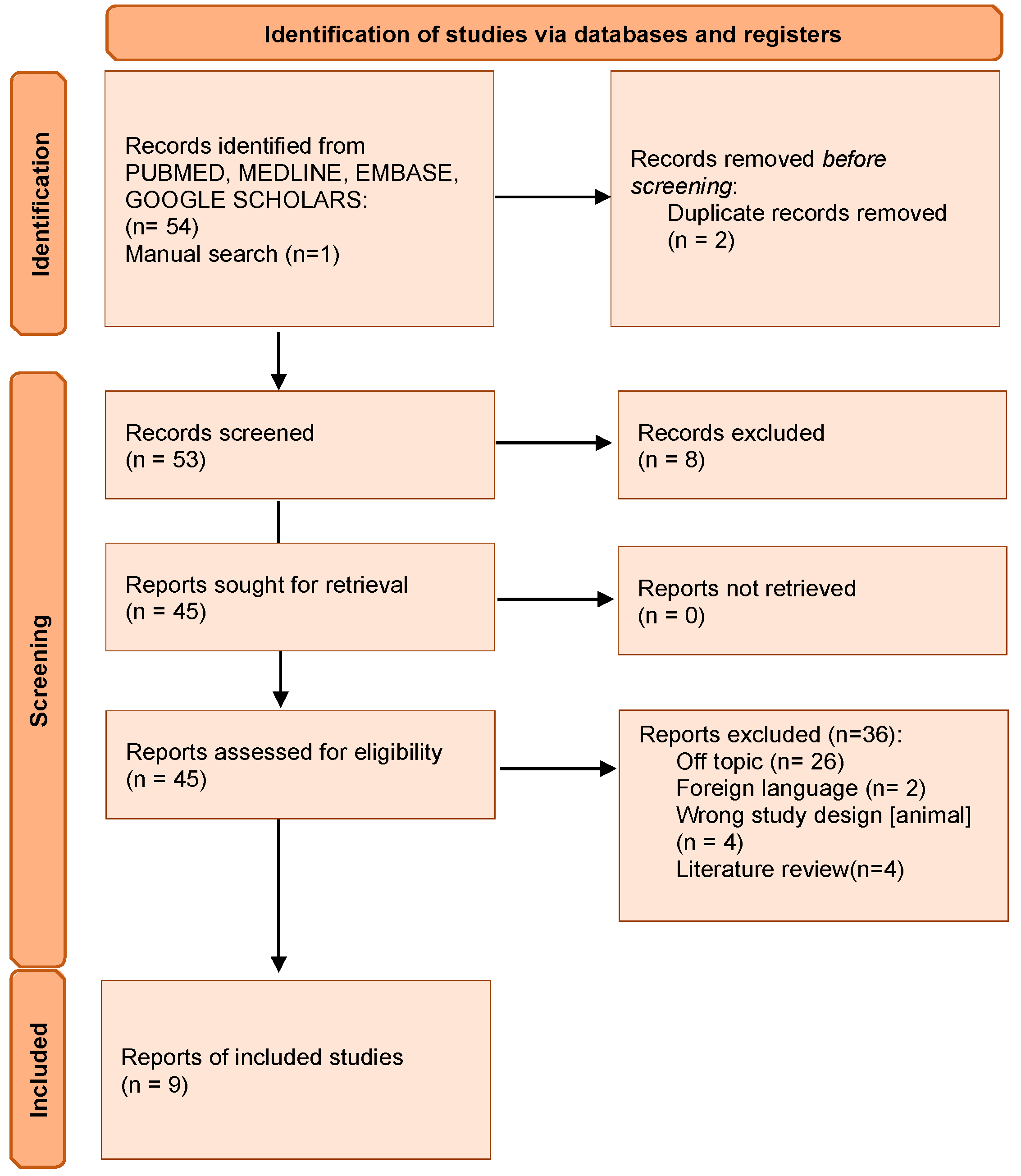
3.1. Preliminary Screening
3.2. Characteristics of the Studies Included
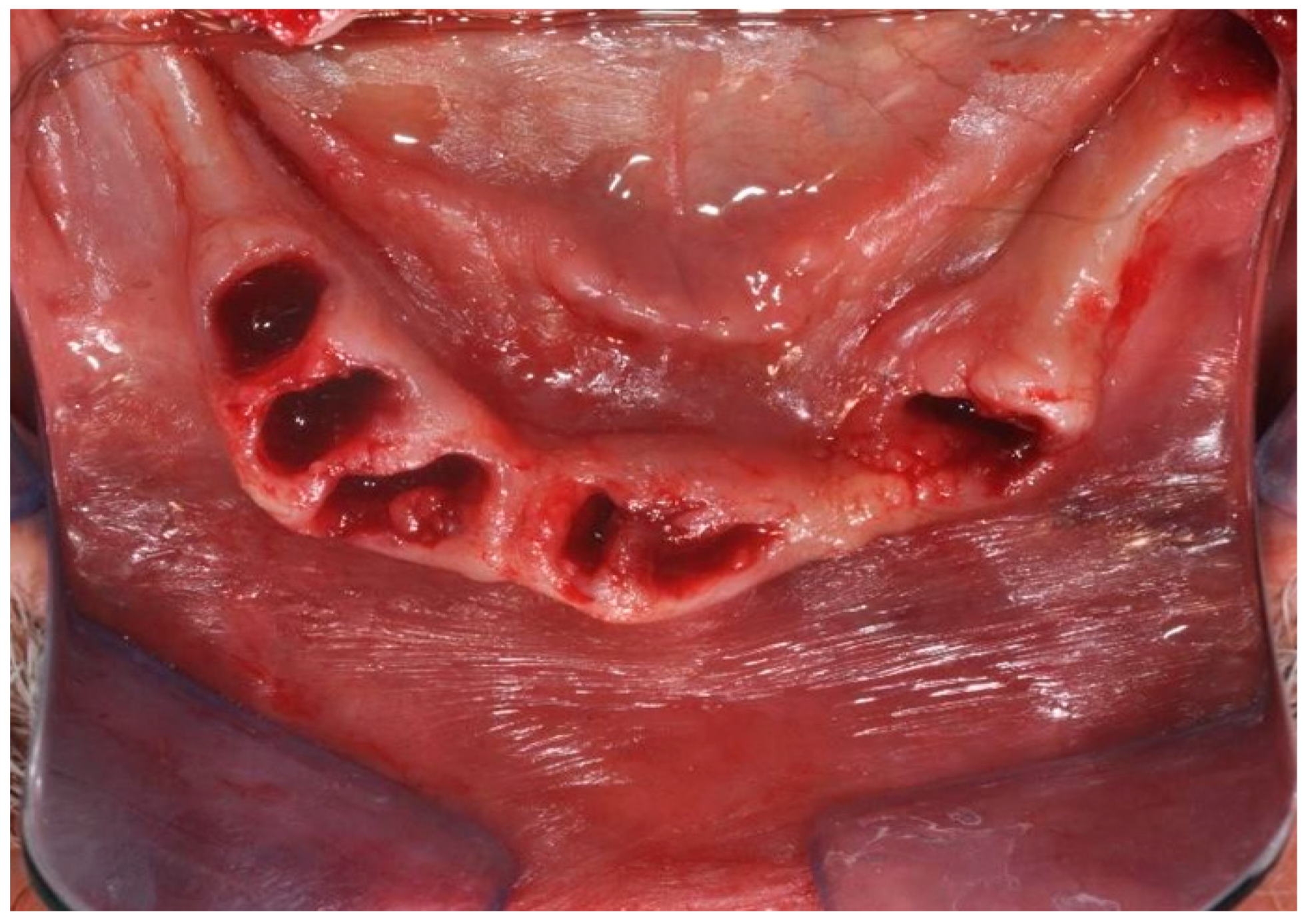
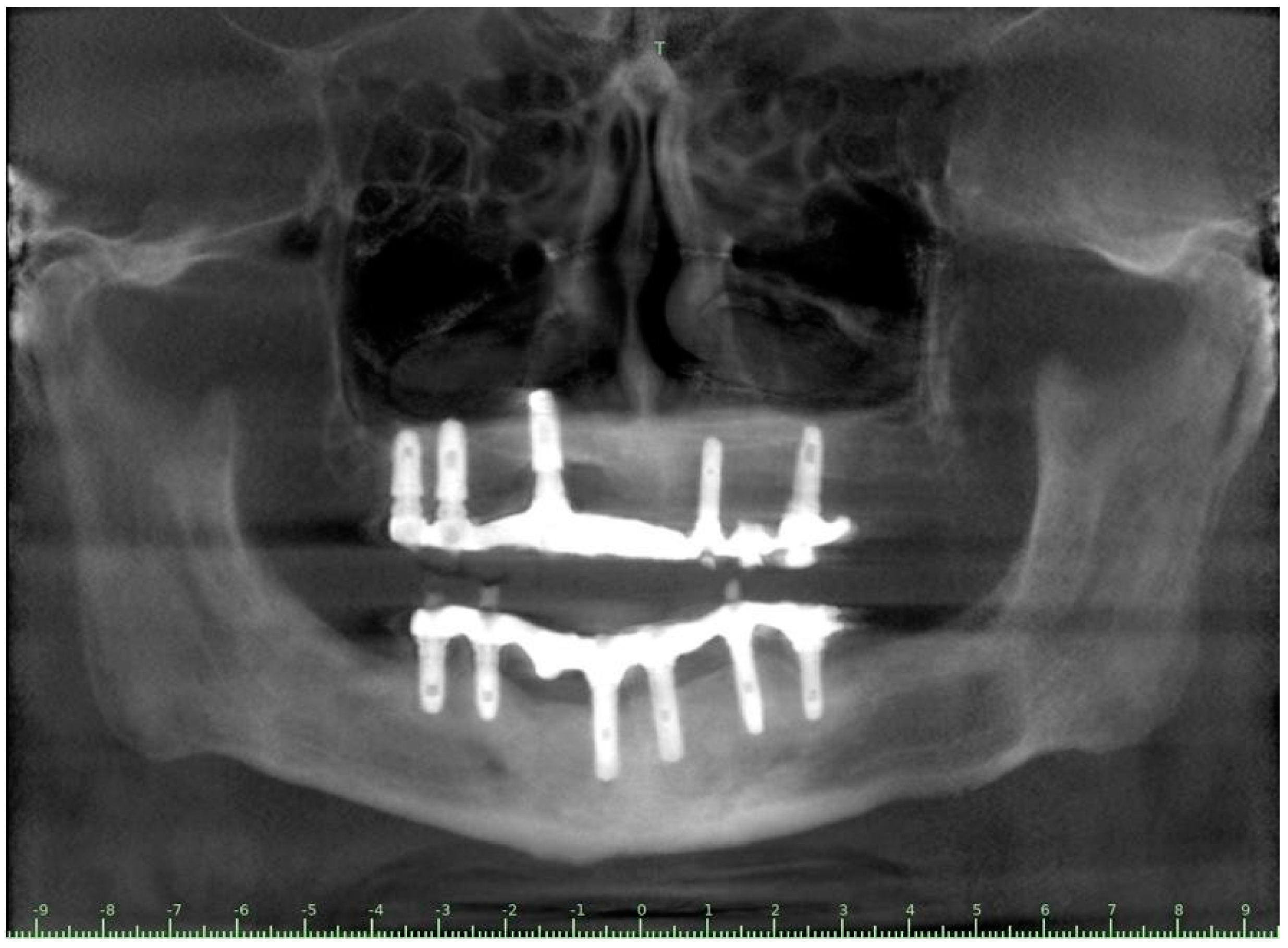
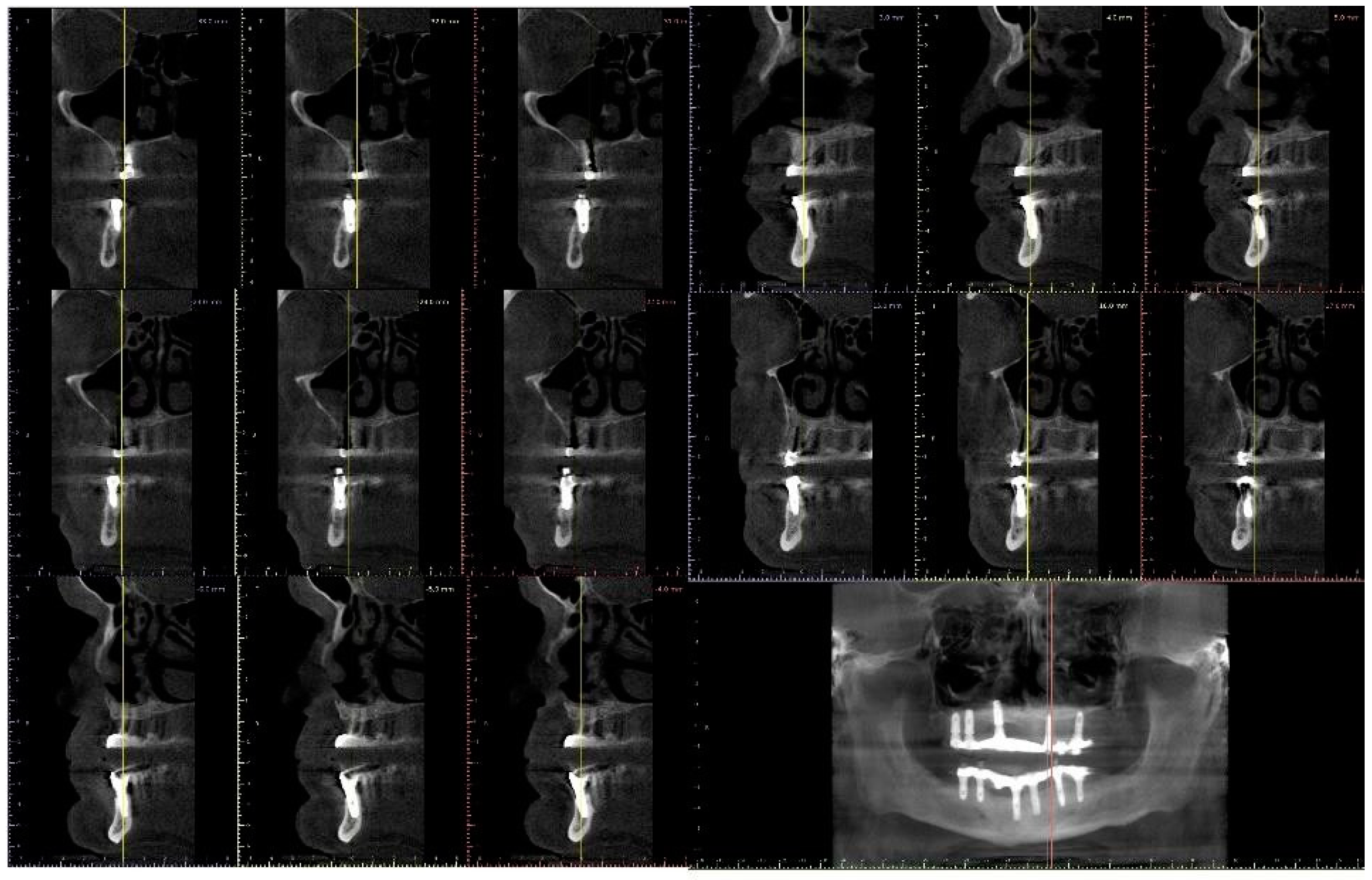
3.3. Case Report
4. Discussion
4.1. Advanced Chronic Kidney Disease and IgA Nephropathy
4.2. Transplanted Patients
4.3. Renal Osteodystrophy
4.4. Enamel-Renal Syndrome (FAM 20A)
4.5. X-Linked Hypophosphatemia
4.6. Fraser’s Syndrome
4.7. PIP Treatment
4.8. Glomerulonephritis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Beschnidt, S.M.; Cacaci, C.; Dedeoglu, K.; Hildebrand, D.; Hulla, H.; Iglhaut, G.; Krennmair, G.; Schlee, M.; Sipos, P.; Stricker, A.; et al. Implant Success and Survival Rates in Daily Dental Practice: 5-Year Results of a Non-Interventional Study Using CAMLOG SCREW-LINE Implants with or without Platform-Switching Abutments. Int. J. Implant Dent. 2018, 4, 33. [Google Scholar] [CrossRef] [PubMed]
- Albrektsson, T.; Brånemark, P.-I.; Hansson, H.-A.; Lindström, J. Osseointegrated Titanium Implants: Requirements for Ensuring a Long-Lasting, Direct Bone-to-Implant Anchorage in Man. Acta Orthop. Scand. 1981, 52, 155–170. [Google Scholar] [CrossRef] [PubMed]
- Buser, D.; Sennerby, L.; De Bruyn, H. Modern Implant Dentistry Based on Osseointegration: 50 Years of Progress, Current Trends and Open Questions. Periodontol. 2000 2017, 73, 7–21. [Google Scholar] [CrossRef] [PubMed]
- Cornelini, R.; Scarano, A.; Covani, U.; Petrone, G.; Piattelli, A. Immediate One-Stage Postextraction Implant: A Human Clinical and Histologic Case Report. Int. J. Oral Maxillofac. Implants 2000, 15, 432–437. [Google Scholar]
- Scarano, A.; Petrini, M.; Mastrangelo, F.; Noumbissi, S.; Lorusso, F. The Effects of Liquid Disinfection and Heat Sterilization Processes on Implant Drill Roughness: Energy Dispersion X-Ray Microanalysis and Infrared Thermography. J. Clin. Med. 2020, 9, 1019. [Google Scholar] [CrossRef] [PubMed]
- Elias, C.N.; Rocha, F.A.; Nascimento, A.L.; Coelho, P.G. Influence of Implant Shape, Surface Morphology, Surgical Technique and Bone Quality on the Primary Stability of Dental Implants. J. Mech. Behav. Biomed. Mater. 2012, 16, 169–180. [Google Scholar] [CrossRef]
- Scarano, A.; Murmura, G.; Carinci, F.; Lauritano, D. Immediately Loaded Small-Diameter Dental Implants: Evaluation of Retention, Stability and Comfort for the Edentulous Patient. Eur. J. Inflamm. 2012, 10, 19–23. [Google Scholar]
- Cavallaro, J.; Greenstein, B.; Greenstein, G. Clinical Methodologies for Achieving Primary Dental Implant Stability. J. Am. Dent. Assoc. 2009, 140, 1366–1372. [Google Scholar] [CrossRef]
- Scarano, A.; Piattelli, A.; Polimeni, A.; Di Iorio, D.; Carinci, F. Bacterial Adhesion on Commercially Pure Titanium and Anatase-Coated Titanium Healing Screws: An in Vivo Human Study. J. Periodontol. 2010, 81, 1466–1471. [Google Scholar] [CrossRef]
- Scarano, A.; Barros, R.R.M.; Iezzi, G.; Piattelli, A.; Novaes, A.B. Acellular Dermal Matrix Graft for Gingival Augmentation: A Preliminary Clinical, Histologic, and Ultrastructural Evaluation. J. Periodontol. 2009, 80, 253–259. [Google Scholar] [CrossRef]
- Gehrke, S.A.; Marin, G.W. Biomechanical Evaluation of Dental Implants with Three Different Designs: Removal Torque and Resonance Frequency Analysis in Rabbits. Ann. Anat. Anat. Anz. Off. Organ Anat. Ges. 2015, 199, 30–35. [Google Scholar] [CrossRef]
- Alonso, F.R.; Triches, D.F.; Mezzomo, L.A.M.; Teixeira, E.R.; Shinkai, R.S.A. Primary and Secondary Stability of Single Short Implants. J. Craniofac. Surg. 2018, 29, e548–e551. [Google Scholar] [CrossRef] [PubMed]
- Monje, A.; Ravidà, A.; Wang, H.-L.; Helms, J.; Brunski, J. Relationship between Primary/Mechanical and Secondary/Biological Implant Stability. Int. J. Oral Maxillofac. Implants 2019, 34, s7–s23. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.G.; Yun, P.-Y.; Kim, Y.-K.; Kim, I. Comparison of Sandblasted and Acid-Etched Surface Implants and New Hydrophilic Surface Implants in the Posterior Maxilla Using a 3-Month Early-Loading Protocol: A Randomized Controlled Trial. J. Korean Assoc. Oral Maxillofac. Surg. 2021, 47, 175–182. [Google Scholar] [CrossRef] [PubMed]
- Cueto-Manzano, A.M.; Konel, S.; Freemont, A.J.; Adams, J.E.; Mawer, B.; Gokal, R.; Hutchison MD, A.J. Effect of 1,25-Dihydroxyvitamin D3 and Calcium Carbonate on Bone Loss Associated with Long-Term Renal Transplantation. Am. J. Kidney Dis. 2000, 35, 227–236. [Google Scholar] [CrossRef]
- Eastwood, J.B.; Bordier, P.J.; Clarkson, E.M.; Tun Chot, S.; de Wardener, H.E. The Contrasting Effects on Bone Histology of Vitamin D and of Calcium Carbonate in the Osteomalacia of Chronic Renal Failure. Clin. Sci. Mol. Med. 1974, 47, 23–42. [Google Scholar] [CrossRef]
- Siddiqui, J.A.; Partridge, N.C. Physiological Bone Remodeling: Systemic Regulation and Growth Factor Involvement. Physiology 2016, 31, 233–245. [Google Scholar] [CrossRef]
- Freemont, T.; Malluche, H.H. Utilization of Bone Histomorphometry in Renal Osteodystrophy: Demonstration of a New Approach Using Data from a Prospective Study of Lanthanum Carbonate. Clin. Nephrol. 2005, 63, 138–145. [Google Scholar] [CrossRef]
- Argilés, A.; Mourad, G.; Mion, C. Oral Vitamin D or Calcium Carbonate in the Prevention of Renal Bone Disease? Curr. Opin. Nephrol. Hypertens. 1996, 5, 329–336. [Google Scholar] [CrossRef]
- Zhao, D.; Zhang, S.; Chen, X.; Liu, W.; Sun, N.; Guo, Y.; Dong, Y.; Mo, A.; Yuan, Q. Evaluation of Periodontitis and Bone Loss in Patients Undergoing Hemodialysis. J. Periodontol. 2014, 85, 1515–1520. [Google Scholar] [CrossRef]
- Dijakiewicz, M.; Wojtowicz, A.; Dijakiewicz, J.; Szycik, V.; Rutkowski, P.; Rutkowski, B. Is Implanto-Prosthodontic Treatment Available for Haemodialysis Patients? Nephrol. Dial. Transplant. 2007, 22, 2722–2724. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. Int. J. Surg. 2010, 8, 336–341. [Google Scholar] [CrossRef] [PubMed]
- Flanagan, D.; Mancini, M. Bimaxillary Full Arch Fixed Dental Implant Supported Treatment for a Patient with Renal Failure and Secondary Hyperparathyroidism and Osteodystrophy. J. Oral Implantol. 2015, 41, e36–e43. [Google Scholar] [CrossRef] [PubMed]
- Gallottini, M.; Llanos, A.H.; Romito, G.A.; Romano, M.M.; de Oliveira, F.B.; de Rezende, N.P.M. Oral Manifestations and Rehabilitation in Fraser Syndrome: A Case Report. In Special Care in Dentistry; Wiley: Hoboken, NJ, USA, 2018; Volume 38, pp. 249–254. [Google Scholar] [CrossRef]
- Malaescu, M.; Tabacaru, B.; Stanca, S.; Stanca, T.H. Bilateral Central Retinal Vein Occlusion, Multiple Dental Implants and Severe Glomerulonephtitis—Any Connection? Romanian J. Ophthalmol. 2019, 63, 287–296. [Google Scholar] [CrossRef]
- Hernández, G.; Paredes, V.; López-Pintor, R.M.; de Andrés, A.; de Vicente, J.C.; Sanz, M. Implant Treatment in Immunosuppressed Renal Transplant Patients: A Prospective Case-Controlled Study. Clin. Oral Implants Res. 2019, 30, 524–530. [Google Scholar] [CrossRef]
- Radzewski, R.; Osmola, K. Osseointegration of Dental Implants in Organ Transplant Patients Undergoing Chronic Immunosuppressive Therapy. Implant Dent. 2019, 28, 447–454. [Google Scholar] [CrossRef]
- Mauprivez, C.; Nguyen, J.-F.; de la Dure-Molla, M.; Naveau, A. Prosthetic Rehabilitation of a Patient with Rare and Severe Enamel Renal Syndrome. Int. J. Prosthodont. 2018, 31, 31–34. [Google Scholar] [CrossRef]
- Lee, B.-N.; Jung, H.-Y.; Chang, H.-S.; Hwang, Y.-C.; Oh, W.-M. Dental Management of Patients with X-Linked Hypophosphatemia. Restor. Dent. Endod. 2017, 42, 146–151. [Google Scholar] [CrossRef]
- Friberg, B.; Sennerby, L.; Linden, B.; Gröndahl, K.; Lekholm, U. Stability Measurements of One-Stage Brånemark Implants during Healing in Mandibles. Int. J. Oral Maxillofac. Surg. 1999, 28, 266–272. [Google Scholar] [CrossRef]
- Di Stefano, D.; Arosio, P.; Perrotti, V.; Iezzi, G.; Scarano, A.; Piattelli, A. Correlation between Implant Geometry, Bone Density, and the Insertion Torque/Depth Integral: A Study on Bovine Ribs. Dent. J. 2019, 7, 25. [Google Scholar] [CrossRef]
- Yuan, Q.; Xiong, Q.-C.; Gupta, M.; López-Pintor, R.M.; Chen, X.-L.; Seriwatanachai, D.; Densmore, M.; Man, Y.; Gong, P. Dental Implant Treatment for Renal Failure Patients on Dialysis: A Clinical Guideline. Int. J. Oral Sci. 2017, 9, 125–132. [Google Scholar] [CrossRef] [PubMed]
- Allen, M.R.; Chen, N.X.; Gattone II, V.H.; Moe, S.M. Adverse Mandibular Bone Effects Associated with Kidney Disease Are Only Partially Corrected with Bisphosphonate and/or Calcium Treatment. Am. J. Nephrol. 2013, 38, 458–464. [Google Scholar] [CrossRef] [PubMed]





| Population\Patients | Intervention | Comparison | Outcomes |
|---|---|---|---|
| Subjects suffering from pathologies and disorders affecting the kidneys who are candidates for implant therapy. | Placement of dental implants in partial/total edentulous crests. | Patients who are healthy/not affected by kidney diseases and disorders | Implant efficacy and survival rate in patients with renal disorders. |
| Search Strategies | |
|---|---|
| Keywords: | Advanced keyword search: (chronic kidney disease OR chronic renal disease OR dialysis OR hemodialysis OR renal failure OR glomerulonephritis OR hypophosphatemia) AND dental implant) |
| Databases | PubMed/Medline, EMBASE, Google Scholars |
| Authors | Journal | Year | Methods | Population | Inc./Excl. Criteria-Subject Characteristics | Main Outcome |
|---|---|---|---|---|---|---|
| Hernández G. et al. [26] | Clin Oral Impl Res | 2019 | Histology; CBCT | -28 partially edentulous RTP -28 control patients | Inc. criteria (1) Renal transplant (>18 months) immunosuppressive treatment. (2) Edentulism (>6 months). (3) Presence of teeth or fixed prosthesis in the opposing arch. (4) Sufficient bone volume for standard implant placement [no graft]. (5) Stable systemic health and clearance Excl. criteria: untreated periodontitis, smokers, radiotherapy, severe or uncontrolled metabolic diseases or lack of compliance. | -Similar ISR T and C groups (~98%) -PImuc [T:46.80%; C: 48.80%]. PImp [T:5.10% T;C: 8.10%]. -Similar wound healing and post-operative pain -No significant comorbidities (age, gender, oral diseases) (p > 0.05) -Significant difference of ISR for implants placed in the anterior mandible higher in C. |
| Flanagan D. et al. [23] | J Oral Implantol | 2015 | clinical and radiographic: full-mouth radiographic series, panoramic and a bimaxillary cone beam computerized scan and mounted study casts | -One patient | Subject of 34 yo male; severely carious teeth and associated chronic abscesses (kidney transplant delayed) Comorbidities: IgA nephropathy, tabagism, hypertension and secondary hyperparathyroidism. Hemodialysis three times weekly. Ph. Therapy: Nephrocaps vitamin (B) supplement, amlodepine, besylate, cinacalcet, metoprolol, paroxetine. Bilateral compound ulnar and radial fractures, 2 blood transfusions. | Successfully treated with dental implant-supported fixed prostheses: fixed bimaxillary porcelain fused to metal implant-supported complete dentures |
| Radzewsk et al. [27] | Implant Dentistry | 2019 | RVG | 21 patients/24 implant 15 subjects/15 implants | Inc.T: 25 yo, 1 year after organ transplant, at least one tooth missing, suff. bone volume and density. [no graft]. Incl. C: No serious systemic diseases, >25 years of age, at least one tooth missing, bone volume and density. [no graft]. Excl. T/C: active periodontitis, occlusion disorders, bone and blood coagulation disorders, untreated dyslipidemia, or smoker. | T: 0.325 mm (min 0–max 0.95) C: 0.5 mm (min 0.15–max 1.8). CBL medians revealed no significant differences (p = 0.089). |
| Lee et al. [29] | Restorative Dentistry and Endodontics | 2016 | Rx, microscopic observ (Carl Zeiss Surgical GmbH) | case 1: 14 yo M (no implat th.) case 2: 38 yo F | XLH: X-linked hypophosphatemia | Implants with consistent hypermobility probably due to the interruption of medication (pregnancy and breastfeeding) |
| Gallottini et al. [24] | Spec Care Dentist | 2018 | One subject [16-yo Female] | FS: Fraser syndrome and kidney disease The patient presented four of the six major criteria for FS, (syndactyly, cryptophthalmos spectrum, one kidney agenesia, and tracheal anomaly). Several oral alterations, anodontia and short dental roots. Intervention: extractions and dental implant planning +administration of oral bisphosphonate (7 years) and osteopenia. -Osteopenia was attributed to the mildrenal insufficiency associated to one kidney and oestrogen deficiency | Total of 2 implants in the two maxillary central incisor sites with low bone density, hand osteotomes with drilling in the maxilla. Implant positioned with bone graft (Bio-Oss). | |
| Mauprivez et al. [28] | The International Journal of Prosthodontics | 2018 | Panoramic radiograph, ceph., Tomography | Case 1: 18-yo M Case 2: (Retrospective cohort study) 3559 I. in 999 patients | Case 1: Enamel Renal Syndrome, FAM20A (family with sequence similarities 20A) gene mutations. Case 2: Medical the with PIP (CDK) | Case 1: 2 symphyseal I. to support an overdenture. One implant failure due to alveolar ridge thinness. Based on successful osseointegration of one implant, decided to perform a bone graft for 2 I. Case 2: PPI intake statistically significant negative effect for implant survival rate (hazard ratio 2.811; 95% CI: 1.139 to 6.937; p = 0.025) |
| Dijakiewicz M. et al. [21] | Oxford Journal | 2007 | -Radiometric analysis of panoramic tomography (DPT), -EPR (electron paramagnetic resonance), radiometric, densitometric, histological and histomorphometry implants simulation, biochemical markers of bone metabolism (calcium, phosphate, PTH, alkaline phosphatase). | T: 100 (HD) haemodialysis C: 50 healthy | ESRD (renal osteodystrophy) | -Decreased quantity and quality of bone tissue of the maxilla and mandible in renal osteodystrophy. -A total of 4 patients excluded due to the time of haemodialysis therapy (<bone density and bone decrease). -No exclusions on potential implant installation in the maxilla -normal function of the implants in patients suffering from renal osteodystrophy. |
| Friberg B. et al. [30] | International Journal of Periodontics & Restorative Dentistry | 2013 | Rx, Computed tomography scans | Case 1: 44 yo F Case 2: 43 yo M Case 3: 63 yo F | X-linked hypophosphatemia | Case 1: <periodontal bone support around remaining teeth, extend the healing period, bone response in relation to all 4 implants was unremarkable. Case 2: 4 regular-platform implants allowed to heal for 12 months prior to abutment connection. Fixed prosthesis positioned and normal bone response around all implants after 20 months post insertion. Case 3 overall majority of placed implants ended in early failure. Present outcome, with all 18 implants successfully in function after up to 5 years, better understanding of this slow bone turnover, allowing for markedly longer healing periods after extraction and implant placement |
| Malaescu M. et al. [25] | Romanian Journal of Ophtalmology | 2019 | -External and slit-lamp examination of the anterior segment of central retinal vein series of clinical, paraclinical and laboratory investigations -Blood count, coagulogram, and erythrocyte sedimentation rate; | -one subject: [54 yo, untreated chronic hepatitis C] | Bilateral central retinal vein occlusion after dental implant procedure. -high AST, ALT, and GGT levels due to hepatitis C infection and normal urea and creatinine values. Glucose levels were normal. -No significant findings at the cardio-vascular and rheumatologic exam. Nephrotic Syndrome and Stage III Renal Failure, leading to the diagnosis of Idiopathic Glomerulonephritis. Renal transplant bacterial endocarditis with MRSA and required minimally invasive mitral valve replacement | Decrease of visual acuity after the patient received 11 I., in over 1 year. Bilateral Central Retinal Vein Occlusion with Non-tractional Macular Edema OS > OD. In the following years, the general condition deteriorated, several systemic pathologies: arterial hypertension, hypertensive cardiomyopathy and nyha ii heart failure. |
| Authors | Journal | Year | Study Findings | Implant Failure | Follow Up | Renal Disease |
|---|---|---|---|---|---|---|
| Hernández G. et al. [26] | Clin Oral Impl Res | 2019 | AI, MCI and TP reduction in mineral density of the cortical and trabecular bone in CRF patients and more severely in patients under haemodialysis compared to peritoneal dialysis | 1 IF in T | Mean follow-up of 116.8 months range from 84 to 192 months) | Renal transplant patients, are subjected pharmacological immunosuppression therapy |
| Flanagan D. et al. [23] | J Oral Implantol | 2015 | -Implant treatment for patients with IgA nephropathy (secondary hyperparathyroidism and osteodystrophy) may be successful. -Appropriate calcium therapy is important serum calcium to prevent inappropriate bone remodeling | 2 years | Long-term dialysis patient with end-stage renal disease (ESRD)also referred to as chronic kidney disease (CKD) due to IgA nephropathy complicated by severe secondary hyperparathyroidism and renal osteodystrophy | |
| Radzewsk et al. [27] | Implant Dentistry | 2019 | Patients with organ transplants can safely and effectively undergo dental implant treatment. | 2 years | Renal transplant patients, are subjected to pharmacological immunosuppression therapy | |
| Lee et al. [29] | Restorative Dentistry and Endodontics | 2016 | -Implant installation is not contraindicated for patients with XLH. -Uncertain possible prognoses. Interruption of medication may have negative influence on bone healing. -Blood calcium and phosphate concentrations in XLH patients should be monitored before surgery. | Case 2: hypermobility | Case 2: 1 year and 6 months | XLH: hereditary metabolic disease caused by the loss of phosphate through the renal tubules into the urine, and an associated decrease in serum calcium and potassium phosphate. XLH is the most common form of hypophosphatemic vitamin D-resistant rickets is a metabolic disorder involving <levels of Calcium and potassium phosphate due to the abnormal excretion of phosphate from the kidneys |
| Gallottini et al. [24] | Spec Care Dentist | 2018 | Imminent dental loss of the two upper central incisors (3 mobility-very short roots). -Suspended oral alendronate for 3 months before and 3 months after surgery. -Bisphosphonate oral use has also, albeit more rarely, been linked to osteonecrosis of the jaw; besides that, in this specific case, the dental roots of both teeth were very short, requiring less bone remodeling in the cicatricial process | 4 months | FS, rare Ar malformation disorder | |
| Mauprivez et al. [28] | The International Journal of Prosthodontics | 2018 | Case 1: Lost implant due to thinness of the alveolar ridge. Based on successful osseointegration of one implant, a bone graft for the second implant was performed. Case 2: Intake of Proton Pump Inhibitors-associated with the incidence of chronic kidney disease (Ckd), its progression or end-stage renal disease- is also associated with an increased risk of dental implant failure | Case 1: 1 IF Case 2: -45/178 IF implant failure rates 12.0% (30/250) for PPI users and 4.5% (148/3309) for nonusers. -45 /178 (25.3%) failed implants were lost up to abutment connection (6 in PPI users, 39 in nonusers), with an early-to-late failure ratio of 0.34:1. | Case 1: 2 (control for 1 st I.) - 3 (2 nd I.)-4 (control 2 nd) 6 months (control) Case 2: 34 years | Case 1:FAM20A (family with sequence similarities 20 A) Case 2: PIP associated with the incidence of chronic kidney disease (Ckd) |
| Dijakiewicz M. et al. [21] | Oxford Journal | 2007 | -No contraindication to implant treatment. -HD patients need more frequent professional advice on oral hygiene and microbiological control using RT-PCR | 5 years | “Renal osteodystrophy, ESRD patients are immunodeficient, a condition caused by disturbances of the cellular and humoral immunological response” | |
| Friberg B. et al. [30] | The International Journal of Periodontics & Restorative Dentistry | 2013 | Excellent marginal bone response seen over time; one could strongly recommend implant treatment in patients with XLH. | 4 Implants failed (Case 3) | Case 1: 50 and 31 months. Case 2: 2 years. Other case study: 5 years. | XLH is an inborn X-linked D osteomalacia Patients show a defect in the phosphate-regulating gene with increased urinary excretion of phosphate, resulting in hypophosphatemia and low vitamin D activity |
| Malaescu M. et al. [25] | Romanian Journal of Ophtalmology | 2019 | Excluded acquired or genetic causes, Bilateral central retinal vein occlusion is a rare occurrence. The fact that the patient developed a drop in visual acuity in both eyes over a period of a few days pointed to the fact that systemic imbalance or disease must exist. -More severe complications like permanent amaurosis, orbital cellulitis, orbital abscess, and endophthalmitis were reported in the literature due to local anesthetic solution reaching the orbit through vascular, neurological, or lymphatic network. -The toxic effect of some of the implanted materials could also be a cause for the vein occlusion, due to hypotized toxic, irritant, and allergenic properties of dental materials. | 4 years | Bilateral Central Retinal Vein Occlusion, Idiopathic Glomerulonephritis |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alla, I.; Lorusso, F.; Gehrke, S.A.; Inchingolo, F.; Di Carmine, M.; Scarano, A. Implant Survival in Patients with Chronic Kidney Disease: A Case Report and Systematic Review of the Literature. Int. J. Environ. Res. Public Health 2023, 20, 2401. https://doi.org/10.3390/ijerph20032401
Alla I, Lorusso F, Gehrke SA, Inchingolo F, Di Carmine M, Scarano A. Implant Survival in Patients with Chronic Kidney Disease: A Case Report and Systematic Review of the Literature. International Journal of Environmental Research and Public Health. 2023; 20(3):2401. https://doi.org/10.3390/ijerph20032401
Chicago/Turabian StyleAlla, Iris, Felice Lorusso, Sergio Alexandre Gehrke, Francesco Inchingolo, Maristella Di Carmine, and Antonio Scarano. 2023. "Implant Survival in Patients with Chronic Kidney Disease: A Case Report and Systematic Review of the Literature" International Journal of Environmental Research and Public Health 20, no. 3: 2401. https://doi.org/10.3390/ijerph20032401
APA StyleAlla, I., Lorusso, F., Gehrke, S. A., Inchingolo, F., Di Carmine, M., & Scarano, A. (2023). Implant Survival in Patients with Chronic Kidney Disease: A Case Report and Systematic Review of the Literature. International Journal of Environmental Research and Public Health, 20(3), 2401. https://doi.org/10.3390/ijerph20032401











