Comparison of Single Target-Controlled Infusion Pump-Delivered Mixed Propofol and Remifentanil with Two Target-Controlled Infusion Pumps-Delivered Propofol and Remifentanil in Patients Undergoing Breast Cancer Surgery—A Prospective Study
Abstract
1. Introduction
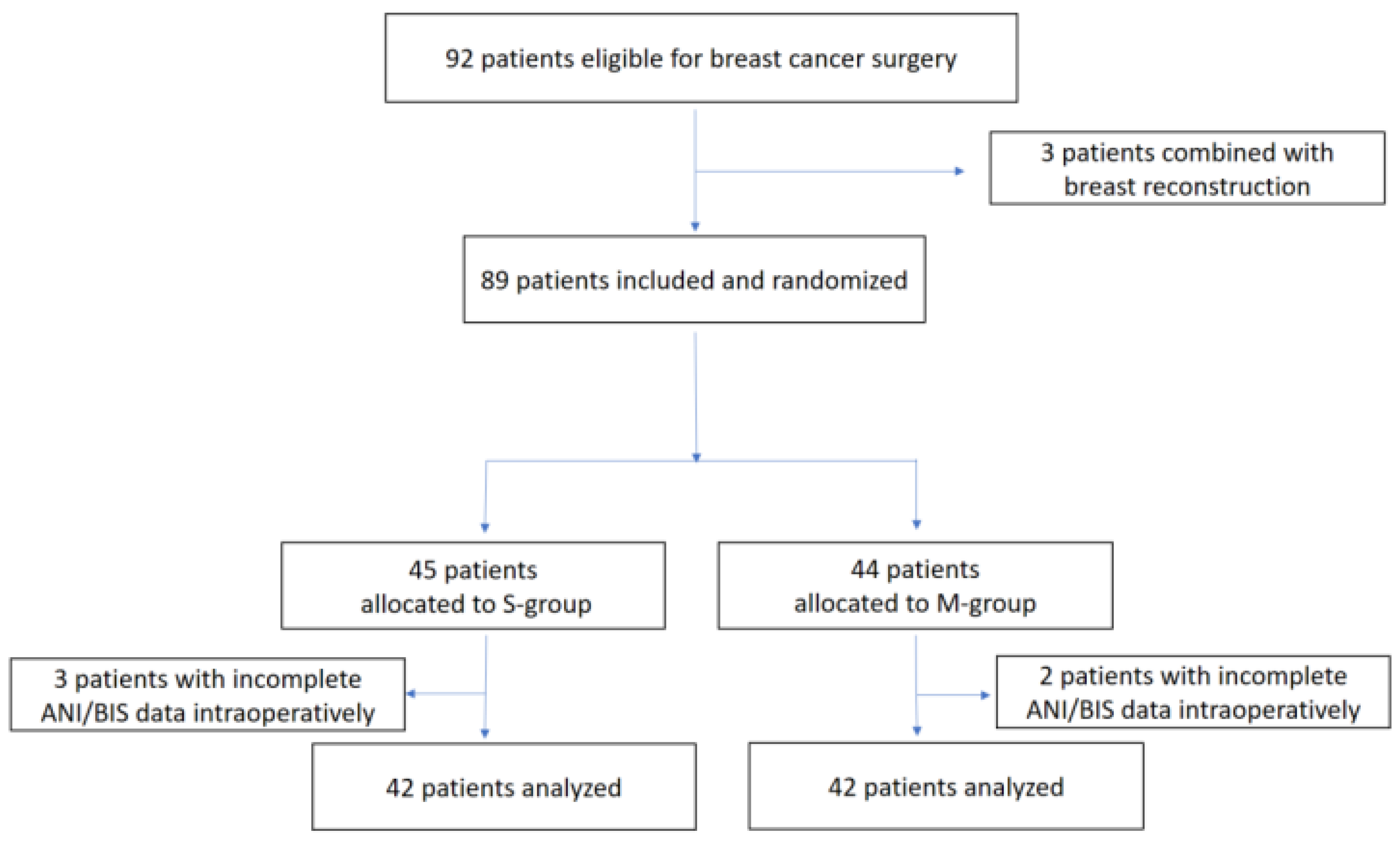
2. Materials and Methods
2.1. Study Design and Setting
2.2. Participants and Data Sources
2.3. Mixture Preparation
2.4. Anesthesia and Monitoring
2.5. Induction and Maintenance
2.6. Emergence from Anesthesia
2.7. Outcomes
2.8. Statistical Analysis
2.9. Power and Sample Size
3. Results
3.1. Baseline Characteristics
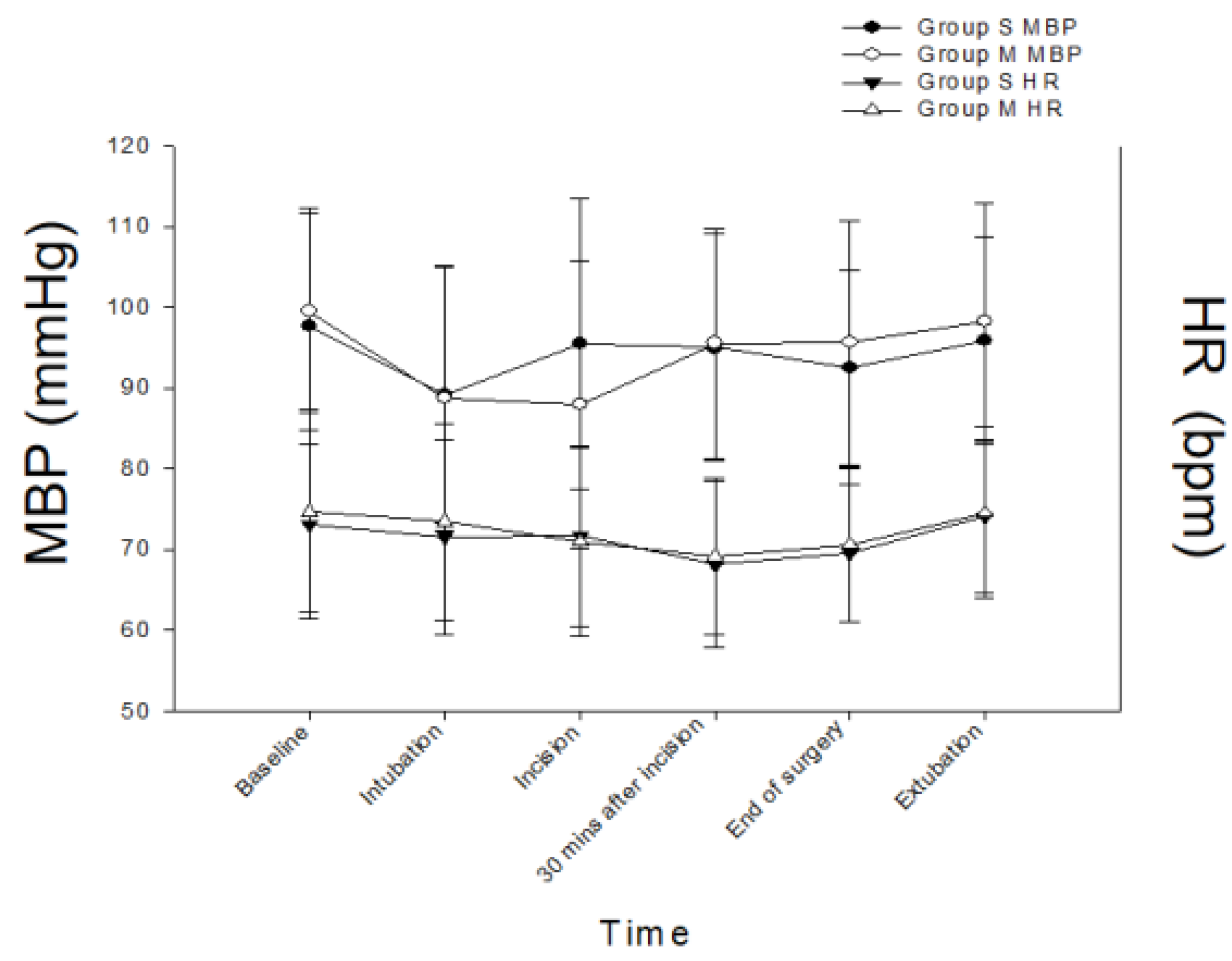
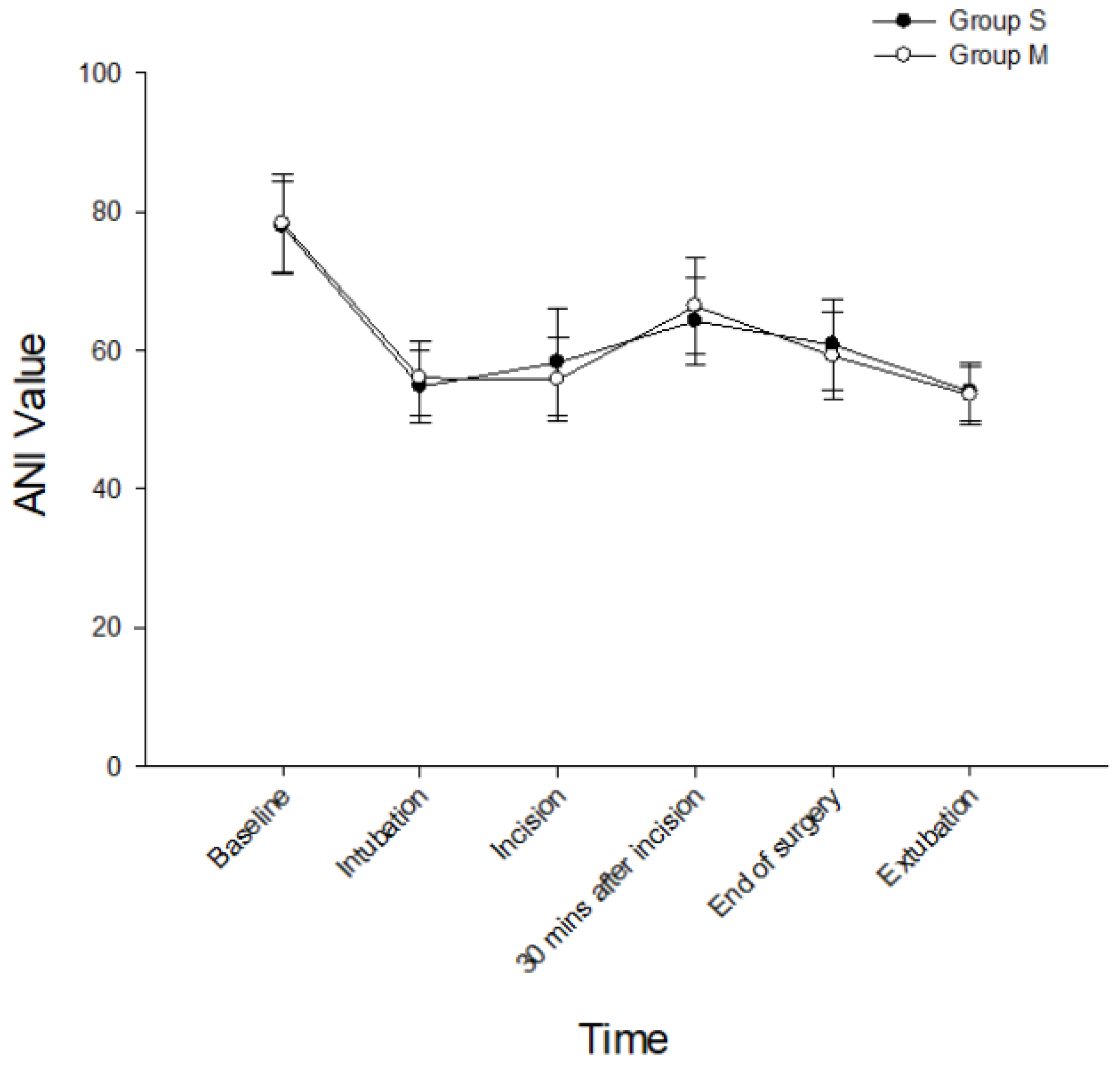
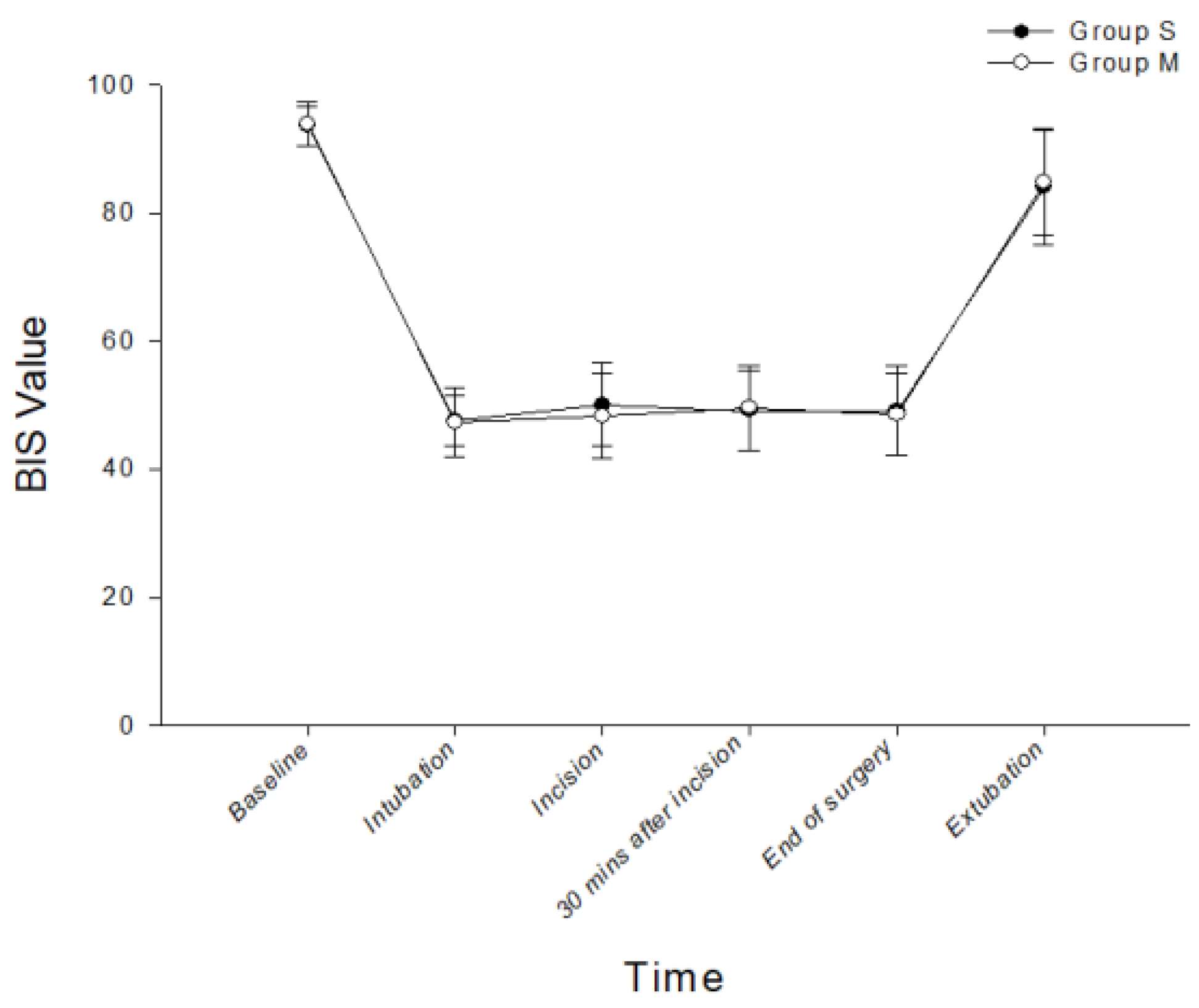
3.2. Perioperative Parameters for the Two Groups
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Vuyk, J. Pharmacokinetic and pharmacodynamic interactions between opioids and propofol. J. Clin. Anesth. 1997, 9 (Suppl. S6), 23s–26s. [Google Scholar] [CrossRef]
- Santonocito, C.; Noto, A.; Crimi, C.; Sanfilippo, F. Remifentanil-induced postoperative hyperalgesia: Current perspectives on mechanisms and therapeutic strategies. Local Reg. Anesth. 2018, 11, 15–23. [Google Scholar] [CrossRef] [PubMed]
- Al-Rifai, Z.; Mulvey, D. Principles of total intravenous anaesthesia: Basic pharmacokinetics and model descriptions. BJA Educ. 2016, 16, 92–97. [Google Scholar] [CrossRef]
- Berkenbosch, J.W.; Graff, G.R.; Stark, J.M.; Ner, Z.; Tobias, J.D. Use of a remifentanil-propofol mixture for pediatric flexible fiberoptic bronchoscopy sedation. Paediatr. Anesth. 2004, 14, 941–946. [Google Scholar] [CrossRef] [PubMed]
- Tsui, B.C.; Wagner, A.; Usher, A.G.; Cave, D.A.; Tang, C. Combined propofol and remifentanil intravenous anesthesia for pediatric patients undergoing magnetic resonance imaging. Paediatr. Anesth. 2005, 15, 397–401. [Google Scholar] [CrossRef]
- Pedersen, N.A.; Jensen, A.G.; Kilmose, L.; Olsen, K.S. Propofol-remifentanil or sevoflurane for children undergoing magnetic resonance imaging? A randomised study. Acta Anaesthesiol. Scand. 2013, 57, 988–995. [Google Scholar] [CrossRef]
- Lai, H.C.; Wu, T.S.; Lai, M.F.; Huang, Y.H.; Chen, J.Y.; Lin, Y.T.; Wu, Z.F. A comparison of two proportions of remifentanil–propofol mixture administered with target-controlled infusion for patients undergoing colonoscopy. J. Med. Sci. 2020, 40, 272–278. [Google Scholar]
- Mandel, J.E.; Tanner, J.W.; Lichtenstein, G.R.; Metz, D.C.; Katzka, D.A.; Ginsberg, G.G.; Kochman, M.L. A randomized, controlled, double-blind trial of patient-controlled sedation with propofol/remifentanil versus midazolam/fentanyl for colonoscopy. Anesth. Analg. 2008, 106, 434–439. [Google Scholar] [CrossRef]
- Joo, J.D.; In, J.H.; Kim, D.W.; Jung, H.S.; Kang, J.H.; Yeom, J.H.; Choi, J.W. The comparison of sedation quality, side effect and recovery profiles on different dosage of remifentanil patient-controlled sedation during breast biopsy surgery. Korean J. Anesth. 2012, 63, 431–435. [Google Scholar] [CrossRef]
- Joo, H.S.; Perks, W.J.; Kataoka, M.T.; Errett, L.; Pace, K.; Honey, R.J. A comparison of patient-controlled sedation using either remifentanil or remifentanil-propofol for shock wave lithotripsy. Anesth. Analg. 2001, 93, 1227–1232. [Google Scholar] [CrossRef]
- Fish, W.H.; Hobbs, A.J.; Daniels, M.V. Comparison of sevoflurane and total intravenous anaesthesia for daycase urological surgery. Anaesthesia 1999, 54, 1002–1006. [Google Scholar] [CrossRef]
- Goudra, B.G.; Singh, P.M.; Sinha, A. Providing anesthesia in a remote location for radiation oncology in an adult—Problems and solutions. J. Anaesthesiol. Clin. Pharm. 2014, 30, 114–116. [Google Scholar] [CrossRef] [PubMed]
- Ryu, J.H.; Kim, M.; Bahk, J.H.; Do, S.H.; Cheong, I.Y.; Kim, Y.C. A comparison of retrobulbar block, sub-Tenon block, and topical anesthesia during cataract surgery. Eur. J. Ophthalmol. 2009, 19, 240–246. [Google Scholar] [CrossRef] [PubMed]
- Kramer, K.J.; Ganzberg, S.; Prior, S.; Rashid, R.G. Comparison of propofol-remifentanil versus propofol-ketamine deep sedation for third molar surgery. Anesth. Prog. 2012, 59, 107–117. [Google Scholar] [CrossRef] [PubMed]
- Mazanikov, M.; Udd, M.; Kylänpää, L.; Mustonen, H.; Lindström, O.; Halttunen, J.; Färkkilä, M.; Pöyhiä, R. Patient-controlled sedation for ERCP: A randomized double-blind comparison of alfentanil and remifentanil. Endoscopy 2012, 44, 487–492. [Google Scholar] [CrossRef]
- Brady, W.J.; Meenan, D.R.; Shankar, T.R.; Balon, J.A.; Mennett, D.R. Use of a remifentanil and propofol combination in outpatients to facilitate rapid discharge home. AANA J. 2005, 73, 207–210. [Google Scholar]
- Bagshaw, O.; McCormack, J.; Brooks, P.; Marriott, D.; Baxter, A. The safety profile and effectiveness of propofol-remifentanil mixtures for total intravenous anesthesia in children. Paediatr. Anesth. 2020, 30, 1331–1339. [Google Scholar] [CrossRef]
- Bakan, M.; Umutoglu, T.; Topuz, U.; Guler, E.Y.; Uysal, H.; Ozturk, E. Prospective evaluation of remifentanil-propofol mixture for total intravenous anesthesia: A randomized controlled study. Exp Ther. Med. 2021, 22, 1198. [Google Scholar] [CrossRef]
- Malherbe, S.; Barker, N. Mixing of propofol and remifentanil. Paediatr. Anesth. 2021, 31, 504–505. [Google Scholar] [CrossRef]
- Stewart, J.T.; Warren, F.W.; Maddox, F.C.; Viswanathan, K.; Fox, J.L. The stability of remifentanil hydrochloride and propofol mixtures in polypropylene syringes and polyvinylchloride bags at 22 degrees-24 degrees C. Anesth. Analg. 2000, 90, 1450–1451. [Google Scholar] [CrossRef]
- Eleveld, D.J.; Colin, P.; Absalom, A.R.; Struys, M.M.R.F. Pharmacokinetic-pharmacodynamic model for propofol for broad application in anaesthesia and sedation. Br. J. Anesth. 2018, 120, 942–959. [Google Scholar] [CrossRef]
- Nestor, C.C.; Sepúlveda, V.P.O.; Irwin, M.G. Drug mixtures and infusion technology. MasterChef or Hell’s Kitchen? Anaesthesia 2022, 77, 260–263. [Google Scholar] [CrossRef] [PubMed]
- Gruenewald, M.; Ilies, C.; Herz, J.; Schoenherr, T.; Fudickar, A.; Höcker, J.; Bein, B. Influence of nociceptive stimulation on analgesia nociception index (ANI) during propofol-remifentanil anaesthesia. Br. J. Anesth. 2013, 110, 1024–1030. [Google Scholar] [CrossRef] [PubMed]
- Funcke, S.; Sauerlaender, S.; Pinnschmidt, H.O.; Saugel, B.; Bremer, K.; Reuter, D.A.; Nitzschke, R. Validation of innovative techniques for monitoring nociception during general anesthesia: A clinical study using tetanic and intracutaneous electrical stimulation. Anesthesiology 2017, 127, 272–283. [Google Scholar] [CrossRef] [PubMed]
- Dundar, N.; Kus, A.; Gurkan, Y.; Toker, K.; Solak, M. Analgesia nociception index (ani) monitoring in patients with thoracic paravertebral block: A randomized controlled study. J. Clin. Monit. Comput. 2018, 32, 481–486. [Google Scholar] [CrossRef] [PubMed]
- Sabourdin, N.; Burey, J.; Tuffet, S.; Thomin, A.; Rousseau, A.; Al-Hawari, M.; Taconet, C.; Louvet, N.; Constant, I. Analgesia nociception index-guided remifentanil versus standard care during propofol anesthesia: A randomized controlled trial. J. Clin. Med. 2022, 11, 333. [Google Scholar] [CrossRef]
- Aydogmus, M.T.; Türk, H.S.; Oba, S.; Gokalp, O. A comparison of different proportions of a ketamine-propofol mixture administered in a single injection for patients undergoing colonoscopy. Arch. Med. Sci. 2015, 11, 570–576. [Google Scholar] [CrossRef]
- Huang, Y.H.; Lee, M.S.; Lin, Y.T.; Huang, N.C.; Kao, J.; Lai, H.C.; Lin, B.F.; Cheng, K.I.; Wu, Z.F. Postoperative drip-infusion of remifentanil reduces postoperative pain-a retrospective observative study. Int. J. Environ. Res. Public Health 2021, 18, 9225. [Google Scholar] [CrossRef]
- Comelon, M.; Raeder, J.; Stubhaug, A.; Nielsen, C.S.; Draegni, T.; Lenz, H. Gradual withdrawal of remifentanil infusion may prevent opioid-induced hyperalgesia. Br. J. Anesth. 2016, 116, 524–530. [Google Scholar] [CrossRef] [PubMed]
- Nelson, G.; Altman, A.D.; Nick, A.; Meyer, L.A.; Ramirez, P.T.; Achtari, C.; Antrobus, J.; Huang, J.; Scott, M.; Wijk, L.; et al. Guidelines for pre- and intra-operative care in gynecologic/oncology surgery: Enhanced Recovery After Surgery (ERAS®) Society recommendations—Part I. Gynecol. Oncol. 2016, 140, 313–322. [Google Scholar] [CrossRef] [PubMed]
- Smischney, N.J.; Beach, M.L.; Loftus, R.W.; Dodds, T.M.; Koff, M.D. Ketamine/propofol admixture (ketofol) is associated with improved hemodynamics as an induction agent: A randomized, controlled trial. J. Trauma Acute Care Surg. 2012, 73, 94–101. [Google Scholar] [CrossRef]
- Slavik, V.C.; Zed, P.J. Combination ketamine and propofol for procedural sedation and analgesia. Pharmacotherapy 2007, 27, 1588–1598. [Google Scholar] [CrossRef] [PubMed]
- Jalili, M.; Bahreini, M.; Doosti-Irani, A.; Masoomi, R.; Arbab, M.; Mirfazaelian, H. Ketamine-propofol combination (ketofol) vs propofol for procedural sedation and analgesia: Systematic review and meta-analysis. Am. J. Emerg. Med. 2016, 34, 558–569. [Google Scholar] [CrossRef] [PubMed]
- Sim, K.M.; Boey, S.K.; Heng, P.W.; Chan, Y.W. Total intravenous anaesthesia using 3-in-1 mixture of propofol, alfentanil and mivacurium. Ann. Acad. Med. Singap. 2000, 29, 182–188. [Google Scholar] [PubMed]
- Taylor, I.N.; Kenny, G.N.; Glen, J.B. Pharmacodynamic stability of a mixture of propofol and alfentanil. Br. J. Anesth. 1992, 69, 168–171. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, S.; Zhang, Y.L.; Christians, U.; Morrison, J.E., Jr.; Friesen, R.H. Remifentanil and propofol undergo separation and layering when mixed in the same syringe for total intravenous anesthesia. Paediatr. Anesth. 2016, 26, 703–709. [Google Scholar] [CrossRef] [PubMed]
- Absalom, A.R.; Rigby-Jones, A.E.; Rushton, A.R.; Robert-Sneyd, J. De-mystifying the “Mixifusor”. Paediatr. Anesth. 2020, 30, 1292–1298. [Google Scholar] [CrossRef] [PubMed]
- Henkel, E.; Vella, R.; Behan, K.; Austin, D.; Kruger, P.; Fenning, A. The effect of concentration, reconstitution solution and pH on the stability of a remifentanil hydrochloride and propofol admixture for simultaneous co-infusion. BMC Anesth. 2020, 20, 283. [Google Scholar] [CrossRef]
- Wylie, N.; Beale, L.; Westley, I. Consistency of remifentanil concentrations in propofol-remifentanil infusions. A laboratory-based study. Paediatr. Anesth. 2022, 32, 727–731. [Google Scholar] [CrossRef]
- Nimmo, A.F.; Absalom, A.R.; Bagshaw, O.; Biswas, A.; Cook, T.M.; Costello, A.; Grimes, S.; Mulvey, D.; Shinde, S.; Whitehouse, T.; et al. Guidelines for the safe practice of total intravenous anaesthesia (TIVA): Joint Guidelines from the Association of Anaesthetists and the Society for Intravenous anaesthesia. Anaesthesia 2019, 74, 211–224. [Google Scholar] [CrossRef] [PubMed]
- Nestor, C.C.; Sepulveda, P.; Irwin, M.G. Drug mixtures and infusion technology: Replies. Anaesthesia 2022, 77, 837–838. [Google Scholar] [CrossRef] [PubMed]
- Lai, H.C.; Huang, Y.H.; Chen, J.Y.; Wong, C.S.; Cheng, K.I.; Shen, C.H.; Wu, Z.F. Safe practice of total intravenous anesthesia with target-controlled infusion in Taiwan: A recommendation. Asian J. Anesth. 2021, 59, 123–134. [Google Scholar]
- Zhang, C.; Xu, L.; Ma, Y.Q.; Sun, Y.X.; Li, Y.H.; Zhang, L.; Feng, C.S.; Luo, B.; Zhao, Z.L.; Guo, J.R.; et al. Bispectral index monitoring prevent awareness during total intravenous anesthesia: A prospective, randomized, double-blinded, multi-center controlled trial. Chin. Med. J. 2011, 124, 3664–3669. [Google Scholar]
- Gao, W.W.; He, Y.H.; Liu, L.; Yuan, Q.; Wang, Y.F.; Zhao, B. BIS Monitoring on Intraoperative Awareness: A Meta-analysis. Curr. Med. Sci. 2018, 38, 349–353. [Google Scholar] [CrossRef] [PubMed]
- Schnider, T.W.; Minto, C.F.; Egan, T.D.; Filipovic, M. Relationship between propofol target concentrations, bispectral index, and patient covariates during anesthesia. Anesth. Analg. 2021, 132, 735–742. [Google Scholar] [CrossRef]
- Jiao, Y.; He, B.; Tong, X.; Xia, R.; Zhang, C.; Shi, X. Intraoperative monitoring of nociception for opioid administration: A meta-analysis of randomized controlled trials. Minerva Anestesiol. 2019, 85, 522–530. [Google Scholar] [CrossRef] [PubMed]
- Yi, P.; Pryzbylkowski, P. Opioid induced hyperalgesia. Pain Med 2015, 16 (Suppl. S1), S32–S36. [Google Scholar] [CrossRef]
- Rolke, R.; Magerl, W.; Andrews Campbell, K.; Schalber, C.; Caspari, S.; Birklein, F.; Treede, R.-D. Quantitative sensory testing: A comprehensive protocol for clinical trials. Eur. J. Pain. 2006, 10, 77–88. [Google Scholar] [CrossRef]
- Jo, H.R.; Chae, Y.K.; Kim, Y.H.; Chai, H.S.; Lee, W.K.; Choi, S.S.; Min, J.H.; Choi, I.G.; Choi, Y.S. Remifentanil-induced pronociceptive effect and its prevention with pregabalin. Korean J. Anesthesiol. 2011, 60, 198–204. [Google Scholar] [CrossRef]
| Variables | S-Group (n = 42) | M-Group (n = 42) | p Value |
|---|---|---|---|
| Age (y/o) | 55.4 ± 10.1 | 56.9 ± 11.5 | 0.520 |
| Height (cm) | 158.5 ± 6.4 | 156.4 ± 6.3 | 0.135 |
| Weight (kg) | 59.1 ± 10.3 | 59.4 ± 11.0 | 0.882 |
| BMI (kg.m−2) | 23.6 ± 4.3 | 24.3 ± 4.1 | 0.444 |
| ASA class, II/III (n [%]) | 41/1 (97.6%/2.4%) | 40/2 (95%/5%) | 1 |
| Comorbidities (n) | |||
| Hypertension | 9 | 9 | 1 |
| Diabetes mellitus | 3 | 6 | 0.483 |
| Bronchial asthma | 3 | 0 | 0.241 |
| Thyroid disorder | 3 | 4 | 1 |
| Surgical procedures (n [%]) | 0.130 | ||
| MRM | 19(45%) | 22 (52%) | |
| BCS | 23 (55%) | 20 (48%) | |
| Surgical time (min) | 50.7 ± 10.4 | 51.73 ± 10.9 | 0.646 |
| Anesthetic time (min) | 67.4 ± 10.8 | 68.2 ± 10.1 | 0.715 |
| Emergence time (min) | 3.9 ± 2.7 | 2.9 ± 2.5 | 0.065 |
| Variables | S-Group (n = 42) | M-Group (n = 42) | p Value |
|---|---|---|---|
| Frequency of TCI device adjustments (times) | 3 (0–6) | 2 (0–6) | 0.005 |
| Increase | 1 (0–3) | 1 (0–3) | 0.068 |
| Reduce Bolus (times) | 2 (0–4) | 1 (0–4) | 0.016 |
| Remifentanil | N/A | 0 (0–1) | N/A |
| Propofol | N/A | 0 (0–1) | N/A |
| Total consumption | |||
| Propofol (mg) | 437.0 ± 92.2 | 454.3 ± 87.6 | 0.380 |
| Remifentanil (µg) | 240.6 ± 71.9 | 228.5 ± 43.3 | 0.353 |
| Postoperative analgesics rescue | 12/42 | 14/42 | 0.814 |
| (n [%]) | (28.6%) | (33.3%) | |
| Patient satisfaction | 4 (3–5) | 4 (3–5) | 0.610 |
| PONV (n [%]) RIH (n [%]) | 0 (0%) 0 (0%) | 1 (2.4%) 0 (0%) | 1 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lai, H.-C.; Lai, M.-F.; Huang, Y.-H.; Yu, J.-C.; Tseng, W.-C.; Wu, Z.-F. Comparison of Single Target-Controlled Infusion Pump-Delivered Mixed Propofol and Remifentanil with Two Target-Controlled Infusion Pumps-Delivered Propofol and Remifentanil in Patients Undergoing Breast Cancer Surgery—A Prospective Study. Int. J. Environ. Res. Public Health 2023, 20, 2094. https://doi.org/10.3390/ijerph20032094
Lai H-C, Lai M-F, Huang Y-H, Yu J-C, Tseng W-C, Wu Z-F. Comparison of Single Target-Controlled Infusion Pump-Delivered Mixed Propofol and Remifentanil with Two Target-Controlled Infusion Pumps-Delivered Propofol and Remifentanil in Patients Undergoing Breast Cancer Surgery—A Prospective Study. International Journal of Environmental Research and Public Health. 2023; 20(3):2094. https://doi.org/10.3390/ijerph20032094
Chicago/Turabian StyleLai, Hou-Chuan, Meng-Fu Lai, Yi-Hsuan Huang, Jyh-Cherng Yu, Wei-Cheng Tseng, and Zhi-Fu Wu. 2023. "Comparison of Single Target-Controlled Infusion Pump-Delivered Mixed Propofol and Remifentanil with Two Target-Controlled Infusion Pumps-Delivered Propofol and Remifentanil in Patients Undergoing Breast Cancer Surgery—A Prospective Study" International Journal of Environmental Research and Public Health 20, no. 3: 2094. https://doi.org/10.3390/ijerph20032094
APA StyleLai, H.-C., Lai, M.-F., Huang, Y.-H., Yu, J.-C., Tseng, W.-C., & Wu, Z.-F. (2023). Comparison of Single Target-Controlled Infusion Pump-Delivered Mixed Propofol and Remifentanil with Two Target-Controlled Infusion Pumps-Delivered Propofol and Remifentanil in Patients Undergoing Breast Cancer Surgery—A Prospective Study. International Journal of Environmental Research and Public Health, 20(3), 2094. https://doi.org/10.3390/ijerph20032094







