Clinical and Forensic Aspects of the Management of Child Abuse: The Experience of the Paediatric Emergency Department in Novara, North-West Italy
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Approval
2.2. Setting
2.3. Data Collection
2.4. Statistical Analysis
3. Results
3.1. General Characteristics of Minors
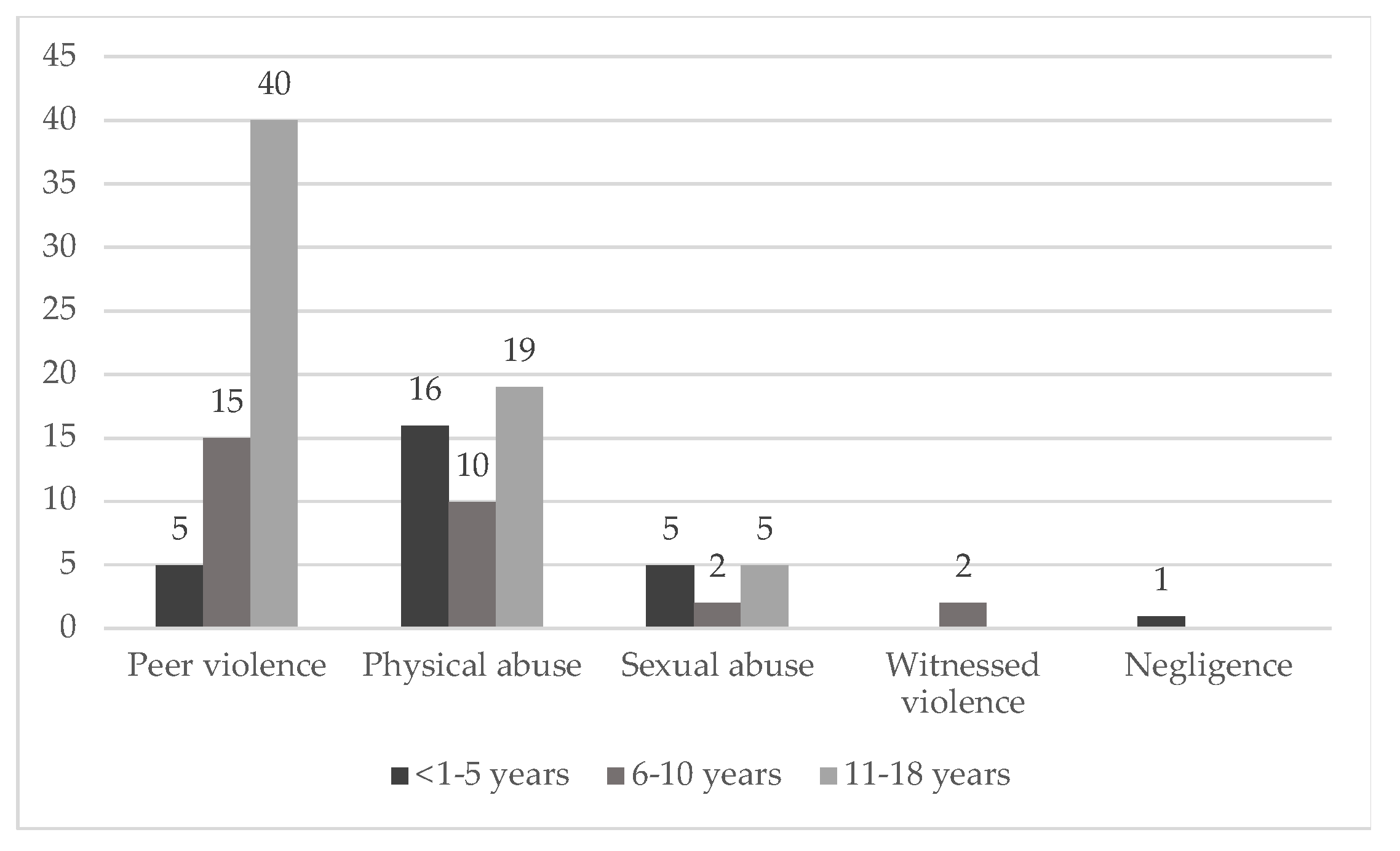
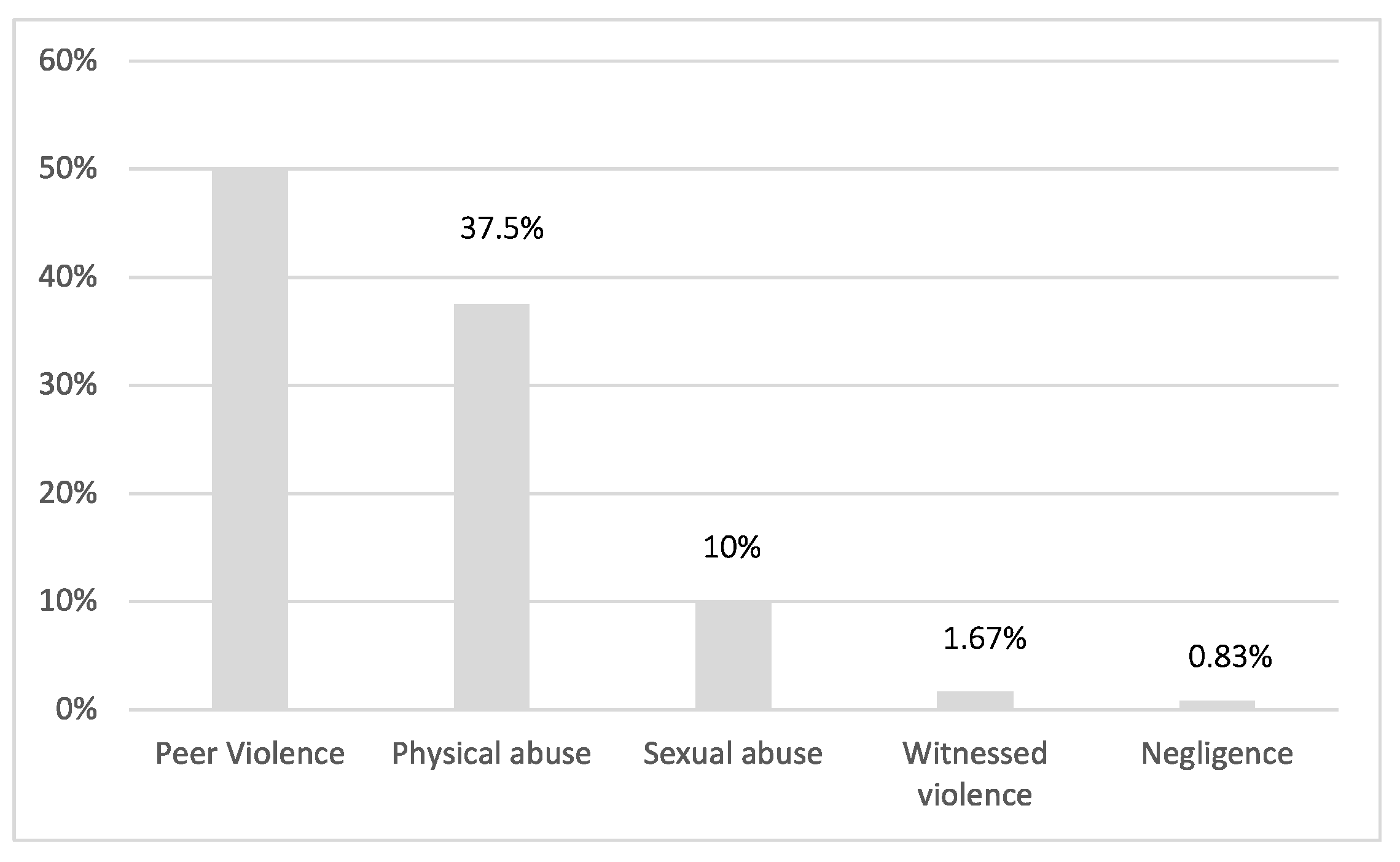
3.2. Types of Abuse
3.3. Maltreatment and Sexual Abuse in the Pre-COVID and COVID Period
3.4. Relationship between Victim and Aggressor
3.5. Injuries
3.6. Specialist Advice
3.7. Prognosis
3.8. Child Abuse and Legal Procedures Undertaken by Health Professionals
3.8.1. Art. 403 Italian Civil Code
3.8.2. Reporting to the Judicial Authorities
3.8.3. Distribution of Subject’s Characteristics According to the Event
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Consultation on Child Abuse Prevention (1999: Geneva, Switzerland), World Health Organization. Violence and Injury Prevention Team & Global Forum for Health Research. (1999). Report of the Consultation on Child Abuse Prevention, 29-31 March 1999, WHO, Geneva. World Health Organization. Available online: https://apps.who.int/iris/handle/10665/65900 (accessed on 30 September 2022).
- Demofonti, K. Informativa OMS: Maltrattamenti infantili. Ministero Della Salute, Traduzione Non Ufficiale. Available online: https://www.salute.gov.it/imgs/C_17_pagineAree_3664_listaFile_itemName_6_file.pdf (accessed on 30 September 2022).
- Gruppo di Lavoro, S.I.N.P.I.A. Sugli Abusi in Età Evolutiva. Linee Guida in Tema di Abuso sui Minori. Revisione Approvata in CD SINPIA il 15 Febbraio. 2007. Available online: https://www.sinpia.eu/wp-content/uploads/2019/02/2007_1.pdf (accessed on 30 September 2022).
- Montecchi, F. Gli Abusi All’infanzia-Dalla Ricerca All’intervento Clinico; Carocci: Roma, Italy, 1994. [Google Scholar]
- Cismai. Requisiti Minimi Degli Interventi nei casi di Violenza Assistita da Maltrattamento Sulle Madri. 2017. Available online: https://cismai.it/wp-content/uploads/2017/05/Opuscolo_ViolenzaAssistita_Bassa.pdf (accessed on 30 September 2022).
- Espelage, D.L.; Holt, M.K. Suicidal ideation and school bullying experiences after controlling for depression and delinquency. J. Adolesc. Health 2013, 53 (Suppl. 1), S27–S31. [Google Scholar] [CrossRef] [PubMed]
- Borowsky, I.W.; Taliaferro, L.A.; McMorris, B.J. Suicidal thinking and behavior among youth involved in verbal and social bullying: Risk and protective factors. J. Adolesc. Health 2013, 53 (Suppl. 1), S4–S12. [Google Scholar] [CrossRef] [PubMed]
- WHO. Child Maltreatment, Violence info. Available online: apps.who.int/violence-info/child-maltreatment/ (accessed on 30 September 2022).
- Progetto Revamp. Riconoscere, Accogliere e Accompagnare le Persone Vittime di Violenza Relazionale. Guida Per Gli Operatori di Pronto Soccorso. 2017. Available online: http://www.sossanita.it/doc/2017_11_violenza-guida-report_progetto-revamp.pdf (accessed on 30 September 2022).
- Palazzi, S.; de Girolamo, G.; Liverani, T. Observational study of suspected maltreatment in Italian paediatric emergency departments. Arch. Dis. Child. 2005, 90, 406–410. [Google Scholar] [CrossRef] [PubMed]
- Jackson, A.M.; Deye, K. Aspects of Abuse: Consequences of Childhood Victimization. Curr. Probl. Pediatr. Adolesc. Health Care 2015, 45, 86–93. [Google Scholar] [CrossRef] [PubMed]
- des Hommes, T. La condizione delle bambine e delle ragazze nel mondo. Indifesa 2021, 86–87. Available online: https://www.uil.it/documents/Dossier-indifesa-tdh-2021_BAMBINE_.pdf (accessed on 30 September 2022).
- Sanford, E.L.; Zagory, J.; Blackwell, J.M.; Szmuk, P.; Ryan, R.; Ambardekar, A. Changes in pediatric trauma during COVID-19 stay-at-home epoch at a tertiary pediatric hospital. J. Pediatr. Surg. 2021, 56, 918–922. [Google Scholar] [CrossRef] [PubMed]
- Scaramuzza, A.; Tagliaferri, F.; Bonetti, L.; Soliani, M.; Morotti, F.; Bellone, S.; Cavalli, C.; Rabbone, I. Changing admission patterns in paediatric emergency departments during the COVID-19 pandemic. Arch. Dis. Child. 2020, 105, 704–706. [Google Scholar] [CrossRef]
- Offidani, C.; Villani, A.; Reale, A.; Marchili, M.R.; Aufiero, L.R.; Moras, P.; Lodise, M.; Raucci, U.; Barbieri, M.A.; Raponi, M. Early recognition of child abuse through screening indicators at the emergency department: Experience of a tertiary urban pediatric hospital. Ital. J. Pediatr. 2022, 48, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Teeuw, A.H.; Kraan, R.B.J.; van Rijn, R.R.; Bossuyt, P.M.M.; Heymans, H.S.A. Screening for child abuse using a checklist and physical examinations in the emergency department led to the detection of more cases. Acta Paediatr. 2019, 108, 300–313. [Google Scholar] [CrossRef]
- Louwers, E.C.; Korfage, I.J.; Affourtit, M.J.; Ruige, M.; van den Elzen, A.P.; de Koning, H.J.; Moll, H.A. Accuracy of a screening instrument to identify potential child abuse in emergency departments. Child Abus. Negl. 2014, 38, 1275–1281. [Google Scholar] [CrossRef]
- ISTAT. Indagine Conoscitiva Sulle Forme di Violenza Fra I Minori E ai Danni di Bambini E Adolescenti. 2020. Available online: https://www.istat.it/it/archivio/243969 (accessed on 30 September 2022).
- Kee, D.M.H.; Al-Anesi, M.A.L.; Al-Anesi, S.A.L. Cyberbullying on social media under the influence of COVID-19. Glob. Bus. Organ. Excell. 2022, 41, 11–22. [Google Scholar] [CrossRef]
- Caron, F.; Plancq, M.C.; Tourneux, P.; Gouron, R.; Klein, C. Was child abuse underdetected during the COVID-19 lockdown? Arch Pediatr. 2020, 27, 399–400. [Google Scholar] [CrossRef] [PubMed]
- Caron, F.; Tourneux, P.; Tchidjou, H.K.; Taleb, A.; Gouron, R.; Panuel, M.; Klein, C. Incidence of child abuse with subdural hemorrhage during the first year of the COVID-19 pandemic: A nationwide study in France. Eur. J. Pediatr. 2022, 181, 2433–2438. [Google Scholar] [CrossRef] [PubMed]
- Chong, S.-L.; Soo, J.S.L.; Allen, J.C.J.; Ganapathy, S.; Lee, K.P.; Tyebally, A.; Yung, C.F.; Thoon, K.C.; Ng, Y.H.; Oh, J.Y.; et al. Impact of COVID-19 on pediatric emergencies and hospitalizations in Singapore. BMC Pediatr. 2020, 20, 562. [Google Scholar] [CrossRef]
- Kovler, M.L.; Ziegfeld, S.; Ryan, L.M.; Goldstein, M.A.; Gardner, R.; Garcia, A.V.; Nasr, I.W. Increased proportion of physical child abuse injuries at a level I pediatric trauma center during the COVID-19 pandemic. Child Abus. Negl. 2021, 116, 104756. [Google Scholar] [CrossRef]
- Lawson, M.; Piel, M.H.; Simon, M. Child Maltreatment during the COVID-19 Pandemic: Consequences of Parental Job Loss on Psychological and Physical Abuse Towards Children. Child Abus. Negl. 2020, 110, 104709. [Google Scholar] [CrossRef]
- Sidpra, J.; Abomeli, D.; Hameed, B.; Baker, J.; Mankad, K. Rise in the incidence of abusive head trauma during the COVID-19 pandemic. Arch. Dis. Child. 2021, 106, e14. [Google Scholar] [CrossRef]
- Rapoport, E.; Reisert, H.; Schoeman, E.; Adesman, A. Reporting of child maltreatment during the SARS-CoV-2 pandemic in New York City from March to May 2020. Child Abus. Negl. 2020, 116, 104719. [Google Scholar] [CrossRef]
- Kaiser, S.V.; Kornblith, A.E.; Richardson, T.; Pantell, M.S.; Fleegler, E.W.; Fritz, C.Q.; Parikh, K.; Zagel, A.; Sills, M.R.; Souza, H.G.; et al. Emergency Visits and Hospitalizations for Child Abuse During the COVID-19 Pandemic. Pediatrics 2021, 147, e2020038489. [Google Scholar] [CrossRef]
- Wongcharoenwatana, J.; Tarugsa, J.; Kaewpornsawan, K.; Eamsobhana, P.; Chotigavanichaya, C.; Ariyawatkul, T. Identifying children at high risk for recurrence child abuse. J. Orthop. Surg. 2021, 29, 2309499021996411. [Google Scholar] [CrossRef]
- Solís-García, G.; Marañón, R.; Medina Muñoz, M.; de Lucas Volle, S.; García-Morín, M.; Rivas García, A. Child abuse in the Emergency department: Epidemiology, management, and follow-up. An. De Pediatría 2019, 91, 37–41. [Google Scholar] [CrossRef] [PubMed]
- Ermertcan, A.T.; Ertan, P. Skin manifestations of child abuse. Indian J. Dermatol. Venereol. Leprol. 2010, 76, 317–326. [Google Scholar] [CrossRef] [PubMed]
- Gino, S.; Bo, M.; Ricciardelli, R.; Alù, M.; Boschi, I.; Carnevali, E.; Fabbri, M.; Fattorini, P.; Piccinini, A.; Previderè, C.; et al. Evaluation of critical aspects in clinical and forensic management of sexual violence: A multicentre Ge.F.I. project. Forensic Sci. Int. 2020, 314, 110387. [Google Scholar] [CrossRef]
- Golan, A.; Dishi-Galitzky, M.; Barda, J.; Lurie, S. The care of sexual assault victims: The first regional center in Israel—10 years experience. Isr. Med. Assoc. J. IMAJ 2012, 14, 658–661. [Google Scholar] [PubMed]
- Hwa, H.L.; Chen, S.C.; Wu, M.Z.; Shun, C.T.; Liu, S.K.; Lee, J.C.; Chen, Y.C. Analysis of cases of sexual assault presenting at a medical center in Taipei. Taiwan. J. Obstet. Gynecol. 2010, 49, 165–169. [Google Scholar] [CrossRef] [PubMed]
- Karanfil, R.; Keten, A.; Zeren, C.; Arslan, M.M.; Eren, A. Evaluation of sexual assaults in Turkey. J. Forensic Leg. Med. 2013, 20, 404–407. [Google Scholar] [CrossRef]
- Politi, C.; Gabbin, A.; D’angiolella, G.; Sanavio, M.; Gino, S. The importance of a specific medical-legal training for health care professionals in the management of sexual assault victims. J. Integr. Omics 2020, 10, 15–18. [Google Scholar] [CrossRef]
- Tozzo, P.; Politi, C.; Gabbin, A.; Gino, S.; Caenazzo, L. Improving assistance to elderly victims of violence: Healthcare personnel as a window for opportunity. Acta Med. Mediterr. 2021, 37, 783–790. [Google Scholar]
- Giolito, M.R.; Gruppo di Lavoro per l’abuso e il Maltrattamento dell’infanzia. L’abuso Sessuale nei Bambini Prepuberi. Requisiti E Raccomandazioni per Una Valutazione Appropriata, Il Pensiero Scientifico Editore, Roma. 2010. Available online: https://www.salute.gov.it/portale/donna/dettaglioPubblicazioniDonna.jsp?lingua=italiano&id=1522 (accessed on 13 January 2023).
- D.P.C.M. 24.11.2017 Linee Guida Nazionali Soccorso E Assistenza Socio-Sanitaria alle Donne Vittime di Violenza, Gazzetta Ufficiale–Serie Generale n. 24 del 30 Gennaio. 2018. Available online: http://www.gazzettaufficiale.it/eli/id/2018/01/30/18A00520/SG (accessed on 13 January 2023).
- Donati, F.; Costici, P.F.; De Salvatore, S.; Burrofato, A.; Micciulli, E.; Maiese, A.; Santoro, P.; La Russa, R. A Perspective on Management of Limb Fractures in Obese Children: Is It Time for Dedicated Guidelines? Front. Pediatr. 2020, 8, 207. [Google Scholar] [CrossRef]
- Maiese, A.; Iannaccone, F.; Scatena, A.; Del Fante, Z.; Oliva, A.; Frati, P.; Fineschi, V. Pediatric Abusive Head Trauma: A Systematic Review. Diagnostics 2021, 11, 734. [Google Scholar] [CrossRef]
- Blandino, A.; Maggioni, L.; Chiaffarino, F.; Parazzini, F.; Capano, D.; Florio, E.M.; Margherita, M.; Bertelle, G.M.; Franceschetti, L.; Amadasi, A.; et al. Sexual assault and abuse committed against family members: An analysis of 1342 legal outcomes and their motivations. PLoS ONE 2021, 29, e0253980. [Google Scholar] [CrossRef] [PubMed]


| N = 120 | |
|---|---|
| Variable | N (%) |
| Sex | |
| F | 54 (45.00) |
| M | 66 (55.00) |
| Age, mean (SD) | 9.92 (4.54) |
| Time period | |
| COVID | 58 (48.33) |
| Pre-COVID | 62 (51.67) |
| Year | |
| 2017 | 18 (15.00) |
| 2018 | 20 (16.67) |
| 2019 | 24 (20.00) |
| 2020 | 22 (18.33) |
| 2021 | 36 (30.00) |
| Origin | |
| Italian | 90 (75.00) |
| Foreign | 30 (25.00) |
| Type of abuse | |
| Physical abuse | 45 (37.50) |
| Sexual abuse | 12 (10.00) |
| Negligence | 1 (0.83) |
| Witnessed violence | 2 (1.67) |
| Peer violence | 60 (50.00) |
| Abuser | |
| Peer | 37 (30.84) |
| Relative | 28 (23.33) |
| Adult (not relative) | 19 (15.83) |
| Not reported | 14 (11.67) |
| Group violence | 22 (18.33) |
| Reported use of objects in abuse | |
| No | 105 (87.50) |
| Yes | 15 (12.50) |
| Physical or mental deficit | |
| No | 118 (98.33) |
| Yes | 2 (1.67) |
| Child protection services (403 Activation) | |
| No | 119 (99.17) |
| Yes | 1 (0.83) |
| Report to the judicial authority | |
| No | 46 (38.33) |
| Yes | 74 (61.67) |
| Forensic advice sought | |
| No | 103 (85.83) |
| Yes | 17 (14.17) |
| Presence of injuries | |
| No | 27 (22.5) |
| Yes | 93 (77.5) |
| Need for hospital admission | |
| No | 111 (92.50) |
| Yes | 7 (5.83) |
| Missing | 2 (1.67) |
| Prognosis (days) median, Q1–Q3 | 2 (0–3) |
| Report to the Judicial Authority | Presence of Injuries | Forensic Advice | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No N = 46 | Yes N = 74 | p-Value | pRR (95% CI) | No N = 27 | Yes N = 93 | p-Value | pRR (95% CI) | No N = 103 | Yes N = 17 | p-Value | pRR (95% CI) | |
| Variable | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | ||||||
| Sex | ||||||||||||
| F | 20 (43.48) | 34 (45.95) | 0.7916 | 1 | 17 (62.96) | 37 (39.78) | 0.0331 | 1 | 42 (40.78) | 12 (70.59) | 0.0221 | 1 |
| M | 26 (56.52) | 40 (54.05) | 1.04 (0.78–1.38) | 10 (37.04) | 56 (60.22) | 0.81 (0.67–0.99) | 61 (59.22) | 5 (29.41) | 2.93 (1.10–7.81) | |||
| Age, mean (SD) | 9.24 (4.64) | 10.4 (4.45) | 0.1984 | 1.02 (0.99–1.06) | 8.81 (4.95) | 10.24 (4.39) | 0.1525 | 1.02 (0.99–1.04) | 10.11 (4.89) | 8.76 (4.79) | 0.2602 | 0.95 (0.87–1.04) |
| Time period | ||||||||||||
| COVID | 22 (47.83) | 36 (48.65) | 0.9301 | 1 | 14 (51.85) | 44 (47.31) | 0.6777 | 1 | 47 (45.63) | 11 (64.71) | 0.1448 | 1 |
| Pre-COVID | 24 (52.17) | 38 (51.35) | 1.01 (0.76–1.34) | 13 (48.15) | 49 (52.69) | 0.96 (0.79–1.17) | 56 (54.37) | 6 (35.29) | 1.96 (0.78–4.96) | |||
| Year | ||||||||||||
| 2017 | 10 (21.74) | 8 (10.81) | 0.4534 | 1 | 6 (22.22) | 12 (12.9) | 0.4799 * | 1 | 14 (13.59) | 4 (23.53) | 0.3524 § | 1§ |
| 2018 | 6 (13.04) | 14 (18.92) | 1.58 (0.87–2.84) | 3 (11.11) | 17 (18.28) | 1.28 (0.88–1.86) | 18 (17.48) | 2 (11.76) | 0.45 (0.09–2.17) | |||
| 2019 | 8 (17.39) | 16 (21.62) | 1.50 (0.83–2.70) | 4 (14.81) | 20 (21.51) | 1.25 (0.86–1.81) | 24 (23.3) | 0 (0.00) | Not estimable | |||
| 2020 | 7 (15.22) | 15 (20.27) | 1.53 (0.85–2.77) | 7 (25.93) | 15 (16.13) | 1.02 (0.66–1.58) | 20 (19.42) | 2 (11.76) | 0.41 (0.08–1.98) | |||
| 2021 | 15 (32.61) | 21 (28.38) | 1.31 (0.73–2.36) | 7 (25.93) | 29 (31.18) | 1.21 (0.84–1.74) | 27 (26.21) | 9 (52.94) | 1.13 (0.40–3.16) | |||
| Origin | ||||||||||||
| Italian | 35 (76.09) | 55 (74.32) | 0.8284 | 1 | 19 (70.37) | 71 (76.34) | 0.528 | 1 | 80 (77.67) | 10 (58.82) | 0.1291* | 1 |
| Foreign | 11 (23.91) | 19 (25.68) | 1.04 (0.75–1.43) | 8 (29.63) | 22 (23.66) | 0.93(0.73–1.18) | 23 (22.33) | 7 (41.18) | 2.10 (0.88–5.03) | |||
| Type of abuse | ||||||||||||
| Physical abuse | 11 (25.58) | 34 (45.95) | 0.0286 | 1 | 7 (29.17) | 38 (40.86) | 0.0028 | 1 | 37 (37) | 8 (47.06) | <0.0001 | 1 |
| Sexual abuse | 3 (6.98) | 9 (12.16) | 0.99 (0.69–1.43) | 7 (29.17) | 5 (5.38) | 0.49(0.25–0.98) | 4 (4) | 8 (47.06) | 3.75 (1.78–7.90) | |||
| Peer violence | 29 (67.44) | 31 (41.89) | 0.68 (0.51–0.92) | 10 (41.67) | 50 (53.76) | 0.99 (0.83–1.17) | 59 (59) | 1 (5.88) | 0.09 (0.01–0.72) | |||
| Relationship between victim and aggressor | ||||||||||||
| Peer | 25 (54.35) | 12 (16.22) | 0.0002 | 1 | 3 (11.11) | 34 (36.56) | 0.0114 * | 1 | 35 (33.98) | 2 (11.76) | 0.0005 § | 1 § |
| Relative | 7 (15.22) | 21 (28.38) | 2.31 (1.39–3.86) | 4 (14.81) | 24 (25.81) | 0.93 (0.78–1.12) | 20 (19.42) | 8 (47.06) | 5.29 (1.22–22.98) | |||
| Adult (not relative) | 4 (8.7) | 15 (20.27) | 2.43 (1.45–4.09) | 8 (29.63) | 11 (11.83) | 0.63 (0.42–0.94) | 13 (12.62) | 6 (35.29) | 5.84 (1.30–26.23) | |||
| Not reported | 6 (13.04) | 8 (10.81) | 1.76 (0.92–3.37) | 5 (18.52) | 9 (9.68) | 0.70 (0.47–1.05) | 14 (13.59) | 0 (0.00) | Not estimable | |||
| Group violence | 4 (8.7) | 18 (24.32) | 2.52 (1.52–4.18) | 7 (25.93) | 15 (16.13) | 0.74 (0.55–1.00) | 21 (20.39) | 1 (5.88) | 0.84 (0.08–8.75) | |||
| Use of objects | ||||||||||||
| No | 39 (84.78) | 66 (89.19) | 0.4779 | 1 | 90 (87.38) | 15 (88.24) | 1.0000 * | 1 | ||||
| Yes | 7 (15.22) | 8 (10.81) | 0.85 (0.52–1.39) | 13 (12.62) | 2 (11.76) | 0.93 (0.24–3.68) | ||||||
| Prognosis (days) median, Q1–Q3 | 0.5 (0–2) | 3 (0–4) | 0.0013^ | 1.06 (1.01–1.11) | 0 (0–3) | 2 (0–3) | 0.0238^ | 1.02 (0.98–1.07) | 2 (0–3) | 2 (0–3) | 0.9168 ^ | 0.98 (0.84–1.15) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Puppi, M.; Rota, L.; Scotti, L.; Rabbone, I.; Gino, S. Clinical and Forensic Aspects of the Management of Child Abuse: The Experience of the Paediatric Emergency Department in Novara, North-West Italy. Int. J. Environ. Res. Public Health 2023, 20, 2028. https://doi.org/10.3390/ijerph20032028
Puppi M, Rota L, Scotti L, Rabbone I, Gino S. Clinical and Forensic Aspects of the Management of Child Abuse: The Experience of the Paediatric Emergency Department in Novara, North-West Italy. International Journal of Environmental Research and Public Health. 2023; 20(3):2028. https://doi.org/10.3390/ijerph20032028
Chicago/Turabian StylePuppi, Micol, Linda Rota, Lorenza Scotti, Ivana Rabbone, and Sarah Gino. 2023. "Clinical and Forensic Aspects of the Management of Child Abuse: The Experience of the Paediatric Emergency Department in Novara, North-West Italy" International Journal of Environmental Research and Public Health 20, no. 3: 2028. https://doi.org/10.3390/ijerph20032028
APA StylePuppi, M., Rota, L., Scotti, L., Rabbone, I., & Gino, S. (2023). Clinical and Forensic Aspects of the Management of Child Abuse: The Experience of the Paediatric Emergency Department in Novara, North-West Italy. International Journal of Environmental Research and Public Health, 20(3), 2028. https://doi.org/10.3390/ijerph20032028






