Cancer Care Team’s Management of Clinical Alerts Generated by Electronically Collected Patient Reported Outcomes: We Could Do Better
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
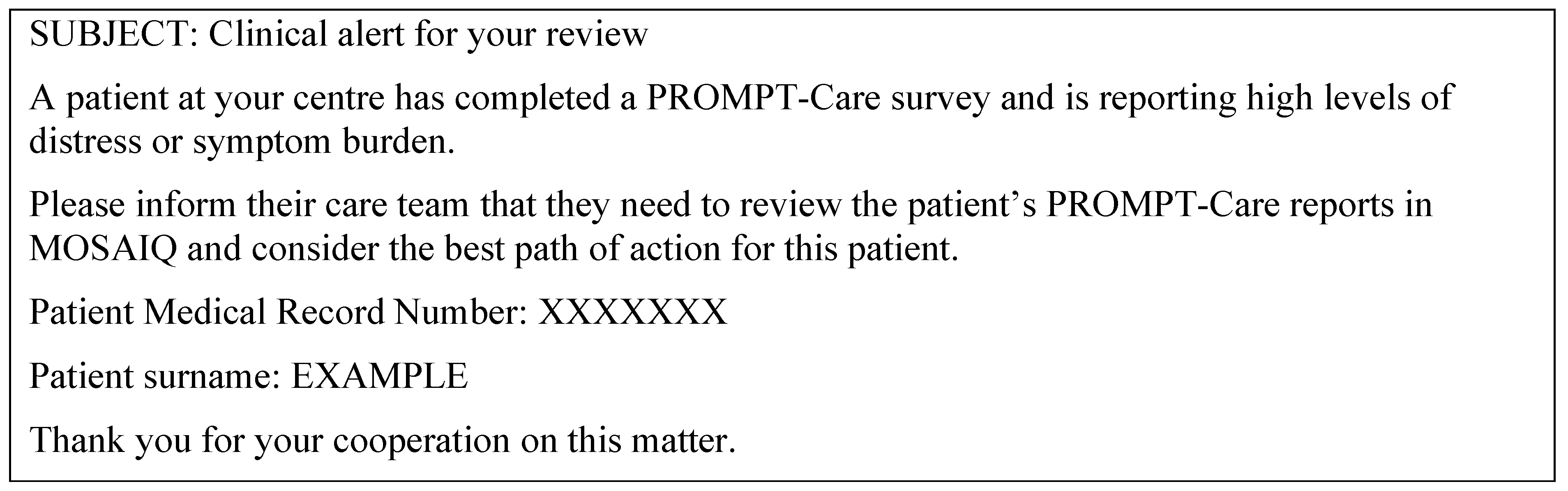
2.2. The PROMPT-Care 2.0 Intervention–Clinical Alerts
2.3. Procedures
2.4. Outcome Measures
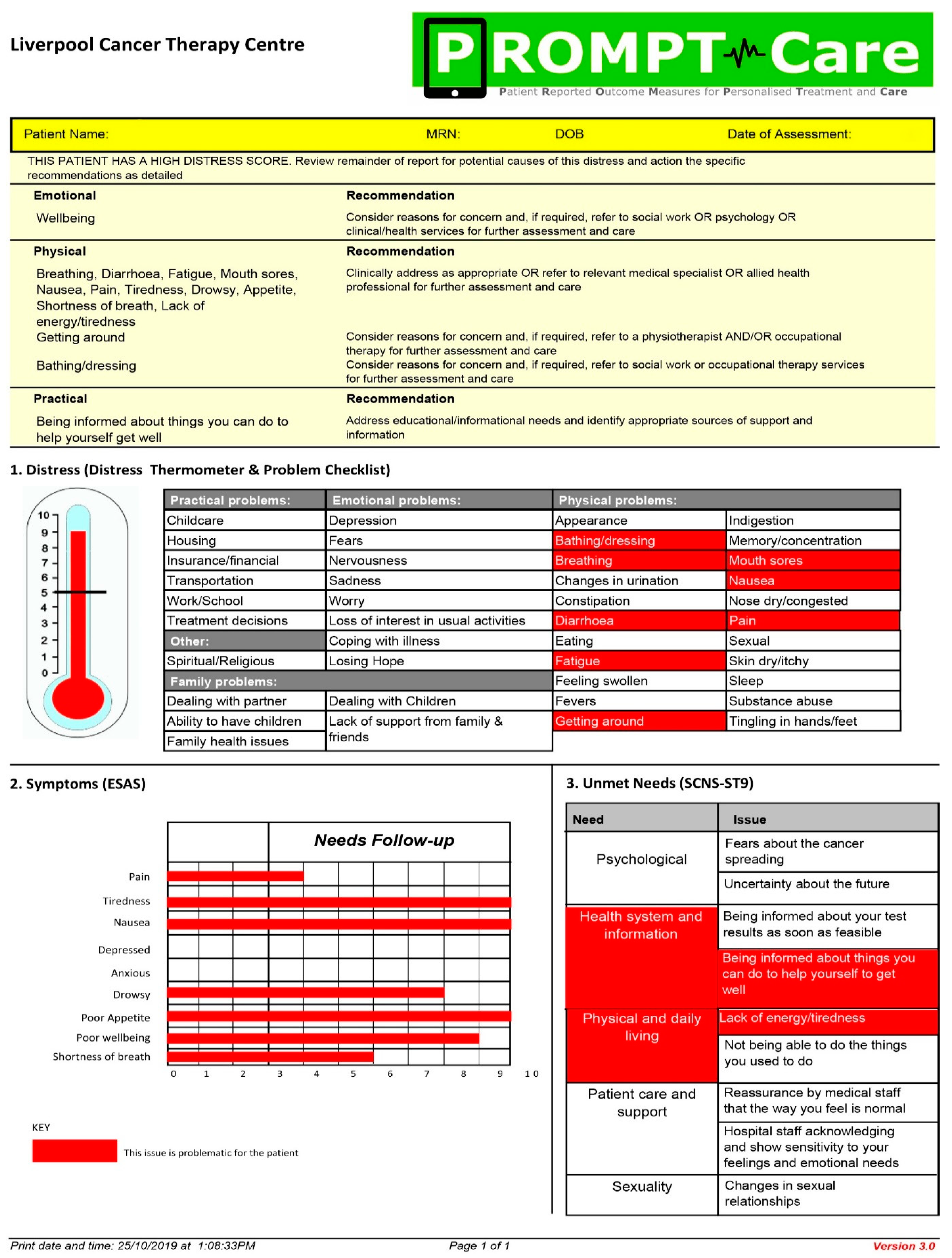
2.4.1. Clinical Alert Activity and Cancer Care Team Response
2.4.2. Patient Perceptions of the CCT Responses
2.5. Analysis
3. Results
3.1. Participant Characteristics
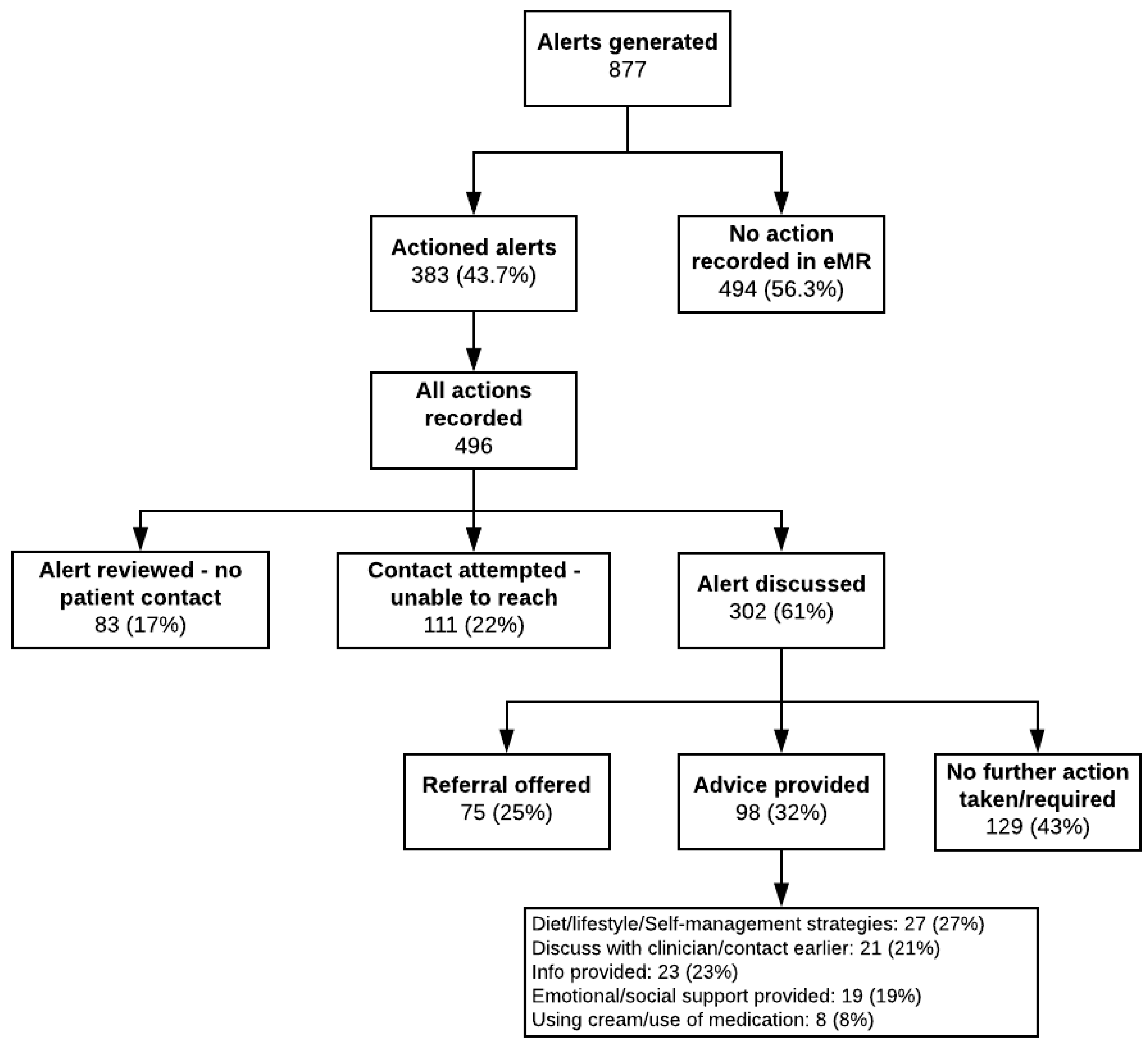
3.2. Clinical Alert Activity and Response
3.2.1. Clinical Alerts and Breached Items
3.2.2. Cancer Care Team Responses to Clinical Alerts
3.2.3. Participant Evaluation Surveys
3.3. Qualitative Findings
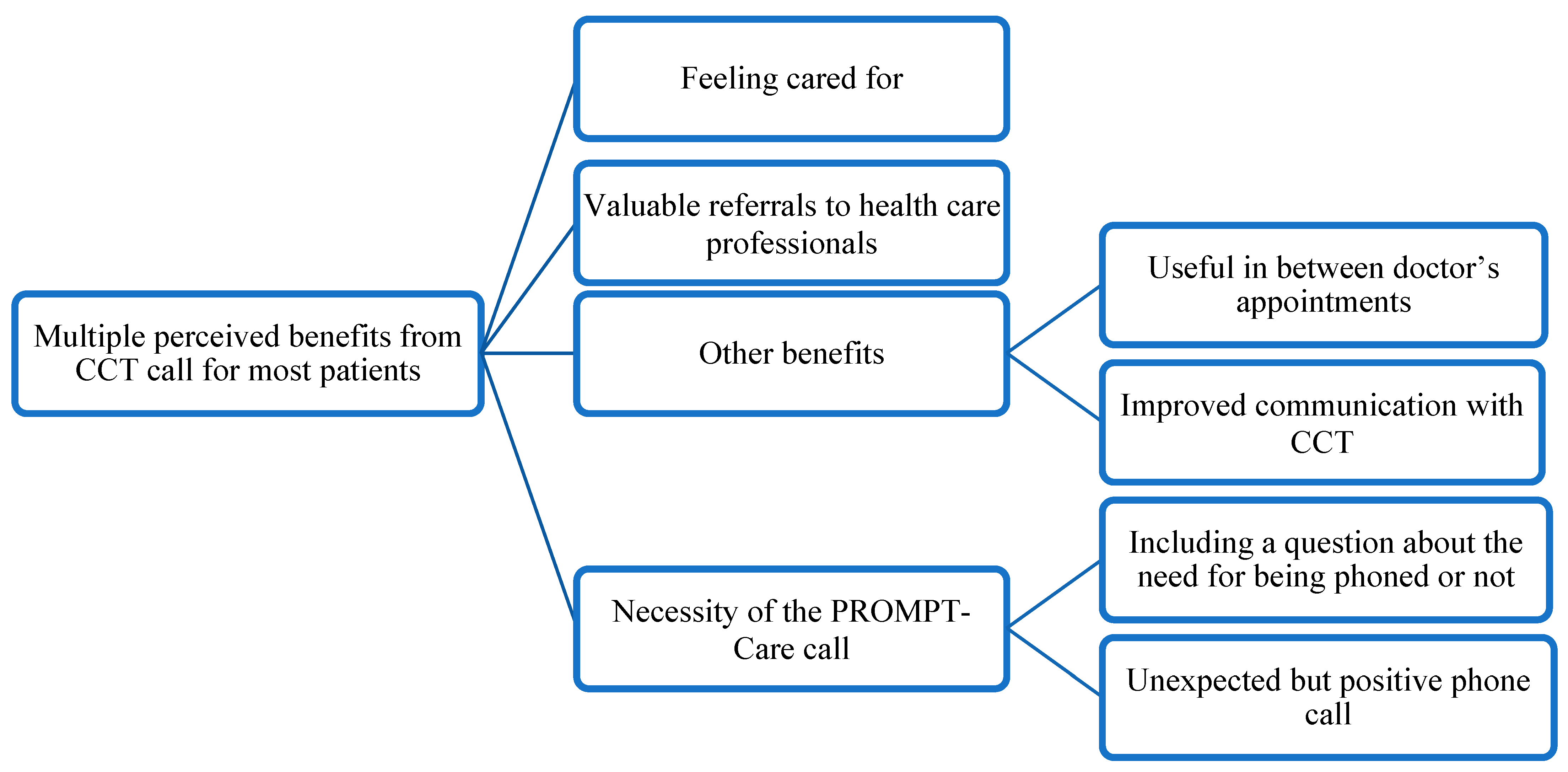
3.3.1. Overarching Theme: Multiple Perceived Benefits from the Cancer Care Team Call for Most Patients
I suppose there are so many people like me in the hospital system. It’s like you do feel you become a number. It just made me feel important, like I mattered, my treatment mattered, and care mattered… not just paperwork and then filed. There was an actual result from someone rang me up and quite quickly actually. I was very impressed with that. I think it is important that people think that their treatment—it’s not just a number. They’re treating people not just numbers.(L136)
3.3.2. Main Themes
- Feeling cared for
- Valuable referrals to HCPs
- Other benefits
- Necessity of the PROMPT-Care phone call
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
Appendix B
‘I think it’s really good because I think it [receiving a call after completing the survey] gives you a bit of confidence that there are people there who cared about your wellbeing, they’re checking up on you between the doctor’s visits and you might have an issue that they either say, “Well, look, I’ve got a bit of bone pain,” or something like that, so they’ll say, “Oh, okay,” and then investigate it a bit more and get a bit of feedback, take it in and pass onto the doctor for your next visit. So, I think anything with PROMPT-Care is good. I can’t say enough about it. It benefits me and it benefits a lot of other people and it’s a good system.’(M064)
‘…it’s just like genuine care [the phone call]. They’re genuine, and I don’t know if it’s because it’s cancer or what, but you don’t seem to get that with other problems… they take the time out to ring and check up on you. …… I just really appreciated it.’(M123)
‘…you really need to feel that someone is checking on you, and I felt that through the survey. I knew that I had that and that it was coming regularly.’(L082)
‘I know someone would ring me. When I filled out the surveys, someone was going to ring me and discuss it with me, even if it was me not understanding and I think that’s really important because sometimes not everybody gets a chance to get to the doctor or look up on the internet which is probably more dangerous…’(L136)
‘So, the nurse calls me up and she asks me a few questions and I think, “Oh, okay, that’s nice.” They’re looking after me even when I’m far away… so it’s reassuring.’(M064)
‘If you’re very worried what’s happened to you, even though the way the treatment of your cancer is getting well but still you’re not convinced that it is going well, it’s good to have communication through this survey to reassure you of whatever your problem is.’(I020)
‘Well, to know that someone’s interested in my case, it’s an amazing factor, it alleviates some of the worry that I’ve had. I think it’s been very helpful that you get feedback from them.’(L140)
‘…I did have an issue there at one stage where everything was tasting wrong and I just didn’t have an appetite and this and that, and I noted down and [nurse name] rang me within a couple of days and she said, “Oh, do you want me to make an appointment with a dietician for you?” and I said “Yes, please.” So she did that, she made the appointment I went to go and see the dietician… and it was really good… So she [nurse who made the PROMPT-Care call] pointed me in the right direction…’(L037)
‘I was lucky that I actually did this PROMPT survey and that the [nurse] got on to it straightaway and got actions for me [referral to the Wellness Centre and acupuncture sessions]. Now, I’m really grateful for that.’(L082)
‘It was good that they saw that I indicated the depression was on the higher side and they gave me a referral to see a psychologist…’(L140)
- A.
- Useful in between doctor’s appointments
‘I think it’s very important [the phone call] because—it’s something about my experience but my problem is that I don’t have a regular GP to talk to all the time, and as I said sometimes when you go to see [your specialist], you feel stressed because you know he has a lot of patients to go through, and you don’t want to worry him down with all your problems and so on. I think it’s a very good way [survey and phone call] of patients that needed to get help and they could express what they’re feeling to the survey.’(I020)
‘So I think it’s good [the survey and phone call]. It’s kind of a doctor’s visit without actually going to the doctor. So they’re asking you the questions, they can see your state of mind and based how you’re feeling and if all is good, “Well, okay, fine. He’s okay.” … Like I say if I tick something and highlights something and say I’m between doctor’s visits, so they may ring up and say, “Well, look, you’ve ticked this, this hasn’t been ticked before. Is it a major concern or anything like that?” and you’ll say, “Well, look, it’s just a little niggly pain I’ve been getting that I didn’t have before,” or something like that. I think it’s good that maybe we can catch something early or it’s nothing to be concerned with…’(M064)
- B.
- Improved communication with CCT
‘So, knowing that there is a phone call for when you’re really feeling a bit low or something is wrong that you’re not—you can talk to someone who understands what you’re talking about because they’ve seen it and experienced a lot of other patients having the same things. Well, I think that’s important. So, yeah, it’s a good service.’(L094)
‘… it was just someone different to talk to that knew about what treatment you’d been through and your care afterwards, basically, and your wellbeing after your treatment.’(S012)
‘…a lot of times that I received that call, although I appreciated the call, I didn’t really need the call.’ I appreciate—definitely appreciated the call ‘cause I know that they’re watching, but to—I mean, even for them, I know ‘cause they’re really busy… but still in saying that I didn’t really need the call, it was nice that they did call because I know that they’re actually reading it.’(M108)
‘Interviewee: …when the results are two or three levels out of normal,—yes, that phone call is really appreciated and it matters… only for the ones that are really obviously out of normal range—are sicker than usual, more nausea, or really important issues—diarrhoea, constipation, vomiting, all those sorts of things. That’s the sort of thing where you need advice…’(M028)
- A.
- Including a question about the need for being phoned or not
‘I think it will be good because then you can indicate whether you want to be contacted or not, so I think it’s a good question… It would be useful, yeah.’(I020)
‘That probably would be helpful, but then again, as I said to you, sometimes you think that you’re just having a bad day, and it might be a little bit more than that ….. that’s my only concern.’(L013)
‘I think that would be a really good thing, just to say, “I would appreciate a phone call concerning this issue,” or, “There’s no need for a phone call at this time”.’(S018)
‘…if people say no and they really need to be contacted, then you’ve stopped that approach because people will say no when they really do need it, so I don’t know. Just say, “When would be a good time for people to contact you?” something like that, maybe, so that you’re not asking them to say no.’(M048)
- B.
- Unexpected but positive call
‘…it was actually a surprise for me when I was phoned the next day. It was a surprise and I was very grateful for that.’(L082)
‘I’m kind of amazed. The first time I got the call, I was a bit surprised that I got a call…’(L090)
‘…I was a bit surprised. I wasn’t expecting it and then I thought to myself, I was like, “Oh, that’s what that was from,” so I probably was a little bit taken back because I hadn’t initiated it, but in some ways, I thought it was good that someone was checking in on me as well.’(M048)
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Australian Institute of Health and Welfare. Cancer data in Australia. In Vol Cat. no: CAN 122; Australian Institute of Health and Welfare: Canberra, Australia, 2022. [Google Scholar]
- Australian Institute of Health and Welfare. Cancer in Australia 2021. In Vol Cat. no: CAN 144; Australian Institute of Health and Welfare: Canberra, Australia, 2021. [Google Scholar]
- International WCRF. Cancer Survival Statistics. 2022. Available online: https://www.wcrf.org/cancer-trends/cancer-survival-statistics/ (accessed on 15 November 2022).
- Australia CC. Cancer Side Effects. 2021. Available online: https://www.cancer.org.au/cancer-information/cancer-side-effects, (accessed on 7 November 2022).
- Stein, K.D.; Syrjala, K.L.; Andrykowski, M.A. Physical and psychological long-term and late effects of cancer. Cancer 2008, 112 (Suppl. S11), 2577–2592. [Google Scholar] [CrossRef] [PubMed]
- van Leeuwen, M.; Husson, O.; Alberti, P.; Arraras, J.I.; Chinot, O.L.; Costantini, A.; Darlington, A.-S.; Dirven, L.; Eichler, M.; Hammerlid, E.B.; et al. Understanding the quality of life (QOL) issues in survivors of cancer: Towards the development of an EORTC QOL cancer survivorship questionnaire. Health Qual Life Outcomes 2018, 16, 114. [Google Scholar] [CrossRef] [PubMed]
- Aapro, M.; Bossi, P.; Dasari, A.; Fallowfield, L.; Gascón, P.; Geller, M.; Jordan, K.; Kim, J.; Martin, K.; Porzig, S. Digital Health for Optimal Supportive Care in Oncology: Benefits, Limits, and Future Perspectives. Kompass Nutr. Diet. 2021, 1, 72–90. [Google Scholar] [CrossRef]
- LeBlanc, T.W.; Abernethy, A.P. Patient-reported outcomes in cancer care—Hearing the patient voice at greater volume. Nat. Rev. Clin. Oncol. 2017, 14, 763–772. [Google Scholar] [CrossRef] [PubMed]
- Nordan, L.; Blanchfield, L.; Niazi, S.; Sattar, J.; Coakes, C.E.; Uitti, R.; Vizzini, M.; Naessens, J.M.; Spaulding, A. Implementing electronic patient-reported outcomes measurements: Challenges and success factors. BMJ Qual. Saf. 2018, 27, 852–856. [Google Scholar] [CrossRef]
- Basch, E.; Deal, A.M.; Kris, M.G.; Scher, H.I.; Hudis, C.A.; Sabbatini, P.; Rogak, L.; Bennett, A.V.; Dueck, A.C.; Atkinson, T.M.; et al. Symptom Monitoring With Patient-Reported Outcomes During Routine Cancer Treatment: A Randomized Controlled Trial. J. Clin. Oncol. 2016, 34, 557–565. [Google Scholar] [CrossRef] [PubMed]
- Graupner, C.; Kimman, M.L.; Mul, S.; Slok, A.H.M.; Claessens, D.; Kleijnen, J.; Dirksen, C.D.; Breukink, S.O. Patient outcomes, patient experiences and process indicators associated with the routine use of patient-reported outcome measures (PROMs) in cancer care: A systematic review. Support. Care Cancer 2020, 29, 573–593. [Google Scholar] [CrossRef]
- Skovlund, P.C.; Ravn, S.; Seibaek, L.; Thaysen, H.V.; Lomborg, K.; Nielsen, B.K. The development of PROmunication: A training-tool for clinicians using patient-reported outcomes to promote patient-centred communication in clinical cancer settings. J. Patient-Rep. Outcomes 2020, 4, 1–11. [Google Scholar] [CrossRef]
- Chen, J.; Ou, L.; Hollis, S.J. A systematic review of the impact of routine collection of patient reported outcome measures on patients, providers and health organisations in an oncologic setting. BMC Health Serv. Res. 2013, 13, 211. [Google Scholar] [CrossRef]
- Basch, E.; Deal, A.M.; Dueck, A.C.; Scher, H.I.; Kris, M.G.; Hudis, C.; Schrag, D. Overall Survival Results of a Trial Assessing Patient-Reported Outcomes for Symptom Monitoring During Routine Cancer Treatment. JAMA 2017, 318, 197–198. [Google Scholar] [CrossRef] [PubMed]
- Girgis, A.; Durcinoska, I.; Arnold, A.; Descallar, J.; Kaadan, N.; Koh, E.-S.; Miller, A.; Ng, W.; Carolan, M.; Della-Fiorentina, S.A.; et al. Web-Based Patient-Reported Outcome Measures for Personalized Treatment and Care (PROMPT-Care): Multicenter Pragmatic Nonrandomized Trial. J. Med. Internet Res. 2020, 22, e19685. [Google Scholar] [CrossRef] [PubMed]
- Efficace, F.; Collins, G.S.; Cottone, F.; Giesinger, J.M.; Sommer, K.; Anota, A.; Schlussel, M.M.; Fazi, P.; Vignetti, M. Patient-Reported Outcomes as Independent Prognostic Factors for Survival in Oncology: Systematic Review and Meta-Analysis. Value Health 2021, 24, 250–267. [Google Scholar] [CrossRef] [PubMed]
- Calvert, M.; Kyte, D.; Price, G.; Valderas, J.M.; Hjollund, N.H. Maximising the impact of patient reported outcome assessment for patients and society. BMJ 2019, 364, k5267. [Google Scholar] [CrossRef] [PubMed]
- Foster, A.; Croot, L.; Brazier, J.; Harris, J.; O’Cathain, A. The facilitators and barriers to implementing patient reported outcome measures in organisations delivering health related services: A systematic review of reviews. J. Patient-Rep. Outcomes 2018, 2, 46. [Google Scholar] [CrossRef] [PubMed]
- Girgis, A.; Durcinoska, I.; Gerges, M.; Kaadan, N.; Arnold, A.; Descallar, J.; Delaney, G.P. Study protocol for a controlled trial of an eHealth system utilising patient reported outcome measures for personalised treatment and care: PROMPT-Care 2.0. BMC Cancer 2018, 18, 845. [Google Scholar] [CrossRef]
- Girgis, A.; Delaney, G.P.; Arnold, A.; Miller, A.A.; Levesque, J.V.; Kaadan, N.; Carolan, M.G.; Cook, N.; Masters, K.; Tran, T.T.; et al. Development and Feasibility Testing of PROMPT-Care, an eHealth System for Collection and Use of Patient-Reported Outcome Measures for Personalized Treatment and Care: A Study Protocol. JMIR Res. Protoc. 2016, 5, e227. [Google Scholar] [CrossRef]
- Bamgboje-Ayodele, A.; Durcinoska, I.; Rincones, O.; Wu, V.S.; Anthony, A.; Geoff, P.D.; Afaf, G. Supporting cancer patients to self-manage: Extent of use and perceptions of “trusted” online self-management resources. Patient Educ. Couns. 2022, 105, 2240–2247. [Google Scholar]
- New South Wales Government. South Western Sydney Local Health District Strategic Plan; District South Western Sydney Local Health District, Ed.; New South Wales Government: Liverpool, Australia, 2020. [Google Scholar]
- New South Wales Government. Strategic Direction for Illawarra Shoalhaven Local Health District: 2017–2020; District ISLH, Ed.; New South Wales Government: Illawarra, Australia, 2017. [Google Scholar]
- World Medical Association. World Medical Association Declaration of Helsinki. Ethical principles for medical research involving human subjects. Bull. World Health Organ. 2001, 79, 373. [Google Scholar]
- National Health and Medical Research Council. Australian Code for the Responsible Conduct of Research; National Health and Medical Research Council: Canberra, Australia, 2018. [Google Scholar]
- Riba, M.B.; Donovan, K.A.; Andersen, B.; Braun, I.; Breitbart, W.S.; Brewer, B.W.; Buchmann, L.O.; Clark, M.M.; Collins, M.; Corbett, C.; et al. Distress management, version 3.2019, NCCN clinical practice guidelines in oncology. J. Natl. Compr. Cancer Netw. 2019, 17, 1229–1249. [Google Scholar] [CrossRef]
- Richardson, L.; Jones, G. A review of the reliability and validity of the Edmonton Symptom Assessment System. Curr. Oncol. 2009, 16, 53–64. [Google Scholar] [CrossRef]
- Girgis, A.; Stojanovski, E.; Boyes, A.; King, M.; Lecathelinais, C. The next generation of the supportive care needs survey: A brief screening tool for administration in the clinical oncology setting. Psycho-Oncology 2011, 21, 827–835. [Google Scholar] [CrossRef]
- Girgis, A.; Durcinoska, I.; Koh, E.-S.; Ng, W.; Arnold, A.; Delaney, G.P.; PROMPT-Care Pathways Working Group. Development of Health Pathways to Standardize Cancer Care Pathways Informed by Patient-Reported Outcomes and Clinical Practice Guidelines. JCO Clin. Cancer Inform. 2018, 2, 1–13. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Yogananda, M.N.; Muthu, V.; Prasad, K.T.; Kohli, A.; Behera, D.; Singh, N. Utility of the revised Edmonton Symptom Assessment System (ESAS-r) and the Patient-Reported Functional Status (PRFS) in lung cancer patients. Support. Care Cancer 2018, 26, 767–775. [Google Scholar] [CrossRef] [PubMed]
- Absolom, K.; Warrington, L.; Hudson, E.; Hewison, J.; Morris, C.; Holch, P.; Carter, R.; Gibson, A.; Holmes, M.; Clayton, B.; et al. Phase III Randomized Controlled Trial of eRAPID: eHealth Intervention During Chemotherapy. J. Clin. Oncol. 2021, 39, 734–747. [Google Scholar] [CrossRef] [PubMed]
- Bhargava, R.; Keating, B.; Isenberg, S.R.; Subramaniam, S.; Wegier, P.; Chasen, M. RELIEF: A Digital Health Tool for the Remote Self-Reporting of Symptoms in Patients with Cancer to Address Palliative Care Needs and Minimize Emergency Department Visits. Curr. Oncol. 2021, 28, 4273–4280. [Google Scholar] [CrossRef]
- Bootsma, T.I.; Schellekens, M.P.; van Woezik, R.A.; Slatman, J.; van der Lee, M.L. Using smartphone-based ecological momentary assessment and personalized feedback for patients with chronic cancer-related fatigue: A proof-of-concept study. Internet Interv. 2022, 30, 100568. [Google Scholar] [CrossRef]
- Basch, E.; Stover, A.M.; Schrag, D.; Chung, A.; Jansen, J.; Henson, S.; Carr, P.; Ginos, B.; Deal, A.; Spears, P.A.; et al. Clinical Utility and User Perceptions of a Digital System for Electronic Patient-Reported Symptom Monitoring During Routine Cancer Care: Findings From the PRO-TECT Trial. JCO Clin. Cancer Inform. 2020, 4, 947–957. [Google Scholar] [CrossRef]
- Funk, R.; Cisneros, C.; Williams, R.C.; Kendall, J.; Hamann, H.A. What happens after distress screening? Patterns of supportive care service utilization among oncology patients identified through a systematic screening protocol. Support. Care Cancer 2016, 24, 2861–2868. [Google Scholar] [CrossRef]
- Dilworth, S.; Higgins, I.; Parker, V.; Kelly, B.; Turner, J. Patient and health professional’s perceived barriers to the delivery of psychosocial care to adults with cancer: A systematic review. Psycho-Oncology 2014, 23, 601–612. [Google Scholar] [CrossRef] [PubMed]
- Cohen, A.; Ianovski, L.E.; Frenkiel, S.; Hier, M.; Zeitouni, A.; Kost, K.; Mlynarek, A.; Richardson, K.; Black, M.; MacDonald, C.; et al. Barriers to psychosocial oncology service utilization in patients newly diagnosed with head and neck cancer. Psycho-Oncology 2018, 27, 2786–2793. [Google Scholar] [CrossRef] [PubMed]
- Holland, J.C.; Kelly, B.J.; Weinberger, M.I. Why psychosocial care is difficult to integrate into routine cancer care: Stigma is the elephant in the room. J. Natl. Compr. Cancer Netw. 2010, 8, 362–366. [Google Scholar] [CrossRef] [PubMed]
- O’Reilly, M.; Mellotte, G.; Ryan, B.; O’Connor, A. Gastrointestinal side effects of cancer treatments. Ther. Adv. Chronic Dis. 2020, 11, 2040622320970354. [Google Scholar] [CrossRef] [PubMed]
- Rock, C.L.; Thomson, C.; Gansler, T.; Gapstur, S.M.; McCullough, M.L.; Patel, A.V.; Bandrews, K.S.; Bandera, E.V.; Spees, C.K.; Robien, K.; et al. American Cancer Society guideline for diet and physical activity for cancer prevention. CA: A Cancer J. Clin. 2020, 70, 245–271. [Google Scholar] [CrossRef] [PubMed]
- Consolo, L.; Castellini, G.; Cilluffo, S.; Basile, I.; Lusignani, M. Electronic patient-reported outcomes (e-PROMs) in palliative cancer care: A scoping review. J. Patient-Rep. Outcomes 2022, 6, 102. [Google Scholar] [CrossRef]
- Basch, E.; Charlot, M.; Dueck, A.C. Population-level evidence of survival benefits of patient-reported outcome symptom monitoring software systems in routine cancer care. Cancer Med. 2020, 9, 7797–7799. [Google Scholar] [CrossRef]
- Rocque, G.B.; Dent, D.A.N.; Ingram, S.A.; Caston, N.E.; Thigpen, H.B.; Lalor, F.R.; Jamy, O.H.; Giri, S.; Azuero, A.; Pierce, J.Y.; et al. Adaptation of Remote Symptom Monitoring Using Electronic Patient-Reported Outcomes for Implementation in Real-World Settings. JCO Oncol. Pract. 2022, 18, e1943–e1952. [Google Scholar] [CrossRef]

| Characteristics | n (%) |
|---|---|
| Age (years), mean (range) | 62.4 (25–86) |
| Sex, n (%) | |
| Male | 133 (40.6) |
| Female | 195 (59.5) |
| Site of cancer | |
| Breast | 132 (40.2) |
| Prostate | 51 (15.6) |
| Colorectal | 37 (11.3) |
| Respiratory | 29 (8.8) |
| Gynaecological | 16 (4.9) |
| Upper gastrointestinal | 15 (4.6) |
| Skin | 11 (3.4) |
| Oral | 10 (3.1) |
| Other | 27 (8.2) |
| Stage of disease | |
| 0/I | 66 (22.1) |
| II | 90 (27.4) |
| III | 57 (17.4) |
| IV | 80 (24.4) |
| Missing | 35 (10.7) |
| Treatment status | |
| Active treatment b | 139 (42.4) |
| Follow-up care | 189 (57.6) |
| Socioeconomic status (IRSD) c | |
| 1 | 54 (16.4) |
| 2 | 97 (29.6) |
| 3 | 52 (15.9) |
| 4 | 35 (10.7) |
| 5 | 90 (27.4) |
| Relationship status a | |
| Single | 71 (23.1) |
| Partnered | 236 (76.9) |
| Education status a | |
| High school or less | 122 (39.7) |
| Post-secondary education | 185 (60.3) |
| Employment a | |
| Employed | 129 (42) |
| Retired | 155 (50.5) |
| Other | 23 (7.5) |
| Referral | Total Offered | Accepted |
|---|---|---|
| Clinical psychology | 55 | 18 (32.7) |
| Dietetics | 11 | 8 (72.7) |
| Social work | 9 | 2 (22.2) |
| Physiotherapy | 3 | 3 (100) |
| Prostate cancer nurse | 3 | 3 (100) |
| Medical oncology | 2 | 2 (100) |
| Unknown * | 3 | 0 |
| Total | 86 | 36 (41.9) |
| 3 Months | 6 Months | 9 Months | ||||
|---|---|---|---|---|---|---|
| (n = 221) | (n = 78) | (n = 93) | ||||
| n | % | n | % | n | % | |
| Do you recall receiving a phone call from the nursing team at your Cancer Care Centre in response to your PROMPT-Care assessments? | ||||||
| Yes | 72 | 32.6 | 21 | 26.9 | 26 | 28 |
| I found receiving a phone call from the nursing team at my Cancer Care Centre beneficial | ||||||
| Strongly Agree/Agree | 58 | 80.6 | 17 | 81.0 | 22 | 84.6 |
| Neutral | 12 | 16.7 | 3 | 14.3 | 3 | 11.5 |
| Strongly Disagree/Disagree | 2 | 2.8 | 1 | 4.8 | 1 | 3.8 |
| The phone call from the nursing team helped me deal with ongoing problems I was experiencing | ||||||
| Strongly Agree/Agree | 46 | 63.9 | 12 | 57.1 | 17 | 65.4 |
| Neutral | 22 | 30.6 | 7 | 33.3 | 8 | 30.8 |
| Strongly Disagree/Disagree | 4 | 5.6 | 2 | 9.5 | 1 | 3.8 |
| Contact with my Cancer Care Centre linked me back to appropriate support services to help with my problems (e.g., Dietitian, Psychologist) | ||||||
| Strongly Agree/Agree | 45 | 62.5 | 8 | 38.1 | 18 | 69.2 |
| Neutral | 22 | 30.6 | 9 | 42.9 | 7 | 26.9 |
| Strongly Disagree/Disagree | 5 | 6.9 | 3 | 14.3 | 1 | 3.8 |
| The nursing team provided me with enough information and support | ||||||
| Strongly Agree/Agree | 59 | 81.9 | 14 | 66.7 | 21.0 | 80.8 |
| Neutral | 12 | 16.7 | 6 | 28.6 | 4.0 | 15.4 |
| Strongly Disagree/Disagree | 1 | 1.4 | 1 | 4.8 | 1.0 | 3.8 |
| I would have preferred not to receive a phone call from the nursing team in response to my PROMPT-Care assessments | ||||||
| Strongly Agree/Agree | 6 | 8.3 | 1 | 4.8 | 2 | 7.7 |
| Neutral | 8 | 11.1 | 3 | 14.3 | 4 | 15.4 |
| Strongly Disagree/Disagree | 58 | 80.6 | 17 | 81 | 20 | 76.9 |
| I would have preferred to be able to contact the nursing team when I needed assistance | ||||||
| Strongly Agree/Agree | 26 | 36.1 | 7 | 33.3 | 5 | 19.2 |
| Neutral | 22 | 30.6 | 7 | 33.3 | 11 | 42.3 |
| Strongly Disagree/Disagree | 23 | 31.9 | 7 | 33.3 | 10 | 38.5 |
| I found receiving a phone call from the nursing team bothersome | ||||||
| Strongly Agree/Agree | 3 | 4.2 | 1 | 4.8 | 1 | 3.8 |
| Neutral | 8 | 11.1 | 1 | 4.8 | 2 | 7.7 |
| Strongly Disagree/Disagree | 61 | 84.7 | 19 | 90.5 | 23 | 88.5 |
| The phone call from the nursing team facilitated better communication with my Cancer Care Centre on how I was doing | ||||||
| Strongly Agree/Agree | 45 | 62.5 | 14 | 66.7 | 15 | 57.7 |
| Neutral | 20 | 27.8 | 5 | 23.8 | 11 | 42.3 |
| Strongly Disagree/Disagree | 5 | 6.9 | 2 | 9.5 | - | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rincones, O.; Bamgboje-Ayodele, A.; Arnold, A.; Delaney, G.P.; Durcinoska, I.; Avery, S.; Sandell, T.; Della-Fiorentina, S.A.; Pearson, J.; The PROMPT-Care Co-Authorship Group; et al. Cancer Care Team’s Management of Clinical Alerts Generated by Electronically Collected Patient Reported Outcomes: We Could Do Better. Int. J. Environ. Res. Public Health 2023, 20, 2001. https://doi.org/10.3390/ijerph20032001
Rincones O, Bamgboje-Ayodele A, Arnold A, Delaney GP, Durcinoska I, Avery S, Sandell T, Della-Fiorentina SA, Pearson J, The PROMPT-Care Co-Authorship Group, et al. Cancer Care Team’s Management of Clinical Alerts Generated by Electronically Collected Patient Reported Outcomes: We Could Do Better. International Journal of Environmental Research and Public Health. 2023; 20(3):2001. https://doi.org/10.3390/ijerph20032001
Chicago/Turabian StyleRincones, Orlando, Adeola Bamgboje-Ayodele, Anthony Arnold, Geoff P. Delaney, Ivana Durcinoska, Sandra Avery, Tiffany Sandell, Stephen A. Della-Fiorentina, Joanne Pearson, The PROMPT-Care Co-Authorship Group, and et al. 2023. "Cancer Care Team’s Management of Clinical Alerts Generated by Electronically Collected Patient Reported Outcomes: We Could Do Better" International Journal of Environmental Research and Public Health 20, no. 3: 2001. https://doi.org/10.3390/ijerph20032001
APA StyleRincones, O., Bamgboje-Ayodele, A., Arnold, A., Delaney, G. P., Durcinoska, I., Avery, S., Sandell, T., Della-Fiorentina, S. A., Pearson, J., The PROMPT-Care Co-Authorship Group, & Girgis, A. (2023). Cancer Care Team’s Management of Clinical Alerts Generated by Electronically Collected Patient Reported Outcomes: We Could Do Better. International Journal of Environmental Research and Public Health, 20(3), 2001. https://doi.org/10.3390/ijerph20032001






