“Faith Is Not Enough?” Ego-Resiliency and Religiosity as Coping Resources with Pandemic Stress—Mediation Study
Abstract
1. Introduction
2. Methods
2.1. Participants
2.2. Measures and Procedures
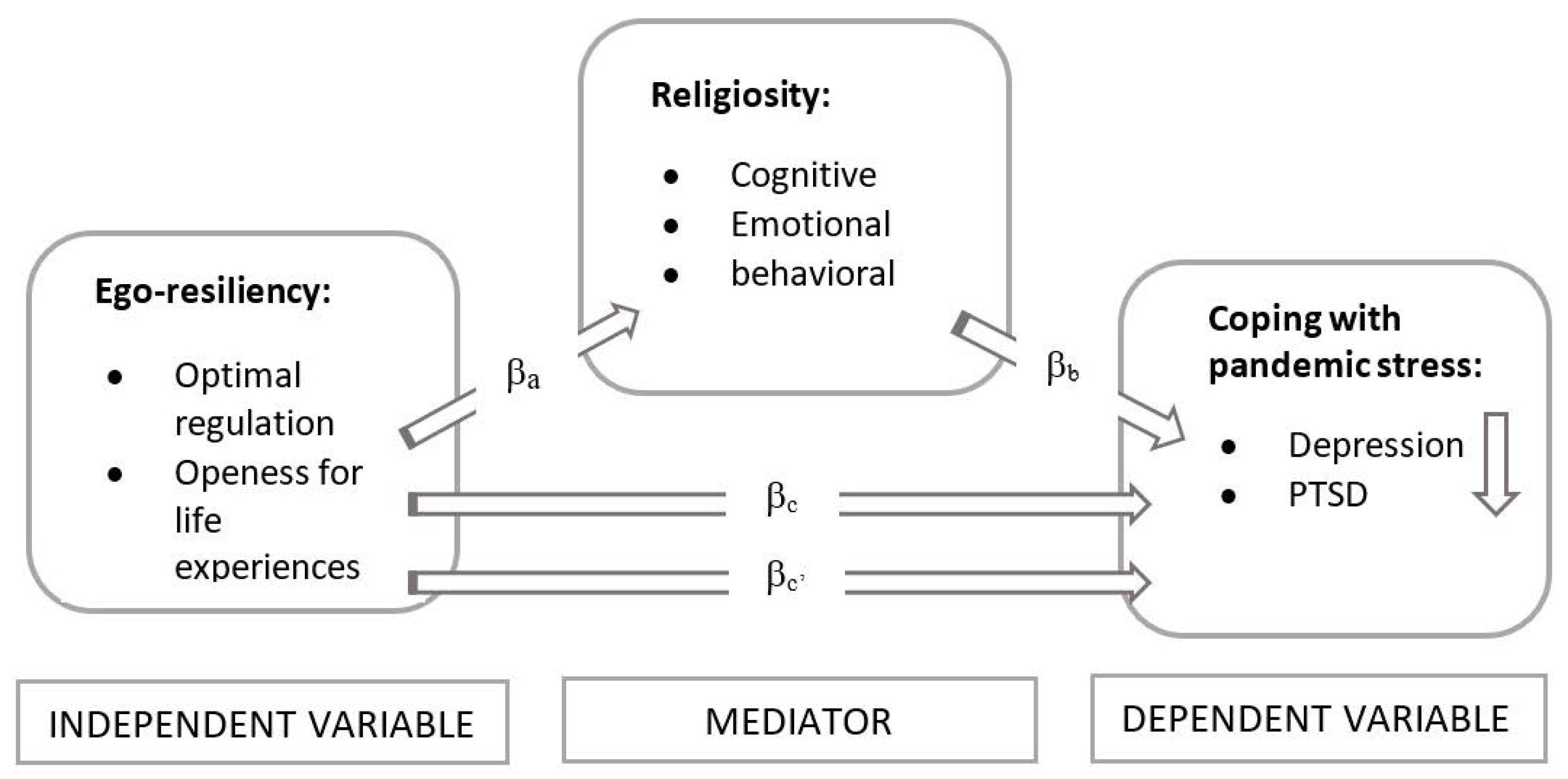
2.3. Design and Construction of a Mediation Model
2.4. Statistical Analysis
3. Results
3.1. Correlation Analysis
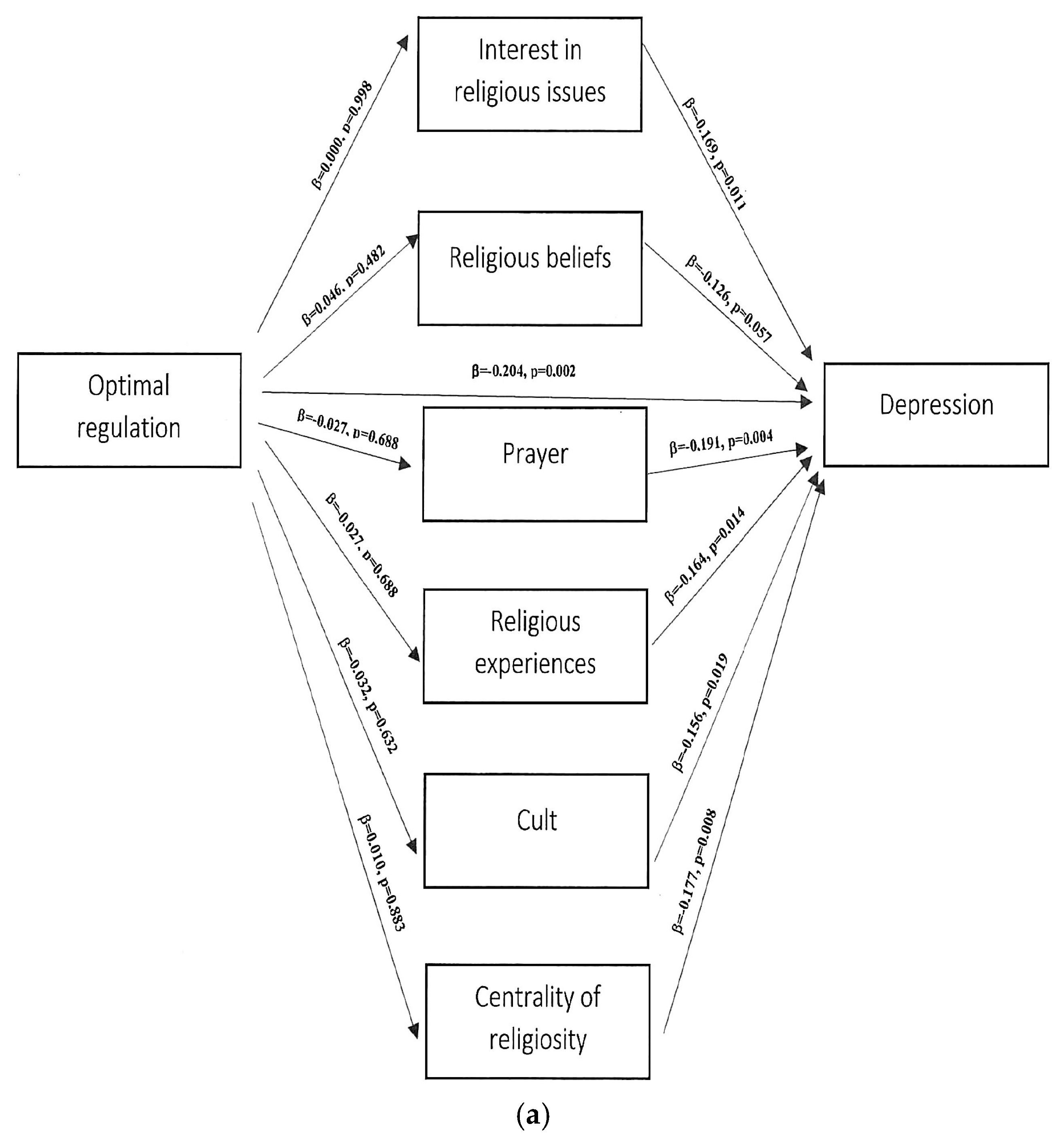
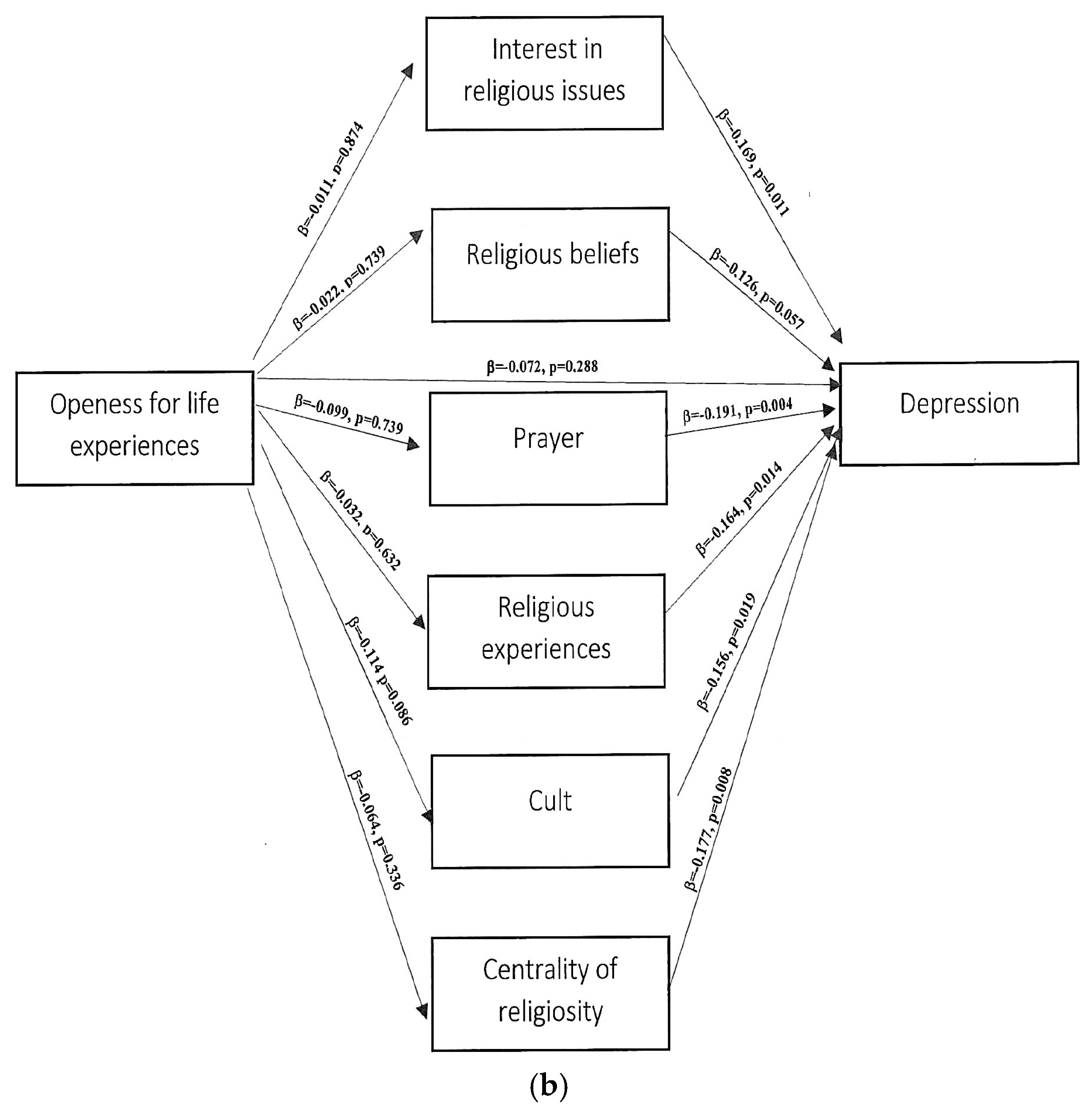
3.2. Regression Analysis
3.3. Path Analysis
3.4. Mediation Analysis
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Krok, D. Współzależność religijności z poczuciem sensu życia i nadzieją w okresie późnej adolescencji [The interdependence of religiosity with the sense of meaning in life and hope in late adolescence]. Psychol. Rozw. 2016, 21, 65–76. [Google Scholar]
- Block, J.H.; Block, J. The Role of Ego-control and Ego-resiliency in the Organization of Behavior. In Development of Cognition, Affect, and Social Relations; Collins, W., Ed.; Psychology Press: London, UK, 1980; Volume 13, pp. 39–101. [Google Scholar]
- Block, J.; Kremen, A.M. IQ and ego-resiliency: Conceptual and empirical connections and separateness. J. Pers. Soc. Psychol. 1996, 70, 349–361. [Google Scholar] [CrossRef]
- Letzring, T.D.; Block, J.; Funder, D.C. Ego-control and ego-resiliency: Generalization of self-report scales based on personality descriptions from acquaintances, clinicians, and the self. J. Res. Pers. 2005, 39, 395–422. [Google Scholar] [CrossRef]
- Kaczmarek, L.; Sęk, H.; Ziarko, M. Sprężystość psychiczna i zmienne pośredniczące w jej wpływie na zdrowie [Ego Resiliency and the mediators of its effect on health]. Przegląd Psychol. 2011, 54, 29–46. [Google Scholar]
- Farkas, D.; Orosz, G. Ego-resiliency reloaded: A three-component model of general resiliency. PLoS ONE 2015, 10, e0120883. [Google Scholar] [CrossRef] [PubMed]
- Kózka, A.; Przybyła-Basista, H. Perceived stress, ego-resiliency, and relational resources as predictors of psychological well-being in parents of children with Down syndrome. Health Psychol. Rep. 2018, 6, 50–59. [Google Scholar] [CrossRef]
- Ahern, N.R. Adolescent resilience: An evolutionary concept analysis. J. Pediatr. Nurs. 2006, 21, 175–185. [Google Scholar] [CrossRef]
- Connor, K.M.; Davidson, J.R. Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC). Depress. Anxiety 2003, 18, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Nelson-Becker, H.B. Meeting Life Challenges: A Hierarchy of Coping Styles in African American and Jewish American Older Adults. J. Hum. Behav. Soc. Environ. 2004, 10, 155–174. [Google Scholar] [CrossRef]
- Nelson-Becker, H.B. Voices of Resilience: Older Adults in Hospice Care. J. Soc. Work Life Palliat. Care 2006, 2, 87–106. [Google Scholar] [CrossRef]
- Nelson-Becker, H.B. Resilience in Aging: Moving Through Challenge to Wisdom. In Handbook of Family Resilience; Becvar, D.S., Ed.; Springer Science + Business Media: New York, NY, USA, 2013; pp. 339–357. [Google Scholar]
- Nelson-Becker, H.B.; Thomas, M. Religious/Spiritual Struggles and Spiritual Resilience in Marginalised Older Adults. Religions 2020, 11, 431. [Google Scholar] [CrossRef]
- Kubo, T.; Sugawara, D.; Masuyama, A. The effect of ego-resiliency and COVID-19-related stress on mental health among the Japanese population. Personal. Individ. Differ. 2021, 175, 1107026. [Google Scholar] [CrossRef] [PubMed]
- Hayward, R.D.; Krause, N. Religion, mental health and well-being: Social aspects. In Religion, Personality, and Social Behavior; Saroglou, V., Ed.; Psychology Press: New York, NY, USA, 2014; pp. 255–280. [Google Scholar]
- Alessandri, G.; De Longis, E.; Eisenberg, N.; Hobfoll, S.E. A multilevel moderated mediational model of the daily relationships between hassles, exhaustion, ego-resiliency and resulting emotional inertia. J. Res. Pers. 2020, 85, 103913. [Google Scholar] [CrossRef]
- Galatzer-Levy, I.R.; Bonanno, G.A. Heterogeneous Patterns of Stress Over the Four Years of College: Associations with Anxious Attachment and Ego-Resiliency. J. Pers. 2013, 81, 476–486. [Google Scholar] [CrossRef]
- Pressman, S.D.; Cohen, S. Does positive affect influence health? Psychol. Bull. 2005, 131, 925–971. [Google Scholar] [CrossRef] [PubMed]
- Tugade, M.M.; Fredrickson, B.L. Resilient Individuals Use Positive Emotions to Bounce Back from Negative Emotional Experiences. J. Pers. Soc. Psychol. 2004, 86, 320–333. [Google Scholar] [CrossRef]
- Vanistendael, S.; Lecomte, J. Le Bonheur est Toujours Possible. In Construire la Resilience [Happiness is Always Possible. Building Resilience]; Bayard: Paris, France, 2000. [Google Scholar]
- Dębski, P.; Florek, S.; Piegza, M.; Pudlo, R.; Gorczyca, P. Is it good to be resilient during the COVID-19 period? The role of ego-resiliency in the intensity of symptoms of anxiety, alcohol use and aggression among Polish people. Int. J. Occup. Med. Environ. Health 2021, 34, 289–300. [Google Scholar] [CrossRef]
- Karaşar, B.; Canli, D. Psychological Resilience and Depression during the COVID-19 Pandemic in Turkey. Psychiatr. Danub. 2011, 32, 273–279. [Google Scholar] [CrossRef] [PubMed]
- Friedrich-Killinger, S. Centrality of Religiosity as a Resource for Therapy Outcome? Religions 2020, 11, 155. [Google Scholar] [CrossRef]
- Koenig, H.G. Religion, spirituality, and health: The research and clinical implications. ISRN Psychiatry 2012, 2012, 278730. [Google Scholar] [CrossRef]
- Koenig, H.G.; King, D.E.; Carson, V.B. Handbook of Religion and Health, 2nd ed.; Oxford University Press: Oxford, UK, 2012. [Google Scholar]
- Pargament, K.I. Of means and ends: Religion and the search for significance. Int. J. Psychol. Relig. 1992, 2, 201–229. [Google Scholar] [CrossRef]
- Pargament, K.I. Religious methods of coping: Resources for the conservation and transformation of significance. In Religion and the Clinical Practice of Psychology; Shafranske, E.P., Ed.; American Psychological Association: Washington, DC, USA, 1996; pp. 215–239. [Google Scholar]
- Krok, D. Religijny system znaczeń i poczucie sensu życia jako predyktory eudajmonistycznego dobrostanu psychicznego u osób chorych na nowotwór [Religious meaning system and meaning in life as predictors of eudaimonistic psychological well-being in people with cancer]. Stud. Psychol. UKSW 2014, 14, 25–40. [Google Scholar]
- Pargament, K.I. The Psychology of Religion and Coping: Theory, Research, Practice; Guilford Press: New York, NY, USA, 1997. [Google Scholar]
- Park, C.L. Religiousness/spirituality and health: A meaning systems perspective. J. Behav. Med. 2007, 30, 319–328. [Google Scholar] [CrossRef] [PubMed]
- Park, C.L. Religion and Meaning. In Handbook of the Psychology of Religion and Spirituality; Paloutzian, R.F., Park, C.J., Eds.; Guilford Press: New York, NY, USA, 2013; pp. 357–379. [Google Scholar]
- Krok, D. Religijność a duchowość—Różnice i podobieństwa z perspektywy psychologii religii [Religiousness and spirituality—Differences and similarities from the perspective of psycholology of religion]. Pol. Forum Psychol. 2009, 14, 126–141. [Google Scholar]
- Huber, S. Zentralität und Inhalt. In Ein Neues Multidimensionales Messmodell der Religiosität; Leske + Budrich: Leverkusen, Germany, 2003. [Google Scholar]
- Allport, G.W.; Ross, J.M. Personal religious orientation and prejudice. J. Pers. Soc. Psychol. 1967, 5, 4432–4443. [Google Scholar] [CrossRef]
- Glock, C.Y.; Stark, R. Religion and Society in Tension; Rand McNally: Chicago, IL, USA, 1965. [Google Scholar]
- Szałachowski, R.; Tuszyńska-Bogucka, W. “Dies Irae?” The Role of Religiosity in Dealing with Psychological Problems Caused by The COVID-19 Pandemic—Studies on a Polish Sample. Religions 2021, 12, 267. [Google Scholar] [CrossRef]
- Kołodziej-Zaleska, A.; Przybyła-Basista, H. Ego-resiliency jako zasób osobisty—Narzędzie pomiaru i jego wykorzystanie w badaniach interdyscyplinarnych [Ego-resiliency as a personal resource—a measurement tool and its use in interdisciplinary research]. Czas. Psychol. 2018, 24, 159–170. [Google Scholar]
- Zarzycka, B. Skala Centralności Religijności Stefana Hubera [The Polish Version of S. Huber’s Centrality of Religiosity Scale]. Rocz. Psychol. 2007, 10, 133–157. [Google Scholar]
- Juczyński, Z.; Ogińska-Bulik, N. Pomiar zaburzeń po stresie traumatycznym—Polska wersja Zrewidowanej Skali Wpływu Zdarzeń [Measurement of post-traumatic stress disorder—Polish version of Impact Event Scale-Revised]. Psychiatry 2009, 6, 15–25. [Google Scholar]
- Kokoszka, A.; Jastrzębski, A.; Obrębski, M. Psychometric properties of the polish version of Patient Health Questionnaire-9. Psychiatry 2016, 13, 187–193. [Google Scholar]
- Babbie, E.E. The Practice of Social Research, 14th ed.; Cengage Learning: Boston, MA, USA, 2016. [Google Scholar]
- Chaim, W. (Wielo)wymiarowość religijności [(Multi)dimensionality of religiosity]. Stud. Psychol. 2012, 12, 55–94. [Google Scholar]
- Baron, R.M.; Kenny, D.A. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J. Pers. Soc. Psychol. 1986, 51, 1173–1182. [Google Scholar] [CrossRef] [PubMed]
- Huey, S.J., Jr.; Weisz, J.R. Ego control, Ego resiliency, and the Five-Factor Model as predictors of behavioral and emotional problems in clinic-referred children and adolescents. J. Abnorm. Psychol. 1997, 106, 404–415. [Google Scholar] [CrossRef] [PubMed]
- Besharat, M.A.; Ramesh, S.; Moghimi, E. Spiritual health mediates the relationship between ego-strength and adjustment to heart disease. Health Psychol. Open 2018, 5, 1–8. [Google Scholar] [CrossRef]
- Catalano, D.; Chan, F.; Wilson, L.; Chiu, C.-Y.; Muller, V.R. The buffering effect of resilience on depression among individuals with spinal cord injury: A structural equation model. Rehabil. Psychol. 2011, 56, 200–211. [Google Scholar] [CrossRef]
- Ziarko, M.; Siemiątkowska, K.; Sieński, M.; Samborski, W.; Samborska, J.; Mojs, E. Mental Health and Rheumatoid Arthritis: Toward Understanding the Emotional Status of People with Chronic Disease. Biomed. Res. Int. 2019, 1, 1473925. [Google Scholar] [CrossRef] [PubMed]
- Taylor, Z.E.; Jones, B.L. Cultural Contributors to Ego-Resiliency and Associations with Depressive Problems in Midwestern Latino Youth. J. Res. Adolesc. 2020, 30, 349–361. [Google Scholar] [CrossRef]
- Bensimon, M. Elaboration on the association between trauma, PTSD and posttraumatic growth: The role of trait resilience. Personal. Individ. Differ. 2012, 52, 782–787. [Google Scholar] [CrossRef]
- Besser, A.; Weinberg, M.; Zeigler-Hill, V.; Neria, Y. Acute symptoms of posttraumatic stress and dissociative experiences among female israeli civilians exposed to war: The roles of intrapersonal and interpersonal sources of resilience. J. Clin. Psychol. 2014, 70, 1227–1239. [Google Scholar] [CrossRef]
- Ying, L.; Wu, X.; Lin, C.; Jiang, L. Traumatic severity and trait resilience as predictors of posttraumatic stress disorder and depressive symptoms among adolescent survivors of the Wenchuan earthquake. PLoS ONE 2014, 9, e89401. [Google Scholar] [CrossRef]
- Lu, Y.; Yang, D.; Niu, Y.; Zhang, H.; Du, B.; Jiang, X. Factors associated with the resilience of Tibetan adolescent survivors five years after the 2010 Yushu earthquake. PLoS ONE 2020, 15, e0231736. [Google Scholar] [CrossRef]
- Scali, J.; Gandubert, C.; Ritchie, K.; Soulier, M.; Ancelin, M.-L.; Chaudieu, I. Measuring resilience in adult women using the 10-items Connor-Davidson Resilience Scale (CD-RISC). Role of trauma exposure and anxiety disorders. PLoS ONE 2012, 7, e39879. [Google Scholar] [CrossRef] [PubMed]
- Lim, Y.K.; Cho, S.J.; Min, S.; Park, J.H.; Park, S.H. The Differential Effect of Ego-Resiliency on the Relationship between Emotional Labor and Salivary Cortisol Level in Bank Clerks. Int. J. Environ. Res. Public Health 2018, 15, 2576. [Google Scholar] [CrossRef]
- Galea, S.; Merchant, R.M.; Lurie, N. The mental health consequences of COVID-19 and physical distancing: The need for prevention and early intervention. JAMA Intern. Med. 2020, 180, 817–818. [Google Scholar] [CrossRef]
- Lucchetti, G.; Góes, L.G.; Amaral, S.G.; Ganadjian, G.T.; Andrade, I.; Almeida, P.; Do Carmo, V.M.; Manso, M. Spirituality, religiosity and the mental health consequences of social isolation during COVID-19 pandemic. Int. J. Soc. Psychiatry 2021, 67, 672–679. [Google Scholar] [CrossRef] [PubMed]
- Modell, S.M.; Kardia, S. Religion as a Health Promoter During the 2019/2020 COVID Outbreak: View from Detroit. J. Relig. Health 2020, 59, 2243–2255. [Google Scholar] [CrossRef] [PubMed]
- Pirutinsky, S.; Cherniak, A.D.; Rosmarin, D.H. COVID-19, Mental Health, and Religious Coping Among American Orthodox Jews. J. Relig. Health 2020, 59, 2288–2301. [Google Scholar] [CrossRef]
- Weinberger-Litman, S.L.; Litman, L.; Rosen, Z.; Rosmarin, D.H.; Rosenzweig, C. A Look at the First Quarantined Community in the USA: Response of Religious Communal Organizations and Implications for Public Health During the COVID-19 Pandemic. J. Relig. Health 2020, 59, 2269–2282. [Google Scholar] [CrossRef]
- Hall, T.W.; Brokaw, B.F. The relationship of spiritual maturity to level of object relations development and God image. Pastoral Psychol. 1995, 43, 373–391. [Google Scholar] [CrossRef]
- King, D.E.; Cummings, D.; Whetstone, L. Attendance at religious services and subsequent mental health in midlife women. Int. J. Psychiatry Med. 2005, 35, 287–297. [Google Scholar] [CrossRef]
- Koenig, H.G. Religion and medicine II: Religion, mental health, and related behaviors. Int. J. Psychiatry Med. 2001, 31, 97–109. [Google Scholar] [CrossRef] [PubMed]
- Koenig, H.G. Religion and medicine IV: Religion, physical health, and clinical implications. Int. J. Psychiatry Med. 2001, 31, 321–336. [Google Scholar] [CrossRef] [PubMed]
- Larson, D.B.; Sherrill, K.A.; Lyons, J.S.; Craigie, F.C., Jr.; Thielman, S.B.; Greenwold, M.A.; Larson, S.S. Associations between dimensions of religious commitment and mental health reported in the American Journal of Psychiatry and Archives of General Psychiatry: 1978–1989. Am. J. Psychiatry 1992, 149, 557–559. [Google Scholar] [PubMed]
- Maredpour, A. The Relationship between Religiosity and Mental Health in High School Students Using the Mediating Role of Social Support. Health Spiritual. Med. Ethics 2017, 4, 47–53. [Google Scholar]
- Merrill, R.M.; Salazar, R.D. Relationship between church attendance and mental health among Mormons and non-Mormons in Utah. Ment. Health Relig. Cult. 2002, 5, 17–33. [Google Scholar] [CrossRef]
- O’Connor, S.; Vandenberg, B. Psychosis or faith? Clinicians’ assessment of religious beliefs. J. Consul. Clin. Psychol. 2005, 73, 610–616. [Google Scholar] [CrossRef]
- Pargament, K.I.; Magyar-Russell, G.M.; Murray-Swank, N.A. The sacred and the search for significance: Religion as a unique process. J. Soc. Issues 2005, 61, 665–687. [Google Scholar] [CrossRef]
- Rippentrop, A.E.; Altmaier, E.M.; Chen, J.J.; Found, E.M.; Keffala, V.J. The relationship between religion/spirituality and physical health, mental health, and pain in a chronic pain population. Pain 2005, 116, 311–321. [Google Scholar] [CrossRef]
- Smith, T.B.; McCullough, M.E.; Poll, J. Religiousness and depression: Evidence for a main effect and the moderating influence of stressful life events. Psychol. Bull. 2003, 129, 614–636. [Google Scholar] [CrossRef]
- Chen, Y.; Koh, H.K.; Kawachi, I.; Botticelli, M.; VanderWeele, T.J. Religious Service Attendance and Deaths Related to Drugs, Alcohol, and Suicide Among US Health Care Professionals. JAMA Psychiatry 2020, 77, 737–744. [Google Scholar] [CrossRef]
- Ano, G.G.; Vasconcelles, E.B. Religious coping and psychological adjustment to stress: A meta-analysis. J. Clin. Psychol. 2005, 61, 461–480. [Google Scholar] [CrossRef]
- Carleton, R.A.; Esparza, P.; Thaxter, P.J.; Grant, K.E. Stress, religious coping resources, and depressive symptoms in an urban adolescent sample. J. Sci. Study Relig. 2008, 47, 113–121. [Google Scholar] [CrossRef]
- Carpenter, T.P.; Laney, T.; Mezulis, A. Religious coping, stress, and depressive symptoms among adolescents: A prospective study. Psycholog. Relig. Spiritual. 2012, 4, 19–30. [Google Scholar] [CrossRef]
- Lee, S.A.; Choi, E.J.; Ryu, H.U. Negative, but not positive, religious coping strategies are associated with psychological distress, independent of religiosity, in Korean adults with epilepsy. Epilepsy Behav. 2019, 90, 57–60. [Google Scholar] [CrossRef]
- Reutter, K.K.; Bigatti, S.M. Religiosity and Spirituality as Resiliency Resources: Moderation, Mediation, or Moderated Mediation? J. Sci. Study Relig. 2014, 53, 56–72. [Google Scholar] [CrossRef]
- Aflakseir, A.; Mahdiyar, M. The Role of Religious Coping Strategies in Predicting Depression among a Sample of Women with Fertility Problems in Shiraz. J. Reprod. Infertil. 2016, 17, 117–122. [Google Scholar]
- Bonelli, R.; Dew, R.E.; Koenig, H.G.; Rosmarin, D.H.; Vasegh, S. Religious and spiritual factors in depression: Review and integration of the research. Depress. Res. Treat. 2012, 2012, 962860. [Google Scholar] [CrossRef]
- Chida, Y.; Steptoe, A.; Powell, L.H. Religiosity/spirituality and mortality. A systematic quantitative review. Psychother. Psychosom. 2009, 78, 81–90. [Google Scholar] [CrossRef]
- Fradelos, E.C.; Latsou, D.; Mitsi, D.; Tsaras, K.; Lekka, D.; Lavdaniti, M.; Tzavella, F.; Papathanasiou, I.V. Assessment of the relation between religiosity, mental health, and psychological resilience in breast cancer patients. Contemp. Oncol. 2018, 22, 172–177. [Google Scholar] [CrossRef]
- Holt, C.L.; Wang, M.Q.; Caplan, L.; Schulz, E.; Blake, V.; Southward, V.L. Role of religious involvement and spirituality in functioning among African Americans with cancer: Testing a mediational model. J. Behav. Med. 2011, 34, 437–448. [Google Scholar] [CrossRef]
- Inzlicht, M.; Tullett, A.M. Reflecting on God: Religious primes can reduce neurophysiological response to errors. Psychol. Sci. 2010, 21, 1184–1190. [Google Scholar] [CrossRef]
- Kasen, S.; Wickramaratne, P.; Gameroff, M.J.; Weissman, M.M. Religiosity and resilience in persons at high risk for major depression. Psychol. Med. 2012, 42, 509–519. [Google Scholar] [CrossRef] [PubMed]
- Mosqueiro, B.P.; Da Rocha, N.S.; Fleck, M. Intrinsic religiosity, resilience, quality of life, and suicide risk in depressed inpatients. J. Affect. Disord. 2015, 179, 128–133. [Google Scholar] [CrossRef] [PubMed]
- Mystakidou, K.; Tsilika, E.; Parpa, E.; Pathiaki, M.; Patiraki, E.; Galanos, A.; Vlahos, L. Exploring the relationships between depression, hopelessness, cognitive status, pain, and spirituality in patients with advanced cancer. Arch. Psychiatr. Nurs. 2007, 21, 150–161. [Google Scholar] [CrossRef] [PubMed]
- Neeleman, J.; Lewis, G. Religious identity and comfort beliefs in three groups of psychiatric patients and a group of medical controls. Int. J. Soc. Psychiatry 1994, 40, 124–134. [Google Scholar] [CrossRef] [PubMed]
- Rammohan, A.; Rao, K.; Subbakrishna, D.K. Religious coping and psychological wellbeing in carers of relatives with schizophrenia. Acta Psychiatr. Scand. 2020, 105, 356–362. [Google Scholar] [CrossRef] [PubMed]
- Schnall, E.; Wassertheil-Smoller, S.; Swencionis, C.; Zemon, V.; Tinker, L.; O’Sullivan, M.J.; Van Horn, L.; Goodwin, M. The relationship between religion and cardiovascular outcomes and all-cause mortality in the Women’s Health Initiative Observational Study. Psychol. Health 2010, 25, 249–263. [Google Scholar] [CrossRef]
- Tepper, L.; Rogers, S.A.; Coleman, E.M.; Malony, H.N. The prevalence of religious coping among persons with persistent mental illness. Psychiatr. Serv. 2001, 52, 660–665. [Google Scholar] [CrossRef]
- Miller, L.; Warner, V.; Wickramaratne, P.; Weissman, M.M. Religiosity and depression: Ten-year follow-up of depressed mothers and offspring. Child Adolesc. Psychiatr. 1997, 36, 1416–1425. [Google Scholar] [CrossRef]
- Miller, L.; Wickramaratne, P.; Gameroff, M.J.; Sage, M.; Tenke, C.E.; Weissman, M.M. Religiosity and major depression in adults at high risk: A ten-year prospective study. Am. J. Psychiatry 2012, 169, 89–94. [Google Scholar] [CrossRef]
- Svob, C.; Reich, L.; Wickramaratne, P.; Warner, V.; Weissman, M.M. Religion and spirituality predict lower rates of suicide attempts and ideation in children and adolescents at risk for major depressive disorder. J. Am. Acad. Child Adolesc. Psychiatry 2016, 55, 251. [Google Scholar] [CrossRef]
- Svob, C.; Wickramaratne, P.J.; Reich, L.; Zhao, R.; Talati, A.; Gameroff, M.J.; Saeed, R.; Weissman, M.M. Association of Parent and Offspring Religiosity with Offspring Suicide Ideation and Attempts. JAMA Psychiatry 2018, 75, 1062–1070. [Google Scholar] [CrossRef]
- De Berardis, D.; Olivieri, L.; Rapini, G.; Serroni, N.; Fornaro, M.; Valchera, A.; Carano, A.; Vellante, F.; Bustini, M.; Serafini, G.; et al. Religious Coping, Hopelessness, and Suicide Ideation in Subjects with First-Episode Major Depression: An Exploratory Study in the Real World Clinical Practice. Brain Sci. 2020, 10, 912. [Google Scholar] [CrossRef]
- Pirutinsky, S.; Rosmarin, D.H.; Pargament, K.I.; Midlarsky, E. Does negative religious coping accompany, precede, or follow depression among Orthodox Jews? J. Affect. Disord. 2011, 132, 401–405. [Google Scholar] [CrossRef]
- Pargament, K.I.; Lomax, J.W. Understanding and addressing religion among people with mental illness. World Psychiatry 2013, 12, 26–32. [Google Scholar] [CrossRef]
- Weber, S.R.; Pargament, K.I.; Kunik, M.E.; Lomax, J.W., II; Stanley, M.A. Psychological distress among religious nonbelievers: A systematic review. J. Relig. Health 2012, 51, 72–86. [Google Scholar] [CrossRef]
- Kay, A.C.; Gaucher, D.; McGregor, I.; Nash, K. Religious belief as compensatory control. Pers. Soc. Psychol. Rev. 2010, 14, 37–48. [Google Scholar] [CrossRef]
- Jantos, M.; Kiat, H. Prayer as medicine: How much have we learned? Med. J. Aust. 2007, 186, 51–53. [Google Scholar] [CrossRef]
- Johannessen-Henry, C.T.; Deltour, I.; Bidstrup, P.E.; Dalton, S.O.; Johansen, C. Associations between faith, distress and mental adjustment–a Danish survivorship study. Acta Oncol. 2013, 52, 364–371. [Google Scholar] [CrossRef]
- Schreiber, J.A.; Brockopp, D.Y. Twenty-five years later—what do we know about religion/spirituality and psychological well-being among breast cancer survivors? A systematic review. J. Cancer. Surviv. 2012, 6, 82–94. [Google Scholar] [CrossRef]
- Zimmer, Z.; Jagger, C.; Chiu, C.T.; Ofstedal, M.B.; Rojo, F.; Saito, Y. Spirituality, religiosity, aging and health in global perspective: A review. SSM Popul. Health 2016, 2, 373–381. [Google Scholar] [CrossRef]
- Mancini, A.D.; Bonanno, G.A. Predictors and parameters of resilience to loss: Toward an individual differences model. J. Pers. 2009, 77, 1805–1832. [Google Scholar] [CrossRef]
- Huber, S. Kerndimensionen, Zentralität und Inhalt. Ein interdisziplinäres Modell der Religiosität. J. Psychol. 2008, 16, 5. Available online: http://www.journal-fuer-psychologie.de/jfp-3-2008-05.html (accessed on 20 December 2020).
- Zarzycka, B.; Bartczuk, R.P.; Rybarski, R. Centrality of Religiosity Scale in Polish Research: A Curvilinear Mechanism that Explains the Categories of Centrality of Religiosity. Religions 2020, 11, 64. [Google Scholar] [CrossRef]
- McFadden, S.H. Old persons, old age, aging, and religion. In Handbook of the Psychology of Religion and Spirituality; Paloutzian, R.F., Park, C.L., Eds.; Guilford Press: New York, NY, USA, 2013; pp. 198–212. [Google Scholar]
- Krok, D.; Zarzycka, B. Interpersonal Forgiveness and Meaning in Life in Older Adults: The Mediating and Moderating Roles of the Religious Meaning System. Religions 2021, 12, 37. [Google Scholar] [CrossRef]
- Davie, G.; Vincent, J. Religion and old age. Ageing Soc. 1998, 18, 101–110. [Google Scholar] [CrossRef]
- Madge, N.; Hemming, P.J. Young British religious ‘nones’: Findings from the Youth on Religion study. J. Youth Stud. 2017, 20, 872–888. [Google Scholar] [CrossRef]
- Manuti, A.; Scardigno, Z.R.; Mininni, G. Me, myself, and God: Religion as a psychocultural resource of meaning in later life. Cult. Psychol. 2016, 22, 3–34. [Google Scholar] [CrossRef]
- Markstrom-Adams, C.; Smith, M. Identity formation and religious orientation among high school students from the United States and Canada. J. Youth. Adolesc. 1996, 23, 453–469. [Google Scholar] [CrossRef]
- Allen, R.O.; Spilka, B. Committed and consensual religion: A specification of religion-prejudice relationships. J. Sci. Study Relig. 1967, 6, 191–206. [Google Scholar] [CrossRef]
- Hebert, R.; Zdaniuk, B.; Schulz, R.; Scheier, M. Positive and Negative Religious Coping and Well-Being in Women with Breast Cancer. J. Palliat. Med. 2009, 12, 537–545. [Google Scholar] [CrossRef] [PubMed]
- Manning-Walsh, J. Spiritual struggle: Effect on quality of life and life satisfaction in women with breast cancer. J. Holist. Nurs. 2005, 23, 120–140. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, B.; Shrestha, S.; Stanley, M.A.; Pargament, K.I.; Cummings, J.; Kunik, M.E.; Fletcher, T.L.; Cortes, J.; Ramsey, D.; Amspoker, A.B. Positive and negative religious coping as predictors of distress among minority older adults. Int. J. Geriatr. Psychiatry 2019, 34, 54–59. [Google Scholar] [CrossRef] [PubMed]
- Pargament, I.K.; Smith, B.W.; Koenig, H.G.; Perez, L. Patterns of positive and negative religious coping with major life stressors. J. Sci. Study Relig. 1998, 37, 710–724. [Google Scholar] [CrossRef]
- Dein, S.; Loewenthal, K.; Lewis, C.A.; Pargament, K.I. COVID-19, mental health and religion: An agenda for future research. Ment. Health Relig. Cult. 2020, 23, 1–9. [Google Scholar] [CrossRef]
- Isiko, P.A. Religious construction of disease: An exploratory appraisal of religious responses to the COVID-19 pandemic in Uganda. J. Afr. Stud. Dev. 2020, 12, 77–96. [Google Scholar]
- Ahrenfeldt, L.J.; Möller, S.; Andersen-Ranberg, K.; Vitved, A.R.; Lindahl-Jacobsen, R.; Hvidt, N.C. Religiousness and health in Europe. Eur. J. Epidemiol. 2017, 32, 921–929. [Google Scholar] [CrossRef]
- Ćurković, M.; Košec, A.; Ćurković, D. Math and aftermath of COVID-19 pandemic and its interrelationship from the resilience perspective. J. Infect. 2020, 81, e173–e174. [Google Scholar] [CrossRef]
- Fullana, M.A.; Hidalgo-Mazzei, D.; Vieta, E.; Radua, J. Coping behaviors associated with decreased anxiety and depressive symptoms during the COVID-19 pandemic and lockdown. J. Affect. Disord. 2020, 275, 80–81. [Google Scholar] [CrossRef]
- Knolle, F.; Ronan, L.; Murray, G.K. The impact of the COVID-19 pandemic on mental health in the general population: A comparison between Germany and the UK. BMC Psychol. 2021, 9, 60. [Google Scholar] [CrossRef]
- Nikolaidis, A.; Paksarian, D.; Alexander, L.; Derosa, J.; Dunn, J.; Nielson, D.M.; Droney, I.; Kang, M.; Douka, I.; Bromet, E.; et al. The Coronavirus Health and Impact Survey (CRISIS) reveals reproducible correlates of pandemic-related mood states across the Atlantic. Sci. Rep. 2021, 11, 8139. [Google Scholar] [CrossRef] [PubMed]
- Padmanabhanunni, A.; Pretorius, T. The Loneliness–Life Satisfaction Relationship: The Paralleland Serial Mediating Role of Hopelessness, Depression and Ego-Resilience among Young Adults in South Africa during COVID-19. Int. J. Environ. Res. Public Health 2021, 18, 3613. [Google Scholar] [CrossRef] [PubMed]
- Palgi, Y.; Shrira, A.; Ring, L.; Bodner, E.; Avidor, S.; Bergman, Y.; Cohen-Fridel, S.; Keisari, S.; Hoffman, Y. The loneliness pandemic: Loneliness and other concomitants of depression, anxiety and their comorbidity during the COVID-19 outbreak. J. Affect. Disord. 2020, 275, 109–111. [Google Scholar] [CrossRef] [PubMed]
- Pierce, M.; Hope, H.; Ford, T.; Hatch, S.; Hotopf, M.; John, A.; Kontopantelis, E.; Webb, R.; Wessely, S.; McManus, S.; et al. Mental health before and during the COVID-19 pandemic: A longitudinal probability sample survey of the UK population. Lancet Psychiatry 2020, 7, 883–892. [Google Scholar] [CrossRef]
- Rigoli, F. The Link Between COVID-19, Anxiety, and Religious Beliefs in the United States and the United Kingdom. J. Relig. Health 2021, 60, 2196–2208. [Google Scholar] [CrossRef]
- Królikowska, A. Współczesna polska religijność w kontekście teorii anomii R. K. Mertona [Contemporary Polish religiosity in the context of R. K. Merton’s theory of anomie.]. Ruch Praw. Ekon. I Socjol. 2001, 1, 171–185. [Google Scholar]
- Mariański, J. Religijność społeczeństwa polskiego w perspektywie europejskiej: Próba syntezy socjologicznej. In The Religiosity of Polish Society in the European Perspective. An Attempt at a Sociological Synthesis; Zakład Wydawniczy Nomos: Kraków, Poland, 2004. [Google Scholar]


| Female | Male | p | Female | Male | p | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | (%) | n | (%) | n | % | n | % | ||||
| Place of residence | 0.480 | Marital status | 0.094 | ||||||||
| village | 21 | 12 | 8 | 14 | single | 90 | 51.4 | 21 | 36.8 | ||
| town of up to 25,000 thousand | 17 | 9.7 | 4 | 7 | married | 74 | 42.3 | 30 | 52.6 | ||
| small town of 25–50 thousand | 13 | 7.4 | 4 | 7 | divorced | 11 | 6.3 | 5 | 8.8 | ||
| average city of 50–300 thousand | 31 | 17.7 | 5 | 8.8 | separated | - | - | 1 | 1.8 | ||
| large city of more than 300 thousand | 93 | 53.1 | 36 | 63.2 | widowed | - | - | - | - | ||
| Education | 0.593 | Having children | 0.129 | ||||||||
| primary education | 2 | 1.1 | 1 | 1.8 | |||||||
| secondary education | 19 | 10.9 | 10 | 17.5 | yes | 78 | 44.6 | 32 | 56.1 | ||
| secondary education and studying | 38 | 21.7 | 11 | 19.3 | |||||||
| higher education | 91 | 52 | 30 | 52.6 | no | 97 | 55.4 | 25 | 43.9 | ||
| higher education and studying | 25 | 14.3 | 5 | 8.8 | |||||||
| Assessment of material status | 0.408 | Assessment of health status | 0.920 | ||||||||
| very poor | 1 | 0.6 | - | - | very poor | - | - | - | - | ||
| poor | 8 | 4.6 | 3 | 5.3 | poor | 8 | 4.6 | 3 | 5.3 | ||
| average | 65 | 37.1 | 14 | 24.6 | average | 29 | 16.6 | 10 | 17.5 | ||
| good | 78 | 44.6 | 33 | 57.9 | good | 89 | 50.9 | 26 | 45.6 | ||
| very good | 23 | 13.1 | 7 | 12.3 | very good | 49 | 28 | 18 | 31.6 | ||
| M | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. OR | r | 22.27 | 4.32 | - | |||||||||||
| p | - | ||||||||||||||
| 2. OL | r | 11.57 | 2.65 | 0.544 | |||||||||||
| p | 0.000 | ||||||||||||||
| 3. I | r | 11.57 | 2.65 | −0.127 | −0.054 | ||||||||||
| p | 0.054 | 0.417 | |||||||||||||
| 4. H | r | 8.6 | 6.7 | −0.129 | −0.111 | 0.885 | |||||||||
| p | 0.053 | 0.096 | 0.000 | ||||||||||||
| 5. A | r | 9.25 | 6.03 | 0.015 | −0.015 | 0.695 | 0.703 | ||||||||
| p | 0.816 | 0.828 | 0.000 | 0.000 | |||||||||||
| 6. D | r | 6.96 | 6.56 | −0.204 | −0.072 | 0.560 | 0.619 | 0.368 | |||||||
| p | 0.002 | 0.288 | 0.000 | 0.000 | 0.000 | ||||||||||
| 7. IRI | r | 9.35 | 3.99 | 0.000 | −0.011 | −0.126 | −0.188 | −0.156 | −0.169 | ||||||
| p | 0.998 | 0.874 | 0.056 | 0.004 | 0.018 | 0.011 | |||||||||
| 8. RB | r | 11.95 | 4.02 | 0.046 | −0.022 | −0.062 | −0.141 | −0.081 | −0.126 | 0.699 | |||||
| p | 0.482 | 0.739 | 0.350 | 0.034 | 0.224 | 0.057 | 0.000 | ||||||||
| 9. P | r | 10.41 | 4.5 | −0.027 | −0.099 | −0.112 | −0.188 | −0.207 | −0.191 | 0.848 | 0.805 | ||||
| p | 0.688 | 0.137 | 0.091 | 0.004 | 0.002 | 0.004 | 0.000 | 0.000 | |||||||
| 10. RE | r | 9.29 | 3.93 | 0.069 | −0.032 | 0.021 | −0.034 | −0.061 | −0.164 | 0.733 | 0.757 | 0.809 | |||
| p | 0.299 | 0.632 | 0.754 | 0.612 | 0.358 | 0.014 | 0.000 | 0.000 | 0.000 | ||||||
| 11. C | r | 9.68 | 4.73 | −0.032 | −0.114 | −0.089 | −0.174 | −0.178 | −0.156 | 0.821 | 0.774 | 0.890 | 0.779 | ||
| p | 0.632 | 0.086 | 0.177 | 0.008 | 0.007 | 0.019 | 0.000 | 0.000 | 0.000 | 0.000 | |||||
| 12. CoR | r | 50.71 | 19.37 | 0.010 | −0.064 | −0.083 | −0.161 | −0.153 | −0.177 | 0.898 | 0.882 | 0.956 | 0.889 | 0.939 | |
| p | 0.883 | 0.336 | 0.213 | 0.015 | 0.020 | 0.008 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | ||||
| 13. PTSD | r | 27.14 | 18.78 | −0.092 | −0.074 | 0.945 | 0.948 | 0.856 | 0.555 | −0.167 | −0.087 | −0.171 | −0.013 | −0.150 | −0.132 |
| p | 0.165 | 0.268 | 0.000 | 0.000 | 0.000 | 0.000 | 0.011 | 0.187 | 0.010 | 0.845 | 0.023 | 0.046 | |||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | ||||
| Dependent Variable | Independent Variables | (Beta) | R | R2 | F | SR2 |
|---|---|---|---|---|---|---|
| Predictors of Depression—MODELS 1–3 | ||||||
| Depression | Optimal regulation (N = 226) | −0.204 | 0.204 | 0.042 | 9.740 * | 0.037 |
| Religiosity (N = 227) | ||||||
| Interest in religious issues | −0.169 | 0.169 | 0.029 | 6.603 * | 0.024 | |
| Prayer | −0.260 | 0.260 | 0.037 | 8.532 ** | 0.032 | |
| Religious experience | −0.164 | 0.164 | 0.027 | 6.185 * | 0.022 | |
| Cult | −0.156 | 0.156 | 0.024 | 5.624 * | 0.020 | |
| Centrality of religiosity (N = 226) | −0.177 | 0.177 | 0.031 | 7.271 ** | 0.027 | |
| Predictors of PTSD (N = 230)—MODEL 4 | ||||||
| Hyperarousal | Interest in religious issues | −0.188 | 0.188 | 0.035 | 8.280 ** | 0.031 |
| Prayer | −0.188 | 0.188 | 0.035 | 8.253 ** | 0.031 | |
| Religious beliefs | −0.141 | 0.141 | 0.020 | 4.559 * | 0.015 | |
| Cult | −0.174 | 0.174 | 0.030 | 7.094 ** | 0.026 | |
| Avoidance | Interest in religious issues | −0.156 | 0.156 | 0.024 | 5.663 * | 0.020 |
| Prayer | −0.207 | 0.207 | 0.043 | 1.284 ** | 0.039 | |
| Cult | −0.178 | 0.178 | 0.032 | 7.473 ** | 0.003 | |
| OR/Religiosity/Depression | OL/Religiosity/Depression | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Z | p | βc | p | βc’ | p | Z | p | βc | ip | βc’ | p | |
| IRI | 0.000 | 0.999 | −0.204 | 0.002 | −0.242 | 0.000 | 0.010 | 0.991 | −0.072 | 0.288 | −0.027 | 0.680 |
| RB | −0.647 | 0.517 | −0.204 | 0.002 | −0.238 | 0.000 | −0.711 | 0.476 | −0.072 | 0.288 | −0.109 | 0.099 |
| P | 0.407 | 0.684 | −0.204 | 0.002 | −0.247 | 0.000 | 1.610 | 0.107 | −0.072 | 0.288 | −0.184 | 0.005 |
| RE | −0.930 | 0.352 | −0.204 | 0.002 | −0.234 | 0.000 | 0.932 | 0.351 | −0.072 | 0.288 | −0.142 | 0.031 |
| C | 0.476 | 0.634 | −0.204 | 0.002 | −0.247 | 0.000 | 1.512 | 0.131 | −0.072 | 0.288 | −0.157 | 0.018 |
| CoR | −0.168 | 0.866 | −0.204 | 0.002 | −0.241 | 0.000 | 1.165 | 0.244 | −0.072 | 0.288 | −0.165 | 0.012 |
| OR/Religiosity/PTSD | OL/Religiosity/PTSD | |||||||||||
| IRI | 0.000 | 0.999 | −0.092 | 0.165 | −0.134 | 0.039 | −0.010 | 0.991 | −0.074 | 0.268 | −0.701 | 0.484 |
| RB | −0.639 | 0.523 | −0.092 | 0.165 | −0.131 | 0.047 | 0.701 | 0.484 | −0.074 | 0.268 | −0.007 | 0.325 |
| P | 0.408 | 0.683 | −0.092 | 0.165 | −0.139 | 0.032 | 0.653 | 0.632 | −0.074 | 0.268 | −0.087 | 0.189 |
| RE | −0.555 | 0.579 | −0.092 | 0.165 | −0.133 | 0.045 | 0.554 | 0.579 | −0.074 | 0.268 | −0.063 | 0.343 |
| C | 0.478 | 0.633 | −0.092 | 0.165 | −0.140 | 0.032 | 1.587 | 0.112 | −0.074 | 0.268 | −0.083 | 0.206 |
| CoR | 0.168 | 0.866 | −0.092 | 0.165 | −0.133 | 0.042 | −1.265 | 0.206 | −0.074 | 0.268 | −0.073 | 0.264 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Szałachowski, R.R.; Tuszyńska-Bogucka, W. “Faith Is Not Enough?” Ego-Resiliency and Religiosity as Coping Resources with Pandemic Stress—Mediation Study. Int. J. Environ. Res. Public Health 2023, 20, 1942. https://doi.org/10.3390/ijerph20031942
Szałachowski RR, Tuszyńska-Bogucka W. “Faith Is Not Enough?” Ego-Resiliency and Religiosity as Coping Resources with Pandemic Stress—Mediation Study. International Journal of Environmental Research and Public Health. 2023; 20(3):1942. https://doi.org/10.3390/ijerph20031942
Chicago/Turabian StyleSzałachowski, Roman Ryszard, and Wioletta Tuszyńska-Bogucka. 2023. "“Faith Is Not Enough?” Ego-Resiliency and Religiosity as Coping Resources with Pandemic Stress—Mediation Study" International Journal of Environmental Research and Public Health 20, no. 3: 1942. https://doi.org/10.3390/ijerph20031942
APA StyleSzałachowski, R. R., & Tuszyńska-Bogucka, W. (2023). “Faith Is Not Enough?” Ego-Resiliency and Religiosity as Coping Resources with Pandemic Stress—Mediation Study. International Journal of Environmental Research and Public Health, 20(3), 1942. https://doi.org/10.3390/ijerph20031942






