Effect of the Case for Carpule as a Visual Passive Distraction Tool on Dental Fear and Anxiety: A Pilot Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Aspects
2.2. Experimental Design and Subjects of the Study
2.3. Administration of the Inferior Alveolar Nerve Block
2.4. Evaluate Fear and Anxiety through Behavioral Management
2.5. Evaluate Fear and Anxiety through Physiological Changes
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Murad, M.H.; Ingle, N.A.; Assery, M.K. Evaluating factors associated with fear and anxiety to dental treatment: A systematic review. J. Fam. Med. Prim. Care 2020, 9, 4530–4535. [Google Scholar] [CrossRef] [PubMed]
- Armfield, J.M.; Heaton, L.J. Management of fear and anxiety in the dental clinic: A review. Aust. Dent. J. 2013, 58, 390–407. [Google Scholar] [CrossRef] [PubMed]
- Ran, L.; Zhao, N.; Fan, L.; Zhou, P.; Zhang, C.; Yu, C. Application of virtual reality on non-drug behavioral management of short- term dental procedure in children. Trials 2021, 22, 562. [Google Scholar] [CrossRef]
- Song, J.S.; Chung, H.C.; Sohn, S.; Kim, Y.J. Effects of psychological behaviour management programme on dental fear and anxiety in children: A randomised controlled clinical trial. Eur. J. Paediatr. Dent. 2020, 21, 287–291. [Google Scholar]
- Scandurra, C.; Gasparro, R.; Dolce, P.; Bochicchio, V.; Muzii, B.; Sammartino, G. The role of cognitive and non-cognitive factors in dental anxiety: A mediation model. Eur. J. Oral Sci. 2021, 129, e12793. [Google Scholar] [CrossRef]
- Shekhar, S.; Suprabha, B.S.; Shenoy, R.; Rao, A.; Rao, A. Effect of active and passive distraction techniques while administering local anaesthesia on the dental anxiety, behaviour and pain levels of children: A randomised controlled trial. Eur. Arch. Paediatr. Dent. 2022, 23, 417–427. [Google Scholar] [CrossRef]
- Lin, C.S.; Wu, S.Y.; Yi, C.A. Association between anxiety and pain in dental treatment: A systematic review and meta-analysis. J. Dent. Res. 2017, 96, 153–162. [Google Scholar] [CrossRef]
- Murillo-Benítez, M.; Martín-González, J.; Jiménez-Sánchez, M.C.; Cabanillas-Balsera, D.; Velasco-Ortega, E.; Segura-Egea, J.J. Association between dental anxiety and intraoperative pain during root canal treatment: A cross-sectional study. Int. Endod. J. 2020, 53, 447–454. [Google Scholar] [CrossRef]
- van Wijk, A.J.; Makkes, P.C. Highly anxious dental patients report more pain during dental injections. Br. Dent. J. 2008, 205, E7. [Google Scholar] [CrossRef]
- Witcraft, S.M.; Wickenhauser, M.E.; Maack, D.J.; Dixon, L.J. What sensitivities matter in dental anxiety? Investigating sensitivity to anxiety, pain, and disgust. Psychol. Health Med. 2021, 26, 313–321. [Google Scholar] [CrossRef]
- American Academy of Pediatric Dentistry. Behavior Guidance for the Pediatric Dental Patient. Available online: https://www.aapd.org/research/oral-health-policies--recommendations/behavior-guidance-for-the-pediatric-dental-patient/ (accessed on 10 January 2023).
- Sathyamoorthy, M.; Hamilton, T.B.; Wilson, G.; Talluri, R.; Fawad, L.; Adamiak, B.; Wallace, C.; Borisova, I.; Heard, C. Pre-medication before dental procedures: A randomized controlled study comparing intranasal dexmedetomidine with oral midazolam. Acta Anaesthesiol. Scand. 2019, 63, 1162–1168. [Google Scholar] [CrossRef]
- Guney, S.E.; Araz, C.; Tirali, R.E.; Cehreli, S.B. Dental anxiety and oral health-related quality of life in children following dental rehabilitation under general anesthesia or intravenous sedation: A prospective cross-sectional study. Niger. J. Clin. Pract. 2018, 21, 1304–1310. [Google Scholar]
- Stefano, R.; Bruno, A.; Muscatello, M.R.; Cedro, C.; Cervino, G.; Fiorillo, L. Fear and anxiety managing methods during dental treatments: A systematic review of recent data. Minerva Stomatol. 2019, 68, 317–331. [Google Scholar] [CrossRef] [PubMed]
- Desai, S.P.; Shah, P.P.; Jajoo, S.S.; Smita, P.S. Assessment of parental attitude toward different behavior management techniques used in pediatric dentistry. J. Indian Soc. Pedod. Prev. Dent. 2019, 37, 350–359. [Google Scholar] [CrossRef] [PubMed]
- Guinot, F.; Virolés, M.; Lluch, C.; Costa, A.L.; Veloso, A. Spanish and portuguese parental acceptance of behavior management techniques in pediatric dentistry. J. Clin. Pediatr. Dent. 2021, 45, 247–252. [Google Scholar] [CrossRef]
- Ghadimi, S.; Estaki, Z.; Rahbar, P.; Shamshiri, A.R. Effect of visual distraction on children’s anxiety during dental treatment: A crossover randomized clinical trial. Eur. Arch. Paediatr. Dent. 2018, 19, 239–244. [Google Scholar] [CrossRef] [PubMed]
- Robertson, M.; Araújo, M.; Innes, N. Anxiety and fear management in paediatric dentistry using distraction techniques. Evid. Based Dent. 2019, 20, 50–51. [Google Scholar] [CrossRef]
- Kakkar, M.; Wahi, A.; Thakkar, R.; Vohra, I.; Shukla, A.K. Prevalence of dental anxiety in 10-14 years old children and its implications. J. Dent. Anesth. Pain Med. 2016, 16, 199–202. [Google Scholar] [CrossRef]
- Dahlander, A.; Soares, F.; Grindefjord, M.; Dahllöf, G. Factors associated with dental fear and anxiety in children aged 7 to 9 years. Dent. J. 2019, 7, 68. [Google Scholar] [CrossRef]
- Tollili, C.; Katsouda, M.; Coolidge, T.; Kotsanos, N.; Karagiannis, V.; Arapostathis, K.N. Child dental fear and past dental experience: Comparison of parents’ and children’s ratings. Eur. Arch. Paediatr. Dent. 2020, 21, 597–608. [Google Scholar] [CrossRef]
- Frankl, S.N.; Shiere, F.R.; Fogels, H.R. Should the parent remain with the child in the dental operatory? J. Dent. Child. 1962, 29, 150–163. [Google Scholar]
- Curcio, W.B.; Abreu, L.G.; Carrada, C.F.; Scalioni, F.A.R.; Ribeiro, R.A. Relationship between salivary cortisol levels and children’s behavior during a dental examination. J. Dent. Child. 2017, 84, 80–85. [Google Scholar]
- Sridhar, S.; Suprabha, B.S.; Shenoy, R.; Shwetha, K.T.; Rao, A. Effect of a relaxation training exercise on behaviour, anxiety, and pain during buccal infiltration anaesthesia in children: Randomized clinical trial. Int. J. Paediatr. Dent. 2019, 29, 596–602. [Google Scholar] [CrossRef]
- Almaummar, M.; Althabit, H.O.; Pani, S. The impact of dental treatment and age on salivary cortisol and alpha-amylase levels of patients with varying degrees of dental anxiety. BMC Oral Health 2019, 6, 211. [Google Scholar] [CrossRef]
- Beaudette, J.; Fritz, P.; Sullivan, P.; Ward, W. Oral health, nutritional choices, and dental fear and anxiety. Dent. J. 2017, 5, 8. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Manso, J.C.; Gujarathi, R.; Varacallo, M. Autonomic Dysfunction. In StatPearls]; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Chojnowska, S.; Ptaszyńska-Sarosiek, I.; Kepka, A.; Knaz, M.; Waszkiewicz, M. Salivary biomarkers of stress, anxiety and depression. J. Clin. Med. 2021, 10, 517. [Google Scholar] [CrossRef]
- Lós, K.; Waszkiewicz, N. Biological markers in anxiety disorders. J. Clin. Med. 2021, 17, 1744. [Google Scholar] [CrossRef]
- Birnie, K.A.; Hundert, A.S.; Lalloo, C.; Nguyen, C.; Stins, J.N. Recommendations for selection of self-report pain intensity measures in children and adolescents: A systematic review and quality assessment of measurement properties. Pain 2019, 160, 5–18. [Google Scholar] [CrossRef]

| Rating | Description |
|---|---|
| Definitely negative | Refusal of treatment, crying forcefully, fearful, or any other overt evidence of extreme negativism. |
| Negative | Reluctant to accept treatment, uncooperative, or some evidence of negative attitude but not pronounced, i.e., sullen and withdrawn. |
| Positive | Acceptance of treatment, at times cautious, willingness to comply with the dentist, at times with reservation, but follows the dentist’s directions cooperatively. |
| Definitely positive | Good rapport with the dentist, interested in the dental procedure, laughing, and enjoying the situation. |
| Characteristics | Negative | Positive | Definitely Positive | Total | |
|---|---|---|---|---|---|
| Sex n (%) | |||||
| Girls | 2 (15.4) | 3 (23.1) | 3 (23.1) | 8 (61.5) | |
| Boys | 3 (23.1) | 1 (7.7) | 1 (7.7) | 5 (38.5) | |
| Treatment with visual passive distractive crocodile case device for carpule | |||||
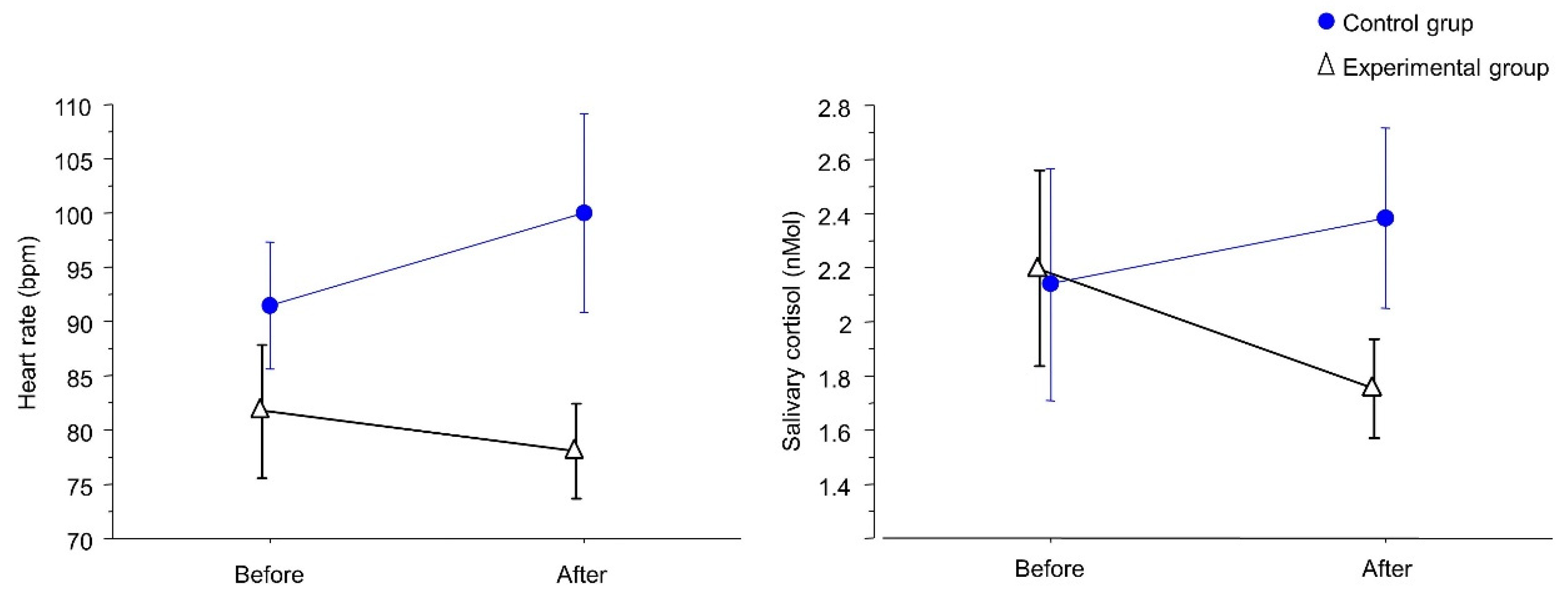
| Before the procedure | Heart rate Mean (SD) | 95 (19.8) | 78 (18.9) | 58.5 (42.3) | 81.8 (18.5) |
| Min.–Max. | 81–109 | 51–93 | 55–92 | 51–109 | |
| Salivary cortisol Mean (SD) | 2.7 (1.7) | 2.1 (1.3) | 1.5 (0) | 2.0 (1.1) | |
| Min.–Max. | 1.5–3.9 | 1.5–4 | 1.5–1.5 | 1.5–4 | |
| After the procedure | Heart rate Mean (SD) | 75 (15.6) | 76 (11) | 62.3 (44) | 78.1 (13) |
| Min.–Max. | 64–86 | 62–87 | 63–97 | 62–97 | |
| Salivary cortisol Mean (SD) | 2.2 (1.2) | 1.5 (0.2) | 1.4 (0.1) | 1.6 (0.5) | |
| Min.–Max. | 1.3–3 | 1.2–1.7 | 1.3–1.5 | 1.2–3 | |
| Treatment with normal carpule | |||||
| Before the procedure | Heart rate Mean (SD) | 100.3 (27.1) | 92.5 (14.8) | 81.5 (16.9) | 91.4 (20.1) |
| Min.–Max. | 62–120 | 81–112 | 61–102 | 61–120 | |
| Salivary cortisol Mean (SD) | 2.9 (2.4) | 1.9 (0.7) | 1.5 (0) | 2.1 (1.6) | |
| Min.–Max. | 1.5–7 | 1.5–2.9 | 1.5–1.5 | 1.5–7 | |
| After the procedure | Heart rate Mean (SD) | 116.8 (47.9) | 97 (25.3) | 86.3 (10.7) | 100 (31.7) |
| Min.–Max. | 60–177 | 61–116 | 73–99 | 60–177 | |
| Salivary cortisol Mean (SD) | 2.5 (1.3) | 2.1 (0.9) | 2.6 (1.6) | 2.4 (1.2) | |
| Min.–Max. | 1.5–4.9 | 1.5–3.4 | 1.5–4.9 | 1.5–4.9 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barbosa, N.B.; Rodrigues, B.R.; Madalena, I.R.; de Menezes, F.C.H.; Lepri, C.P.; de Oliveira, M.B.C.R.; Campos, M.G.D.; Oliveira, M.A.H.d.M. Effect of the Case for Carpule as a Visual Passive Distraction Tool on Dental Fear and Anxiety: A Pilot Study. Int. J. Environ. Res. Public Health 2023, 20, 1793. https://doi.org/10.3390/ijerph20031793
Barbosa NB, Rodrigues BR, Madalena IR, de Menezes FCH, Lepri CP, de Oliveira MBCR, Campos MGD, Oliveira MAHdM. Effect of the Case for Carpule as a Visual Passive Distraction Tool on Dental Fear and Anxiety: A Pilot Study. International Journal of Environmental Research and Public Health. 2023; 20(3):1793. https://doi.org/10.3390/ijerph20031793
Chicago/Turabian StyleBarbosa, Nayara Bertoldo, Bárbara Rocha Rodrigues, Isabela Ribeiro Madalena, Fernando Carlos Hueb de Menezes, César Penazzo Lepri, Maria Beatriz Carvalho Ribeiro de Oliveira, Michelle Gomides Dumont Campos, and Maria Angélica Hueb de Menezes Oliveira. 2023. "Effect of the Case for Carpule as a Visual Passive Distraction Tool on Dental Fear and Anxiety: A Pilot Study" International Journal of Environmental Research and Public Health 20, no. 3: 1793. https://doi.org/10.3390/ijerph20031793
APA StyleBarbosa, N. B., Rodrigues, B. R., Madalena, I. R., de Menezes, F. C. H., Lepri, C. P., de Oliveira, M. B. C. R., Campos, M. G. D., & Oliveira, M. A. H. d. M. (2023). Effect of the Case for Carpule as a Visual Passive Distraction Tool on Dental Fear and Anxiety: A Pilot Study. International Journal of Environmental Research and Public Health, 20(3), 1793. https://doi.org/10.3390/ijerph20031793






