Prevalence of Anemia among Children and Adolescents of Bangladesh: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Methods
2.1. Eligibility Criteria
2.2. Search Strategy
2.3. Study Selection
2.4. Definitions and Data Extraction
2.5. Quality Assessment
2.6. Data Analyses
2.7. Subgroup and Sensitivity Analyses
3. Results
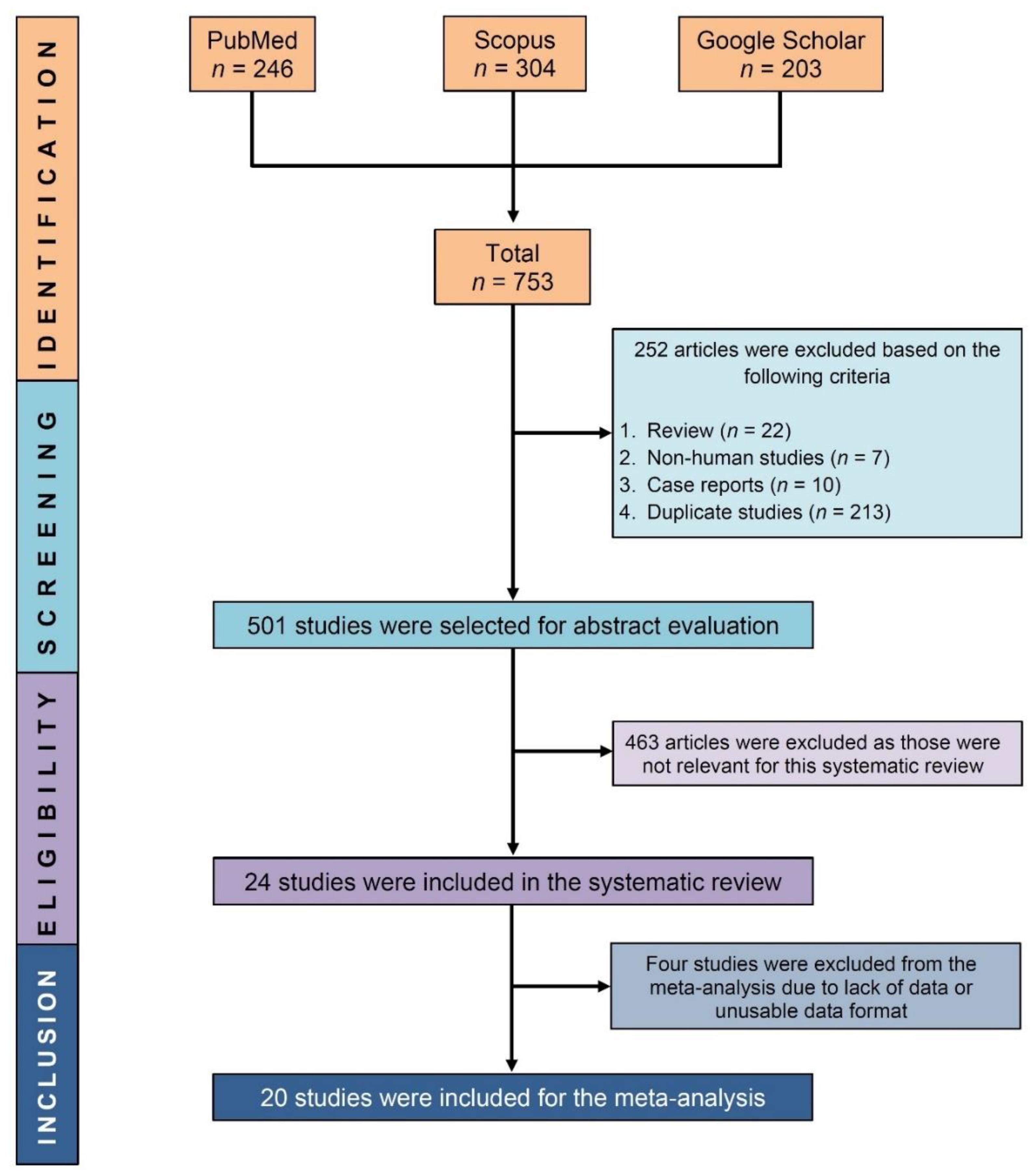
3.1. Study Selection
3.2. Study Characteristics
3.3. Quality Assessment
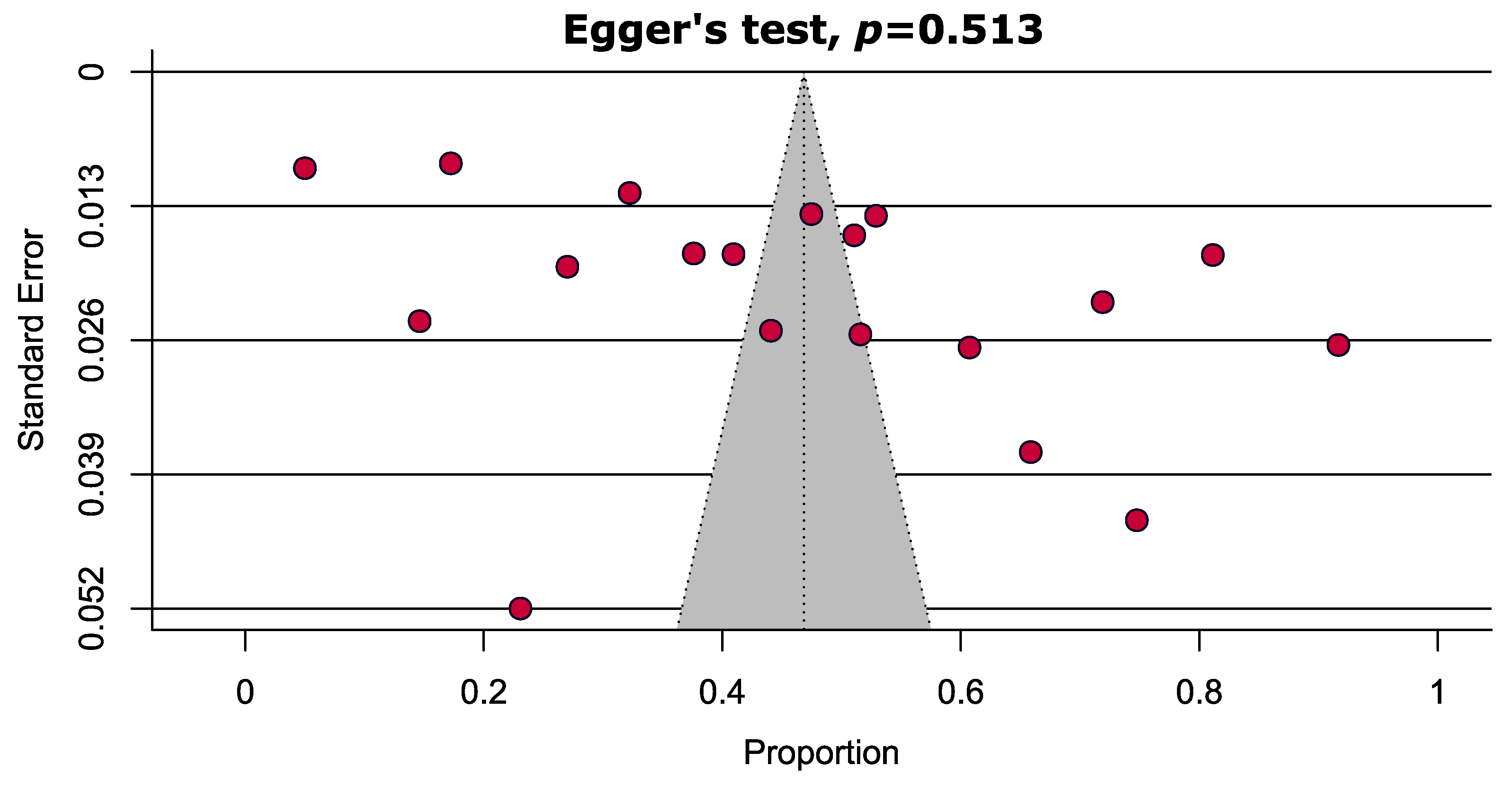
3.4. Outcomes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tvedten, H. Classification and laboratory evaluation of anemia. Schalm’s Vet. Hematol. 2022, 198–208. [Google Scholar] [CrossRef]
- Kumar, S.B.; Arnipalli, S.R.; Mehta, P.; Carrau, S.; Ziouzenkova, O. Iron Deficiency Anemia: Efficacy and Limitations of Nutritional and Comprehensive Mitigation Strategies. Nutrients 2022, 14, 2976. [Google Scholar] [CrossRef]
- Moscheo, C.; Licciardello, M.; Samperi, P.; La Spina, M.; Di Cataldo, A.; Russo, G. New Insights into Iron Deficiency Anemia in Children: A Practical Review. Metabolites 2022, 12, 289. [Google Scholar] [CrossRef]
- WHO. The Global Prevalence of Anaemia in 2011; World Health Organization: Geneva, Switzerland, 2015.
- Allali, S.; Brousse, V.; Sacri, A.-S.; Chalumeau, M.; de Montalembert, M. Anemia in children: Prevalence, causes, diagnostic work-up, and long-term consequences. Expert Rev. Hematol. 2017, 10, 1023–1028. [Google Scholar] [CrossRef] [PubMed]
- Chaparro, C.M.; Suchdev, P.S. Anemia epidemiology, pathophysiology, and etiology in low-and middle-income countries. Ann. N. Y. Acad. Sci. 2019, 1450, 15–31. [Google Scholar] [CrossRef] [PubMed]
- Weiss, G.; Goodnough, L.T. Anemia of chronic disease. N. Engl. J. Med. 2005, 352, 1011–1023. [Google Scholar] [CrossRef] [PubMed]
- Yang, F.; Liu, X.; Zha, P. Trends in socioeconomic inequalities and prevalence of anemia among children and nonpregnant women in low-and middle-income countries. JAMA 2018, 1, e182899. [Google Scholar] [CrossRef]
- Balarajan, Y.; Ramakrishnan, U.; Özaltin, E.; Shankar, A.H.; Subramanian, S. Anaemia in low-income and middle-income countries. Lancet 2011, 378, 2123–2135. [Google Scholar] [CrossRef]
- Baranwal, A.; Baranwal, A.; Roy, N. Association of household environment and prevalence of anemia among children under-5 in India. Front. Public Health 2014, 2, 196. [Google Scholar] [CrossRef]
- de Andrade Cairo, R.C.; Silva, L.R.; Bustani, N.C.; Marques, C.D.F. Iron deficiency anemia in adolescents; a literature review. Nutr. Hosp. 2014, 29, 1240–1249. [Google Scholar]
- Balcı, Y.I.; Karabulut, A.; Gürses, D.; Çövüt, İ.E. Prevalence and risk factors of anemia among adolescents in Denizli, Turkey. Iran. J. Pediatr. 2012, 22, 77–81. [Google Scholar]
- Le, C.H.H. The prevalence of anemia and moderate-severe anemia in the US population (NHANES 2003–2012). PLoS ONE 2016, 11, e0166635. [Google Scholar]
- Milman, N. Anemia—Still a major health problem in many parts of the world! Ann. Hematol. 2011, 90, 369–377. [Google Scholar] [CrossRef] [PubMed]
- Akbari, M.; Moosazadeh, M.; Tabrizi, R.; Khatibi, S.R.; Khodadost, M.; Heydari, S.T.; Tahami, A.N.; Lankarani, K.B. Estimation of iron deficiency anemia in Iranian children and adolescents: A systematic review and meta-analysis. Hematology 2017, 22, 231–239. [Google Scholar] [CrossRef] [PubMed]
- Chalise, B.; Aryal, K.K.; Mehta, R.K.; Dhimal, M.; Sapkota, F.; Mehata, S.; Karki, K.B.; Madjdian, D.; Patton, G.; Sawyer, S. Prevalence and correlates of anemia among adolescents in Nepal: Findings from a nationally representative cross-sectional survey. PLoS ONE 2018, 13, e0208878. [Google Scholar] [CrossRef]
- Sumarlan, E.S.; Windiastuti, E.; Gunardi, H. Iron status, prevalence and risk factors of iron deficiency anemia among 12-to 15-year-old adolescent girls from different socioeconomic status in Indonesia. Makara J. Health Res. 2018, 22, 46–52. [Google Scholar] [CrossRef]
- Rosado, J.L.; González, K.E.; del C Caamaño, M.; García, O.P.; Preciado, R.; Odio, M. Efficacy of different strategies to treat anemia in children: A randomized clinical trial. Nutr. J. 2010, 9, 40. [Google Scholar] [CrossRef]
- Aggarwal, A.; Aggarwal, A.; Goyal, S.; Aggarwal, S. Iron-deficiency anemia among adolescents: A global public health concern. Int. J. Adv. Community Med. 2020, 3, 35–40. [Google Scholar] [CrossRef]
- Hussain, D.A.; Arefin, M.; Hussain, B.; Sarker, A. Prevalence of Iron Deficiency Anemia and its Biochemical Parameters among the Selected School-going Under-priviledged Children in Dhaka City. J. Med. 2013, 14, 130–134. [Google Scholar] [CrossRef]
- Ahmed, F.; Khan, M.; Islam, M.; Kabir, I.; Fuchs, G.J. Anaemia and iron deficiency among adolescent schoolgirls in peri-urban Bangladesh. Eur. J. Clin. Nutr. 2000, 54, 678–683. [Google Scholar] [CrossRef]
- Islam, M.A.; Alam, S.S.; Kundu, S.; Hossan, T.; Kamal, M.A.; Cavestro, C. Prevalence of Headache in Patients With Coronavirus Disease 2019 (COVID-19): A Systematic Review and Meta-Analysis of 14,275 Patients. Front. Neurol. 2020, 11, 562634. [Google Scholar] [CrossRef] [PubMed]
- Hajissa, K.; Islam, M.A.; Hassan, S.A.; Zaidah, A.R.; Ismail, N.; Mohamed, Z. Seroprevalence of SARS-CoV-2 Antibodies in Africa: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 7257. [Google Scholar] [CrossRef]
- Viechtbauer, W. Conducting meta-analyses in R with the metafor package. J. Stat. Softw. 2010, 36, 1–48. [Google Scholar] [CrossRef]
- Adams, A.M.; Ahmed, R.; Latif, A.M.; Rasheed, S.; Das, S.K.; Hasib, E.; Farzana, F.D.; Ferdous, F.; Ahmed, S.; Faruque, A. Impact of fortified biscuits on micronutrient deficiencies among primary school children in Bangladesh. PLoS ONE 2017, 12, e0174673. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, F.; Hasan, N.; Kabir, Y. Vitamin A deficiency among adolescent female garment factory workers in Bangladesh. Eur. J. Clin. Nutr. 1997, 51, 698–702. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, F.; Rahman, A.; Noor, A.N.; Akhtaruzzaman, M.; Hughes, R. Anaemia and vitamin A status among adolescent schoolboys in Dhaka City, Bangladesh. Public Health Nutr. 2006, 9, 345–350. [Google Scholar] [CrossRef]
- Ahmed, F.; Khan, M.; Banu, C.; Qazi, M.; Akhtaruzzaman, M. The coexistence of other micronutrient deficiencies in anaemic adolescent schoolgirls in rural Bangladesh. Eur. J. Clin. Nutr. 2008, 62, 365–372. [Google Scholar] [CrossRef]
- Banu, H.; Khanum, H.; Hossain, M.A. Relationships between anaemia and parasitic infections in adolescent girls of Bangladesh. Bangladesh J. Zool. 2014, 42, 91–103. [Google Scholar] [CrossRef]
- Bhargava, A.; Bouis, H.E.; Hallman, K.; Hoque, B.A. Coliforms in the water and hemoglobin concentration are predictors of gastrointestinal morbidity of Bangladeshi children ages 1–10 years. Am. J. Hum. Biol. 2003, 15, 209–219. [Google Scholar] [CrossRef]
- Faruque, A.S.; Khan, A.; Malek, M.A.; Huq, S.; Wahed, M.A.; Salam, M.A.; Fuchs, G.J.; Khaled, M.A. Childhood anemia and vitamin A deficiency in rural Bangladesh. Southeast Asian J. Trop. Med. Public Health 2006, 37, 771–777. [Google Scholar]
- Goto, R.; Devine, J.; Mascie-Taylor, C.N.; Ormand, J.; Jufry, A.J. The impact of an income-generating activities programme on children and mothers’ undernutrition in extreme poor rural Bangladeshi households. Public Health Nutr. 2019, 22, 3073–3082. [Google Scholar] [CrossRef] [PubMed]
- Hoque, M.; Ahmed, A.; Quaderi, H. Prevalence and Risk Factors of Iron Deficiency Anaemia in Children admitted in a Tertiary Care Hospital of Bangladesh. J. Nepal Paediatr. Soc. 2015, 35, 38–43. [Google Scholar] [CrossRef]
- Kabir, Y.; Shahjalal, H.M.; Saleh, F.; Obaid, W. Dietary pattern, nutritional status, anaemia and anaemia-related knowledge in urban adolescent college girls of Bangladesh. J. Pak. Med. Assoc. 2010, 60, 633–638. [Google Scholar] [PubMed]
- Kalter, H.; Burnham, G.; Kolstad, P.; Hossain, M.; Schillinger, J.; Khan, N.; Saha, S.; De Wit, V.; Kenya-Mugisha, N.; Schwartz, B. Evaluation of clinical signs to diagnose anaemia in Uganda and Bangladesh, in areas with and without malaria. Bull. WHO 1997, 75, 103. [Google Scholar] [PubMed]
- Mahfuz, M.; Murray-Kolb, L.E.; Hasan, S.; Das, S.; Fahim, S.M.; Alam, M.A.; Caulfield, L.; Ahmed, T. Why do children in slums suffer from anemia, iron, zinc, and vitamin A deficiency? Results from a birth cohort study in Dhaka. Nutrients 2019, 11, 3025. [Google Scholar] [CrossRef] [PubMed]
- Mannan, T.; Ahmed, S.; Akhtar, E.; Roy, A.K.; Haq, M.A.; Roy, A.; Kippler, M.; Ekström, E.-C.; Wagatsuma, Y.; Raqib, R. Maternal micronutrient supplementation and long term health impact in children in rural Bangladesh. PLoS ONE 2016, 11, e0161294. [Google Scholar]
- Miah, M.S.; Rahman, N.; Prodhan, U.; Linkon, M.; Rahman, S. Prevalence of iron deficiency anemia among adolescent girls and its risk factors in tangail region of Bangladesh. Int. J. Res. Eng. Technol. 2014, 3, 613–619. [Google Scholar]
- Mistry, S.K.; Jhohura, F.T.; Khanam, F.; Akter, F.; Khan, S.; Yunus, F.M.; Hossain, M.B.; Afsana, K.; Haque, M.R.; Rahman, M. An outline of anemia among adolescent girls in Bangladesh: Findings from a cross-sectional study. BMC Hematol. 2017, 17, 13. [Google Scholar] [CrossRef]
- Persson, V.; Ahmed, F.; Gebre-Medhin, M.; Greiner, T. Relationships between vitamin A, iron status and helminthiasis in Bangladeshi school children. Public Health Nutr. 2000, 3, 83–89. [Google Scholar] [CrossRef]
- Harun-Or-Rashid, M.; Khatun, U.F.; Yoshida, Y.; Morita, S.; Chowdhury, N.; Sakamoto, J. Iron and iodine deficiencies among under-2 children, adolescent girls, and pregnant women of Bangladesh: Association with common diseases. Nagoya J. Med. Sci. 2009, 71, 39–49. [Google Scholar]
- Saha, S.; Farzana, S.; Begum, A. Dietary pattern and anaemia among female adolescent garment workers in Bangladesh. Acta Medica Int. 2014, 1, 103–106. [Google Scholar] [CrossRef]
- Shahabuddin, A.; Talukder, K.; Talukder, M.-K.; Hassan, M.; Seal, A.; Rahman, Q.; Mannan, A.; Tomkins, A.; Costello, A. Adolescent nutrition in a rural community in Bangladesh. Indian J. Pediatr. 2000, 67, 93–98. [Google Scholar] [CrossRef] [PubMed]
- Shakur, Y.A.; Choudhury, N.; Hyder, S.Z.; Zlotkin, S.H. Unexpectedly high early prevalence of anaemia in 6-month-old breast-fed infants in rural Bangladesh. Public Health Nutr. 2010, 13, 4–11. [Google Scholar] [CrossRef]
- Uddin, M.; Sardar, M.; Hossain, M.; Alam, M.; Bhuya, M.; Uddin, M.; Rahman, M. Prevalence of anaemia in children of 6 months to 59 months in Narayanganj, Bangladesh. J. Dhaka Med. Coll. 2010, 19, 126–130. [Google Scholar] [CrossRef]
- Wendt, A.S.; Waid, J.L.; Gabrysch, S. Dietary factors moderate the relation between groundwater iron and anemia in women and children in rural Bangladesh. Curr. Dev. Nutr. 2019, 3, nzz093. [Google Scholar] [CrossRef] [PubMed]
- Afroja, S.; Kabir, M.R.; Islam, M.A. Analysis of determinants of severity levels of childhood anemia in Bangladesh using a proportional odds model. Clin. Epidemiol. Glob. Health 2020, 8, 175–180. [Google Scholar] [CrossRef]
- Ali, M.; Amin, M.; Jarl, J.; Chisholm, N.; Saha, S. Maternal health status and household food security on determining childhood anemia in Bangladesh-a nationwide cross-sectional study. BMC Public Health 2021, 21, 1581. [Google Scholar] [CrossRef] [PubMed]
- Stevens, G.A.; Finucane, M.M.; De-Regil, L.M.; Paciorek, C.J.; Flaxman, S.R.; Branca, F.; Peña-Rosas, J.P.; Bhutta, Z.A.; Ezzati, M.; Group, N.I.M.S. Global, regional, and national trends in haemoglobin concentration and prevalence of total and severe anaemia in children and pregnant and non-pregnant women for 1995–2011: A systematic analysis of population-representative data. Lancet Glob. Health 2013, 1, e16–e25. [Google Scholar] [CrossRef]
- WHO. Global Nutrition Targets 2025: Policy Brief Series. 2014. Available online: https://www.who.int/publications/i/item/WHO-NMH-NHD-14.2 (accessed on 24 July 2022).
- Onyeneho, N.G.; Ozumba, B.C.; Subramanian, S. Determinants of childhood anemia in India. Sci. Rep. 2019, 9, 16540. [Google Scholar] [CrossRef]
- Khan, J.R.; Awan, N.; Misu, F. Determinants of anemia among 6–59 months aged children in Bangladesh: Evidence from nationally representative data. BMC Pediatr. 2016, 16, 3. [Google Scholar] [CrossRef]
- Gebrie, A.; Alebel, A. A systematic review and meta-analysis of the prevalence and predictors of anemia among children in Ethiopia. Afr. Health Sci. 2020, 20, 2007–2021. [Google Scholar] [CrossRef] [PubMed]
- Woldie, H.; Kebede, Y.; Tariku, A. Factors associated with anemia among children aged 6–23 months attending growth monitoring at Tsitsika Health Center, Wag-Himra Zone, Northeast Ethiopia. J. Nutr. Metab. 2015, 2015, 928632. [Google Scholar] [CrossRef] [PubMed]
- Tezera, R.; Sahile, Z.; Yilma, D.; Misganaw, E.; Mulu, E. Prevalence of anemia among school-age children in Ethiopia: A systematic review and meta-analysis. Syst. Rev. 2018, 7, 80. [Google Scholar] [CrossRef] [PubMed]
- Tariku, E.Z.; Abebe, G.A.; Melketsedik, Z.A.; Gutema, B.T.; Megersa, N.D.; Sorrie, M.B.; Weldehawariat, F.G.; Getahun, E.A. Anemia and its associated factors among school-age children living in different climatic zones of Arba Minch Zuria District, Southern Ethiopia. BMC Hematol. 2019, 19, 6. [Google Scholar] [CrossRef]
- Le, H.T.; Brouwer, I.D.; Verhoef, H.; Nguyen, K.C.; Kok, F.J. Anemia and intestinal parasite infection in school children in rural Vietnam. Asia Pac. J. Clin. Nutr. 2007, 16, 716–723. [Google Scholar]
- Rahman, A.S.; Sarker, S.A.; Ahmed, T.; Islam, R.; Wahed, M.A.; Sack, D.A. Relationship of intestinal parasites, H. pylori infection with anemia or iron status among school age children in rural Bangladesh. J. Gastroenterol. Hepatol. Res. 2013, 2, 769–773. [Google Scholar]
- Muthayya, S.; Thankachan, P.; Zimmermann, M.B.; Andersson, M.; Eilander, A.; Misquith, D.; Hurrell, R.F.; Kurpad, A.V. Low anemia prevalence in school-aged children in Bangalore, South India: Possible effect of school health initiatives. Eur. J. Clin. Nutr. 2007, 61, 865–869. [Google Scholar] [CrossRef]
- Mantadakis, E.; Chatzimichael, E.; Zikidou, P. Iron deficiency anemia in children residing in high and low-income countries: Risk factors, prevention, diagnosis and therapy. Mediterr. J. Hematol. Infect. Dis. 2020, 12, e2020041. [Google Scholar] [CrossRef]
- Black, R.E.; Victora, C.G.; Walker, S.P.; Bhutta, Z.A.; Christian, P.; De Onis, M.; Ezzati, M.; Grantham-McGregor, S.; Katz, J.; Martorell, R. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013, 382, 427–451. [Google Scholar] [CrossRef]
- Sundararajan, S.; Rabe, H. Prevention of iron deficiency anemia in infants and toddlers. Pediatr. Res. 2021, 89, 63–73. [Google Scholar] [CrossRef]
- Salam, R.A.; MacPhail, C.; Das, J.K.; Bhutta, Z.A. Effectiveness of micronutrient powders (MNP) in women and children. BMC Public Health 2013, 13, S22. [Google Scholar] [CrossRef]
- Pinhas-Hamiel, O.; Newfield, R.; Koren, I.; Agmon, A.; Lilos, P.; Phillip, M. Greater prevalence of iron deficiency in overweight and obese children and adolescents. Int. J. Obes. 2003, 27, 416–418. [Google Scholar] [CrossRef]
- Nazari, M.; Mohammadnejad, E.; Dalvand, S.; Gheshlagh, R.G. Prevalence of iron deficiency anemia in Iranian children under 6 years of age: A systematic review and meta-analysis. J. Blood Med. 2019, 10, 111. [Google Scholar] [CrossRef] [PubMed]
- Ferrara, M.; Coppola, L.; Coppola, A.; Capozzi, L. Iron deficiency in childhood and adolescence: Retrospective review. Hematology 2006, 11, 183–186. [Google Scholar] [CrossRef] [PubMed]
- Massey, A.C. Microcytic anemia. Differential diagnosis and management of iron deficiency anemia. Med. Clin. N. Am. 1992, 76, 549–566. [Google Scholar] [CrossRef]
- Chen, M.-H.; Su, T.-P.; Chen, Y.-S.; Hsu, J.-W.; Huang, K.-L.; Chang, W.-H.; Chen, T.-J.; Bai, Y.-M. Association between psychiatric disorders and iron deficiency anemia among children and adolescents: A nationwide population-based study. BMC Psychiatry 2013, 13, 161. [Google Scholar] [CrossRef]
- Muoneke, V.U.; Ibekwe, R.C.; Nebe-Agumadu, H.U.; Ibe, B.C. Factors associated with mortality in under-five children with severe anemia in Ebonyi, Nigeria. Indian Pediatr. 2012, 49, 119–123. [Google Scholar] [CrossRef]
- Otieno, R.O.; Ouma, C.; Ong’echa, J.M.; Keller, C.C.; Were, T.; Waindi, E.N.; Michaels, M.G.; Day, R.D.; Vulule, J.M.; Perkins, D.J. Increased severe anemia in HIV-1-exposed and HIV-1-positive infants and children during acute malaria. AIDS 2006, 20, 275–280. [Google Scholar] [CrossRef]
- Cooke, A.G.; McCavit, T.L.; Buchanan, G.R.; Powers, J.M. Iron deficiency anemia in adolescents who present with heavy menstrual bleeding. J. Pediatr. Adolesc. Gynecol. 2017, 30, 247–250. [Google Scholar] [CrossRef]
- Chandrakumari, A.S.; Sinha, P.; Singaravelu, S.; Jaikumar, S. Prevalence of anemia among adolescent girls in a rural area of Tamil Nadu, India. J. Fam. Med. Prim. Care 2019, 8, 1414. [Google Scholar] [CrossRef]
- Habib, N.; Abbasi, S.-U.-R.S.; Aziz, W. An analysis of societal determinant of anemia among adolescent girls in Azad Jammu and Kashmir, Pakistan. Anemia 2020, 2020, 1628357. [Google Scholar] [CrossRef] [PubMed]
- Gardner, W.; Kassebaum, N. Global, regional, and national prevalence of anemia and its causes in 204 countries and territories, 1990–2019. Curr. Dev. Nutr. 2020, 4, 830. [Google Scholar] [CrossRef]
- Habtegiorgis, S.D.; Petrucka, P.; Telayneh, A.T.; Getahun, D.S.; Getacher, L.; Alemu, S.; Birhanu, M.Y. Prevalence and associated factors of anemia among adolescent girls in Ethiopia: A systematic review and meta-analysis. PLoS ONE 2022, 17, e0264063. [Google Scholar] [CrossRef] [PubMed]


| Study ID [References] | Study Design | Location | Patient Enrollment Time | Total Number of Hb Level Examined Patients (Girls) | Age (Range/Mean ± SD) | Hb Level Measurement Methods | Hb Concentration (Mean ± SD) (g/L) | Cut Off Value for Hb Concentration(g/L) |
|---|---|---|---|---|---|---|---|---|
| Adams 2017 [25] | Cohort | NR | September 2011 to November 2012 | 368 (171) | 6 to 11 years | NR | 124.4 ± 8.7 | 115 |
| Ahmed 1997 [26] | Cross-sectional | Dhaka | December 1995 to January 1996 | 388 (388) | 12 to 19 years | CMH method | 119.7 ± 14.0 | 120 |
| Ahmed 2000 [21] | Cross-sectional | Dhaka | September to November 1996 | 548 (548) | 14.2 ± 1.3 years | CMH method | 125.6 ± 11.6 | 120 |
| Ahmed 2006 [27] | Cross-sectional | Dhaka | September to October 2000 | 381 (381) | 11 to 16 years | CMH method | 142.6 ± 13.2 | 11 years: 115 12–14 years: 120 15–16 years: 130 |
| Ahmed 2008 [28] | Cross-sectional | Dhaka | March to May 2003 | 1800 (NR) | 14 to 18 years | Using HA and CMH method | NR | 120 |
| Banu 2014 [29] | Cross-sectional | Dhaka | June 2006 to May 2009 | 1570 (1570) | 10 to 19 years | Sahli’s method | NR | 120 |
| Bhargava 2003 [30] | Cross-sectional | Manikganj | June 1999 to May 2000 | 99 (60) | 1 to 10 years | Using HA | 115.3 ± 10.8 | 120 |
| Faruque 2006 [31] | Cross-sectional | NR | October 1997 to December 1999 | 1302 (642) | 24 to 72 months | CMH method | 110.0 ±11.0 | 110 |
| Goto 2019 [32] | Cohort | NR | 2008 to 2016 | 382 (NR) | <5 years | Using HA | NR | 110 |
| Hoque 2015 [33] | Cross-sectional | Dhaka | June to August 2010 | 331 (126) | 6 to 36 months | Using HA | NR | 110 |
| Hussain 2013 [20] | Cross-sectional | Dhaka | July 2011 to June 2012 | 164 (NR) | 10 to 18 years | NR | 108.0 ± 7.0 | 120 |
| Kabir 2010 [34] | Cross-sectional | Dhaka | NR | 65 (65) | 15 to 19 years | Using commercial kits | 128.0 ± 16.0 | 120 |
| Kalter 1997 [35] | Cross-sectional | Dhaka | September 1994 to February 1995 | 482 (223) | 2–60 months | Using HA | 95.0 ± 19.0 | 110 |
| Mahfuz 2019 [36] | Cohort | Dhaka | February 2010 to February 2017 | 212 (111) | 5 years | Using HA | NR | 110 |
| Mannan 2016 [37] | Cohort | Dhaka | November 2001 to October 2003 | 540 (NR) | 4.5 years | Using HA | 128.6 ± 13.3 | 110 |
| Miah 2014 [38] | Cross-sectional | Tangail | NR | 120 (120) | 12 to 17 years | Sahli’s method | NR | 120 |
| Mistry 2017 [39] | Cross-sectional | NR | October 2015 to January 2016 | 1269 (1269) | 10 to 19 years | Using HA | 118.2 ± 11.5 | 120 |
| Persson 2000 [40] | Cross-sectional | Panchargarh and Thakurgaon | March to May 1998 | 164 (87) | 6 to 12 years | Using HA | 121.0 ± 10.0 | 115 |
| Rashid 2009 [41] | Cross-sectional | Cumilla | September to December 2005 | 750 (553) | 14.2 ± 3.2 years | Using HA | 118.0 ± 15.9 | Children: 110 Adolescent: 120 |
| Saha 2014 [42] | Cross-sectional | Gazipur | March to June 2008 | 108 (108) | 18 to 19 years | Hemoglobin color scale method | NR | 120 |
| Shahabuddin 2000 [43] | Cross-sectional | Narayanganj | 1995 | 861 (456) | 10 to 17 years | CMH method | NR | Male (10–15 years): 120 Male (15–19 years): 130 Female (10–15 years: 115 Female (15–19 years): 120 |
| Shakur 2009 [44] | Cross-sectional | Gazipur | March 2005 to April 2007 | 402 (197) | 6 months | Using HA | 102.3 ± 12.4 | 110 |
| Uddin 2010 [45] | Cross-sectional | Narayanganj | January to June 2010 | 767 (377) | 6 to 59 months | Sahli’s method | 109.0 ± 16.0 | 110 |
| Wendt 2019 [46] | Cross-sectional | Sylhet | March to May 2015 | 987 (NR) | 6 to 36 months | Using HA | 108.0 ± 13.0 | 110 |
| Subgroups | Pooled Prevalence [95% CIs] (%) | Number of Studies Analyzed | Total Number of Patients | Heterogeneity | ||
|---|---|---|---|---|---|---|
| I2 | p-Value | |||||
| Anemia | 6 months–2 years | 61.0 [47.9–74.2] | 3 | 1163 | 96% | <0.0001 |
| 6 months–5 years | 47.3 [27.0–67.7] | 9 | 4498 | 100% | <0.0001 | |
| 6 months–10 years | 50.8 [34.6–66.9] | 12 | 6095 | 100% | <0.0001 | |
| 10–19 years | 42.1 [28.5–55.7] | 9 | 6267 | 99% | <0.0001 | |
| Iron deficiency anemia | 6 months–5 years | 18.1 [14.0–22.3] | 1 | 331 | NA | NA |
| 10–19 years | 12.5 [5.9–19.1] | 4 | 2134 | 95% | <0.0001 | |
| Severe anemia | 6 months–19 years | 0.7 [0.1–1.4] | 7 | 4110 | 86% | <0.0001 |
| 6 months–2 years | 1.0 [0.0–2.0] | 1 | 402 | NA | NA | |
| 6 months–5 years | 0.7 [0.3–1.2] | 3 | 1720 | 0% | 0.56 | |
| 10–19 years | 0.6 [0.0–1.8] | 4 | 2390 | 92% | <0.0001 | |
| Non- severe anemia | 6 months–19 years | 56.4 [39.6–73.1] | 7 | 4110 | 99% | <0.0001 |
| 6 months–2 years | 70.9 [66.5–75.3] | 1 | 402 | NA | NA | |
| 6 months–5 years | 60.2 [47.5–73.0] | 3 | 1720 | 96% | <0.0001 | |
| 10–19 years | 53.5 [26.2–80.8] | 4 | 2390 | 99% | <0.0001 | |
| Anemia (Female) | 6 months–10 years | 48.2 [35.9–50.5] | 3 | 1145 | 100% | <0.0001 |
| 10–19 years | 42.3 [27.7–57.0] | 7 | 4303 | 99% | <0.0001 | |
| Anemia (Male) | 6 months–10 years | 50.4 [42.9–57.9] | 3 | 1255 | 100% | <0.0001 |
| Strategies of Sensitivity Analyses | Prevalence of Anemia (95% CIs) (%) | Difference of Pooled Prevalence Compared to the Main Result | Number of Studies Analyzed | Total Number Patients | Heterogeneity | |
|---|---|---|---|---|---|---|
| I2 | p-Value | |||||
| Prevalence of anemia | ||||||
| Excluding small studies (n < 200) | 42.3 [31.0–53.7] | 4.5% lower | 15 | 11,730 | 100% | <0.0001 |
| Excluding low- and moderate-quality studies | 47.1 [34.9–59.2] | 0.3% higher | 16 | 10,635 | 100% | <0.0001 |
| Excluding outlier studies | 46.7 [37.3–56.1] | 0.1% lower | 17 | 11,518 | 99% | <0.0001 |
| Prevalence of iron deficiency anemia | ||||||
| Excluding small studies (n < 200) | 15.0 [7.9–22.0] | 1.4% higher | 3 | 2181 | 95% | <0.0001 |
| Excluding low- and moderate-quality studies | 14.4 [7.1–21.7] | 0.8% higher | 3 | 999 | 89% | <0.0001 |
| Excluding outlier studies | 13.6 [8.0–19.2] | No changes | 5 | 2465 | 93% | <0.0001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kundu, S.; Alam, S.S.; Mia, M.A.-T.; Hossan, T.; Hider, P.; Khalil, M.I.; Musa, K.I.; Islam, M.A. Prevalence of Anemia among Children and Adolescents of Bangladesh: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2023, 20, 1786. https://doi.org/10.3390/ijerph20031786
Kundu S, Alam SS, Mia MA-T, Hossan T, Hider P, Khalil MI, Musa KI, Islam MA. Prevalence of Anemia among Children and Adolescents of Bangladesh: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2023; 20(3):1786. https://doi.org/10.3390/ijerph20031786
Chicago/Turabian StyleKundu, Shoumik, Sayeda Sadia Alam, Md Al-Tareq Mia, Tareq Hossan, Phil Hider, Md. Ibrahim Khalil, Kamarul Imran Musa, and Md Asiful Islam. 2023. "Prevalence of Anemia among Children and Adolescents of Bangladesh: A Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 20, no. 3: 1786. https://doi.org/10.3390/ijerph20031786
APA StyleKundu, S., Alam, S. S., Mia, M. A.-T., Hossan, T., Hider, P., Khalil, M. I., Musa, K. I., & Islam, M. A. (2023). Prevalence of Anemia among Children and Adolescents of Bangladesh: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 20(3), 1786. https://doi.org/10.3390/ijerph20031786












