Climate Change-Related Environmental Exposures and Perinatal and Maternal Health Outcomes in the U.S.
Abstract
1. Introduction
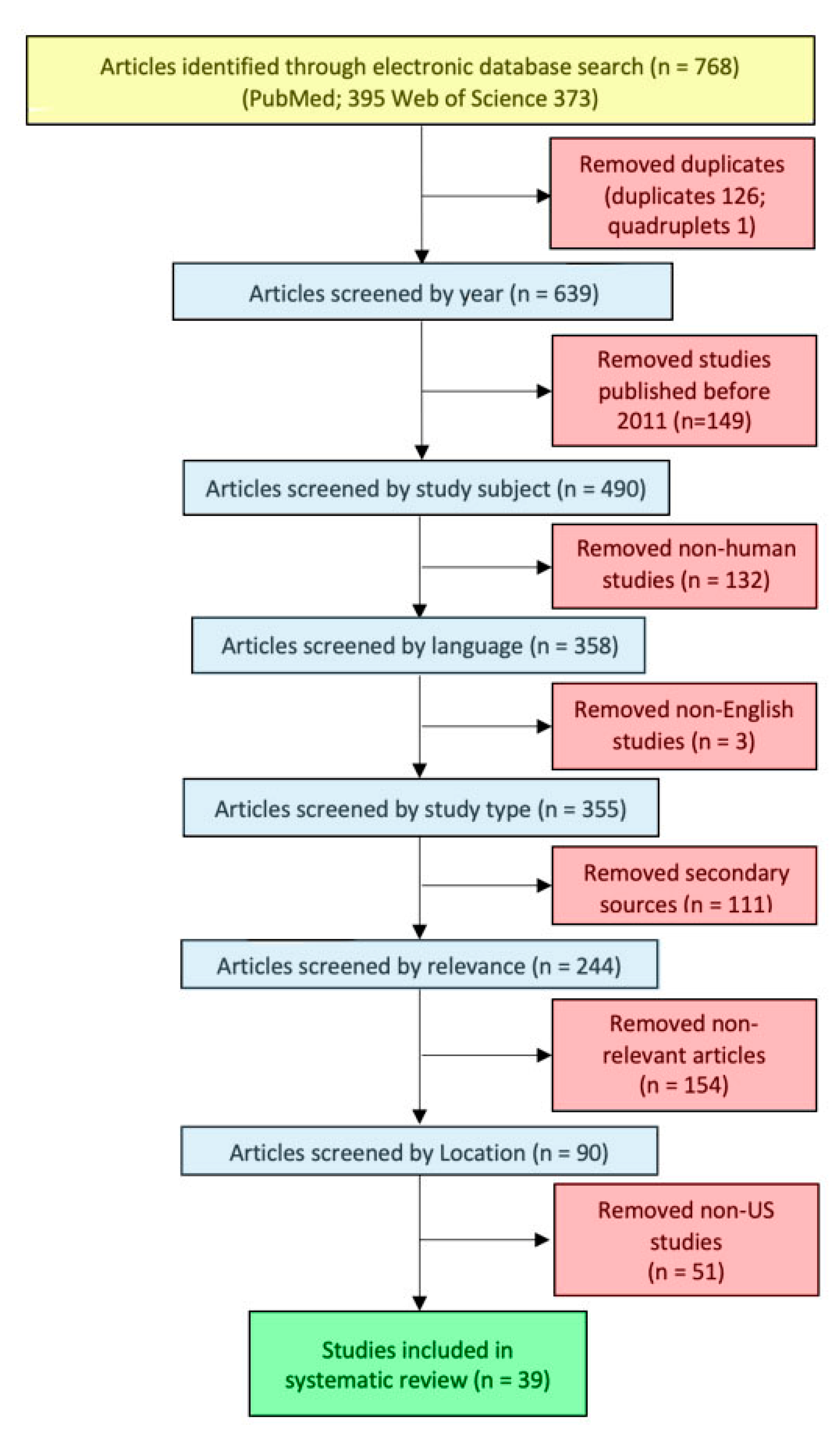
2. Design and Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Data Extraction and Analysis
3. Results
3.1. Study Characteristics and Findings
3.1.1. Extreme Temperature Exposure Studies
3.1.2. Air Pollution Exposure Studies
3.1.3. Natural Disaster Exposure Studies
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Intergovernmental Panel on Climate Change (IPCC). Global Warming of 1.5 °C. An IPCC Special Report on the Impacts of Global Warming of 1.5 °C above Pre-Industrial Levels and Related Global Greenhouse Gas Emission Pathways, in the Context of Strengthening the Global Response to the Threat of Climate Change, Sustainable Development, and Efforts to Eradicate Poverty. 2018. Available online: https://www.ipcc.ch/sr15/ (accessed on 1 June 2022).
- Intergovernmental Panel on Climate Change (IPCC). Climate Change 2021: The Physical Science Basis. Contribution of Working Group I to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change. 2021. Available online: https://www.ipcc.ch/report/sixth-assessment-report-working-group-i/ (accessed on 1 June 2022).
- Overpeck, J.T.; Udall, B. Climate change and the aridification of North America. Proc. Natl. Acad. Sci. USA 2020, 117, 11856–11858. [Google Scholar] [CrossRef]
- Intergovernmental Panel on Climate Change (IPCC). AR5 Climate Change 2014: Impacts, Adaptation, and Vulnerability. North America. Available online: https://www.ipcc.ch/report/ar5/wg2/north-america/ (accessed on 10 January 2023).
- American College of Obstetricians and Gynecologists (ACOG). Position Statement: Addressing Climate Change. 2021. Available online: https://www.acog.org/clinical-information/policy-and-position-statements/position-statements/2021/addressing-climate-change (accessed on 1 June 2022).
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gotzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef] [PubMed]
- Barreca, A.; Schaller, J. The impact of high ambient temperatures on delivery timing and gestational lengths. Nat. Clim. Chang. 2020, 10, 77–82. [Google Scholar] [CrossRef]
- Basu, R.; Sarovar, V.; Malig, B.J. Association Between High Ambient Temperature and Risk of Stillbirth in California. Am. J. Epidemiol. 2016, 183, 894–901. [Google Scholar] [CrossRef]
- Basu, R.; Rau, R.; Pearson, D.; Malig, B. Temperature and Term Low Birth Weight in California. Am. J. Epidemiol. 2018, 187, 2306–2314. [Google Scholar] [CrossRef] [PubMed]
- Cil, G.; Cameron, T.A. Potential Climate Change Health Risks from Increases in Heat Waves: Abnormal Birth Outcomes and Adverse Maternal Health Conditions. Risk Anal. 2017, 37, 2066–2079. [Google Scholar] [CrossRef]
- Ha, S.; Zhu, Y.; Liu, D.; Sherman, S.; Mendola, P. Ambient temperature and air quality in relation to small for gestational age and term low birthweight. Environ. Res. 2017, 155, 394–400. [Google Scholar] [CrossRef] [PubMed]
- Ha, S.; Liu, D.; Zhu, Y.; Soo Kim, S.; Sherman, S.; Grantz, K.L.; Mendola, P. Ambient Temperature and Stillbirth: A Multi-Center Retrospective Cohort Study. Environ. Health Perspect. 2017, 125, 067011. [Google Scholar] [CrossRef]
- Ha, S.; Nguyen, K.; Liu, D.; Mannisto, T.; Nobles, C.; Sherman, S.; Mendola, P. Ambient temperature and risk of cardiovascular events at labor and delivery: A case-crossover study. Environ. Res. 2017, 159, 622–628. [Google Scholar] [CrossRef]
- Ha, S.; Liu, D.; Zhu, Y.; Sherman, S.; Mendola, P. Acute Associations Between Outdoor Temperature and Premature Rupture of Membranes. Epidemiology 2018, 29, 175–182. [Google Scholar] [CrossRef]
- Huang, M.; Strickland, M.J.; Richards, M.; Holmes, H.A.; Newman, A.J.; Garn, J.V.; Liu, Y.; Warren, J.L.; Chang, H.H.; Darrow, L.A. Acute associations between heatwaves and preterm and early-term birth in 50 US metropolitan areas: A matched case-control study. Environ. Health 2021, 20, 47. [Google Scholar] [CrossRef] [PubMed]
- Lin, G.; Zhang, T. Examining Extreme Weather Effects on Birth Weight from the Individual Effect to Spatiotemporal Aggregation Effects. J. Agric. Biol. Environ. Stat. 2012, 17, 490–507. Available online: http://www.jstor.org/stable/41724585 (accessed on 7 May 2022). [CrossRef]
- Monteblanco, A.D.; Vanos, J.K. Community-based maternal health workers’ perspectives on heat risk and safety: A pilot qualitative study. Health Care Women Int. 2021, 42, 657–677. [Google Scholar] [CrossRef] [PubMed]
- Ngo, N.S.; Horton, R.M. Climate change and fetal health: The impacts of exposure to extreme temperatures in New York City. Environ. Res. 2016, 144 Pt A, 158–164. [Google Scholar] [CrossRef]
- Rammah, A.; Whitworth, K.W.; Han, I.; Chan, W.; Hess, J.W.; Symanski, E. Temperature, placental abruption and stillbirth. Environ. Int. 2019, 131, 105067. [Google Scholar] [CrossRef]
- Smith, M.L.; Hardeman, R.R. Association of Summer Heat Waves and the Probability of Preterm Birth in Minnesota: An Exploration of the Intersection of Race and Education. Int. J. Environ. Res. Public Health 2020, 17, 6391. [Google Scholar] [CrossRef]
- Sun, S.; Spangler, K.R.; Weinberger, K.R.; Yanosky, J.D.; Braun, J.M.; Wellenius, G.A. Ambient Temperature and Markers of Fetal Growth: A Retrospective Observational Study of 29 Million U.S. Singleton Births. Environ. Health Perspect. 2019, 127, 67005. [Google Scholar] [CrossRef]
- Sun, Y.; Ilango, S.D.; Schwarz, L.; Wang, Q.; Chen, J.C.; Lawrence, J.M.; Wu, J.; Benmarhnia, T. Examining the joint effects of heatwaves, air pollution, and green space on the risk of preterm birth in California. Environ. Res. Lett. 2020, 15, 104099. [Google Scholar] [CrossRef]
- Van Zutphen, A.R.; Hsu, W.H.; Lin, S. Extreme winter temperature and birth defects: A population-based case-control study. Environ. Res. 2014, 128, 1–8. [Google Scholar] [CrossRef]
- Yu, X.; Feric, Z.; Cordero, J.F.; Meeker, J.D.; Alshawabkeh, A. Potential influence of temperature and precipitation on preterm birth rate in Puerto Rico. Sci. Rep. 2018, 8, 16106. [Google Scholar] [CrossRef]
- Zhang, W.; Spero, T.L.; Nolte, C.G.; Garcia, V.C.; Lin, Z.; Romitti, P.A.; Shaw, G.M.; Sheridan, S.C.; Feldkamp, M.L.; Woomert, A. Projected Changes in Maternal Heat Exposure During Early Pregnancy and the Associated Congenital Heart Defect Burden in the United States. J. Am. Heart Assoc. 2019, 8, e010995. [Google Scholar] [CrossRef] [PubMed]
- Sarovar, V.; Malig, B.J.; Basu, R. A case-crossover study of short-term air pollution exposure and the risk of stillbirth in California, 1999–2009. Environ. Res. 2020, 191, 110103. [Google Scholar] [CrossRef] [PubMed]
- Antipova, A.; Curtis, A. The post-disaster negative health legacy: Pregnancy outcomes in Louisiana after Hurricane Andrew. Disasters 2015, 39, 665–686. [Google Scholar] [CrossRef]
- Brock, R.L.; O’Hara, M.W.; Hart, K.J.; McCabe, J.E.; Williamson, J.A.; Laplante, D.P.; Yu, C.; King, S. Partner support and maternal depression in the context of the Iowa floods. J. Fam. Psychol. 2014, 28, 832–843. [Google Scholar] [CrossRef] [PubMed]
- Brock, R.L.; O’Hara, M.W.; Hart, K.J.; McCabe-Beane, J.E.; Williamson, J.A.; Brunet, A.; Laplante, D.P.; Yu, C.; King, S. Peritraumatic Distress Mediates the Effect of Severity of Disaster Exposure on Perinatal Depression: The Iowa Flood Study. J. Trauma. Stress 2015, 28, 515–522. [Google Scholar] [CrossRef]
- Currie, J.; Rossin-Slater, M. Weathering the storm: Hurricanes and birth outcomes. J. Health Econ. 2013, 32, 487–503. [Google Scholar] [CrossRef]
- Giarratano, G.P.; Barcelona, V.; Savage, J.; Harville, E. Mental health and worries of pregnant women living through disaster recovery. Health Care Women Int. 2019, 40, 259–277. [Google Scholar] [CrossRef]
- Grabich, S.C.; Robinson, W.R.; Engel, S.M.; Konrad, C.E.; Richardson, D.B.; Horney, J.A. Hurricane Charley Exposure and Hazard of Preterm Delivery, Florida 2004. Matern. Child. Health J. 2016, 20, 2474–2482. [Google Scholar] [CrossRef]
- Grabich, S.C.; Robinson, W.R.; Konrad, C.E.; Horney, J.A. Impact of Hurricane Exposure on Reproductive Health Outcomes, Florida, 2004. Disaster Med. Public Health Prep. 2017, 11, 407–411. [Google Scholar] [CrossRef]
- Grech, V.; Scherb, H. Hurricane Katrina: Influence on the Male-to-Female Birth Ratio. Med. Princ. Pr. 2015, 24, 477–485. [Google Scholar] [CrossRef]
- Harville, E.W.; Giarratano, G.; Savage, J.; Barcelona de Mendoza, V.; Zotkiewicz, T. Birth Outcomes in a Disaster Recovery Environment: New Orleans Women After Katrina. Matern. Child. Health J. 2015, 19, 2512–2522. [Google Scholar] [CrossRef] [PubMed]
- Harville, E.W.; Xiong, X.; David, M.; Buekens, P. The Paradoxical Effects of Hurricane Katrina on Births and Adverse Birth Outcomes. Am. J. Public Health 2020, 110, 1466–1471. [Google Scholar] [CrossRef] [PubMed]
- Hilmert, C.J.; Kvasnicka-Gates, L.; Teoh, A.N.; Bresin, K.; Fiebiger, S. Major flood related strains and pregnancy outcomes. Health Psychol. 2016, 35, 1189–1196. [Google Scholar] [CrossRef] [PubMed]
- Mendez-Figueroa, H.; Chauhan, S.P.; Tolcher, M.C.; Shamshirsaz, A.A.; Sangi-Haghpeyker, H.; Pace, R.M.; Chu, D.M.; Aagaard, K. Peripartum outcomes before and after hurricane Harvey. Obs. Gynecol. 2019, 134, 1005. [Google Scholar] [CrossRef] [PubMed]
- Oni, O.; Harville, E.W.; Xiong, X.; Buekens, P. Impact of coping styles on post-traumatic stress disorder and depressive symptoms among pregnant women exposed to Hurricane Katrina. Am. J. Disaster Med. 2012, 7, 199–209. [Google Scholar] [CrossRef]
- Oni, O.; Harville, E.; Xiong, X.; Buekens, P. Relationships among stress coping styles and pregnancy complications among women exposed to Hurricane Katrina. J. Obs. Gynecol. Neonatal. Nurs. 2015, 44, 256–267. [Google Scholar] [CrossRef]
- Pan, K.; Beitsch, L.; Gonsoroski, E.; Sherchan, S.P.; Uejio, C.K.; Lichtveld, M.Y.; Harville, E.W. Effects of Hurricane Michael on Access to Care for Pregnant Women and Associated Pregnancy Outcomes. Int. J. Environ. Res. Public Health 2021, 18, 390. [Google Scholar] [CrossRef]
- Silva-Suarez, G.; Rabionet, S.E.; Zorrilla, C.D.; Perez-Menendez, H.; Rivera-Leon, S. Pregnant Women’s Experiences during Hurricane Maria: Impact, Personal Meaning, and Health Care Needs. Int. J. Environ. Res. Public Health 2021, 18, 8541. [Google Scholar] [CrossRef]
- Sun, S.; Weinberger, K.R.; Yan, M.; Brooke Anderson, G.; Wellenius, G.A. Tropical cyclones and risk of preterm birth: A retrospective analysis of 20 million births across 378 US counties. Environ. Int. 2020, 140, 105825. [Google Scholar] [CrossRef]
- Xiao, J.; Huang, M.; Zhang, W.; Rosenblum, A.; Ma, W.; Meng, X.; Lin, S. The immediate and lasting impact of Hurricane Sandy on pregnancy complications in eight affected counties of New York State. Sci. Total Environ. 2019, 678, 755–760. [Google Scholar] [CrossRef]
- Xiao, J.; Zhang, W.; Huang, M.; Lu, Y.; Lawrence, W.R.; Lin, Z.; Primeau, M.; Dong, G.; Liu, T.; Tan, W. Increased risk of multiple pregnancy complications following large-scale power outages during Hurricane Sandy in New York State. Sci. Total Environ. 2021, 770, 145359. [Google Scholar] [CrossRef] [PubMed]
- Bekkar, B.; Pacheco, S.; Basu, R.; DeNicola, N. Association of Air Pollution and Heat Exposure With Preterm Birth, Low Birth Weight, and Stillbirth in the US: A Systematic Review. JAMA Netw. Open 2020, 3, e208243. [Google Scholar] [CrossRef] [PubMed]
- Poursafa, P.; Keikha, M.; Kelishadi, R. Systematic Review on Adverse Birth Outcomes of Climate Change. J. Res. Med. Sci. 2015, 20, 397–402. Available online: https://www.ncbi.nlm.nih.gov/pubmed/26109998 (accessed on 7 May 2022). [PubMed]
- Rylander, C.; Odland, J.O.; Sandanger, T.M. Climate change and the potential effects on maternal and pregnancy outcomes: An assessment of the most vulnerable--the mother, fetus, and newborn child. Glob. Health Action. 2013, 6, 19538. [Google Scholar] [CrossRef]
- Dadvand, P.; Basagana, X.; Sartini, C.; Figueras, F.; Vrijheid, M.; de Nazelle, A.; Sunyer, J.; Nieuwenhuijsen, M.J. Climate extremes and the length of gestation. Environ. Health Perspect. 2011, 119, 1449–1453. [Google Scholar] [CrossRef]
- Abdo, M.; Ward, I.; O’Dell, K.; Ford, B.; Pierce, J.R.; Fischer, E.V.; Crooks, J.L. Impact of Wildfire Smoke on Adverse Pregnancy Outcomes in Colorado, 2007–2015. Int. J. Environ. Res. Public Health 2019, 16, 3720. [Google Scholar] [CrossRef]
- Qiu, X.; Fong, K.C.; Shi, L.; Papatheodorou, S.; Di, Q.; Just, A.; Annaa, K.; Carmen, M.; Schwartz, J.D. Prenatal exposure to particulate air pollution and gestational age at delivery in Massachusetts neonates 2001-2015: A perspective of causal modeling and health disparities. Environ. Epidemiol. 2020, 4, e113. [Google Scholar] [CrossRef]
- Harville, E.W.; Beitsch, L.; Uejio, C.K.; Sherchan, S.; Lichtveld, M.Y. Assessing the effects of disasters and their aftermath on pregnancy and infant outcomes: A conceptual model. Int. J. Disaster. Risk Reduct. 2021, 62, 102415. [Google Scholar] [CrossRef]
| Group | Topic | Terms | PubMed | Web of Science |
|---|---|---|---|---|
| A | Climate Change | climate change OR global warming OR climatic processes | 108,017 | 491,785 |
| B | Environmental Exposure | disasters OR natural disasters OR extreme weather events OR wildfire smoke OR air pollution OR ozone OR particulate matter OR temperature OR hot temperature OR heat exposure OR heat event OR heat wave | 1,247,159 | 4,290,162 |
| C | Maternal Health | pregnancy OR pregnancy outcome OR pregnancy complications OR perinatal mortality OR birth weight OR birth outcome OR fetal health OR gestational age | 1,197,108 | 633,994 |
| D | A + C | 748 | 777 | |
| E | B + C | 22,645 | 9737 | |
| F | A + B + C | 395 | 373 |
| Author, Year, Citation Number | Location | Temperature Exposure | Perinatal and Maternal Outcome |
|---|---|---|---|
| Barreca, A. and Schaller, J., 2020 [7] | United States | Heat exposure; air conditioning effects | Gestational days |
| Basu, R., et al., 2016 [8] | California | Mean apparent temperature | Stillbirth |
| Basu, R., et al., 2018 [9] | California | Apparent temperature; air pollutants as confounders or effect modifiers | Term low birth weight |
| Cil, G., and Cameron, T.A., 2017 [10] | United States | Heat waves | Abnormal conditions of the newborn and adverse maternal health conditions |
| Ha, S., et al., 2017 [11] | United States | Temperature extremes; air pollutants | Small for gestational age; term low birth weight |
| Ha, S., et al., 2017 [12] | United States | Acute and chronic extreme temperature exposures | Stillbirth |
| Ha, S., et al., 2017 [13] | United States | Ambient temperature | Cardiovascular event during labor and delivery |
| Ha, S., et al., 2018 [14] | United States | Ambient temperature | Preterm; premature rupture of membranes |
| Huang, M.J., et al., 2021 [15] | United States | Heat waves | Preterm birth and early term birth |
| Lin, G. and Zhang, T.L., 2012 [16] | United States | National Climatic Data Center Summary of the Day Data weather variables | Birthweight |
| Monteblanco, A.D., and Vanos, J.K., 2021 [17] | El Paso, Texas | Heat exposure | Awareness of health risks of extreme heat exposure |
| Ngo, N.S. and Horton, R.M., 2016 [18] | New York | Extreme temperatures | Birth weight and gestational age |
| Rammah, A., et al., 2019 [19] | Harris County, Texas | Apparent temperature; air pollutants | Stillbirths |
| Smith, M.L., et al., 2020 [20] | Minnesota | Heat exposure | Preterm birth |
| Sun, S., et al., 2019 [21] | United States | Ambient temperature exposure by trimester | Small for gestational age; birth weight |
| Sun, Y., et al., 2020 [22] | California | Combined effects of heat waves, air pollution and green space exposure | Preterm birth |
| Van Zutphen, A.R., et al., 2014 [23] | New York | Examined the relationship between extreme winter temperatures and birth defects | Birth defects |
| Yu, X., et al., 2018 [24] | Puerto Rico | Weather variables included monthly precipitation intensity, number of days with ≥ 25 mm rain in the month, monthly average temperature, monthly precipitation frequency (number of days with > −32.2 degrees Celsius in the month), storm events (heavy rain, hurricane, tornado and tropical storm), and flood events (flash flood and flood) | Preterm birth |
| Zhang, W., et al., 2019 [25] | United States | Ambient temperature changes and maternal heat exposure | Congenital heart defects |
| Author, Year, Citation Number | Location | Air Pollutants | Perinatal Outcome |
|---|---|---|---|
| Basu, R., et al., 2018 [8] | California | PM2.5, ozone, carbon monoxide, nitrogen dioxide, and sulfur dioxide | Term low birth weight |
| Ha, S.D., et al., 2017c [14] | United States | Carbon monoxide, nitrogen oxides, ozone, PM2.5, PM10, sulfur dioxide, and individual constituents of PM2.5 including elemental carbon, organic compound, ammonium ions, sulfate particles, nitrate particles, and dust particles | Small for gestational age and term low birth weight |
| Rammah, A., et al., 2019 [19] | Texas | PM2.5, nitrogen dioxide, and ozone | Stillbirth |
| Sarovar, V., et al., 2020 [26] | California | PM2.5, PM10, ozone, nitrogen dioxide, sulfur dioxide, and carbon dioxide | Stillbirth |
| Sun, Y., et al., 2020 [22] | California | PM2.5, PM10, ozone, and nitrogen dioxide | Preterm birth |
| Author, Year, Citation Number | Location | Disaster Type | Perinatal and Maternal Outcome |
|---|---|---|---|
| Antipova, A., and Curtis, A., 2015 [27] | Louisiana | Hurricane | Birthweight; preterm deliveries |
| Brock, R.L., et al., 2014 [28] | Iowa | Flash flood | Maternal mental health |
| Brock, R.L., et al., 2015 [29] | Iowa | Flash flood | Maternal mental health |
| Currie, J., and Rossin-Slater, M., 2013 [30] | Texas | Hurricane | Birthweight; newborn abnormal conditions; labor and delivery complications |
| Giarratano, G.P., et al., 2019 [31] | Louisiana | Hurricane | Maternal mental health |
| Grabich, S.C., et al., 2016 [32] | Florida | Hurricane | Extremely preterm and preterm delivery |
| Grabich, S.C., et al., 2017 [33] | Florida | Hurricane | Birthweight |
| Grech, V., et al., 2015 [34] | Alabama, Florida, Louisiana, Mississippi | Hurricane | Male:female birth ratio |
| Harville, E.W., et al., 2015 [35] | Louisiana | Hurricane | Birthweight |
| Harville, E.W., et al., 2020 [36] | Alabama, Louisiana, Mississippi | Hurricane | Birthweight |
| Hilmert, C.J., et al., 2016 [37] | Fargo, North Dakota | Flash flood | Birthweight |
| Mendez-Figueroa, H., et al., 2019 [38] | Texas | Hurricane | Composite maternal and neonatal morbidity |
| Oni, O., et al., 2012 [39] | Louisiana | Hurricane | Maternal mental health |
| Oni, O., et al., 2015 [40] | Louisiana | Hurricane | Maternal stress and pregnancy complications |
| Pan, K., et al., 2021 [41] | Florida | Hurricane | Birthweight; maternity care and support services |
| Silva-Suarez, G., et al., 2021 [42] | Puerto Rico | Hurricane | Maternity care and support services |
| Sun, S., et al., 2020 [43] | United States | Tropical cyclone | Preterm birth |
| Xiao, J., et al., 2019 [44] | New York | Hurricane | Emergency department visits for pregnancy complications |
| Xiao, J, et al., 2021 [45] | New York | Hurricane | Emergency department visits for pregnancy complications |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Veenema, R.J.; Hoepner, L.A.; Geer, L.A. Climate Change-Related Environmental Exposures and Perinatal and Maternal Health Outcomes in the U.S. Int. J. Environ. Res. Public Health 2023, 20, 1662. https://doi.org/10.3390/ijerph20031662
Veenema RJ, Hoepner LA, Geer LA. Climate Change-Related Environmental Exposures and Perinatal and Maternal Health Outcomes in the U.S. International Journal of Environmental Research and Public Health. 2023; 20(3):1662. https://doi.org/10.3390/ijerph20031662
Chicago/Turabian StyleVeenema, Ryne J., Lori A. Hoepner, and Laura A. Geer. 2023. "Climate Change-Related Environmental Exposures and Perinatal and Maternal Health Outcomes in the U.S." International Journal of Environmental Research and Public Health 20, no. 3: 1662. https://doi.org/10.3390/ijerph20031662
APA StyleVeenema, R. J., Hoepner, L. A., & Geer, L. A. (2023). Climate Change-Related Environmental Exposures and Perinatal and Maternal Health Outcomes in the U.S. International Journal of Environmental Research and Public Health, 20(3), 1662. https://doi.org/10.3390/ijerph20031662








