Building Consensus on the Point-of-Care Ultrasound Skills Required for Effective Healthcare Service Delivery at District Hospitals in South Africa: A Delphi Study
Abstract
:1. Introduction
2. Methods
2.1. Study Design
2.2. Survey Development
2.3. Panel Recruitment
2.4. Ethical Clearance
2.5. Patient and Public Involvement
2.6. The Delphi Process
2.6.1. Round 1
2.6.2. Round 2
2.6.3. Round 3
2.6.4. Round 4
2.6.5. Round 5
2.7. Data Analysis
2.8. Role of the Funding Source
3. Results
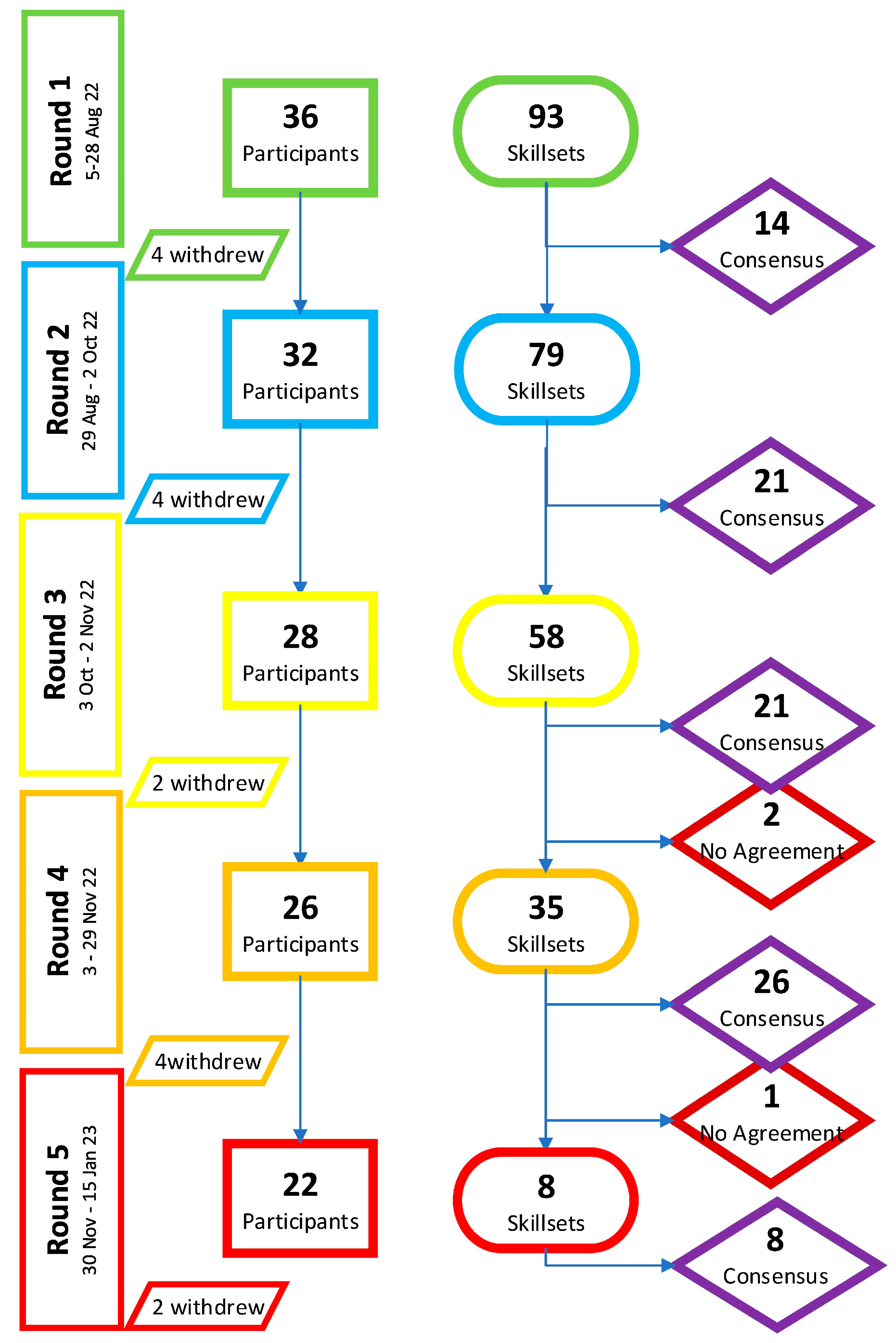
3.1. Participants
3.2. Skillsets
3.2.1. Round 1
3.2.2. Round 2
3.2.3. Round 3
3.2.4. Round 4
3.2.5. Round 5
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Narula, J.; Chandrashekhar, Y.; Braunwald, E. Time to Add a Fifth Pillar to Bedside Physical Examination: Inspection, Palpation, Percussion, Auscultation, and Insonation. JAMA Cardiol. 2018, 3, 346–350. [Google Scholar] [CrossRef] [PubMed]
- Moore, C.L.C.; Copel, J.A.J. Point-of-Care Ultrasonography. N. Engl. J. Med. 2011, 364, 749–757. [Google Scholar] [CrossRef] [PubMed]
- Could Ultrasound Replace the Stethoscope?|The New Yorker. Available online: https://www.newyorker.com/science/annals-of-medicine/could-ultrasound-replace-the-stethoscope (accessed on 21 February 2023).
- Szabó, G.V.; Szigetváry, C.; Szabó, L.; Dembrovszky, F.; Rottler, M.; Ocskay, K.; Madzsar, S.; Hegyi, P.; Molnár, Z. Point-of-care ultrasound improves clinical outcomes in patients with acute onset dyspnea: A systematic review and meta-analysis. Intern. Emerg. Med. 2022, 18, 639–653. [Google Scholar] [CrossRef] [PubMed]
- Andersen, C.A.; Holden, S.; Vela, J.; Rathleff, M.S.; Jensen, M.B. Point-of-care ultrasound in general practice: A systematic review. Ann. Fam. Med. 2019, 17, 61–69. [Google Scholar] [CrossRef] [PubMed]
- Abrokwa, S.K.; Ruby, L.C.; Heuvelings, C.C.; Bélard, S. Task shifting for point of care ultrasound in primary healthcare in low- and middle-income countries-a systematic review. eClinicalMedicine 2022, 45, 101333. [Google Scholar] [CrossRef] [PubMed]
- Butterfly Network, Inc.|Bill & Melinda Gates Foundation. Available online: https://www.gatesfoundation.org/about/committed-grants/2022/03/inv040773 (accessed on 21 February 2023).
- Constantine, E.; Levine, M.; Abo, A.; Arroyo, A.; Ng, L.; Kwan, C.; Baird, J.; Shefrin, A.E.; P2 Network Point-of-care Ultrasound Fellowship Delphi Group. Core Content for Pediatric Emergency Medicine Ultrasound Fellowship Training: A Modified Delphi Consensus Study. AEM Educ. Train. 2020, 4, 130–138. [Google Scholar] [CrossRef]
- Arishenkoff, S.; Blouw, M.; Card, S.; Conly, J.; Gebhardt, C.; Gibson, N.; Lenz, R.; Ma, I.W.Y.; Meneilly, G.S.; Reimche, L.; et al. Expert Consensus on a Canadian Internal Medicine Ultrasound Curriculum. Can. J. General. Intern. Med. 2014, 9, 106–111. [Google Scholar] [CrossRef]
- Atkinson, P.; Bowra, J.; Lambert, M.; Lamprecht, H.; Noble, V.; Jarman, B. International federation for emergency medicine point of care ultrasound curriculum. Can. J. Emerg. Med. 2015, 17, 161–170. [Google Scholar] [CrossRef]
- Salmon, M.; Landes, M.; Hunchak, C.; Paluku, J.; Kalisya, L.M.; Salmon, C.; Muller, M.M.; Wachira, B.; Mangan, J.; Chhaganlal, K.; et al. Getting It Right the First Time: Defining Regionally Relevant Training Curricula and Provider Core Competencies for Point-of-Care Ultrasound Education on the African Continent. Ann. Emerg. Med. 2017, 69, 218–226. [Google Scholar] [CrossRef]
- Sriram, V.; Bennett, S. Strengthening medical specialisation policy in low-income and middle-income countries Handling editor Seye Abimbola. BMJ Glob. Health 2020, 5, 2053. [Google Scholar] [CrossRef]
- Løkkegaard, T.; Todsen, T.; Nayahangan, L.J.; Andersen, C.A.; Jensen, M.B.; Konge, L. Point-of-care ultrasound for general practitioners: A systematic needs assessment. Scand. J. Prim. Health Care 2020, 38, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Homar, V.; Gale, Z.K.; Lainscak, M.; Svab, I. Knowledge and skills required to perform point-of-care ultrasonography in family practice—A modified Delphi study among family physicians in Slovenia. BMC Fam. Pr. 2020, 21, 4–9. [Google Scholar] [CrossRef] [PubMed]
- Nixon, G.; Blattner, K.; Muirhead, J.; Finnie, W.; Lawrenson, R.; Kerse, N. Scope of point-of-care ultrasound practice in rural New Zealand. J. Prim. Health Care 2018, 10, 224–236. [Google Scholar] [CrossRef]
- Haldeman, M.S.; Kunka, E.; Makasa, M.; Birkland, B. Resident perception on the impact of point-of-care ultrasound in clinical care at a family medicine training program in Zambia. Ultrasound J. 2022, 14, 18. [Google Scholar] [CrossRef] [PubMed]
- Shah, S.P.; Epino, H.; Bukhman, G.; Umulisa, I.; Dushimiyimana, J.M.V.; Reichman, A.; Noble, V.E. Impact of the introduction of ultrasound services in a limited resource setting: Rural Rwanda 2008. BMC Int. Health Hum. Rights 2009, 9, 4. [Google Scholar] [CrossRef] [PubMed]
- Henwood, P.C.; Mackenzie, D.C.; Rempell, J.S.; Douglass, E.; Dukundane, D.; Liteplo, A.S.; Leo, M.M.; Murray, A.F.; Vaillancourt, S.; Dean, A.J.; et al. Intensive point-of-care ultrasound training with long-term follow-up in a cohort of Rwandan physicians. Trop. Med. Int. Health 2016, 21, 1531–1538. [Google Scholar] [CrossRef] [PubMed]
- Bell, G.; Wachira, B.; Denning, G. A pilot training program for point-of-care ultrasound in Kenya. Afr. J. Emerg. Med. 2016, 6, 132–137. [Google Scholar] [CrossRef]
- Sabatino, V.; Caramia, M.R.; Curatola, A.; Vassallo, F.; Deidda, A.; Cinicola, B.; Iodice, F.; Caffarelli, C.; Sverzellati, N.; Buonsenso, D. Point-of-care ultrasound (POCUS) in a remote area of Sierra Leone: Impact on patient management and training program for community health officers. J. Ultrasound 2020, 23, 521–527. [Google Scholar] [CrossRef]
- Niederberger, M.; Spranger, J. Delphi Technique in Health Sciences: A Map. Front. Public. Health 2020, 8, 457. [Google Scholar] [CrossRef]
- Humphrey-Murto, S.; Wood, T.J.; Gonsalves, C.; Mascioli, K.; Varpio, L. The Delphi Method. Acad. Med. 2020, 95, 168. [Google Scholar] [CrossRef]
- Ma, I.W.Y.; Steinmetz, P.; Weerdenburg, K.; Woo, M.Y.; Olszynski, P.; Heslop, C.L.; Miller, S.; Sheppard, G.; Daniels, V.; Desy, J.; et al. The Canadian Medical Student Ultrasound Curriculum: A Statement From the Canadian Ultrasound Consensus for Undergraduate Medical Education Group. J. Ultrasound Med. 2020, 39, 1279–1287. [Google Scholar] [CrossRef] [PubMed]
- Mans, P.A.; Yogeswaran, P.; Adeniyi, O.V. Protocol for a Delphi Consensus Study to Determine the Essential and Optional Ultrasound Skills for Medical Practitioners Working in District Hospitals in South Africa. Int. J. Environ. Res. Public. Health 2022, 19, 9640. [Google Scholar] [CrossRef] [PubMed]
- Jünger, S.; Payne, S.A.; Brine, J.; Radbruch, L.; Brearley, S.G. Guidance on Conducting and REporting DElphi Studies (CREDES) in palliative care: Recommendations based on a methodological systematic review. Palliat. Med. 2017, 31, 684–706. [Google Scholar] [CrossRef]
- Recommended Curriculum Guidelines for Family Medicine Residents. AAFP Reprint No. 290D. 2016, pp. 1–14. Available online: https://www.aafp.org/dam/AAFP/documents/medical_education_residency/program_directors/Reprint290D_POCUS.pdf (accessed on 21 February 2023).
- Perera, P.; Mailhot, T.; Riley, D.; Mandavia, D. The RUSH exam 2012: Rapid ultrasound in shock in the evaluation of the critically Ill patient. Ultrasound Clin. 2012, 7, 255–278. [Google Scholar] [CrossRef]
- Kimura, B.J.; Shaw, D.J.; Amundson, S.A.; Phan, J.N.; Blanchard, D.G.; DeMaria, A.N. Cardiac limited ultrasound examination techniques to augment the bedside cardiac physical examination. J. Ultrasound Med. 2015, 34, 1683–1690. [Google Scholar] [CrossRef] [PubMed]
- Manson, W.C.; Kirksey, M.; Boublik, J.; Wu, C.L.; Haskins, S.C. Focused assessment with sonography in trauma (FAST) for the regional anesthesiologist and pain specialist. Reg. Anesth. Pain. Med. 2019, 44, 540–548. [Google Scholar] [CrossRef]
- Lichtenstein, D.A.; Mezière, G.A. Relevance of lung ultrasound in the diagnosis of acute respiratory failure the BLUE protocol. Chest 2008, 134, 117–125. [Google Scholar] [CrossRef]
- Khanyi, H.B.; Naicker, B.; Khanyi, H. The use of point-of-care ultrasound in a regional emergency department in KwaZulu-Natal, South Africa. S. Afr. Fam. Pract. 2021, 63, a5269. [Google Scholar] [CrossRef]
- Ganas, U.; Malan, J.J.; Bruijns, S.R. A descriptive study of the use of cardiac point of care ultrasound (PoCUS) in public emergency centres in Cape Town. Afr. J. Emerg. Med. 2020, 10, 239–242. [Google Scholar] [CrossRef]
- Atkinson, P.R.; Milne, J.; Diegelmann, L.; Lamprecht, H.; Stander, M.; Lussier, D.; Pham, C.; Henneberry, R.; Fraser, J.M.; Howlett, M.K.; et al. Does Point-of-Care Ultrasonography Improve Clinical Outcomes in Emergency Department Patients with Undifferentiated Hypotension? An International Randomized Controlled Trial from the SHoC-ED Investigators. Ann. Emerg. Med. 2018, 72, 478–489. [Google Scholar] [CrossRef]
- Van Hoving, D.J.; Kenge, A.P.; Maartens, G.; Meintjes, G. Point-of-care ultrasound predictors for the diagnosis of tuberculosis in HIV-positive patients presenting to an emergency center. J. Acquir. Immune Defic. Syndr. 2020, 83, 415–423. [Google Scholar] [CrossRef] [PubMed]
- Fourie, L.; Pather, M.; Hendricks, G. Point-of-care ultrasound: The new district focus. Afr. J. Prim. Health Care Fam. Med. 2023, 15, e1–e8. [Google Scholar] [CrossRef] [PubMed]
- Wells, M.; Goldstein, L.N.; Beringer, C. Emergency medicine society of South Africa guidelines for the training and credentialing in emergency point-of-care ultrasound. S. Afr. Med. J. 2021, 111, 491–512. [Google Scholar] [CrossRef] [PubMed]
- Lane, J.; Andrews, G.; Orange, E.; Brezak, A.; Tanna, G.; Lebese, L.; Carter, T.; Naidoo, E.; Levendal, E.; Katz, A. Strengthening health policy development and management systems in low- and middle- income countries: South Africa’s approach. Health Policy Open 2020, 1, 100010. [Google Scholar] [CrossRef]
- Chamsi-Pasha, M.A.; Sengupta, P.P.; Zoghbi, W.A. Handheld Echocardiography. Circulation 2017, 136, 2178–2188. [Google Scholar] [CrossRef]
- Heller, T.; Mtemang’ombe, E.A.; Huson, M.A.M.; Heuvelings, C.C.; Bélard, S.; Janssen, S.; Phiri, S.; Grobusch, M.P. Ultrasound for patients in a high HIV/tuberculosis prevalence setting: A needs assessment and review of focused applications for Sub-Saharan Africa. Int. J. Infect. Dis. 2017, 56, 229–236. [Google Scholar] [CrossRef] [PubMed]
- National Guidelines on the Treatment of Tuberculosis Infection. 2023. Available online: https://knowledgehub.health.gov.za (accessed on 26 July 2023).
- South Africa’s National Strategic Plan on HIV, TB and STI’s 2017–2022. 2016. Available online: https://sanac.org.za/about-sanac/the-national-strategic-plan/ (accessed on 26 July 2023).
- Duggan, N.M.; Shokoohi, H.; Liteplo, A.S.; Huang, C.; Goldsmith, A.J. Best Practice Recommendations for Point-of-Care Lung Ultrasound in Patients with Suspected COVID-19. J. Emerg. Med. 2020, 59, 515–520. [Google Scholar] [CrossRef]
- Kaswa, R.; Govender, I. Novel coronavirus pandemic: A clinical overview. S. Afr. Fam. Pract. 2020, 62, e1–e5. [Google Scholar] [CrossRef]
- Hammadah, M.; Ponce, C.; Sorajja, P.; Cavalcante, J.L.; Garcia, S.; Gössl, M. Point-of-care ultrasound: Closing guideline gaps in screening for valvular heart disease. Clin. Cardiol. 2020, 43, 1368–1375. [Google Scholar] [CrossRef]
- Gundersen, G.H.; Norekval, T.M.; Haug, H.H.; Skjetne, K.; Kleinau, J.O.; Graven, T.; Dalen, H. Adding point of care ultrasound to assess volume status in heart failure patients in a nurse-led outpatient clinic. A randomised study. Heart 2016, 102, 29–34. [Google Scholar] [CrossRef]
- Kreiser, M.A.; Hill, B.; Karki, D.; Wood, E.; Shelton, R.; Peterson, J.; Riccio, J.; Zapata, I.; Khalil, P.A.; Gubler, D.; et al. Point-of-Care Ultrasound Use by EMS Providers in out-of-Hospital Cardiac Arrest. Prehosp Disaster Med. 2022, 37, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Nathanson, R.; Williams, J.P.; Gupta, N.; Rezigh, A.; Mader, M.J.; Haro, E.K.; Drum, B.; O’Brien, E.; Khosla, R.; Boyd, J.S.; et al. Current Use and Barriers to Point-of-Care Ultrasound in Primary Care: A National Survey of VA Medical Centers. Am. J. Med. 2023, 136, 592–595.e2. [Google Scholar] [CrossRef] [PubMed]
- Zhao, R.T.; Deng, J.; Ghanem, G.; Steiger, A.; Tang, L.; Haase, D.; Sadeghinejad, S.E.; Shibata, J.; Chiem, A.T. Using tele-ultrasound to teach medical students: A randomised control equivalence study. Australas. J. Ultrasound Med. 2023, 26, 91–99. [Google Scholar] [CrossRef]
- Hari, R.; Caprez, R.; Dolmans, D.; Huwendiek, S.; Robbiani, S.; Stalmeijer, R.E. Describing Ultrasound Skills Teaching by Near-Peer and Faculty Tutors Using Cognitive Apprenticeship. Teach. Learn. Med. 2022, 1–10. [Google Scholar] [CrossRef]
- Van Hoving, D.J.; Lamprecht, H.H.; Stander, M.; Vallabh, K.; Fredericks, D.; Louw, P.; Müller, M.; Malan, J.J. Adequacy of the emergency point-of-care ultrasound core curriculum for the local burden of disease in South Africa. Emerg. Med. J. 2013, 30, 312–315. [Google Scholar] [CrossRef]
| Clinical Domains | Number of Skillsets (N = 93) |
|---|---|
| 1. Obstetrics and gynaecology | 20 |
| 2. Cardiology | 10 |
| 3. Trauma | 4 |
| 4. Abdominal | 17 |
| 5. Vascular | 3 |
| 6. Musculoskeletal | 10 |
| 7. Pulmonary | 8 |
| 8. Ocular | 6 |
| 9. Procedural | 10 |
| 10. Ultrasound protocols | 5 |
| Variables | Frequency |
|---|---|
| Provincial distribution of panelists | |
| Eastern Cape | 5 |
| Free State | 3 |
| Gauteng | 6 |
| KwaZulu-Natal | 3 |
| Limpopo | 1 |
| Mpumalanga | 4 |
| Northern Cape | 2 |
| Western Cape | 7 |
| North-West | 1 |
| No response | 4 |
| Training in ultrasound | |
| Postgraduate Diploma in US | 1 |
| FPD US courses | 7 |
| EMSSA POCUS | 6 |
| Other US short courses | 9 |
| Informal training in US | 2 |
| No response | 4 |
| Experience in patient evaluation with US (years) | |
| ≤3 | 8 |
| 4–6 | 8 |
| 7–9 | 6 |
| ≥10 | 10 |
| No response | 4 |
| Clinical Domain | Skillsets (90) | Essential | Optional | Non-Essential |
|---|---|---|---|---|
| Obstetrics and Gynaecology | 20 | 16 | 3 | 1 |
| Cardiology | 10 | 4 | 6 | 0 |
| Trauma | 4 | 4 | 0 | 0 |
| Abdominal | 15 | 7 | 8 | 0 |
| Vascular | 3 | 2 | 1 | 0 |
| Musculoskeletal | 9 | 0 | 4 | 5 |
| Pulmonary | 8 | 3 | 3 | 2 |
| Ocular | 6 | 0 | 0 | 6 |
| Procedural | 10 | 6 | 3 | 1 |
| Ultrasound protocols | 5 | 4 | 1 | 0 |
| 1.1.1 | Identification of the presence of an intrauterine pregnancy | Essential | R1 |
| 1.1.2 | Determination of the viability of an intrauterine pregnancy | Essential | R1 |
| 1.1.3 | Detection of the fetal heart rate using M-Mode | Essential | R2 |
| 1.1.4 | First trimester pregnancy gestational age assessment by crown rump length detection | Essential | R1 |
| 1.1.5 | Recognition of molar pregnancy | Essential | R1 |
| 1.2.1 | Determination of placental position | Essential | R1 |
| 1.2.2 | Determination of the fetal presentation | Essential | R1 |
| 1.2.3 | Performing a gestational age assessment and fetal weight estimation using abdominal circumference (AC), biparietal diameter (BPD), and femoral length (FL). | Essential | R1 |
| 1.2.10 | Confirmation of fetal death | Essential | R1 |
| 1.2.4 | Assessment of the amniotic fluid volume using either the four-quadrant calculation or deepest single pocket approach | Essential | R2 |
| 1.2.5 | Assessment of the placenta for features of placental abruption | Essential | R2 |
| 1.2.8 | Assessment of fetal well-being using the biophysical profile | Essential | R4 |
| 1.2.9 | Assessment of fetal well-being during third trimester using umbilical artery doppler | Essential | R5 |
| 1.3.1 | Confirmation of intrauterine device (IUD) position | Essential | R3 |
| 1.3.2 | Measurement of endometrial thickness | Essential | R2 |
| 1.3.3 | Assessment of an adnexal mass: simple, complex, and hemorrhagic cysts | Essential | R5 |
| 2.1 | Detection of a pericardial effusion | Essential | R1 |
| 2.10 | Measurement of inferior vena cava (IVC) diameter and collapsibility to approximate volume status | Essential | R5 |
| 2.2 | Assessment of global left ventricle contractility (hyperdynamic/normal/decreased) | Essential | R4 |
| 3.1 | Assessment of free fluid in the abdominal cavity | Essential | R1 |
| 3.2 | Assessment of free fluid around the heart with a sub-xyphoid view | Essential | R1 |
| 3.3 | Assessment of a pneumothorax | Essential | R2 |
| 3.4 | Assessment of a hemothorax | Essential | R2 |
| 4.1.1 | Detection of an abdominal aortic aneurysm | Essential | R3 |
| 4.2.1 | Assessment of the gallbladder for cholelithiasis | Essential | R2 |
| 4.2.2 | Assessment for acute cholecystitis | Essential | R2 |
| 4.2.3 | Assessment for common bile duct (CBD) obstruction (choledocholithiasis) | Essential | R5 |
| 4.2.4 | Assessment for hepato-splenomegaly | Essential | R5 |
| 4.4.1 | Assessment of renal size | Essential | R4 |
| 4.4.5 | Identification of a testicular torsion | Essential | R2 |
| 5.1 | Identification of lower extremity DVT in low-risk cases with 2-Zone discrimination technique | Essential | R1 |
| 5.2 | Identification of lower extremity DVT with color Doppler and graded compression of the entire limb | Essential | R3 |
| 7.1 | Identification of pulmonary oedema | Essential | R5 |
| 7.3 | Identification of pneumothorax | Essential | R2 |
| 7.4 | Identification of pleural effusion or hemothorax | Essential | R2 |
| 9.1 | Thoracentesis | Essential | R2 |
| 9.2 | Paracentesis | Essential | R2 |
| 9.3 | Peripheral IV placement | Essential | R2 |
| 9.4 | Central line placement | Essential | R1 |
| 9.7 | Foreign body identification and removal | Essential | R2 |
| 9.8 | Fine-needle aspiration/biopsy | Essential | R2 |
| 10.1 | FAST/E-FAST: Focused assessment with sonography for trauma | Essential | R1 |
| 10.2 | RUSH: Rapid ultrasound for shock and hypotension | Essential | R2 |
| 10.3 | BLUE: Bedside lung ultrasound in emergency | Essential | R2 |
| 10.4 | CLUE: Cardiac limited ultrasound exam | Essential | R2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mans, P.-A.; Yogeswaran, P.; Adeniyi, O.V. Building Consensus on the Point-of-Care Ultrasound Skills Required for Effective Healthcare Service Delivery at District Hospitals in South Africa: A Delphi Study. Int. J. Environ. Res. Public Health 2023, 20, 7126. https://doi.org/10.3390/ijerph20237126
Mans P-A, Yogeswaran P, Adeniyi OV. Building Consensus on the Point-of-Care Ultrasound Skills Required for Effective Healthcare Service Delivery at District Hospitals in South Africa: A Delphi Study. International Journal of Environmental Research and Public Health. 2023; 20(23):7126. https://doi.org/10.3390/ijerph20237126
Chicago/Turabian StyleMans, Pierre-Andre, Parimalaranie Yogeswaran, and Oladele Vincent Adeniyi. 2023. "Building Consensus on the Point-of-Care Ultrasound Skills Required for Effective Healthcare Service Delivery at District Hospitals in South Africa: A Delphi Study" International Journal of Environmental Research and Public Health 20, no. 23: 7126. https://doi.org/10.3390/ijerph20237126
APA StyleMans, P.-A., Yogeswaran, P., & Adeniyi, O. V. (2023). Building Consensus on the Point-of-Care Ultrasound Skills Required for Effective Healthcare Service Delivery at District Hospitals in South Africa: A Delphi Study. International Journal of Environmental Research and Public Health, 20(23), 7126. https://doi.org/10.3390/ijerph20237126





