Mindfulness Intervention Improves Coping and Perceptions of Children’s Behavior among Families with Elevated Risk
Abstract
:1. Introduction
1.1. Stress, Parenting, and Mindfulness
1.2. The Role of Coping
1.3. Coping and Children’s Behavior Problems
1.4. Mindfulness-Informed Interventions for Underrepresented Populations
1.5. The Current Study
2. Materials and Methods
2.1. Participant Characteristics
2.2. Procedures
Mindfulness-Informed Intervention
2.3. Measures
2.3.1. Parental Cognitive–Emotion Coping
2.3.2. Parental Perceptions of Children’s Behavior Problems
2.3.3. Covariate
2.4. Data Analysis
3. Results
3.1. Factor Extraction and Rotation
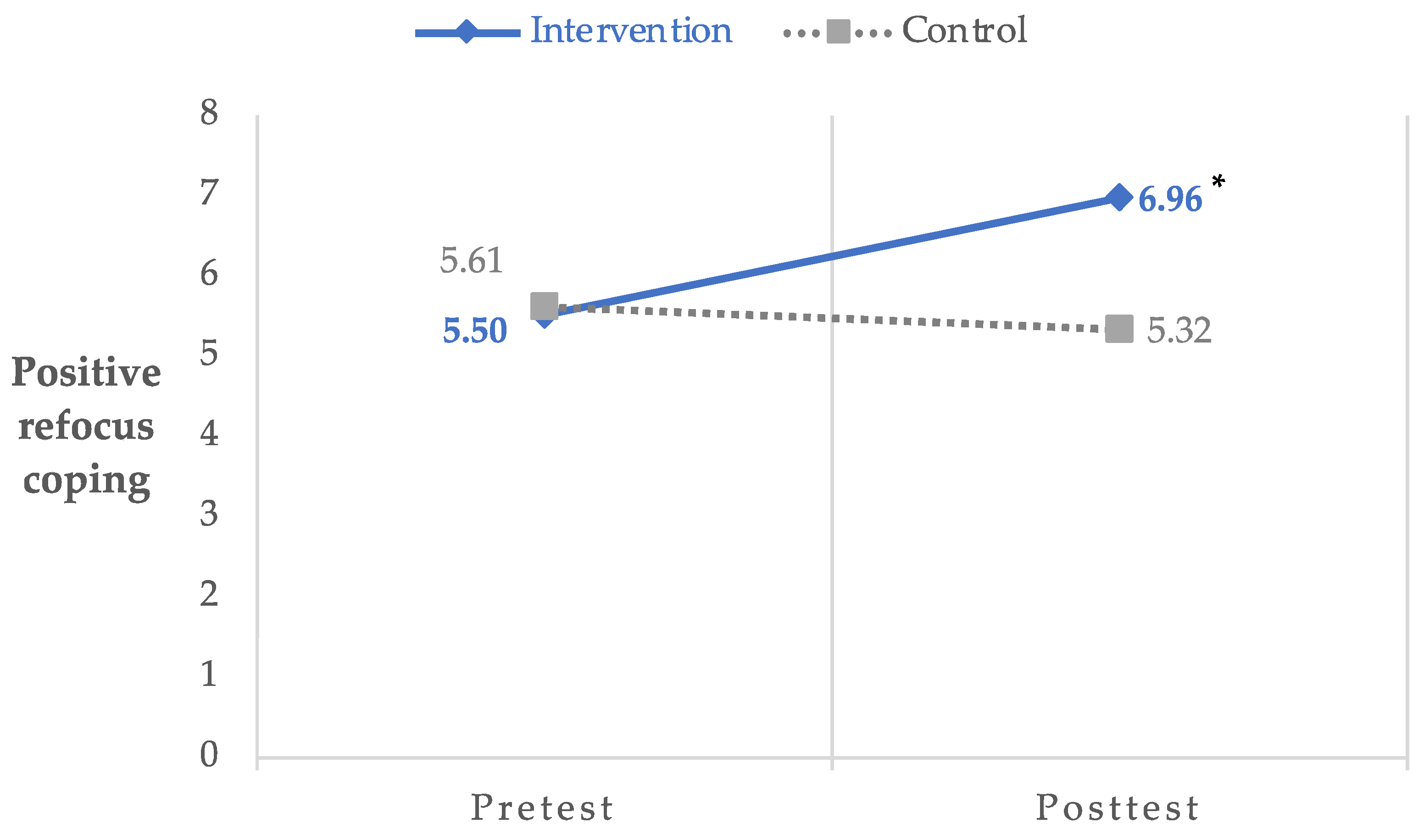
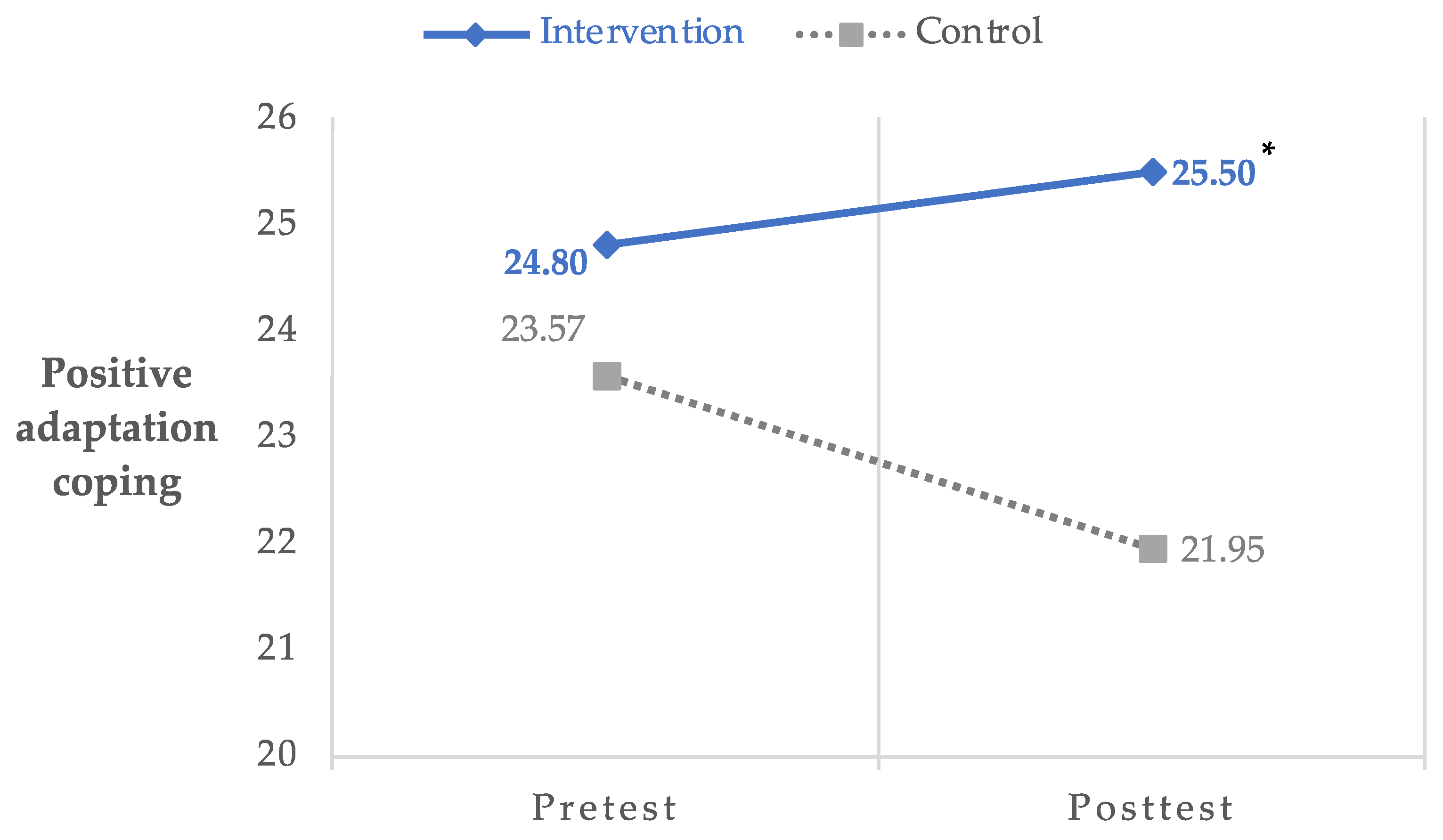
3.2. Coping Strategies
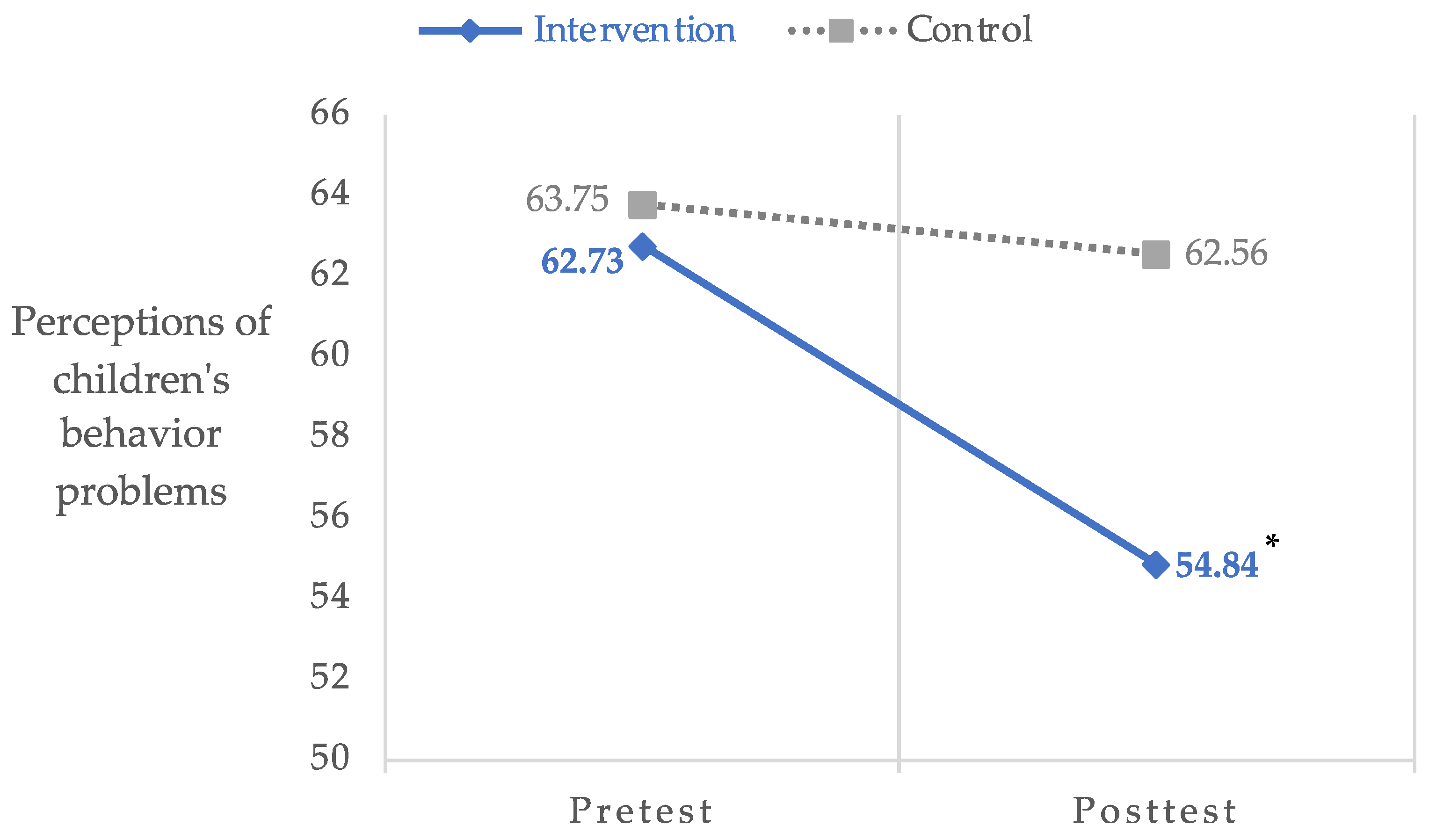
3.3. Perceptions of Children’s Behavior Problems
4. Discussion
Limitations and Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Beuchel, P.; Groß Ophoff, J.; Cramer, C.; Hautzinger, M. Promoting Occupational Health and Teaching Quality: The Impact of a Mindfulness Intervention in Teacher Training. Teach. Teach. Educ. 2022, 114, 103703. [Google Scholar] [CrossRef]
- Liu, F.; Zhang, Z.; Liu, S.; Feng, Z. Effectiveness of Brief Mindfulness Intervention for College Students’ Problematic Smartphone Use: The Mediating Role of Self-Control. PLoS ONE 2022, 17, e0279621. [Google Scholar] [CrossRef]
- Lunsky, Y.; Redquest, B.; Albaum, C.; Hutton, S.; Share, M.; Share-Strom, D.; Weiss, J. Virtual Group–Based Mindfulness Intervention for Autistic Adults: A Feasibility Study. Mindfulness 2022, 13, 1706–1718. [Google Scholar] [CrossRef]
- Mirabito, G.; Verhaeghen, P. The Effects of Mindfulness Interventions on Older Adults’ Cognition: A Meta-Analysis. J. Gerontol. Ser. B 2023, 78, 394–408. [Google Scholar] [CrossRef]
- Cheung, R.Y.M.; Chan, S.K.C.; Chui, H.; Chan, W.M.; Ngai, S.Y.S. Enhancing Parental Well-Being: Initial Efficacy of a 21-Day Online Self-Help Mindfulness-Based Intervention for Parents. Mindfulness 2022, 13, 2812–2826. [Google Scholar] [CrossRef]
- Lunsky, Y.; Albaum, C.; Baskin, A.; Hastings, R.P.; Hutton, S.; Steel, L.; Wang, W.; Weiss, J. Group Virtual Mindfulness-Based Intervention for Parents of Autistic Adolescents and Adults. J. Autism Dev. Disord. 2021, 51, 3959–3969. [Google Scholar] [CrossRef]
- Burgdorf, V.; Szabó, M.; Abbott, M.J. The Effect of Mindfulness Interventions for Parents on Parenting Stress and Youth Psychological Outcomes: A Systematic Review and Meta-Analysis. Front. Psychol. 2019, 10, 1336. [Google Scholar] [CrossRef]
- Kabat-Zinn, J. Where You Go, There You Are: Mindfulness Meditation in Everyday Life; Hyperion: New York, NY, USA, 1994. [Google Scholar]
- Zhang, D.; Lee, E.K.P.; Mak, E.C.W.; Ho, C.Y.; Wong, S.Y.S. Mindfulness-Based Interventions: An Overall Review. Br. Med. Bull. 2021, 138, 41–57. [Google Scholar] [CrossRef]
- Collins, K.R.L.; Best, I.; Stritzke, W.G.K.; Page, A.C. Mindfulness and Zest for Life Buffer the Negative Effects of Experimentally-Induced Perceived Burdensomeness and Thwarted Belongingness: Implications for Theories of Suicide. J. Abnorm. Psychol. 2016, 125, 704–714. [Google Scholar] [CrossRef]
- Geronimi, E.M.C.; Arellano, B.; Woodruff-Borden, J. Relating Mindfulness and Executive Function in Children. Clin. Child Psychol. Psychiatry 2020, 25, 435–445. [Google Scholar] [CrossRef]
- Jespersen, J.E.; Morris, A.S.; Hubbs-Tait, L.; Washburn, I.J. Evaluation of a Parent Education Program Emphasizing Responsive Parenting and Mindfulness: An Inclusive Randomized Controlled Trial. Child Youth Care Forum 2021, 50, 859–883. [Google Scholar] [CrossRef]
- Mouton, B.; Loop, L.; Stiévenart, M.; Roskam, I. Confident Parents for Easier Children: A Parental Self-Efficacy Program to Improve Young Children’s Behavior. Educ. Sci. 2018, 8, 134. [Google Scholar] [CrossRef]
- Neece, C.L. Mindfulness-Based Stress Reduction for Parents of Young Children with Developmental Delays: Implications for Parental Mental Health and Child Behavior Problems. J. Appl. Res. Intellect. Disabil. 2014, 27, 174–186. [Google Scholar] [CrossRef]
- Parent, J.; McKee, L.G.; Rough, J.N.; Forehand, R. The Association of Parent Mindfulness with Parenting and Youth Psychopathology Across Three Developmental Stages. J. Abnorm. Child Psychol. 2016, 44, 191–202. [Google Scholar] [CrossRef]
- Dunning, D.L.; Griffiths, K.; Kuyken, W.; Crane, C.; Foulkes, L.; Parker, J.; Dalgleish, T. Research Review: The Effects of Mindfulness-based Interventions on Cognition and Mental Health in Children and Adolescents—A Meta-analysis of Randomized Controlled Trials. J. Child Psychol. Psychiatry 2019, 60, 244–258. [Google Scholar] [CrossRef]
- Agnafors, S.; Barmark, M.; Sydsjö, G. Mental Health and Academic Performance: A Study on Selection and Causation Effects from Childhood to Early Adulthood. Soc. Psychiatry Psychiatr. Epidemiol. 2021, 56, 857–866. [Google Scholar] [CrossRef]
- Ezmeci, F.; Akman, B. The Impact of the Pre-School Self-Regulation Program on the Self-Regulation, Problem Behavior and Social Skills of Children. Int. J. Educ. Res. 2023, 118, 102156. [Google Scholar] [CrossRef]
- Holtmann, M.; Buchmann, A.F.; Esser, G.; Schmidt, M.H.; Banaschewski, T.; Laucht, M. The Child Behavior Checklist-Dysregulation Profile Predicts Substance Use, Suicidality, and Functional Impairment: A Longitudinal Analysis: CBCL-DP Long-Term Outcome. J. Child Psychol. Psychiatry 2011, 52, 139–147. [Google Scholar] [CrossRef]
- Jiang, Q.; Wang, D.; Yang, Z.; Choi, J. Bidirectional Relationships between Parenting Stress and Child Behavior Problems in Multi-stressed, Single-mother Families: A Cross-lagged Panel Model. Fam. Process 2023, 62, 671–686. [Google Scholar] [CrossRef]
- Heberle, A.E.; Chazan-Cohen, R. Longitudinal and Reciprocal Relations Among Parent and Child Outcomes for Black Early Head Start Families. Early Educ. Dev. 2023, 34, 387–407. [Google Scholar] [CrossRef]
- Mackler, J.S.; Kelleher, R.T.; Shanahan, L.; Calkins, S.D.; Keane, S.P.; O’Brien, M. Parenting Stress, Parental Reactions, and Externalizing Behavior From Ages 4 to 10. J. Marriage Fam. 2015, 77, 388–406. [Google Scholar] [CrossRef]
- Quan, H.; He, J.; Li, C. The Influence of Parental Mindfulness on Preschool Child Behavior Problems: A Chain-Mediated Model Analysis. Int. J. Environ. Res. Public Health 2023, 20, 812. [Google Scholar] [CrossRef]
- Han, Z.R.; Ahemaitijiang, N.; Yan, J.; Hu, X.; Parent, J.; Dale, C.; DiMarzio, K.; Singh, N.N. Parent Mindfulness, Parenting, and Child Psychopathology in China. Mindfulness 2021, 12, 334–343. [Google Scholar] [CrossRef]
- Mann, F.D.; Cuevas, A.G.; Krueger, R.F. Cumulative Stress: A General “s” Factor in the Structure of Stress. Soc. Sci. Med. 2021, 289, 114405. [Google Scholar] [CrossRef]
- Fang, Y.; Luo, J.; Boele, M.; Windhorst, D.; Van Grieken, A.; Raat, H. Parent, Child, and Situational Factors Associated with Parenting Stress: A Systematic Review. Eur. Child Adolesc. Psychiatry 2022. [Google Scholar] [CrossRef]
- Thompson, R.A. Emotional Regulation and Emotional Development. Educ. Psychol. Rev. 1991, 3, 269–307. [Google Scholar] [CrossRef]
- Ochsner, K.N.; Gross, J.J. Thinking Makes It so: A Social Cognitive Neuroscience Approach to Emotion Regulation. In Handbook of Self-Regulation: Research, Theory, and Applications; Baumeister, R.F., Vohs, K.D., Eds.; The Guilford Press: New York, NY, USA, 2004; pp. 229–255. [Google Scholar]
- Masarik, A.S.; Conger, R.D. Stress and Child Development: A Review of the Family Stress Model. Curr. Opin. Psychol. 2017, 13, 85–90. [Google Scholar] [CrossRef]
- Belsky, J. The Determinants of Parenting: A Process Model. Child Dev. 1984, 55, 83. [Google Scholar] [CrossRef]
- Gard, A.M.; McLoyd, V.C.; Mitchell, C.; Hyde, L.W. Evaluation of a Longitudinal Family Stress Model in a Population-based Cohort. Soc. Dev. 2020, 29, 1155–1175. [Google Scholar] [CrossRef]
- Kavanaugh, S.A.; Neppl, T.K.; Melby, J.N. Economic Pressure and Depressive Symptoms: Testing the Family Stress Model from Adolescence to Adulthood. J. Fam. Psychol. 2018, 32, 957–965. [Google Scholar] [CrossRef]
- Taraban, L.; Shaw, D.S. Parenting in Context: Revisiting Belsky’s Classic Process of Parenting Model in Early Childhood. Dev. Rev. 2018, 48, 55–81. [Google Scholar] [CrossRef]
- Van Eldik, W.M.; De Haan, A.D.; Arends, L.R.; Belsky, J.; Prinzie, P. Personality, Depressive Symptoms, the Interparental Relationship and Parenting: Prospective Associations of an Actor–Partner Interdependency Model. J. Fam. Psychol. 2019, 33, 671–681. [Google Scholar] [CrossRef]
- Patterson, G.R. Coercive Family Processes; Castalia: Eugene, OR, USA, 1982. [Google Scholar]
- Lunkenheimer, E.; Sturge-Apple, M.L.; Kelm, M.R. The Importance of Parent Self-regulation and Parent–Child Coregulation in Research on Parental Discipline. Child Dev. Perspect. 2023, 17, 25–31. [Google Scholar] [CrossRef]
- Brown, E.D.; Holochwost, S.J.; Laurenceau, J.; Garnett, M.L.; Anderson, K.E. Deconstructing Cumulative Risk: Poverty and Aspects of Instability Relate Uniquely to Young Children’s Basal Cortisol. Child Dev. 2021, 92, 1067–1082. [Google Scholar] [CrossRef]
- Goulet, M.; Clément, M.-E.; Helie, S.; Villatte, A. Longitudinal Association Between Risk Profiles, School Dropout Risk, and Substance Abuse in Adolescence. Child Youth Care Forum 2020, 49, 687–706. [Google Scholar] [CrossRef]
- Fan, X.; Fang, X.; Zhao, X.; Chen, F. The Effect of Cumulative Risk Related to Family Adversity on Social Adjustment among Left-behind Children in China: The Mediating Role of Stress and the Moderating Role of Psychosocial Resources. Acta Psychol. Sin. 2023, 55, 1270. [Google Scholar] [CrossRef]
- Rodriguez-JenKins, J.; Marcenko, M.O. Parenting Stress among Child Welfare Involved Families: Differences by Child Placement. Child. Youth Serv. Rev. 2014, 46, 19–27. [Google Scholar] [CrossRef]
- Jennings, W.G.; Reingle, J.M.; Staras, S.A.S.; Maldonado-Molina, M.M. Substance Use as a Risk Factor for Intimate Partner Violence Overlap: Generational Differences Among Hispanic Young Adults. Int. Crim. Justice Rev. 2012, 22, 139–152. [Google Scholar] [CrossRef]
- Deighton, J.; Lereya, S.T.; Casey, P.; Patalay, P.; Humphrey, N.; Wolpert, M. Prevalence of Mental Health Problems in Schools: Poverty and Other Risk Factors among 28 000 Adolescents in England. Br. J. Psychiatry 2019, 215, 565–567. [Google Scholar] [CrossRef]
- Parra, G.R.; Smith, G.L.; Mason, W.A.; Savolainen, J.; Chmelka, M.B.; Miettunen, J.; Järvelin, M.-R.; Moilanen, I.; Veijola, J. Profiles of Contextual Risk at Birth and Adolescent Substance Use. J. Child Fam. Stud. 2018, 27, 717–724. [Google Scholar] [CrossRef]
- Hassan-Abbas, N.M. Resilience and Risk Factors Predict Family Stress Among Married Palestinians in Israel During the COVID-19 Pandemic. Front. Psychol. 2022, 13, 913330. [Google Scholar] [CrossRef]
- Steele, H.; Bate, J.; Steele, M.; Dube, S.R.; Danskin, K.; Knafo, H.; Nikitiades, A.; Bonuck, K.; Meissner, P.; Murphy, A. Adverse Childhood Experiences, Poverty, and Parenting Stress. Can. J. Behav. Sci. Rev. Can. Sci. Comport. 2016, 48, 32–38. [Google Scholar] [CrossRef]
- de Carvalho, J.S.; Oliveira, S.; Roberto, M.S.; Gonçalves, C.; Bárbara, J.M.; de Castro, A.F.; Pereira, R.; Franco, M.; Cadima, J.; Leal, T.; et al. Effects of a Mindfulness-Based Intervention for Teachers: A Study on Teacher and Student Outcomes. Mindfulness 2021, 12, 1719–1732. [Google Scholar] [CrossRef]
- Kinman, G.; Grant, L.; Kelly, S. ‘It’s My Secret Space’: The Benefits of Mindfulness for Social Workers. Br. J. Soc. Work 2020, 50, 758–777. [Google Scholar] [CrossRef]
- Creswell, J.D.; Lindsay, E.K. How Does Mindfulness Training Affect Health? A Mindfulness Stress Buffering Account. Curr. Dir. Psychol. Sci. 2014, 23, 401–407. [Google Scholar] [CrossRef]
- Lucas-Thompson, R.G.; Prince, M.A.; Adams, M.S.; Miller, R.L.; Moran, M.J.; Rayburn, S.R.; Seiter, N.S. Does a Mindfulness-Based Intervention Strengthen Mindfulness Stress Buffering Effects in Adolescence? A Preliminary Investigation. Curr. Psychol. 2023. [Google Scholar] [CrossRef]
- MacAulay, R.K.; Brown, L.F.; Moore, L. Mindfulness Stress-Buffering Model of Health: Implications for Successful Aging. Aging Ment. Health 2023, 27, 1592–1599. [Google Scholar] [CrossRef]
- Mutumba, M.; Moskowitz, J.T.; Neilands, T.B.; Lee, J.-Y.; Dilworth, S.E.; Carrico, A.W. A Mindfulness-Based, Stress and Coping Model of Craving in Methamphetamine Users. PLoS ONE 2021, 16, e0249489. [Google Scholar] [CrossRef]
- Kudesia, R.S.; Pandey, A.; Reina, C.S. Doing More With Less: Interactive Effects of Cognitive Resources and Mindfulness Training in Coping With Mental Fatigue From Multitasking. J. Manag. 2022, 48, 410–439. [Google Scholar] [CrossRef]
- Chaplin, T.M.; Mauro, K.L.; Curby, T.W.; Niehaus, C.; Fischer, S.; Turpyn, C.C.; Martelli, A.M.; Miller, A.B.; Leichtweis, R.N.; Baer, R.; et al. Effects of A Parenting-Focused Mindfulness Intervention on Adolescent Substance Use and Psychopathology: A Randomized Controlled Trial. Res. Child Adolesc. Psychopathol. 2021, 49, 861–875. [Google Scholar] [CrossRef]
- Brown, S.M.; Bellamy, J. Feasibility, Acceptability, and Clinical Trends of a Mindfulness-Informed Child Welfare Intervention: Implications for Trauma-Focused Practice. Adv. Soc. Work 2017, 18, 369–386. [Google Scholar] [CrossRef]
- Reid, N.; Dawe, S.; Harnett, P.; Shelton, D.; Hutton, L.; O’Callaghan, F. Feasibility Study of a Family-Focused Intervention to Improve Outcomes for Children with FASD. Res. Dev. Disabil. 2017, 67, 34–46. [Google Scholar] [CrossRef]
- Zhang, L.; Lopes, S.; Lavelle, T.; Jones, K.O.; Chen, L.; Jindal, M.; Zinzow, H.; Shi, L. Economic Evaluations of Mindfulness-Based Interventions: A Systematic Review. Mindfulness 2022, 13, 2359–2378. [Google Scholar] [CrossRef]
- Singh, N.N.; Lancioni, G.E.; Medvedev, O.N.; Hwang, Y.-S.; Myers, R.E. A Component Analysis of the Mindfulness-Based Positive Behavior Support (MBPBS) Program for Mindful Parenting by Mothers of Children with Autism Spectrum Disorder. Mindfulness 2021, 12, 463–475. [Google Scholar] [CrossRef]
- Compas, B.E.; Jaser, S.S.; Bettis, A.H.; Watson, K.H.; Gruhn, M.A.; Dunbar, J.P.; Williams, E.; Thigpen, J.C. Coping, Emotion Regulation, and Psychopathology in Childhood and Adolescence: A Meta-Analysis and Narrative Review. Psychol. Bull. 2017, 143, 939–991. [Google Scholar] [CrossRef]
- Lazarus, R.S.; Folkman, S. Stress, Appraisal, and Coping; Springer Publishing Company: New York, NY, USA, 1984; ISBN 978-0-8261-4192-7. [Google Scholar]
- Kalisch, R.; Müller, M.B.; Tüscher, O. A Conceptual Framework for the Neurobiological Study of Resilience. Behav. Brain Sci. 2015, 38, e92. [Google Scholar] [CrossRef]
- Riepenhausen, A.; Wackerhagen, C.; Reppmann, Z.C.; Deter, H.-C.; Kalisch, R.; Veer, I.M.; Walter, H. Positive Cognitive Reappraisal in Stress Resilience, Mental Health, and Well-Being: A Comprehensive Systematic Review. Emot. Rev. 2022, 14, 310–331. [Google Scholar] [CrossRef]
- de Vibe, M.; Solhaug, I.; Rosenvinge, J.H.; Tyssen, R.; Hanley, A.; Garland, E. Six-Year Positive Effects of a Mindfulness-Based Intervention on Mindfulness, Coping and Well-Being in Medical and Psychology Students; Results from a Randomized Controlled Trial. PLoS ONE 2018, 13, e0196053. [Google Scholar] [CrossRef]
- Choi, H.S.; Lee, K.E.; Shin, Y. Effects of an Emotional Regulation Program on Maladaptive Cognitive Emotion Regulation, Stress, Anxiety, and Postpartum Depression among South Korean Mothers of Premature Infants in the Neonatal Intensive Care Unit. Child Health Nurs. Res. 2021, 27, 24–33. [Google Scholar] [CrossRef]
- Kakhki, Z.B.; Mashhadi, A.; Yazdi, S.A.A.; Saleh, S. The Effect of Mindful Parenting Training on Parent–Child Interactions, Parenting Stress, and Cognitive Emotion Regulation in Mothers of Preschool Children. J. Child Fam. Stud. 2022, 31, 3113–3124. [Google Scholar] [CrossRef]
- Jones, D.R.; Lehman, B.J.; Noriega, A.; Dinnel, D.L. The Effects of a Short-Term Mindfulness Meditation Intervention on Coping Flexibility. Anxiety Stress Coping 2019, 32, 347–361. [Google Scholar] [CrossRef]
- Tang, Y.-Y.; Hölzel, B.K.; Posner, M.I. Traits and States in Mindfulness Meditation. Nat. Rev. Neurosci. 2016, 17, 59. [Google Scholar] [CrossRef]
- Götmann, A.; Bechtoldt, M.N. Coping with COVID-19—Longitudinal Analysis of Coping Strategies and the Role of Trait Mindfulness in Mental Well-Being. Personal. Individ. Differ. 2021, 175, 110695. [Google Scholar] [CrossRef]
- Folkman, S.; Moskowitz, J.T. Coping: Pitfalls and Promise. Annu. Rev. Psychol. 2004, 55, 745–774. [Google Scholar] [CrossRef]
- Almeida, D.; Monteiro, D.; Rodrigues, F. Satisfaction with Life: Mediating Role in the Relationship between Depressive Symptoms and Coping Mechanisms. Healthcare 2021, 9, 787. [Google Scholar] [CrossRef]
- Kaba, D.; Hasanlı, J.; Efe, A.; Yavuz-Çolak, M.; Akın-Sarı, B. Predictors of Burnout and Distress in Parents of Children with Autism Spectrum Disorder during COVID-19 Home Confinement. Child. Health Care 2023, 52, 409–429. [Google Scholar] [CrossRef]
- Hamama-Raz, Y.; Pat-Horenczyk, R.; Perry, S.; Ziv, Y.; Bar-Levav, R.; Stemmer, S.M. The Effectiveness of Group Intervention on Enhancing Cognitive Emotion Regulation Strategies in Breast Cancer Patients: A 2-Year Follow-Up. Integr. Cancer Ther. 2016, 15, 175–182. [Google Scholar] [CrossRef]
- Salgó, E.; Szeghalmi, L.; Bajzát, B.; Berán, E.; Unoka, Z. Emotion Regulation, Mindfulness, and Self-Compassion among Patients with Borderline Personality Disorder, Compared to Healthy Control Subjects. PLoS ONE 2021, 16, e0248409. [Google Scholar] [CrossRef]
- de Kruijff, L.G.M.; Moussault, O.R.M.; Plat, M.-C.J.; Hoencamp, R.; van der Wurff, P. Coping Strategies of Dutch Servicemembers after Deployment. Mil. Med. Res. 2019, 6, 9. [Google Scholar] [CrossRef]
- Ni’matuzahroh; Suen, M.-W.; Ningrum, V.; Widayat; Yuniardi, M.S.; Hasanati, N.; Wang, J.-H. The Association between Parenting Stress, Positive Reappraisal Coping, and Quality of Life in Parents with Autism Spectrum Disorder (ASD) Children: A Systematic Review. Healthcare 2021, 10, 52. [Google Scholar] [CrossRef]
- Skinner, E.A.; Zimmer-Gembeck, M.J. Parenting, Family Stress, Developmental Cascades, and the Differential Development of Coping. In The Development of Coping; Springer International Publishing: Cham, Switzerland, 2016; pp. 239–261. ISBN 978-3-319-41738-7. [Google Scholar]
- Dix, T. Attributing Dispositions to Children: An Interactional Analysis of Attribution in Socialization. Pers. Soc. Psychol. Bull. 1993, 19, 633–643. [Google Scholar] [CrossRef]
- Miller, N.V.; Johnston, C. Associations Between Parent and Child Attributions for Negative Events. Merrill-Palmer Q. 2019, 65, 183. [Google Scholar] [CrossRef]
- McCubbin, H.I.; Patterson, J.M. The Family Stress Process: The Double ABCX Model of Adjustment and Adaptation. Marriage Fam. Rev. 1983, 6, 7–37. [Google Scholar] [CrossRef]
- Meleady, J.; Nearchou, F.; Bramham, J.; Carr, A. Family Adaptation among Parents of Children on the Autism Spectrum without a Comorbid Intellectual Disability: A Test of the Double ABCX Model. Res. Autism Spectr. Disord. 2020, 78, 101637. [Google Scholar] [CrossRef]
- Brown, S.M.; Bender, K.A.; Bellamy, J.L.; Garland, E.L.; Dmitrieva, J.; Jenson, J.M. A Pilot Randomized Trial of a Mindfulness-Informed Intervention for Child Welfare-Involved Families. Mindfulness 2021, 12, 420–435. [Google Scholar] [CrossRef]
- Enke, B.; Gneezy, U.; Hall, B.; Martin, D.; Nelidov, V.; Offerman, T.; Van De Ven, J. Cognitive Biases: Mistakes or Missing Stakes? Rev. Econ. Stat. 2023, 105, 818–832. [Google Scholar] [CrossRef]
- Sittenthaler, H.M.; Mohnen, A. Cash, Non-Cash, or Mix? Gender Matters! The Impact of Monetary, Non-Monetary, and Mixed Incentives on Performance. J. Bus. Econ. 2020, 90, 1253–1284. [Google Scholar] [CrossRef]
- Taani, M.H.; Zabler, B.; Fendrich, M.; Schiffman, R. Lessons Learned for Recruitment and Retention of Low-Income African Americans. Contemp. Clin. Trials Commun. 2020, 17, 100533. [Google Scholar] [CrossRef]
- Garnefski, N.; Kraaij, V. Cognitive Emotion Regulation Questionnaire—Development of a Short 18-Item Version (CERQ-Short). Personal. Individ. Differ. 2006, 41, 1045–1053. [Google Scholar] [CrossRef]
- Keleynikov, M.; Benatov, J.; Berger, R. Preschool Teachers’ Psychological Distress and Work Engagement during COVID-19 Outbreak: The Protective Role of Mindfulness and Emotion Regulation. Int. J. Environ. Res. Public. Health 2022, 19, 2645. [Google Scholar] [CrossRef]
- Mason, C.K.; Mullins-Sweatt, S.N. Catastrophizing, Negative Affectivity, and Borderline Personality Disorder. Personal. Ment. Health 2021, 15, 283–292. [Google Scholar] [CrossRef]
- Koç, M.S.; Uzun, R.B. Investigating the Link Between Dispositional Mindfulness, Beliefs About Emotions, Emotion Regulation and Psychological Health: A Model Testing Study. J. Ration.-Emotive Cogn.-Behav. Ther. 2023. [Google Scholar] [CrossRef]
- Achenbach, T.M.; Rescorla, L.A. Manual for the ASEBA Preschool Forms & Profiles; University of Vermont, Research Center for Children, Youth & Famillies: Burlington, VT, USA, 2000. [Google Scholar]
- Achenbach, T.M.; Rescorla, L.A. Manual for the ASEBA School-Age Forms & Profiles; University of Vermont, Research Center for Children, Youth & Famillies: Burlington, VT, USA, 2001. [Google Scholar]
- Mansolf, M.; Blackwell, C.K.; Cummings, P.; Choi, S.; Cella, D. Linking the Child Behavior Checklist to the Strengths and Difficulties Questionnaire. Psychol. Assess. 2022, 34, 233–246. [Google Scholar] [CrossRef]
- Tiego, J.; Martin, E.A.; DeYoung, C.G.; Hagan, K.; Cooper, S.E.; Pasion, R.; Satchell, L.; Shackman, A.J.; Bellgrove, M.A.; Fornito, A.; et al. Precision Behavioral Phenotyping as a Strategy for Uncovering the Biological Correlates of Psychopathology. Nat. Ment. Health 2023, 1, 304–315. [Google Scholar] [CrossRef]
- Lees, B.; Stapinski, L.A.; Teesson, M.; Squeglia, L.M.; Jacobus, J.; Mewton, L. Problems Experienced by Children from Families with Histories of Substance Misuse: An ABCD Study®. Drug Alcohol Depend. 2021, 218, 108403. [Google Scholar] [CrossRef]
- Osborne, C.; Berger, L.M. Parental Substance Abuse and Child Well-Being: A Consideration of Parents’ Gender and Coresidence. J. Fam. Issues 2009, 30, 341–370. [Google Scholar] [CrossRef]
- Küchler, A.-M.; Schultchen, D.; Dretzler, T.; Moshagen, M.; Ebert, D.D.; Baumeister, H. A Three-Armed Randomized Controlled Trial to Evaluate the Effectiveness, Acceptance, and Negative Effects of StudiCare Mindfulness, an Internet- and Mobile-Based Intervention for College Students with No and “On Demand” Guidance. Int. J. Environ. Res. Public Health 2023, 20, 3208. [Google Scholar] [CrossRef]
- DeVellis, R.F. Scale Development: Theory and Applications; Sage Publications, Inc.: Thousand Oaks, CA, USA, 1991. [Google Scholar]
- Dziuban, C.D.; Shirkey, E.C. When Is a Correlation Matrix Appropriate for Factor Analysis? Some Decision Rules. Psychol. Bull. 1974, 81, 358–361. [Google Scholar] [CrossRef]
- Pett, M.A.; Lackey, N.R.; Sullivan, J.J. Making Sense of Factor Analysis: The Use of Factor Analysis for Instrument Development in Health Care Reserach; SAGE Publications, Inc.: Thousand Oaks, CA, USA, 2003. [Google Scholar]
- Tabachnick, B.G.; Fidell, L.S. Using Multivariate Statistics, 5th ed.; Allyn & Bacon/Pearson Education: Boston, MA, USA, 2007. [Google Scholar]
- Ledesma, R.D.; Valero-Mora, P. Determining the Number of Factors to Retain in EFA: An Easy-to-Use Computer Program for Carrying out Parallel Analysis. Pract. Assess. Res. Evalution 2019, 12, 2. [Google Scholar] [CrossRef]
- Comrey, A.L.; Lee, H.B. A First Course in Factor Analysis, 2nd ed.; Lawrence Erlbaum Associates, Inc.: Mahwah, NJ, USA, 1992. [Google Scholar]
- McCoy, E. Understanding the Intention-to-Treat Principle in Randomized Controlled Trials. West. J. Emerg. Med. 2017, 18, 1075–1078. [Google Scholar] [CrossRef]
- Hedges, L.V. Distribution Theory for Glass’s Estimator of Effect Size and Related Estimators. J. Educ. Stat. 1981, 6, 107. [Google Scholar] [CrossRef]
- Ewert, C.; Vater, A.; Schröder-Abé, M. Self-Compassion and Coping: A Meta-Analysis. Mindfulness 2021, 12, 1063–1077. [Google Scholar] [CrossRef]
- Shorey, S.; Ng, E.D. The Efficacy of Mindful Parenting Interventions: A Systematic Review and Meta-Analysis. Int. J. Nurs. Stud. 2021, 121, 103996. [Google Scholar] [CrossRef]
- Schumm, W.R. Navigating Treacherous Waters—One Researcher’s 40 Years of Experience with Controversial Scientific Research. Compr. Psychol. 2015, 4, 17.CP.4.24. [Google Scholar] [CrossRef]
- Bernardi, R.A.; Nash, J. The Importance and Efficacy of Controlling for Social Desirability Response Bias. Ethics Behav. 2023, 33, 413–429. [Google Scholar] [CrossRef]
- Baminiwatta, A.; Solangaarachchi, I. Trends and Developments in Mindfulness Research over 55 Years: A Bibliometric Analysis of Publications Indexed in Web of Science. Mindfulness 2021, 12, 2099–2116. [Google Scholar] [CrossRef]
- Baer, R.A.; Smith, G.T.; Lykins, E.; Button, D.; Krietemeyer, J.; Sauer, S.; Walsh, E.; Duggan, D.; Williams, J.M.G. Construct Validity of the Five Facet Mindfulness Questionnaire in Meditating and Nonmeditating Samples. Assessment 2008, 15, 329–342. [Google Scholar] [CrossRef]
- Bednar, K.; Voracek, M.; Tran, U.S. Common Factors Underlying the Five Facets of Mindfulness and Proposed Mechanisms: A Psychometric Study Among Meditators and Non-Meditators. Mindfulness 2020, 11, 2804–2817. [Google Scholar] [CrossRef]
- Meier, B.P.; Konrath, S.; Fetterman, A.K.; Dillard, A.J.; James, C.; Weinstein, E.; Bushman, B.J. Development and Validation of the Single-Item Mindfulness Scale (SIMS). J. Pers. Assess. 2023, 105, 807–819. [Google Scholar] [CrossRef]
| Session | Cohort 1 | Cohort 2 |
|---|---|---|
| 1 | Mindfulness in the context of automatic habits | Mindful parenting and problem solving |
| 2 | Mindful reappraisal | Triggers of stress |
| 3 | Savoring positive experiences | Children’s needs |
| 4 | Triggers of stress | Stress reduction |
| 5 | Mindful parenting | Problem solving |
| 6 | Mindful planning | Mindful planning |
| Item | Loadings | ||
|---|---|---|---|
| 1 | 2 | 3 | |
| I think that I can become a stronger person because of what has happened | 0.785 | −0.166 | −0.201 |
| I think I can learn something from this situation | 0.750 | −0.142 | −0.265 |
| I think that I have to accept the situation | 0.575 | 0.197 | −0.455 |
| I think about how to change the situation | 0.621 | 0.342 | 0.141 |
| I think about a plan of what I can do best | 0.681 | 0.060 | −0.169 |
| I tell myself that there are worse things in life | 0.589 | −0.369 | −0.040 |
| I often think about how I feel about what I have experienced | 0.343 | 0.615 | 0.149 |
| I am preoccupied with what I think and feel about what I have experienced | −0.147 | 0.723 | 0.240 |
| I keep thinking about how terrible it is what I have experienced | 0.130 | 0.817 | −0.034 |
| I continually overthink how horrible the situation has been | −0.076 | 0.816 | −0.222 |
| I think of pleasant things that have nothing to do with it | 0.520 | −0.076 | 0.670 |
| I think of something nice instead of what has happened | 0.392 | −0.055 | 0.747 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Krause, J.T.; Brown, S.M. Mindfulness Intervention Improves Coping and Perceptions of Children’s Behavior among Families with Elevated Risk. Int. J. Environ. Res. Public Health 2023, 20, 7092. https://doi.org/10.3390/ijerph20237092
Krause JT, Brown SM. Mindfulness Intervention Improves Coping and Perceptions of Children’s Behavior among Families with Elevated Risk. International Journal of Environmental Research and Public Health. 2023; 20(23):7092. https://doi.org/10.3390/ijerph20237092
Chicago/Turabian StyleKrause, Jill T., and Samantha M. Brown. 2023. "Mindfulness Intervention Improves Coping and Perceptions of Children’s Behavior among Families with Elevated Risk" International Journal of Environmental Research and Public Health 20, no. 23: 7092. https://doi.org/10.3390/ijerph20237092
APA StyleKrause, J. T., & Brown, S. M. (2023). Mindfulness Intervention Improves Coping and Perceptions of Children’s Behavior among Families with Elevated Risk. International Journal of Environmental Research and Public Health, 20(23), 7092. https://doi.org/10.3390/ijerph20237092






