Sex Differences in E-Cigarette Use and Related Health Effects
Abstract
1. Introduction
2. Materials and Methods
3. Results
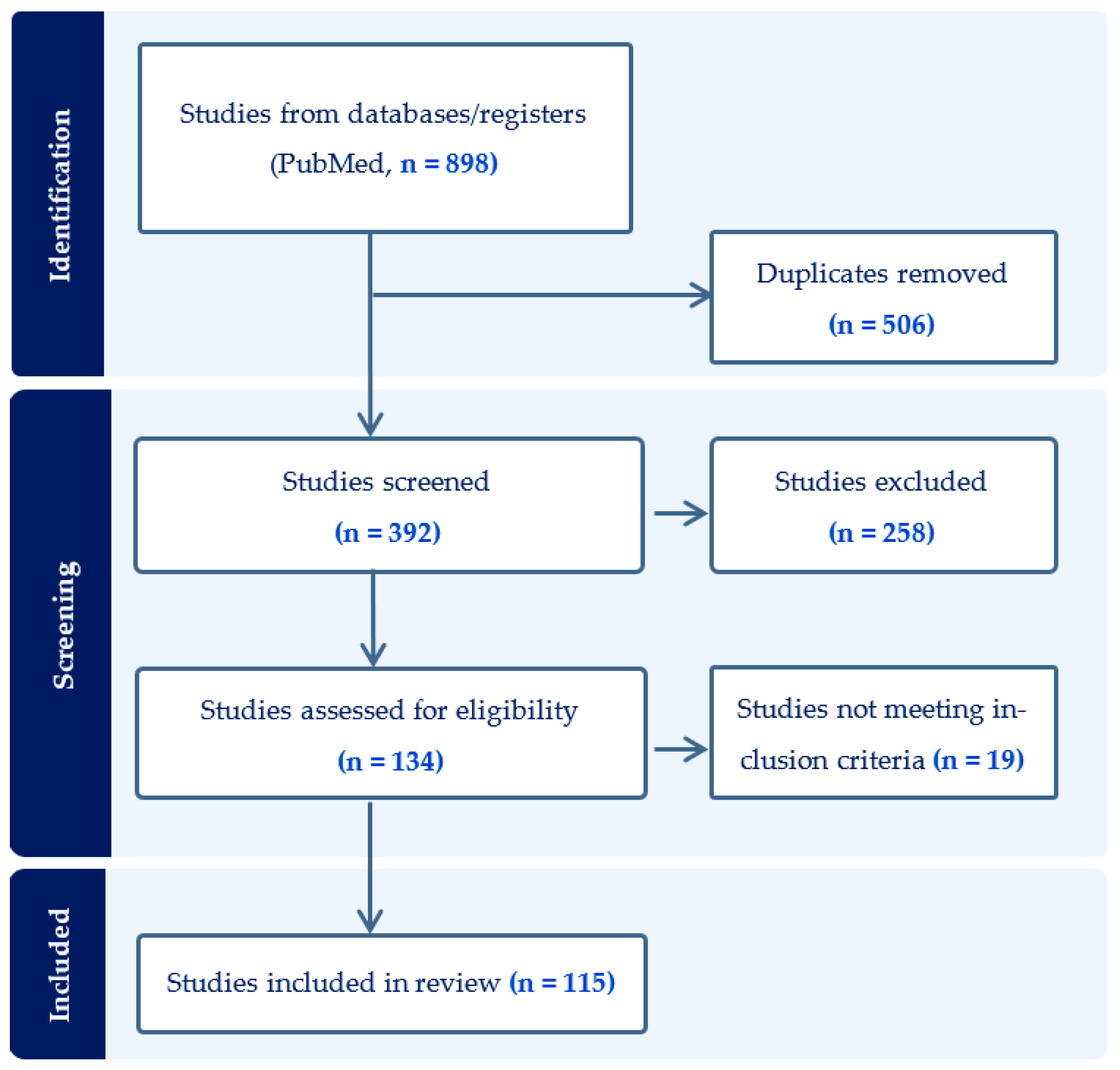
3.1. Search Results
3.2. Sex Differences in Predictors and Risk Factors for E-Cigarette Use
3.2.1. Sex Differences in E-Cigarette Use and Initiation
3.2.2. Sex Differences in E-Cigarette Use for Smoking Cessation and Polysubstance Use
3.2.3. Sex Differences in E-Cigarette Flavor Use, Device Choice, and Preference
3.2.4. Impact of the COVID-19 Pandemic on E-Cigarette Use
3.2.5. Other Sex-Specific Factors Influencing E-Cigarette Use
3.3. Sex Differences in General Effects of E-Cigarette Use in Organ Systems
3.3.1. Clinical Studies Assessing Organ System Effects in Males and Females
Cardiopulmonary Effects
Central Nervous System Effects
3.3.2. Preclinical Studies Assessing Organ System Effects in Males and Females
3.4. Sex Differences in Behavioral Effects and Gender-Specific Effects of E-Cigarette Use
3.4.1. Sex-Dependent Behavioral Effects Associated with E-Cigarette Use
3.4.2. E-Cigarette Use in Sexual Minorities
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Marques, P.; Piqueras, L.; Sanz, M.J. An updated overview of e-cigarette impact on human health. Respir. Res. 2021, 22, 151. [Google Scholar] [CrossRef]
- Esteban-Lopez, M.; Perry, M.D.; Garbinski, L.D.; Manevski, M.; Andre, M.; Ceyhan, Y.; Caobi, A.; Paul, P.; Lau, L.S.; Ramelow, J.; et al. Health effects and known pathology associated with the use of E-cigarettes. Toxicol. Rep. 2022, 9, 1357–1368. [Google Scholar] [CrossRef]
- Tsai, M.; Byun, M.K.; Shin, J.; Crotty Alexander, L.E. Effects of e-cigarettes and vaping devices on cardiac and pulmonary physiology. J. Physiol. 2020, 598, 5039–5062. [Google Scholar] [CrossRef]
- Birdsey, J.; Cornelius, M.; Jamal, A.; Park-Lee, E.; Cooper, M.; Wang, J.; Sawdey, M.; Cullen, K.; Neff, L. Tobacco Product Use among U.S. Middle and High School Students—National Youth Tobacco Survey, 2023; MMWR Morb Mortal Wkly Rep 2023; pp. 1173–1182. Available online: https://www.cdc.gov/mmwr/volumes/72/wr/mm7244a1.htm (accessed on 12 October 2023).
- Butler, A.R.; Lindson, N.; Fanshawe, T.R.; Theodoulou, A.; Begh, R.; Hajek, P.; McRobbie, H.; Bullen, C.; Notley, C.; Rigotti, N.A.; et al. Longer-term use of electronic cigarettes when provided as a stop smoking aid: Systematic review with meta-analyses. Prev. Med. 2022, 165, 107182. [Google Scholar] [CrossRef]
- Hartmann-Boyce, J.; Lindson, N.; Butler, A.R.; McRobbie, H.; Bullen, C.; Begh, R.; Theodoulou, A.; Notley, C.; Rigotti, N.A.; Turner, T.; et al. Electronic cigarettes for smoking cessation. Cochrane Database Syst. Rev. 2022, 11, CD010216. [Google Scholar] [CrossRef]
- Polosa, R.; Morjaria, J.B.; Prosperini, U.; Busà, B.; Pennisi, A.; Malerba, M.; Maglia, M.; Caponnetto, P. COPD smokers who switched to e-cigarettes: Health outcomes at 5-year follow up. Ther. Adv. Chronic Dis. 2020, 11, 2040622320961617. [Google Scholar] [CrossRef]
- Hajek, P.; Phillips-Waller, A.; Przulj, D.; Pesola, F.; Myers Smith, K.; Bisal, N.; Li, J.; Parrott, S.; Sasieni, P.; Dawkins, L.; et al. A Randomized Trial of E-Cigarettes versus Nicotine-Replacement Therapy. N. Engl. J. Med. 2019, 380, 629–637. [Google Scholar] [CrossRef]
- Fetterman, J.L.; Keith, R.J.; Palmisano, J.N.; McGlasson, K.L.; Weisbrod, R.M.; Majid, S.; Bastin, R.; Stathos, M.M.; Stokes, A.C.; Robertson, R.M.; et al. Alterations in Vascular Function Associated With the Use of Combustible and Electronic Cigarettes. J. Am. Heart Assoc. 2020, 9, e014570. [Google Scholar] [CrossRef]
- Sathish, V.; Freeman, M.R.; Long, E.; Thompson, M.A.; Pabelick, C.M.; Prakash, Y.S. Cigarette Smoke and Estrogen Signaling in Human Airway Smooth Muscle. Cell Physiol. Biochem. 2015, 36, 1101–1115. [Google Scholar] [CrossRef]
- Gasperino, J. Gender is a risk factor for lung cancer. Med. Hypotheses 2011, 76, 328–331. [Google Scholar] [CrossRef]
- Liao, M.; Braunstein, Z.; Rao, X. Sex differences in particulate air pollution-related cardiovascular diseases: A review of human and animal evidence. Sci. Total Environ. 2023, 884, 163803. [Google Scholar] [CrossRef]
- Zou, M.L.; Huang, H.C.; Chen, Y.H.; Jiang, C.B.; Wu, C.D.; Lung, S.C.; Chien, L.C.; Lo, Y.C.; Chao, H.J. Sex-differences in the effects of indoor air pollutants and household environment on preschool child cognitive development. Sci. Total Environ. 2023, 860, 160365. [Google Scholar] [CrossRef]
- Shin, H.H.; Maquiling, A.; Thomson, E.M.; Park, I.W.; Stieb, D.M.; Dehghani, P. Sex-difference in air pollution-related acute circulatory and respiratory mortality and hospitalization. Sci. Total Environ. 2022, 806, 150515. [Google Scholar] [CrossRef] [PubMed]
- Shin, H.H.; Parajuli, R.P.; Gogna, P.; Maquiling, A.; Dehghani, P. Pollutant-sex specific differences in respiratory hospitalization and mortality risk attributable to short-term exposure to ambient air pollution. Sci. Total Environ. 2021, 755, 143135. [Google Scholar] [CrossRef] [PubMed]
- Vancza, E.M.; Galdanes, K.; Gunnison, A.; Hatch, G.; Gordon, T. Age, strain, and gender as factors for increased sensitivity of the mouse lung to inhaled ozone. Toxicol. Sci. 2009, 107, 535–543. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sabeti, Z.; Ansarin, A.; Ansarin, K.; Zafari, V.; Seyedrezazadeh, E.; Shakerkhatibi, M.; Asghari-Jafarabadi, M.; Dastgiri, S.; Zoroufchi Benis, K.; Sepehri, M.; et al. Sex-specific association of exposure to air pollutants and Nrf2 gene expression and inflammatory biomarkers in exhaled breath of healthy adolescents. Environ. Pollut. 2023, 326, 121463. [Google Scholar] [CrossRef] [PubMed]
- Lanza, H.I.; Teeter, H. Electronic Nicotine Delivery Systems (E-cigarette/Vape) use and Co-Occurring Health-Risk Behaviors Among an Ethnically Diverse Sample of Young Adults. Subst. Use Misuse 2018, 53, 154–161. [Google Scholar] [CrossRef]
- Browne, M.; Todd, D.G. Then and now: Consumption and dependence in e-cigarette users who formerly smoked cigarettes. Addict. Behav. 2018, 76, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Kong, G.; Morean, M.E.; Cavallo, D.A.; Camenga, D.R.; Krishnan-Sarin, S. Sources of electronic cigarette acquisition among adolescents in Connecticut. Tob. Regul. Sci. 2017, 3, 10–16. [Google Scholar] [CrossRef]
- Wong, D.N.; Fan, W. Ethnic and sex differences in E-cigarette use and relation to alcohol use in California adolescents: The California Health Interview Survey. Public Health 2018, 157, 147–152. [Google Scholar] [CrossRef]
- Bunch, K.; Fu, M.; Ballbè, M.; Matilla-Santader, N.; Lidón-Moyano, C.; Martin-Sanchez, J.C.; Fernandez, E.; Martínez-Sánchez, J.M. Motivation and main flavour of use, use with nicotine and dual use of electronic cigarettes in Barcelona, Spain: A cross-sectional study. BMJ Open 2018, 8, e018329. [Google Scholar] [CrossRef] [PubMed]
- Kopp, B.T.; Hinton, A.; Lu, R.; Cooper, S.; Nagaraja, H.; Wewers, M.E. Impact of Presence of Children on Indoor Tobacco Restrictions in Households of Urban and Rural Adult Tobacco Users. Acad. Pediatr. 2018, 18, 920–927. [Google Scholar] [CrossRef] [PubMed]
- Mostafa, A.; El Houssinie, M.; Fotouh, A.A. Multiple tobacco use among young adult waterpipe smokers in Egypt. East. Mediterr. Health J. 2018, 24, 7–17. [Google Scholar] [CrossRef] [PubMed]
- King, J.L.; Reboussin, D.; Cornacchione Ross, J.; Wiseman, K.D.; Wagoner, K.G.; Sutfin, E.L. Polytobacco Use Among a Nationally Representative Sample of Adolescent and Young Adult E-Cigarette Users. J. Adolesc. Health 2018, 63, 407–412. [Google Scholar] [CrossRef]
- Jongenelis, M.I.; Brennan, E.; Slevin, T.; Kameron, C.; Rudaizky, D.; Pettigrew, S. Differences in use of electronic nicotine delivery systems by smoking status and demographic characteristics among Australian young adults. Health Promot. J. Aust. 2019, 30, 207–211. [Google Scholar] [CrossRef]
- Morean, M.E.; Krishnan-Sarin, S.; Sussman, S.; Foulds, J.; Fishbein, H.; Grana, R.; Halpern-Felsher, B.; Kim, H.; Weaver, S.R.; O’Malley, S.S. Development and psychometric validation of a novel measure of sensory expectancies associated with E-cigarette use. Addict. Behav. 2019, 91, 208–215. [Google Scholar] [CrossRef]
- Hammond, D.; Wackowski, O.A.; Reid, J.L.; O’Connor, R.J. Use of JUUL E-cigarettes Among Youth in the United States. Nicotine Tob. Res. 2020, 22, 827–832. [Google Scholar] [CrossRef]
- Ma, J.Z.; Hart, J.L.; Walker, K.L.; Giachello, A.L.; Groom, A.; Landry, R.L.; Tompkins, L.K.; Vu, T.T.; Mattingly, D.T.; Sears, C.G.; et al. Perceived health risks of electronic nicotine delivery systems (ENDS) users: The role of cigarette smoking status. Addict. Behav. 2019, 91, 156–163. [Google Scholar] [CrossRef]
- Kasza, K.A.; Coleman, B.; Sharma, E.; Conway, K.P.; Cummings, K.M.; Goniewicz, M.L.; Niaura, R.S.; Lambert, E.Y.; Schneller, L.M.; Feirman, S.P.; et al. Correlates of Transitions in Tobacco Product Use by U.S. Adult Tobacco Users between 2013–2014 and 2014–2015: Findings from the PATH Study Wave 1 and Wave 2. Int. J. Environ. Res. Public Health 2018, 15, 2556. [Google Scholar] [CrossRef]
- Lee, J.; Oh, M. The moderating effect of gender on the association between E-cigarette use and smoking status: A cross-sectional study. Addict. Behav. 2019, 93, 108–114. [Google Scholar] [CrossRef]
- Owens, V.L.; Ha, T.; Soulakova, J.N. Widespread use of flavored e-cigarettes and hookah tobacco in the United States. Prev. Med. Rep. 2019, 14, 100854. [Google Scholar] [CrossRef] [PubMed]
- Abrams, L.R.; Kalousova, L.; Fleischer, N.L. Gender differences in relationships between sociodemographic factors and e-cigarette use with smoking cessation: 2014–2015 current population survey tobacco use supplement. J. Public Health 2020, 42, e42–e50. [Google Scholar] [CrossRef] [PubMed]
- Coleman, B.; Chang, J.T.; Rostron, B.L.; Johnson, S.E.; Das, B.; Del Valle-Pinero, A.Y. An Examination of Device Types and Features Used by Adult Electronic Nicotine Delivery System (ENDS) Users in the PATH Study, 2015–2016. Int. J. Environ. Res. Public Health 2019, 16, 2329. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Bolaños, R.; Arillo-Santillán, E.; Barrientos-Gutiérrez, I.; Zavala-Arciniega, L.; Ntansah, C.A.; Thrasher, J.F. Sex Differences in Becoming a Current Electronic Cigarette User, Current Smoker and Current Dual User of Both Products: A Longitudinal Study among Mexican Adolescents. Int. J. Environ. Res. Public Health 2019, 17, 196. [Google Scholar] [CrossRef]
- Smit, T.; Olofsson, H.; Nizio, P.; Garey, L.; Zvolensky, M.J. Pain severity and e-cigarette health literacy: The moderating role of sex. Subst. Abuse 2019, 13, 1178221819897070. [Google Scholar] [CrossRef] [PubMed]
- Pang, R.D.; Goldenson, N.I.; Kirkpatrick, M.; Barrington-Trimis, J.L.; Cho, J.; Leventhal, A.M. Sex differences in the appeal of flavored e-cigarettes among young adult e-cigarette users. Psychol. Addict. Behav. 2020, 34, 303–307. [Google Scholar] [CrossRef] [PubMed]
- Kasza, K.A.; Edwards, K.C.; Tang, Z.; Stanton, C.A.; Sharma, E.; Halenar, M.J.; Taylor, K.A.; Donaldson, E.; Hull, L.C.; Day, H.; et al. Correlates of tobacco product initiation among youth and adults in the USA: Findings from the PATH Study Waves 1–3 (2013–2016). Tob. Control 2020, 29, s191–s202. [Google Scholar] [CrossRef] [PubMed]
- Edwards, K.C.; Kasza, K.A.; Tang, Z.; Stanton, C.A.; Sharma, E.; Halenar, M.J.; Taylor, K.A.; Donaldson, E.A.; Hull, L.C.; Bansal-Travers, M.; et al. Correlates of tobacco product reuptake and relapse among youth and adults in the USA: Findings from the PATH Study Waves 1–3 (2013–2016). Tob. Control 2020, 29, s216–s226. [Google Scholar] [CrossRef]
- Groom, A.L.; Vu, T.T.; Kesh, A.; Hart, J.L.; Walker, K.L.; Giachello, A.L.; Sears, C.G.; Tompkins, L.K.; Mattingly, D.T.; Landry, R.L.; et al. Correlates of youth vaping flavor preferences. Prev. Med. Rep. 2020, 18, 101094. [Google Scholar] [CrossRef]
- Azagba, S.; Mensah, N.A.; Shan, L.; Latham, K. Bullying Victimization and e-Cigarette Use among Middle and High School Students. J. Sch. Health 2020, 90, 545–553. [Google Scholar] [CrossRef]
- Villarroel, M.A.; Cha, A.E.; Vahratian, A. Electronic Cigarette Use Among U.S. Adults, 2018. NCHS Data Brief. 2020, 1–8. Available online: https://www.cdc.gov/nchs/products/databriefs/db365.htm (accessed on 17 November 2023).
- Yimsaard, P.; McNeill, A.; Yong, H.H.; Cummings, K.M.; Chung-Hall, J.; Hawkins, S.S.; Quah, A.C.K.; Fong, G.T.; O’Connor, R.J.; Hitchman, S.C. Gender Differences in Reasons for Using Electronic Cigarettes and Product Characteristics: Findings From the 2018 ITC Four Country Smoking and Vaping Survey. Nicotine Tob. Res. 2021, 23, 678–686. [Google Scholar] [CrossRef] [PubMed]
- Azagba, S.; King, J.; Shan, L. Associations between e-cigarette pack size and vaping frequency among U.S. adults. Prev. Med. 2021, 143, 106332. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Z.; Zhang, M.; Wu, J.; Xu, X.; Yin, P.; Huang, Z.; Zhang, X.; Zhou, Y.; Zhang, X.; Li, C.; et al. E-cigarette use among adults in China: Findings from repeated cross-sectional surveys in 2015–2016 and 2018–2019. Lancet Public Health 2020, 5, e639–e649. [Google Scholar] [CrossRef] [PubMed]
- Fish, J.N.; Bishop, M.D.; Russell, S.T. Developmental Differences in Sexual Orientation and Gender Identity-Related Substance Use Disparities: Findings From Population-Based Data. J. Adolesc. Health 2021, 68, 1162–1169. [Google Scholar] [CrossRef]
- Pérez, A.; Kuk, A.E.; Bluestein, M.A.; Penedo, E.; N’hpang, R.S.; Chen, B.; Perry, C.L.; Sterling, K.L.; Harrell, M.B. Prospective estimation of the age of initiation of cigarettes among young adults (18–24 years old): Findings from the Population Assessment of Tobacco and Health (PATH) waves 1–4 (2013–2017). PLoS ONE 2021, 16, e0251246. [Google Scholar] [CrossRef]
- Duan, Z.; Wang, Y.; Huang, J. Sex Difference in the Association between Electronic Cigarette Use and Subsequent Cigarette Smoking among U.S. Adolescents: Findings from the PATH Study Waves 1–4. Int. J. Environ. Res. Public Health 2021, 18, 1695. [Google Scholar] [CrossRef]
- Wamamili, B.; Lawler, S.; Wallace-Bell, M.; Gartner, C.; Sellars, D.; Grace, R.C.; Courtney, R.; Coope, P. Cigarette smoking and e-cigarette use among university students in Queensland, Australia and New Zealand: Results of two cross-sectional surveys. BMJ Open 2021, 11, e041705. [Google Scholar] [CrossRef]
- Hopkins, D.B.; Al-Hamdani, M. Young Canadian e-Cigarette Users and the COVID-19 Pandemic: Examining Vaping Behaviors by Pandemic Onset and Gender. Front. Public Health 2020, 8, 620748. [Google Scholar] [CrossRef]
- Lanza, H.I.; Bello, M.S.; Cho, J.; Barrington-Trimis, J.L.; McConnell, R.; Braymiller, J.L.; Krueger, E.A.; Leventhal, A.M. Tobacco and cannabis poly-substance and poly-product use trajectories across adolescence and young adulthood. Prev. Med. 2021, 148, 106545. [Google Scholar] [CrossRef]
- Wang, T.W.; Gentzke, A.S.; Neff, L.J.; Glidden, E.V.; Jamal, A.; Park-Lee, E.; Ren, C.; Cullen, K.A.; King, B.A.; Hacker, K.A. Characteristics of e-Cigarette Use Behaviors Among US Youth, 2020. JAMA Netw. Open 2021, 4, e2111336. [Google Scholar] [CrossRef]
- Evans-Polce, R.J.; Veliz, P.; Kcomt, L.; Boyd, C.J.; McCabe, S.E. Nicotine and Tobacco Product Use and Dependence Symptoms among US Adolescents and Adults: Differences by Age, Sex, and Sexual Identity. Nicotine Tob. Res. 2021, 23, 2065–2074. [Google Scholar] [CrossRef]
- Patanavanich, R.; Aekplakorn, W.; Glantz, S.A.; Kalayasiri, R. Use of E-Cigarettes and Associated Factors among Youth in Thailand. Asian Pac. J. Cancer Prev. 2021, 22, 2199–2207. [Google Scholar] [CrossRef]
- Ihongbe, T.O.; Olayinka, P.O.; Curry, S. Association Between Bully Victimization and Vaping Among Texas High School Students. Am. J. Prev. Med. 2021, 61, 910–918. [Google Scholar] [CrossRef] [PubMed]
- Wamamili, B.; Coope, P.; Grace, R.C. Cigarette smoking and e-cigarette use among university students in New Zealand before and after nicotine-containing e-cigarettes became widely available: Results from repeat cross-sectional surveys. N. Z. Med. J. 2021, 134, 90–102. [Google Scholar] [PubMed]
- Pang, R.D.; Mason, T.B.; Kapsner, A.K.; Leventhal, A.M. Parsing Intra- and Inter-Individual Covariation Between the Sensory Attributes and Appeal of E-Cigarettes: Associations and Gender Differences. Nicotine Tob. Res. 2022, 24, 1012–1019. [Google Scholar] [CrossRef]
- Pérez, A.; Bluestein, M.A.; Kuk, A.E.; Chen, B.; Sterling, K.L.; Harrell, M.B. Age of Onset of Susceptibility to Different Tobacco Products Among Non-Susceptible US Young Adults: Findings from the Population Assessment of Tobacco and Health Study Waves 2–4 (2014–2017). Tob. Use Insights 2021, 14, 1179173X211065643. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, S.; Wang, T.; Schwartz, R.; Bondy, S.J. Predictors of pod-type e-cigarette device use among Canadian youth and young adults. Health Promot. Chronic Dis. Prev. Can. 2022, 42, 12–20. [Google Scholar] [CrossRef]
- Stanton, C.A.; Tang, Z.; Sharma, E.; Seaman, E.; Gardner, L.D.; Silveira, M.L.; Hatsukami, D.; Day, H.R.; Cummings, K.M.; Goniewicz, M.L.; et al. Predictors of E-cigarette and Cigarette Use Trajectory Classes from Early Adolescence to Emerging Adulthood Across Four Years (2013–2017) of the PATH Study. Nicotine Tob. Res. 2023, 25, 421–429. [Google Scholar] [CrossRef]
- Hennigan, K.M.; Olson, K.R.; Baker, J.H.; Munn-Chernoff, M.A. Associations between eating disorder symptoms and smoking and vaping use and motives in college students. Eat. Behav. 2022, 46, 101652. [Google Scholar] [CrossRef]
- Davis, D.R.; Bold, K.W.; Camenga, D.; Kong, G.; Jackson, A.; Lee, J.; Rajesh-Kumar, L.; Krishnan-Sarin, S.; Morean, M.E. Use and Product Characteristics of “Tobacco Free Nicotine” E-Cigarettes Among Young Adults. Nicotine Tob. Res. 2023, 25, 379–385. [Google Scholar] [CrossRef] [PubMed]
- Neale, J.; Parkin, S.; Hermann, L.; Metrebian, N.; Roberts, E.; Robson, D.; Strang, J. Substance use and homelessness: A longitudinal interview study conducted during COVID-19 with implications for policy and practice. Int. J. Drug Policy 2022, 108, 103818. [Google Scholar] [CrossRef]
- Green, M.J.; Maddock, J.; Di Gessa, G.; Wielgoszewska, B.; Parsons, S.; Griffith, G.J.; Croft, J.; Stevenson, A.J.; Huggins, C.F.; Booth, C.; et al. The UK Coronavirus Job Retention Scheme and smoking, alcohol consumption and vaping during the COVID-19 pandemic: Evidence from eight longitudinal population surveys. BMC Med. 2022, 20, 345. [Google Scholar] [CrossRef] [PubMed]
- Mattingly, D.T.; Agbonlahor, O.; Rai, J.; Hart, J.L.; McLeish, A.C.; Walker, K.L. Harm perceptions of secondhand e-cigarette aerosol among youth in the United States. Addict. Behav. 2023, 137, 107535. [Google Scholar] [CrossRef] [PubMed]
- Hochgraf, A.K.; Fosco, G.M.; Lanza, S.T. Age-Varying Associations between Attempts to Lose Weight and Nicotine Vaping Across Adolescence: Results From a Nationally Representative Sample. J. Adolesc. Health 2023, 72, 352–358. [Google Scholar] [CrossRef]
- Williams, P.J.; Cheeseman, H.; Arnott, D.; Bunce, L.; Hopkinson, N.S.; Laverty, A.A. Use of tobacco and e-cigarettes among youth in Great Britain in 2022: Analysis of a cross-sectional survey. Tob. Induc. Dis 2023, 21, 05. [Google Scholar] [CrossRef] [PubMed]
- Vilcassim, M.J.R.; Jacob, D.; Stowe, S.; Fifolt, M.; Zierold, K.M. Sex Differences in Electronic Cigarette Device Use Among College Students. J. Community Health 2023, 48, 585–592. [Google Scholar] [CrossRef]
- Alnasser, A.H.A.; Al-Tawfiq, J.A.; Kheimi, R.M.A.; Alibrahim, R.M.S.; Albanawi, N.A.H.; Almeshal, A.K.A.; Alsomali, H.M.H.; Al Kalif, M.S.H.; Al Sayed Ahmed, H.H.; Khamees, S.H.A.; et al. Gender Differences in Smoking Attitude among Saudi Medical Students. Asian Pac. J. Cancer Prev. 2022, 23, 2089–2093. [Google Scholar] [CrossRef]
- Bedi, M.K.; Bedi, D.K.; Ledgerwood, D.M. Gender Differences in Reasons for Using Electronic Cigarettes: A Systematic Review. Nicotine Tob. Res. 2022, 24, 1355–1362. [Google Scholar] [CrossRef]
- Cavallo, D.A.; Kong, G.; Ells, D.M.; Camenga, D.R.; Morean, M.E.; Krishnan-Sarin, S. Youth generated prevention messages about electronic cigarettes. Health Educ. Res. 2019, 34, 247–256. [Google Scholar] [CrossRef]
- Chesaniuk, M.; Sokolovsky, A.W.; Ahluwalia, J.S.; Jackson, K.M.; Mermelstein, R. Dependence motives of young adult users of electronic nicotine delivery systems. Addict. Behav. 2019, 95, 1–5. [Google Scholar] [CrossRef]
- Perrine, C.G.; Pickens, C.M.; Boehmer, T.K.; King, B.A.; Jones, C.M.; DeSisto, C.L.; Duca, L.M.; Lekiachvili, A.; Kenemer, B.; Shamout, M.; et al. Characteristics of a Multistate Outbreak of Lung Injury Associated with E-cigarette Use, or Vaping—United States, 2019. MMWR Morb. Mortal Wkly. Rep. 2019, 68, 860–864. [Google Scholar] [CrossRef]
- Eltorai, A.E.; Choi, A.R.; Eltorai, A.S. Impact of Electronic Cigarettes on Various Organ Systems. Respir. Care 2019, 64, 328–336. [Google Scholar] [CrossRef]
- Wang, J.B.; Olgin, J.E.; Nah, G.; Vittinghoff, E.; Cataldo, J.K.; Pletcher, M.J.; Marcus, G.M. Cigarette and e-cigarette dual use and risk of cardiopulmonary symptoms in the Health eHeart Study. PLoS ONE 2018, 13, e0198681. [Google Scholar] [CrossRef] [PubMed]
- Antoniewicz, L.; Bosson, J.A.; Kuhl, J.; Abdel-Halim, S.M.; Kiessling, A.; Mobarrez, F.; Lundbäck, M. Electronic cigarettes increase endothelial progenitor cells in the blood of healthy volunteers. Atherosclerosis 2016, 255, 179–185. [Google Scholar] [CrossRef] [PubMed]
- Carnevale, R.; Sciarretta, S.; Violi, F.; Nocella, C.; Loffredo, L.; Perri, L.; Peruzzi, M.; Marullo, A.G.; De Falco, E.; Chimenti, I.; et al. Acute Impact of Tobacco vs Electronic Cigarette Smoking on Oxidative Stress and Vascular Function. Chest 2016, 150, 606–612. [Google Scholar] [CrossRef] [PubMed]
- Kelesidis, T.; Tran, E.; Arastoo, S.; Lakhani, K.; Heymans, R.; Gornbein, J.; Middlekauff, H.R. Elevated Cellular Oxidative Stress in Circulating Immune Cells in Otherwise Healthy Young People Who Use Electronic Cigarettes in a Cross-Sectional Single-Center Study: Implications for Future Cardiovascular Risk. J. Am. Heart Assoc. 2020, 9, e016983. [Google Scholar] [CrossRef] [PubMed]
- Shi, H.; Leventhal, A.M.; Wen, Q.; Ossip, D.J.; Li, D. Sex Differences in the Association of E-cigarette and Cigarette Use and Dual Use With Self-Reported Hypertension Incidence in US Adults. Nicotine Tob. Res. 2023, 25, 478–485. [Google Scholar] [CrossRef]
- Joshi, D.; Duong, M.; Kirkland, S.; Raina, P. Impact of electronic cigarette ever use on lung function in adults aged 45–85: A cross-sectional analysis from the Canadian Longitudinal Study on Aging. BMJ Open 2021, 11, e051519. [Google Scholar] [CrossRef]
- Antwi, G.O.; Rhodes, D.L. Association between E-cigarette use and chronic obstructive pulmonary disease in non-asthmatic adults in the USA. J. Public Health 2022, 44, 158–164. [Google Scholar] [CrossRef]
- Cook, S.F.; Hirschtick, J.L.; Fleischer, N.L.; Arenberg, D.A.; Barnes, G.D.; Levy, D.T.; Sanchez-Romero, L.M.; Jeon, J.; Meza, R. Cigarettes, ENDS Use, and Chronic Obstructive Pulmonary Disease Incidence: A Prospective Longitudinal Study. Am. J. Prev. Med. 2023, 65, 173–181. [Google Scholar] [CrossRef] [PubMed]
- Entwistle, M.R.; Valle, K.; Schweizer, D.; Cisneros, R. Electronic cigarette (e-cigarette) use and frequency of asthma symptoms in adult asthmatics in California. J. Asthma Off. J. Assoc. Care Asthma 2021, 58, 1460–1466. [Google Scholar] [CrossRef] [PubMed]
- Solingapuram Sai, K.K.; Zuo, Y.; Rose, J.E.; Garg, P.K.; Garg, S.; Nazih, R.; Mintz, A.; Mukhin, A.G. Rapid Brain Nicotine Uptake from Electronic Cigarettes. J. Nucl. Med. 2020, 61, 928–930. [Google Scholar] [CrossRef] [PubMed]
- Leslie, F.M. Unique, long-term effects of nicotine on adolescent brain. Pharmacol. Biochem. Behav. 2020, 197, 173010. [Google Scholar] [CrossRef] [PubMed]
- Ayesha, A. A Review of Electronic Cigarettes and Liquid Nicotine Poisoning Exposure Cases in the United States. J. Pharm. Pharm. Sci. 2022, 25, 354–368. [Google Scholar] [CrossRef]
- Shittu, A.A.T.; Kumar, B.P.; Okafor, U.; Berkelhamer, S.K.; Goniewicz, M.L.; Wen, X. Changes in e-cigarette and cigarette use during pregnancy and their association with small-for-gestational-age birth. Am. J. Obstet. Gynecol. 2022, 226, e730–e731. [Google Scholar] [CrossRef]
- Sikic, A.; Frie, J.A.; Khokhar, J.Y.; Murray, J.E. Sex Differences in the Behavioural Outcomes of Prenatal Nicotine and Tobacco Exposure. Front. Neurosci. 2022, 16, 921429. [Google Scholar] [CrossRef]
- Ruffolo, J.; Frie, J.A.; Thorpe, H.H.A.; Talhat, M.A.; Khokhar, J.Y. Alcohol and Vaporized Nicotine Co-exposure During Adolescence Contribute Differentially to Sex-Specific Behavioral Effects in Adulthood. Nicotine Tob. Res. 2022, 24, 1177–1185. [Google Scholar] [CrossRef]
- Nguyen, J.D.; Creehan, K.M.; Kerr, T.M.; Taffe, M.A. Lasting effects of repeated ∆9-tetrahydrocannabinol vapour inhalation during adolescence in male and female rats. Br. J. Pharmacol. 2020, 177, 188–203. [Google Scholar] [CrossRef]
- Ruiz, C.M.; Torrens, A.; Lallai, V.; Castillo, E.; Manca, L.; Martinez, M.X.; Justeson, D.N.; Fowler, C.D.; Piomelli, D.; Mahler, S.V. Pharmacokinetic and pharmacodynamic properties of aerosolized (“vaped”) THC in adolescent male and female rats. Psychopharmacology 2021, 238, 3595–3605. [Google Scholar] [CrossRef]
- Whitehead, A.K.; Meyers, M.C.; Taylor, C.M.; Luo, M.; Dowd, S.E.; Yue, X.; Byerley, L.O. Sex-Dependent Effects of Inhaled Nicotine on the Gut Microbiome. Nicotine Tob. Res. 2022, 24, 1363–1370. [Google Scholar] [CrossRef] [PubMed]
- Xue, S.; Behnood-Rod, A.; Wilson, R.; Wilks, I.; Tan, S.; Bruijnzeel, A.W. Rewarding Effects of Nicotine in Adolescent and Adult Male and Female Rats as Measured Using Intracranial Self-stimulation. Nicotine Tob. Res. 2020, 22, 172–179. [Google Scholar] [CrossRef] [PubMed]
- Honeycutt, S.C.; Garrett, P.I.; Barraza, A.G.; Maloy, A.N.; Hillhouse, T.M. Repeated nicotine vapor inhalation induces behavioral sensitization in male and female C57BL/6 mice. Behav. Pharmacol. 2020, 31, 583–590. [Google Scholar] [CrossRef] [PubMed]
- Kaisar, M.A.; Sivandzade, F.; Bhalerao, A.; Cucullo, L. Conventional and electronic cigarettes dysregulate the expression of iron transporters and detoxifying enzymes at the brain vascular endothelium: In vivo evidence of a gender-specific cellular response to chronic cigarette smoke exposure. Neurosci. Lett. 2018, 682, 1–9. [Google Scholar] [CrossRef]
- Wang, Q.; Khan, N.A.; Muthumalage, T.; Lawyer, G.R.; McDonough, S.R.; Chuang, T.D.; Gong, M.; Sundar, I.K.; Rehan, V.K.; Rahman, I. Dysregulated repair and inflammatory responses by e-cigarette-derived inhaled nicotine and humectant propylene glycol in a sex-dependent manner in mouse lung. FASEB Bioadv. 2019, 1, 609–623. [Google Scholar] [CrossRef]
- Lallai, V.; Manca, L.; Fowler, C.D. E-cigarette vape and lung ACE2 expression: Implications for coronavirus vulnerability. Environ. Toxicol. Pharmacol. 2021, 86, 103656. [Google Scholar] [CrossRef] [PubMed]
- Naidu, V.; Zeki, A.A.; Sharma, P. Sex differences in the induction of angiotensin converting enzyme 2 (ACE-2) in mouse lungs after e-cigarette vapor exposure and its relevance to COVID-19. J. Investig. Med. 2021, 69, 954–961. [Google Scholar] [CrossRef]
- Carll, A.P.; Arab, C.; Salatini, R.; Miles, M.D.; Nystoriak, M.A.; Fulghum, K.L.; Riggs, D.W.; Shirk, G.A.; Theis, W.S.; Talebi, N.; et al. E-cigarettes and their lone constituents induce cardiac arrhythmia and conduction defects in mice. Nat. Commun. 2022, 13, 6088. [Google Scholar] [CrossRef]
- Wang, Q.; Sundar, I.K.; Blum, J.L.; Ratner, J.R.; Lucas, J.H.; Chuang, T.D.; Wang, Y.; Liu, J.; Rehan, V.K.; Zelikoff, J.T.; et al. Prenatal Exposure to Electronic-Cigarette Aerosols Leads to Sex-Dependent Pulmonary Extracellular-Matrix Remodeling and Myogenesis in Offspring Mice. Am. J. Respir. Cell Mol. Biol. 2020, 63, 794–805. [Google Scholar] [CrossRef]
- Sussan, T.E.; Gajghate, S.; Thimmulappa, R.K.; Ma, J.; Kim, J.H.; Sudini, K.; Consolini, N.; Cormier, S.A.; Lomnicki, S.; Hasan, F.; et al. Exposure to electronic cigarettes impairs pulmonary anti-bacterial and anti-viral defenses in a mouse model. PLoS ONE 2015, 10, e0116861. [Google Scholar] [CrossRef]
- Hwang, J.H.; Lyes, M.; Sladewski, K.; Enany, S.; McEachern, E.; Mathew, D.P.; Das, S.; Moshensky, A.; Bapat, S.; Pride, D.T.; et al. Electronic cigarette inhalation alters innate immunity and airway cytokines while increasing the virulence of colonizing bacteria. J. Mol. Med. 2016, 94, 667–679. [Google Scholar] [CrossRef] [PubMed]
- Lefever, T.W.; Thomas, B.F.; Kovach, A.L.; Snyder, R.W.; Wiley, J.L. Route of administration effects on nicotine discrimination in female and male mice. Drug Alcohol. Depend. 2019, 204, 107504. [Google Scholar] [CrossRef] [PubMed]
- Chellian, R.; Behnood-Rod, A.; Wilson, R.; Kamble, S.H.; Sharma, A.; McCurdy, C.R.; Bruijnzeel, A.W. Adolescent nicotine and tobacco smoke exposure enhances nicotine self-administration in female rats. Neuropharmacology 2020, 176, 108243. [Google Scholar] [CrossRef] [PubMed]
- Lallai, V.; Chen, Y.C.; Roybal, M.M.; Kotha, E.R.; Fowler, J.P.; Staben, A.; Cortez, A.; Fowler, C.D. Nicotine e-cigarette vapor inhalation and self-administration in a rodent model: Sex- and nicotine delivery-specific effects on metabolism and behavior. Addict. Biol. 2021, 26, e13024. [Google Scholar] [CrossRef] [PubMed]
- Fried, N.D.; Whitehead, A.; Lazartigues, E.; Yue, X.; Gardner, J.D. Ovarian hormones do not mediate protection against pulmonary hypertension and right ventricular remodeling in female mice exposed to chronic, inhaled nicotine. Am. J. Physiol. Heart Circ. Physiol. 2022, 323, H941–H948. [Google Scholar] [CrossRef]
- Chellian, R.; Behnood-Rod, A.; Wilson, R.; Lin, K.; Wing-Yan King, G.; Bruijnzeel, A.W. The D1/D2-like receptor antagonist flupentixol and the D2-like receptor antagonist L-741626 decrease operant responding for nicotine and food and locomotor activity in male and female rats. J. Psychopharmacol. 2023, 37, 216–228. [Google Scholar] [CrossRef]
- Alasmari, F.; Alasmari, A.F.; Elzayat, E.; Alotaibi, M.M.; Alotaibi, F.M.; Attwa, M.W.; Alanazi, F.K.; Abdelgadir, E.H.; Ahmad, S.R.; Alqahtani, F.; et al. Nicotine and cotinine quantification after a 4-week inhalation of electronic cigarette vapors in male and female mice using UPLC-MS/MS. Saudi Med. J. 2022, 43, 678–686. [Google Scholar] [CrossRef]
- Bricknell, R.A.T.; Ducaud, C.; Figueroa, A.; Schwarzman, L.S.; Rodriguez, P.; Castro, G.; Zevallos, J.C.; Barengo, N.C. An association between electronic nicotine delivery systems use and a history of stroke using the 2016 behavioral risk factor surveillance system. Medicine 2021, 100, e27180. [Google Scholar] [CrossRef]
- Milicic, S.; Piérard, E.; DeCicca, P.; Leatherdale, S.T. Examining the Association Between Physical Activity, Sedentary Behavior and Sport Participation With E-Cigarette Use and Smoking Status in a Large Sample of Canadian Youth. Nicotine Tob. Res. 2019, 21, 285–292. [Google Scholar] [CrossRef]
- Morean, M.E.; Krishnan-Sarin, S.; Sussman, S.; Foulds, J.; Fishbein, H.; Grana, R.; O’Malley, S.S. Psychometric Evaluation of the E-cigarette Dependence Scale. Nicotine Tob. Res. 2019, 21, 1556–1564. [Google Scholar] [CrossRef]
- Li, J.; Haardörfer, R.; Vu, M.; Windle, M.; Berg, C.J. Sex and sexual orientation in relation to tobacco use among young adult college students in the US: A cross-sectional study. BMC Public Health 2018, 18, 1244. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.; Lee, K.S. Association of Depression and Suicidality with Electronic and Conventional Cigarette Use in South Korean Adolescents. Subst. Use Misuse 2019, 54, 934–943. [Google Scholar] [CrossRef] [PubMed]
- Aleyan, S.; East, K.; McNeill, A.; Cummings, K.M.; Fong, G.T.; Yong, H.H.; Thrasher, J.F.; Borland, R.; Hitchman, S.C. Differences in norms towards the use of nicotine vaping products among adult smokers, former smokers and nicotine vaping product users: Cross-sectional findings from the 2016 ITC Four Country Smoking and Vaping Survey. Addiction 2019, 114 (Suppl. 1), 97–106. [Google Scholar] [CrossRef] [PubMed]
- Shilco, P.; Golshan, T.; Lande, S.; Nickfardjam, K.; Roitblat, Y.; Morgan, A.; Nehuliaieva, L.; Shterenshis, M. Knowledge and attitudes of adolescents to e-cigarettes: An international prospective study. Int. J. Adolesc. Med. Health 2020, 34, 20190210. [Google Scholar] [CrossRef] [PubMed]
- Grigsby, T.J.; Rogers, C.J.; Albers, L.D.; Benjamin, S.M.; Lust, K.; Eisenberg, M.E.; Forster, M. Adverse Childhood Experiences and Health Indicators in a Young Adult, College Student Sample: Differences by Gender. Int. J. Behav. Med. 2020, 27, 660–667. [Google Scholar] [CrossRef]
- Mayorga, N.A.; Smit, T.; Shepherd, J.M.; Orr, M.F.; Garey, L.; Zvolensky, M.J. Worry and e-cigarette cognition: The moderating role of sex. Addict. Behav. 2021, 112, 106621. [Google Scholar] [CrossRef]
- Huh, J.; Meza, L.; Galstyan, E.; Galimov, A.; Yu, S.; Unger, J.B.; Baezconde-Garbanati, L.; Sussman, S. Signs and customer behaviors at vape shops: Multivariate multilevel model analysis. Addict. Behav. Rep. 2020, 12, 100299. [Google Scholar] [CrossRef]
- Rapp, J.L.; Alpert, N.; Wilson, K.M.; Flores, R.M.; Taioli, E. Changes in E-Cigarette Perceptions Over Time: A National Youth Tobacco Survey Analysis. Am. J. Prev. Med. 2021, 61, 174–181. [Google Scholar] [CrossRef]
- Thorisdottir, I.E.; Asgeirsdottir, B.B.; Kristjansson, A.L.; Valdimarsdottir, H.B.; Jonsdottir Tolgyes, E.M.; Sigfusson, J.; Allegrante, J.P.; Sigfusdottir, I.D.; Halldorsdottir, T. Depressive symptoms, mental wellbeing, and substance use among adolescents before and during the COVID-19 pandemic in Iceland: A longitudinal, population-based study. Lancet Psychiatry 2021, 8, 663–672. [Google Scholar] [CrossRef]
- Jones, D.M.; Masyn, K.E.; Spears, C.A. Discrimination, psychological functioning, and substance use among U.S. young adults aged 18-28, 2017. Exp. Clin. Psychopharmacol. 2022, 30, 884–896. [Google Scholar] [CrossRef]
- Romano, I.; Patte, K.A.; de Groh, M.; Jiang, Y.; Wade, T.J.; Bélanger, R.E.; Leatherdale, S.T. Substance-related coping behaviours among youth during the early months of the COVID-19 pandemic. Addict. Behav. Rep. 2021, 14, 100392. [Google Scholar] [CrossRef] [PubMed]
- Morean, M.E.; Davis, D.R.; Bold, K.W.; Kong, G.; Jackson, A.; Lee, J.; Rajesh Kumar, L.; Krishnan-Sarin, S. Psychometric Evaluation of the Short-Form Vaping Consequences Questionnaire for Use With High School Adolescents Who Use and Do Not Use E-cigarettes. Nicotine Tob. Res. 2022, 24, 699–709. [Google Scholar] [CrossRef] [PubMed]
- Baiden, P.; Szlyk, H.S.; Cavazos-Rehg, P.; Onyeaka, H.K.; Peoples, J.E.; Kasson, E. Use of electronic vaping products and mental health among adolescent high school students in the United States: The moderating effect of sex. J. Psychiatr. Res. 2022, 147, 24–33. [Google Scholar] [CrossRef]
- Chankaew, T.; Baiya, P.; Chinwong, D.; Yoodee, V.; Chinwong, S. Electronic Cigarettes in Thailand: Behaviour, Rationale, Satisfaction, and Sex Differences. Int. J. Environ. Res. Public Health 2022, 19, 8229. [Google Scholar] [CrossRef]
- Hung, M.; Spencer, A.; Hon, E.S.; Licari, F.W.; Cheever, V.J.; Moffat, R.; Goh, C.; Raymond, B.; Lipsky, M.S. E-cigarette addiction and harm perception: Does initiation flavor choice matter? BMC Public Health 2022, 22, 1780. [Google Scholar] [CrossRef] [PubMed]
- Azagba, S.; Ebling, T.; Shan, L. Sexual Minority Youth E-Cigarette Use. Pediatrics 2023, 151, e2022058414. [Google Scholar] [CrossRef] [PubMed]
- Keogh-Clark, F.; Whaley, R.C.; Leventhal, A.M.; Krueger, E.A. Sex differences in the association between parental monitoring and substance use initiation among adolescents. Addict. Behav. 2021, 122, 107024. [Google Scholar] [CrossRef]
- Pederson, L.L.; Koval, J.J.; Vingilis, E. E-cigarette use by Ontario public elementary school and secondary school students: Has the use among sociodemographic groups changed from 2017 to 2019? Prev. Med. Rep. 2023, 34, 102257. [Google Scholar] [CrossRef]
- Aghar, H.; El-Khoury, N.; Reda, M.; Hamadeh, W.; Krayem, H.; Mansour, M.; Raouf, H.; Jaffa, M.A. Knowledge and attitudes towards E-cigarette use in Lebanon and their associated factors. BMC Public Health 2020, 20, 278. [Google Scholar] [CrossRef]
- Bertoni, N.; Szklo, A.; Boni, R.; Coutinho, C.; Vasconcellos, M.; Nascimento Silva, P.; de Almeida, L.M.; Bastos, F.I. Electronic cigarettes and narghile users in Brazil: Do they differ from cigarettes smokers? Addict. Behav. 2019, 98, 106007. [Google Scholar] [CrossRef]
- Do, M.T.; McFaull, S.R.; Guttman, L.; Ghandour, L.; Hardy, J. Strengthening surveillance of consumer products in Canada: The vaping example. Health Promot. Chronic Dis. Prev. Can. 2020, 40, 309–313. [Google Scholar] [CrossRef] [PubMed]
- Trapl, E.; Pike Moore, S.; Osborn, C.; Gupta, N.; Love, T.E.; Kinzy, T.G.; Kinsella, A.; Frank, S. Evaluation of Restrictions on Tobacco Sales to Youth Younger Than 21 Years in Cleveland, Ohio, Area. JAMA Netw. Open 2022, 5, e2222987. [Google Scholar] [CrossRef]
- Ogunwale, M.A.; Li, M.; Ramakrishnam Raju, M.V.; Chen, Y.; Nantz, M.H.; Conklin, D.J.; Fu, X.A. Aldehyde Detection in Electronic Cigarette Aerosols. ACS Omega 2017, 2, 1207–1214. [Google Scholar] [CrossRef] [PubMed]
- Samburova, V.; Bhattarai, C.; Strickland, M.; Darrow, L.; Angermann, J.; Son, Y.; Khlystov, A. Aldehydes in Exhaled Breath during E-Cigarette Vaping: Pilot Study Results. Toxics 2018, 6, 46. [Google Scholar] [CrossRef]
- Belok, S.H.; Parikh, R.; Bernardo, J.; Kathuria, H. E-cigarette, or vaping, product use-associated lung injury: A review. Pneumonia 2020, 12, 12. [Google Scholar] [CrossRef]
- Mughal, M.S.; Dalmacion, D.L.V.; Mirza, H.M.; Kaur, I.P.; Dela Cruz, M.A.; Kramer, V.E. E-cigarette or vaping product use associated lung injury, (EVALI)—A diagnosis of exclusion. Respir. Med. Case Rep. 2020, 31, 101174. [Google Scholar] [CrossRef] [PubMed]
- Soto, B.; Costanzo, L.; Puskoor, A.; Akkari, N.; Geraghty, P. The implications of Vitamin E acetate in E-cigarette, or vaping, product use-associated lung injury. Ann. Thorac. Med. 2023, 18, 1–9. [Google Scholar] [CrossRef]
- Elliott, B.M.; Faraday, M.M.; Phillips, J.M.; Grunberg, N.E. Effects of nicotine on elevated plus maze and locomotor activity in male and female adolescent and adult rats. Pharmacol. Biochem. Behav. 2004, 77, 21–28. [Google Scholar] [CrossRef]
- Cao, J.; Belluzzi, J.D.; Loughlin, S.E.; Dao, J.M.; Chen, Y.; Leslie, F.M. Locomotor and stress responses to nicotine differ in adolescent and adult rats. Pharmacol. Biochem. Behav. 2010, 96, 82–90. [Google Scholar] [CrossRef]
- Ray, J.L.; Fletcher, P.; Burmeister, R.; Holian, A. The role of sex in particle-induced inflammation and injury. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2020, 12, e1589. [Google Scholar] [CrossRef]
- Calder, R.; Gant, E.; Bauld, L.; McNeill, A.; Robson, D.; Brose, L.S. Vaping in Pregnancy: A Systematic Review. Nicotine Tob. Res. 2021, 23, 1451–1458. [Google Scholar] [CrossRef] [PubMed]
| Topic | # of Articles | Refs. |
|---|---|---|
| Sex differences in predictors, risk factors, and epidemiology. | 56 | [18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73] |
| Sex differences in organ systems effects (clinical and preclinical). | 36 | [74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109] |
| Sex and gender differences in behavioral effects. | 23 | [110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132] |
| Study | Exposure/Model | Results |
|---|---|---|
| Pulmonary | ||
| Wang et al., 2019 [96] | Acute (2 h/day) 3-day exposure to e-cigarette aerosols (Joytech eVIC VTC mini-ENDS) containing PG +/-nicotine (vs. air-exposed controls) in C57BL/6J mice (14–16 weeks old). | Males only: increased BALF IL-3, IL-4, IL-9, IL-12p70, IFNγ, GM-CSF, Eotaxin, and MIP-1β with PG+nicotine; increased CTNN1B with PG only. Females only: increased BALF neutrophil CD8a+ T-lymphocytes and IL-1β, and lung tissue ADRP with PG+nicotine; increased lung tissue ADRP and PPARγ with PG+/−nicotine. Both sexes: higher BALF MPO activity and lung tissue ADRP with PG only; lower MPO activity with PG+nicotine; higher lung tissue nAChRα3 and nAChRα7 in both PG+/−nicotine (effect more robust in females). |
| Lallai et al., 2021 [97] | PV/VG + nicotine vapor exposure (1 h/day, 5 days, 1 puff every 5 min) in a sealed chamber (adult C57BL6/J mice). | Males only: increased ACE2 mRNA expression and cell density in the lungs exposed to nicotine. Both sexes: increased cotinine levels, downregulated nAChR α5 subunit. |
| Naidu et al., 2021 [98] | A 30 min e-cigarette vapor exposure (+/−nicotine), 2 times/day for 21 days (adult BALB/c mice). | Females only: significant increase in AHR with nicotine exposure. Both sexes: vapor increased BALF MCP-1, IL-1β, and KC levels. Nicotine induced lung ACE-2 expression (higher in males). |
| Wang et al., 2020 [100] | Pregnant CD-1 mice exposed to e-cigarette aerosols (PV/VG +/- nicotine), 3 h/day, 5 days/week, 3 weeks. Adult (6-weeks old) offspring analyzed. | Females only: upregulated LEF-1, HDAC-1, and fibronectin in pups exposed to PG/VG. Males only: increased lung PPARγ, CNN1, ACTA2, and α-SMA; decreased e-cadherin in pups exposed to PG/VG+nicotine. Both sexes: increased PAI-1 and decreased MMP9 levels in pups exposed to PG/VG+nicotine. |
| Cardiovascular | ||
| Carll et al., 2022 [99] | Performed 9 min puff sessions three times; 2 sessions with PG/VG and menthol (bluPLUS+ cartridges) in telemetered C56BL/6/mice (12–30 weeks old). | Males only: significant HR and HRV responses and solvent-induced bradyarrhythmias and bradycardia than females. More susceptible to bradypnea, cardiac depression, and mortality upon acute exposures to high acrolein, and had higher VPBs with exposure to menthol-containing aerosols. Both sexes: e-cigarette exposure increased the frequency of ventricular tachyarrhythmias. |
| Central nervous system | ||
| Nguyen et al., 2020 [90] | PG or THC vapor exposure 2 times/day for 30 min using an e-cigarette system in Wistar adolescent and adult rats. | Males only: consumed more food after repeated adolescent THC and had significantly lower body weight during the second treatment week. Females only: developed rapid tolerance (adolescents); self-administered more fentanyl with repeated THC exposure. Both sexes: hypothermic after THC vapor inhalation; had persisting tolerance as adults. |
| Honeycutt et al., 2020 [94] | Vaporized nicotine exposure once daily for 5 days in C56BL/6 adult mice. | Females only: more sensitive to hypothermic effects. No sex differences in locomotor activity. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alam, F.; Silveyra, P. Sex Differences in E-Cigarette Use and Related Health Effects. Int. J. Environ. Res. Public Health 2023, 20, 7079. https://doi.org/10.3390/ijerph20227079
Alam F, Silveyra P. Sex Differences in E-Cigarette Use and Related Health Effects. International Journal of Environmental Research and Public Health. 2023; 20(22):7079. https://doi.org/10.3390/ijerph20227079
Chicago/Turabian StyleAlam, Fatima, and Patricia Silveyra. 2023. "Sex Differences in E-Cigarette Use and Related Health Effects" International Journal of Environmental Research and Public Health 20, no. 22: 7079. https://doi.org/10.3390/ijerph20227079
APA StyleAlam, F., & Silveyra, P. (2023). Sex Differences in E-Cigarette Use and Related Health Effects. International Journal of Environmental Research and Public Health, 20(22), 7079. https://doi.org/10.3390/ijerph20227079






