Are Sexual Assaults Related to Functional Somatic Disorders? A Cross-Sectional Study
Abstract
:1. Introduction
- Being exposed to SA is associated with experiencing FSD.
- ii.
- SA victims have a higher prevalence and more severe single somatic symptoms than individuals not exposed to SA.
- iii.
- There is a correlation between SA severity and the development of FSD.
- iv.
- Associations between SA and FSDs are specific and distinct from associations between SA and mental health.
2. Materials and Methods
2.1. Study Design and Population
Ethics
2.2. Primary Variables: Exposure
Sexual Assault
2.3. Primary Variables: Outcomes
2.3.1. Functional Somatic Disorder Conceptualized as Bodily Distress Syndrome (BDS)
2.3.2. Single-Organ FSD
2.3.3. Multi-Organ FSD
2.3.4. FSS
2.3.5. Somatic Symptoms
2.3.6. Emotional Distress
2.3.7. Health Anxiety
2.4. Secondary Variables: Descriptive Data and Confounders
2.4.1. Age at Time of Inclusion
2.4.2. Age at Time of SA
2.4.3. Sex
2.4.4. Vocational Training
2.4.5. Self-Reported Social Status
2.4.6. Adverse Childhood Environment
2.4.7. Abuse
2.5. Statistical Analysis
2.5.1. General Statistics
2.5.2. Regression Model
3. Results
3.1. Descriptive Analysis
Analysis of Missing SA Victims
3.2. Crude and Adjusted Analysis of FSD
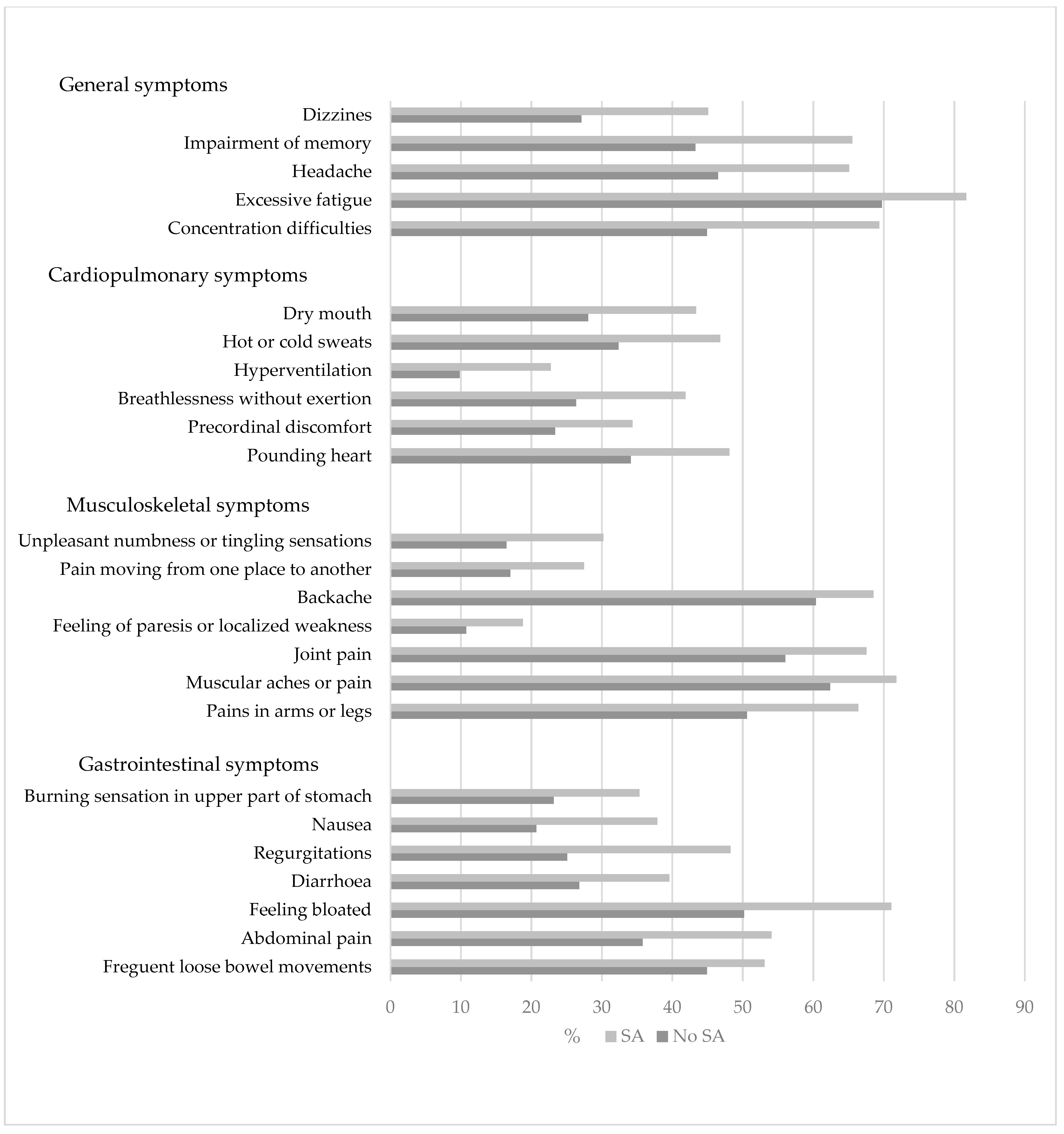
3.3. Descriptive Analysis of Somatic Symptoms
3.4. Analysis of Subdivisions: Rape and Groping
3.5. Analysis of the Mental Health Components
3.6. Analysis of Physical and Emotional Abuse
4. Discussion
4.1. Strengths and Limitations
4.2. Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Forskningskontor, J. Udsathed for Vold og Andre Former for Kriminalitet: Offerundersøgelserne 2005–2018; Rigspolitiet, Københavns Universitet, Det Kriminalpræventive Råd: København, Denmark, 2018. [Google Scholar]
- Deen, L.; Johansen, K.; Møller, S.; Laursen, B. Vold og Seksuelle Krænkelser: En Afdækning af Omfang og Udvikling af Fysisk Vold og Seksuelle Overgreb og Omfang af Seksuelle Krænkelser Samt en Analyse af Erfaringer Med Digitale Seksuelle Krænkelser; Statens Institut for Folkesundhed, University of Southern Denmark: Odense, Denmark, 2018. [Google Scholar]
- Statistik, D. Kriminalitet 2018; Danmarks Statistik: København, Denmark, 2019. [Google Scholar]
- WHO. Violence Against Women Prevalence Estimates, 2018: Global, Regional and National Prevalence Estimates for Intimate Partner Violence against Women and Global and Regional Prevalence Estimates for Non-Partner Sexual Violence against Women; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Paras, M.L.; Murad, M.H.; Chen, L.P.; Goranson, E.N.; Sattler, A.L.; Colbenson, K.M.; Elamin, M.B.; Seime, R.J.; Prokop, L.J.; Zirakzadeh, A. Sexual abuse and lifetime diagnosis of somatic disorders: A systematic review and meta-analysis. JAMA 2009, 302, 550–561. [Google Scholar] [CrossRef] [PubMed]
- Ulirsch, J.C.; Ballina, L.E.; Soward, A.C.; Rossi, C.; Hauda, W.; Holbrook, D.; Wheeler, R.; Foley, K.A.; Batts, J.; Collette, R.; et al. Pain and somatic symptoms are sequelae of sexual assault: Results of a prospective longitudinal study. Eur. J. Pain 2014, 18, 559–566. [Google Scholar] [CrossRef] [PubMed]
- McLean, S.A.; Soward, A.C.; Ballina, L.E.; Rossi, C.; Rotolo, S.; Wheeler, R.; Foley, K.A.; Batts, J.; Casto, T.; Collette, R.; et al. Acute severe pain is a common consequence of sexual assault. J. Pain 2012, 13, 736–741. [Google Scholar] [CrossRef] [PubMed]
- Short, N.A.; Tungate, A.S.; Bollen, K.A.; Sullivan, J.; D’Anza, T.; Lechner, M.; Bell, K.; Black, J.; Buchanan, J.; Reese, R.; et al. Pain is common after sexual assault and posttraumatic arousal/reactivity symptoms mediate the development of new or worsening persistent pain. Pain 2022, 163, e121–e128. [Google Scholar] [CrossRef]
- Frostholm, L.F.; Martin, A.P. Bodily distress syndromes and health anxiety. In Textbook of Applied Medical Psychology: A Multi-Disciplinary Approach; Pedersen, S., Roessler, K., Andersen, T., Johnsen, A., Pouwer, F., Eds.; University Press of Southern Denmark: Odense, Denmark, 2022; pp. 349–370. [Google Scholar]
- Moss-Morris, R.; Deary, V.; Castell, B. Chronic fatigue syndrome. Handb. Clin. Neurol. 2013, 110, 303–314. [Google Scholar] [CrossRef]
- Hou, R.; Moss-Morris, R.; Peveler, R.; Mogg, K.; Bradley, B.P.; Belli, A. When a minor head injury results in enduring symptoms: A prospective investigation of risk factors for postconcussional syndrome after mild traumatic brain injury. J. Neurol. Neurosurg. Psychiatry 2012, 83, 217–223. [Google Scholar] [CrossRef]
- Bohman, T.; Côté, P.; Boyle, E.; Cassidy, J.D.; Carroll, L.J.; Skillgate, E. Prognosis of patients with whiplash-associated disorders consulting physiotherapy: Development of a predictive model for recovery. BMC Musculoskelet. Disord. 2012, 13, 264. [Google Scholar] [CrossRef]
- Craig, T.K.; Cox, A.D.; Klein, K. Intergenerational transmission of somatization behaviour: A study of chronic somatizers and their children. Psychol. Med. 2002, 32, 805–816. [Google Scholar] [CrossRef]
- Afari, N.; Ahumada, S.M.; Wright, L.J.; Mostoufi, S.; Golnari, G.; Reis, V.; Cuneo, J.G. Psychological trauma and functional somatic syndromes: A systematic review and meta-analysis. Psychosom. Med. 2014, 76, 2–11. [Google Scholar] [CrossRef]
- Spiegel, D.R.; Shaukat, A.M.; McCroskey, A.L.; Chatterjee, A.; Ahmadi, T.; Simmelink, D.; Oldfield, E.C.; Pryor, C.R.; Faschan, M.; Raulli, O. Conceptualizing a subtype of patients with chronic pain: The necessity of obtaining a history of sexual abuse. Int. J. Psychiatry Med. 2016, 51, 84–103. [Google Scholar] [CrossRef]
- Drossman, D.A.; Leserman, J.; Nachman, G.; Li, Z.M.; Gluck, H.; Toomey, T.C.; Mitchell, C.M. Sexual and physical abuse in women with functional or organic gastrointestinal disorders. Ann. Intern. Med. 1990, 113, 828–833. [Google Scholar] [CrossRef] [PubMed]
- Baccini, F.; Pallotta, N.; Calabrese, E.; Pezzotti, P.; Corazziari, E. Prevalence of sexual and physical abuse and its relationship with symptom manifestations in patients with chronic organic and functional gastrointestinal disorders. Dig. Liver Dis. 2003, 35, 256–261. [Google Scholar] [CrossRef] [PubMed]
- Basile, K.C.; Smith, S.G.; Chen, J.; Zwald, M. Chronic Diseases, Health Conditions, and Other Impacts Associated With Rape Victimization of U.S. Women. J. Interpers. Violence 2020, 36, NP12504–NP12520. [Google Scholar] [CrossRef] [PubMed]
- Heitkemper, M.; Jarrett, M.; Taylor, P.; Walker, E.; Landenburger, K.; Bond, E.F. Effect of sexual and physical abuse on symptom experiences in women with irritable bowel syndrome. Nurs. Res. 2001, 50, 15–23. [Google Scholar] [CrossRef] [PubMed]
- Walker, E.A.; Katon, W.J.; Roy-Byrne, P.P.; Jemelka, R.P.; Russo, J. Histories of sexual victimization in patients with irritable bowel syndrome or inflammatory bowel disease. Am. J. Psychiatry 1993, 150, 1502–1506. [Google Scholar] [CrossRef]
- Rosenblat, J.D.; Mansur, R.B.; Brietzke, E.; Kennedy, S.H.; Carvalho, A.F.; Lee, Y.; Subramaniapillai, M.; Muzina, D.J.; Dale, R.; Tamura, J.K.; et al. Association of history of adverse childhood experiences with irritable bowel syndrome (IBS) in individuals with mood disorders. Psychiatry Res. 2020, 288, 112967. [Google Scholar] [CrossRef]
- Kaleycheva, N.; Cullen, A.E.; Evans, R.; Harris, T.; Nicholson, T.; Chalder, T. The role of lifetime stressors in adult fibromyalgia: Systematic review and meta-analysis of case-control studies. Psychol. Med. 2021, 51, 177–193. [Google Scholar] [CrossRef]
- Mason, F.; Lodrick, Z. Psychological consequences of sexual assault. Best Pract. Res. Clin. Obstet. Gynaecol. 2013, 27, 27–37. [Google Scholar] [CrossRef]
- Stein, M.B.; Lang, A.J.; Laffaye, C.; Satz, L.E.; Lenox, R.J.; Dresselhaus, T.R. Relationship of sexual assault history to somatic symptoms and health anxiety in women. Gen. Hosp. Psychiatry 2004, 26, 178–183. [Google Scholar] [CrossRef]
- Barsky, A.J.; Wool, C.; Barnett, M.C.; Cleary, P.D. Histories of childhood trauma in adult hypochondriacal patients. Am. J. Psychiatry 1994, 151, 397–401. [Google Scholar] [CrossRef]
- Winding, T.N.; Andersen, J.H. Do negative childhood conditions increase the risk of somatic symptoms in adolescence?—A prospective cohort study. BMC Public Health 2019, 19, 828. [Google Scholar] [CrossRef] [PubMed]
- Halpern, C.T.; Tucker, C.M.; Bengtson, A.; Kupper, L.L.; McLean, S.A.; Martin, S.L. Somatic symptoms among US adolescent females: Associations with sexual and physical violence exposure. Matern. Child Health J. 2013, 17, 1951–1960. [Google Scholar] [CrossRef] [PubMed]
- Taylor, R.R.; Jason, L.A. Chronic fatigue, abuse-related traumatization, and psychiatric disorders in a community-based sample. Soc. Sci. Med. 2002, 55, 247–256. [Google Scholar] [CrossRef]
- Bonvanie, I.J.; Janssens, K.A.; Rosmalen, J.G.; Oldehinkel, A.J. Life events and functional somatic symptoms: A population study in older adolescents. Br. J. Psychol. 2017, 108, 318–333. [Google Scholar] [CrossRef]
- Hauser, W.; Kosseva, M.; Uceyler, N.; Klose, P.; Sommer, C. Emotional, physical, and sexual abuse in fibromyalgia syndrome: A systematic review with meta-analysis. Arthritis Care Res. 2011, 63, 808–820. [Google Scholar] [CrossRef] [PubMed]
- Taylor, R.R.; Jason, L.A. Sexual abuse, physical abuse, chronic fatigue, and chronic fatigue syndrome: A community-based study. J. Nerv. Ment. Dis. 2001, 189, 709–715. [Google Scholar] [CrossRef]
- Bonvanie, I.J.; van Gils, A.; Janssens, K.A.; Rosmalen, J.G. Sexual abuse predicts functional somatic symptoms: An adolescent population study. Child Abuse Negl. 2015, 46, 1–7. [Google Scholar] [CrossRef]
- Nelson, S.; Baldwin, N.; Taylor, J. Mental health problems and medically unexplained physical symptoms in adult survivors of childhood sexual abuse: An integrative literature review. J. Psychiatr. Ment. Health Nurs. 2012, 19, 211–220. [Google Scholar] [CrossRef]
- Schnabel, K.; Petzke, T.M.; Witthöft, M. The emotion regulation process in somatic symptom disorders and related conditions—A systematic narrative review. Clin. Psychol. Rev. 2022, 97, 102196. [Google Scholar] [CrossRef]
- Lumley, M.A.; Schubiner, H. Emotional Awareness and Expression Therapy for Chronic Pain: Rationale, Principles and Techniques, Evidence, and Critical Review. Curr. Rheumatol. Rep. 2019, 21, 30. [Google Scholar] [CrossRef]
- Abbass, A.; Lumley, M.A.; Town, J.; Holmes, H.; Luyten, P.; Cooper, A.; Russell, L.; Schubiner, H.; De Meulemeester, C.; Kisely, S. Short-term psychodynamic psychotherapy for functional somatic disorders: A systematic review and meta-analysis of within-treatment effects. J. Psychosom. Res. 2021, 145, 110473. [Google Scholar] [CrossRef]
- Sanzarello, I.; Merlini, L.; Rosa, M.A.; Perrone, M.; Frugiuele, J.; Borghi, R.; Faldini, C. Central sensitization in chronic low back pain: A narrative review. J. Back Musculoskelet. Rehabil. 2016, 29, 625–633. [Google Scholar] [CrossRef] [PubMed]
- Sonu, S.; Post, S.; Feinglass, J. Adverse childhood experiences and the onset of chronic disease in young adulthood. Prev. Med. 2019, 123, 163–170. [Google Scholar] [CrossRef] [PubMed]
- McEwen, B.S. Allostasis and the Epigenetics of Brain and Body Health Over the Life Course: The Brain on Stress. JAMA Psychiatry 2017, 74, 551–552. [Google Scholar] [CrossRef]
- Iloson, C.; Möller, A.; Sundfeldt, K.; Bernhardsson, S. Symptoms within somatization after sexual abuse among women: A scoping review. Acta Obstet. Gynecol. Scand. 2021, 100, 758–767. [Google Scholar] [CrossRef] [PubMed]
- Dantoft, T.M.; Ebstrup, J.F.; Linneberg, A.; Skovbjerg, S.; Madsen, A.L.; Mehlsen, J.; Brinth, L.; Eplov, L.F.; Carstensen, T.W.; Schroder, A.; et al. Cohort description: The Danish study of Functional Disorders. Clin. Epidemiol. 2017, 9, 127–139. [Google Scholar] [CrossRef] [PubMed]
- Seery, M.D.; Holman, E.A.; Silver, R.C. Whatever does not kill us: Cumulative lifetime adversity, vulnerability, and resilience. J. Personal. Soc. Psychol. 2010, 99, 1025–1041. [Google Scholar] [CrossRef] [PubMed]
- Seery, M.D.; Leo, R.J.; Holman, E.A.; Silver, R.C. Lifetime exposure to adversity predicts functional impairment and healthcare utilization among individuals with chronic back pain. Pain 2010, 150, 507–515. [Google Scholar] [CrossRef] [PubMed]
- Carstensen, T.B.W.; Ørnbøl, E.; Fink, P.; Jørgensen, T.; Dantoft, T.M.; Madsen, A.L.; Buhmann, C.C.B.; Eplov, L.F.; Frostholm, L. Adverse life events in the general population—A validation of the cumulative lifetime adversity measure. Eur. J. Psychotraumatol. 2020, 11, 1717824. [Google Scholar] [CrossRef]
- Petersen, M.W.; Schröder, A.; Eliasen, M.H.; Fink, P.; Dantoft, T.M.; Jørgensen, T. Three different approaches to delimitation of functional somatic disorders: DanFunD. J. Psychosom. Res. 2021, 145, 110475. [Google Scholar] [CrossRef]
- Petersen, M.W.; Schröder, A.; Jørgensen, T.; Ørnbøl, E.; Dantoft, T.M.; Eliasen, M.; Carstensen, T.W.; Falgaard Eplov, L.; Fink, P. Prevalence of functional somatic syndromes and bodily distress syndrome in the Danish population: The DanFunD study. Scand. J. Public Health 2020, 48, 567–576. [Google Scholar] [CrossRef] [PubMed]
- Burton, C.; Fink, P.; Henningsen, P.; Löwe, B.; Rief, W. Functional somatic disorders: Discussion paper for a new common classification for research and clinical use. BMC Med. 2020, 18, 34. [Google Scholar] [CrossRef] [PubMed]
- Budtz-Lilly, A.; Fink, P.; Ørnbøl, E.; Vestergaard, M.; Moth, G.; Christensen, K.S.; Rosendal, M. A new questionnaire to identify bodily distress in primary care: The ‘BDS checklist’. J. Psychosom. Res. 2015, 78, 536–545. [Google Scholar] [CrossRef] [PubMed]
- Petersen, M.W.; Schröder, A.; Jørgensen, T.; Ørnbøl, E.; Dantoft, T.M.; Eliasen, M.; Thuesen, B.H.; Fink, P. The unifying diagnostic construct of bodily distress syndrome (BDS) was confirmed in the general population. J. Psychosom. Res. 2020, 128, 109868. [Google Scholar] [CrossRef] [PubMed]
- Fink, P.; Schröder, A. One single diagnosis, bodily distress syndrome, succeeded to capture 10 diagnostic categories of functional somatic syndromes and somatoform disorders. J. Psychosom. Res. 2010, 68, 415–426. [Google Scholar] [CrossRef]
- Fink, P.; Toft, T.; Hansen, M.S.; Ørnbøl, E.; Olesen, F. Symptoms and syndromes of bodily distress: An exploratory study of 978 internal medical, neurological, and primary care patients. Psychosom. Med. 2007, 69, 30–39. [Google Scholar] [CrossRef]
- Wolfe, F.; Smythe, H.A.; Yunus, M.B.; Bennett, R.M.; Bombardier, C.; Goldenberg, D.L.; Tugwell, P.; Campbell, S.M.; Abeles, M.; Clark, P.; et al. The American College of Rheumatology 1990 Criteria for the Classification of Fibromyalgia. Report of the Multicenter Criteria Committee. Arthritis Rheum 1990, 33, 160–172. [Google Scholar] [CrossRef]
- White, K.P.; Harth, M.; Speechley, M.; Ostbye, T. Testing an instrument to screen for fibromyalgia syndrome in general population studies: The London Fibromyalgia Epidemiology Study Screening Questionnaire. J. Rheumatol. 1999, 26, 880–884. [Google Scholar]
- Kay, L.; Jørgensen, T. Redefining Abdominal Syndromes Results of a Population-Based Study. Scand. J. Gastroenterol. 1996, 31, 469–475. [Google Scholar] [CrossRef]
- Chalder, T.; Berelowitz, G.; Pawlikowska, T.; Watts, L.; Wessely, S.; Wright, D.; Wallace, E.P. Development of a fatigue scale. J. Psychosom. Res. 1993, 37, 147–153. [Google Scholar] [CrossRef]
- Kasch, H.; Qerama, E.; Kongsted, A.; Bendix, T.; Jensen, T.S.; Bach, F.W. Clinical assessment of prognostic factors for long-term pain and handicap after whiplash injury: A 1-year prospective study. Eur. J. Neurol. 2008, 15, 1222–1230. [Google Scholar] [CrossRef] [PubMed]
- Lacour, M.; Zunder, T.; Schmidtke, K.; Vaith, P.; Scheidt, C. Multiple chemical sensitivity syndrome (MCS)–suggestions for an extension of the U.S. MCS-case definition. Int. J. Hyg. Environ. Health 2005, 208, 141–151. [Google Scholar] [CrossRef] [PubMed]
- Multiple chemical sensitivity: A 1999 consensus. Arch. Environ. Health 1999, 54, 147–149. [CrossRef] [PubMed]
- Fink, P.; Ørnbøl, E.; Hansen, M.S.; Søndergaard, L.; De Jonge, P. Detecting mental disorders in general hospitals by the SCL-8 scale. J. Psychosom. Res. 2004, 56, 371–375. [Google Scholar] [CrossRef] [PubMed]
- Derogatis, L.R. SCL-90-R: Administration, Scoring & Procedures Manual-II for the R(evised) Version and Other Instruments of the Psychopathology Rating Scale Series; Clinical Psychometric Research: Towson, MD, USA, 1992. [Google Scholar]
- Derogatis, L.R.; Lipman, R.S.; Covi, L. SCL-90: An outpatient psychiatric rating scale–preliminary report. Psychopharmacol. Bull. 1973, 9, 13–28. [Google Scholar]
- Christensen, K.S.; Fink, P.; Toft, T.; Frostholm, L.; Ørnbøl, E.; Olesen, F. A brief case-finding questionnaire for common mental disorders: The CMDQ. Fam. Pract. 2005, 22, 448–457. [Google Scholar] [CrossRef]
- Carstensen, T.B.W.; Ørnbøl, E.; Fink, P.; Pedersen, M.M.; Jørgensen, T.; Dantoft, T.M.; Benros, M.E.; Frostholm, L. Detection of illness worry in the general population: A specific item on illness rumination improves the Whiteley Index. J. Psychosom. Res. 2020, 138, 110245. [Google Scholar] [CrossRef]
- Demakakos, P.; Nazroo, J.; Breeze, E.; Marmot, M. Socioeconomic status and health: The role of subjective social status. Soc. Sci. Med. 2008, 67, 330–340. [Google Scholar] [CrossRef]
- StataCorp. Stata Statistical Software: Release 16; StataCorp LLC.: College Station, TX, USA, 2019. [Google Scholar]
- Peduzzi, P.; Concato, J.; Kemper, E.; Holford, T.R.; Feinstein, A.R. A simulation study of the number of events per variable in logistic regression analysis. J. Clin. Epidemiol. 1996, 49, 1373–1379. [Google Scholar] [CrossRef]
- Harrell, F.E. Regression Modeling Strategies: With Applications to Linear Models, Logistic Regression, and Survival Analysis; Springer: New York, NY, USA, 2001. [Google Scholar] [CrossRef]
- Casanovas, M.; Kramer, T.; Clarke, V.; Goddard, A.; Elena, G.M.; Khadr, S. Somatic symptoms following sexual assault in adolescents: A prospective longitudinal study. Psychol. Health Med. 2022, 27, 546–558. [Google Scholar] [CrossRef]
- Schou-Bredal, I.; Bonsaksen, T.; Ekeberg, Ø.; Skogstad, L.; Grimholt, T.K.; Lerdal, A.; Heir, T. Sexual Assault and the Association With Health, Quality of Life, and Self-Efficacy in the General Norwegian Population. J. Interpers. Violence 2022, 37, 1878–1901. [Google Scholar] [CrossRef] [PubMed]
- Byrne, C.A.; Resnick, H.S.; Kilpatrick, D.G.; Best, C.L.; Saunders, B.E. The socioeconomic impact of interpersonal violence on women. J. Consult. Clin. Psychol. 1999, 67, 362–366. [Google Scholar] [CrossRef] [PubMed]
- Bailey, B.E.; Freedenfeld, R.N.; Kiser, R.S.; Gatchel, R.J. Lifetime physical and sexual abuse in chronic pain patients: Psychosocial correlates and treatment outcomes. Disabil. Rehabil. 2003, 25, 331–342. [Google Scholar] [CrossRef] [PubMed]
- Salim, S.R.; Bhuptani, P.H.; Eshelman, L.R.; LaPlena, N.M.; Messman, T.L. Trauma-Related Shame Mediates the Associations Between Self-Blame, Bisexual Minority Stress, and Rape-Related PTSD Symptoms. J. Interpers. Violence 2023, 38, 10259–10281. [Google Scholar] [CrossRef] [PubMed]
- Scheer, J.R.; Harney, P.; Esposito, J.; Woulfe, J.M. Self-Reported Mental and Physical Health Symptoms and Potentially Traumatic Events Among Lesbian, Gay, Bisexual, Transgender, and Queer Individuals: The Role of Shame. Psychol. Violence 2020, 10, 131–142. [Google Scholar] [CrossRef] [PubMed]
- Schovsbo, S.U.; Dantoft, T.M.; Thuesen, B.H.; Leth-Møller, K.B.; Eplov, L.F.; Petersen, M.W.; Jørgensen, T.; Osler, M. Social position and functional somatic disorders: The DanFunD study. Scand. J. Public Health 2021, 1051, 225–232. [Google Scholar] [CrossRef]
- Petersen, M.W.; Ørnbøl, E.; Dantoft, T.M.; Fink, P. Assessment of functional somatic disorders in epidemiological research: Self-report questionnaires versus diagnostic interviews. J. Psychosom. Res. 2021, 146, 110491. [Google Scholar] [CrossRef]
- Mueser, K.T.; Goodman, L.B.; Trumbetta, S.L.; Rosenberg, S.D.; Osher, F.C.; Vidaver, R.; Auciello, P.; Foy, D.W. Trauma and Posttraumatic Stress Disorder in Severe Mental Illness. J. Consult. Clin. Psychol. 1998, 66, 493–499. [Google Scholar] [CrossRef]
- Mueser, K.T.; Rosenberg, S.D.; Goodman, L.A.; Trumbetta, S.L. Trauma, PTSD, and the course of severe mental illness: An interactive model. Schizophr. Res. 2002, 53, 123–143. [Google Scholar] [CrossRef]
| Variables (Measure) | Categories | Type of Assault | |||
|---|---|---|---|---|---|
| Total Population n = 7493 | Exposed to Sexual Assault n = 235 | Subdivisions on Sexual Assault | |||
| Rape n = 139 | Groping n = 179 | ||||
| Age at inclusion: Median (IQR) Age at exposure to SA% (n) | Baseline | 54 (44–63) | 51 (42–61) | 53 (44–62) | 50 (42–60) |
| <5 years | -- | 11.6 (27) | 6.5 (9) | 15.1 (27) | |
| 6–11 years | -- | 30.0 (70) | 20.9 (29) | 34.1 (61) | |
| 12–18 years | -- | 39.9 (93) | 38.1 (53) | 38.0 (68) | |
| >18 years | -- | 33.0 (77) | 34.5 (48) | 12.9 (23) | |
| Sex% (n) | Male | 46.1 (3456) | 11.1 (26) | 9.35 (13) | 13.41 (24) |
| Female | 53.9 (4037) | 88.9 (209) | 90.64 (126) | 86.59 (155) | |
| Vocational training% (n) | No education | 11.1 (829) | 12.8 (30) | 13.0 (18) | 12.9 (23) |
| <3 years | 15.2 (1142) | 17.0 (40) | 18.7 (26) | 18.4 (33) | |
| 3–4 years | 42.7 (3202) | 38.7 (91) | 37.4 (52) | 38.6 (69) | |
| >4 years | 28.3 (2118) | 27.7 (65) | 27.3 (38) | 26.3 (47) | |
| Missing 2.7 (202) | |||||
| Adverse childhood environment% (n) | Missing 1.7 (125) | 6.6 (491) | 10.6 (25) | 10.8 (15) | 12.9 (23) |
| Physical abuse% (n) | Missing 1.5 (115) | 13.4 (1000) | 50.6 (119) | 60.4 (84) | 53.6 (96) |
| Emotional abuse% (n) | Missing 4.1 (305) | 5.9 (444) | 35.3 (83) | 43.2 (60) | 35.8 (64) |
| Abuse (physical and/or emotional)% (n) | Missing 4.1 (305) | 16.0 (1.199) | 60.4 (142) | 68.3 (95) | 64.2 (115) |
| Social status Median (IQR) | Missing 1.1 (86) | 7 (6–8) | 6 (5–7) | 6 (5–7) | 6 (5–7) |
| Emotional distress% (n) | Missing 1.8 (136) | 4.8 (359) | 11.1 (26) | 13.0 (18) | 12.3 (22) |
| Health anxiety% (n) | Missing 0.5 (39) | 5.6 (421) | 11.5 (27) | 13.7 (19) | 12.3 (22) |
| FSD% (n) | Single-organ | 15.8 (1.184) | 6.0 (71) | 4.0 (47) | 4.3 (51) |
| Multi-organ | 1.1 (84) | 15.5 (13) | 10.7 (9) | 14.3 (12) | |
| Missing 1.8 (135) | |||||
| FSS% (n) | CWP | 4.6 (341) | 8.5 (20) | 10.1 (14) | 9.5 (17) |
| Missing 1.5 (109) | |||||
| IB | 3.6 (269) | 9.4 (22) | 11.5 (16) | 8.4 (15) | |
| Missing 2.3 (171) | |||||
| CF | 9.2 (690) | 22.6 (53) | 27.3 (38) | 25.1 (45) | |
| Missing 1.2 (93) | |||||
| MCS | 2.1 (156) | 7.2 (17) | 8.6 (12) | 6.7 (12) | |
| Missing 1.7 (130) | |||||
| WAD | 1.6 (121) | 4.7 (11) | 5.0 (7) | 4.5 (8) | |
| Missing 2.1 (160) | |||||
| FSD Cases | Crude | Adjusted * | ||||
|---|---|---|---|---|---|---|
| RR | 95% CI | p-Value | RR | 95% CI | p-Value | |
| Single-organ Crude n = 7096 Adjusted n = 6861 | 2.05 | (1.68–2.51) | <0.001 | 1.51 | (1.22–1.87) | <0.001 |
| Multi-organ Crude n = 6035 Adjusted n = 5840 | 6.95 | (3.91–12.32) | <0.001 | 3.51 | (1.89–6.49) | <0.001 |
| FSS Cases | ||||||
| CWP Crude n = 7112 Adjusted n = 6886 | 1.93 | 1.25–2.98 | 0.003 | 1.28 | 0.83–1.98 | 0.261 |
| IB Crude n = 7061 Adjusted n = 6829 | 2.76 | 1.82–4.18 | <0.001 | 2.00 | 1.30–3.07 | 0.002 |
| CF Crude n = 7135 Adjusted n = 6897 | 2.54 | 1.98–3.26 | <0.001 | 1.81 | 1.42–2.32 | <0.001 |
| MCS Crude n = 7107 Adjusted n = 6872 | 3.77 | 2.32–6.14 | <0.001 | 3.04 | 1.79–5.17 | <0.001 |
| WAD Crude n = 7075 Adjusted n = 6841 | 3.12 | 1.70–5.57 | <0.001 | 2.62 | 1.37–5.03 | 0.004 |
| FSD Cases | Crude | Adjusted * | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Groping | Rape | Groping | Rape | |||||||||
| RR | 95% CI | p-Value | RR | 95% CI | p-Value | RR | 95% CI | p-Value | RR | 95% CI | p-Value | |
| Single-organ | 1.94 | (1.54–2.46) | <0.001 | 2.31 | (1.83–2.92) | <0.001 | 1.39 | (1.08–1.80) | 0.011 | 1.64 | (1.28–2.09) | <0.001 |
| Multi-organ | 8.13 | (4.51–14.63) | <0.001 | 8.41 | (4.33–16.33) | <0.001 | 3.76 | (1.99–7.09) | <0.001 | 5.18 | (2.73–9.86) | <0.001 |
| FSS Cases | ||||||||||||
| CWP | 2.15 | (1.35–3.42) | 0.001 | 2.29 | (1.38–3.80) | 0.001 | 1.35 | (0.85–2.14) | 0.211 | 1.35 | (0.79–2.30) | 0.271 |
| IB | 2.41 | (1.46–3.98) | 0.001 | 3.42 | (2.13–5.13) | <0.001 | 1.68 | (1.00–2.82) | 0.049 | 2.59 | (1.61–4.16) | <0.001 |
| CF | 2.82 | (2.17–3.68) | <0.001 | 3.06 | (2.31–4.05) | <0.001 | 1.89 | (1.46–2.45) | <0.001 | 2.14 | (1.64–2.79) | <0.001 |
| MCS | 3.40 | (1.92–6.01) | <0.001 | 4.78 | (2.54–7.89) | <0.001 | 2.50 | (1.33–4.71) | 0.005 | 3.61 | (1.99–6.58) | <0.001 |
| WAD | 2.91 | (1.44–5.88) | 0.003 | 3.32 | (1.58–7.00) | 0.002 | 2.29 | (1.07–4.90) | 0.033 | 2.97 | (1.39–6.33) | 0.005 |
| FSD Cases | Sexual Assault * | Groping * | Rape * | ||||||
|---|---|---|---|---|---|---|---|---|---|
| RR | 95% CI | p-Value | RR | 95% CI | p-Value | RR | 95% CI | p-Value | |
| Single-organ | 1.23 | (1.08–1.41) | 0.002 | 1.12 | (0.98–1.29) | 0.107 | 1.29 | (1.08–1.53) | 0.004 |
| Multi-organ | 2.45 | (1.25–3.43) | 0.009 | 2.54 | (1.26–5.12) | 0.009 | 3.73 | (1.85–7.52) | <0.0001 |
| FSS Cases | |||||||||
| CWP | 1.05 | (0.67–1.65) | 0.828 | 1.09 | (0.67–1.77) | 0.736 | 1.07 | (0.62–1.86) | 0.804 |
| IB | 1.63 | (1.02–2.62) | 0.041 | 1.26 | (0.71–2.25) | 0.431 | 2.32 | (1.41–3.83) | 0.001 |
| CF | 1.68 | (1.36–2.07) | <0.001 | 1.70 | (1.37–2.10) | <0.0001 | 1.97 | (1.59–2.45) | <0.0001 |
| MCS | 2.52 | (1.26–4.01) | 0.006 | 1.92 | (0.99–3.72) | 0.053 | 2.45 | (1.26–4.76) | 0.008 |
| WAD | 1.98 | (1.00–3.91) | 0.049 | 1.67 | (0.76–3.67) | 0.205 | 2.08 | (0.95–4.59) | 0.068 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jacobsen, S.A.; Frostholm, L.; Buhmann, C.B.; Petersen, M.W.; Ørnbøl, E.; Dantoft, T.M.; Bjerregaard, A.A.; Eplov, L.F.; Carstensen, T.B.W. Are Sexual Assaults Related to Functional Somatic Disorders? A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2023, 20, 6947. https://doi.org/10.3390/ijerph20206947
Jacobsen SA, Frostholm L, Buhmann CB, Petersen MW, Ørnbøl E, Dantoft TM, Bjerregaard AA, Eplov LF, Carstensen TBW. Are Sexual Assaults Related to Functional Somatic Disorders? A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2023; 20(20):6947. https://doi.org/10.3390/ijerph20206947
Chicago/Turabian StyleJacobsen, Sofie Abildgaard, Lisbeth Frostholm, Cæcilie Böck Buhmann, Marie Weinreich Petersen, Eva Ørnbøl, Thomas Meinertz Dantoft, Anne Ahrendt Bjerregaard, Lene Falgaard Eplov, and Tina Birgitte Wisbech Carstensen. 2023. "Are Sexual Assaults Related to Functional Somatic Disorders? A Cross-Sectional Study" International Journal of Environmental Research and Public Health 20, no. 20: 6947. https://doi.org/10.3390/ijerph20206947
APA StyleJacobsen, S. A., Frostholm, L., Buhmann, C. B., Petersen, M. W., Ørnbøl, E., Dantoft, T. M., Bjerregaard, A. A., Eplov, L. F., & Carstensen, T. B. W. (2023). Are Sexual Assaults Related to Functional Somatic Disorders? A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 20(20), 6947. https://doi.org/10.3390/ijerph20206947







