The Impact of the COVID-19 Pandemic on the Severity of Alcohol Use Disorder: Significance of Dual Disorders
Abstract
:1. Introduction
2. Materials and Methods
2.1. Setting
2.2. Statistical Analysis
3. Results
3.1. Sample Characteristics
3.2. Characteristics of Admissions before and during COVID-19 Pandemic
3.3. Distribution Pattern of Psychiatric Co-Morbidities
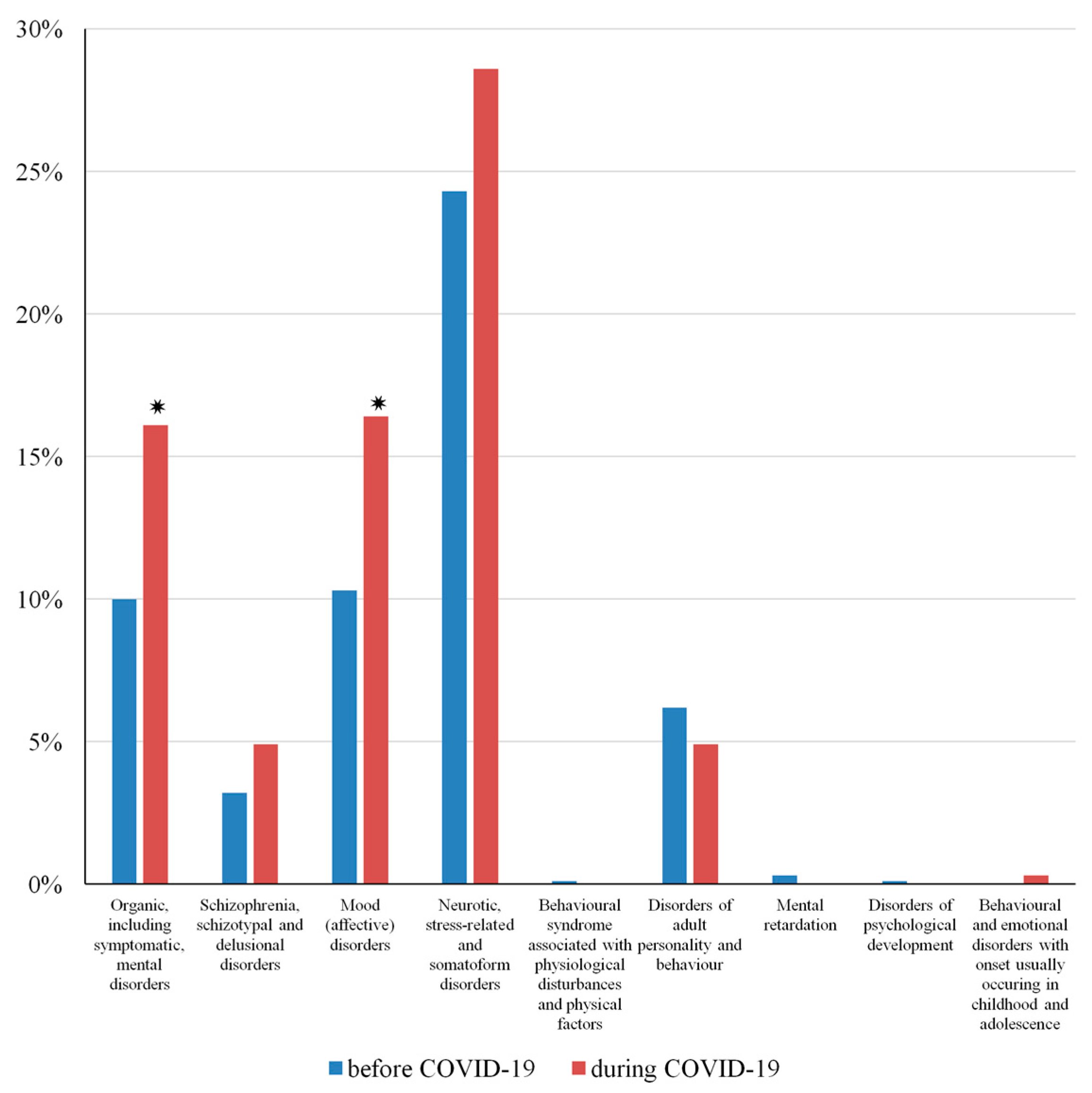
3.4. Contributing Factors to Admissions during COVID-19
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO Coronavirus Disease (COVID-19) Dashboard; WHO: Geneva, Switzerland, 2020.
- Keni, R.; Alexander, A.; Nayak, P.G.; Mudgal, J.; Nandakumar, K. COVID-19: Emergence, Spread, Possible Treatments, and Global Burden. Front. Public Health 2020, 8, 216. [Google Scholar] [CrossRef] [PubMed]
- Lau, E.H.Y.; Leung, G.M. Reply to: Is Presymptomatic Spread a Major Contributor to COVID-19 Transmission? Nat. Med. 2020, 26, 1534–1535. [Google Scholar] [CrossRef] [PubMed]
- Fisayo, T.; Tsukagoshi, S. Three Waves of the COVID-19 Pandemic. Postgrad. Med. J. 2020, 97, 332. [Google Scholar] [CrossRef] [PubMed]
- Pfefferbaum, B.; North, C.S. Mental Health and the COVID-19 Pandemic. N. Engl. J. Med. 2020, 383, 510–512. [Google Scholar] [CrossRef]
- Sher, L. Dual Disorders and Suicide during and Following the COVID-19 Pandemic. Acta Neuropsychiatr. 2020, 33, 49–50. [Google Scholar] [CrossRef] [PubMed]
- Pierce, M.; McManus, S.; Hope, H.; Hotopf, M.; Ford, T.; Hatch, S.L.; John, A.; Kontopantelis, E.; Webb, R.T.; Wessely, S.; et al. Mental Health Responses to the COVID-19 Pandemic: A Latent Class Trajectory Analysis Using Longitudinal UK Data. Lancet Psychiatry 2021, 8, 610–619. [Google Scholar] [CrossRef]
- Zaninotto, L.; Rossi, G.; Danieli, A.; Frasson, A.; Meneghetti, L.; Zordan, M.; Tito, P.; Salvetti, B.; Conca, A.; Ferranti, R.; et al. Exploring the Relationships among Personality Traits, Burnout Dimensions and Stigma in a Sample of Mental Health Professionals. Psychiatry Res. 2018, 264, 327–333. [Google Scholar] [CrossRef]
- Zortea, T.C.; Brenna, C.T.A.; Joyce, M.; McClelland, H.; Tippett, M.; Tran, M.M.; Arensman, E.; Corcoran, P.; Hatcher, S.; Heise, M.J.; et al. The Impact of Infectious Disease-Related Public Health Emergencies on Suicide, Suicidal Behavior, and Suicidal Thoughts. Crisis 2020, 42, 474–487. [Google Scholar] [CrossRef]
- Volkow, N.D.; Torrens, M.; Poznyak, V.; Sáenz, E.; Busse, A.; Kashino, W.; Krupchanka, D.; Kestel, D.; Campello, G.; Gerra, G. Managing Dual Disorders: A Statement by the Informal Scientific Network, UN Commission on Narcotic Drugs. World Psychiatry 2020, 19, 396–397. [Google Scholar] [CrossRef]
- Schmoll, S.; Boyer, L.; Henry, J.-M.; Belzeaux, R. Frequent Visitors to Psychiatric Emergency Service: Demographical and Clinical Analysis. Encephale 2013, 41, 123–129. [Google Scholar] [CrossRef]
- Stahler, G.J.; Mennis, J.; Cotlar, R.; Baron, D.A. The Influence of Neighborhood Environment on Treatment Continuity and Rehospitalization in Dually Diagnosed Patients Discharged from Acute Inpatient Care. Am. J. Psychiatry 2009, 166, 1258–1268. [Google Scholar] [CrossRef] [PubMed]
- Samet, S.; Fenton, M.C.; Nunes, E.; Greenstein, E.; Aharonovich, E.; Hasin, D. Effects of Independent and Substance-Induced Major Depressive Disorder on Remission and Relapse of Alcohol, Cocaine and Heroin Dependence. Addiction 2012, 108, 115–123. [Google Scholar] [CrossRef] [PubMed]
- Fridell, M.; Bäckström, M.; Hesse, M.; Krantz, P.; Perrin, S.; Nyhlén, A. Prediction of Psychiatric Comorbidity on Premature Death in a Cohort of Patients with Substance Use Disorders: A 42-Year Follow-Up. BMC Psychiatry 2019, 19, 150. [Google Scholar] [CrossRef]
- Regier, D.A.; Farmer, M.E.; Rae, D.S.; Locke, B.Z.; Keith, S.J.; Judd, L.L.; Goodwin, F.K. Comorbidity of Mental Disorders with Alcohol and Other Drug Abuse. Results from the Epidemiologic Catchment Area (ECA) Study. JAMA 1990, 264, 2511–2518. [Google Scholar] [CrossRef] [PubMed]
- Toftdahl, N.G.; Nordentoft, M.; Hjorthøj, C. Prevalence of Substance Use Disorders in Psychiatric Patients: A Nationwide Danish Population-Based Study. Soc. Psychiatry Psychiatr. Epidemiol. 2015, 51, 129–140. [Google Scholar] [CrossRef]
- Lehman, A.F.; Myers, C.P.; Corty, E.; Thompson, J.W. Prevalence and Patterns of “Dual Diagnosis” among Psychiatric Inpatients. Compr. Psychiatry 1994, 35, 106–112. [Google Scholar] [CrossRef]
- Temmingh, H.S.; Williams, T.; Siegfried, N.; Stein, D.J. Risperidone versus Other Antipsychotics for People with Severe Mental Illness and Co-Occurring Substance Misuse. Cochrane Database Syst. Rev. 2018, 1, CD011057. [Google Scholar] [CrossRef]
- Carrà, G.; Bartoli, F.; Brambilla, G.; Crocamo, C.; Clerici, M. Comorbid Addiction and Major Mental Illness in Europe: A Narrative Review. Subst. Abus. 2014, 36, 75–81. [Google Scholar] [CrossRef]
- Alsuhaibani, R.; Smith, D.C.; Lowrie, R.; Aljhani, S.; Paudyal, V. Scope, Quality and Inclusivity of International Clinical Guidelines on Mental Health and Substance Abuse in Relation to Dual Diagnosis, Social and Community Outcomes: A Systematic Review. BMC Psychiatry 2021, 21, 209. [Google Scholar] [CrossRef]
- Fantuzzi, C.; Mezzina, R. Dual Diagnosis: A Systematic Review of the Organization of Community Health Services. Int. J. Soc. Psychiatry 2020, 66, 300–310. [Google Scholar] [CrossRef]
- Chen, C.; Balogh, M.; Bathija, J.; Howanitz, E.; Plutchik, R.; Conte, H.R. Substance Abuse among Psychiatric Inpatients. Compr. Psychiatry 1992, 33, 60–64. [Google Scholar] [CrossRef]
- Roberts, A.; Rogers, J.; Mason, R.; Siriwardena, A.N.; Hogue, T.; Whitley, G.A.; Law, G.R. Alcohol and Other Substance Use during the COVID-19 Pandemic: A Systematic Review. Drug Alcohol Depend. 2021, 229, 109150. [Google Scholar] [CrossRef] [PubMed]
- Boehnke, K.F.; McAfee, J.; Ackerman, J.M.; Kruger, D.J. Medication and Substance Use Increases among People Using Cannabis Medically during the COVID-19 Pandemic. Int. J. Drug Policy 2020, 92, 103053. [Google Scholar] [CrossRef] [PubMed]
- Lechner, W.V.; Laurene, K.R.; Patel, S.; Anderson, M.; Grega, C.; Kenne, D.R. Changes in Alcohol Use as a Function of Psychological Distress and Social Support Following COVID-19 Related University Closings. Addict. Behav. 2020, 110, 106527. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Li, Y.; Bao, Y.; Meng, S.; Sun, Y.; Schumann, G.; Kosten, T.; Strang, J.; Lu, L.; Shi, J. Brief Report: Increased Addictive Internet and Substance Use Behavior During the COVID-19 Pandemic in China. Am. J. Addict. 2020, 29, 268–270. [Google Scholar] [CrossRef]
- Sohi, I.; Chrystoja, B.R.; Rehm, J.; Wells, S.; Monteiro, M.; Ali, S.; Shield, K.D. Changes in Alcohol Use during the COVID-19 Pandemic and Previous Pandemics: A Systematic Review. Alcohol Clin. Exp. Res. 2022, 46, 498–513. [Google Scholar] [CrossRef] [PubMed]
- Killgore, W.D.S.; Cloonan, S.A.; Taylor, E.C.; Lucas, D.A.; Dailey, N.S. Alcohol Dependence during COVID-19 Lockdowns. Psychiatry Res. 2020, 296, 113676. [Google Scholar] [CrossRef]
- Foran, H.M.; O’Leary, K.D. Alcohol and Intimate Partner Violence: A Meta-Analytic Review. Clin. Psychol. Rev. 2008, 28, 1222–1234. [Google Scholar] [CrossRef]
- Saengow, U.; Assanangkornchai, S.; Casswell, S. Alcohol: A Probable Risk Factor of COVID-19 Severity. Addiction 2020, 116, 204–205. [Google Scholar] [CrossRef]
- Wood, E.; Albarqouni, L.; Tkachuk, S.; Green, C.J.; Ahamad, K.; Nolan, S.; McLean, M.; Klimas, J. Will This Hospitalized Patient Develop Severe Alcohol Withdrawal Syndrome?: The Rational Clinical Examination Systematic Review. JAMA 2018, 320, 825–833. [Google Scholar] [CrossRef]
- Pribék, I.K.; Kádár, B.K.; Péter, L.; Daróczy, J.; Bajsz, A.; Kovács, C.S.; Demeter, I.; Janka, Z.; Urbán, R.; Demetrovics, Z.; et al. Seasonality and Delirium Tremens in Hospitalized Patients with Alcohol Dependence Syndrome. Eur. Addict. Res. 2023, 29, 83–91. [Google Scholar] [CrossRef] [PubMed]
- Maldonado, J.R. Novel Algorithms for the Prophylaxis and Management of Alcohol Withdrawal Syndromes-Beyond Benzodiazepines. Crit. Care Clin. 2017, 33, 559–599. [Google Scholar] [CrossRef] [PubMed]
- Maldonado, J.R.; Sher, Y.; Das, S.; Hills-Evans, K.; Frenklach, A.; Lolak, S.; Talley, R.; Neri, E. Prospective Validation Study of the Prediction of Alcohol Withdrawal Severity Scale (PAWSS) in Medically Ill Inpatients: A New Scale for the Prediction of Complicated Alcohol Withdrawal Syndrome. Alcohol Alcohol. 2015, 50, 509–518. [Google Scholar] [CrossRef] [PubMed]
- Maldonado, J.R. Delirium in the Acute Care Setting: Characteristics, Diagnosis and Treatment. Crit. Care Clin. 2008, 24, 657–722. [Google Scholar] [CrossRef] [PubMed]
- Goodson, C.M.; Clark, B.J.; Douglas, I.S. Predictors of Severe Alcohol Withdrawal Syndrome: A Systematic Review and Meta-Analysis. Alcohol Clin. Exp. Res. 2014, 38, 2664–2677. [Google Scholar] [CrossRef] [PubMed]
- Eyer, F.; Schuster, T.; Felgenhauer, N.; Pfab, R.; Strubel, T.; Saugel, B.; Zilker, T. Risk Assessment of Moderate to Severe Alcohol Withdrawal—Predictors for Seizures and Delirium Tremens in the Course of Withdrawal. Alcohol Alcohol. 2011, 46, 427–433. [Google Scholar] [CrossRef]
- IBM Corp. Released 2016. IBM SPSS Statistics for Windows, Version 24.0; IBM Corp: Armonk, NY, USA, 2016.
- Filip, R.; Gheorghita Puscaselu, R.; Anchidin-Norocel, L.; Dimian, M.; Savage, W.K. Global Challenges to Public Health Care Systems during the COVID-19 Pandemic: A Review of Pandemic Measures and Problems. J. Pers. Med. 2022, 12, 1295. [Google Scholar] [CrossRef]
- Haldane, V.; De Foo, C.; Abdalla, S.M.; Jung, A.-S.; Tan, M.; Wu, S.; Chua, A.; Verma, M.; Shrestha, P.; Singh, S.; et al. Health Systems Resilience in Managing the COVID-19 Pandemic: Lessons from 28 Countries. Nat. Med. 2021, 27, 964–980. [Google Scholar] [CrossRef]
- Brülhart, M.; Klotzbücher, V.; Lalive, R.; Reich, S.K. Mental Health Concerns during the COVID-19 Pandemic as Revealed by Helpline Calls. Nature 2021, 600, 121–126. [Google Scholar] [CrossRef]
- McPhee, M.D.; Keough, M.T.; Rundle, S.; Heath, L.M.; Wardell, J.D.; Hendershot, C.S. Depression, Environmental Reward, Coping Motives and Alcohol Consumption During the COVID-19 Pandemic. Front. Psychiatry 2020, 11, 574676. [Google Scholar] [CrossRef]
- Błaszczyk-Bębenek, E.; Jagielski, P.; Bolesławska, I.; Jagielska, A.; Nitsch-Osuch, A.; Kawalec, P. Nutrition Behaviors in Polish Adults before and during COVID-19 Lockdown. Nutrients 2020, 12, 3084. [Google Scholar] [CrossRef] [PubMed]
- Niedzwiedz, C.L.; Green, M.J.; Benzeval, M.; Campbell, D.; Craig, P.; Demou, E.; Leyland, A.; Pearce, A.; Thomson, R.; Whitley, E.; et al. Mental Health and Health Behaviours before and during the Initial Phase of the COVID-19 Lockdown: Longitudinal Analyses of the UK Household Longitudinal Study. J. Epidemiol. Community Health 2020, 75, 224–231. [Google Scholar] [CrossRef] [PubMed]
- Mansfield, K.E.; Mathur, R.; Tazare, J.; Henderson, A.D.; Mulick, A.R.; Carreira, H.; Matthews, A.A.; Bidulka, P.; Gayle, A.; Forbes, H.; et al. Indirect effects of the COVID-19 pandemic on physical and mental health in the UK: A population-based study. Lancet Digit Health 2021, 3, 217–230. [Google Scholar] [CrossRef]
- Gotlib, I.H.; Borchers, L.R.; Chahal, R.; Gifuni, A.J.; Teresi, G.I.; Ho, T.C. Early Life Stress Predicts Depressive Symptoms in Adolescents During the COVID-19 Pandemic: The Mediating Role of Perceived Stress. Front. Psychol. 2021, 11, 603748. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Shuai, L.; Yu, H.; Wang, Z.; Qiu, M.; Lu, L.; Cao, X.; Xia, W.; Wang, Y.; Chen, R. Acute Stress, Behavioural Symptoms and Mood States among School-Age Children with Attention-Deficit/Hyperactive Disorder during the COVID-19 Outbreak. Asian J. Psychiatr. 2020, 51, 102077. [Google Scholar] [CrossRef] [PubMed]
- Samji, H.; Wu, J.; Ladak, A.; Vossen, C.; Stewart, E.; Dove, N.; Long, D.; Snell, G. Review: Mental Health Impacts of the COVID-19 Pandemic on Children and Youth—A Systematic Review. Child Adolesc. Ment. Health 2021, 27, 173–189. [Google Scholar] [CrossRef] [PubMed]
- Barach, P.; Fisher, S.D.; Adams, M.J.; Burstein, G.R.; Brophy, P.D.; Kuo, D.Z.; Lipshultz, S.E. Disruption of Healthcare: Will the COVID Pandemic Worsen Non-COVID Outcomes and Disease Outbreaks? Prog. Pediatr. Cardiol. 2020, 59, 101254. [Google Scholar] [CrossRef]
- Rawaf, S.; Allen, L.N.; Stigler, F.L.; Kringos, D.; Quezada Yamamoto, H.; van Weel, C.; Global Forum on Universal Health Coverage and Primary Health Care. Lessons on the COVID-19 Pandemic, for and by Primary Care Professionals Worldwide. Eur. J. Gen. Pract. 2020, 26, 129–133. [Google Scholar] [CrossRef]
- Tuczyńska, M.; Matthews-Kozanecka, M.; Baum, E. Accessibility to Non-COVID Health Services in the World During the COVID-19 Pandemic: Review. Front. Public Health 2021, 9, 760795. [Google Scholar] [CrossRef]
- Bower, M.; Smout, S.; Donohoe-Bales, A.; O’Dean, S.; Teesson, L.; Boyle, J.; Lim, D.; Nguyen, A.; Calear, A.L.; Batterham, P.J.; et al. A Hidden Pandemic? An Umbrella Review of Global Evidence on Mental Health in the Time of COVID-19. Front. Psychiatry 2023, 14, 1107560. [Google Scholar] [CrossRef]
- Katz, B.A.; Yovel, I. Mood Symptoms Predict COVID-19 Pandemic Distress but Not Vice Versa: An. PLoS ONE 2022, 17, e0273945. [Google Scholar] [CrossRef] [PubMed]
- Olié, E.; Dubois, J.; Benramdane, M.; Guillaume, S.; Courtet, P. Psychological State of a Sample of Patients with Mood Disorders during the First French COVID-19 Lockdown. Sci. Rep. 2021, 11, 23711. [Google Scholar] [CrossRef] [PubMed]
- Wei, G.; Diehl-Schmid, J.; Matias-Guiu, J.A.; Pijnenburg, Y.; Landin-Romero, R.; Bogaardt, H.; Piguet, O.; Kumfor, F. The Effects of the COVID-19 Pandemic on Neuropsychiatric Symptoms in Dementia and Carer Mental Health: An International Multicentre Study. Sci. Rep. 2022, 12, 2418. [Google Scholar] [CrossRef] [PubMed]
- Gaigher, J.M.; Lacerda, I.B.; Dourado, M.C.N. Dementia and Mental Health during the COVID-19 Pandemic: A Systematic Review. Front. Psychiatry 2022, 13, 879598. [Google Scholar] [CrossRef]
| ‘Before COVID-19’ n = 753 | ‘During COVID-19’ n = 329 | |
|---|---|---|
| Mean age (SD) | 50.920 (11.853) | 52.500 (11.567) * |
| Male (adj. res.) | 81.7% (1.1) | 78.7% (−1.1) |
| Female (adj. res.) | 18.3% (−1.1) | 21.3% (1.1) |
| Somatic co-morbidity (adj. res.) | 65.1% (0.2) | 63.8% (−0.2) |
| Psychiatric co-morbidity (adj. res.) | 48.1% (−4.7) | 63.8% (4.7) * |
| AWS (adj. res.) | 72.7% (1.4) | 68.7% (−1.4) |
| DT (adj. res.) | 7.2% (−3.1) | 13.1% (3.1) * |
| ARS (adj. res.) | 9.8% (−1.0) | 12.2% (1.0) |
| GGT (mean, SD) | 271.757 (747.787) | 361.665 (665.594) |
| SGOT (mean, SD) | 73.150 (125.092) | 75.780 (71.314) |
| SGPT (mean, SD) | 54.64 (64.728) | 54.43 (37.183) |
| SGOT/SGPT (mean, SD) | 1.424 (0.776) | 1.454 (0.818) |
| Sodium (mean, SD) | 138.974 (4.073) | 138.668 (4.508) |
| Potassium (mean, SD) | 4.010 (0.543) | 4.03 (0.639) |
| Platelet number (mean, SD) | 215.650 (106.223) | 225.570 (139.651) |
| B | SE | df | p | OR | 95% Confidence Interval for OR | ||
|---|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||||
| Age | 0.128 | 0.073 | 1 | 0.080 | 1.137 | 0.985 | 1.311 |
| DT− | −0.711 | 0.228 | 1 | 0.002 * | 0.491 | 0.314 | 0.767 |
| DT+ | 0 | 0 | |||||
| Psychiatric co-morbidity− | −0.636 | 0.152 | 1 | <0.001 * | 0.529 | 0.393 | 0.713 |
| Psychiatric co-morbidity+ | 0 | 0 | |||||
| B | SE | df | p | OR | 95% Confidence Interval for OR | ||
|---|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||||
| DT− * Age | 0.0800 | 0.101 | 1 | 0.430 | 1.083 | 0.888 | 1.321 |
| DT+ * Age | 0.398 | 0.223 | 1 | 0.074 | 1.488 | 0.962 | 2.302 |
| DT− * Psychiatric co-morbidity− | −1.400 | 0.380 | 1 | <0.001 * | 0.247 | 0.117 | 0.520 |
| DT− * Psychiatric co-morbidity+ | −0.802 | 0.376 | 1 | 0.033 * | 0.448 | 0.214 | 0.937 |
| DT+ * Psychiatric co-morbidity− | −0.918 | 0.451 | 1 | 0.042 * | 0.399 | 0.165 | 0.966 |
| DT+ * Psychiatric co-morbidity+ | 0 | 0 | |||||
| Psychiatric co-morbidity− * Age | 0.007 | 0.149 | 1 | 0.961 | 1.007 | 0.753 | 1.349 |
| Psychiatric co-morbidity+ * Age | 0 | 0 | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gajdics, J.; Bagi, O.; Farkas, F.F.; Andó, B.; Pribék, I.K.; Lázár, B.A. The Impact of the COVID-19 Pandemic on the Severity of Alcohol Use Disorder: Significance of Dual Disorders. Int. J. Environ. Res. Public Health 2023, 20, 6939. https://doi.org/10.3390/ijerph20206939
Gajdics J, Bagi O, Farkas FF, Andó B, Pribék IK, Lázár BA. The Impact of the COVID-19 Pandemic on the Severity of Alcohol Use Disorder: Significance of Dual Disorders. International Journal of Environmental Research and Public Health. 2023; 20(20):6939. https://doi.org/10.3390/ijerph20206939
Chicago/Turabian StyleGajdics, Janka, Otília Bagi, Fanni Fruzsina Farkas, Bálint Andó, Ildikó Katalin Pribék, and Bence András Lázár. 2023. "The Impact of the COVID-19 Pandemic on the Severity of Alcohol Use Disorder: Significance of Dual Disorders" International Journal of Environmental Research and Public Health 20, no. 20: 6939. https://doi.org/10.3390/ijerph20206939
APA StyleGajdics, J., Bagi, O., Farkas, F. F., Andó, B., Pribék, I. K., & Lázár, B. A. (2023). The Impact of the COVID-19 Pandemic on the Severity of Alcohol Use Disorder: Significance of Dual Disorders. International Journal of Environmental Research and Public Health, 20(20), 6939. https://doi.org/10.3390/ijerph20206939







