Nursing Home Residents Hospitalization at the End of Life: Experience and Predictors in Portuguese Nursing Homes
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
Study Population
2.2. Variables and Instruments
2.3. Statistical Analysis
3. Results
3.1. Residents
3.2. Hospitalizations and In-Hospital Death
3.3. Bivariate Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hoogendijk, E.O.; Afilalo, J.; Ensrud, K.E.; Kowal, P.; Onder, G.; Fried, L.P. Frailty: Implications for clinical practice and public health. Lancet 2019, 394, 1365–1375. [Google Scholar] [CrossRef]
- World Health Organization. World Report on Ageing and Health; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Manfredi, G.; Midão, L.; Paúl, C.; Cena, C.; Duarte, M.; Costa, E. Prevalence of frailty status among the European elderly population: Findings from the Survey of Health, Aging and Retirement in Europe. Geriatr. Gerontol. Int. 2019, 19, 723–729. [Google Scholar] [CrossRef] [PubMed]
- Clegg, A.; Young, J.; Iliffe, S.; Rikkert, M.O.; Rockwood, K. Frailty in elderly people. Lancet 2013, 381, 752–762. [Google Scholar] [CrossRef] [PubMed]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in Older adults: Evidence for a phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, M146–M156. [Google Scholar] [CrossRef] [PubMed]
- O’Caoimh, R.; Sezgin, D.; O’Donovan, M.R.; Molloy, D.W.; Clegg, A.; Rockwood, K.; Liew, A. Prevalence of frailty in 62 countries across the world: A systematic review and meta-analysis of population-level studies. Age Ageing 2021, 50, 96–104. [Google Scholar] [CrossRef] [PubMed]
- Bone, A.E.; Gomes, B.; Etkind, S.N.; Verne, J.; Murtagh, F.; Evans, C.J.; Higginson, I.J. What is the impact of population ageing on the future provision of end-of-life care? Population-based projections of place of death. Palliat. Med. 2018, 32, 329–336. [Google Scholar] [CrossRef]
- Lim, W.S.; Wong, S.F.; Leong, I.; Choo, P.; Pang, W.S. Forging a Frailty-Ready Healthcare System to Meet Population Ageing. Int. J. Environ. Res. Public Health 2017, 14, 1448. [Google Scholar] [CrossRef]
- Blumenthal, D.; Dixon, J. Health-care reforms in the USA and England: Areas for useful learning. Lancet 2012, 380, 1352–1357. [Google Scholar] [CrossRef]
- Graverholt, B.; Forsetlund, L.; Jamtvedt, G. Reducing hospital admissions from nursing homes: A systematic review. BMC Health Serv. Res. 2014, 14, 36. [Google Scholar] [CrossRef]
- Bone, A.E.; Evans, C.J.; A Henson, L.; Gao, W.; Higginson, I.J. Patterns of emergency department attendance among older people in the last three months of life and factors associated with frequent attendance: A mortality follow-back survey. Age Ageing 2019, 48, 680–687. [Google Scholar] [CrossRef]
- Wiggins, N.; Droney, J.; Mohammed, K.; Riley, J.; E Sleeman, K. Understanding the factors associated with patients with dementia achieving their preferred place of death: A retrospective cohort study. Age Ageing 2019, 48, 433–439. [Google Scholar] [CrossRef]
- Hockley, J.; Watson, J.; Oxenham, D.; Murray, S. The integrated implementation of two end-of-life care tools in nursing care homes in the UK: An in-depth evaluation. Palliat. Med. 2010, 24, 828–838. [Google Scholar] [CrossRef] [PubMed]
- Allers, K.; Hoffmann, F.; Schnakenberg, R. Hospitalizations of nursing home residents at the end of life: A systematic review. Palliat. Med. 2019, 33, 1282–1298. [Google Scholar] [CrossRef] [PubMed]
- Hsu, Y.H.; Chou, M.Y.; Chen, H.-M.; Chang, W.-C.; Chu, C.S.; Wang, Y.-C.; Hsu, C.-L.; Liang, C.-K.; Lee, C.-C.; Lin, Y.T. The Trend of Aggressive Treatments in End-of-Life Care for Older People with Dementia after a Policy Change in Taiwan. J. Am. Med. Dir. Assoc. 2020, 21, 858–863.e1. [Google Scholar] [CrossRef] [PubMed]
- Bone, A.E.; Evans, C.J.; Etkind, S.N.; Sleeman, K.E.; Gomes, B.; Aldridge, M.; Keep, J.; Verne, J.; Higginson, I.J. Factors associated with older people’s emergency department attendance towards the end of life: A systematic review. Eur. J. Public Health 2019, 29, 67–74. [Google Scholar] [CrossRef] [PubMed]
- Reyniers, T.; Deliens, L.; Pasman, H.R.W.; Stichele, R.V.; Sijnave, B.; Houttekier, D.; Cohen, J. Appropriateness and avoidability of terminal hospital admissions: Results of a survey among family physicians. Palliat. Med. 2017, 31, 456–464. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, S.L.; Teno, J.M.; Kiely, D.K.; Shaffer, M.L.; Jones, R.; Prigerson, H.G.; Volicer, L.; Givens, J.L.; Hamel, M.B. The Clinical Course of Advanced Dementia. N. Engl. J. Med. 2009, 361, 1529–1538. [Google Scholar] [CrossRef]
- Gozalo, P.; Teno, J.M.; Mitchell, S.L.; Skinner, J.; Bynum, J.; Tyler, D.; Mor, V. End-of-Life Transitions among Nursing Home Residents with Cognitive Issues. N. Engl. J. Med. 2011, 365, 1212–1221. [Google Scholar] [CrossRef]
- Lopez, R.P.; Mitchell, S.L.; Givens, J.L. Preventing burdensome transitions of nursing home residents with advanced de-mentia: It’s more than advance directives. J. Palliat. Med. 2017, 20, 1205–1209. [Google Scholar] [CrossRef]
- Miller, S.C.; Lima, J.C.; Intrator, O.; Martin, E.; Bull, J.; Hanson, L.C. Palliative Care Consultations in Nursing Homes and Reductions in Acute Care Use and Potentially Burdensome End-of-Life Transitions. J. Am. Geriatr. Soc. 2016, 64, 2280–2287. [Google Scholar] [CrossRef]
- Lage, D.E.; Lee, Y.; Mitchell, S.L.; Temel, J.S.; Berry, S.; El-Jawahri, A. Burdensome end-of-life (EOL) transitions among frail older adults with advanced cancer. J. Clin. Oncol. 2018, 36, 6534. [Google Scholar] [CrossRef]
- Hanna, N.; Quach, B.; Scott, M.; Qureshi, D.; Tanuseputro, P.; Webber, C. Operationalizing Burdensome Transitions Among Adults at the End of Life: A Scoping Review. J. Pain Symptom Manag. 2021, 61, 1261–1277.e10. [Google Scholar] [CrossRef] [PubMed]
- Sleeman, K.E.; Perera, G.; Stewart, R.; Higginson, I.J. Predictors of emergency department attendance by people with dementia in their last year of life: Retrospective cohort study using linked clinical and administrative data. Alzheimer’s Dement. 2018, 14, 20–27. [Google Scholar] [CrossRef] [PubMed]
- Organization for Economic Co-operation and Development. Health at a Glance 2021; Organization for Economic Co-operation and Development: Paris, France, 2021; p. 274. Available online: https://www.oecd-ilibrary.org/social-issues-migration-health/health-at-a-glance-2021_ae3016b9-en (accessed on 12 November 2022).
- Instituto Nacional de Estatística. Estatísticas de Saúde—2019; Instituto Nacional de Estatística: Lisbon, Portugal, 2021; pp. 1–74. Available online: https://www.ine.pt/xportal/xmain?xpid=INE&xpgid=ine_publicacoes&PUBLICACOESpub_boui=257483090&PUBLICACOESmodo=2 (accessed on 13 November 2022).
- Sarmento, V.; Higginson, I.J.; Ferreira, P.; Gomes, B. Past trends and projections of hospital deaths to inform the integration of palliative care in one of the most ageing countries in the world. Palliat. Med. 2016, 30, 363–373. [Google Scholar] [CrossRef]
- Gomes, B.; Pinheiro, M.J.; Lopes, S.; de Brito, M.; Sarmento, V.P.; Ferreira, P.L.; Barros, H. Risk factors for hospital death in conditions needing palliative care: Nationwide population-based death certificate study. Palliat. Med. 2018, 32, 891–901. [Google Scholar] [CrossRef]
- Ministério da Saúde. Monitorização da Rede Nacional de Cuidados Continuados Integrados (RNCCI); Ministério da Saúde: Lisbon, Portugal, 2019.
- Zheng, N.T.; Mukamel, D.B.; Friedman, B.; Caprio, T.V.; Temkin-Greener, H. The Effect of Hospice on Hospitalizations of Nursing Home Residents. J. Am. Med. Dir. Assoc. 2015, 16, 155–159. [Google Scholar] [CrossRef][Green Version]
- Mukamel, D.B.; Caprio, T.; Ahn, R.; Zheng, N.; Norton, S.; Quill, T.; Temkin-Greener, H. End-of-Life Quality-of-Care Measures for Nursing Homes: Place of Death and Hospice. J. Palliat. Med. 2012, 15, 438–446. [Google Scholar] [CrossRef]
- Li, Q.; Zheng, N.T.; Temkin-Greener, H. Quality of End-of-Life Care of Long-Term Nursing Home Residents with and without Dementia. J. Am. Geriatr. Soc. 2013, 61, 1066–1073. [Google Scholar] [CrossRef]
- Cai, S.; Miller, S.C.; Mukamel, D.B. Racial Differences in Hospitalizations of Dying Medicare-Medicaid Dually Eligible Nursing Home Residents. J. Am. Geriatr. Soc. 2016, 64, 1798–1805. [Google Scholar] [CrossRef]
- Oken, M.; Creech, R.; Tormey, D.; Horton, J.; Davis, T.; McFadden, E.; Carbone, P. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am. J. Clin. Oncol. 1982, 5, 649–656. Available online: https://journals.lww.com/amjclinicaloncology/Abstract/1982/12000/Toxicity_and_response_criteria_of_the_Eastern.14.aspx (accessed on 24 May 2022). [CrossRef]
- Krishnan, P.; Thompson, G.; McClement, S. Predicting hospital transfers among nursing home residents in the last months of life. Int. J. Palliat. Nurs. 2017, 23, 535–542. [Google Scholar] [CrossRef]
- Takezako, Y.; Tamiya, N.; Kajii, E. The nursing home versus the hospital as the place of dying for nursing home residents in Japan. Health Policy 2007, 81, 280–288. [Google Scholar] [CrossRef]
- Menec, V.H.; Nowicki, S.; Blandford, A.; Veselyuk, D. Hospitalizations at the End of Life Among Long-Term Care Residents. J. Gerontol. A Biol. Sci. Med. Sci. 2009, 64, 395–402. [Google Scholar] [CrossRef] [PubMed]
- Unroe, K.T.; Carnahan, J.L.; Hickman, S.E.; Sachs, G.A.; Hass, Z.; Arling, G. The Complexity of Determining Whether a Nursing Home Transfer Is Avoidable at Time of Transfer. J. Am. Geriatr. Soc. 2018, 66, 895–901. [Google Scholar] [CrossRef]
- Abraham, S.; Menec, V. Transitions between Care Settings at the End of Life among Older Homecare Recipients: A Population-Based Study. Gerontol. Geriatr. Med. 2016, 2. [Google Scholar] [CrossRef]
- O’Neill, B.; Parkinson, L.; Dwyer, T.; Reid-Searl, K. Nursing home nurses’ perceptions of emergency transfers from nursing homes to hospital: A review of qualitative studies using systematic methods. Geriatr. Nurs. 2015, 36, 423–430. [Google Scholar] [CrossRef] [PubMed]
- Ersek, M.; Carpenter, J. Geriatric Palliative Care in Long-Term Care Settings with a Focus on Nursing Homes. J. Palliat. Med. 2013, 16, 1180–1187. [Google Scholar] [CrossRef] [PubMed]
- Carlson, M.D.A.; Lim, B.; Meier, D.E. Strategies and Innovative Models for Delivering Palliative Care in Nursing Homes. J. Am. Med. Dir. Assoc. 2011, 12, 91–98. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Morkisch, N.; Upegui-Arango, L.D.; Cardona, M.I.; van den Heuvel, D.; Rimmele, M.; Sieber, C.C.; Freiberger, E. Components of the transitional care model (TCM) to reduce readmission in geriatric patients: A systematic review. BMC Geriatr. 2020, 20, 1–18. [Google Scholar] [CrossRef]
- Talari, K.; Goyal, M. Retrospective Studies—Utility and Caveats. J. R. Coll. Physicians Edinb. 2020, 50, 398–402. [Google Scholar] [CrossRef]
- Trahan, L.M.; Spiers, J.A.; Cummings, G.G. Decisions to Transfer Nursing Home Residents to Emergency Departments: A Scoping Review of Contributing Factors and Staff Perspectives. J. Am. Med. Dir. Assoc. 2016, 17, 994–1005. [Google Scholar] [CrossRef] [PubMed]
| Variable | Value | |
|---|---|---|
| Residents, N | 176 | |
| Socio-demographic characteristics | ||
| Gender, N (%) | Male | 53 (30.1) |
| Female | 123 (69.9) | |
| Age at death; years, mean ± SD | 85.6 ± 8.6 | |
| Length of stay; months, mean ± SD | 52.6 ± 46.0 | |
| Civil status, N (%) | Single Married Divorced Widowed | 19 (10.8) 46 (26.1) 14 (8.0) 96 (54.5) |
| Family, N (%) | No family | 32 (18.5) |
| 1st degree | 119 (68.8) | |
| 2nd degree | 22 (12.5) | |
| Schooling, years, mean ± SD | 3.5 ± 2.6 | |
| Annual income, Euro, mean ± SD | 7023.9 ± 4178.0 | |
| Clinical Characteristics | ||
| Performance Status, N (%) | 2 | 7 (4.0) |
| 3 | 46 (26.1) | |
| 4 | 123 (69.9) | |
| Number of chronic diseases, N mean ± SD | 3.5±1.5 | |
| Chronic diseases, N (%) | Dementia | 153 (86.9) |
| Arterial Hypertension | 121 (68.8) | |
| Heart Disease | 76 (43.2) | |
| Diabetes mellitus | 56 (31.8) | |
| Stroke | 41 (23.3) | |
| Chronic Renal Disease | 32 (18.2) | |
| Lung Disease | 24 (13.6) | |
| Cancer | 24 (13.6) | |
| Cause of death, N (%) | Infection Neurological Cardiac Cancer Other | 80 (45.5) 29 (16.5) 21 (11.9) 15 (8.5) 31 (17.6) |
| Variable | Value |
|---|---|
| Referrals to Acute Care in the Last Year of Life, N | 288 |
| Referrals to Acute Care in the last year per resident, N (%) | |
| 0 1 ≥2 | 31 (17.6) 66 (37.5) 79 (44.8) |
| Number of nights at hospital per episode, N (%) | |
| 0–1 2–10 >10 | 148 (51.4) 104 (36.1) 36 (12.5) |
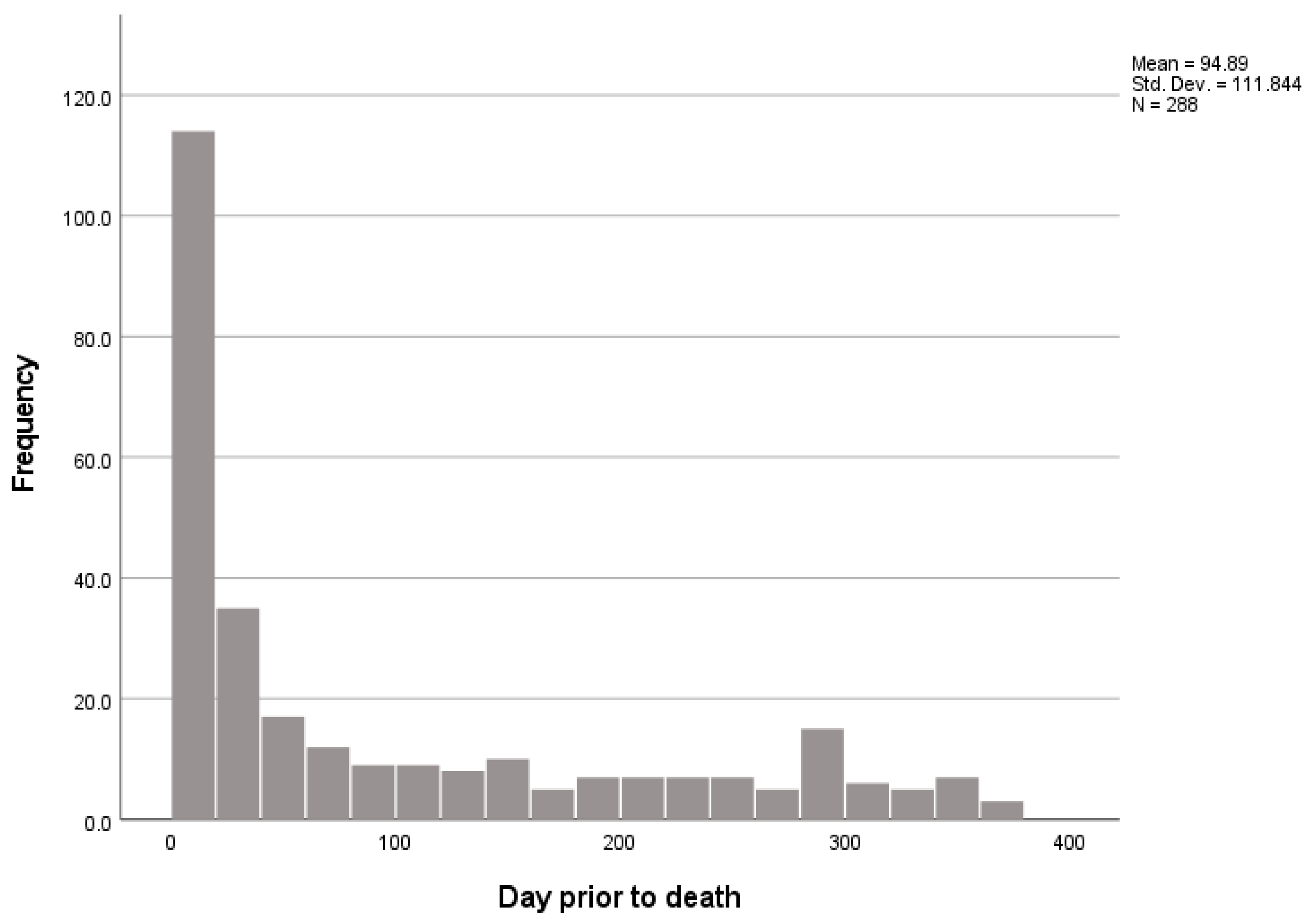
| Days prior to death | |
| At day of death 1–3 days 4–30 days 31–90 days >90 days | 26 (8.2) 38 (11.9) 69 (21.6) 51 (16.0) 104 (32.6) |
| Reason for referral, N (%) | |
| Dyspnea and other respiratory symptoms Focal neurological symptoms Falls Bleeding (all causes) Altered consciousness Other | 111 (39.2) 45 (15.9) 30 (10.6) 24 (8.5) 19 (6.7) 54 (19.1) |
| Discharge diagnosis, N (%) | |
| Infection Neurological Trauma Cardiac Cancer Other | 124 (43.1) 40 (13.9) 29 (10.1) 21 (7.3) 19 (6.6) 55 (19.1) |
| Care integration quality indicators | |
| Referral information Discharge information Health hazards | 88% 95% 24 (8.3%) |
| Death at Hospital | Burdensome Transition Last 3 Days | Burdensome Transition Last 90 Days | |
|---|---|---|---|
| Residents, N (%) | 92 (52.3) | 59 (33.5) | 85 (48.3) |
| Socio-demographic Variables | |||
| Gender Male (ref. Female) | 0.75 | 0.91 | 0.75 |
| Age at death >85 years (ref. ≤85) | 0.45 (0.24–0.84) | 0.51 (0.27–0.97) | 0.36 (0.18–0.65) |
| Length of stay | 1.00 | 0.83 | 1.00 |
| Civil status Single Married Divorced Widowed | ref 1.07 0.66 1.00 | ref 1.53 0.59 0.97 | ref 3.08 2.89 1.80 |
| Family No family 1st degree 2nd degree | ref 0.72 0.68 | ref 0.63 0.43 | ref 0.74 0.47 |
| Schooling | 1.02 | 1.06 | 1.09 |
| Annual income | 1.00 | 1.00 | 1.00 |
| Clinical Variables | |||
| Performance Status 2 3 4 | Ref 0.34 0.14 | ||
| Number of chronic diseases | 1.15 | 0.77 | 1.04 |
| Chronic diseases Dementia Arterial Hypertension Heart Disease Diabetes mellitus Stroke Chronic Renal Disease Lung Disease Cancer | 0.82 0.97 1.49 1.48 1.22 1.67 2.00 0.61 | 1.50 1.05 0.86 1.15 1.37 1.24 1.83 1.50 | 1.54 0.86 1.03 0.90 1.03 1.27 4.95 (1.76–13.95) 0.60 |
| Cause of death, N (%) Infection Neurological disease Cardiac disease Cancer Lung disease Other | 2.36 (1.28–4.34) 0.42 (0.18–0.96) 0.18 (0.06–0.56) 0.58 2.36 5.26 (1.47–18.88) | ||
| Facility Characteristics | |||
| N residents | 1.02 (1.01–1.04) | 1.02 (1.01–1.04) | 1.02 (1.00–1.03) |
| Physician/resident ratio | 5.16 (1.74–15.30) | 6.56 (1.86–23.12) | 1.26 |
| Nurse/resident ratio | 3.61 (1.86–6.99) | 2.09 (1.05–4.16) | 3.54 (1.83–6.88) |
| Caregiver/resident ratio | 1.33 (1.12–1.58) | 1.35 (1.11–1.64) | 1.15 |
| LTCF | 0.57 | 0.92 | 0.48 |
| Palliative Care Support | 0.24 (0.11–0.54) | 0.37 (0.15–0.91) | 0.48 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bárrios, H.; Nunes, J.P.; Teixeira, J.P.A.; Rego, G. Nursing Home Residents Hospitalization at the End of Life: Experience and Predictors in Portuguese Nursing Homes. Int. J. Environ. Res. Public Health 2023, 20, 947. https://doi.org/10.3390/ijerph20020947
Bárrios H, Nunes JP, Teixeira JPA, Rego G. Nursing Home Residents Hospitalization at the End of Life: Experience and Predictors in Portuguese Nursing Homes. International Journal of Environmental Research and Public Health. 2023; 20(2):947. https://doi.org/10.3390/ijerph20020947
Chicago/Turabian StyleBárrios, Helena, José Pedro Nunes, João Paulo Araújo Teixeira, and Guilhermina Rego. 2023. "Nursing Home Residents Hospitalization at the End of Life: Experience and Predictors in Portuguese Nursing Homes" International Journal of Environmental Research and Public Health 20, no. 2: 947. https://doi.org/10.3390/ijerph20020947
APA StyleBárrios, H., Nunes, J. P., Teixeira, J. P. A., & Rego, G. (2023). Nursing Home Residents Hospitalization at the End of Life: Experience and Predictors in Portuguese Nursing Homes. International Journal of Environmental Research and Public Health, 20(2), 947. https://doi.org/10.3390/ijerph20020947







