Influence of Job Insecurity on Musculoskeletal Disorders: A Mediation Model with Nursing Aides
Abstract
1. Introduction
- Job insecurity and physical workload are relevant variables for the presence and development of MSSs;
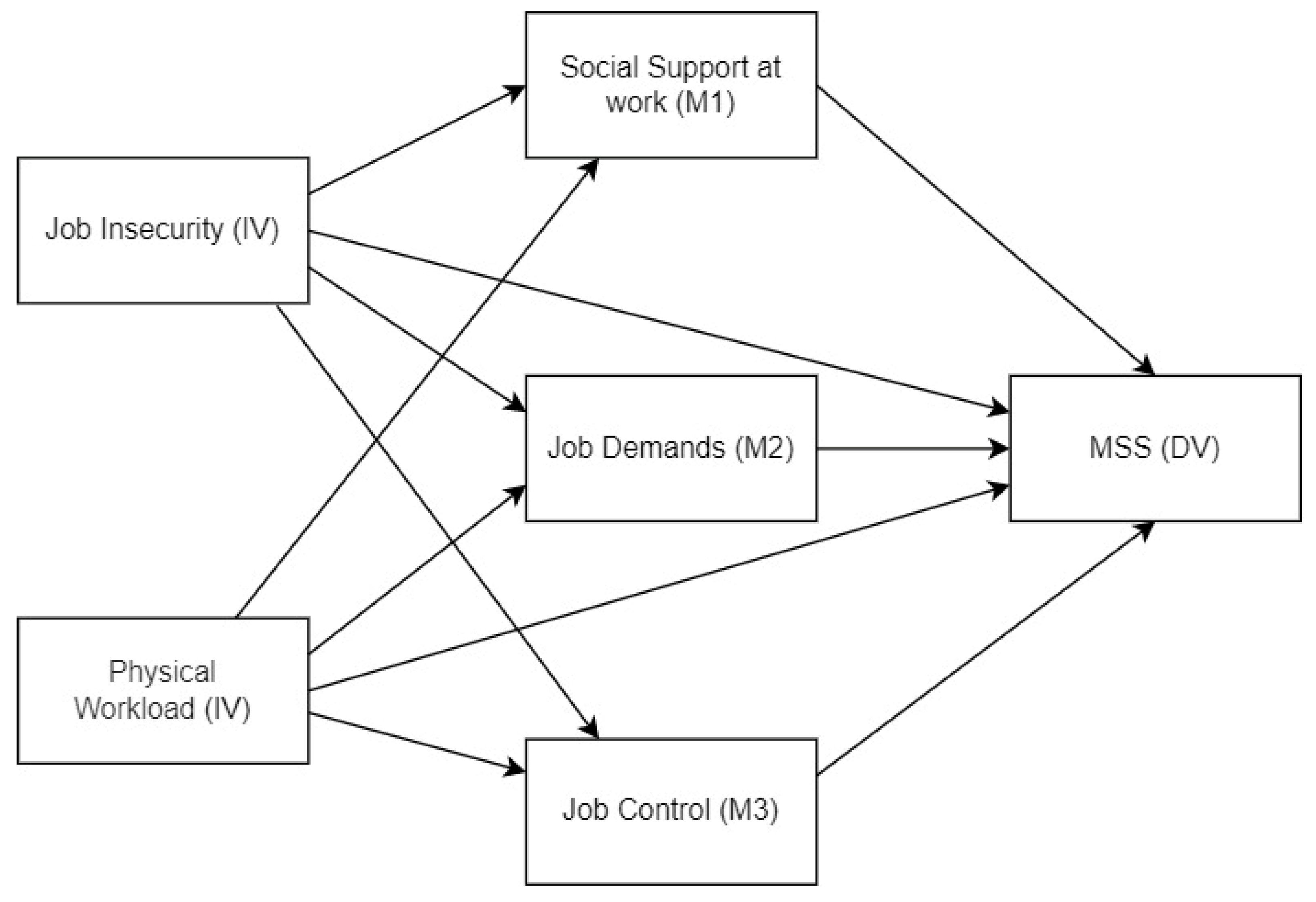
- Psychosocial risks (measured in terms of job demands, social support at work, and job control) have a mediating role in the relationship described in Hypothesis 1. The parallel mediation path model hypothesised is shown in Figure 1.
2. Materials and Methods
2.1. Sample
2.2. Instruments
2.2.1. Nordic Musculoskeletal Questionnaire (NMQ)
2.2.2. Job Insecurity Scale-8 (JIS-8)
2.2.3. Job Content Questionnaire (JCQ)
2.2.4. Physical Workload Questionnaire (PWQ)
2.2.5. Sociodemographic Data
2.3. Procedure
2.4. Data Analysis
3. Results
3.1. Descriptive Analysis and Correlations
3.2. Hypothesis 1
3.3. Hypothesis 2
4. Discussion
Implications for Practice
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Punnett, L.; Wegman, D.H. Work-related musculoskeletal disorders: The epidemiologic evidence and the debate. J. Electromyogr. Kinesiol. 2004, 14, 13–23. [Google Scholar] [CrossRef] [PubMed]
- Worl Health Organization. Musculoskeletal Health. Available online: https://www.who.int/news-room/fact-sheets/detail/musculoskeletal-conditions (accessed on 16 December 2022).
- Tavakkol, R.; Kavi, E.; Hassanipour, S.; Rabiei, H.; Malakoutikhah, M. The global prevalence of musculoskeletal disorders among operating room personnel: A systematic review and meta-analysis. Clin. Epidemiol. Glob. Health 2020, 8, 1053–1061. [Google Scholar] [CrossRef]
- Russeng, S.S.; Saleh, L.M.; Wahyulianti, W.N.; Palutturi, S. The Effect of Age and Workload on Work Posture toward Musculoskeletal Disorders Complain on Loading and Unloading Workers. Open Access Maced. J. Med. Sci. 2021, 9, 1115–1121. [Google Scholar] [CrossRef]
- Du, J.; Zhang, L.; Xu, C.; Qiao, J. Relationship Between the Exposure to Occupation-related Psychosocial and Physical Exertion and Upper Body Musculoskeletal Diseases in Hospital Nurses: A Systematic Review and Meta-analysis. Asian Nurs. Res. 2021, 15, 163–173. [Google Scholar] [CrossRef]
- Taibi, Y.; Metzler, Y.A.; Bellingrath, S.; Müller, A. A systematic overview on the risk effects of psychosocial work characteristics on musculoskeletal disorders, absenteeism, and workplace accidents. Appl. Ergon. 2021, 95, 103434. [Google Scholar] [CrossRef]
- Cox, T.; Griffiths, A.; Barlowe, C.; Randall, R.; Thomson, L.; Rial-Gonzalez, E. Organisational Interventions for Work Stress: A risk Management Approach; Institute of Work, Health and Organisations, University of Nottingham, Business School: Nottingham, UK, 2000; p. 3. ISBN 0717618382. [Google Scholar]
- Karasek, R.; Theorell, T. Healthy Work: Stress, Productivity, and the Reconstruction of Working Life; Basic Book: New York, NY, USA, 1990; ISBN 10 0465028969. [Google Scholar]
- Sverke, M.; Hellgren, J.; Näswall, K. No security: A meta-analysis and review of job insecurity and its consequences. J. Occup. Health Psychol. 2002, 7, 242–264. [Google Scholar] [CrossRef]
- Ganster, D.C. The stressful workplace: Mental and physical health and the problem of prevention. In Socioeconomic Conditions, Stress and Mental Disorders: Toward a New Synthesis of Research and Public Policy; Maney, A., Ramos, J., Eds.; Mental Health Statistical Improvement Program, National Institute of Mental Health: Washington, DC, USA, 2002; p. 2004. [Google Scholar]
- De Witte, H.; Vander Elst, T.; De Cuyper, N. Job insecurity, health, and well-being. In Sustainable Working Lives; Springer: Dordrecht, The Netherlands, 2015; pp. 109–128. ISBN 978-94-017-9798-6. [Google Scholar]
- Kim, T.J.; Von Dem Knesebeck, O. Is an insecure job better for health than having no job at all? A systematic review of studies investigating the health-related risks of both job insecurity and unemployment. BMC Public Health 2015, 15, 985. [Google Scholar] [CrossRef]
- Llosa, J.A.; Menéndez-Espina, S.; Agulló-Tomás, E.; Rodríguez-Suárez, J. Job insecurity and mental health: A meta-analytical review of the consequences of precarious work in clinical disorders. An. Psicol. 2018, 34, 211–223. [Google Scholar] [CrossRef]
- Prado-Gascó, V.; Giménez-Espert, M.D.C.; De Witte, H. Job Insecurity in Nursing: A Bibliometric Analysis. Int. J. Environ. Res. Public Health 2021, 18, 663. [Google Scholar] [CrossRef]
- Yang, M.H.; Jhan, C.J.; Hsieh, P.C.; Kao, C.C. A Study on the Correlations between Musculoskeletal Disorders and Work-Related Psychosocial Factors among Nursing Aides in Long-Term Care Facilities. Int. J. Environ. Health Res. 2022, 19, 255. [Google Scholar] [CrossRef]
- Kuorinka, I.; Jonsson, B.; Kilbom, A.; Vinterberg, H.; Biering-Sørensen, F.; Andersson, G.; Jørgensen, K. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl. Ergon. 1987, 18, 233–237. [Google Scholar] [CrossRef] [PubMed]
- Pinheiro, F.A.; Troccoli, B.T.; Carvalho, C.V. Validity of the Nordic Musculoskeletal Questionnaire as morbidity measurement tool. Rev. Saude Publica 2002, 36, 307–312. [Google Scholar] [CrossRef] [PubMed]
- Borg, I.; Elizur, D. Job Insecurity: Correlates, Moderators and Measurement. Int. J. Manpow. 1992, 13, 13–26. [Google Scholar] [CrossRef]
- Llosa, J.A.; Menéndez-Espina, S.; Rodríguez-Suárez, J.; Agulló-Tomás, E.; Boada-Grau, J. Spanish validation of the Job Insecurity Scale JIS-8: Viability of the cognitive and affective model. Psicothema 2017, 29, 577–583. [Google Scholar] [CrossRef] [PubMed]
- Escribà-Agüir, V.; Más Pons, R.; Flores Reus, E. Validation of the Job Content Questionnaire in hospital nursing staff. Gac. Sanit. 2001, 15, 142–149. [Google Scholar] [CrossRef] [PubMed]
- Hollmann, S.; Klimmer, F.; Schmidt, K.H.; Kylian, H. Validation of a questionnaire for assessing physical workload. Scand. J. Work Environ. Health 1999, 25, 105–114. [Google Scholar] [CrossRef]
- Jager, M.; Luttmann, A.; Laurig, W. Lumbar load during one handed bricklaying. Int. J. Ind. Ergon. 1991, 8, 261–277. [Google Scholar] [CrossRef]
- EuroQol Research Foundation. EQ-5D-5L User Guide. 2019. Available online: https://euroqol.org/publications/user-guides (accessed on 16 December 2022).
- Katz, M.H. Multivariable Analysis: A Practical Guide for Clinicians and Public Health Researchers; Cambridge University Press: Cambridge, UK, 2011; ISBN 10 0521141079. [Google Scholar]
- Yu, Y.; Shen, M.; Niu, L.; Liu, Y.; Xiao, S.; Tebes, J.K. The relationship between clinical recovery and personal recovery among people living with schizophrenia: A serial mediation model and the role of disability and quality of life. Schizophr. Res. 2022, 239, 168–175. [Google Scholar] [CrossRef] [PubMed]
- Zeytinoglu, I.U.; Denton, M.; Plenderleith, J.; Chowhan, J. Associations between workers’ health, and non-standard hours and insecurity: The case of home care workers in Ontario, Canada. Int. J. Hum. Resour. Manag. 2015, 26, 2503–2522. [Google Scholar] [CrossRef]
- Ordóñez-Camblor, N.; Paino, M.; Fonseca-Pedrero, E.; Pizarro-Ruiz, J.P. Mediation of the stigma in the influence of negative symptomatology over recovery in psychosis. Int. J. Clin. Health Psichol. 2021, 21, 100220. [Google Scholar] [CrossRef] [PubMed]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach; Guilford Press: New York, NY, USA, 2017; ISBN 9781462549030. [Google Scholar]
- Santos Nobre, J.; da Motta Singer, J. Residual Analysis for Linear Mixed Models. Biom. J. 2007, 49, 863–875. [Google Scholar] [CrossRef]
- Zeytinoglu, I.U.; Denton, M.; Davies, S.; Plenderleith, J.M. Office home care workers’ occupational health: Associations with workplace flexibility and worker insecurity. Healthc. Policy 2009, 4, 108–121. [Google Scholar] [CrossRef] [PubMed]
- Jahoda, M. Employment and Unemployment: A Social-Psychological Analysis; Cambridge University Press: Cambridge, UK, 1982; ISBN 9780521285865. [Google Scholar]
- Westman, M.; Hobfoll, S.E.; Chen, S.; Davidson, O.B.; Laski, S. Organizational stress through the lens of conservation of resources (COR) theory. In Exploring Interpersonal Dynamics (Research in Occupational Stress and Well Being); Perrewe, P.L., Ganster, D.C., Eds.; Emerald Group Publishing Limited: Bingley, UK, 2004; Volume 4, pp. 167–220. ISBN 978-0-76231-153-8. [Google Scholar]
- Ryan, R.M.; Deci, E.L. The darker and brighter sides of human existence: Basic psy chological needs as a unifying concept. Psychol. Inq. 2000, 11, 319–338. [Google Scholar] [CrossRef]
- Warr, P.B. Work, Unemployment, and Mental Health; Oxford University Press: Oxford, UK, 1987; ISBN 10 0198521588. [Google Scholar]
- De Cuyper, N.; De Witte, H. The impact of job insecurity and contract type on attitudes, well-being and behavioural reports: A psychological contract perspective. J. Occup. Organ. Psychol. 2006, 79, 395–409. [Google Scholar] [CrossRef]
- Lipscomb, H.; Kucera, K.; Epling, C.; Dement, J. Upper extremity musculoskeletal symptoms and disorders among a cohort of women employed in poultry processing. Am. J. Ind. Med. 2008, 51, 24–36. [Google Scholar] [CrossRef]
- Hauke, A.; Flintrop, J.; Brun, E.; Rugulies, R. The impact of work-related psychosocial stressors on the onset of musculoskeletal disorders in specific body regions: A review and metaanalysis of 54 longitudinal studies. Work Stress 2011, 25, 243–256. [Google Scholar] [CrossRef]
- Probst, T.M. Countering the negative effects of job insecurity through participative decision making: Lessons from the demand-control model. J. Occup. Health Psychol. 2005, 10, 320–329. [Google Scholar] [CrossRef]
- Szeto, G.P.; Wong, T.K.; Law, R.K.; Lee, E.W.; Lau, T.; So, B.C.; Law, S.W. The impact of a multifaceted ergonomic intervention program on promoting occupational health in community nurses. Appl. Ergon. 2013, 44, 414–422. [Google Scholar] [CrossRef]
- Shoss, M.K.; Jiang, L.; Probst, T.M. Bending without breaking: A two-study examination of employee resilience in the face of job insecurity. J. Occup. Health Psychol. 2018, 23, 112–126. [Google Scholar] [CrossRef]

| SEX (Mean Age) | ||||
|---|---|---|---|---|
| Type of Contract | Female | Male | Total | |
| Permanent | Count | 214 | 10 | 224 |
| % within column | 49.7 % | 38.5 % | 49 % | |
| Temporary | Count | 217 | 16 | 233 |
| % within column | 50.3 % | 61.5 % | 51 % | |
| Total | Count | 431 (49.90) | 26 (49.35) | 457 (49.69) |
| % within column | 100 % | 100 % | 100 % | |
| Mean | Std. Deviation | Minimum | Maximum | ||
|---|---|---|---|---|---|
| Total_NMQ | Female | 13.66 | 7.82 | 0.00 | 36.00 |
| Male | 10.35 | 9.53 | 0.00 | 30.00 | |
| Total | 13.74 | 7.95 | 0.00 | 36.00 | |
| PWQ_Index | Female | 39.56 | 10.36 | 10.15 | 56.17 |
| Male | 37.80 | 12.10 | 18.17 | 56.17 | |
| Total | 39.49 | 39.49 | 10.15 | 56.17 | |
| JIS_TOTAL | Female | 19.18 | 5.73 | 8.00 | 38.00 |
| Male | 20.04 | 7.34 | 8.00 | 36.00 | |
| Total | 19.24 | 5.84 | 8.00 | 38.00 | |
| JCQ_Demand | Female | 18.00 | 3.24 | 6.00 | 24.00 |
| Male | 17.15 | 3.84 | 11.00 | 24.00 | |
| Total | 17.95 | 3.28 | 6.00 | 24.00 | |
| JCQ_Control | Female | 18.60 | 3.42 | 7.00 | 28.00 |
| Male | 18.15 | 3.22 | 10.00 | 24.00 | |
| Total | 18.57 | 3.40 | 7.00 | 28.00 | |
| JCQ_Support | Female | 25.48 | 4.47 | 9.00 | 36.00 |
| Male | 25.00 | 5.25 | 13.00 | 34.00 | |
| Total | 25.47 | 4.52 | 9.00 | 36.00 |
| Variable | Total_NMQ | PWQ_I | JIS_TOTAL | JCQ_Demand | JCQ_Control | JCQ_Support |
|---|---|---|---|---|---|---|
| 1. Total_NMQ | — | |||||
| 2. PWQ_Index | 0.214 *** | — | ||||
| 3. JIS_TOTAL | 0.136 ** | 0.028 | — | |||
| 4. JCQ_Demand | 0.251 *** | 0.284 *** | 0.108 * | — | ||
| 5. JCQ_Control | 0.045 | 0.070 | 0.009 | 0.250 *** | — | |
| 6. JCQ_Support | −0.182 *** | −0.069 | −0.142 ** | −0.074 | 0.258 *** | — |
| Estimate | Std. Error | z-Value | p | ||
|---|---|---|---|---|---|
| JIS_TOTAL → Total_NMQ | 0.179 ** | 0.063 | 2.861 | 0.004 | |
| PWQ_Index → Total_NMQ | 0.171 ** | 0.035 | 4.931 | <0.001 | |
| Estimate | Std. Error | z-Value | p | |
|---|---|---|---|---|
| IV: Job insecurity; DV: MSSs | ||||
| Direct Effect JIS_TOTAL→ Total_NMQ | 0.125 * | 0.062 | 2.032 | 0.042 |
| Total indirect effect | 0.054 ** | 0.019 | 2.854 | 0.004 |
| JIS_TOTAL → JCQ_Support→ Total_NMQ | 0.027 * | 0.013 | 2.148 | 0.032 |
| JIS_TOTAL → JCQ_Demand→ Total_NMQ | 0.027 * | 0.014 | 1.922 | 0.055 |
| IV: Physical workload; DV: MSSs | ||||
| Direct Effect PWQ_Index→ Total_NMQ | 0.123 ** | 0.035 | 3.497 | <0.001 |
| Total indirect effect | 0.049 ** | 0.013 | 3.707 | <0.001 |
| PWQ_Index → JCQ_Support→ Total_NMQ | 0.008 | 0.006 | 1.364 | 0.173 |
| PWQ_Index→ JCQ_Demand→ Total_NMQ | 0.041 ** | 0.012 | 3.464 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mateos-González, L.; Rodríguez-Suárez, J.; Llosa, J.A.; Agulló-Tomás, E.; Herrero, J. Influence of Job Insecurity on Musculoskeletal Disorders: A Mediation Model with Nursing Aides. Int. J. Environ. Res. Public Health 2023, 20, 1586. https://doi.org/10.3390/ijerph20021586
Mateos-González L, Rodríguez-Suárez J, Llosa JA, Agulló-Tomás E, Herrero J. Influence of Job Insecurity on Musculoskeletal Disorders: A Mediation Model with Nursing Aides. International Journal of Environmental Research and Public Health. 2023; 20(2):1586. https://doi.org/10.3390/ijerph20021586
Chicago/Turabian StyleMateos-González, Laura, Julio Rodríguez-Suárez, José Antonio Llosa, Esteban Agulló-Tomás, and Juan Herrero. 2023. "Influence of Job Insecurity on Musculoskeletal Disorders: A Mediation Model with Nursing Aides" International Journal of Environmental Research and Public Health 20, no. 2: 1586. https://doi.org/10.3390/ijerph20021586
APA StyleMateos-González, L., Rodríguez-Suárez, J., Llosa, J. A., Agulló-Tomás, E., & Herrero, J. (2023). Influence of Job Insecurity on Musculoskeletal Disorders: A Mediation Model with Nursing Aides. International Journal of Environmental Research and Public Health, 20(2), 1586. https://doi.org/10.3390/ijerph20021586







