Digital Trends, Digital Literacy, and E-Health Engagement Predictors of Breast and Colorectal Cancer Survivors: A Population-Based Cross-Sectional Survey
Abstract
1. Introduction
2. Methods
2.1. Study Design and Setting
2.2. Study Population
2.3. Participants and Recruitment
2.4. Sampling Procedure and Randomisation
2.5. Survey Design
2.6. Piloting Survey Questionnaire
2.7. Analysis
2.8. Ethical Approvals
3. Results
3.1. Participant Characteristics
3.2. Mobile App Ownership and Apps Use
3.3. Internet Use for Cancer-Related Information and Influential Factors
3.4. Online Cancer Information Acquisition across Cancer Continuum
3.5. Barriers to Accessing Online Cancer-Related Information
3.6. Association between Digital Literacy and the Demographics Breast and Colorectal Cancer Survivors
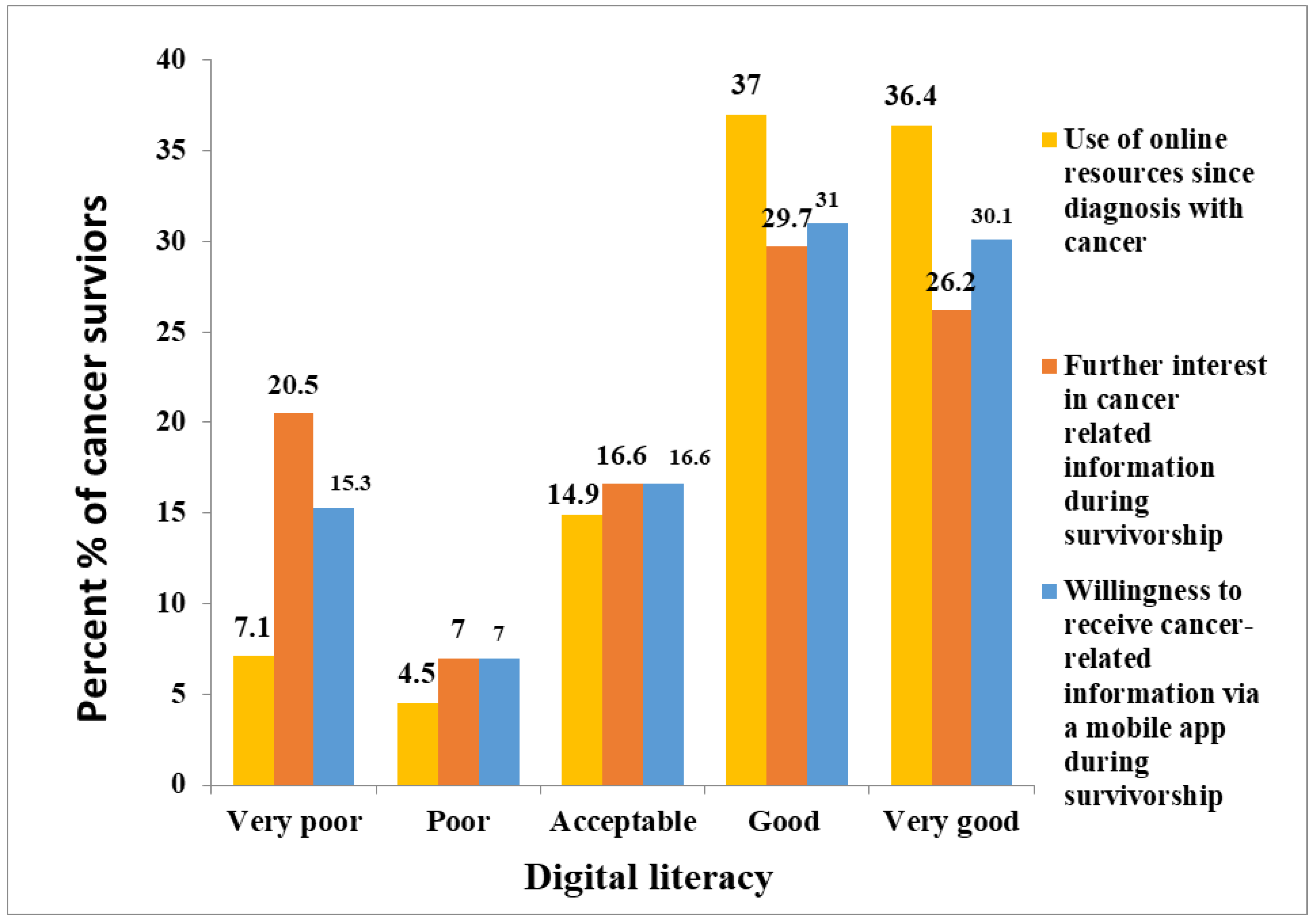
3.7. Digital Trends of Breast and Colorectal Cancer Survivors
3.8. Further Interest in Information
3.9. Predictors of M-Health Engagement and Online Information-Seeking during Survivorship
4. Discussion
5. Conclusions
6. Limitations
7. Practice Implications
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424, Erratum in CA Cancer J. Clin. 2020, 70, 313. [Google Scholar] [CrossRef] [PubMed]
- Jiang, S.; Liu, P.L. Digital divide and Internet health information seeking among cancer survivors: A trend analysis from 2011 to 2017. Psychooncology 2020, 29, 61–67. [Google Scholar] [CrossRef] [PubMed]
- Melhem, S.J.; Nabhani-Gebara, S.; Kayyali, R. Informational needs and predictors of Jordanian breast and colorectal cancer survivors: A national cross-sectional study. Support. Care Cancer 2022, 30, 6827–6837. [Google Scholar] [CrossRef] [PubMed]
- Maddock, C.; Camporesi, S.; Lewis, I.; Ahmad, K.; Sullivan, R. Online information as a decision making aid for cancer patients: Recommendations from the Eurocancercoms project. Eur. J. Cancer. 2012, 48, 1055–1059. [Google Scholar] [CrossRef]
- Rozmovits, L.; Ziebland, S. What do patients with prostate or breast cancer want from an Internet site? A qualitative study of information needs. Patient Educ. Couns. 2004, 53, 57–64. [Google Scholar] [CrossRef]
- Sheikhtaheri, A.; Nahvijou, A.; Mashoof, E. Information Needs of Women with Breast Cancer: A Review of the Literature. Front. Health Inform. 2020, 9, 30. [Google Scholar] [CrossRef]
- Alnaim, L. Evaluation Breast Cancer Information on The Internet in Arabic. J. Cancer Educ. 2018, 34, 810–818. [Google Scholar] [CrossRef]
- Lawrentschuk, N.; Abouassaly, R.; Hewitt, E.; Mulcahy, A.; Bolton, D.M.; Jobling, T. Health information quality on the internet in gynecological oncology: A multilingual evaluation. Eur. J. Gynaecol. Oncol. 2016, 37, 478–483. [Google Scholar]
- Rutten, L.J.F.; Arora, N.K.; Bakos, A.D.; Aziz, N.; Rowland, J. Information needs and sources of information among cancer patients: A systematic review of research (1980–2003). Patient Educ. Couns. 2005, 57, 250–261. [Google Scholar] [CrossRef]
- Quinn, E.M.; Corrigan, M.A.; McHugh, S.M.; Murphy, D.; O’Mullane, J.; Hill, A.D.; Redmond, H.P. Who’s talking about breast cancer? Analysis of daily breast cancer posts on the Internet. Breast 2013, 22, 24–27. [Google Scholar] [CrossRef]
- Foley, N.M.; O’Mahony, M.; Lehane, E.A.; Cil, T.; Corrigan, M.A. A Qualitative Content Analysis of Breast Cancer Narratives Hosted through the Medium of Social Media. Br. J. Med. Med. Res. 2015, 6, 474–483. [Google Scholar] [CrossRef] [PubMed]
- Daabes, A.S.; Kharbat, F.F. A content analysis of Arabic YouTube videos for cancer treatment. Int. J. Health Gov. 2019, 24, 267–273. [Google Scholar] [CrossRef]
- Ayoub, G.; Chalhoub, E.; Sleilaty, G.; Kourie, H.R. YouTube as a source of information on breast cancer in the Arab world. Support. Care Cancer 2021, 29, 8009–8017. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Infodemic Management: An Overview of Infodemic Management during COVID-19, January 2020–May 2021; World Health Organization: Geneve, Switzerland, 2021. [Google Scholar]
- Gage-Bouchard, E.A.; LaValley, S.; Warunek, M.; Beaupin, L.K.; Mollica, M. Is cancer information exchanged on social media scientifically accurate? J. Cancer Educ. 2018, 33, 1328–1332. [Google Scholar] [CrossRef] [PubMed]
- Vargas, C.R.; Chuang, D.J.; Ganor, O.; Lee, B.T. Readability of online patient resources for the operative treatment of breast cancer. Surgery 2014, 156, 311–318. [Google Scholar] [CrossRef] [PubMed]
- Jefford, M.; Tattersall, M.H. Informing and involving cancer patients in their own care. Lancet Oncol. 2002, 3, 629–637. [Google Scholar] [CrossRef]
- Arora, N.K.; Hesse, B.W.; Rimer, B.K.; Viswanath, K.; Clayman, M.L.; Croyle, R.T. Frustrated and Confused: The American Public Rates its Cancer-Related Information-Seeking Experiences. J. Gen. Intern. Med. 2007, 23, 223–228. [Google Scholar] [CrossRef] [PubMed]
- Mitgang, E.A.; Blaya, J.A.; Chopra, M. Digital Health in Response to COVID-19 in Low-and Middle-income Countries: Opportu-nities and Challenges. Glob. Policy 2021, 12, 107–109. [Google Scholar] [CrossRef]
- Harris, B.; Ajisola, M.; Alam, R.M.; Watkins, J.A.; Arvanitis, T.N.; Bakibinga, P.; Chipwaza, B.; Choudhury, N.N.; Kibe, P.; Fayehun, O.; et al. Mobile consulting as an option for delivering healthcare services in low-resource settings in low- and middle-income countries: A mixed-methods study. Digit. Health 2021, 19, 20552076211033425. [Google Scholar] [CrossRef]
- World Health Organization. Global Diffusion of eHealth: Making Universal Health Coverage Achievable: Report of the Third Global Survey on eHealth; World Health Organization: Geneve, Switzerland, 2017. [Google Scholar]
- Brodie, M.; Flournoy, R.E.; Altman, D.E.; Blendon, R.J.; Benson, J.M.; Rosenbaum, M.D. Health Information, The Internet, And the Digital Divide: Despite recent improvements, Americans’ access to the Internet—And to the growing body of health information there—Remains uneven. Health Aff. 2000, 19, 255–265. [Google Scholar] [CrossRef]
- Zhou, J.; Wang, C. Improving cancer survivors’e-health literacy via online health communities (OHCs): A social support per-spective. J. Cancer Surviv. 2020, 14, 244–252. [Google Scholar] [CrossRef] [PubMed]
- Neter, E.; Brainin, E. eHealth Literacy: Extending the Digital Divide to the Realm of Health Information. J. Med. Internet Res. 2012, 14, e19. [Google Scholar] [CrossRef] [PubMed]
- Diviani, N.; van den Putte, B.; Giani, S.; Van Weert, J.C. Low Health Literacy and Evaluation of Online Health Information: A Systematic Review of the Literature. J. Med. Internet Res. 2015, 17, e112. [Google Scholar] [CrossRef] [PubMed]
- Halwas, N.; Griebel, L.; Huebner, J. eHealth literacy, Internet and eHealth service usage: A survey among cancer patients and their relatives. J. Cancer Res. Clin. Oncol. 2017, 143, 2291–2299. [Google Scholar] [CrossRef]
- Shuren, J.; Patel, B.; Gottlieb, S. FDA Regulation of Mobile Medical Apps. JAMA 2018, 320, 337–338. [Google Scholar] [CrossRef]
- Yang, K.; Hu, Y.; Qi, H. Digital Health Literacy: Bibliometric Analysis. J. Med. Internet Res. 2022, 24, e35816. [Google Scholar] [CrossRef]
- Norman, C.D.; Skinner, H.A. eHealth Literacy: Essential Skills for Consumer Health in a Networked World. J. Med. Internet Res. 2006, 8, e9. [Google Scholar] [CrossRef]
- Dadaczynski, K.; Okan, O.; Messer, M.; Leung, A.Y.M.; Rosário, R.; Darlington, E.; Rathmann, K. Digital Health Literacy and Web-Based Information-Seeking Behaviors of University Students in Germany During the COVID-19 Pandemic: Cross-sectional Survey Study. J. Med. Internet Res. 2021, 23, e24097. [Google Scholar] [CrossRef]
- Krejcie, R.V.; Morgan, D.W. Determining Sample Size for Research Activities. Educ. Psychol. Meas. 1970, 30, 607–610. [Google Scholar] [CrossRef]
- Tian, L.; Cao, X.; Feng, X. Evaluation of psychometric properties of needs assessment tools in cancer patients: A systematic liter-ature review. PloS ONE 2019, 14, e0210242. [Google Scholar] [CrossRef]
- Huang, Y.-J.; Lin, G.-H.; Lu, W.-S.; Tam, K.-W.; Chen, C.; Hou, W.-H.; Hsieh, C.-L. Validation of the European Health Literacy Survey Questionnaire in Women with Breast Cancer. Cancer Nurs. 2018, 41, E40–E48. [Google Scholar] [CrossRef] [PubMed]
- Van Der Vaart, R.; Drossaert, C. Development of the digital health literacy instrument: Measuring a broad spectrum of health 1.0 and health 2.0 skills. J. Med. Internet Res. 2017, 19, e6709. [Google Scholar] [CrossRef] [PubMed]
- IC-Health—Improving Digital Health Literacy in Europe. Available online: https://ehma.org/research-projects/past-projects/ic-health-improving-digital-health-literacy-europe/ (accessed on 22 October 2022).
- Mayer, D.K.; Nasso, S.F.; Earp, J.A. Defining cancer survivors, their needs, and perspectives on survivorship health care in the USA. Lancet Oncol. 2017, 18, e11–e18. [Google Scholar] [CrossRef] [PubMed]
- Hassan, Z.A.; Schattner, P.; Mazza, D. Doing a pilot study: Why is it essential? Malays. Fam. Physician Off. J. Acad. Fam. Physicians Malays. 2006, 1, 70. [Google Scholar]
- Williams, A. How to Write and analyse a questionnaire. J. Orthod. 2003, 30, 245–252. [Google Scholar] [CrossRef] [PubMed]
- Tarrant, C.; Angell, E.; Baker, R.; Boulton, M.; Freeman, G.; Wilkie, P.; Jackson, P.; Wobi, F.; Ketley, D. Responsiveness of primary care services: Development of a patient-report measure—Qualitative study and initial quantitative pilot testing. Health Serv. Deliv. Res. 2014, 2, 1–368. [Google Scholar] [CrossRef] [PubMed]
- CPQOL Cerebral CPQOL Palsy Quality of—AusAC-PDM. Available online: https://www.ausacpdm.org.au/wp-content/uploads/2019/01/CPQOL-Translation-manual.pdf (accessed on 22 October 2022).
- Kim, H.; Xie, B. Health literacy and internet- and mobile app-based health services: A systematic review of the literature. Proc. Assoc. Inf. Sci. Technol. 2015, 52, 1–4. [Google Scholar] [CrossRef]
- Chan, C.V.; Kaufman, D.R. A Framework for Characterizing eHealth Literacy Demands and Barriers. J. Med. Internet Res. 2011, 13, e94. [Google Scholar] [CrossRef] [PubMed]
- Bender, J.L.; Yue, R.Y.K.; Eccleston, C.; Deacken, L.; Jadad, A.R. A Lot of Action, But Not in the Right Direction: Systematic Review and Content Analysis of Smartphone Applications for the Prevention, Detection, and Management of Cancer. J. Med. Internet Res. 2013, 15, e287. [Google Scholar] [CrossRef]
- Division of Cancer Control and Population Sciences (DCCPS), National Cancer Institute. Available online: https://cancercontrol.cancer.gov/ocs/statistics#definitions (accessed on 22 October 2022).
- Nguyen, S.; Ingledew, P. Abstract P5-12-02: Tangled in the Breast Cancer Web: An Evaluation of the Usage of Web-based Information Resources by Breast Cancer Patients. J. Cancer Educ. 2012, 28, 662–668. [Google Scholar] [CrossRef]
- Hasannejadasl, H.; Roumen, C.; Smit, Y.; Dekker, A.; Fijten, R. Health Literacy and eHealth: Challenges and Strategies. JCO Clin. Cancer Inform. 2022, 6, e2200005. [Google Scholar] [CrossRef]
- Neves, A.L.; Smalley, K.R.; Freise, L.; Harrison, P.; Darzi, A.; Mayer, E.K. Determinants of Use of the Care Information Exchange Portal: Cross-sectional Study. J. Med. Internet Res. 2021, 23, e23481. [Google Scholar] [CrossRef] [PubMed]
- Lepore, S.J.; Rincon, M.A.; Buzaglo, J.S.; Golant, M.; Lieberman, M.A.; Bass, S.B.; Chambers, S. Digital literacy linked to engagement and psychological benefits among breast cancer survivors in Internet-based peer support groups. Eur. J. Cancer Care 2019, 28, e13134. [Google Scholar] [CrossRef] [PubMed]
- Latulippe, K.; Hamel, C.; Giroux, D. Social Health Inequalities and eHealth: A Literature Review With Qualitative Synthesis of Theoretical and Empirical Studies. J. Med. Internet Res. 2017, 19, e136. [Google Scholar] [CrossRef] [PubMed]
- Hoogland, A.I.; Mansfield, J.; Lafranchise, E.A.; Bulls, H.W.; Johnstone, P.A.; Jim, H.S. eHealth literacy in older adults with cancer. J. Geriatr. Oncol. 2020, 11, 1020–1022. [Google Scholar] [CrossRef]
- Johnson, S.B.; Parsons, M.; Dorff, T.; Moran, M.S.; Ward, J.H.; A Cohen, S.; Akerley, W.; Bauman, J.; Hubbard, J.; E Spratt, D.; et al. Cancer Misinformation and Harmful Information on Facebook and Other Social Media: A Brief Report. Gynecol. Oncol. 2021, 114, 1036–1039. [Google Scholar] [CrossRef] [PubMed]
- Arif, N.; Ghezzi, P. Quality of online information on breast cancer treatment options. Breast 2018, 37, 6–12. [Google Scholar] [CrossRef]
- Nghiem, A.Z.; Mahmoud, Y.; Som, R. Evaluating the quality of internet information for breast cancer. Breast 2016, 25, 34–37. [Google Scholar] [CrossRef]
- Chua, G.P.; Ng, Q.S.; Tan, H.K.; Ong, W.S. Cancer Survivors: What Are Their Information Seeking Behaviours? J. Cancer Educ. 2020, 36, 1237–1247. [Google Scholar] [CrossRef]
- Shea–Budgell, M.; Kostaras, X.; Myhill, K.; Hagen, N. Information Needs and Sources of Information for Patients during Cancer Follow-Up. Curr. Oncol. 2014, 21, 165–173. [Google Scholar] [CrossRef]
- López-Gómez, M.; Ortega, C.; Suárez, I.; Serralta, G.; Madero, R.; Gómez-Raposo, C.; Sereno, M.; Casado, E.; Espinosa, E.; Lobo, F.; et al. Internet use by cancer patients: Should oncologists ‘prescribe’ accurate web sites in combination with chemotherapy? A survey in a Spanish cohort. Ann. Oncol. 2011, 23, 1579–1585. [Google Scholar] [CrossRef]
- Basch, E.M.; Thaler, H.T.; Shi, W.; Yakren, S.; Schrag, D. Use of information resources by patients with cancer and their companions. Cancer 2004, 100, 2476–2483. [Google Scholar] [CrossRef] [PubMed]
- Obeidat, R.; I Khrais, H. Jordanian physicians’ attitudes toward disclosure of cancer information and patient participation in treatment decision-making. Asia-Pac. J. Oncol. Nurs. 2016, 3, 281–288. [Google Scholar] [CrossRef]
- Cooley, M.E.; Nayak, M.M.; Abrahm, J.L.; Braun, I.M.; Rabin, M.S.; Brzozowski, J.; Lathan, C.; Berry, D.L. Patient and caregiver perspectives on decision support for symptom and quality of life management during cancer treatment: Implications for eHealth. Psycho-Oncol. 2017, 26, 1105–1112. [Google Scholar] [CrossRef] [PubMed]
- Kemp, E.; Trigg, J.; Beatty, L.; Christensen, C.; Dhillon, H.M.; Maeder, A.; Williams, P.A.H.; Koczwara, B. Health literacy, digital health literacy and the implementation of digital health technologies in cancer care: The need for a strategic approach. Health Promot. J. Aust. 2020, 32, 104–114. [Google Scholar] [CrossRef] [PubMed]
- Domecq, J.P.; Prutsky, G.; Elraiyah, T.; Wang, Z.; Nabhan, M.; Shippee, N.; Brito, J.P.; Boehmer, K.; Hasan, R.; Firwana, B.; et al. Patient engagement in research: A systematic review. BMC Health Serv. Res. 2014, 14, 89. [Google Scholar] [CrossRef]
- Leader, A.E.; Capparella, L.M.; Waldman, L.B.; Cammy, R.B.; Petok, A.R.; Dean, R.; Shimada, A.; Yocavitch, L.; Rising, K.L.; Garber, G.D.; et al. Digital literacy at an urban cancer center: Implications for technology use and vulnerable patients. JCO Clin. Cancer Inform. 2021, 5, 872–880. [Google Scholar] [CrossRef]
- Ii, A.C.O.; Seitz, A.J.; Peterson, S.K. Digital Health Navigation: An Enabling Infrastructure for Optimizing and Integrating Virtual Care Into Oncology Practice. JCO Clin. Cancer Inform. 2021, 5, 1151–1154. [Google Scholar] [CrossRef]
- Huhta, A.-M.; Hirvonen, N.; Huotari, M.-L. Health Literacy in Web-Based Health Information Environments: Systematic Review of Concepts, Definitions, and Operationalization for Measurement. J. Med. Internet Res. 2018, 20, e10273. [Google Scholar] [CrossRef]
| Cancer Type | Male (s) | Female (s) | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|
| N | Eligible Sample (n) | Response Sample (n) | N | Eligible Sample (n) | Response Sample (n) | N | Eligible Sample (n) | Response Sample (n) | |
 Breast Breast | 11 | 11 | 4 | 1142 | 292 | 251 | 1153 | 303 | 225 |
 Colon Colon | 185 | 47 | 38 | 130 | 33 | 21 | 315 | 80 | 59 |
 Rectum Rectum | 52 | 14 | 12 | 47 | 12 | 9 | 99 | 26 | 21 |
| Total | 248 | 72 | 54 | 1319 | 337 | 281 | 1567 ** | 409 * | 335 ◊ |
| Socio-Demographic Characteristics (n = 335) | Online Resources Use for Cancer Related Information since Diagnosis | p Value | |
|---|---|---|---|
| Yes | No | ||
| n (%) | n (%) | p | |
| Gender | 0.05 | ||
| Male | 18 (33.3) | 36 (66.7) | |
| Female | 136 (48.4) | 145(51.6) | |
| Age | 0.00 | ||
| less than 40 | 19 (86.4) | 3 (13.6) | |
| 40–49 | 45 (62.5) | 27 (37.5) | |
| 50–59 | 58 (50.0) | 58 (50.0) | |
| 60–69 | 23 (33.8) | 45 (66.2) | |
| 70+ | 9 (15.8) | 48 (84.2) | |
| Regions of residence | 0.10 | ||
| Middle region | 127 (48.1) | 137 (51.9) | |
| North region | 20 (33.9) | 39 (66.1) | |
| South region | 7 (58.3) | 5 (41.7) | |
| Employment (paid or unpaid) | 0.00 | ||
| Housewife | 43 (75.4) | 14 (24.6) | |
| Retired | 83 (40.7) | 121 (59.3) | |
| Student | 0 (0.0) | 0 (0.0) | |
| Employed (paid or unpaid) | 28 (41.2) | 40 (58.8) | |
| Employed (paid or unpaid) | 0 (0.0) | 6 (100.0) | |
| Monthly income in Jordanian Dinars (US $) | 0.00 | ||
| less than 100 JOD (< 140$) | 2 (12.5) | 14 (87.5) | |
| 100–199 JOD (140-280$) | 9 (37.5) | 15 (62.5) | |
| 200–299 JOD (282-422$) | 15 (35.7) | 27 (64.3) | |
| 300–499 JOD (423-704$) | 23 (36.5) | 40 (63.5) | |
| 500 JOD or more (≥705$) | 44 (71.0) | 18 (29.0) | |
| I don’t know | 35 (45.5) | 42 (54.5) | |
| Refuse to answer | 26 (51.0) | 25 (49.0) | |
| Education highest level of Education | 0.00 | ||
| Illiterate | 0 (0.0) | 26 (100.0) | |
| Elementary school | 11 (14.1) | 67 (85.9) | |
| High school | 47 (51.6) | 44 (48.4) | |
| Diploma | 38 (56.7) | 29 (43.3) | |
| Bachelor’s degree | 49 (77.8) | 14 (22.2) | |
| Masters/PhD | 9 (90.0) | 1 (10.0) | |
| I don’t know | 0 | 0 | |
| Refuse to answer | 0 | 0 | |
| Type of cancer | 0.02 | ||
| Breast | 128 (50.2) | 127 (49.8) | |
| Colon | 20 (33.9) | 39 (66.1) | |
| Rectum | 6 (28.6) | 15 (71.4) | |
| Chronic Disease (diabetes, hypertension, cardiovascular disease, Others) | 0.00 | ||
| Yes | 71 (29.8) | 168 (70.2) | |
| No | 98 (30.0) | 77 (70.0) | |
| Action Taken to Verify Cancer Health Information | n (%) |
|---|---|
| Asking doctor or a health professional | 97 (63.0) |
| Verify results on other websites | 39 (25.3) |
| Check other information sources | 10 (6.5) |
| Ask the opinion of others | 15 (9.7) |
| Do nothing | 28 (18.2) |
| Variables | Digital Health Literacy | |||||
|---|---|---|---|---|---|---|
| Very Poor | Poor | Acceptable | Good | Very Good | p-Value | |
| Sex | 0.884 | |||||
| Male | 19 (35.20) | 4 (7.40) | 7 (13.00) | 11 (20.40) | 13 (24.10) | |
| Female | 91 (32.40) | 18 (6.40) | 39 (13.90) | 75 (26.70) | 58 (20.60) | |
| Age group(years) | 0.000 | |||||
| ≤40 | 1 (9 %) | 0 (0.0) | 3 (6.5) | 11 (12.8) | 7 (9.9) | |
| 40–49 | 13 (11.8) | 6 (27.3) | 7 (15.2) | 21 (24.4) | 25 (35.2) | |
| 50–59 | 23 (20.9) | 12 (54.5) | 21 (45.7) | 31 (36.0) | 29 (40.8) | |
| 60–69 | 30 (27.3) | 2 (9.1) | 12 (26.1) | 16 (18.6) | 8 (11.3) | |
| ≥70 | 43 (39.1) | 2 (9.1) | 3 (6.5) | 7 (8.1) | 2 (2.8) | |
| Cancer type | 0.546 | |||||
| Breast | 78 (30.60) | 18 (7.1) | 37 (14.5) | 67 (26.3) | 55 (21.6) | |
| Colon | 25 (42.40) | 4 (6.8) | 5 (8.5) | 12 (20.3) | 13 (22.0) | |
| Rectum | 7 (33.30) | 0 (0.0) | 4 (19.0) | 7 (33.3) | 3 (14.3) | |
| Residence | 0.58 | |||||
| Middle region | 85 (32.2) | 15 (5.7) | 38 (14.4) | 67 (25.4) | 59 (22.3) | |
| North region | 23 (39.0) | 6 (10.2) | 7 (11.9) | 15 (25.4) | 8 (13.6) | |
| South region | 2 (16.7) | 1 (8.3) | 1 (8.3) | 4 (33.3) | 4 (33.3) | |
| Marital status | 0.032 | |||||
| Single | 4 (21.1) | 1 (5.3) | 2 (10.5) | 5 (26.3) | 7 (26.8) | |
| Married | 83 (30.2) | 17 (6.2) | 43 (15.6) | 71 (25.8) | 61 (22.2) | |
| Divorced | 2 (66.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (33.3) | |
| separated | 3 (33.3) | 1 (11.1) | 0 (0.0) | 5 (55.6) | 0 (0.0) | |
| Widowed | 18 (62.1) | 3 (10.3) | 1 (3.4) | 5 (17.2) | 2 (6.9) | |
| Employment status | 0.000 | |||||
| Employed (paid or unpaid | 4 (7.0) | 2 (3.5) | 10 (17.5) | 17 (29.8) | 24 (42.1) | |
| Unemployed (capable or in capable) | 5 (83.3) | 1 (16.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Housewife | 79 (38.7) | 16 (7.8) | 26 (12.7) | 53 (26.0) | 30 (14.7) | |
| Student | 0 (0.0)) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Retired | 22 (32.4) | 3 (4.4) | 10 (14.7) | 16 (23.5) | 17 (25.0) | |
| Refuse to answer | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Monthly income in Jordanian Dinars (US$) | 0.000 | |||||
| Less than 100 (140) | 11 (68.8) | 1(6.3) | 0 (0.0) | 3 (18.8) | 1 (6.3) | |
| 100–199 (140–280) | 12 (50.0) | 2 (8.3) | 4 (16.7) | 3 (12.5) | 3 (12.5) | |
| 200–299 (281–421) | 17 (40.5) | 4 (9.5) | 5 (11.9) | 6 (14.3) | 10 (23.8) | |
| 300–499 (422–703) | 20 (31.7) | 1 (1.6) | 16 (25.4) | 17 (27.0) | 9 (14.3) | |
| 500 (704) or more | 9 (14.5) | 2 (3.2) | 8 (12.9) | 17 (27.4) | 26 (41.9) | |
| Don’t know | 24 (31.2) | 6 (7.8) | 9 (11.7) | 25 (32.6) | 13 (16.9) | |
| Refuse to answer | 17 (33.3) | 6 (11.8) | 4 (7.8) | 15 (29.4) | 9 (17.6) | |
| Education status | 0.000 | |||||
| Illiterate | 24 (92.3) | 1 (3.8) | 1 (3.8) | 0 (0.0) | 0 (0.0) | |
| Elementary school | 44 (58.4) | 9 (11.5) | 11 (14.1) | 7 (9.0) | 7 (9.0) | |
| High school (Tawjihi) | 21 (23.1) | 8 (8.8) | 18 (19.8) | 32 (25.2) | 12 (13.2) | |
| Diploma | 13 (19.4) | 2 (3.0) | 10 (14.9) | 24 (35.8) | 18 (26.9) | |
| University /bachelor’s degree | 7 (11.1) | 2 (3.2) | 6 (9.5) | 20 (31.7) | 28 (44.4) | |
| Masters/PhD | 1 (10.0) | 0 (0.0) | 0 (0.0) | 3 (30.0) | 6 (60.0) | |
| Variables | Use of Online Resources since Diagnosis with Cancer n = (%) | p | Interest to Receive Cancer-Related Information during Survivorship n = (%) | p | Willingness to Use a Mobile a Dedicated App to Receive Cancer-Related Information during Survivorship n = (%) | p-Value | |||
|---|---|---|---|---|---|---|---|---|---|
| Digital health literacy | Yes (n = 154) % | No (n = 181) % | 0.00 | Yes (n = 229) % | No (n = 106) % | 0.00 | Yes (n = 229) % | No (n = 106) % | 0.00 |
| Very poor | 11 (7.1) | 99 (54.7) | 47 (20.5) | 63 (59.4) | 35 (15.3) | 75 (70.8) | |||
| Poor | 7 (4.5) | 15 (8.3) | 16 (7.0) | 6 (5.7) | 16 (7.0) | 6 (5.7) | |||
| Acceptable | 23 (14.9) | 23 (12.7) | 38 (16.6) | 8 (7.5) | 38(16.6) | 8 (7.5) | |||
| Good | 57 (37.0) | 29 (16.0) | 68 (29.7) | 18 (17.0) | 71 (31.0) | 15(14.2) | |||
| Very good | 56 (36.4) | 15 (8.3) | 60 (26.2) | 11 (10.4) | 69 (30.1) | 2 (1.9) | |||
| Variable (s) | Interest in Receiving Health Information during Survivorship | COR (95% CI) | AOR (95% CI) | p Value | |||
|---|---|---|---|---|---|---|---|
| YES, n = (229) | No; n = (106) | ||||||
| Gender | |||||||
| Male | 33 (9.9%) | 21 (6.3%) | 1.571 (0.909, 2.716) | 1.295 (0.429, 3.908) | 0.646 | ||
| Female | 196 (58.5%) | 85 (25.4%) | Referent | ||||
| Age (years) | 0.395 | ||||||
| <40 | 18 (5.4%) | 4 (1.2%) | 4.500 (1.523, 13.296) | 0.997 (0.144, 6.882) | 0.997 | ||
| 40-49 | 58 (17.3%) | 14 (4.2%) | 4.143 (2.311, 7.426) | 1.362 (0.409, 4.541) | 0.615 | ||
| 50-59 | 82 (24.5%) | 34 (10.1%) | 2.412 (1.1617, 3.597) | 0.555 (0.189, 1.632) | 0.285 | ||
| 60-69 | 48 (14.3%) | 20 (6.0%) | 2.400 (1.425, 4.043) | 1.303 (0.432, 3.927) | 0.638 | ||
| ≥70 | 23 (6.9%) | 34 (10.1%) | Referent | ||||
| Education | 0.395 | ||||||
| Illiterate | 7 (2.1%) | 19 (5.7%) | 0.368 (0.155, 0.876) | 0.288 (0.33, 2.513) | 0.260 | ||
| Elementary School | 42 (12.5%) | 36 (10.7%) | 1.167 (0.748, 1.821) | 1.212 (0.210, 6.984) | 0.829 | ||
| High School | 69 (20.6%) | 22 (6.6%) | 3.136 (1.941, 5.068) | 1.519 (0.279, 8.280) | 0.629 | ||
| Diploma | 50 (14.9%) | 17 (5.1%) | 2.941 (1.696, 5.099) | 1.697 (0.299, 9.644) | 0.551 | ||
| University Degree | 53 (15.8%) | 10 (3.0%) | 5.300 (2.697, 10.417) | 3.575 (0.583, 21.936) | 0.169 | ||
| Masters/PhD | 8 (2.4%) | 2 (0.6%) | Referent | ||||
| Type of cancer | 0.337 | ||||||
| Breast | 183 (54.6%) | 72 (21.5%) | 2.542 (1.935, 3.338) | 1.608 (0.428, 6.043) | 0.482 | ||
| Colon | 33 (9.9%) | 26 (7.8%) | 1.269 (0.759, 2.122) | 0.723 (0.202, 2.585) | 0.618 | ||
| Rectum | 13 (3.9%) | 8 (2.4%) | Referent | ||||
| Monthly Income | 0.768 | ||||||
| <100 JOD (<140 $) | 9 (4.3%) | 7 (3.4%) | 1.286 (0.479, 3.452) | 1.245 (0.25, 6.208) | 0.790 | ||
| 100-199 JOD (140–279 $) | 14 (6.8%) | 10 (4.8%) | 1.400 (0.622, 3.152) | 0.573 (0.144, 2.272) | 0.428 | ||
| 200-299 JOD (280–419 $) | 26 (12.6%) | 16 (7.7%) | 1.625 (0.872, 3.029) | 0.610 (0.194, 1.919) | 0.398 | ||
| 300-499 JOD (749–500$) | 44 (21.3%) | 19 (9.2%) | 2.316 (1.352, 3.966) | 0.686 (0.232, 2.033) | 0.497 | ||
| ≥500 JOD (750$) | 51 (24.6%) | 11 (5.3%) | Referent | ||||
| Region | 0.228 | ||||||
| North Region | 185 (55.2%) | 79 (23.6%) | 2.342 (1.799, 3.048) | 3.697 (0.821, 16.655) | 0.089 | ||
| Middle Region | 36 (10.7%) | 23 (6.9%) | 1.565 (0.928, 2.641) | 2.990 (0.564, 15.850) | 0.198 | ||
| South Region | 8 (2.4%) | 4 (1.2%) | Referent | ||||
| Digital health literacy | 0.006 * | ||||||
| Very poor | 47 (14.0%) | 63 (18.8%) | 0.746 (0.511, 1.088) | 0.194 (0.060,0.623) | 0.006 * | ||
| Poor | 16 (4.8%) | 6 (1.8%) | 2.667 (1.043, 6.815) | 0.730 (0.127, 4.199) | 0.725 | ||
| Acceptable | 38 (11.3%) | 8 (2.4%) | 4.750 (2.216, 10.181) | 1.362 (0.338, 5.493) | 0.664 | ||
| Good | 68 (20.3%) | 18 (5.4%) | 3.778 (2.247, 6.351) | 0.828 (0.253, 2.709) | 0.755 | ||
| Very good | 60 (17.9%) | 11 (3.3%) | Referent | ||||
| Omnibus Tests of Model Coefficients | |||||||
| Chi-square | df | Sig. | |||||
| Step 1 | Step | 88.031 | 22 | 0.000 | |||
| Block | 88.031 | 22 | 0.000 | ||||
| Model | 88.031 | 22 | 0.000 | ||||
| Model Summary | |||||||
| Step 1 | −2 Log likelihood | Cox & Snell R Square | Nagelkerke R Square | ||||
| 198.932a | 0.346 | 0.462 | |||||
| Variable (s) | Willingness to Use M-Health App/Portal for Self-Management | COR (95% CI) | AOR (95% CI) | p Value | |
|---|---|---|---|---|---|
| YES, n = (229) | NO; n = (106) | ||||
| Gender | |||||
| Male | 35 (10.4%) | 19 (5.7%) | 1.842 (1.054, 3.220) | 1.469 (0.413, 5.233) | 0.553 |
| Female | 194(57.9%) | 87(26.0%) | Referent | ||
| Age | 0.218 | ||||
| <40 | 20 (6.0%) | 2 (0.6%) | 10.00 (2.337, 42.783) | 5.985 (0.460, 77.920) | 0.172 |
| 40–49 | 55 (16.4%) | 17 (5.1%) | 3.235 (1.878, 5.573) | 2.032 (0.566, 7.295) | 0.277 |
| 50–59 | 90 (26.9%) | 26 (7.8%) | 3.462 (2.237,5.355) | 3.386 (1.030, 11.130) | 0.045 |
| 60–69 | 46 (13.7%) | 22 (6.6%) | 2.091 (1.258,3.475) | 3.353 (1.039, 10.824) | 0.043 |
| ≥70 | 18 (5.4%) | 39 (11.6%) | Referent | ||
| Education | 0.783 | ||||
| Illiterate | 5 (1.5%) | 21 (6.3%) | 0.238 (0.090, 0.631) | 0.278 (0.022, 3.476) | 0.321 |
| Elementary School | 39 (11.6%) | 39 (11.6%) | 1.000 (0.642, 1.559) | 0.567 (0.065, 4.943) | 0.607 |
| High School | 71 (21.2%) | 20 (6.0%) | 3.550 (2.161, 5.831) | 0.828 (0.102, 6.715) | 0.859 |
| Diploma | 51 (15.2%) | 16 (4.8%) | 3.187 (1.818, 5.589) | 0.605 (0.72, 5.078) | 0.644 |
| University Degree | 53 (15.8%) | 10 (3.0%) | 5.300 (2.697, 10.417) | 1.113 (0.127, 9.767) | 0.923 |
| Masters/PhD | 10 (3.0%) | 0 (0.0%) | Referent | ||
| Type of cancer | 0.504 | ||||
| Breast | 179 (53.4%) | 76 (22.7%) | 2.355 (1.801, 3.080) | 2.174 (0.517, 9.142) | 0.289 |
| Colon | 37 (11.0%) | 22 (6.6%) | 1.682 (0.992, 2.851) | 2.216 (0.521, 8.679) | 0.293 |
| Rectum | 13 (3.9%) | 8 (2.4%) | Referent | ||
| Monthly Income | 0.874 | ||||
| <100 JOD (<140$) | 9 (4.3%) | 7 (3.4%) | 1.286 (0.479, 3.452) | 2.061 (0.362, 11.718) | 0.415 |
| 100–199 JOD (140–279$) | 14 (6.8%) | 10 (4.8%) | 1.400 (.622, 3.152) | 1.319 (0.273, 6.373) | 0.730 |
| 200–299 JOD (280–419$) | 26 (12.6%) | 16 (7.7%) | 1.625 (0.872, 3.029) | 0.897 (0.251, 3.208) | 0.867 |
| 300–499 JOD (749–500$) | 41 (19.8%) | 22 (10.6%) | 1.864 (1.110, 3.128) | 0.989 (0.312, 3.133) | 0.985 |
| ≥500 JOD (750$) | 52 (25.1%) | 10 (4.8%) | Referent | ||
| Region | 0.029 * | ||||
| Middle Region | 186 (55.5%) | 78 (23.3%) | 2.385 (1.831, 3.106) | 13.285 (1.793, 98.414) | 0.011 * |
| North Region | 34 (10.1%) | 25 (7.5%) | 1.360 (0.811, 2.279) | 7.382 (0.907, 60.096) | 0.062 |
| South Region | 9 (2.7%) | 3 (0.9%) | Referent | ||
| Digital health literacy | 0.000 * | ||||
| Very poor | 35 (10.4%) | 75 (22.4%) | 0.467 (0.312, 0.697) | 0.013 (0.002, 0.112) | 0.000 * |
| Poor | 16 (4.8%) | 6 (1.8%) | 2.667 (1.043, 6.815) | 0.052 (0.004, 0.635) | 0.021 * |
| Acceptable | 38 (11.3%) | 8 (2.4%) | 4.750 (2.216, 10.181) | 0.089 (0.101, 0.816) | 0.032 * |
| Good | 71 (21.2%) | 15 (4.5%) | 4.733 (2.712, 8.261) | 0.082 (0.010, 0.658) | 0.019 * |
| Very good | 69 (2.06%) | 2 (0.6%) | Referent | ||
| Omnibus Tests of Model Coefficients | |||||
| Chi-square | df | Sig. | |||
| Step 1 | Step | 116.632 | 22 | 0.000 | |
| Block | 116.632 | 22 | 0.000 | ||
| Model | 116.632 | 22 | 0.000 | ||
| Model Summary | |||||
| Step 1 | −2 Log likelihood | Cox & Snell R Square | Nagelkerke R Square | ||
| 170.331a | 0.431 | 0.574 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Melhem, S.J.; Nabhani-Gebara, S.; Kayyali, R. Digital Trends, Digital Literacy, and E-Health Engagement Predictors of Breast and Colorectal Cancer Survivors: A Population-Based Cross-Sectional Survey. Int. J. Environ. Res. Public Health 2023, 20, 1472. https://doi.org/10.3390/ijerph20021472
Melhem SJ, Nabhani-Gebara S, Kayyali R. Digital Trends, Digital Literacy, and E-Health Engagement Predictors of Breast and Colorectal Cancer Survivors: A Population-Based Cross-Sectional Survey. International Journal of Environmental Research and Public Health. 2023; 20(2):1472. https://doi.org/10.3390/ijerph20021472
Chicago/Turabian StyleMelhem, Samar J., Shereen Nabhani-Gebara, and Reem Kayyali. 2023. "Digital Trends, Digital Literacy, and E-Health Engagement Predictors of Breast and Colorectal Cancer Survivors: A Population-Based Cross-Sectional Survey" International Journal of Environmental Research and Public Health 20, no. 2: 1472. https://doi.org/10.3390/ijerph20021472
APA StyleMelhem, S. J., Nabhani-Gebara, S., & Kayyali, R. (2023). Digital Trends, Digital Literacy, and E-Health Engagement Predictors of Breast and Colorectal Cancer Survivors: A Population-Based Cross-Sectional Survey. International Journal of Environmental Research and Public Health, 20(2), 1472. https://doi.org/10.3390/ijerph20021472









