The Role of Adaptive Goal Processes in Mental Wellbeing in Chronic Pain
Abstract
1. Introduction
2. Materials and Methods
2.1. Research Design
2.2. Participants
2.3. Measures
2.3.1. Demographic Information
2.3.2. Pain Characteristics
2.3.3. Goal Tenacity and Goal Flexibility
2.3.4. Mental Wellbeing
2.4. Procedure
2.5. Data Analysis
3. Results
3.1. Preliminary Analysis
3.2. Model Testing
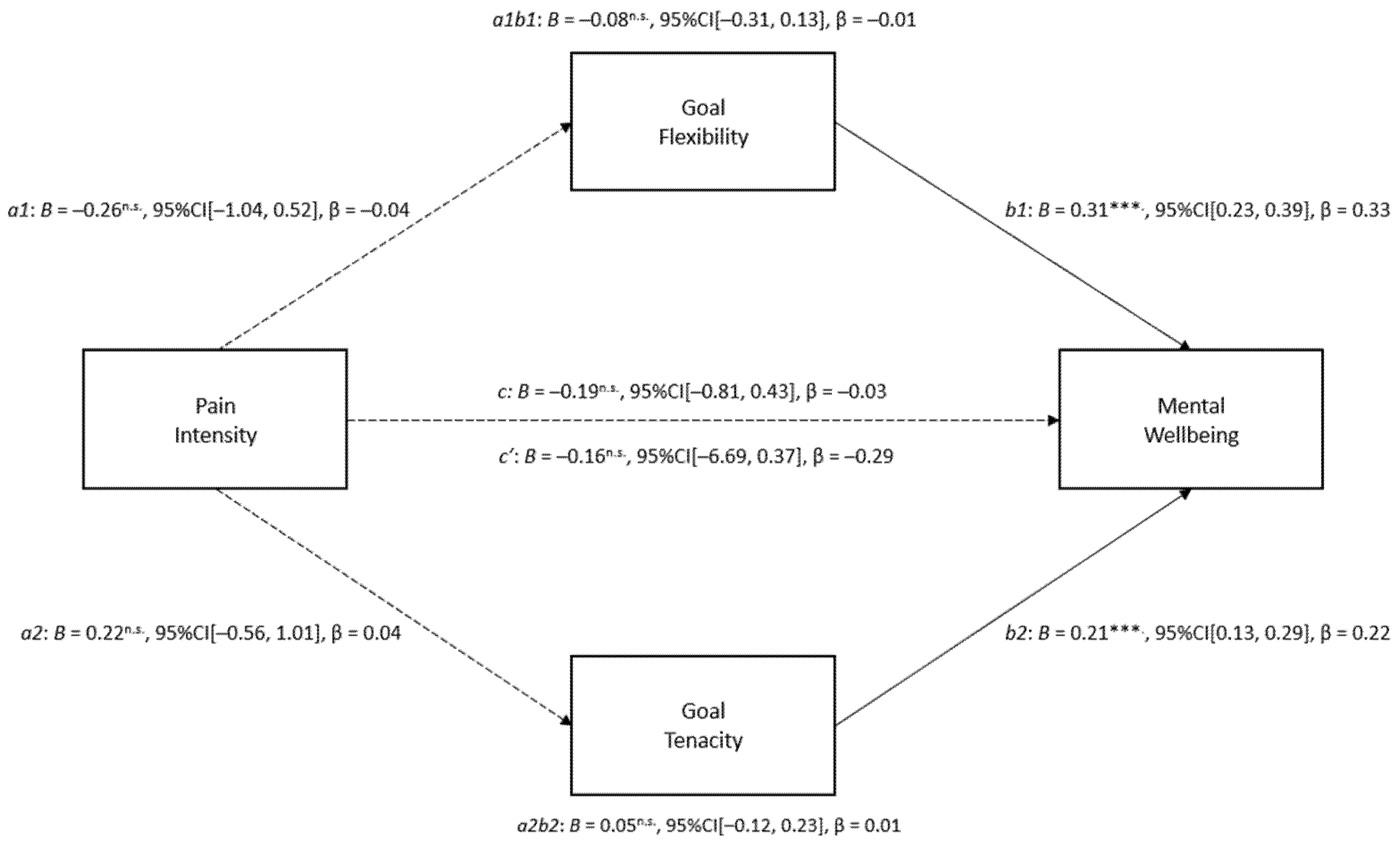
3.2.1. Model One: Pain Intensity, Goal Flexibility and Goal Tenacity, and Mental Wellbeing
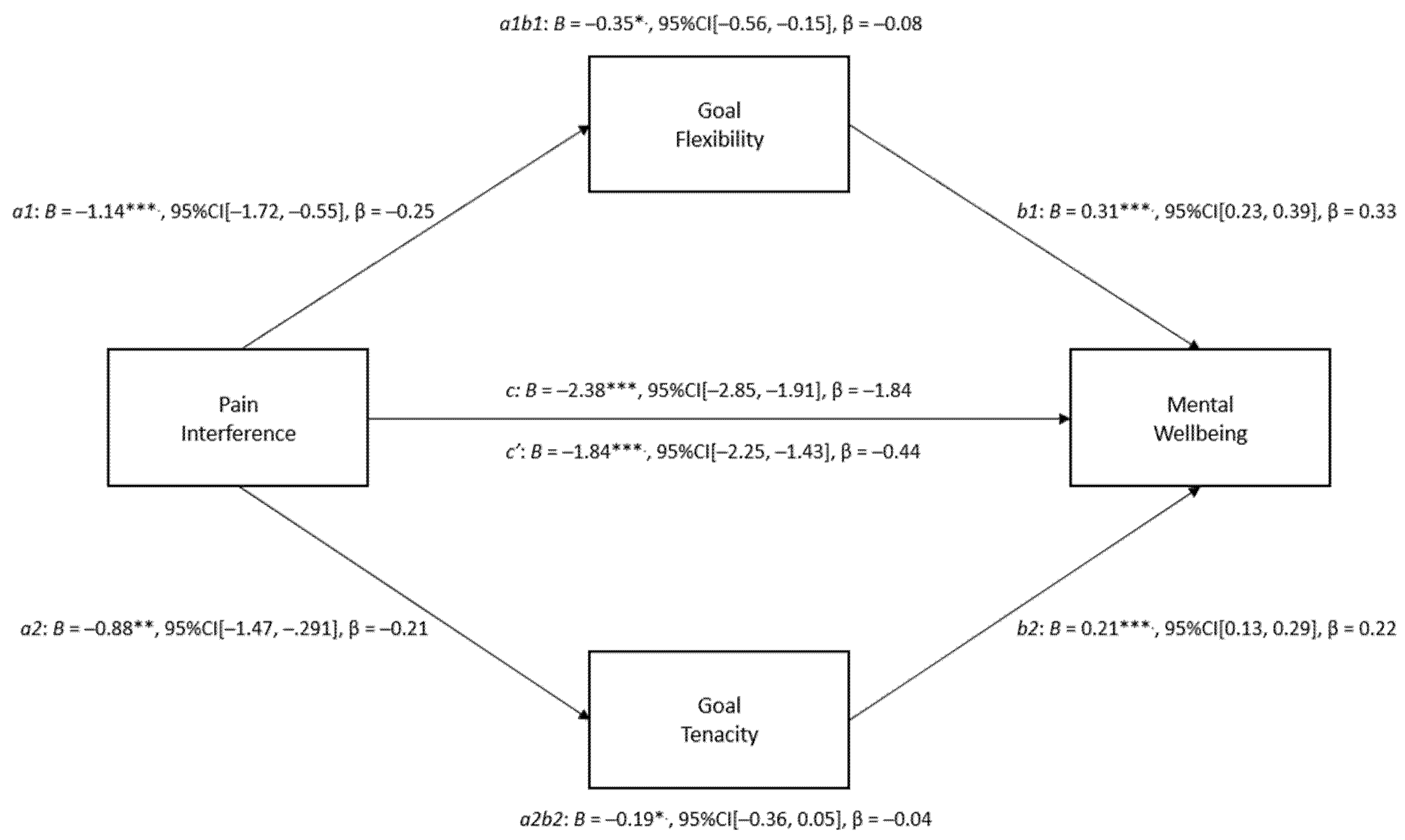
3.2.2. Model Two: Pain Interference, Goal Flexibility and Goal Tenacity, and Mental Wellbeing
4. Discussion
4.1. Implications
4.2. Limitations and Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Merskey, H.; Bogduk, N. Classification of Chronic Pain, 2nd ed.; IASP Press: Seattle, WC, USA, 1994; pp. 209–214. [Google Scholar]
- Henderson, J.V.; Harrison, C.M.; Britt, H.C.; Bayram, C.F.; Miller, G.C. Prevalence, Causes, Severity, Impact, and Management of Chronic Pain in Australian General Practice Patients. Pain Med. 2013, 14, 1346–1361. [Google Scholar] [CrossRef] [PubMed]
- Yong, J.; Mullins, M.; Bhattacharyya, N. Prevalence of chronic pain among adults in the United States. Pain 2022, 163, 328–332. [Google Scholar] [CrossRef] [PubMed]
- Reid, J.; Harker, J.; Bala, M.; Truyers, C.; Kellen, E.; Bekkering, G.E.; Kleijnen, J. Epidemiology of chronic non-cancer pain in Europe: Narrative review of prevalence, pain treatments and pain impact. Curr. Med. Res. Opin. 2011, 27, 449–462. [Google Scholar] [CrossRef] [PubMed]
- Kawai, K.; Kawai, A.; Wollan, P.; Yawn, B.P. Adverse impacts of chronic pain on health-related quality of life, work productivity, depression and anxiety in a community-based study. Fam. Pract. 2017, 34, 656–661. [Google Scholar] [CrossRef] [PubMed]
- Vadivelu, N.; Kai, A.M.; Kodumudi, G.; Babayan, K.; Fontes, M.; Burg, M.M. Pain and Psychology-A Reciprocal Relationship. Ochsner J. 2017, 17, 173–180. [Google Scholar] [PubMed]
- Doorley, J.D.; Greenberg, J.; Bakhshaie, J.; Fishbein, N.S.; Vranceanu, A.-M. Depression explains the association between pain intensity and pain interference among adults with neurofibromatosis. J. Neuro-Oncol. 2021, 154, 257–263. [Google Scholar] [CrossRef] [PubMed]
- Du, S.; Hu, Y.; Bai, Y.; Hu, L.; Dong, J.; Jin, S.; Zhang, H. Emotional distress correlates among patients with chronic nonspecific low back pain: A hier-archical linear regression analysis. Pain Pract. 2019, 19, 510–521. [Google Scholar] [CrossRef]
- Iddon, J.E.; Taylor, P.J.; Unwin, J.; Dickson, J.M. The role of positive goal engagement in increased mental well-being among individuals with chronic non-cancer pain. Br. J. Pain 2019, 13, 230–238. [Google Scholar] [CrossRef]
- Dickson, J.; Moberly, N.; Preece, D.; Dodd, A.; Huntley, C. Self-Regulatory Goal Motivational Processes in Sustained New Year Resolution Pursuit and Mental Wellbeing. Int. J. Environ. Res. Public Health 2021, 18, 3084. [Google Scholar] [CrossRef]
- Landmark, T.; Dale, O.; Romundstad, P.; Woodhouse, A.; Kaasa, S.; Borchgrevink, P.C. Development and course of chronic pain over 4 years in the general population: The HUNT pain study. Eur. J. Pain 2018, 22, 1606–1616. [Google Scholar] [CrossRef]
- Austin, T.; Vancouver, B. Goal constructs in psychology: Structure, process, and content. Psychol. Bull. 1996, 120, 338–375. [Google Scholar] [CrossRef]
- Van Damme, S.; Crombez, G.; Eccleston, C. Coping with pain: A motivational perspective. Pain 2008, 139, 1–4. [Google Scholar] [CrossRef]
- Ramírez-Maestre, C.; Esteve, R.; López-Martínez, A.E.; Serrano-Ibáñez, E.R.; Ruiz-Párraga, G.T.; Peters, M. Goal Adjustment and Well-Being: The Role of Optimism in Patients with Chronic Pain. Ann. Behav. Med. 2019, 53, 597–607. [Google Scholar] [CrossRef]
- Brandtstädter, J.; Renner, G. Tenacious goal pursuit and flexible goal adjustment: Explication and age-related analysis of assimilative and accommodative strategies of coping. Psychol. Aging 1990, 5, 58–67. [Google Scholar] [CrossRef]
- Brandtstädter, J. Goal pursuit and goal adjustment: Self-regulation and intentional self-development in changing develop-mental contexts. Adv. Life Course Res. 2009, 14, 52–62. [Google Scholar] [CrossRef]
- Schmitz, U.; Saile, H.; Nilges, P. Coping with chronic pain: Flexible goal adjustment as an interactive buffer against pain-related distress. Pain 1996, 67, 41–51. [Google Scholar] [CrossRef]
- Roux, L.; Gustin, S.M.; Newton-John, T.R. To persist or not to persist? The dilemma of goal adjustment in chronic pain. Pain 2021, 163, 820–823. [Google Scholar] [CrossRef]
- Arends, R.Y.; Bode, C.; Taal, E.; Van de Laar, M.A. The role of goal management for successful adaptation to arthritis. Patient Educ. Couns. 2013, 93, 130–138. [Google Scholar] [CrossRef]
- Arends, R.Y.; Bode, C.; Taal, E.; Van De Laar, M.A.F.J. The longitudinal relation between patterns of goal management and psychological health in people with arthritis: The need for adaptive flexibility. Br. J. Heal. Psychol. 2016, 21, 469–489. [Google Scholar] [CrossRef]
- Brandstätter, V.; Herrmann, M.; Schüler, J. The struggle of giving up personal goals: Affective, physiological, and cognitive consequences of an action crisis. Personal. Soc. Psychol. Bull. 2013, 39, 1668–1682. [Google Scholar] [CrossRef]
- Crombez, G.; Eccleston, C.; De Vlieger, P.; Van Damme, S.; De Clercq, A. Is it better to have controlled and lost than never to have controlled at all? An experimental investigation of control over pain. Pain 2008, 137, 631–639. [Google Scholar] [CrossRef] [PubMed]
- Brands, I.; Stapert, S.; Wade, D.; Van Heugten, C.; Köhler, S. Life goal attainment in the adaptation process after acquired brain injury: The influence of self-efficacy and of flexibility and tenacity in goal pursuit. Clin. Rehabil. 2014, 29, 611–622. [Google Scholar] [CrossRef] [PubMed]
- Kelly, R.E.; Wood, A.M.; Mansell, W. Flexible and tenacious goal pursuit lead to improving well-being in an aging population: A ten-year cohort study. Int. Psychogeriatr. 2012, 25, 16–24. [Google Scholar] [CrossRef] [PubMed]
- Van Damme, S.; De Waegeneer, A.; Debruyne, J. Do flexible goal adjustment and acceptance help preserve quality of life in patients with multiple sclerosis? Int. J. Behav. Med. 2016, 23, 333–339. [Google Scholar] [CrossRef] [PubMed]
- Cleeland, C. The Brief Pain Inventory User Guide. 2009. Available online: https://www.mdanderson.org/documents/Departments-and-Divisions/Symptom-Research/BPI_UserGuide.pdf (accessed on 20 September 2022).
- Treede, R.D.; Rief, W.; Barke, A. A classification of chronic pain for ICD-11. Pain 2015, 6, 1003–1007. [Google Scholar] [CrossRef]
- Fordyce, W. Pain in cancer and chronic non-cancer conditions: Similarities and differences. Acta Anaesthesiol. Scand. 2001, 45, 1086–1089. [Google Scholar] [CrossRef]
- Fritz, M.S.; Mackinnon, D.P. Required sample size to detect the mediated effect. Psychol. Sci. 2007, 18, 233–239. [Google Scholar] [CrossRef]
- Cleeland, C.S.; Ryan, K.M. Pain Assessment: Global use of the Brief Pain Inventory. Ann. Acad. Med. Singap. 1994, 23, 129–138. [Google Scholar]
- Lapane, K.L.; Quilliam, B.J.; Benson, C.; Chow, W.; Kim, M. One, Two, or Three? Constructs of the Brief Pain Inventory Among Patients With Non-Cancer Pain in the Outpatient Setting. J. Pain Symptom Manag. 2013, 47, 325–333. [Google Scholar] [CrossRef]
- Tennant, R.; Hiller, L.; Fishwich, R. The Warwick-Edinburgh Mental Well-being Scale (WEMBS) development and UK validation. Health Qual. Life Outcomes 2007, 5, 63. [Google Scholar] [CrossRef]
- Lloyd, K.; Devine, P. Psychometric properties of the Warwick–Edinburgh Mental Well-being Scale (WEMWBS) in Northern Ireland. J. Ment. Health 2012, 21, 257–263. [Google Scholar] [CrossRef]
- Swannell, E.R.; Brown, C.; Jones, A.; Brown, R. Some Words Hurt More Than Others: Semantic Activation of Pain Concepts in Memory and Subsequent Experiences of Pain. J. Pain 2016, 17, 336–349. [Google Scholar] [CrossRef]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis a Regression-Based Approach, 1st ed.; The Guildford Press: New York, NY, USA, 2018. [Google Scholar]
- Tabachnick, B.G.; Fidell, L.S. Using Multivariate Statistics, 7th ed.; Pearson: Hoboken, NJ, USA, 2019. [Google Scholar]
- Meints, S.M.; Edwards, R.R. Evaluating psychosocial contributions to chronic pain outcomes. Prog. Neuropsychopharmacol. Biol. Psychiatry 2018, 20, 168–182. [Google Scholar] [CrossRef]
- Carver, S.; Scheier, F. Scaling back goals and recalibration of the affect system are processes in normal adaptive self-regulation: Understanding ‘response shift’ phenomena. Soc. Sci. Med. 2000, 50, 1715–1722. [Google Scholar] [CrossRef]
- Cuff, L.; Fann, J.R.; Bombardier, C.H. Depression, pain intensity, and interference in acute spinal cord injury. Inj. Rehabil 2014, 20, 32–39. [Google Scholar] [CrossRef]
- Gentili, C.; Rickardsson, J.; Zetterqvist, V.; Simons, L.E.; Lekander, M.; Wicksell, R.K. Psychological Flexibility as a Resilience Factor in Individuals With Chronic Pain. Front. Psychol. 2019, 10, 2016. [Google Scholar] [CrossRef]
- Dargan, P.J.; Simm, R.; Murray, C. New approaches towards chronic pain: Patient experiences of a solution-focused pain man-agement programme. Br. J. Pain. 2014, 8, 34–42. [Google Scholar] [CrossRef]
- Simm, R.; Iddon, J.; Barker, C. A community pain service solution-focused pain management programme: Delivery and pre-liminary outcome data. Br. J. Pain. 2014, 8, 49–56. [Google Scholar] [CrossRef]

| Diagnosis | n | % |
|---|---|---|
| Ankylosing Spondylitis | 12 | 2.5 |
| Arthritis | 86 | 17.6 |
| Arthritis type unspecified | 24 | 4.9 |
| Osteoarthritis | 37 | 7.6 |
| Psoriatic Arthritis | 10 | 2.0 |
| Rheumatoid Arthritis | 15 | 3.1 |
| Back Pain | 44 | 9.0 |
| Chronic Regional Pain Syndrome | 11 | 2.2 |
| Complex Regional Pain Syndrome | 14 | 2.9 |
| Ehlers–Danlos Syndrome | 21 | 4.3 |
| Endometriosis | 24 | 4.9 |
| Fibromyalgia | 142 | 29.0 |
| Headaches | 26 | 5.3 |
| Neuropathic Pain | 14 | 2.9 |
| Pelvic Pain | 12 | 2.5 |
| Scoliosis | 10 | 2.0 |
| Other | 73 | 14.9 |
| Variable | Descriptive Statistics | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|---|
| M (SD) | |||||||||
| 1. Formal diagnosis a b | - | - | 0.01 | −0.03 | −0.02 | −0.05 | 0.85 | 0.01 | 0.02 |
| 2. Age | 40.63 (12.31) | - | 0.35 ** | 0.02 | 0.02 | 0.25 ** | −0.04 | 0.15 ** | |
| 3. Time experienced pain (years) | 12.61 (10.18) | - | 0.10 | 0.05 | 0.12 ** | 0.06 | 0.10 | ||
| 4. Pain Intensity | 5.31(1.51) | 0.61 ** | −0.20 ** | −0.09 | −0.38 ** | ||||
| 5. Pain Interference | 6.57 (2.01) | - | −0.27 ** | −0.18 ** | −0.59 ** | ||||
| 6. Goal Flexibility | 44.96 (9.06) | - | 0.32 ** | 0.56 ** | |||||
| 7. Goal Tenacity | 43.75 (8.58) | - | 0.40 ** | ||||||
| 8. Mental Wellbeing | 38.50 (8.41) | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Swindells, T.; Iddon, J.; Dickson, J.M. The Role of Adaptive Goal Processes in Mental Wellbeing in Chronic Pain. Int. J. Environ. Res. Public Health 2023, 20, 1278. https://doi.org/10.3390/ijerph20021278
Swindells T, Iddon J, Dickson JM. The Role of Adaptive Goal Processes in Mental Wellbeing in Chronic Pain. International Journal of Environmental Research and Public Health. 2023; 20(2):1278. https://doi.org/10.3390/ijerph20021278
Chicago/Turabian StyleSwindells, Tara, Joanne Iddon, and Joanne M. Dickson. 2023. "The Role of Adaptive Goal Processes in Mental Wellbeing in Chronic Pain" International Journal of Environmental Research and Public Health 20, no. 2: 1278. https://doi.org/10.3390/ijerph20021278
APA StyleSwindells, T., Iddon, J., & Dickson, J. M. (2023). The Role of Adaptive Goal Processes in Mental Wellbeing in Chronic Pain. International Journal of Environmental Research and Public Health, 20(2), 1278. https://doi.org/10.3390/ijerph20021278







