A Retrospective Longitudinal Analysis of Mental Health Admissions: Measuring the Fallout of the Pandemic
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Boldrini, T.; Girardi, P.; Clerici, M.; Conca, A.; Creati, C.; Di Cicilia, G.; Ducci, G.; Durbano, F.; Maci, C.; Maone, A.; et al. Consequences of the COVID-19 pandemic on admissions to general hospital psychiatric wards in Italy: Reduced psychiatric hospitalizations and increased suicidality. Prog. Neuropsychopharmacol. Biol. Psychiatry 2021, 110, 110304. [Google Scholar] [CrossRef] [PubMed]
- Ambrosetti, J.; Macheret, L.; Folliet, A.; Wullschleger, A.; Amerio, A.; Aguglia, A.; Serafini, G.; Prada, P.; Kaiser, S.; Bondolfi, G.; et al. Impact of the COVID-19 Pandemic on Psychiatric Admissions to a Large Swiss Emergency Department: An Observational Study. Int. J. Environ. Res. Public Health 2021, 18, 1174. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Ramiro, M.; Fico, G.; Anmella, G.; Vázquez, M.; Sagué-Vilavella, M.; Hidalgo-Mazzei, D.; Pacchiarotti, I.; Garriga, M.; Murru, A.; Parellada, E.; et al. Changing trends in psychiatric emergency service admissions during the COVID-19 outbreak: Report from a worldwide epicentre. J. Affect. Disord. 2021, 282, 26–32. [Google Scholar] [CrossRef] [PubMed]
- Rømer, T.B.; Christensen, R.H.B.; Blomberg, S.N.; Folke, F.; Benros, M. Psychiatric Admissions, Referrals, and Suicidal Behavior Before and during the COVID-19 Pandemic in Denmark: A Time-Trend Study. Eur. Psychiatry 2021, 65, 553–562. [Google Scholar] [CrossRef]
- Simpson, S.A.; Loh, R.M.; Cabrera, M.; Cahn, M.; Gross, A.; Hadley, A.; Lawrence, R.E. The Impact of the COVID-19 Pandemic on Psychiatric Emergency Service Volume and Hospital Admissions. J. Acad. Consult. Liaison Psychiatry 2021, 62, 588–594. [Google Scholar] [CrossRef]
- Grimshaw, B.; Chaudhuri, E. Mental-health-related admissions to the acute medical unit during COVID-19. Clin. Med. 2021, 21, 77–79. [Google Scholar] [CrossRef]
- O’Connor, R.C.; Wetherall, K.; Cleare, S.; McClelland, H.; Melson, A.J.; Niedzwiedz, C.L.; O’Carroll, R.E.; O’Connor, D.B.; Platt, S.; Scowcroft, E.; et al. Mental health and well-being during the COVID-19 pandemic: Longitudinal analyses of adults in the UK COVID-19 Mental Health & Wellbeing study. Br. J. Psychiatry 2021, 218, 326–333. [Google Scholar] [CrossRef]
- Rajkumar, R.P. COVID-19 and mental health: A review of the existing literature. Asian J. Psychiatry 2020, 52, 102066. [Google Scholar] [CrossRef]
- Berardelli, I.; Sarubbi, S.; Rogante, E.; Cifrodelli, M.; Erbuto, D.; Innamorati, M.; Lester, D.; Pompili, M. The impact of the COVID-19 pandemic on suicide ideation and suicide attempts in a sample of psychiatric inpatients. Psychiatry Res. 2021, 303, 114072. [Google Scholar] [CrossRef]
- Hawton, K.; Casey, D.; Bale, E.; Brand, F.; Ness, J.; Waters, K.; Kelly, S.; Geulayov, G. Self-harm during the early period of the COVID-19 pandemic in England: Comparative trend analysis of hospital presentations. J. Affect. Disord. 2021, 282, 991–995. [Google Scholar] [CrossRef]
- Job, E.; Steptoe, A.; Fancourt, D. Abuse, self-harm and suicidal ideation in the UK during the COVID-19 pandemic. Br. J. Psychiatry 2020, 217, 543–546. [Google Scholar]
- First Coronavirus Case Reported in Malta. [Internet] Times of Malta 2020. Available online: https://timesofmalta.com/articles/view/first-coronavirus-case-reported-in-malta.776288 (accessed on 28 December 2022).
- [WATCH] Coronavirus: Mandatory Quarantine Introduced against €1000 Fine. [Internet] Maltatoday 2020. Available online: https://www.maltatoday.com.mt/news/national/100934/coronavirus_robert_abela_expected_to_announce_new_measures#.Y67lOHbMK5c (accessed on 28 December 2022).
- [WATCH] All Schools, Childcare Centres to Close for a Week from Tomorrow. [Internet] Maltatoday 2020. Available online: https://www.maltatoday.com.mt/news/national/100955/live_prime_minister_to_announce_new_measures_related_to_coronavirus#.Y68KcnbMK5c (accessed on 28 December 2022).
- Press Release by the Ministry for Education and Employment: The Government Announces Seven Decisions regarding Schools, Educational Institutions and Examinations. [Internet] PR200570en 2020. Available online: https://www.gov.mt/en/Government/DOI/Press%20Releases/Pages/2020/March/28/pr200570en.aspx (accessed on 6 August 2022).
- Statement by the Office of the Deputy Prime Minister and Ministry for Health. [Internet] PR200423en 2020. Available online: https://www.gov.mt/en/Government/DOI/Press%20Releases/Pages/2020/March/22/pr200539en.aspx (accessed on 6 August 2022).
- COVID-19 Transitioning—Standards for Gatherings and Events. [Internet] 2020. Available online: https://deputyprimeminister.gov.mt/en/health-promotion/covid-19/Documents/mitigation-conditions-and-guidances/Standards_Gatherings_And_Mass_Events.pdf (accessed on 6 August 2022).
- COVID-19: Confirmed Patients Who Ignore Isolation Orders to be Fined €10,000. [Internet] 2020. Available online: https://timesofmalta.com/articles/view/covid-19-fines-may-be-increased-up-to-10000.780452 (accessed on 28 December 2022).
- [WATCH] New COVID-19 Restrictions: Schools to Close from Monday Non-Essential Shops and Services to Shut from Thursday. [Internet] Maltatoday 2021. Available online: https://www.maltatoday.com.mt/news/national/108269/prime_minister_to_announce_more_covid19_restrictions#.Y6833XbMK5c (accessed on 28 December 2022).
- Watch: Malta’s Vaccine Certificate Unveiled. [Internet] Times of Malta 2021. Available online: https://timesofmalta.com/articles/view/watch-prime-minister-health-minister-to-hold-press-conference.875911 (accessed on 6 August 2022).
- [WATCH] COVID-19: Vaccinated Contacts to Quarantine for Seven Days, Booster Shots for Elderly in September. [Internet] Maltatoday 2021. Available online: https://www.maltatoday.com.mt/news/national/111322/covid-19-vaccinated-contacts-to-quaratine-for-seven-days-booster-shots-for-elderly-in-september#.Y687aXbMK5c (accessed on 28 December 2022).
- Explained: The New Quarantine Rules Starting Monday. [Internet] Times of Malta 2021. Available online: https://timesofmalta.com/articles/view/explained-the-new-quarantine-rules-starting-monday.924700 (accessed on 28 December 2022).
- [WATCH] Omicron Variant Detected in Malta, from Monday Only Seated Events Allowed. [Internet] Maltatoday 2021. Available online: https://www.maltatoday.com.mt/news/national/114000/health_minister_to_announce_new_measures1#.Y69CCHbMK5c (accessed on 28 December 2022).
- Google. COVID-19 Community Mobility Reports. Available online: https://www.google.com/covid19/mobility/ (accessed on 4 October 2022).
- Hartnett, Y.; Alshurafa, K.; McAndrew, J.; Daly, D.; Alsaffar, M.; Cotter, D.; Cannon, M.; MacHale, S.; Murphy, K.C.; Barry, H. One year of psychiatric presentations to a hospital emergency department during COVID-19. Ir. J. Psychol. Med. 2022, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Zielasek, J.; Vrinssen, J.; Gouzoulis-Mayfrank, E. Utilization of Inpatient Mental Health Care in the Rhineland During the COVID-19 Pandemic. Front. Public Health 2021, 9, 593307. [Google Scholar] [CrossRef] [PubMed]
- Leeb, R.T.; Bitsko, R.H.; Radhakrishnan, L.; Martinez, P.; Njai, R.; Holland, K.M. Mental Health-Related Emergency Department Visits Among Children Aged <18 Years During the COVID-19 Pandemic—United States, January 1–October 17, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1675–1680. [Google Scholar] [PubMed]
- Czeisler, M.É.; Marynak, K.; Clarke, K.E.N.; Salah, Z.; Shakya, L.; Thierry, J.A.M.; Ali, N.; McMillan, H.; Wiley, J.F.; Weaver, M.D.; et al. Delay or Avoidance of Medical Care Because of COVID-19-Related Concerns—United States, June 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1250–1257. [Google Scholar] [CrossRef]
- Luming, L. Challenges and Priorities in Responding to COVID-19 in Inpatient Psychiatry. Psychiatr. Serv. 2020, 71, 624–626. [Google Scholar]
- Schulmeister, P.; Tsoulou Malakoudi, D.; Velasco Monasterio, G.; Alpoegger, M.; Büttner, M.; Chiesa, A.; Hallaouy, S.; Maggio, L.; Perinat, M. Eurobarometer: Resilience and Recovery, Public Opinion One Year into the Pandemic. Directorate General for Communication (DG COMM) of the European Parliament 2021. Available online: https://www.europarl.europa.eu/atyourservice/files/beheard/eurobarometer/2021/spring-2021-survey/report.pdf (accessed on 6 August 2022).
- Doctors’ Face-To-Face Visits down by almost 70 Per Cent. [Internet] Times of Malta 2020. Available online: https://timesofmalta.com/articles/view/doctors-face-to-face-visits-down-by-almost-70-per-cent.830554 (accessed on 26 August 2022).
- Skorburg, J.A.; Yam, J. Is There an App for That?: Ethical Issues in the Digital Mental Health Response to COVID-19. AJOB Neurosci. 2021, 13, 177–190. [Google Scholar] [CrossRef]
- Qian, F.; Hastings, J.F.; Ahmed, R. Overcoming telemental health disparities during the COVID-19 pandemic. Int. J. Qual. Health Care 2021, 33, mzab127. [Google Scholar] [CrossRef]
- Jaffe, D.H.; Lee, L.; Huynh, S.; Haskell, T.P. Health Inequalities in the Use of Telehealth in the United States in the Lens of COVID-19. Popul. Health Manag. 2020, 23, 368–377. [Google Scholar] [CrossRef]
- United Nations High Commissioner for Refugees (UNHCR) Figures at a Glance—Mediterranean Arrivals. [Internet] 2022. Available online: https://www.unhcr.org/mt/figures-at-a-glance (accessed on 3 September 2022).
- Seidel, R.W.; Kilgus, M.D. Agreement between telepsychiatry assessment and face-to-face assessment for Emergency Department psychiatry patients. J. Telemed. Telecare 2014, 20, 59–62. [Google Scholar] [CrossRef]
- O’Reilly, R.; Bishop, J.; Maddox, K.; Hutchinson, L.; Fisman, M.; Takhar, J. Is Telepsychiatry Equivalent to Face-to-Face Psychiatry? Results From a Randomized Controlled Equivalence Trial. Psychiatr. Serv. 2007, 58, 836–843. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Glecia, A.; Kent-Wilkinson, A.; Leidl, D.; Kleib, M.; Risling, T. Transition of Mental Health Service Delivery to Telepsychiatry in Response to COVID-19: A Literature Review. Psychiatr. Q. 2021, 93, 181–197. [Google Scholar] [CrossRef] [PubMed]
- Troyer, E.A.; Kohn, J.N.; Hong, S. Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Neuropsychiatric symptoms and potential immunologic mechanisms. Brain Behav. Immun. 2020, 87, 34–39. [Google Scholar] [CrossRef] [PubMed]
- Raony, Í.; de Figueiredo, C.S.; Pandolfo, P.; Giestal-De-Araujo, E.; Bomfim, P.O.-S.; Savino, W. Psycho-Neuroendocrine-Immune Interactions in COVID-19: Potential Impacts on Mental Health. Front. Immunol. 2020, 11, 1170. [Google Scholar] [CrossRef]
- Lee, J. Mental health effects of school closures during COVID-19. Lancet Child Adolesc. Health 2020, 4, 421. [Google Scholar] [CrossRef]
- Hawrilenko, M.; Kroshus, E.; Tandon, P.; Christakis, D. The Association Between School Closures and Child Mental Health During COVID-19. JAMA Netw. Open. 2021, 4, e2124092. [Google Scholar] [CrossRef]
- Baweja, R.; Brown, S.L.; Edwards, E.M.; Murray, M.J. COVID-19 Pandemic and Impact on Patients with Autism Spectrum Disorder. J. Autism Dev. Disord. 2022, 52, 473–482. [Google Scholar] [CrossRef]
- Oomen, D.; Nijhof, A.D.; Wiersema, J.R. The psychological impact of the COVID-19 pandemic on adults with autism: A survey study across three countries. Mol. Autism 2021, 12, 21. [Google Scholar] [CrossRef]
- Vasa, R.A.; Singh, V.; Holingue, C.; Kalb, L.G.; Jang, Y.; Keefer, A. Psychiatric problems during the COVID-19 pandemic in children with autism spectrum disorder. Autism Res. 2021, 14, 2113–2119. [Google Scholar] [CrossRef]
- Vadivel, R.; Shoib, S.; El Halabi, S.; El Hayek, S.; Essam, L.; Bytyçi, D.G.; Karaliuniene, R.; Teixeira, A.L.S.; Nagendrappa, S.; Ramalho, R.; et al. Mental health in the post-COVID-19 era: Challenges and the way forward. Gen. Psychiatry 2021, 34, e100424. [Google Scholar] [CrossRef]
- Aknin, B.L.; De Neve, J.; Dunn, E.W.; Fancourt, D.E.; Goldberg, E.; Helliwell, J.F.; Jones, S.P.; Karam, E.; Layard, R.; Lyubomirsky, S.; et al. Mental Health During the First Year of the COVID-19 Pandemic: A Review and Recommendations for Moving Forward. Perspect. Psychol. Sci. 2022, 17, 915–936. [Google Scholar] [CrossRef]
- Bourmistrova, N.W.; Solomon, T.; Braude, P.; Strawbridge, R.; Carter, B. Long-term effects of COVID-19 on mental health: A systematic review. J. Affect. Disord. 2022, 299, 118–125. [Google Scholar] [CrossRef]
- Kumar, S.; Veldhuis, A.; Malhotra, T. Neuropsychiatric and Cognitive Sequelae of COVID-19. Front. Psychol. 2021, 12, 577529. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Xu, X.; Chen, Z.; Duan, J.; Hashimoto, K.; Yang, L.; Liu, C.; Yang, C. Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain Behav. Immun. 2020, 87, 18–22. [Google Scholar] [CrossRef] [PubMed]
- Poletti, S.; Palladini, M.; Mazza, M.G.; De Lorenzo, R.; Furlan, R.; Ciceri, F.; Rovere-Querini, P.; Benedetti, F.; Irene, B.; Sara, B.; et al. Long-term consequences of COVID-19 on cognitive functioning up to 6 months after discharge: Role of depression and impact on quality of life. Eur. Arch. Psychiatry Clin. Neurosci. 2021, 272, 773–782. [Google Scholar] [CrossRef] [PubMed]
- Helms, J.; Kremer, S.; Merdji, H.; Clere-Jehl, R.; Schenck, M.; Kummerlen, C.; Collange, O.; Boulay, C.; Fafi-Kremer, S.; Ohana, M.; et al. Neurologic features in severe SARS-CoV-2 infection. N. Engl. J. Med. 2020, 382, 2268–2270. [Google Scholar] [CrossRef]
| Mean Monthly Presentations | Difference | p-Value | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Diagnostic Group | 2019 (SD) | 2020 (SD) | 2021 (SD) | 2019 vs. 2020 (95% CI) | 2019 vs. 2021 (95% CI) | 2020 vs. 2021 (95% CI) | 2019 vs. 2020 | 2019 vs. 2021 | 2020 vs. 2021 |
| Organic disorders | 2.6 (1.62) | 2.9 (1.93) | 4.3 (3.31) | 0.3 (−1.16, 1.83) | 1.7 (−0.47, 3.97) | 1.4 (−1.35, 4.19) | 0.630 | 0.110 | 0.284 |
| Substance-use disorders | 53.8 (8.24) | 47.7 (12.47) | 52.6 (8.99) | −6.1 (−12.74, 0.41) | −1.2 (−6.79, 4.29) | 4.9 (−3.49, 13.33) | 0.063 | 0.629 | 0.225 |
| Schizophrenia, schizotypal and delusional disorders | 17.9 (4.36) | 20.1 (5.14) | 23.8 (5.20) | 2.2 (−2.87, 7.21) | 5.9 (2.80, 9.04) | 3.7 (−1.17, 8.67) | 0.364 | 0.002 | 0.121 |
| Mood disorders | 27.2 (4.59) | 33.8 (13.2) | 42.5 (7.24) | 6.6 (−1.87, 15.21) | 15.3 (9.83, 20.84) | 8.7 (2.88, 17.04) | 0.114 | <0.001 | 0.044 |
| Anxiety disorders | 15.8 (3.59) | 15.0 (5.59) | 20.3 (4.70) | −0.8 (−4.14, 2.47) | 4.5 (1.24, 7.76) | 5.3 (2.02, 8.64) | 0.590 | 0.011 | 0.005 |
| Eating disorders | 0.1 (0.29) | 0.3 (0.62) | 0.8 (1.42) | 0.2 (−0.2, 0.53) | 0.7 (−0.29, 1.62) | 0.5 (−0.50, 1.50) | 0.339 | 0.151 | 0.293 |
| Personality disorders | 6.9 (2.02) | 7.7 (5.16) | 12.6 (6.50) | 0.8 (−3.38, 4.88) | 5.7 (1.52, 9.81) | 4.9 (−1.14, 10.98) | 0.697 | 0.012 | 0.102 |
| Intellectual disability | 3.0 (1.48) | 2.7 (1.72) | 4.3 (2.57) | −0.3 (−1.97, 1.30) | 1.3 (−0.53, 3.20) | 1.6 (−0.20, 3.53) | 0.662 | 0.144 | 0.075 |
| Autism spectrum disorder | 1.5 (1.38) | 1.8 (1.03) | 3.0 (1.86) | 0.3 (−0.73, 1.39) | 1.5 (0.16, 2.84) | 1.2 (−0.10, 2.43) | 0.500 | 0.032 | 0.067 |
| Childhood behavioural and emotional disorders | 2.8 (1.64) | 0.8 (0.97) | 3.0 (2.26) | −2.0 (−3.18, −0.98) | 0.2 (1.84, 2.17) | 2.2 (0.71, 3.79) | 0.002 | 0.858 | 0.008 |
| Mean Monthly Presentations | Difference | p-Value | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Age Group | 2019 (SD) | 2020 (SD) | 2021 (SD) | 2019 vs. 2020 (95% CI) | 2019 vs. 2021 (95% CI) | 2020 vs. 2021 (95% CI) | 2019 vs. 2020 | 2019 vs. 2021 | 2020 vs. 2021 |
| 0–17 | 5.4 (1.44) | 3.3 (1.97) | 5.8 (3.31) | −2.1 (−3.53, −0.64) | 0.4 (−2.26, 0.87) | 2.5 (−0.01, 4.85) | 0.009 | 0.710 | 0.051 |
| 18–29 | 29.8 (5.31) | 32.5 (8.94) | 31 (7.90) | 2.7 (−3.65, 8.98) | 1.2 (−3.05, 5.38) | −1.5 (−6.83, 3.83) | 0.373 | 0.555 | 0.548 |
| 30–39 | 26.7 (5.12) | 30.3 (6.92) | 33.5 (8.42) | 3.6 (−0.86, 8.03) | 6.8 (2.19, 11.48) | 3.2 (−2.76, 9.26) | 0.104 | 0.008 | 0.259 |
| 40–49 | 22.2 (3.16) | 21.3 (7.20) | 22.9 (4.64) | −0.9 (−5.59, 3.92) | 0.7 (−3.01, 4.51) | 1.6 (−3.07, 6.23) | 0.707 | 0.669 | 0.469 |
| 50–59 | 15.3 (3.77) | 14.4 (4.14) | 18 (3.79) | −0.9 (−4.34, 2.50) | 2.7 (−1.25, 6.59) | 3.6 (0.25, 6.92) | 0.567 | 0.162 | 0.037 |
| 60–69 | 7.4 (2.47) | 7.8 (2.69) | 13 (4.69) | 0.4 (−1.22, 2.05) | 5.6 (2.15, 9.02) | 5.2 (1.51, 8.82) | 0.586 | 0.004 | 0.01 |
| 70+ | 5.5 (2.75) | 5.1 (2.94) | 6.3 (2.71) | −0.4 (−2.91, 2.07) | 0.8 (−2.06, 3.72) | 1.3 (−0.99, 3.49) | 0.720 | 0.539 | 0.244 |
| Sex | |||||||||
| Male | 76.7 (7.44) | 79.7 (18.30) | 80.7 (10.55) | 3.0 (−7.35, 13.35) | 4.0 (−1.78, 9.78) | 1 (−8.09, 10.09) | 0.537 | 0.156 | 0.813 |
| Female | 35.7 (7.01) | 35.2 (6.60) | 49.8 (15.46) | −0.5 (−4.37, 3.37) | 14.1 (6.29, 22.05) | 14.6 (5.53, 23.80) | 0.781 | 0.002 | 0.005 |
| Nationality | |||||||||
| Maltese | 89.7 (9.85) | 86.3 (17.20) | 102.8 (19.17) | −3.4 (−12.14, 5.31) | 13.1 (1.74, 24.43) | 16.5 (3.72, 29.28) | 0.407 | 0.028 | 0.016 |
| Non-Maltese | 22.7 (5.02) | 28.7 (6.89) | 27.8 (7.21) | 6.0 (2.17, 9.83) | 5.1 (−0.05, 10.21) | −0.9 (−5.46, 3.63) | 0.005 | 0.052 | 0.666 |
| Admission Status | |||||||||
| Voluntary | 80.8 (8.96) | 78.0 (17.52) | 84.1 (17.33) | −2.8 (−12.80, 7.13) | 3.3 (−5.63, 12.13) | 6.1 (−5.51, 17.68) | 0.544 | 0.437 | 0.273 |
| Involuntary | 31.5 (6.57) | 36.8 (11.33) | 46.4 (9.01) | 5.3 (−4.55, 15.22) | 14.9 (7.37, 22.46) | 9.6 (4.05, 15.12) | 0.260 | 0.001 | 0.003 |
| Mean Monthly Presentations | Difference | p-Value | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 2019 (SD) | 2020 (SD) | 2021 (SD) | 2019 vs. 2020 (95% CI) | 2019 vs. 2021 (95% CI) | 2020 vs. 2021 (95% CI) | 2019 vs. 2020 | 2019 vs. 2021 | 2020 vs. 2021 | |
| NSSI | 5.6 (2.54) | 8.6 (7.33) | 9.0 (4.69) | 3 (−1.76, 7.76) | 3.4 (0.41, 6.43) | 0.4 (−4.83, 5.67) | 0.193 | 0.030 | 0.864 |
| SI | 23.2 (3.79) | 36.1 (13.85) | 44.8 (11.26) | 12.9 (5.21, 20.62) | 21.6 (15.34, 27.83) | 8.7 (2.49, 14.85) | 0.004 | <0.001 | 0.01 |
| SSI | 7.8 (2.08) | 11.3 (5.19) | 13.3 (4.19) | 3.5 (0.01, 6.83) | 5.5 (2.38, 8.62) | 2 (−1.15, 5.32) | 0.050 | 0.003 | 0.184 |
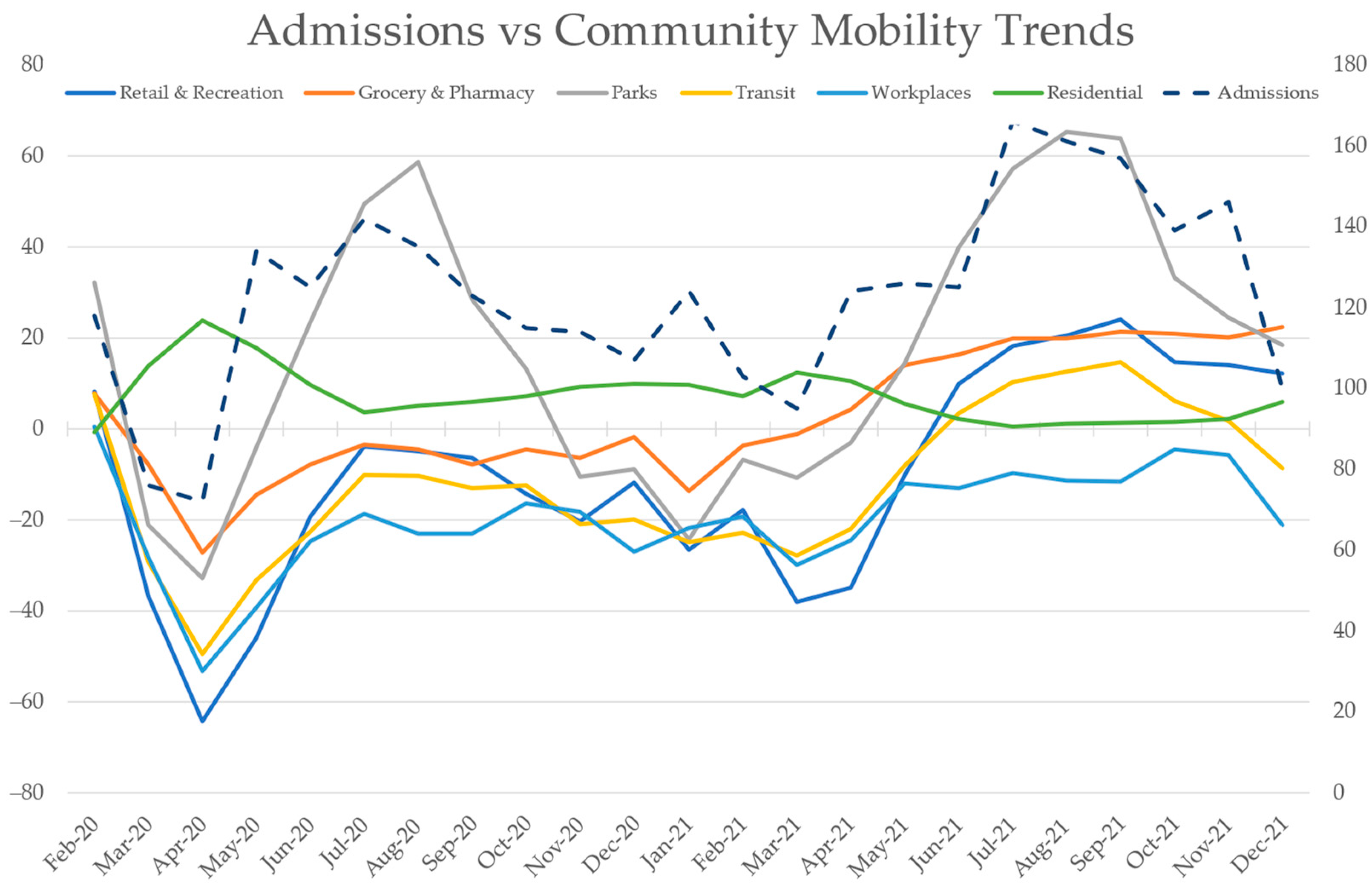
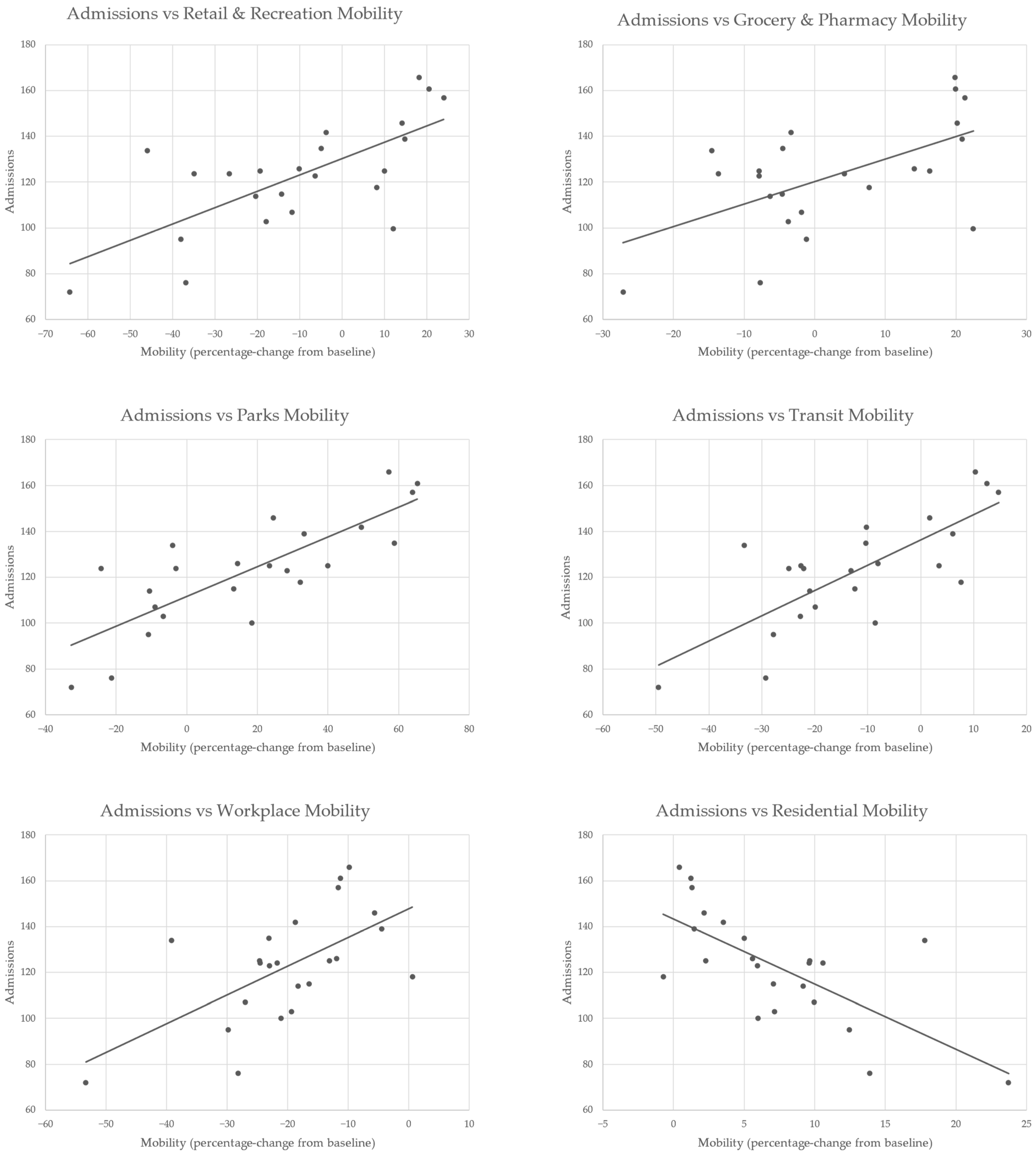
| No. | Mean | SD | Min | Max | r (with Admissions) | p-Value | |
|---|---|---|---|---|---|---|---|
| Admissions | 23 | 122.9 | 24.15 | 72 | 166 | ||
| Retail & Recreation | 23 | −10.2 | 23.64 | −64.3 | 24.0 | 0.699 | <0.001 |
| Grocery & Pharmacy | 23 | 2.7 | 14.13 | −27.1 | 22.5 | 0.577 | 0.004 |
| Parks | 23 | 17.3 | 29.75 | −32.8 | 65.3 | 0.800 | <0.001 |
| Transit | 23 | −12.1 | 16.56 | −49.5 | 14.7 | 0.755 | <0.001 |
| Workplaces | 23 | −19.8 | 11.69 | −53.3 | 0.6 | 0.607 | 0.002 |
| Residences | 23 | 7.2 | 5.95 | −0.7 | 23.7 | −0.699 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Warwicker, S.; Sant, D.; Richard, A.; Cutajar, J.; Bellizzi, A.; Micallef, G.; Refalo, D.; Camilleri, L.; Grech, A. A Retrospective Longitudinal Analysis of Mental Health Admissions: Measuring the Fallout of the Pandemic. Int. J. Environ. Res. Public Health 2023, 20, 1194. https://doi.org/10.3390/ijerph20021194
Warwicker S, Sant D, Richard A, Cutajar J, Bellizzi A, Micallef G, Refalo D, Camilleri L, Grech A. A Retrospective Longitudinal Analysis of Mental Health Admissions: Measuring the Fallout of the Pandemic. International Journal of Environmental Research and Public Health. 2023; 20(2):1194. https://doi.org/10.3390/ijerph20021194
Chicago/Turabian StyleWarwicker, Sean, Denise Sant, Adrian Richard, Jake Cutajar, Annalise Bellizzi, Gertrude Micallef, Daniel Refalo, Liberato Camilleri, and Anton Grech. 2023. "A Retrospective Longitudinal Analysis of Mental Health Admissions: Measuring the Fallout of the Pandemic" International Journal of Environmental Research and Public Health 20, no. 2: 1194. https://doi.org/10.3390/ijerph20021194
APA StyleWarwicker, S., Sant, D., Richard, A., Cutajar, J., Bellizzi, A., Micallef, G., Refalo, D., Camilleri, L., & Grech, A. (2023). A Retrospective Longitudinal Analysis of Mental Health Admissions: Measuring the Fallout of the Pandemic. International Journal of Environmental Research and Public Health, 20(2), 1194. https://doi.org/10.3390/ijerph20021194








