Using Sensor Data to Identify Factors Affecting Internal Air Quality within 279 Lower Income Households in Cornwall, South West of England
Abstract
1. Introduction
2. Materials and Methods
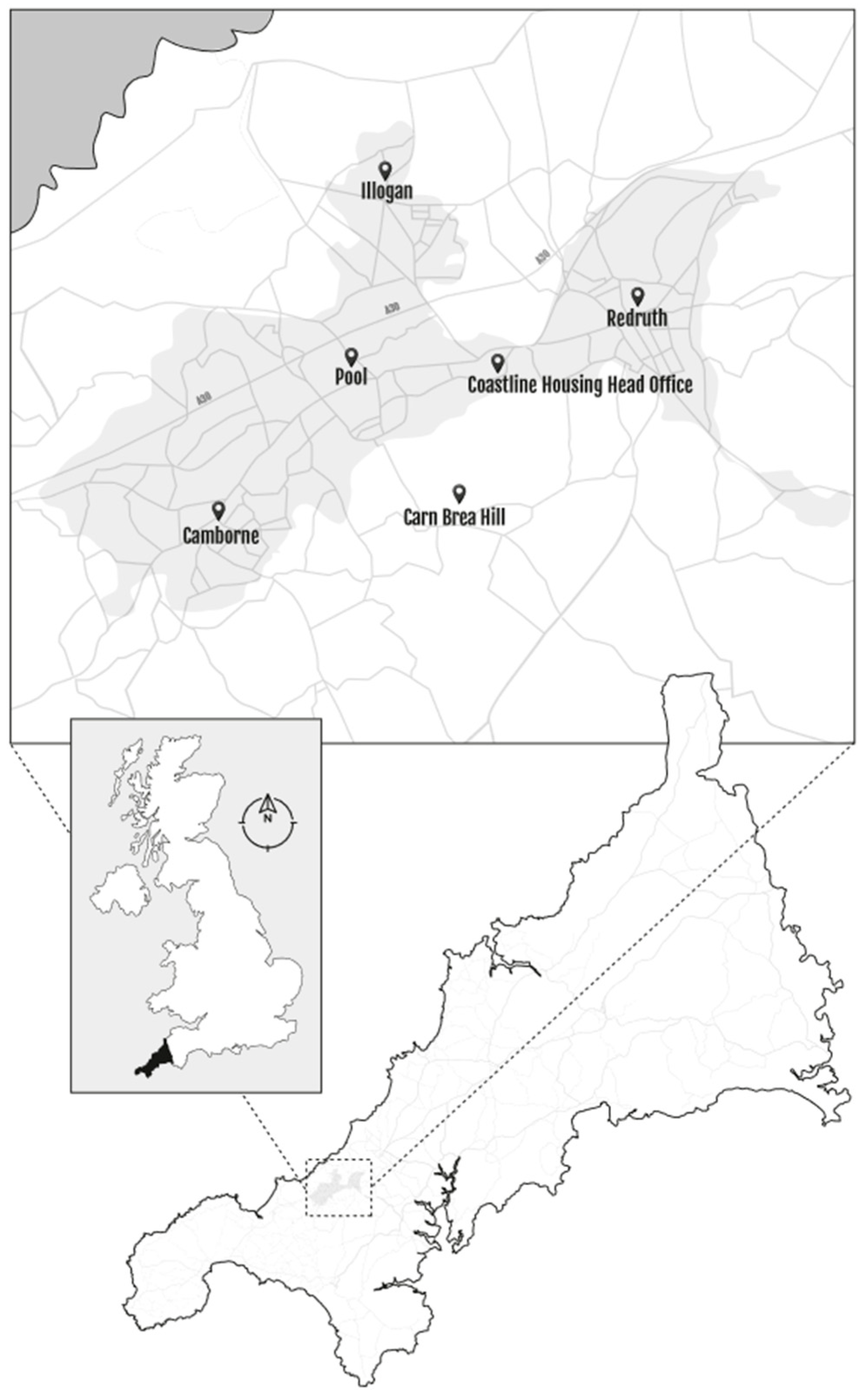
2.1. Context
2.2. Study Participants
2.3. Indoor Sensors
2.4. Behavioural Factors
2.5. Building Characteristics
2.6. Statistical Analyses
3. Results
3.1. Participant and Building Characteristics
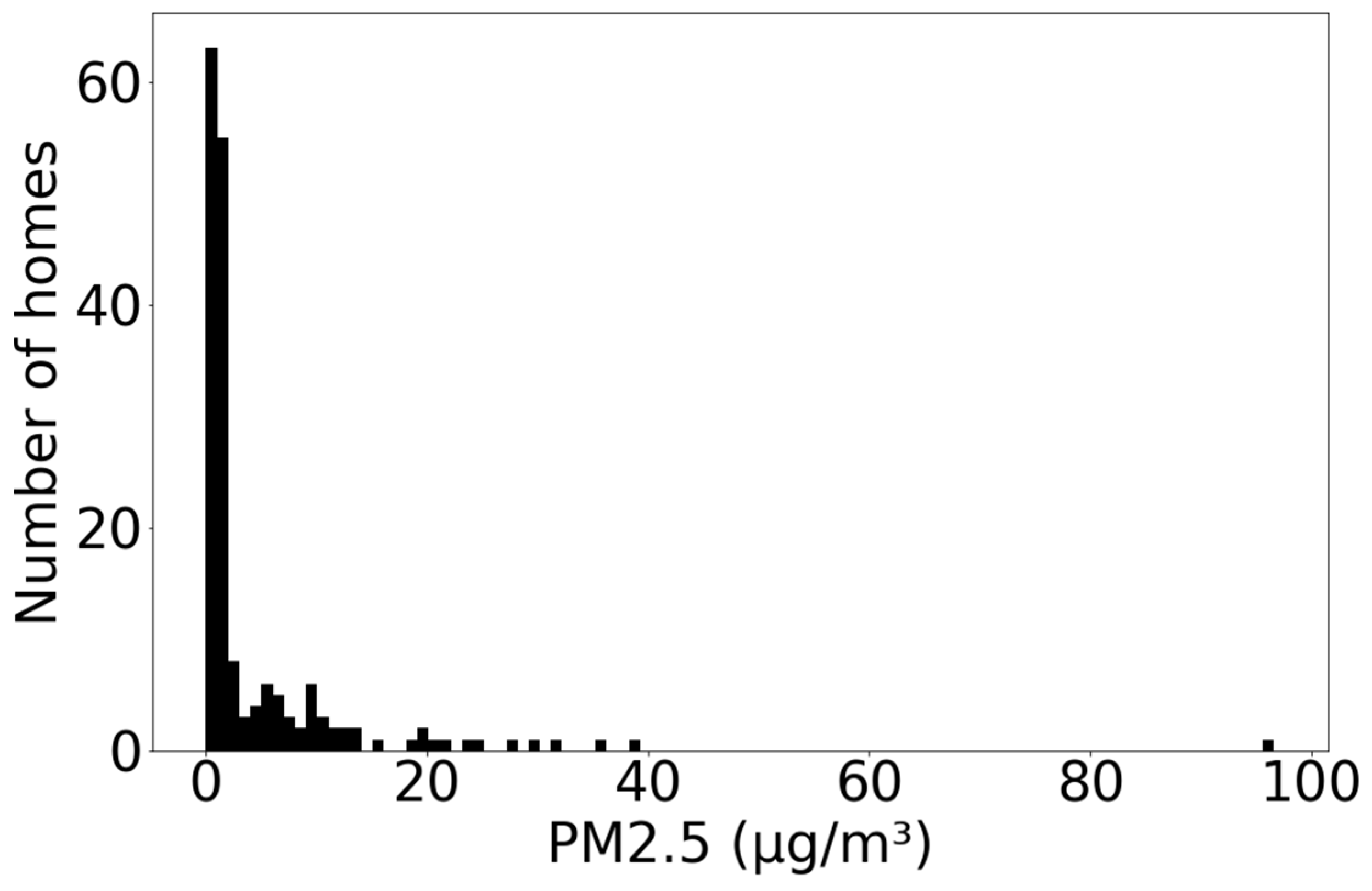
3.2. Association between PM2.5 Concentrations and Behavioural Factors
3.3. Association between PM2.5 Concentrations and Factors Related to the Building
3.4. Association between PM2.5 Concentrations and Factors Related to the Building
3.5. Smoking and Vaping Analysis
4. Discussion
4.1. Factors Influencing Indoor PM
4.2. Indoor PM and Health
4.3. Study Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Burden of Disease from Household Air Pollution for 2012; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Department of Health and Social Care. Chief Medical Officer’s Annual Report 2022—Air Pollution; DHSC: London, UK, 2022.
- Klepeis, N.E.; Nelson, W.C.; Ott, W.R.; Robinson, J.P.; Tsang, A.M.; Switzer, P.; Behar, J.V.; Hern, S.C.; Engelmann, W.H. The National Human Activity Pattern Survey (NHAPS): A resource for assessing exposure to environmental pollutants. J. Expo. Sci. Environ. Epidemiol. 2001, 11, 231–252. [Google Scholar] [CrossRef]
- Conrad, A.; Seiwert, M.; Hünken, A.; Quarcoo, D.; Schlaud, M.; Groneberg, D. The German Environmental Survey for Children (GerES IV): Reference values and distributions for time-location patterns of German children. Int. J. Hyg. Environ. Health 2013, 216, 25–34. [Google Scholar] [CrossRef] [PubMed]
- Matz, C.J.; Stieb, D.M.; Davis, K.; Egyed, M.; Rose, A.; Chou, B.; Brion, O. Effects of age, season, gender and urban-rural status on time-activity: Canadian Human Activity Pattern Survey 2 (CHAPS 2). Int. J. Environ. Res. Public Health 2014, 11, 2108–2124. [Google Scholar] [CrossRef]
- Hussein, T.; Paasonen, P.; Kulmala, M. Activity pattern of a selected group of school occupants and their family members in Helsinki-Finland. Sci. Total Environ. 2012, 425, 289–292. [Google Scholar] [CrossRef]
- Kelly, F. No Threshold Is Safe. Environ. Health News 2021, 36, 20–21. [Google Scholar]
- Sharpe, R.A.; Taylor, T.; Fleming, L.E.; Morrissey, K.; Morris, G.; Wigglesworth, R. Making the Case for “Whole System” Approaches: Integrating Public Health and Housing. Int. J. Environ. Res. Public Health 2018, 15, 2345. [Google Scholar] [CrossRef] [PubMed]
- Abdel-Salam, M.M.M. Indoor particulate matter in urban residences of Alexandria, Egypt. J. Air Waste Manag. Assoc. 2013, 63, 956–962. [Google Scholar] [CrossRef] [PubMed]
- Urso, P.; Cattaneo, A.; Garramone, G.; Peruzzo, C.; Cavallo, D.M.; Carrer, P. Identification of particulate matter determinants in residential homes. Build. Environ. 2015, 86, 61–69. [Google Scholar] [CrossRef]
- BeruBe, K.A.; Sexton, K.J.; Jones, T.P.; Moreno, T.; Anderson, S.; Richards, R.J. The spatial and temporal variations in PM10 mass from six UK homes. Sci. Total Environ. 2004, 324, 41–53. [Google Scholar] [CrossRef]
- Huang, L.; Pu, Z.; Li, M.; Sundell, J. Characterizing the indoor-outdoor relationship of fine particulate matter in non-heating season for urban residences in Beijing. PLoS ONE 2015, 10, e0138559. [Google Scholar] [CrossRef]
- Jeong, C.H.; Salehi, S.; Wu, J.; North, M.L.; Kim, J.S.; Chow, C.W.; Evans, G.J. Indoor measurements of air pollutants in residential houses in urban and suburban areas: Indoor versus ambient concentrations. Sci. Total Environ. 2019, 693, 133446. [Google Scholar] [CrossRef] [PubMed]
- Jones, N.C.; Thornton, C.A.; Mark, D.; Harrison, R.M. Indoor/outdoor relationships of particulate matter in domestic homes with roadside, urban and rural locations. Atmos. Environ. 2000, 34, 2603–2612. [Google Scholar] [CrossRef]
- Tan, C.C.L.; Finney, K.N.; Chen, Q.; Russell, N.V.; Sharifi, V.N.; Swithenbank, J. Experimental Investigation of Indoor Air Pollutants in Residential Buildings. Indoor Built Environ. 2013, 22, 471–489. [Google Scholar] [CrossRef]
- Aquilina, N.J.; Camilleri, S.F. Impact of daily household activities on indoor PM2.5 and Black Carbon concentrations in Malta. Build. Environ. 2022, 207, 108422. [Google Scholar] [CrossRef]
- McCormack, M.C.; Breysse, P.N.; Hansel, N.N.; Matsui, E.C.; Tonorezos, E.S.; Curtin-Brosnan, J.; Williams, D.L.; Buckley, T.J.; Eggleston, P.A.; Diette, G.B. Common household activities are associated with elevated particulate matter concentrations in bedrooms of inner-city Baltimore pre-school children. Environ. Res. 2008, 106, 148–155. [Google Scholar] [CrossRef] [PubMed]
- Ferro, A.R.; Kopperud, R.J.; Hildemann, L.M. Elevated personal exposure to particulate matter from human activities in a residence. J. Expo. Anal. Environ. Epidemiol. 2004, 14, S34–S40. [Google Scholar] [CrossRef]
- Custodio, D.; Pinho, I.; Cerqueira, M.; Nunes, T.; Pio, C. Indoor and outdoor suspended particulate matter and associated carbonaceous species at residential homes in northwestern Portugal. Sci. Total Environ. 2014, 473, 72–76. [Google Scholar] [CrossRef]
- Habre, R.; Coull, B.; Moshier, E.; Godbold, J.; Grunin, A.; Nath, A.; Castro, W.; Schachter, N.; Rohr, A.; Kattan, M.; et al. Sources of indoor air pollution in New York City residences of asthmatic children. J. Expo. Sci. Environ. Epidemiol. 2014, 24, 269–278. [Google Scholar] [CrossRef]
- Madureira, J.; Slezakova, K.; Costa, C.; Pereira, M.C.; Teixeira, J.P. Assessment of indoor air exposure among newborns and their mothers: Levels and sources of PM10, PM2.5 and ultrafine particles at 65 home environments. Environ. Pollut. 2020, 264, 114746. [Google Scholar] [CrossRef]
- Semple, S.; Garden, C.; Coggins, M.; Galea, K.S.; Whelan, P.; Cowie, H.; Sanchez-Jimenez, A.; Thorne, P.S.; Hurley, J.F.; Ayres, J.G. Contribution of solid fuel, gas combustion, or tobacco smoke to indoor air pollutant concentrations in Irish and Scottish homes. Indoor Air 2012, 22, 212–223. [Google Scholar] [CrossRef]
- Stranger, M.; Potgieter-Vermaak, S.S.; Van Grieken, R. Particulate matter and gaseous pollutants in residences in Antwerp, Belgium. Sci. Total Environ. 2009, 407, 1182–1192. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Liu, L.; Xu, C.; Li, N.; Liu, Z.; Wang, Q.; Xu, D. Source apportionment and influencing factor analysis of residential indoor PM2.5 in Beijing. Int. J. Environ. Res. Public Health 2018, 15, 686. [Google Scholar] [CrossRef]
- Zhang, Z.; Gao, Y.; Yuan, Q.; Tan, Y.; Li, H.; Cui, L.; Huang, Y.; Cheng, Y.; Xiu, G.; Lai, S.; et al. Effects of indoor activities and outdoor penetration on PM2.5 and associated organic/elemental carbon at residential homes in four Chinese cities during winter. Sci. Total Environ. 2020, 739, 139684. [Google Scholar] [CrossRef] [PubMed]
- Nishihama, Y.; Jung, C.-R.; Nakayama, S.F.; Tamura, K.; Isobe, T.; Michikawa, T.; Iwai-Shimada, M.; Kobayashi, Y.; Sekiyama, M.; Taniguchi, Y.; et al. Indoor air quality of 5,000 households and its determinants. Part A: Particulate matter (PM2.5 and PM10–2.5) concentrations in the Japan Environment and Children’s Study. Environ. Res. 2021, 198, 111196. [Google Scholar] [CrossRef] [PubMed]
- Fernández, E.; Ballbè, M.; Sureda, X.; Fu, M.; Saltó, E.; Martínez-Sánchez, J.M. Particulate Matter from Electronic Cigarettes and Conventional Cigarettes: A Systematic Review and Observational Study. Curr. Environ. Health Rep. 2015, 2, 423–429. [Google Scholar] [CrossRef]
- Protano, C.; Avino, P.; Manigrasso, M.; Vivaldi, V.; Perna, F.; Valeriani, F.; Vitali, M. Environmental Electronic Vape Exposure from Four Different Generations of Electronic Cigarettes: Airborne Particulate Matter Levels. Int. J. Environ. Res. Public Health 2018, 15, 2172. [Google Scholar] [CrossRef]
- Brown, V.M.; Crump, D.R.; Harrison, P.T.C. Assessing and controlling risks from the emission of organic chemicals from construction products into indoor environments. Environ. Sci. Process. Impacts 2013, 15, 2164–2177. [Google Scholar] [CrossRef]
- Royal College of Physicians. Every Breath We Take: The Lifelong Impact of Air Pollution; Royal College of Physicians: London, UK, 2017. [Google Scholar]
- Ferguson, L.; Taylor, J.; Davies, M.; Shrubsole, C.; Symonds, P.; Dimitroulopoulou, S. Exposure to indoor air pollution across socio-economic groups in high-income countries: A scoping review of the literature and a modelling methodology. Environ. Int. 2020, 143, 105748. [Google Scholar] [CrossRef]
- Shrubsole, C.; Taylor, J.; Das, P.; Hamilton, I.; Oikonomou, E.; Davies, M. Impacts of energy efficiency retrofitting measures on indoor PM2. 5 concentrations across different income groups in England: A modelling study. Adv. Build. Energy Res. 2016, 10, 69–83. [Google Scholar] [CrossRef]
- Ferguson, L.; Taylor, J.; Zhou, K.; Shrubsole, C.; Symonds, P.; Davies, M.; Dimitroulopoulou, S. Systemic inequalities in indoor air pollution exposure in London, UK. Build. Cities 2021, 2, 425. [Google Scholar] [CrossRef]
- Holgate, S.; Grigg, J.; Arshad, H.; Carslaw, N.; Cullinan, P.; Dimitroulopoulou, S.; Greenough, A.; Holland, M.; Jones, B.; Linden, P. The inside story: Health effects of indoor air quality on children and young people. R. Coll. Paediatr. Child Health Lond. 2020. [Google Scholar]
- Abdel-Salam, M.M.M. Seasonal variation in indoor concentrations of air pollutants in residential buildings. J. Air Waste Manag. Assoc. 2021, 71, 761–777. [Google Scholar] [CrossRef] [PubMed]
- Air Quality in England. London Borough of Camden Monitoring Data. Available online: https://www.airqualityengland.co.uk/site/exceedence?site_id=CD009 (accessed on 3 May 2022).
- World Health Organization. Ambient (Outdoor) Air Pollution; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Annesi-Maesano, I. The air of Europe: Where are we going? Eur. Respir. Rev. 2017, 26, 170024. [Google Scholar] [CrossRef] [PubMed]
- Sharpe, R.A.; Thornton, C.R.; Nikolaou, V.; Osborne, N.J. Higher energy efficient homes are associated with increased risk of doctor diagnosed asthma in a UK subpopulation. Environ. Int. 2015, 75, 234–244. [Google Scholar] [CrossRef] [PubMed]
- Sharpe, R.; Machray, K.; Fleming, L.; Taylor, T.; Henley, W.; Chenore, T.; Hutchcroft, I.; Taylor, J.; Heaviside, C.; Wheeler, B. Household energy efficiency and health: Area-level analysis of hospital admissions in England. Environ. Int. 2019, 133, 105164. [Google Scholar] [CrossRef]
- Holgate, S.T. ‘Every breath we take: The lifelong impact of air pollution’—A call for action. Clin. Med. 2017, 17, 8–12. [Google Scholar] [CrossRef] [PubMed]
- Vardoulakis, S.; Dimitroulopoulou, C.; Thornes, J.; Lai, K.-M.; Taylor, J.; Myers, I.; Heaviside, C.; Mavrogianni, A.; Shrubsole, C.; Chalabi, Z. Impact of climate change on the domestic indoor environment and associated health risks in the UK. Environ. Int. 2015, 85, 299–313. [Google Scholar] [CrossRef]
- Paterson, C.A.; Sharpe, R.A.; Taylor, T.; Morrissey, K. Indoor PM2.5, VOCs and asthma outcomes: A systematic review in adults and their home environments. Environ. Res. 2021, 202, 111631. [Google Scholar] [CrossRef]
- Li, S.; Wei, J.; Hu, Y.; Liu, Y.; Hu, M.; Shi, Y.; Xue, Y.; Liu, M.; Xie, W.; Guo, X.; et al. Long-term effect of intermediate particulate matter (PM1–2.5) on incident asthma among middle-aged and elderly adults: A national population-based longitudinal study. Sci. Total Environ. 2023, 859, 160204. [Google Scholar] [CrossRef]
- Block, M.L.; Calderón-Garcidueñas, L. Air pollution: Mechanisms of neuroinflammation and CNS disease. Trends Neurosci. 2009, 32, 506–516. [Google Scholar] [CrossRef]
- Tsoli, S.; Ploubidis, G.B.; Kalantzi, O.-I. Particulate air pollution and birth weight: A systematic literature review. Atmos. Pollut. Res. 2019, 10, 1084–1122. [Google Scholar] [CrossRef]
- Penttinen, P.; Timonen, K.L.; Tiittanen, P.; Mirme, A.; Ruuskanen, J.; Pekkanen, J. Ultrafine particles in urban air and respiratory health among adult asthmatics. Eur. Respir. J. 2001, 17, 428–435. [Google Scholar] [CrossRef] [PubMed]
- Oeder, S.; Jörres, R.A.; Weichenmeier, I.; Pusch, G.; Schober, W.; Pfab, F.; Behrendt, H.; Schierl, R.; Kronseder, A.; Nowak, D. Airborne indoor particles from schools are more toxic than outdoor particles. Am. J. Respir. Cell Mol. Biol. 2012, 47, 575–582. [Google Scholar] [CrossRef]
- Pope, C.A., III; Burnett, R.T.; Thun, M.J.; Calle, E.E.; Krewski, D.; Ito, K.; Thurston, G.D. Lung Cancer, Cardiopulmonary Mortality, and Long-term Exposure to Fine Particulate Air Pollution. JAMA 2002, 287, 1132–1141. [Google Scholar] [CrossRef]
- Cheng, M.; Galbally, I.E.; Molloy, S.B.; Selleck, P.W.; Keywood, M.D.; Lawson, S.J.; Powell, J.C.; Gillett, R.W.; Dunne, E. Factors controlling volatile organic compounds in dwellings in Melbourne, Australia. Indoor Air 2016, 26, 219–230. [Google Scholar] [CrossRef] [PubMed]
- Baxter, L.K.; Clougherty, J.E.; Laden, F.; Levy, J.I. Predictors of concentrations of nitrogen dioxide, fine particulate matter, and particle constituents inside of lower socioeconomic status urban homes. J. Expo. Sci. Environ. Epidemiol. 2007, 17, 433–444. [Google Scholar] [CrossRef] [PubMed]
- Walker, T.; Menneer, T.; Leyshon, C.; Leyshon, M.; Williams, A.J.; Mueller, M.; Taylor, T. Determinants of Volunteering Within a Social Housing Community. VOLUNTAS: Int. J. Volunt. Nonprofit Organ. 2022, 33, 188–200. [Google Scholar] [CrossRef]
- Cornwall Council. Cornwall: A Brief Description (2015); Cornwall Council: Cornwall, UK, 2015. [Google Scholar]
- Cornwall Council. Cornwall Air Quality Action Plan; Cornwall Council: Cornwall, UK, 2020. [Google Scholar]
- London Councils. Demystifying Air Pollution in London; London Councils: London, UK, 2018. [Google Scholar]
- Williams, A.J.; Menneer, T.; Sidana, M.; Walker, T.; Maguire, K.; Mueller, M.; Paterson, C.; Leyshon, M.; Leyshon, C.; Seymour, E.; et al. Fostering Engagement With Health and Housing Innovation: Development of Participant Personas in a Social Housing Cohort. JMIR Public Health Surveill 2021, 7, e25037. [Google Scholar] [CrossRef]
- Ministry of Housing Communities & Local Government. English Housing Survey 2019 to 2020: Social Rented Sector; MHCLG: London, UK, 2021.
- Office for National Statistics. Adult SmokSing Habits in the United Kingdom; ONS: Newport, UK, 2020.
- Menneer, T.; Mueller, M.; Sharpe, R.A.; Townley, S. Modelling mould growth in domestic environments using relative humidity and temperature. Build. Environ. 2022, 208, 108583. [Google Scholar] [CrossRef]
- Menneer, T.; Mueller, M.; Townley, S. A cluster Analysis Approach to Sampling Domestic Properties for Sensor Deployment; European Centre for Environment and Human Health: Truro, UK; College of Engineering, Mathematics and Physical Sciences, University of Exeter: Exeter, UK, 2023; Under Review. [Google Scholar]
- Bell, C. Doogal: Postcodes, Maps and Code. 2019. Available online: https://www.doogal.co.uk/ (accessed on 10 December 2019).
- Google. Google Maps. 2019. Available online: www.google.co.uk/maps/ (accessed on 5 February 2019).
- Department for Business Energy & Industrial Strategy. Standard Assessment Procedure; BEIS: London, UK, 2014. Available online: https://www.gov.uk/guidance/standard-assessment-procedure (accessed on 3 September 2020).
- Dimitroulopoulou, C. Ventilation in European dwellings: A review. Build. Environ. 2012, 47, 109–125. [Google Scholar] [CrossRef]
- Brambilla, A.; Göçer, Ö.; Candido, C. Indoor air quality and early detection of mould growth in residential buildings: A case study. UCL Open Environ. Prepr. 2022, 4, 1–13. [Google Scholar] [CrossRef]
- British Lung Foundation. Lung Disease in the UK—Big Picture Statistics; British Lung Foundation: London, UK, 2016; Available online: https://statistics.blf.org.uk/lung-disease-uk-big-picture (accessed on 11 September 2020).
- Ministry of Housing Communities & Local Government. English Housing Survey 2018: Energy Report; MHCLG: London, UK, 2020.
- Ministry of Housing Communities & Local Government. English Housing Survey 2018 to 2019: Headline Report; MHCLG: London, UK, 2020.
- Office for National Statistics. Population and Household Estimates, England and Wales: Census 2021; ONS: Newport, UK, 2022.
- Department of Health. Towards a Smokefree Generation: A Tobacco Control Plan for England; Department of Health London: London, UK, 2017.
- NHS. Vaping to Quit Smoking. 2022. Available online: https://www.nhs.uk/better-health/quit-smoking/vaping-to-quit-smoking/ (accessed on 23 September 2022).
- Seo, S.; Choung, J.T.; Chen, B.T.; Lindsley, W.G.; Kim, K.Y. The level of submicron fungal fragments in homes with asthmatic children. Environ. Res. 2014, 131, 71–76. [Google Scholar] [CrossRef]
- Sharpe, R.; Thornton, C.; Tyrrell, J.; Nikolaou, V.; Osborne, N. Variable risk of atopic disease due to indoor fungal exposure in NHANES 2005–2006. Clin. Exp. Allergy 2015, 45, 1566–1578. [Google Scholar] [CrossRef] [PubMed]
- Seguel, J.M.; Merrill, R.; Seguel, D.; Campagna, A.C. Indoor Air Quality. Am. J. Lifestyle Med. 2016, 11, 284–295. [Google Scholar] [CrossRef] [PubMed]
- Nazaroff, W.W. Residential air-change rates: A critical review. Indoor Air 2021, 31, 282–313. [Google Scholar] [CrossRef]
- Fu, N.; Kim, M.K.; Chen, B.; Sharples, S. Investigation of outdoor air pollutant, PM2.5 affecting the indoor air quality in a high-rise building. Indoor Built Environ. 2022, 31, 895–912. [Google Scholar] [CrossRef]
- Hiscock, R.; Bauld, L.; Amos, A.; Fidler, J.A.; Munafò, M. Socioeconomic status and smoking: A review. Ann. N. Y. Acad. Sci. 2012, 1248, 107–123. [Google Scholar] [CrossRef]
- Fecht, D.; Fischer, P.; Fortunato, L.; Hoek, G.; de Hoogh, K.; Marra, M.; Kruize, H.; Vienneau, D.; Beelen, R.; Hansell, A. Associations between air pollution and socioeconomic characteristics, ethnicity and age profile of neighbourhoods in England and the Netherlands. Environ. Pollut. 2015, 198, 201–210. [Google Scholar] [CrossRef]

| Variable | Study Participants | Social Rented Sector | National |
|---|---|---|---|
| Age (Years) | 55 | 53 | 54 |
| Gender (Female) | 67.4 | 57.9 | 51 |
| Smokers (%) | 37.51 1 | 28.6 | 14.1 |
| SAP score | 73.21 | 69 | 63 |
| Property type (%) | |||
| House/Bungalow | 48.9 | 56.2 | 79.9 |
| Flat | 51.1 | 43.8 | 20.1 |
| Fuel type (%) | |||
| Gas | 91.1 | 85.8 | |
| Other | 8.9 | 14.2 |
| Variable | n | Mean (Range) | n (%) |
|---|---|---|---|
| Gender of main participant | 258 | ||
| Male | 84 (32.6) | ||
| Female | 174 (67.4) | ||
| Age of main participant | 258 | 55
(19–92) | |
| Property type | 272 | ||
| House/Bungalow | 133 (48.9) | ||
| Flat | 139 (51.1) | ||
| Fuel type | 271 | ||
| Gas | 247 (91.1) | ||
| Other | 24 (8.9) | ||
| SAP score | 224 | 73 (26–86) | |
| Property construction date | 271 | ||
| Pre 1965 | 115 (42.4) | ||
| 1965–1983 | 75 (27.7) | ||
| 1984–2001 | 31 (11.4) | ||
| 2002 onwards | 50 (18.5) | ||
| Number in household | 262 | ||
| 1 | 110 (42.0) | ||
| 2 | 79 (30.2) | ||
| 3 | 34 (13.0) | ||
| 4 or more | 39 (14.9) | ||
| Number of times vacuumed per month | 258 | ||
| Less than once/week | 65 (25.2) | ||
| Between once and twice/week | 48 (18.6) | ||
| More than twice/week but less than once/day | 51 (19.8) | ||
| Once/day or more | 94 (36.4) | ||
| Level of smoking inside house | 260 | ||
| None | 183 (70.4) | ||
| ≤15 times per day | 50 (19.3) | ||
| >15 times per day | 27 (10.4) | ||
| Vaping in property | 279 | ||
| Yes | 41 (14.7) | ||
| No | 238 (85.3) | ||
| Wheeze or cough within household | 279 | ||
| Yes | 107 (38.4) | ||
| No | 172 (61.6) | ||
| Asthma within household | 279 | ||
| Yes | 78 (28.0) | ||
| No | 201 (72.0) | ||
| Chronic bronchitis/Emphysema/COPD within household | 279 | ||
| Yes | 32 (11.5) | ||
| No | 247 (88.5) |
| Variable | n | Mean Indoor PM2.5 | |
|---|---|---|---|
| Mean (SD) | p | ||
| Mean outdoor PM2.5 | 30 | 0.893 (coefficient −0.026) 2 | |
| Level of smoking inside house | 165 | <0.001 (f = 154.826) 3 | |
| None | 121 | 1.08 (1.87) | |
| ≤15 times per day | 26 | 9.20 (2.64) | |
| >15 times per day | 18 | 9.81 (2.03) | |
| Vaping in property | 178 | 0.002 4 | |
| Yes | 26 | 3.95 (2.86) | |
| No | 152 | 1.78 (3.30) | |
| Number of times vacuumed | 164 | 0.154 (f = 1.774) 3 | |
| Less than once/week | 45 | 1.39 (2.70) | |
| Between once and twice/week | 34 | 2.21 (4.69) | |
| More than twice/week but less than once/day | 31 | 1.86 (2.89) | |
| Once/day or more | 54 | 2.31 (3.01) | |
| Number in household | 165 | 0.186 (f = 1.624) 3 | |
| 1 | 75 | 2.26 (3.81) | |
| 2 | 52 | 1.57 (2.89) | |
| 3 | 20 | 2.41 (3.07) | |
| 4 or more | 18 | 1.41 (2.13) | |
| Presence of mould | 163 | 0.776 (f = 0.500) 3 | |
| None | 93 | 2.03 (3.73) | |
| One or two spots | 9 | 1.22 (2.01) | |
| Several small patches (postage stamp) | 11 | 1.51 (2.55) | |
| Bigger than a post card | 10 | 2.49 (2.35) | |
| Up to an arm’s length (1 m) | 18 | 1.79 (2.51) | |
| Bigger than an arm’s length | 22 | 1.89 (2.95) | |
| Distance to A road | 176 | 0.694 (coefficient −0.030) 1 | |
| Fuel type | 174 | 0.841 4 | |
| Gas | 162 | 1.98 (3.30) | |
| Other | 12 | 2.13 (3.33) | |
| Property type | 174 | 0.083 4 | |
| House/Bungalow | 75 | 1.66 (3.19) | |
| Flat | 99 | 2.27 (3.33) | |
| Property construction date | 174 | 0.451 (f = 0.884) 3 | |
| Pre 1965 | 74 | 1.86 (3.15) | |
| 1965–1983 | 48 | 2.48 (2.81) | |
| 1984–2001 | 23 | 1.96 (3.24) | |
| 2002 onwards | 29 | 1.64 (1.49) | |
| SAP score | 143 | 0.705 (coefficient −0.032) 1 | |
| Wheeze/Cough | Asthma | Chronic Bronchitis,
Emphysema or COPD | |||||||
|---|---|---|---|---|---|---|---|---|---|
| n | Odds Ratio (95% CI) | p | n | Odds Ratio
(95% CI) | p | n | Odds Ratio
(95% CI) | p | |
| Mean Indoor PM2.5 | 65 | 1.02
(0.98, 1.06) | 0.350 | 50 | 1.01
(0.97, 1.04) | 0.798 | 19 | 1.07
(0.95, 1.19) | 0.272 |
| Model Outcome: Indoor Annual Mean PM2.5 | Unadjusted Models (From Table 3) | Adjusted Model * | ||||
|---|---|---|---|---|---|---|
| Beta | 95% CI | p | Beta | 95% CI | p | |
| Current smoking level in house | ||||||
| None (ref) | 1 | 1 | ||||
| ≤15 times per day | 8.49 | (6.30, 11.44) | <0.001 | 9.06 | (6.40, 12.82) | <0.001 |
| >15 times per day | 9.05 | (6.39, 12.83) | <0.001 | 11.82 | (7.67, 18.19) | <0.001 |
| Vape in house | ||||||
| No (ref) | 1 | 1 | ||||
| Yes | 2.22 | (1.36, 3.64) | 0.002 | 0.55 | (0.29, 1.07) | 0.593 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Johnes, C.; Sharpe, R.A.; Menneer, T.; Taylor, T.; Nestel, P. Using Sensor Data to Identify Factors Affecting Internal Air Quality within 279 Lower Income Households in Cornwall, South West of England. Int. J. Environ. Res. Public Health 2023, 20, 1075. https://doi.org/10.3390/ijerph20021075
Johnes C, Sharpe RA, Menneer T, Taylor T, Nestel P. Using Sensor Data to Identify Factors Affecting Internal Air Quality within 279 Lower Income Households in Cornwall, South West of England. International Journal of Environmental Research and Public Health. 2023; 20(2):1075. https://doi.org/10.3390/ijerph20021075
Chicago/Turabian StyleJohnes, Christopher, Richard A. Sharpe, Tamaryn Menneer, Timothy Taylor, and Penelope Nestel. 2023. "Using Sensor Data to Identify Factors Affecting Internal Air Quality within 279 Lower Income Households in Cornwall, South West of England" International Journal of Environmental Research and Public Health 20, no. 2: 1075. https://doi.org/10.3390/ijerph20021075
APA StyleJohnes, C., Sharpe, R. A., Menneer, T., Taylor, T., & Nestel, P. (2023). Using Sensor Data to Identify Factors Affecting Internal Air Quality within 279 Lower Income Households in Cornwall, South West of England. International Journal of Environmental Research and Public Health, 20(2), 1075. https://doi.org/10.3390/ijerph20021075






