How Do Health Care Professionals Perceive a Holistic Care Approach for Geriatric Patients? A Focus Group Study
Abstract
1. Introduction
2. The Materials and Methods
2.1. The Project RubiN
2.2. Study Design
2.3. Study Population and Recruitment
2.4. Data Collection
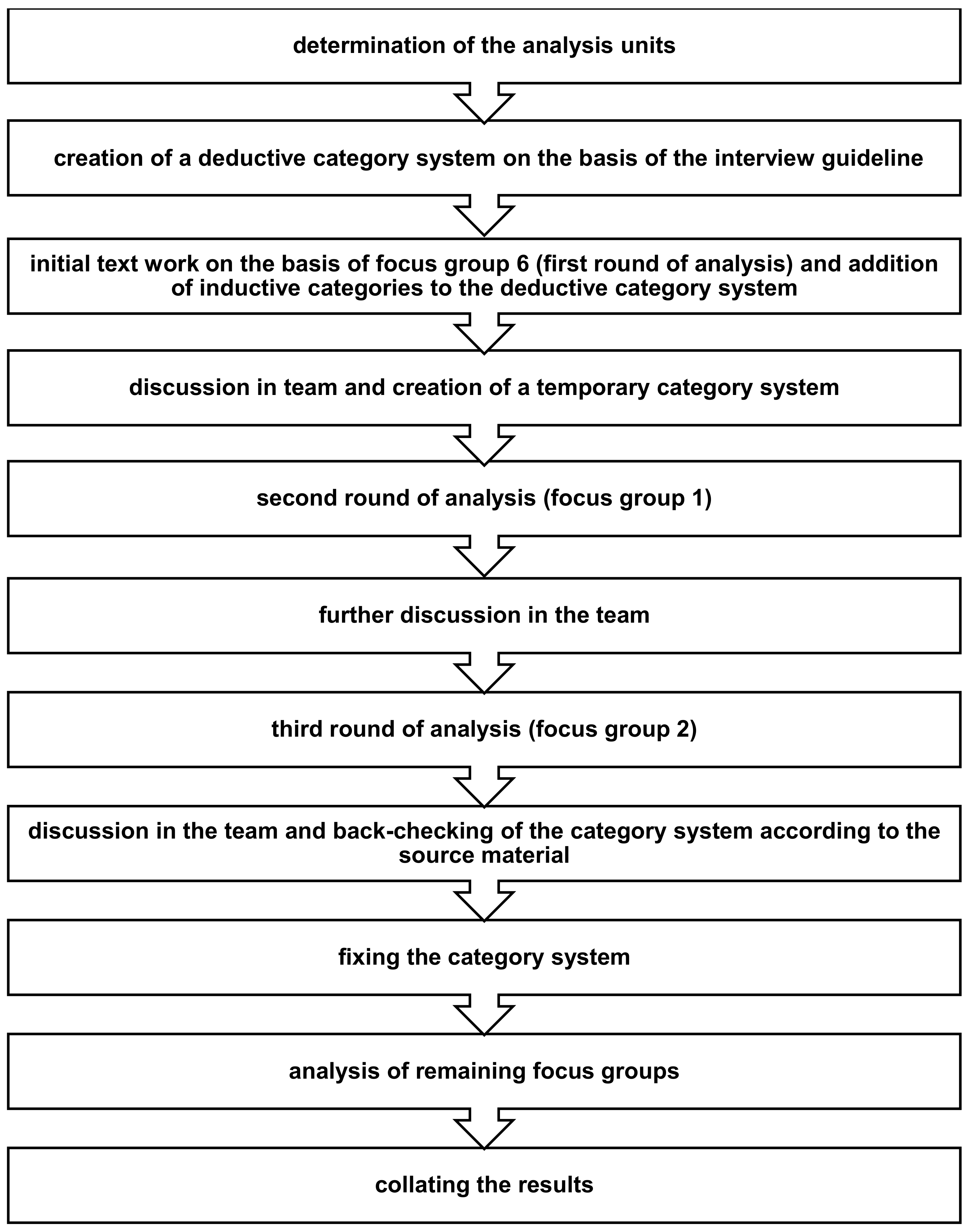
2.5. Data Analysis
2.6. Ethical Approval
3. Results
3.1. Sample Characteristics
3.2. Key Categories
3.3. Subcategory: Insight into Patient’s Living Environment
“In addition, there was a second mainstay of what we could do from a medical perspective. There was somebody who could take a look into the homes. A lot of patients, who might need home visits, or if we say it would make sense, we should go to their home and take a look, we don’t have that time. We have restrictions and we cannot do that. At least, I think that was a big gain from this project, that we got insights in patient’s living environment”.(RubiN_FG6_GP)
“There are many who get dressed up again for the doctor’s office and everything is great and you sit at the doctor’s office and ‘No, no, I’m fine and everything is fine.’ And we come in at home and we see: Okay, it’s not that fine anymore, is it?”(RubiN_FG5_CM)
“You also get to know how the patients are doing, what they are doing and things we didn’t know about”.(RubiN_FG3_HCA)
3.4. Subcategory: Promoting Home Care
“One patient lives alone […] He fell again and again, always came to the clinic. I also made two house visits. The flat was chaotic. It’s not surprising that he fell. Then he only had one cleaning lady who came once a week and by the time we had organized something, he was back in the clinic […] Then I registered him in the RubiN project, then all-round care was organized and since then he has no longer been in the clinic […] now a home help comes and a care service comes once a day and he gets good food and doesn’t eat the moldy things from the fridge and so on”.(RubiN_FG4_CM)
“I make sure that people are cared for at home and are allowed to stay at home to avoid inpatient stays. I believe, that to date, I only had a few patients who were moved to an institution, I think 7 out of over 200 patients. And that’s not a lot”.(RubiN_FG1_CM)
3.5. Subcategory: Quality of Life
“And when you see how happy the patients are and what steps they make, in certain areas, simply because they participate more, then that’s totally awesome”.(RubiN_FG1_CM)
“I also have a 94-year-old patient who lived upstairs for a year, practically locked up on her 1st floor in the apartment, could not go down because she could no longer walk the stairs. And we got her physiotherapy and all sorts of things, together with the general practitioner and now she can walk the stairs again. And that’s easy… And was able to go to a park again and watch her flowers and was super happy”.(RubiN_FG6_CM)
3.6. Subcategory: Patient Satisfaction
“The conversation, well to talk about things that may never have found a place and space. Suddenly, they come to light. And that’s also a form of well-being for the patient. Generally, we want self-determination and stability. And when you are free from circling thoughts, you suddenly feel better. Or to talk to clear their conscience in order to try and change things”.(RubiN_FG2_CM)
“Some patients were just happy, that something new–they were in their daily grind, doesn’t give a lot of variety, or–and we also founded a sports group, and some of them said “Great! Just coming out again, getting new input, someone is coming home”.(RubiN_FG4_CM)
“And then we often get really positive feedback from the patients. That’s nice, it’s going well”.(RubiN_FG9_HCA)
3.7. Subcategory: Feeling of Security
“That’s now a certainty, when you can pour out your heart to someone, and find a trustful level. That’s a feeling of security, if there is someone you can call every time, who is listening to you, is coming to you at home. So that is a very big advantage, I think we have other ways to talk. And that would probably slip through our fingers because we do not go at home and maybe she is not coming to us. Or she is coming, but then everything is a little different. And until we realize that there is a problem, it sometimes takes a little bit longer”.(RubiN_FG6_GP)
“Many single older patients were simply less lonely, less psychologically burdened because of the suggestions of leisure activities, that really was–is just a great help”.(RubiN_FG3_HCA)
“So it is very important for me as a GP that there is also an additional security, of course. That I know that a patient is not only cared for by me, but also by a geriatric coordinator […] because the care of patients is becoming more and more complex, in general. And the demands are increasing overall. And that is also a great help”.(RubiN_FG5_GP)
“So I think it’s nice to work in a team and not to say on your own: Now decide […] but you can exchange ideas together and I think that’s really an enrichment in terms of content, professionally and also mentally, a relief to say: ‘No, we decided together like this, we’ll try it again at home now”.(RubiN_FG7_CM)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Interview Guide for the Multi-Professional Focus Groups
- -
- What does geriatric care usually look like?
- -
- How did you select patients for the RubiN project?
- -
- If a patient agreed to participate in the study, what was the further procedure?
- -
- What changes did participation in the RubiN project lead to in the care of geriatric patients? (Describe concrete changes with an example)
- -
- How do you evaluate the implementation of this care model (RubiN) from your point of view?
- -
- What was good?
- -
- Where do you see a need for improvement?
- -
- How do you feel about working in such a care model? (Satisfaction/dissatisfaction?)
- -
- How far can you imagine offering this type of care to your patients on a permanent basis?
- -
- Which activities should be carried out by the doctor or the doctor’s office?
- -
- Which activities can be taken over by case managers for the care of geriatric patients?
- -
- What else would you like to address that has not yet been discussed?
Appendix B. Illustration of the Process of Qualitative Content Analysis
References
- European Commission. The 2021 Ageing Report: Economic and Budgetary Projections for the EU Member States (2019–2070). Available online: https://ec.europa.eu/info/sites/default/files/economy-finance/ip148_en.pdf (accessed on 20 May 2022).
- Stiel, S.; Krause, O.; Berndt, C.S.; Ewertowski, H.; Müller-Mundt, G.; Schneider, N. Caring for frail older patients in the last phase of life: Challenges for general practitioners in the integration of geriatric and palliative care. Z. Für Gerontol. Und Geriatr. 2020, 53, 763–769. [Google Scholar] [CrossRef] [PubMed]
- Kuhlmey, A.; Dräger, D.; Winter, M.; Beikirch, E. COMPASS—Versichertenbefragung zu Erwartungen und Wünschen an eine qualitativ gute Pflege. Inf. Altersfragen 2010, 37, 4–10. [Google Scholar]
- Golden, A.G.; Tewary, S.; Dang, S.; Roos, B.A. Care management’s challenges and opportunities to reduce the rapid rehospitalization of frail community-dwelling older adults. Gerontologist 2010, 50, 451–458. [Google Scholar] [CrossRef] [PubMed]
- Briggs, A.M.; Valentijn, P.P.; Thiyagarajan, J.A.; Araujo de Carvalho, I. Elements of integrated care approaches for older people: A review of reviews. BMJ Open 2018, 8, e021194. [Google Scholar] [CrossRef] [PubMed]
- Frost, R.; Rait, G.; Wheatley, A.; Wilcock, J.; Robinson, L.; Harrison Dening, K.; Walters, K. What works in managing complex conditions in older people in primary and community care? A state-of-the-art review. Health Soc. Care Community 2020, 28, 1915–1927. [Google Scholar] [CrossRef]
- Deutsche Gesellschaft für Care-und Case-Management. 2021. Available online: www.dgcc.de/case-management/ (accessed on 14 December 2022).
- What Is a Case Manager? Definition of Case Management. Case Management Society of America. 9 September 2020. Available online: https://www.cmsa.org/who-we-are/what-is-a-case-manager/ (accessed on 14 December 2022).
- Sandberg, M.; Jakobsson, U.; Midlöv, P.; Kristensson, J. Case management for frail older people—A qualitative study of receivers’ and providers’ experiences of a complex intervention. BMC Health Serv. Res. 2014, 14, 14. [Google Scholar] [CrossRef]
- Gaertner, B.; Herzog, A.; Holzhausen, M.; Schmidt, S. “Case-Management”—Studien für Personen ab 65 Jahren in Deutschland. Z. Für Gerontol. Und Geriatr. 2015, 48, 529–538. [Google Scholar] [CrossRef]
- Sachverständigenrat zur Begutachtung der Entwicklung im Gesundheitswesen. Kooperation und Verantwortung—Voraussetzung einer Zielorientierten Gesundheitsversorgung—Band I: Sachverständigenrat zur Begutachtung der Entwicklung im Gesundheitswesen. 2007. Available online: https://www.svr-gesundheit.de/fileadmin/Gutachten/Gutachten_2007/Kurzfassung_engl_2007.pdf (accessed on 14 December 2022).
- Sheaff, R.; Boaden, R.; Sargent, P.; Pickard, S.; Gravelle, H.; Parker, S.; Roland, M. Impacts of case management for frail elderly people: A qualitative study. J. Health Serv. Res. Policy 2009, 14, 88–95. [Google Scholar] [CrossRef]
- Saragih, I.D.; Tonapa, S.I.; Lin, C.J.; Lee, B.O. Effects of case management intervention for people with dementia and their carers: A systematic review and meta-analysis of experimental studies. Int. J. Nurs. Stud. 2021, 121, 104012. [Google Scholar] [CrossRef]
- Stokes, J.; Panagioti, M.; Alam, R.; Checkland, K.; Cheraghi-Sohi, S.; Bower, P. Effectiveness of case management for ‘at risk’ patients in primary care: A systematic review and meta-analysis. PLoS ONE 2017, 10, e0132340. [Google Scholar] [CrossRef]
- Low, L.F.; Yap, M.; Brodaty, H. A systematic review of different models of home and community care services for older persons. BMC Health Serv. Res. 2011, 11, 93. [Google Scholar] [CrossRef]
- You, E.C.; Dunt, D.; Doyle, C.; Hsueh, A. Effects of case management in community aged care on client and carer outcomes: A systematic review of randomized trials and comparative observational studies. BMC Health Serv. Res. 2012, 12, 395. [Google Scholar] [CrossRef]
- Berkman, L.F.; Glass, T.; Brissette, I.; Seeman, T.E. From social integration to health: Durkheim in the new millennium. Soc. Sci. Med. 2000, 51, 843–857. [Google Scholar] [CrossRef]
- Di Pollina, L.; Guessous, I.; Petoud, V.; Combescure, C.; Buchs, B.; Schaller, P.; Kossovsky, M.; Gaspoz, J.-M. Integrated care at home reduces unnecessary hospitalizations of community-dwelling frail older adults: A prospective controlled trial. BMC Geriatr. 2017, 17, 53. [Google Scholar] [CrossRef]
- Damery, S.; Flanagan, S.; Combes, G. Does integrated care reduce hospital activity for patients with chronic diseases? An umbrella review of systematic reviews. BMJ Open 2016, 6, e011952. [Google Scholar] [CrossRef]
- Muntinga, M.E.; van Leeuwen, K.M.; Jansen, A.P.D.; Nijpels, G.; Schellevis, F.G.; Abma, T.A. The Importance of trust in successful home visit programs for older people. Glob. Qual. Nurs. Res. 2016, 3, 2333393616681935. [Google Scholar] [CrossRef]
- Götz, K. Qualitative Forschung—Erfahrungen in der Praxis. Gesundh. Und Soz. Z. Für Das Gesamte Gesundh. 2021, 75, 34–39. [Google Scholar]
- Edvardsson, D.; Winblad, B.; Sandman, P.O. Person-centred care of people with severe Alzheimer’s disease: Current status and ways forward. Lancet Neurol. 2008, 7, 362–367. [Google Scholar] [CrossRef]
- American Geriatrics Society Expert Panel on Person-Centered Care. Person-centered care: A definition and essential elements. J. Am. Geriatr. Soc. 2016, 64, 15–18. [Google Scholar] [CrossRef]
- Gloystein, S.; Thomé, F.; Goetz, K.; Warkentin, N.; Mergenthal, K.; Engler, F.; Amelung, V.; Arnold, M.; Freigang, F.; Klähn, A.-K.; et al. RubiN—Continuous care in regional networks: A study protocol for a prospective controlled trial. BMC Geriatr. 2021, 21, 183. [Google Scholar] [CrossRef]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 6, 349–357. [Google Scholar] [CrossRef] [PubMed]
- Bohnsack, R. Rekonstruktive Sozialforschung. Einführung in Qualitative Methoden, 7th ed.; Barbara Budrich: Leverkusen, Germany, 2008. [Google Scholar]
- Krippendorff, K. Content Analysis. An Introduction to Its Methodology, 2nd ed.; Sage: Beverly Hills, CA, USA, 1980. [Google Scholar]
- Forsyth, D.R. Group Dynamics; Wadsworth Cengage learning: Melbourne, Australia, 2013. [Google Scholar]
- Femdal, I.; Solbjor, M. Equality and differences: Group interaction in mixed focus groups of users and professionals discussing power. Soc. Health Vulnerabil. 2018, 9, 1447193. [Google Scholar] [CrossRef]
- ATLAS.ti; Version 8.4.24; Scientific Software Development GmbH: Berlin, Germany, 2020.
- Steinke, I. Gütekriterien qualitativer Forschung. In Qualitative Forschung: Ein Handbuch; Flick, U., von Kardorff, E., Steinke, I., Eds.; Rowohlt: Reinbek, Germany; Hamburg, Germany, 2005; pp. 319–331. [Google Scholar]
- Wilfling, D.; Warkentin, N.; Laag, S.; Goetz, K. “I have such a great care”—Geriatric patients’ experiences with a new healthcare model: A qualitative study. Patient Prefer. Adherence 2021, 5, 309–315. [Google Scholar] [CrossRef] [PubMed]
- Hjelm, M.; Holst, G.; Willman, A.; Bohman, D.; Kristensson, J. The work of case managers as experienced by older persons (75+) with multi-morbidity—A focused ethnography. BMC Geriatr. 2015, 15, 168. [Google Scholar] [CrossRef] [PubMed]
- Sargent, P.; Pickard, S.; Sheaff, R.; Boaden, R. Patient and carer perceptions of case management for long-term conditions. Health Soc. Care Community 2007, 15, 511–519. [Google Scholar] [CrossRef]
- Goetz, K.; Warkentin, N.; Weiss, L.; Kasprick, L. “We are the patients’ advocates”: Care and case managers’ reasons to participate in a geriatric health care project—A qualitative study. Z. Für Evidenz Fortbild. Und Qual. Im Gesundh. 2021, 161, 28–32. [Google Scholar] [CrossRef]
- Warkentin, N.; Wilfling, D.; Laag, S.; Goetz, K. Experiences of family caregivers regarding a community-based care- and case-management intervention. A qualitative study. Health Soc. Care Community 2022, 30, e204–e212. [Google Scholar] [CrossRef]
- Churruca, K.; Pomare, C.; Ellis, L.A.; Long, J.C.; Henderson, S.B.; Murphy, L.E.D.; Leahy, C.J.; Braithwaite, J. Patient-reported outcome measures (PROMs): A review of generic and condition-specific measures and a discussion of trends and issues. Health Expect. 2021, 24, 1015–1024. [Google Scholar] [CrossRef]
- Vidovic, D.; Reinhardt, G.Y.; Hammerton, C. Can social prescribing foster individual and community well-being? A systematic review of the evidence. Int. J. Environ. Res. Public Health 2021, 18, 5276. [Google Scholar] [CrossRef]
- Klaehn, A.K.; Jaschke, J.; Freigang, F.; Arnold, M. Cost-effectiveness of case management: A systematic review. Am. J. Manag. Care 2022, 28, e271–e279. [Google Scholar]
- Mayring, P. Qualitative Content Analysis: Theoretical Foundation, Basic Procedures and Software Solution; Beltz Verlagsgruppe: Klagenfurt, Austria, 2014. [Google Scholar]
| Characteristics | |
|---|---|
| Age in Years, Mean (Standard Deviation) | 46.6 (± 20.5) |
| Gender, Female, n (%) | 37 (80.4) |
| Function in the Medical Practice Network, n | |
| General Practitioners | 15 |
| Health Care Assistants | 14 |
| Case Managers | 17 |
| Years of Working in the Medical Practice Network, n $ | |
| Less Than One Year | 1 |
| One to Five Years | 13 |
| Six to Ten Years | 8 |
| More Than 10 Years | 7 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wilfling, D.; Budke, J.; Warkentin, N.; Goetz, K. How Do Health Care Professionals Perceive a Holistic Care Approach for Geriatric Patients? A Focus Group Study. Int. J. Environ. Res. Public Health 2023, 20, 1033. https://doi.org/10.3390/ijerph20021033
Wilfling D, Budke J, Warkentin N, Goetz K. How Do Health Care Professionals Perceive a Holistic Care Approach for Geriatric Patients? A Focus Group Study. International Journal of Environmental Research and Public Health. 2023; 20(2):1033. https://doi.org/10.3390/ijerph20021033
Chicago/Turabian StyleWilfling, Denise, Jona Budke, Nicole Warkentin, and Katja Goetz. 2023. "How Do Health Care Professionals Perceive a Holistic Care Approach for Geriatric Patients? A Focus Group Study" International Journal of Environmental Research and Public Health 20, no. 2: 1033. https://doi.org/10.3390/ijerph20021033
APA StyleWilfling, D., Budke, J., Warkentin, N., & Goetz, K. (2023). How Do Health Care Professionals Perceive a Holistic Care Approach for Geriatric Patients? A Focus Group Study. International Journal of Environmental Research and Public Health, 20(2), 1033. https://doi.org/10.3390/ijerph20021033